Abstract
Given growing concerns of im/migrant women’s access to sexual and reproductive health (SRH) services, we aimed to (1) describe inequities and determinants of their engagement with SRH services in Canada; and (2) understand their lived experiences of barriers and facilitators to healthcare. Using a comprehensive review methodology, we searched the quantitative and qualitative peer-reviewed literature of im/migrant women’s access to SRH care in Canada from 2008 to 2018. Of 782 studies, 38 met inclusion criteria. Ontario (n = 18), British Columbia (n = 6), and Alberta (n = 6) were primary settings represented. Studies focused primarily on maternity care (n = 20) and sexual health screenings (n = 12). Determinants included health system navigation and service information; experiences with health personnel; culturally safe and language-specific care; social isolation and support; immigration-specific factors; discrimination and racialization; and gender and power relations. There is a need for research that compares experiences across diverse groups of racialized im/migrants and a broader range of SRH services to inform responsive, equity-focused programs and policies.
Keywords: Sexual health, Reproductive health, Immigrant health, Health service access, Health inequities
Introduction
Global migration is escalating, especially among women fleeing humanitarian crises and sexual violence [1–4]. Refugee claims are increasing [5–7], and approximately half of migrants globally are women [8]. Im/migrant women face barriers to health, including insufficient health insurance coverage, discriminatory policies, and inadequate support—yet the structural determinants of im/migrant women’s healthcare access remain poorly understood [9–11], with previous research relying on acculturation, the ‘healthy immigrant effect’, and individual and behavioural explanations for differences among im/migrants [43, 44]. In this study, the term “im/migrant women” includes the diversity of international migrants, refugees, asylum seekers, temporary workers, long-term and recent arrivals, and individuals with and without legal immigration status [12] who self-identify as women (trans-inclusive).
Canada is a key destination for im/migrants globally, who represented 20.6% of its population in 2011, the highest proportion of G8 countries [13]. Im/migrants are projected to represent nearly half of Canada’s population by 2036 [14], continuing to primarily reside in Ontario (32.9%) and British Columbia (BC) (32.3%) [14, 15]. About 20% of women in Canada are im/migrants, most of whom are of reproductive age(15–49 years) and racialized [16, 17], with a projected rise to 27% by 2031 [18]. Women have migrated for reasons including better economic and working conditions, and refuge from hostile and xenophobic policy environments [6, 19]. Despite Canada’s growing im/migrant women population, relatively little is known about their access to and engagement in sexual and reproductive health(SRH) care [20].
Im/migrant women in Canada may face unique migration-related disparities in maternal health care [20–23], pregnancy care [24, 25], mental health support [26–30], contraception [31, 32], sexually transmitted infections (STIs) and HIV testing [33–36], and cervical cancer screening [37–39]; however, diverse migration and SRH experiences, along with varying migrant categorizations, definitions and conceptualizations, make it difficult to compare and draw conclusions to inform policy and practice. Prior reviews of im/migrant health in Canada have infrequently considered gendered inequities in health access [40, 41] such as unequal power dynamics and intimate partner violence. Previous quantitative research has shown differences in perinatal health outcomes across ethnic groups and countries of origin, demonstrating diverse impacts of migration on health [42]. However, there is a need for research to also consider qualitative understandings of women’s lived experiences and the impacts of a wider range of migration experiences (e.g., migration duration, language, immigration status, xenophobia) and types of SRH care.
This analysis was informed by a structural determinants of health approach [46], considering the impacts of macro-structural factors (e.g., policies), im/migration-specific factors (e.g., immigration status, migration duration), health service use and delivery (e.g., system navigation), and individual-level factors (e.g., age, gender) [47] shaping SRH access. This was complemented by intersectionality theory to attend to the cumulative effect of various intersecting forms of marginalization and axes of oppression in influencing health access, such as racism, xenophobia, and ‘othering’ [43–45]. Finally, we drew from frameworks of the multi-staged nature of migrant health [3, 44] to highlight the influence of diverse and complex migration experiences, exposures, and engagement in care in destination, transit, and origin locations. Given gaps in existing research and evidence of SRH inequities among im/migrant women in Canada and globally, this review drew upon 10 years of peer-reviewed literature to (1) describe inequities and determinants of engagement in SRH services among im/migrant women in Canada, and (2) understand their lived experiences of barriers and facilitators.
Methods
Search Strategy
Our search began by exploring SRH inequities faced by im/migrant women globally. As this yielded a large number of records (n = 313), we narrowed our scope to the Canadian context at the final stage of screening using a comprehensive review methodology (see PRISMA diagram [48], Fig. 1). We searched the peer-reviewed literature for qualitative, quantitative and mixed-methods studies describing the determinants and lived experiences of SRH inequities amongst im/migrant women. The review methodology was designed by SM and SG, in consultation with MW; a UBC librarian with specialized skills in systematic reviews also supported development of the search strategy. We searched four databases (Ovid Medline, Social Sciences Citation Index (SSCI), Sciences Citation Index, and CINAHL) using combinations of terms related to SRH, migration, women and research methodologies (Appendix A), subsequently cross-referencing articles and hand-searching to ensure no key studies were missed. These databases were selected based on the scope and topics covered by the comprehensive review. For example, Ovid Medline was selected as an appropriate tool for conducting comprehensive reviews of medical literature, CINAHL for including studies on SRH, migration and women, and SSCI for ensuring coverage of social sciences literature. A limiter was used to identify articles published between 2008 and 2018. Guided by the PRISMA diagram (Fig. 1), we: (1) reviewed titles and abstracts to ensure their relevance to our initial objectives that were globally-focused; (2) reviewed abstracts and narrowed focus to studies describing determinants and lived experiences of SRH access amongst im/migrant women; (3) reviewed full texts to include only Canadian studies.
Fig. 1.
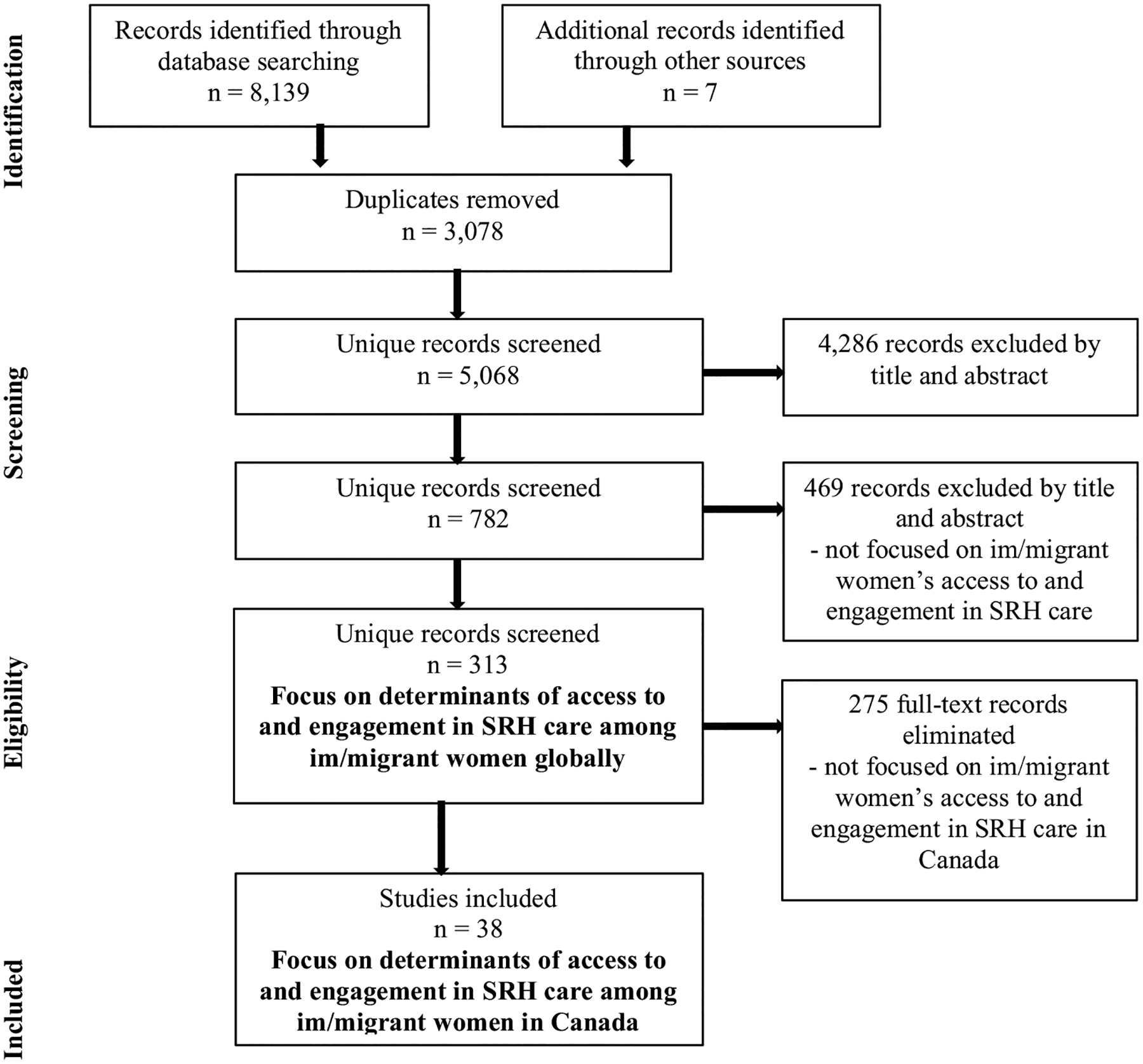
PRISMA Diagram of screening process for studies on determinants of access to and engagement in sexual and reproductive health (SRH) services among im/migrant women in Canada (2008–2018) based on searches in Ovid Medline, Social Sciences Citation Index, Sciences Citation Index, and CINAHL
Inclusion Criteria
Eligible studies at the final stage of screening included primary, peer-reviewed studies that met the following criteria: (i) in English, (ii) published from January 2008 to July 2018, and (iii) focused on im/migrant women’s access to SRH care in Canada. We focused on studies in the last 10 years to ensure relevance to the current im/migration context and provide recent, updated evidence of factors shaping im/migrant women’s SRH access in Canada. Qualitative and quantitative studies were included to capture patterns of SRH service access, such as how often and frequently SRH services were used, as well as determinants of women’s access to and engagement in SRH care. The study population included all im/migrants who self-identify as women (trans-inclusive) of reproductive age, defined by the World Health Organization as 15–49 years. Studies on internal migration and men im/migrants were excluded. Secondary research, grey literature, and studies with no explicit focus on SRH and im/migrant women were also excluded.
Data Extraction and Analysis
Retrieved studies were managed in standard reference management software. We tabulated study characteristics (Table 1) and the following data when available: barrier or facilitator, type of SRH care needed or accessed, qualitative narratives, and epidemiological associations (Appendix B). Tabulated groupings were decided based on similar approaches reported in the literature [49, 50]. We synthesized findings by grouping studies until a comprehensive understanding of key themes (Appendix B) that emerged from both qualitative and quantitative studies was generated. For qualitative studies, we extracted narrative exemplars based on key barriers and facilitators that determined whether and how women accessed SRH care. For quantitative studies, we extracted epidemiological data of relevance to our objectives, such as proportions that described how often and frequently SRH services were accessed, as well as statistical associations (e.g., odds ratios). Finally, we grouped both qualitative and quantitative findings according to determinants of SRH access and engagement amongst im/migrant women in Canada. We interpreted findings considering the various contributions of macro-structural factors, immigration-specific factors, health service use and delivery, and individual-level factors.
Table 1.
Summary of included studies (N = 38) on determinants of access to and engagement in sexual and reproductive health (SRH) services amongst im/migrant women in Canada (2008–2018)
| Type of SRH care | Canadian Province | Study design | Immigration variables | Key findings |
|---|---|---|---|---|
| Ahmad et al. [56] | Ontario | Qualitative | South Asian born in India (68%), Pakistan (27%), and Bangladesh (5%) Mean years lived in Canada: 14.3 |
Social stigma, rigid gender roles, marriage obligations, expected silence, loss of social support, limited knowledge about available resources, myths about partner abuse, and children’s wellbeing delayed help-seeking for GBV. Aspects of HCPs including trust, judgmental, gender, regular inquiries about abuse, and availability of supportive services determined access |
| Alaggia et al. [79] | Ontario | Qualitative | Immigrants and refugees from Punjab, Bengal, South Asia and South America | Barriers to disclosure/reporting GBV: Cultural practices; reluctance of police intervention; isolation; staying for the children; economic barriers; fear of immigration status repercussions Immigration laws and policies contained systemic and structural barriers (e.g., unrealistic criteria required for immigration applications in cases of sponsorship due to IPV) |
| Amankwah et al. [37] | Canada | Quantitative | Chinese, South Asian, Filipino, Other Asian, Black, and Latin American, most of whom lived in Canada for > 10 years | Visible minority women were > 2 × as likely to not get a Pap test. Recent arrivals who did not have a regular doctor were at highest risk for not having a Pap test. Risk AOR for women never having a Pap test: Those living in Canada for < 10 years (AOR 2.2) compared to those living in Canada for > 10 years (AOR 1.1). Not having a regular doctor (AOR 2.8) |
| Chang et al. [52] | British Columbia | Qualitative | Chinese (93.3%) and Taiwanese (7.7%) who migrated in the last 5 years. Lived in Canada for 4–6 years (53.8%) and 1–3 years (46.2%) | Barriers to traditional postpartum practices included a lack of social support, and formal institutional structures. Help from Chinese family members, friends and informed healthcare providers were facilitators. Issues included unregulated/unreliable paid helpers, uninformed/insensitive providers, financial constraints, and structural limitations |
| Donnelly [66] | Canada | Qualitative | Vietnamese Canadian | Challenges included HCPs’ lack of cultural awareness about the private body, patients’ low socioeconomic status, the HCP-patient relationship, and limited institutional support |
| Ganann et al. [65] | Ontario | Quantitative | Immigrants: English and French Canadian, Chinese, South Asian, Jewish, Italian, Portuguese, Other | Immigrant women were significantly more likely to experience fair/poor postpartum health status, higher risk for postpartum depression, and rate community health services as fair/poor (12.2% vs. 3.6%), and were less likely to be able to access care for emotional health problems (5.1% vs. 1.0%) |
| Grewal et al. [53] | British Columbia | Qualitative | Immigrants from Punjab who lived in Canada for 2 years on average | Traditional health beliefs and practices related to the perinatal period included diet, lifestyle, and rituals. The role of family members was important in supporting women during perinatal experiences. Both positive and negative interactions were had with HCPs in the Canadian health system |
| Guruge and Humphreys [70] | Ontario | Qualitative | Sri Lankan Tamil immigrants | Negative GBV support experiences were shaped by services that were unfamiliar, inappropriate, not culturally and linguistically appropriate, uncoordinated, not confidential, and had discriminatory and racist practices |
| Higginbottom et al. [76] | Alberta | Qualitative | Sudanese immigrants who migrated from Sudan, Egypt, and Lebanon in the last 5 years | Pregnancy and delivery were believed to be natural events related to personal agency, without a need for special attention or health interventions. Sub-Saharan culture supported ideology of patriarchy. Pregnancy and birth reflected empowerment for women, which may not have been respected by husbands |
| Higginbottom et al. [80] | Alberta | Qualitative | Immigrant women who spoke Arabic, Urdu, Tagalog, French, Swahili, Hassaniya or Tigriniya | Verbal communication; unshared meaning; non-verbal communication to build relationships based on trust; trauma, culture and open communication determined maternity care experiences, and were impacted by pre-migration histories, cultural factors, accessible healthcare and health outcomes |
| Higginbottom et al. [61] | Alberta | Qualitative | Sudanese (n = 12), Filipino (n = 8), Chinese (n = 6), Colombian (n = 2), n = 1 Tajikistan, India, Mauritania, Pakistan, Eritrea | Accessibility of maternity services was determined by communication barriers, lack of social support, cultural beliefs, lack of information, inadequate health care, and cost of medicines. Determinants of client satisfaction included cultural shock, stereotypes, discrimination, immediate discharge, short consultation time, lack of confidentiality, and lack of consent |
| Hulme et al. [58] | Ontario | Qualitative | Mandarin and Bengali-speaking women | Varied perceptions of risk and preventative health for breast and cervical cancer. Barriers to health system engagement and screening were related to ‘navigating newness’, including transportation, language, time off work, and childcare; fear of screening and cancer; painful or traumatic experiences; access to female providers. Women were generally willing to be screened |
| Jarvis et al. [64] | Quebec | Quantitative | 96% of uninsured women had precarious status; 4% were Canadian citizens; 57.7% were undocumented; 9.9% were visitors or students; 28% were asylum seekers | Uninsured women had fewer prenatal visits than insured women (6.6 vs. 10.7, p = 0.05). Uninsured women presented later in pregnancy and had fewer routine prenatal screening tests. Most uninsured women had inadequate prenatal care utilization (61.9% vs. 11.7%, p < 0.001). There were significant differences in adequacy of services between insured and uninsured women |
| Khadilkar and Chen [82] | Ontario | Quantitative | Recent immigrants (< 10 years) and non-recent immigrants (> 10 years) | Recent immigrant women were less likely to have had a Pap test in the past 3 years than those who were Canadian-born (PR 0.77; 95% CI 0.71, 0.84). Both groups showed similar results for recommended Pap testing intervals. Higher income and level of education, younger age, and being married were independently associated with better Pap testing rates |
| Kingston et al. [51] | Canada | Quantitative | Recent immigrant women (< 5 years) (7.5%), non-recent (> 5 years) (16.3%) and Canadian-born women (76.2%) | Immigrant women were more likely to report high levels of postpartum depression symptoms (13.2% vs. 6.0%), and less likely to have access to social support (74.1% vs. 90% during pregnancy, 67.8% vs. 87.1% during postpartum), and to rate their own/infant’s health as optimal Duration of residence in Canada was a key determinant |
| Lee et al. [54] | Ontario | Qualitative | Women (n = 10) from Hong Kong (n = 3) and Taiwan (n = 2) | Preference for linguistically and culturally competent HCPs, with obstetricians over midwives. Women built strategies to deal with inconveniences of Canada’s healthcare system, and have multiple resources of pregnancy information. Some merits of the Canadian healthcare system, but a need for culturally sensitive care and understandings of Chinese women’s experiences |
| Lofters et al. [73] | Ontario | Quantitative | Global immigrant women who were family sponsored, refugees, economic migrants, and other | Being born in a Muslim-majority country was significantly associated with lower likelihood of being up-to-date on Pap testing after adjustment for region of origin, neighborhood income, and primary care-related factors [ARR 0.93; 95% CI 0.92–0.93]. ARRs were lowest for women with no access to primary care (ARR 0.28; 95% CI 0.27–0.29) |
| Lofters et al. [39] | Ontario | Quantitative | Women were economic migrants (44.3%), family sponsored (40.9%) and refugees (14.2%). 15.1% lived in Canada for < 10 years | Appropriate cervical cancer screening occurred for 61.1% of women. Living in low-income areas was associated with lower rates of cervical cancer screening (ARR 0.88, 95% CI.0.88–0.88) Recent arrival was associated with lower rates (ARR 0.81, 95% CI 0.8–0.81). Cervical cancer screening rate was 53.1% over a 3-year period for immigrant women living in urban areas, lower than expected |
| Logie et al. [57] | Ontario | Quantitative | ACB women living with HIV. Citizens (36%), immigrants (34.8%), asylum seekers (16.8%), refugees (8.1%), undocumented (3.1%) and visa holders (1.2%) | Age was not significantly associated with variables, while income was associated with significantly higher overall quality of life scores, social environments and relationships. Determinants included engagement in and continuity of HIV care, including access, needs-based care, communication with health professionals, and appointment time-keeping |
| Merry et al. [62] | Ontario and Quebec | Qualitative | Asylum seekers from Nigeria, Mexico, India, Colombia, and St. Vincent who lived in Canada for < 2 years | Determinants to postpartum care included isolation; difficulties reaching mothers postpartum; language barriers; low health literacy; lack of psychosocial assessments, support and referrals; and IFHP being limited and confusing |
| Merry et al. [81] | Quebec | Quantitative | Women in Canada for < 5 years. Economic and temporary residents, family sponsored, refugees, asylum seekers, and undocumented | Predictors of unplanned caesareans included being from sub-Saharan Africa/Caribbean (OR 2.37, 95% CI 1.02–5.51) and admission for delivery in early labour (OR 5.43, 95% CI 3.17–9.29). Among women living in Canada for < 2 years (OR 1.77, 95% CI 0.98–3.20), predictors were also being a refugee, asylum seeker, or undocumented (OR 4.24, 95% CI 1.16–15.46) |
| Mumtaz et al. [23] | Alberta, Saskatchewan and Manitoba | Quantitative | Newcomer women (n = 140) included landed immigrants, refugees, students, visitors and temporary workers | Few received information on emotional and physical changes during pregnancy (87% vs. 95%)—more from books (27% vs. 17%) and nurses (20% vs. 13%), and less from family doctors (10% vs. 15%) and friends (10% vs. 20%). Rates of C-sections were higher for newcomers (36.1% vs. 24.7%), who were also less likely to report “very satisfied” with care |
| Ng and Newbold [75] | Ontario | Qualitative | No participant socio-demographic information | Determinants of prenatal care included language; cultural sensitivity and type of care; complexity of delivering care; cultural awareness; provider type; and level of professionalism |
| Newbold and Willinsky [71] | Ontario | Qualitative | No participant socio-demographic information | Barriers to family planning and reproductive health care included language; role of gender in decision-making; misconceptions or a lack of knowledge about family planning; and cultural sensitivity. There were complexities in experiences with professional and non-professional interpreters, and HCP misunderstandings about other cultures |
| Ochoa and Sampalis [69] | Quebec | Qualitative | Permanent residents (n = 11), asylum seekers (n = 10), citizens (n = 1), denied refugee status (n = 2), tourists (n = 1). Lived in Canada for 2–3 years (32%), 6–12 months (24%), 4–5 years (24%) | HIV/STI care experiences characterised by uncertainty, deception and fraud, and included family separation and discrimination. Risk was related to unequal gendered power Vulnerability was determined by experiences across the life course; migratory status; sexual and occupational abuse; language barriers; a lack of social support; and ability to access health services |
| O’Mahony and Donnelly [26] | Canada | Qualitative | Non-European immigrant and refugee women living in Canada for < 10 years | Immigration policy and gender roles were key barriers to postpartum care. Structural barriers, including precarious status and emotional and economic dependence sometimes left women vulnerable and disadvantaged in protecting themselves against postpartum depression |
| O’Mahony et al. [28] | Canada | Qualitative | Women from Central and South America, China, Middle East, and South Asia, and lived in Canada for < 2 years (n = 14), 2–5 years (n = 9), and 6–10 years (n = 7) | Determinants of postpartum depression and seeking for support and treatment included cultural influences (e.g., meaning of postpartum depression, community beliefs), socioeconomic influences (e.g., seeking employment, workplace discrimination), and spiritual and religious beliefs. Social stigma determined decision-making about health practices and coping |
| Pelaez et al. [74] | Quebec | Qualitative | HCPs serving newly arrived im/migrant women No socio-demographic information on im/migrant women | Barriers to maternity care were related to HCP expectations and communication and access to appropriate care. This was influenced by background and social positions and how HCPs balanced women’s needs with the perceived requirement to adhere to standard procedures and regulations |
| Redwood-Campbell et al. [68] | Ontario | Qualitative | Newly immigrated (living in Canada for < 5 years) women and Canadian-born women who spent 0.5–16 years in Canada | Determinants of cervical cancer screening: Knowledge gaps and needs; attitudes towards screening; role of HCPs and health system; culture. Women indicated a strong need for information on screening, and had positive feelings about being proactive. Some differences regarding preferences for female clinicians, which was a higher priority than language |
| Reitmanova and Gustafson [78] | Newfoundland and Labrador | Qualitative | Immigrant Muslim women. Some were Canadian citizens | Women experienced discrimination, insensitivity and a lack of knowledge about religious and cultural practices by providers in accessing pregnancy care, labour and delivery, and postpartum care. Barriers to emotional support and culturally and linguistically appropriate information were further complicated by adjustments associated with immigration |
| Sou et al. [59] | British Columbia | Quantitative | Migrant sex workers from China (76.9%), U.S. (3.8%), and Philippines (2.2%). 41.8% moved to Canada in the last 5 years | Structural determinants of inconsistent condom use included servicing in formal indoor venues (OR 0.17, 95% CI 0.07–0.41), sex work as primary source of income (OR 0.26, 95% CI 0.09–0.76) and difficulty accessing condoms in the workplace (OR 4.75, 95% CI 1.49–15.15). These were independently correlated with increased odds of inconsistent condom use |
| Sou et al. [60] | British Columbia | Quantitative | 10.5% of women were recent im/migrants (< 5 years) and 13.8% were long-term im/migrants (> 5 years) at baseline | In the final model, recent immigration (AOR 3.23, 95% CI 1.93–5.40), long-term immigration (AOR 1.90, 95% CI 1.22–2.96), police harassment including arrest (AOR 1.57; 95% CI 1.15–2.13), and lifetime abuse/trauma (AOR 1.45, 95% CI 1.05–1.99) remained significantly and independently associated with elevated odds of unmet health needs in the last 6 months |
| Vahabi and Lofters [67] | Ontario | Qualitative | Muslim landed immigrants and Canadian citizens from Iran, Pakistan and India. Lived in Canada for > 10 years (n = 18, 60%), 5–9 years (n = 5, 17%), 0–4 years (n = 7, 23%) | Barriers to cervical cancer screening included beliefs and health practices of home countries; limited knowledge about guidelines; a lack of culturally appropriate health information and knowledge about the Canadian health system; access to female physicians; language and ethnic mismatch; long wait times; access to transportation, and time constraints |
| Vanthuyne et al. [77] | Quebec | Quantitative | HCPs and service providers serving immigrant populations No socio-demographic information of im/migrant women |
Some HCPs perceived uninsured migrants as “deserving” of universal access to healthcare, while most viewed those uninsured as “undeserving” of free care. For most, the right to healthcare for immigrants with precarious status was perceived as a “privilege” |
| Vigod et al. [29] | Ontario | Quantitative | Immigrant women (13% refugees, over 50% from Asia). 40% migrated in the last 5 years, 30% 5–10 years ago, and 32% over 10 years ago | Compared to long-term residents, im/migrant women were less likely to use postpartum mental health services (14.1% vs 21.4%, OR 0.60, 95% CI 0.59–0.61). Hospitalization risk was similar and did not change much after adjusting for variables/covariates. 19.4% used mental health services within 1 year postpartum |
| Wiebe [72] | British Columbia | Quantitative | Women born in 75 different countries—38.1% born in Asia and 46.6% born in Canada | Immigrant women presenting for abortion were less likely to be using hormonal contraception when they got pregnant (12.5% vs 23.5%, P < .0.001), had more negative attitudes towards it (62.6% vs 51.6%, P < 0.003), and reported more barriers (24.8% vs 15.3%, P < 0.001). Those who spent more time in Canada were more likely to have similar responses to Canadian-born women |
| Wilson-Mitchell and Rummens [63] | Ontario | Quantitative | South Asian mothers who were asylum seekers, Canadian born and landed immigrants, temporary workers, and visitors | Most uninsured women received less than adequate prenatal care. Over 50% received inadequate prenatal care and 6.5% received none. Uninsured mothers experienced more C-sections due to abnormal fetal heart rates. The number of prenatal visits reported for the uninsured group (mean = 6.04, t = − 6.173, α = 0) was significantly lower than for the insured (mean = 8.70) |
| Winn et al. [55] | Alberta | Qualitative | HCPs providing care for refugee women No socio-demographic information of im/migrant women | Key barriers to maternity care included language, navigating the health system, and culture. Strategies to manage barriers included team-based approaches to care, service coordination, paying out of pocket, and donations to provide care for uninsured. Federal funding cuts left many without coverage, and further strained limited resources |
Results
Our search yielded 782 studies describing SRH inequities faced by im/migrant women globally to determine eligibility, of which we excluded 469 after reviewing abstracts. We hand-reviewed full-texts of 313 potentially eligible studies that focused on access to and engagement in SRH care for im/migrant women globally (Fig. 1). Of 38 Canadian studies that met inclusion criteria, most were conducted in Ontario (n = 18), followed by BC (n = 6), Alberta (n = 6), Quebec (n = 5), Saskatchewan (n = 1), Manitoba (n = 1), and Newfoundland and Labrador (n = 1). Most studies did not differentiate between im/migration categories, and characterized participants as “immigrant women”, “newcomers”, or by ethnicity and/or religion (n = 28). Where immigration status was specified, most studies focused on sponsored refugees and asylum seekers (n = 17); others included temporary workers and students (n = 7), permanent residents (n = 5), visitors (n = 5), family sponsored (n = 3), and undocumented women (n = 3). Only two studies recruited participants below the age of 20 [37, 51].
Of 38 studies, 23 were qualitative and 15 were quantitative (Table 1). No mixed-methods studies met our inclusion criteria. Most studies focused on maternity care (n = 20), followed by sexual health screenings (cervical cancer, HIV/STI) (n = 12), contraception (n = 3), and gender-based violence (GBV) support (n = 3) (Appendix B). While all studies discussed barriers faced by im/migrant women, only seven identified facilitators [52–58].
Our findings are organized by eight determinants of SRH access and engagement, which we identified by grouping and categorizing key barriers and facilitators highlighted in each study (Appendix C): (i) health system navigation and access to SRH service information; (ii) positive and negative experiences with health personnel; (iii) availability of culturally safe care; (iv) language barriers and availability of language-specific care; (v) social isolation and support; (vi)immigration-specific factors; (vii) stigma, discrimination and racialization; and, (viii) gender inequities and power relations. We synthesized quantitative data (e.g., descriptive statistics, odd ratios) to understand determinants of SRH care access, and synthesized narratives and themes reported in qualitative studies to understand inequities and lived experiences of barriers and facilitators to SRH services faced by im/migrant women. Although eligibility included all im/migrants who self-identified as women, few studies specified gender identities [59, 60].
Determinants of SRH Access and Engagement
Our analysis found that existing literature on im/migrant women’s access to and engagement in SRH care in Canada has primarily focused on health service use and delivery, and less on macro-structural and immigration-specific factors.
Health System Navigation and Access to SRH Service Information
Nineteen studies described links between health system navigation challenges and limited access to maternity care [23, 54, 55, 61–65], sexual health screenings (cervical cancer [37, 39, 58, 66–68], HIV/STIs [69]), GBV support [56, 70], and contraception [71, 72].
Qualitative and quantitative studies described the Canadian health system as inconvenient and inadequate due to institutional health system barriers, including challenges finding a family doctor, long wait times, quick hospital discharges, limited and confusing health insurance coverage, and high costs [37, 55, 58, 61, 64, 66, 74]. In a Quebec study, a permanent resident accessing HIV/STI testing during pregnancy explained, “We signed up for a family doctor[…] four years ago, and they still have not called me[…] I had already had two miscarriages and I had a baby with a high-risk pregnancy and I am still waiting”(p. 421) [69]. While few studies described greater access to women providers in Canada compared to home countries [54], accessing women doctors was reported as a key barrier [37, 38, 55, 58, 65–68, 74, 75] for providers, as well as im/migrant women who expressed discomfort with men physicians [55, 58, 66, 75]. Government-funded provincial health insurance influenced access to sexual health screenings and maternity care in several studies [39, 55, 62–64]. In Ontario, for example, rates of cervical cancer screening were low among low-income im/migrant women with health insurance for the last 10 years (31.0%) compared to high-income women who lived in Ontario longer (70.5%) [39].
Health system differences between countries of origin and Canada, as well as limited availability of SRH service information, were common concerns and often limited uptake [56, 61, 63, 76]. Some women feared hospital-based deliveries in Canada, believing caesarean sections were the preferred method of delivery [73], and others’ unfamiliarity with Canadian guidelines for cervical cancer screening determined whether they accessed this service. However, women expressed the desire to learn and made recommendations to raise awareness of available services and health information, such as electronic annual reminders for routine cervical cancer screening, information sessions on available services and referral requirements, and resource booklets [68].
Positive and Negative Experiences with Health Personnel
Sixteen qualitative and quantitative studies identified negative experiences with HCPs for racialized im/migrants– notably judgmental attitudes, insensitive care, and violations of privacy and consent—as barriers to maternity care [52, 53, 55, 61, 62, 73, 75–78], cervical cancer screening [58, 66], HIV/STI [60] testing, GBV support [56, 70], and family planning [71].
Violations of privacy and consent were reported across qualitative studies [61, 66, 69, 70] and negatively impacted healthcare experiences. A woman in Newfoundland & Labrador explained, “I asked nurses if they can knock before they enter so I can get dressed. I also put a sign on the door but they didn’t respect it. This man came and saw me. I was very upset and crying” (p. 106) [78]. In a situation where consent had not been appropriately obtained due to inadequate translation support and rushed interactions, patients who were unclear of the conditions of consent still underwent a procedure [61]. An HCP in Alberta noted, “You’re trying to offer them an operation for what you feel are correct reason[s], so whether they understand English or don’t […] their consent is perhaps not optimal in a stressful situation.” (p. 9) [61].
Unequal power dynamics between providers and patients were also shown to strongly influence im/migrant women’s SRH experiences, and sometimes prevented women from asking for critical health information [66]. Encouragingly, in Ontario and BC, experiences with HCPs were often perceived as culturally safe, supporting im/migrant women’s engagement in maternity care [52, 53, 55], GBV support [56], and sexual health screenings (cervical cancer [58], HIV [57]). In a quantitative study with African, Caribbean and Black im/migrant women living with HIV, tailored, needs-based care and clear communication were positively associated with enhanced quality of life and increased engagement in and continuity of care [57].
Where available, providers with specialized training and experience in refugee health described active, im/migrant-sensitive referrals and collaboration with settlement organizations as critical for facilitating patient engagement with SRH services. In Alberta, HCPs described tailored knowledge of refugee needs and culturally safe models of maternity care, highlighting the ways in which they endeavoured to address complex structural factors influencing im/migrant women’s health access (e.g., transportation, knowledge of available services, language issues [55]). Other HCPs reflected on their unfamiliarity with im/migrant health and expressed a desire for increased training in culturally safe and im/migrant-specific care [55].
Availability of Culturally Safe Care
Eleven studies identified disparities in culturally safe services as barriers to maternity care [26, 28, 54, 63, 65, 73], contraception [71, 72], sexual health screenings (cervical cancer [67], HIV/STI [69]), and GBV support [70]. Socio-cultural differences in SRH norms between home countries and Canada, including gender expectations, sexuality, GBV, and mental health, had profound impacts on access to and engagement in SRH services [26, 66–68, 75]. Community stigma limited knowledge of available GBV support as related discussions were ‘taboo’ and avoided [56]. Anticipated stigma around mental illness in the context of pregnancy was also commonly described as a challenge related to accessing support [26, 74]. Some experienced negative interactions with physicians from the same culture due to fears of confidentiality violations or negative assumptions [66, 67], whereas seeing doctors of the same culture facilitated conversations around SRH for others [67]. A woman accessing cervical cancer screening in Ontario explained how her appearance led to preconceived assumptions: “I’m wearing hijab but maybe I am sexually active so they should not assume.” (p.8) [67].
Language Barriers and Availability of Language-Specific Care
Fourteen studies identified language barriers and disparities in language-specific services as barriers to maternity care(54,63,65), sexual health screenings (cervical cancer [37, 58, 66], HIV/STI [57, 69]), GBV support [70], and family planning [71].
Several studies described the availability of interpretation services as critical to address language barriers faced by different communities of im/migrant women, and highlighted challenges associated with different modalities (e.g., phone, in-person) [54, 55, 63, 69–71, 77, 78]. These included limited time and resources, potentially limited knowledge of medical terminology among interpreters, and concern of stigma or breaches in confidentiality by interpreters with shared cultural backgrounds or communities [63, 70, 71, 77, 78]. An HCP described time constraints: “When you’re in the delivery and there’s an acute situation, and you’ve got to do a vacuum or the obstetrics[…], sometimes there’s not time to go get the language line phone, and then be put on hold, having to have a back and forth conversation translated, back to do you understand what the risks are…” (p. 6) [55]. Although analyses of interpretation services in the context of HIV/STI care were limited, a Quebec study found that im/migrant women often brought members of their social network to appointments when translation services were unavailable; however, this sometimes led to confidentiality issues within smaller communities [69].
Conversely, some women felt that a wide range of SRH services expanded options for language-specific care and enhanced engagement. A Chinese woman in Ontario explained, “My OB didn’t provide me with much pregnancy related information. The nurse[…] can only speak English[…] I can get similar information from the community health centre.”(p. 5) [54]
Social Isolation and Support
Twelve studies identified social isolation as a barrier to maternity care [51, 52, 61, 62, 78], GBV support [56, 79], and sexual health screenings (HIV/STI [69]) attributed to disconnections from family, friends, and community due to migration [56]. Quantitative studies found that im/migrant women were less likely than their Canadian-born peers to have access to social support during pregnancy (74.1% vs. 90%) and postpartum (67.8% vs. 87.1%) [51]. Isolation among im/migrant women experiencing postpartum depression (PPD) also commonly limited health access [51, 52, 62, 78]. Qualitative studies found that social isolation enhanced im/migrant women’s vulnerability to GBV, and providers and advocates explained that immigration policies created significant challenges in reporting GBV for women who lacked social support. For example, in addition to written reports from police or medical services, immigration officials required women to be “settled” in Canada [79]. However, given challenges related to isolation and other factors, an immigration lawyer in Ontario explained, “They have to be these “super women”, so despite being abused, they have to have worked throughout the abuse,[…] established an extensive social network and community ties,[…] it’s a little unrealistic.”(p. 338) [79]. On a positive note, few studies found that support from family members, friends, providers and community organizations mitigated language barriers and fear through accompaniment for appointments and emotional support, enhancing access to healthcare for some [52, 53, 58].
Immigration-Specific Factors
Thirteen studies identified pre-migration experiences, immigration status, and migration duration as determinants of access to maternity care [26, 62–64, 74, 80, 81], sexual health screenings (cervical cancer [37, 73, 82], HIV/STIs [69]), contraception [72], and GBV support [79].
Few studies highlighted differences in SRH access based on immigration status [64, 69, 73], where permanent residents had greater access to services and asylum seekers and undocumented women faced additional barriers [69]. A quantitative study found that compared to insured women, uninsured undocumented women had fewer routine screening tests (93.7% vs. 100%, p = 0.045) and presented later in pregnancy (25.6 vs. 12.0 weeks, p < 0.001) [64]. Asylum seekers and refugees have access to government programmes in Canada, whereas undocumented individuals are somewhat ‘invisible’ in the eyes of the government and healthcare system. Additionally, while some services for asylum seekers are covered by Canada’s Interim Federal Health Program (IFHP) there remain numerous disparities, including pre-approval required from Immigration, Refugees and Citizenship Canada (IRCC) to access some mental health services, impeding access to needed care upon arrival [62]. Qualitative studies found that fear of negative consequences related to having precarious immigration status (i.e. status marked by the absence of rights and entitlements normally associated with permanent residence and citizenship), such as deportation and family separation, prevented women from accessing SRH support [80]. An undocumented woman experiencing PPD explained, “I don’t have insurance. It’s been nine months that I have given birth[…] I need a pap smear but I just don’t have support. I don’t have papers[…] I don’t have the money[…]” (p. 719) [26]. HCPs echoed similar concerns, including high costs of services for those without health insurance [74].
Migration duration also influenced im/migrant women’s access to SRH care [37, 60, 72, 82] where some studies demonstrated improvements in SRH access over integration in Canada [60, 82], while others showed additional barriers for recently arrived im/migrant women. A BC study found that the odds of unmet health needs were highest for recent im/migrants(AOR 3.23, 95% CI 1.93–5.40) [long-term im/migrants (AOR 1.90, 95% CI 1.22–2.96)] [60], while others found that that recent im/migrants (< 10 years in Canada) were at higher risk for never having a Pap test (AOR 2.2) than long-term im/migrants (AOR 1.1) [37], and less likely to have had a Pap test in the past three years (PR 0.77, 95% CI 0.71–0.84) [82] compared to Canadian-born women.
Stigma, Discrimination and Racialization
Eight studies described how experiences of racism, xenophobia, and discrimination based on gender and religion limited im/migrant women’s access to maternity care [26, 61, 78], GBV support [56, 70], and HIV/STI services [60, 69].
A Quebec study with HCPs providing care for uninsured pregnant im/migrant women (N = 237) found that most believed they were “undeserving” of healthcare due to xenophobic and discriminatory perceptions of im/migrants, and an unwillingness to provide care for those with precarious status [77]. Negative interactions with HCPs reported across studies were often due to racial or religious prejudice and resulted in inadequate care, incomplete assessments and culturally unsafe approaches [58, 62, 66, 74, 75, 78]. In a study of asylum seekers, a participant explained, “Here they say that there is no discrimination, well this is the easiest way to be discriminated against, because you have no status. In all situations, you need to take out your papers and they see that you are not a tourist, nor are resident, you are nothing.” (p. 419) [69].
GBV survivors reported that racialization, stigma and shame from community, family members [56] and HCPs [66, 70] often delayed access to support. Narratives of HCPs in some studies reflected discriminatory, or ‘othering’ attitudes towards im/migrants from particular immigration classes or regions of origin: “mostly refugees, I think they come to Canada and [expect] everything to be given to them[…] some of them are very demanding[…] They are all quite easy except for the [ethnic group name]” (p. 10) [68]. One study found that HCPs perceived discrimination to be an instinctive response, as opposed to a structural issue [66], while others were more sensitive to racism and xenophobia faced by im/migrant women, and used approaches that were culturally safe and patient-centered [61].
Gender Inequities and Unequal Power Relations
Five qualitative studies showed that gender inequities undermined access to maternity care [83], sexual health screenings (HIV/STI [60, 69]), GBV support [56], and family planning [71]. Across studies, gender norms related to women’s status and social positioning strongly shaped access to and engagement in SRH care. Studies demonstrated that unequal gendered power dynamics increased unsafe sexual behaviours and exploitation, increasing barriers to SRH support. A Latin American woman needing HIV/STI care explained, “He told me[…] what I want is to sleep with you whether you want it or not, I told him no, […] he got so angry with me that he fired me.” (p. 420) [69].
Unequal gender roles and power dynamics especially hindered access to GBV support, resulting in silence and hidden abuse [56]. One study reported that financial dependence on abusive partners who had control over their immigration status posed additional healthcare barriers [60]. An HCP demonstrated the extent to which women covertly sought birth control: “the women are saying ‘please don’t tell my husband’ or they have come here on the sly[…] they are like, ‘quick, give me a Depo Provera injection and don’t tell him’” (p. 376) [71].
Discussion
This review sheds light on alarming inequities in SRH care for im/migrant women in Canada. Key findings demonstrated that structural challenges associated with health system navigation and knowledge of SRH services, experiences of racism and xenophobia within and outside the health system, and insufficient culturally safe and language-specific services posed the most significant barriers to healthcare. We found that while positive experiences with health personnel and social support facilitated SRH access for some women, social isolation, precarious immigration status, and discrimination and stigma by community members and HCPs presented severe challenges for others. Our study echoes prior research calling for attention to the impacts of immigration-specific factors (e.g., duration of migration, changes across migration, immigration status) on health access [42, 44], and provides unique insights on research gaps and findings regarding SRH access for im/migrant women.
Past reviews of im/migrant women’s SRH access have focused on specific sub-populations (e.g., refugees, internally displaced migrants) [40, 49, 84, 85] and services (e.g., maternal health, HIV/STIs) [20, 40, 42, 50, 84, 86–88]; our findings build on this work by providing a comprehensive overview of inequities and determinants of access to a broader range of SRH services (e.g., sexual health screenings, GBV) amongst im/migrant women in Canada. Consistent with gaps identified in previous literature, heterogeneous definitions of immigrants across studies limited comparisons and understandings of diverse SRH access experiences [42]. Amongst studies that focused on specific populations, most included sponsored refugees and asylum seekers, and few made comparisons between the experiences of diverse groups. However, evidence demonstrated severe SRH inequities based on immigration status where available, highlighting the need for future research unpacking the impacts of immigration status on SRH experiences [69].
Most studies were conducted in Ontario, and limited information was found from other key destination provinces (i.e., BC, Alberta, Quebec). Most studies focused on maternity care and cervical cancer screening, with a dearth of research on contraception services, GBV support, or other types of sexual health screenings. This presents a need for greater understandings of inequities faced by im/migrant women across the full spectrum of SRH services. Some studies included both im/migrant women and provider perspectives, highlighting several multi-level opportunities to address challenges and strengthen supports. For example, women’s preference to see women doctors to avoid potential re-traumatization of sexual violence [80] speaks to a critical need for trauma-informed care in health and settlement settings. Insights provided by immigration lawyers, legal advocates and HCPs demonstrate the impacts of macro-structural factors and the need to include other stakeholders (e.g., settlement workers, government officials) in research to address structural challenges in SRH care.
Qualitative and quantitative findings complemented one another and provided unique insights regarding inequities and determinants of SRH access for im/migrant women. Quantitative findings highlighted statistical descriptions of im/migrant women’s use and access to SRH care, which was explained by various determinants of SRH access highlighted by qualitative findings. However, most studies were cross-sectional, and research using longitudinal methods to understand women’s SRH access over time, across arrival and settlement, is needed.
Although most literature continues to focus on health service use and delivery environments, several studies that did identify macro-structural and immigration-specific determinants of SRH care highlighted the critical influence of immigration status on limited health insurance coverage and other barriers to SRH care. Policies that exacerbate barriers for women experiencing pre-migration trauma or PPD, for example, demonstrate structural inequities that ignore intersecting forms of marginalization based on gender, race, age, and poverty. Most studies did not focus on the roles of macro-structural factors such as stigma, ‘othering’ [43], and immigration policies or the nuances of how these may influence whether and how im/migrant women engage with SRH services [43, 45].
Research gaps identified by our review include a limited focus on SRH access experiences of younger women, undocumented women, and women who speak languages other than English. Although reproductive age is understood to begin at the age of 15, only two studies included women below the age of 20 [37, 51]. While only three studies included undocumented women, one excluded this population [79] and others did not specify explicit inclusion or exclusion of certain subgroups. A large number of studies excluded women who could not communicate in English [56, 61, 67, 70, 77, 80], presenting significant inequities as available evidence demonstrated severe language barriers.
Strengths and Limitations
To our knowledge, our findings are the first to highlight the heterogeneous experiences of different im/migrant women sub-groups across a wide spectrum of SRH care. Our review also uniquely builds on past work by highlighting the nuances of how immigration-specific factors, including how variations based on the duration and type of migration, interact with cross-cutting factors such as gender and socioeconomic status [3, 44, 89], to shape im/migrant women’s SRH access in Canada. However, limitations exist. The studies included may not have captured the many, diverse experiences of im/migrant women’s access to SRH care in Canada. Articles that examined the health access of both im/migrant men and women and that did not have a clear focus on SRH were excluded, thus potentially missing some information on im/migrant women’s SRH access.
Recommendations for Future Research
The findings of this review call for additional research in im/migrant women’s health to highlight the nuanced ways in which structural and intersectional experiences shape SRH access, particularly in the context of maternity care and cervical cancer screening. Future research must engage a broader diversity of im/migrant populations, including youth, undocumented women, and asylum seekers, whose experiences remain underrepresented; this is critical to generate comparable data to inform im/migrant-sensitive health services and system planning. Narratives from stakeholders also demonstrate value in consulting service providers, policymakers and community advocates to understand varied perspectives on im/migrant women’s health access. Certain parts of Canada (e.g., Ontario) were better represented in the literature, and there remains a need for additional research particularly in BC, Alberta, and Quebec. Finally, longitudinal and mixed-methods designs are recommended to examine changes in health experiences and access over time and triangulate epidemiological findings with lived experiences.
Conclusions
The findings of this review highlighted important issues in SRH services faced by racialized im/migrant women in Canada across different types of SRH care, and pointed to key roles of macro-structural, immigration-specific factors, health service use and delivery, and individual-level factors in shaping inequities. Our analysis helps draws on both quantitative and lived experiences of im/migrant women, and points to the need for different types of interventions. Findings provide a comprehensive overview of challenges and supports faced by im/migrant women accessing SRH care in Canada; future research that compares and includes experiences of different im/migrant groups, addresses a wider spectrum of SRH services, and includes marginalized sub-groups is needed. This is essential to expand existing understandings of the diverse and shared needs and realities of im/migrant women to develop responsive, equity-oriented policies and interventions.
Acknowledgements
This study was funded by the Canadian Institutes of Health Research (CIHR), Vancouver Foundation, and Simon Fraser University (SFU). SG is partially supported by a CIHR New Investigator Award and the National Institutes of Health (NIDA). MW is partially supported by a Research Trainee award from the Michael Smith Foundation for Health Research. AES is supported by the National Institutes of Health (NICHD). SM is supported by a Doctoral Fellowship from SFU. We thank the Centre for Gender & Sexual Health Equity for research and administrative support, including Megan Bobetsis and Colette Ryan. We also thank Ursula Ellis, Reference Librarian at UBC’s Woodward Library, for her guidance.
Appendix A
See Table 2.
Table 2.
Combination of search terms used to explore and understand determinants of access to and engagement in sexual and reproductive health(SRH) services amongst im/migrant women in Canada (2008–2018) based on searches in Ovid Medline, Social Sciences Citation Index, Sciences Citation Index, and CINAHL
| Sexual and reproductive health (SRH) | “sexual health” OR “reproductive health” OR “SRH” OR “HIV” or “human immunodeficiency virus” OR “AIDS” or “acquired immune deficiency syndrome” OR “HIV/AIDS” OR “STI*” OR “sexually transmitted infection*” OR “STD*” OR “sexually transmitted disease*” OR “contracept*” OR “miscarriage*” OR “abortion*” OR “stillb*” OR “live birth*” OR “antenatal” OR “prenatal” OR “postnatal” OR “perinatal” OR “postpartum” OR “pregnanc*” OR “maternal mortalit*” OR “maternal health” OR “maternal morbidit*” OR “sexual violence” OR “gender-based violence” OR “violence against women” OR “intimate partner violence” OR “IPV” OR “GBV” OR “reproductive coercion” |
| Migration | “migrant*” OR “migration” OR “immigrant*” OR “immigration” OR “refugee*” OR “asylum seeker*” OR “asylee*” OR “mobile population*” OR “displaced person*” OR “displacement” OR “IDP” OR “newcomer*” OR “deport*” OR “cross-border” OR “across borders” OR “binational” OR “transnational” OR “transmigration” OR “transmigra*” OR “traffick*” OR “undocumented” OR “foreign-born” OR “foreigner*” |
| Women | “women” OR “woman” OR “female*” OR “mother*” OR “maternal” OR “girl*” |
| Methodology | “qualitative” OR “interview*” OR “narrative*” OR “grounded theory” OR “focus group*” OR “ethnograph*” OR “quantitative” OR “epidemiolog*” OR “cross-sectional” OR “cohort” OR “randomized controlled trial” OR “RCT” OR “longitudinal” |
Appendix B
See Table 3.
Table 3.
Types of sexual and reproductive health (SRH) services accessed by im/migrant women in Canada (2008–2018)
| Type of SRH care | |||
|---|---|---|---|
| Maternity care | Sexual health screenings and treatment | Gender-based violence support | Family planning and contraception |
| Prenatal and pregnancy [23, 51, 54, 55, 61, 75–77, 78, 80, 81] | Cervical cancer [37, 39, 58, 66–68, 73, 82] | GBV reporting and help-seeking (including intimate partner violence) [56, 70, 79] | Family planning [71, 72] |
| Postpartum [23, 26, 27, 29, 52, 62, 90] | HIV [57, 60, 69] | Condom use [59] | |
| Perinatal [53, 63] | STIs [60, 69] |
Appendix C
See Table 4.
Table 4.
Additional exemplars and findings of determinants of access to and engagement in sexual and reproductive health(SRH) services amongst im/migrant women in Canada (2008–2018)
| Theme | Population | Main finding | Qualitative exemplars of women’s lived experiences of barriers and facilitators to SRH care | Quantitative findings of barriers and facilitators to SRH care |
|---|---|---|---|---|
| Health system navigation and access to SRH service information | Chinese newcomer women N = 13 |
Positive experiences navigating the Canadian health system facilitated access to maternity care [54] | “Here in Canada it is better because it’s one-to-one when your doctor examines you at prenatal visits. Back home there were often some other women waiting inside the examining room and overheard the conversation between you and your doctor.” (p. 5) | |
| HCPs N = 10 |
Inadequate health insurance coverage, costs and limited understanding of the health system created barriers to maternity care [55] | “P2: We heavily involved like, social work to figure it out [levels of coverage], like all of the front staff, and they had to be like on the ball. And then things kept on changing […] so it just made it very confusing […]” (p. 8) | ||
| “P2: Some did have their kids in the NICU and one even had their child die, and then and they ended up being presented with a massive bill, massive bill. So, it’s just you know, it’s tragic on a personal level, and then to have the added financial burden on top of it, it was cruel. And the babies are Canadian, if they’re born here, they’re born as Canadians.” (p. 9) | ||||
| “P6: So, we had a walk-in in clinic at the Travelodge and I was one of the [health care workers] mandated at the walk-in clinic […] and if they came to me and they were prenatal, I would definitely call the clinic that day and say we need an appointment for this pre- natal patient, can we fit her in? Literally fit her in. So, then we would require some rearranging of appointments, and scheduling and all that stuff…” (p. 9) | ||||
| Immigrant women from 9 different countries N = 33 Social service providers/stakeholders N = 18 HCPs N = 8 |
Inadequate care, high costs, and quick discharge led to poor satisfaction and quality of maternity care [61] | “It’s hard to find a family doctor because I phoned everyone … it took me for a while, and then you can’t go with him because his appointment [book] was full. I phoned a lot of clinics and then they cannot accommodate. (IW-Rural Town) It might take up to one year to find a family doctor. Moreover, after finally getting a family doctor and referral to a specialist clinic there was often another long waiting period because of the shortage of gynecologists or obstetricians. Some women complained that they received their first appointments in the advanced stages of their pregnancy. The issue of long wait periods was a great barrier to accessing care at an appropriate time.” (p. 8) | ||
| “She preferred to stay in the hospital a little bit longer, maybe one more day or anything. But [the] OB didn’t care and sent her home and then she actually fainted or lost consciousness at home and then her husband would have to call 911 and send her back to the hospital.” (IW-Urban Town) (p. 9–10) | ||||
| Latin American immigrant women N = 25 [permanent residents (N = 11), refugee status claimants (N = 10)] |
Shortage of doctors, delays, and a lack of referrals created barriers to accessing HIV/STI services [69] | “I had a high-risk pregnancy, they told me that I had to see a gynaecologist, and that there was a waiting list…. Many women tell me that they come to term in their pregnancy without ever seeing a gynaecologist. I was under a lot of stress because I was already four months pregnant and no one had seen me. I was bleeding eight days in my home, I would go to the health centre and they told me to go home, until the eighth day, I lost the baby.” (p. 422) | ||
| Chinese newcomer women N = 15 |
‘Inconvenient’ health system created barriers to maternity care [54] | “My OB wasn’t on duty and I had another OB that was ‘on call’ and he did not know anything about me and my pregnancy. It was difficult, especially, I had DM (diabetic mellitus) during pregnancy and my labour lasted sixteen hours.” (p. 4) | ||
| Muslim, West and South Asian immigrant women N = 30 |
Lack of knowledge of Canadian health system created challenges in accessing cervical cancer screening [67] | “For an immigrant there are lots of things that you don’t have enough information and you need someone to help you, and fortunately I have friends and family here and ask them to help me, and I chose my family doctor by their recommendation. But if they weren’t here, I think maybe I had a lot of problems, because we are not familiar with this system, it takes time to know how you can do many things”. (p. 7) | ||
| Immigrant women N = 4,55,864 |
Health insurance and characteristics of health providers were predictors of access to cervical cancer screening [39] | Appropriate cervical cancer screening occurred for 61.1% of women. Screening rates were low among women aged 25–49 and living in low-income areas (Absolute Risk Reduction (ARR)) = .88 CI = .88–.88) | ||
| Cervical cancer screening was low amongst women registered with Ontario’s universal health insurance plan in the last 10 years (mainly recent immigrants) | ||||
| Refugee claimant women from five different countries N = 112 |
Difficulties reaching women, and limited and confusing health insurance coverage created barriers to postpartum care [62] | “I called several times. She was unavailable. It was difficult to locate her. A worker states she has left the shelter. ‘Jessica’, a person who lived at the shelter, knows the client and gave me her phone number.” (35 y.o., Nigeria, 7 mos in Canada) (p. 288) | ||
| “Paediatrician refused to see baby because she had no medicare. One month later the paediatrician gave her an appointment but when mother said she still had no medicare then he cancelled it.” (36 y.o., Mexico, 6 mos in Canada, Montreal) (p. 289) | ||||
| Uninsured and insured new immigrant and refugee claimant women N = 437 |
A lack of health insurance negatively influenced perinatal experiences for both mothers and infants [63] | Most uninsured pregnant women received less than adequate prenatal care. More than half received clearly inadequate prenatal care, and 6.5% received no prenatal care. Insurance status related to type of HCP, reason for caesarean section, neonatal resuscitation rates, and maternal length of hospital stay. Uninsured mothers experienced more caesarian sections due to abnormal fetal heart rates, and required more neonatal resuscitations | ||
| Chinese immigrant women N = 13 |
Multiple resources to obtain pregnancy information facilitated access to maternity care [54] | “My own mother couldn’t come due to a visa issue and my husband didn’t know how to cook, so we hired a Yue-Sao. She stayed three hours every morning for a month to cook Zuo Yue Zi meals for me. She was a nurse back home, so she is professional and knowledgeable. She is my consultant for postnatal practices.” (p. 6) | ||
| Immigrant women from 9 different countries N = 33 Social service providers/stakeholders N = 18 HCPs N = 8 |
Limited and inadequate health information negatively influenced access to maternity health services [61] | “The thing is, when people come here, because they have no idea about community resources, they don’t go. They don’t come” (HCP-Rural Town), (p. 7) | ||
| Newcomer women N = 140 Canadian-born women N = 1137 |
Low levels of pregnancy knowledge negatively influenced pregnancy outcomes and experiences [23] | No differences in newcomer ability to access prenatal care compared to Canadian-born women, but fewer received information regarding emotional and physical changes during pregnancy (87% vs. 95%, p < 0.001)—less from friends (10% vs. 20%), more from books (27% vs. 17%), more from nurses (20% vs. 13%), less from family doctors (10% vs. 15%). Rates of C-sections higher for newcomers (36.1% (95% CI 28.2, 44.8) vs. 24.7% (95% CI 22.2, 27.5), p = 0.02), and more likely to be placed in stirrups for birth and have an assisted birth | ||
| Less likely to report “very satisfied” with care received since birth (p = 0.03) | ||||
| Muslim, West and South Asian immigrant women N = 30 |
Limited knowledge about cervical cancer and screening guidelines limited access to screening [67] | “I have a question, what do you mean by screening? Is it a different program than when we go to family doctor and we do a check-up, we do blood testing?” (p. 5) | ||
| “So my family doctor has to ask me to do this? May be sometimes I’m not at risk so my doctor does not do it. Right?” (p. 5) | ||||
| Positive and negative experiences with health personnel | Chinese im/migrant women N = 13 |
Informed HCPs improved access to postpartum care [52] | “My midwife… felt that I was relatively weak due to having a Caesarean, so in the ten days after giving birth, she came to my home three times, that’s why I did not need to go out to see the pediatrician on my own”(P8 (p. 390) | |
| “The community nurses here visit about one hour each time. They would recommend a better place to breast- feed, which posture is better, and they would check if the baby is feeding correctly. She would help you like a postpartum doula. The second time they will call first to ask if you need anything. If there is a need she will come again”(P1)(p. 390) | ||||
| Im/migrant women N = 15 HCPs N = 5 |
Positive interactions with HCPs facilitated perinatal experiences [53] | “…the women describing the nurses as playing a positive and important role in making the childbirth experience less scary by monitoring the women’s labor, encouraging and coaching the women, providing massage, and offering explanations about the stages of labor.”(p. 296–297) | ||
| HCPs N = 10 |
HCPs that specialized in refugee health and practice diverse strategies of care improved maternity care experiences [55] | “P8: [community-based organization] is extremely well supported with other disciplines. So, we work closely with the social workers and they’re very instrumental in helping provide supports, just resources, physical resources, but also trying to get the social supports in place to.”(p. 7) | ||
| African, Caribbean and Black women living with HIV N = 173 |
Factors influencing engagement in and continuity of HIV care subsequently affected quality of life (QOL) [57] | Bivariate correlation results: Age not significantly associated with QOL for African, Caribbean and Black women living with HIV, but income associated with significantly higher overall QOL and social environments and relationships | ||
| Engagement in and continuity of HIV care was significantly associated with QOL (p = 0.003) | ||||
| Chinese im/migrant women N = 13 |
Barriers to implementing traditional postpartum practices due to unregulated, unreliable paid helpers and uninformed, insensitive providers [52] | “[The postpartum doula] has been paid in cash already, and she does not have a license or belong to a postpartum organization, so it is completely non-binding. And we cannot do ten “zuo yue zis” in a lifetime…To Chinese people “zuo yue zi” is done once or twice, at most three times, so postpartum doulas do not mind whether they have recurring customers…You have heard a lot of bad reports. After all, in this market the supply is less than the demand, that is, there are more mothers seeking postpartum doulas and there are less postpartum doulas” (P8) (p. 390–391) | ||
| “[The nurse said]...“Why do you not take a shower?” I felt I was being judged and thought of as “How come you’re so dirty?” Not only was her facial expression clear, her tone of voice was quite obvious to make me feel very uncomfortable” (P8) (p. 391) | ||||
| Health and academic personnel N = 237 |
Negative perceptions of im/migrants by HCPs contribute to stigma and discrimination in maternity care [77] | “Some healthcare workers perceive uninsured migrants as “deserving” of universal access to healthcare | ||
| Negative perceptions of migrants coupled with pragmatic considerations push most workers to view the uninsured as “undeserving” of free care | ||||
| For most participants, the right to healthcare of precarious status immigrants has become a “privilege”, that as taxpayers, they are increasingly less willing to contribute to.” | ||||
| Im/migrant women N = 15 HCPs N = 5 |
Negative interactions with HCPs limited women’s access to perinatal services [53] | “I had lots of pain and I was not in condition to stand up but they said, “No, you have to stand up.” I tried [but] when I stood, I had so much pain that I fell down. The nurses don’t really care what happens to the patients. The nurses told me that you should do your things yourself.” (p. 297) | ||
| Im/migrant women from nine different countries N = 33 Social service providers/stakeholders N = 18 HCPs N = 8 |
Short consultation times, a lack of confidentiality and informed consent, and insensitivity from HCPs limited access to maternity care [61] | “I also have another client who has been hospitalized many times and people will come to visit her, and some people are curious and they will go to the front desk and ask: What happened to her? Why is she sick? And the nurse out loud told them.” (HCP-FGI-Urban Town) (p. 9) | ||
| “Oh. Okay. Do you feel painful?” “No.” “Okay, you can go.” Like I don’t care. That’s the information but, I don’t care about you. Just the doctor in this way, just cold.” (IW-Urban Town) (p. 9) | ||||
| South Asian im/migrant women N = 22 |
Lack of supportive services for intimate partner violence (e.g. trust, non-judgmental) prevented access to care [56] | “Everyone here is telling you more or less that they spoke to the doctors, I think that doctors should be part of the circle that if they get a clue that a lady is going to be abused he should double-check, or confirm. The doctors should be part of the system to check for woman abuse” (FG1, p. 11) (p. 619) | ||
| HCPs N = 10 |
Expectations of provider type and level of professionalism negatively influenced access to prenatal care [75] | “First-generation immigrants often avoid midwifery care, because they see midwifery care where they come from is the lowest level of obstetric care…. They come here, and they have access to the big shiny hospital and the big shiny obstetrician and, in their country, that is a symbol of status and success and probably does reflect good healthcare. So, why would you go to a midwife? You wouldn’t do that. You would go to the big shiny place.” (p. 567) | ||
| “Well, you’re a nurse. How can you be looking after me? You are not a doctor. I need to see the doctor.” And, “I am getting second-rate care because I am seeing a nurse, just a nurse.” (p. 567) | ||||
| Im/migrant Muslim women N = 6 |
Insufficient care provided by HCPs negatively influenced access to maternity health services [78] | “Some women felt that they received inadequate support or inattentive care. One participant reported that when she needed assistance, she found a nurse “reading a fashion magazine and drinking Tim Horton’s [coffee].” (p. 105) | ||
| Refugee claimant women from 5 different countries N = 112 |
Inadequate assessments by nurses created challenges in postpartum care [62] | “She did not mention it [skipping meals] because the [nurse] had not asked.” (p. 288) | ||
| HCPs N = 10 |
Lack of coordination, and HCP’s unfamiliarity with refugee health and inability to address needs created barriers to maternity care [55] | “P7: Not a lot of [health care professionals] take the extra step to look at what’s going to happen when the baby’s born […] sometimes you need the physician who’s the first point of care often for the patients, to recognize their social concerns in terms of you know social detenninants of health […] so that you can refer her to the proper resources because she is so vulnerable, and it’s really common that these women don’t get any services.” (p. 8) | ||
| “P9: Sometimes our [refugee] patients even ask us in triage like financial concerns, and I don’t know what to say at all. Like that’s something I would like to be more educated on, like what kind of services are available to you [refugees].” (p. 10) | ||||
| Language barriers, and availability of culturally safe and language-specific care | Family planning HCPs N = 9 |
Language barriers and judgment in family planning and reproductive health services limited access [71] | “Well, language is a huge barrier… A lot of times women, even if they speak a little bit of English, you know I try to encourage them to go to another clinic because they haven’t had a checkup for, you know, god knows how long. The thing is always that ‘there are some things I want to discuss that I won’t know how to say in English. I may not understand what they are telling me.” (Canadian health care worker) (p. 374) | |
| “I have two Afghani women … and both of them thought they might be pregnant and want abortions. So they came on their own, and they actually didn’t want interpreters because they were worried that the interpreters would judge them because they believed in their interpretation of their religion that you cannot have access to, well, abortion services in general.” (Physician at community health center) (p. 375) | ||||
| Im/migrant Muslim women N = 6 |
A lack of awareness of religious and cultural practices hindered access to maternity health services [78] | “Like when I was pregnant during Ramadan [the month of fasting] and I asked my doctor about fasting. She told me ‘I don’t like to tell you not to fast.’ I prefer if there can be some Muslim physician who can give them more information about such topics. They don’t understand it. If they have more ideas about the issue it will be better.” (p. 107) | ||
| Family planning HCPs N = 9 |
Misconceptions and a lack of knowledge impacted family planning access experiences [71] | “The other thing I find totally doesn’t fly with the immigrant women … a lot of them don’t look down there, they don’t touch down there, they are so ashamed…” (p. 377) | ||
| “So it has been an uphill battle to explain about birth control and family planning. The notion of actually being able to make those decisions is also quite new to many couples. Even as a couple, because often it is traditionally seen as God’s will… [T]hat’s over quite a range of countries throughout the world.” (p. 377) | ||||
| Sri Lankan Tamil community leaders and im/migrants, assisting im/migrant women’s access to formal support for abuse N = 16 |
Lack of knowledge of available services due to language barriers limited access to intimate partner violence support [70] | “Maybe the woman has language issues. If she is a woman who has contacts outside, who’s going outside, and being able to talk to someone, she will know about services. Other women have no way to know who does what and what helps.” (p. 72) | ||
| Latin American im/migrant women N = 25 [permanent residents (N = 11), refugee status claimants (N = 10)] |
Language barriers and a lack of appropriate translation services created challenges in HIV/STI services [69] | “Health centres sometimes offered translating services but when unavailable, women had to find someone who could accompany them to their appointments, which created confidentiality issues. Moreover, many women felt uncomfortable talking about sexual and reproductive health matters in the presence of a translator.” (p. 421) | ||
| Muslim, West and South Asian im/migrant women N = 30 |
Different religious and cultural beliefs, language barriers and a preference for female physicians negatively shaped cervical cancer screening experiences [67] | “Health Care Connect program only ask for location preference, where you live, and then they will try to match in your area. You couldn’t set up for any other preferences. We usually have to find female doctors through friends and family.” (p. 7) | ||
| “There are GP’s who, I guess there are less culturally sensitive. I guess that’s what it is—we go to the doctor with our moms, and I’m not married and I’m not comfortable when my GP says “are you sexually active?” and my mom is sitting beside me. No I’m not!! (Laughs). So, that’s why it’s nice for a lot of us to choose a GP that’s are from our own culture because they won’t ask questions like, “are you sexually active?” (p. 7) | ||||
| New im/migrant women N = 11 |
Embarrassment, preference for female clinicians, and language barriers limited cervical cancer screening [68] | “..and besides there are also the language barrier in this country right? ….how will I make the appointment? … and then when I have the appointment I don’t have someone who will translate for me, and I go looking and there are all these barriers… so someone really needs to have the desire to get it (Pap) done and realize that it’s necessary for her to do so.” (Sp/Sp) (p. 232) | ||
| “Some cultural things affected,…big difference here. Back home, culturally… women is not married, she can’t talk about it like this.” (Ar/Eng) (p. 232) | ||||
| HCPs N = 63 |
Communication challenges due to background and social conditions negatively influenced access to maternity care for newly-arrived women [74] | “Maybe it’s me, but I think that the sociocultural beliefs are the toughest ones because you may need proper language to ask for the appointments and you may count or not on some family or friends to explain to you how to get into the health care system, unknown to you, that’s true. But now, when it comes to sociocultural issues it’s really hard for them because in addition to not having the language and feeling isolated, the only way you have to be emotionally linked to your family is by means of your rituals, your traditions, your beliefs. And for different reasons, usually genuine reasons, we have a hard time to respect them.” (p. 5) | ||
| Immigrant and refugee women N = 30 |
Limited understandings of PPD and community beliefs around mental illness limited access to postpartum care and treatment of PPD [28] | “We don’t have all the circumstances that lead to this. Some of the women will get depressed, but you have your family support, everyone around you, you don’t feel lonely. So it’s really different, here you’re alone and struggling with the baby and don’t know how to seek help … we don’t know all the sources for help, that’s the difference.” (p. 306) | ||
| Im/migrant women from 9 different countries N = 33 Social service providers/stakeholders N = 18 HCPs N = 8 |
Cultural shock and communication barriers hindered access to maternity health care [61] | “… sometimes when we get into hospital … they speak very, like very fast English, and being new to the country you don’t—you are not really used to the accent, you know. And so, and they are scared to ask questions. (IW-FGI-Urban Town)” (p. 8) | ||
| “It’s usually more on the gut feel that this person has no idea what you are talking about, no matter how slowly and simple you explain it. It’s just not getting through … I had someone send one of my patients for a triple screen which came back nicely with a positive for Down Syndrome and I couldn’t explain that in Arabic. (HCP-Rural Town)” (p. 8) | ||||
| Newcomer Chinese women N = 15 |
Limited linguistically and culturally sensitive health services presented barriers to accessing maternity care [54] | “I am worried about the process of delivery. I feel safe if someone can explain to me what’s going on using the language I understand.” (p. 4) | ||
| HCPs N = 10 |
Expectations around culturally appropriate translation, interpretation services, and cultural awareness negatively impacted prenatal care experiences [75] | “Care is also compromised by people simply not understanding what the words mean and understand…so, sometimes, with people who don’t understand English words, so it is hard, so they can’t translate. And even if they can translate, sometimes they still don’t understand the word. That can be very difficult.” (HCP)(p. 565) | ||
| “Many Muslim women… [will assume] that they can be guaranteed a female [provider]. And some of them also don’t want any learners, and we are a teaching site, so they don’t want any medical students or residents… sometimes they will settle: ‘Okay, I will have the male doctor if need be for my delivery, if that is who is on, but no male learners.’ And so, some of them will be… really forceful in that regard, trying to insist, thinking we will call in one of the female physicians.” (HCP) (p. 566) | ||||
| HCPs N = 10 |
Preference for female providers, differences in medical practices, and language barriers influenced access to maternity care [55] | “P2: I think probably the biggest challenge is no male physician for the delivery, and we cannot guarantee that. It’s not the way it works in Canada […] if she goes into hospital and there’s an emergency, it may be a male OB doing the C-Section or you know, helping out with the shoulder dystocia right or whatever it might be.” (p. 7) | ||
| Social isolation and support | Chinese im/migrant women N = 13 |
Support from family members, friends and partners facilitated postpartum care experiences [52] | “If my family is around, I would not let them leave in such a short time. Instead, I would ask my mother-in- law to stay for at least three months. I will not tell her to go after only one month of “zuo yue zi” (P12) (p. 389) | |
| “If during “zuo yue zi”, couples are able to work together to survive and to take care of the baby, this may solidify the couple for the future… If two people are truly able to understand each other, this may be a help to their future, because the wife may not understand her hus- band’s expression of love but she can experience the process of re-shaping the family values” (P5) (p. 389) | ||||
| Im/migrant women N = 15 HCPs N = 5 |
Support from husbands and family members facilitated women’s perinatal experiences [53] | “My husband used to help me so I didn’t have a lot of pressure. After coming from my work, I used to make just the vegetables. Even vacuuming, he used to do and if there was need to clean the kitchen with the broom, he used to do that too. My husband used to say, “It’s not important to clean the house, I will take care of it. Just rest because you are tired from work.” If the woman has to do the outside work as well as the work at home, it can be very difficult.” (p. 296) | ||
| “At the first baby, one doesn’t know what happens. If there is an elderly person in the house, that person can tell about the circumstances, as my mother-in- law [did], who recently came [to Canada] towards the end.” (p. 296) | ||||
| Chinese im/migrant women N = 13 |
Lack of social support posed problems in implementing traditional practices in postpartum care [52] | “[my husband] has to get up at six or seven and when he gets home from work around five or six in the evening, he has to help me take care of the baby so he is… quite exhausted” (P12). (p. 391) | ||
| Recent im/migrant women (< 5 years) N = 5703 Non-recent im/migrant women (> 5 years) N = 12,355 Canadian-born women N = 57,805 |
Less perceived social support during pregnancy or postpartum for im/migrant women leading to higher rates of postpartum depression symptoms [51] | Im/migrant women more likely to report high levels of postpartum depression symptoms (13.2% vs. 6.0%), less likely to have access to social support (74.1% vs. 90% during pregnancy, 67.8% vs. 87.1% during postpartum). Recent and non-recent immigrant women had different experiences—duration of residence in Canada played a role in maternity experiences | ||
| Domestic violence service providers N = 32 Advocates and social service professionals N = 24 Im/migrant women from four different communities N = 21 |
Lack of social support prevented women from leaving intimate partner violence [79] | “For me, I didn’t know what to do—afraid, but I was afraid. Still am. Sometimes they say you have to leave him. Leave him! Where would I go? I don’t know anyone else in Canada”. (Spanish Woman) (p. 338) | ||
| South Asian im/migrant women N = 22 |
Loss of social support after migration delayed help seeking for intimate partner violence support [56] | “(after being abused by partner) Here we just stay inside of the house scared not even calling anyone. What we are thinking at that time is what can I do? Where can I go? I don’t have anyone of my own over here.” (FG3, p. 4) (p. 617) | ||
| “When I first came here my in-laws were in the house… they used to lock the door on me so I could not get out… and they did something to the phone. We could get incoming calls but couldn’t make outgoing calls, [after a year of being beaten by her husband] I looked into my neighbours house from my window and told her… can you call 911… the police came and broke the lock of my door” (FG1, p. 6) (p. 617) | ||||
| Im/migrant women from nine different countries N = 33 Social service providers/stakeholders N = 18 HCPs N = 8 |
Lack of social support and feelings of isolation as barriers to maternity health care [61] | “I was in my eighth month I was still working. You know why? Because I don’t have anyone in the house. I was actually worried that I might give birth here and then I don’t have anybody.” (p. 7) | ||
| Immigration-specific factors | Women at low-risk for unplanned caesareans Cases: unplanned caesareans N = 233 Controls: delivered vaginally N = 1615 |
Poor access to maternity care determined by various migration-related predictors of unplanned caesareans [81] | Predictors of unplanned caesarean: being from sub-Saharan Africa/Caribbean (AOR 2.37, 95% CI 1.02–5.51) | |
| Amongst women living in Canada less than 2 years (AOR 1.77, 95% CI 0.98–3.20), having a humanitarian migration classification increased risk (AOR 1.60, 95% CI 0.72–3.56) | ||||
| Immigrant women N = 22 Refugee women N = 8 |
Consequences of immigration policies and precarious immigration status hindered help-seeking for postpartum depression [26] | “In my heart I always worry that because my husband is still on a work visa and not a Canadian citizen it may affect our immigration application… that’s why I dare not seek any help. I really felt inferior and that’s why I had a feeling that we’re not supposed to get any help without a Canadian citizenship status. To be honest, my husband also faced a lot of unfair kind of treatment in work place. For the first year our lives were really bitter…we could not see any way out and each day was filled with worries and fearing we would be expelled from Canada.” (p. 719) | ||
| HCPs N = 63 |
Barriers to maternity care influenced by migration journey and background, primarily precarious immigration status [74] | “…if you don’t have a Canadian status, well, you will have no rights at all, they have literally nothing, not even access to legal recourses because they cannot even claim for refugee status. These people, it’s sad what I am going to say, but they just live in the shadows, in all possible senses! And for migrant women who are pregnant, the ‘Canadian status’ is crucial because that opens or closes access to free health care. If you have a ‘Canadian status,’ no matter which one, you get access to care…” (p. 5) | ||
| Uninsured refugee claimant and im/migrant women N = 175 Insured refugee claimant and im/migrant women N = 278 |
Most uninsured women received inadequate maternity care, with shorter lengths of hospital stays and higher rates of caesareans due to poor perinatal outcomes [63] | The number of prenatal visits reported for the uninsured group (mean = 6.04, t = −6.173, α = 0) was significantly lower, than for their insured peers (mean = 8.70). No difference was found between the uninsured and insured groups in health care service or treatment during delivery | ||
| Domestic violence service providers (key informant interviews) N = 32 Advocates and social service professionals |
Fear of immigration status repercussions and a reluctance of police intervention prevented women from leaving relationships with intimate partner violence [79] | “She is waiting for papers. That man knows she cannot go. That is why he always tortures her. She is afraid of everything”. (Bengali Woman) | ||
| N = 24 Im/migrant women from four different communities N = 21 |
“Very frightening for women with little kids, involved with CAS, no status here. Trend coming up is that men are bringing their wives to Canada on a visitor visa, so they have no status, and the men have no plan on sponsoring them, dump them, no rights here, terrified, don’t know about legal aid, men withdraw sponsorship at last second” (Service Provider) (p. 339) | |||
| Stigma, discrimination and racism | Im/migrant women from nine different countries N = 33 Social service providers/stakeholders N = 18 HCPs N = 8 |
Perceived discrimination and stereotyping in maternity care led to negative patient experiences [61] | “When you are pregnant and if you are over 30… in the African community, the doctors scared to hell. You have to do this, you have to do that. You do this, we have to test this, we have to give you the amnio… so start talking to you about C-section.” (IW-FGI-Urban Town) (p. 10) | |
| Im/migrant Muslim women N = 6 |
Discrimination and insensitivity about religious practices acted as barriers to maternity health services [78] | “You see their faces. You feel it that they think you are stupid and you don’t know anything about this world.” (p. 107) | ||
| Immigrant and refugee women N = 30 |
Workplace discrimination and stigma from HCPs negatively influenced postpartum depression experiences [28] | “I think it’s just in a square box and they don’t want to [look] beyond … there is no exception or consideration for people like me or other professionals that work and study. I did everything… to be honest I felt sometimes I have more capacity or eagerness to do things than Canadians living here. It is because everything is harder for us, twice or three times… so going through the process and having your credentials, it really bothered me, I think it is discrimination… (pp. 308–309) | ||
| Sri Lankan Tamil community leaders and im/migrants, assisting im/migrant women’s access to formal support for abuse N = 16 |
Discriminatory and racist practices negatively shaped experiences and service delivery for intimate partner violence [70] | “I’ve heard many stereotypical ideas about visible minority people. The service providers’ way is to tell the women, “Do as I say.” If you don’t, the services are withheld or they don’t provide the services in the way the woman wants. Visible minorities are being treated differently…” (p. 75) | ||
| Gender inequities and power relations | HCPs N = 9 |
Unequal gender power dynamics limited family planning access [71] | “I have had lots of women when having a discussion about contraception say that they couldn’t possibly decide. They would have to talk to their husbands, or their husbands would be the ones to decide … That is just a difference in culture, the way that the families are organized. And sometimes it is an issue of power and control.” (p. 376) | |
| Latin American im/migrant women N = 25 [permanent residents (N = 11), refugee status claimants (N = 10)] |
Unequal gendered power dynamics influenced women’s perceptions of HIV/STI risk and limited access to testing [69] | “The doctor told me: you have herpes. He told me it is a disease that I will have for life… I did not know what to do, I was left in shock. When I left to talk to Carlos, he made himself to be the victim. He made it seem like I was the one being needy, he treated me really poorly and made me feel ashamed.” (p. 420) | ||
| Immigrant and refugee women N = 35 [immigrants (N = 22), refugees (N = 8)] |
Gender roles, relationship dominance and control hindered access to postpartum mental health services [26] | “I was evicted by my husband. He pushed me out of the house. The police took me to the YWCA. He took away a lot of my things I really treasure. He wouldn’t let me learn new things or let people help me. My husband would teach me a lot of things the wrong way… like wrong ways of thinking and he made me sign papers. Only now I know it’s the wrong way…” (p. 720) | ||
| “According to Indian culture, men are the wage-earners and women stay at home and take care of their kids. So if the man is earning good, and the woman is working, she’s looked down upon by some elderly people in the household. It’s the woman’s responsibility to take care of the baby completely. If I’m going to work and my baby is getting sick often, then the elderly family members expect I quit my job and take care of my baby. They don’t expect my husband to do the same. If your husband stays home and if the wife goes out for work, it’s kind of looked upon as weird. That’s not the norm, according to the culture.” (p. 721) | ||||
| South Asian im/migrant women N = 22 |
Rigid gender roles and familial expectations (e.g. marriage obligations, expected silence) limited help seeking for intimate partner violence [56] | “Oh, I was told that you are a woman, you can change your husband, you can change your kids, it’s in your hands. If you cannot do it that means you don’t have the quality of a woman, you’re not real woman (other women are agreeing).. You aren’t capable of doing, (participant is crying).as if everything is my fault you know?” (FG3, p. 8) (p. 617) |
References
- 1.Carballo M, Grocutt M, Hadzihasanovic A. Women and migration: a public health issue. World Health Stat Q. 1996;49(2):158–64. [PubMed] [Google Scholar]
- 2.Goldenberg SM, Strathdee SA, Perez-Rosales MD, Sued O. Mobility and HIV in Central America and Mexico: a critical review. J Immigr Minor Health. 2012;14(1):48–64. [DOI] [PubMed] [Google Scholar]
- 3.Zimmerman C, Hossain M, Watts C. Human trafficking and health: a conceptual model to inform policy, intervention and research. Soc Sci Med. 2011;73(2):327–35. [DOI] [PubMed] [Google Scholar]
- 4.Platt L, Grenfell P, Fletcher A, Sorhaindo A, Jolley E, Rhodes T, et al. Systematic review examining differences in HIV, sexually transmitted infections and health-related harms between migrant and non-migrant female sex workers. Sex Transm Infect. 2013;89(4):311–9. [DOI] [PubMed] [Google Scholar]
- 5.Government of Canada. Asylum Claimants Processed by Canada Border Services Agency (CBSA) and Immigration, Refugees and Citizenship Canada (IRCC) Offices, January 2011–December 2018 [Internet]. 2017. [cited 2019 Jan 25]. Available from: https://www.canada.ca/en/immigration-refugees-citizenship/services/refugees/asylum-claims/processed-claims.html
- 6.Toughill K. Chaos coming to Canada after U.S. decision on refugees [Internet]. The conversation [cited 2019 Jan 25]. Available from: http://theconversation.com/chaos-coming-to-canada-afteru-s-decision-on-refugees-98233
- 7.Nixon R. Asylum Claims Jump Despite Trump’s Attempt to Limit Immigration. The New York Times [Internet] 2018. [cited 2019 May 7]; Available from: https://www.nytimes.com/2018/12/10/us/politics/trump-asylum-border-.html
- 8.United Nations. The International Migration Report 2017 (Highlights) | Multimedia Library—United Nations Department of Economic and Social Affairs [Internet]. 2017. [cited 2019 May 3]. Available from: https://www.un.org/development/desa/publications/international-migration-report-2017.html
- 9.Betancourt G, Colarossi L, Perez A. Factors associated with sexual and reproductive health care by Mexican immigrant women in New York City: a mixed method study. J Immigr Minor Health. 2013;15(2):326–33. [DOI] [PubMed] [Google Scholar]
- 10.Nilsson JE, Barazanji DM, Heintzelman A, Siddiqi M, Shilla Y. Somali women’s reflections on the adjustment of their children in the United States. J Multicult Couns Dev. 2012;40(4):240–52. [Google Scholar]
- 11.Salas LM, Ayón C, Gurrola M. Estamos traumados: the effect of anti-immigrant sentiment and policies on the mental health of Mexican immigrant families. J Community Psychol. 2013;41(8):1005–20. [Google Scholar]
- 12.International Organization for Migration. Key migration terms [Internet]. International Organization for Migration. 2015. [cited 2019 Jan 25]. Available from: https://www.iom.int/key-migration-terms [Google Scholar]
- 13.Statistics Canada. Immigration and ethnocultural diversity in Canada [Internet]. 2011. [cited 2019 May 1]. Available from: https://www12.statcan.gc.ca/nhs-enm/2011/as-sa/99-010-x/99-010-x2011001-eng.cfm
- 14.Statistics Canada. Population projections for Canada and its regions, 2011 to 2036 [Internet]. 2017. [cited 2019 Jan 25]. Available from: https://www150.statcan.gc.ca/n1/pub/91-551-x/91-551-x2017001-eng.htm
- 15.Hyndman J, Schuurman N, Fiedler R. Size matters: attracting new immigrants to Canadian cities | SpringerLink [Internet]. SpringerLink. 2006. [cited 2019 Jan 25]. Available from: https://link.springer.com/article/https://doi.org/10.1007/s12134-006-1000-6 [Google Scholar]
- 16.Merry L, Low A, Carnevale F, Gagnon AJ. Participation of childbearing international migrant women in research: the ethical balance. Nurs Ethics. 2016;23(1):61–78. [DOI] [PubMed] [Google Scholar]
- 17.Statistics Canada. Chart 11 Canadian-born females, total female immigrants and recent female immigrants by age group, Canada, 2011 [Internet]. 2015. [cited 2019 Jan 25]. Available from: https://www150.statcan.gc.ca/n1/pub/89-503-x/2015001/article/14217/c-g/c-g11-eng.htm
- 18.Immigration, Refugees, and Citizenship Canada. Departmental Plan 2018–2019 [Internet]. 2018. [cited 2019 Jan 25]. Available from: https://www.canada.ca/en/immigration-refugees-citizenship/corporate/publications-manuals/departmental-plan-2018-2019.html
- 19.National Immigration Forum. Fact sheet: Family separation at the U.S.-Mexico Border [Internet] 2018. [cited 2019 Apr 17]. Available from: https://immigrationforum.org/article/factsheet-family-separation-at-the-u-s-mexico-border/
- 20.Khanlou N, Haque N, Skinner A, Mantini A, Kurtz Landy C. Scoping review on maternal health among immigrant and refugee women in Canada: prenatal, intrapartum, and postnatal care [Internet]. J Pregnancy 2017. [cited 2019 Jan 25]. Available from: https://www.hindawi.com/journals/jp/2017/8783294/ [DOI] [PMC free article] [PubMed]
- 21.Gagnon AJ, Dougherty G, Wahoush O, Saucier J-F, Dennis C-L, Stanger E, et al. International migration to Canada: the post-birth health of mothers and infants by immigration class. Soc Sci Med. 2013;76(1):197–207. [DOI] [PubMed] [Google Scholar]
- 22.Wanigaratne S, Shakya Y, Gagnon AJ, Cole DC, Rashid M, Blake J, et al. Refugee maternal and perinatal health in Ontario, Canada: a retrospective population-based study | BMJ Open. BMJ J [Internet]. 2018. [cited 2019 Jan 25];8(e018979). Available from: https://bmjopen.bmj.com/content/8/4/e018979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mumtaz Z, O’Brien B, Higginbottom G. Navigating maternity health care: a survey of the Canadian prairie newcomer experience. BMC Pregnancy Childbirth [Internet]. 2014. [cited 2019 Jan 16];14(1). Available from: http://bmcpregnancychildbirth.biomedcentral.com/articles/https://doi.org/10.1186/1471-2393-14-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shah RR, Ray JG, Taback N, Meffe F, Glazier RH. Adverse pregnancy outcomes among foreign-born Canadians. J Obstet Gynaecol Can. 2011;33(3):207–15. [DOI] [PubMed] [Google Scholar]
- 25.Moore S, Daniel M, Auger N. Socioeconomic disparities in low birth weight outcomes according to maternal birthplace in Quebec. Canada Ethn Health. 2009;14(1):61–74. [DOI] [PubMed] [Google Scholar]
- 26.O’Mahony JM, Donnelly TT. How does gender influence immigrant and refugee women’s postpartum depression help-seeking experiences?: gender influences on immigrant and refugee women’s PPD. J Psychiatr Ment Health Nurs. 2013;20(8):714–25. [DOI] [PubMed] [Google Scholar]
- 27.O’Mahony J, Donnelly T. Immigrant and refugee women’s postpartum depression help-seeking experiences and access to care: a review and analysis of the literature. J Psychiatr Ment Health Nurs. 2010;17(10):917–28. [DOI] [PubMed] [Google Scholar]
- 28.O’Mahony JM, Donnelly TT, Raffin Bouchal S, Este D. Cultural background and socioeconomic influence of immigrant and refugee women coping with postpartum depression. J Immigr Minor Health. 2013;15(2):300–14. [DOI] [PubMed] [Google Scholar]
- 29.Vigod S, Sultana A, Fung K, Hussain-Shamsy N, Dennis C-L. A population-based study of postpartum mental health service use by immigrant women in Ontario. Canada Can J Psychiatry. 2016;61(11):705–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vigod SN, Bagadia AJ, Hussain-Shamsy N, Fung K, Sultana A, Dennis C-LE. Postpartum mental health of immigrant mothers by region of origin, time since immigration, and refugee status: a population-based study. Arch Womens Ment Health. 2017;20(3):439–47. [DOI] [PubMed] [Google Scholar]
- 31.Aptekman M, Rashid M, Wright V, Dunn S. Unmet contraceptive needs among refugees. Can Fam Physician. 2014;60(12):e613–9. [PMC free article] [PubMed] [Google Scholar]
- 32.Wiedmeyer M, Mayhew M. Reproductive health status of refugee women: characterizing contraceptive screening and use at a refugee clinic in British Columbia. Meeting presented at: North American Primary Care Research Group Annual Meeting (NAP-CRG); 2017; Montreal, Canada. [Google Scholar]
- 33.Government of Canada. HIV and AIDS in Canada: surveillance report to December 31st, 2013 [Internet]. 2014. [cited 2019 Jan 25]. Available from: https://www.canada.ca/en/public-health/services/hiv-aids/publications/hiv-aids-canada-surveillance-report-december-31-2013.html
- 34.Wanigaratne S, Cole DC, Bassil K, Hyman I, Moineddin R, Urquia ML. Contribution of HIV to maternal morbidity among refugee women in Canada. Am J Public Health. 2015;105(12):2449–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Remis RS, Liu J, Loutfy M, Tharao W, Rebbapragada A, Perusini SJ, et al. The epidemiology of sexually transmitted co-infections in HIV-positive and HIV-negative African-Caribbean women in Toronto. BMC Infect Dis. 2013;13:550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ranjan ASK, Chettiar J, Braschel M, Ogilvie G, Goldenberg SM. Barriers and facilitators to hepatitis B immunization among sex workers in Vancouver, Canada: implications for integrated HIV, STI, and viral hepatitis services. Symposium presented at: 16th International Symposium on Viral Hepatitis and Liver Disease (ISVHLD) Global Hepatitis Summit; 2018 Jun 14; Toronto, Canada. [Google Scholar]
- 37.Amankwah E, Ngwakongnwi E, Quan H. Why many visible minority women in Canada do not participate in cervical cancer screening. Ethn Health. 2009;14(4):337–49. [DOI] [PubMed] [Google Scholar]
- 38.Lofters AK, Moineddin R, Hwang SW, Glazier RH. Predictors of low cervical cancer screening among immigrant women in Ontario, Canada. BMC Womens Health [Internet]. 2011. [cited 2019 Jan 16];11(1). Available from: http://bmcwomen-shealth.biomedcentral.com/articles/https://doi.org/10.1186/1472-6874-11-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lofters AK, Moineddin R, Hwang SW, Glazier RH. Low rates of cervical cancer screening among urban immigrants: a population-based study in Ontario. Canada Med Care. 2010;48(7):611–8. [DOI] [PubMed] [Google Scholar]
- 40.Lindert J, von Ehrenstein OS, Priebe S, Mielck A, Brähler E. Depression and anxiety in labor migrants and refugees–a systematic review and meta-analysis. Soc Sci Med. 2009;69(2):246–57. [DOI] [PubMed] [Google Scholar]
- 41.De Maio FG. Immigration as pathogenic: a systematic review of the health of immigrants to Canada | International Journal for Equity in Health | Full Text. Int J Equity Health [Internet]. 2010. [cited 2019 Jan 25];9(27). Available from: https://equityhealthj.biomedcentral.com/articles/https://doi.org/10.1186/1475-9276-9-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gagnon AJ, Zimbeck M, Zeitlin J, ROAM Collaboration, Alexander S, Blondel B, et al. Migration to western industrialised countries and perinatal health: a systematic review. Soc Sci Med. 2009;69(6):934–46. [DOI] [PubMed] [Google Scholar]
- 43.Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75(12):2099–106. [DOI] [PubMed] [Google Scholar]
- 44.Acevedo-Garcia D, Sanchez-Vaznaugh EV, Viruell-Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: a cross-national framework. Soc Sci Med. 2012;75(12):2060–8. [DOI] [PubMed] [Google Scholar]
- 45.Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. 1991;43(6):1241–99. [Google Scholar]
- 46.Rhodes T, Simic M. Transition and the HIV risk environment. BMJ. 2005;331(7510):220–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 48.PRISMA [Internet]. [cited 2019 Sep 18]. Available from: http://prismastatement.org/PRISMAStatement/FlowDiagram.aspx
- 49.Ferguson A, Shannon K, Butler J, Goldenberg S. A comprehensive review of HIV/STI prevention and sexual and reproductive health services among sex Workers in Conflict-Affected Settings: call for an evidence-and rights-based approach in the humanitarian response | Conflict and Health | Full Text. Confl Health [Internet]. 2017. [cited 2019 Jan 25];11(25). Available from: https://conflictandhealth.biomedcentral.com/articles/https://doi.org/10.1186/s13031-017-0124-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Almeida LM, Caldas J, Ayres-de-Campos D, Salcedo-Barrientos D, Dias S. Maternal healthcare in migrants: a systematic review. Matern Child Health J. 2013;17(8):1346–54. [DOI] [PubMed] [Google Scholar]
- 51.Kingston D, Heaman M, Chalmers B, Kaczorowski J, O’Brien B, Lee L, et al. Comparison of maternity experiences of canadian-born and recent and non-recent immigrant women: findings from the Canadian maternity experiences survey. J Obstet Gynaecol Can. 2011;33(11):1105–15. [DOI] [PubMed] [Google Scholar]
- 52.Chang SH-C, Hall WA, Campbell S, Lee L. Experiences of Chinese immigrant women following “Zuo Yue Zi” in British Columbia. J Clin Nurs. 2018;27(7–8):e1385–94. [DOI] [PubMed] [Google Scholar]
- 53.Grewal SK, Bhagat R, Balneaves LG. Perinatal beliefs and practices of immigrant Punjabi women living in Canada. J Obstet Gynecol Neonatal Nurs. 2008;37(3):290–300. [DOI] [PubMed] [Google Scholar]
- 54.Lee T-Y, Landy CK, Wahoush O, Khanlou N, Liu Y-C, Li C-C. A descriptive phenomenology study of newcomers’ experience of maternity care services: Chinese women’s perspectives. BMC Health Serv Res [Internet]. 2014. [cited 2019 Jan 16];14(1). Available from: http://bmchealthservres.biomedcentral.com/articles/https://doi.org/10.1186/1472-6963-14-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Winn A, Hetherington E, Tough S. Caring for pregnant refugee women in a turbulent policy landscape: perspectives of health care professionals in Calgary, Alberta. Int J Equity Health [Internet]. 2018. [cited 2019 Jan 16];17(1). Available from: https://equityhealthj.biomedcentral.com/articles/https://doi.org/10.1186/s12939-018-0801-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ahmad F, Driver N, McNally MJ, Stewart DE. “Why doesn’t she seek help for partner abuse?” An exploratory study with South Asian immigrant women. Soc Sci Med. 2009;69(4):613–22. [DOI] [PubMed] [Google Scholar]
- 57.Logie CH, Kennedy VL, Tharao W, Ahmed U, Loutfy MR. Engagement in and continuity of HIV care among African and Caribbean Black women living with HIV in Ontario, Canada. Int J STD AIDS. 2017;28(10):969–74. [DOI] [PubMed] [Google Scholar]
- 58.Hulme J, Moravac C, Ahmad F, Cleverly S, Lofters A, Ginsburg O, et al. “I want to save my life”: conceptions of cervical and breast cancer screening among urban immigrant women of South Asian and Chinese origin. BMC Public Health. 2016;16(1):1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sou J, Shannon K, Li J, Nguyen P, Strathdee SA, Shoveller J, et al. Structural determinants of inconsistent condom use with clients among migrant sex workers: findings of longitudinal research in an urban Canadian setting. Sex Transm Dis. 2015;42(6):312–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sou J, Goldenberg SM, Duff P, Nguyen P, Shoveller J, Shannon K. Recent im/migration to Canada linked to unmet health needs among sex workers in Vancouver, Canada: findings of a longitudinal study. Health Care Women Int. 2017;38(5):492–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Higginbottom GM, Safipour J, Yohani S, O’Brien B, Mumtaz Z, Paton P, et al. An ethnographic investigation of the maternity healthcare experience of immigrants in rural and urban Alberta, Canada. BMC Pregnancy Childbirth [Internet]. 2016. [cited 2019 Jan 16];16(1). Available from: http://bmcpregnancychildbirth.biomedcentral.com/articles/https://doi.org/10.1186/s12884-015-0773-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Merry LA, Gagnon AJ, Kalim N, Bouris SS. Refugee claimant women and barriers to health and social services post-birth. Can J Public Health. 2011;102(4):286–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wilson-Mitchell K, Rummens J. Perinatal outcomes of uninsured immigrant, refugee and migrant mothers and newborns living in Toronto, Canada. Int J Environ Res Public Health. 2013;10(6):2198–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jarvis C, Munoz M, Graves L, Stephenson R, D’Souza V, Jimenez V. Retrospective review of prenatal care and perinatal outcomes in a group of uninsured pregnant women. J Obstet Gynaecol. 2011;33(3):235–43. [DOI] [PubMed] [Google Scholar]
- 65.Ganann R, Sword W, Thabane L, Newbold B, Black M. Predictors of postpartum depression among immigrant women in the year after childbirth. J Womens Health. 2016;25(2):155–65. [DOI] [PubMed] [Google Scholar]
- 66.Donnelly TT. Challenges in providing breast and cervical cancer screening services to Vietnamese Canadian women: the healthcare providers’ perspective. Nurs Inq. 2008;15(2):158–68. [DOI] [PubMed] [Google Scholar]
- 67.Vahabi M, Lofters A. Muslim immigrant women’s views on cervical cancer screening and HPV self-sampling in Ontario, Canada. BMC Public Health [Internet]. 2016. [cited 2019 Jan 16];16(1). Available from: http://bmcpublichealth.biomedcentral.com/articles/https://doi.org/10.1186/s12889-016-3564-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Redwood-Campbell L, Fowler N, Laryea S, Howard M, Kaczorowski J. “Before you teach me, I cannot know”: immigrant women’s barriers and enablers with regard to cervical cancer screening among different ethnolinguis. Can J Public Health. 2011;102(3):230–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ochoa SC, Sampalis J. Risk perception and vulnerability to STIs and HIV/AIDS among immigrant Latin-American women in Canada. Cult Health Sex. 2014;16(4):412–25. [DOI] [PubMed] [Google Scholar]
- 70.Guruge S, Humphreys J. Barriers affecting access to and use of formal social supports among abused immigrant women. J Sociol Soc Policy. 2009;41(3):22. [PubMed] [Google Scholar]
- 71.Newbold KB, Willinsky J. Providing family planning and reproductive healthcare to Canadian immigrants: perceptions of healthcare providers. Cult Health Sex. 2009;11(4):369–82. [DOI] [PubMed] [Google Scholar]
- 72.Wiebe E. Contraceptive practices and attitudes among immigrant and nonimmigrant women in Canada. Can Fam Physician. 2013;59(10):e451–5. [PMC free article] [PubMed] [Google Scholar]
- 73.Lofters AK, Vahabi M, Kim E, Ellison L, Graves E, Glazier RH. Cervical cancer screening among women from muslim-majority countries in Ontario. Canada Cancer Epidemiol Prev Biomark. 2017;26(10):1493–9. [DOI] [PubMed] [Google Scholar]
- 74.Peláez S, Hendricks KN, Merry LA, Gagnon AJ. Challenges newly-arrived migrant women in Montreal face when needing maternity care: health care professionals’ perspectives. Glob Health [Internet]. 2017. [cited 2019 Jan 16];13(1). Available from: http://globalizationandhealth.biomedcentral.com/articles/https://doi.org/10.1186/s12992-016-0229-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ng C, Newbold KB. Health care providers’ perspectives on the provision of prenatal care to immigrants. Cult Health Sex. 2011;13(5):561–74. [DOI] [PubMed] [Google Scholar]
- 76.Higginbottom GM, Safipour J, Mumtaz Z, Chiu Y, Paton P, Pillay J. “I have to do what I believe”: Sudanese women’s beliefs and resistance to hegemonic practices at home and during experiences of maternity care in Canada. BMC Pregnancy Childbirth [Internet]. 2013. [cited 2019 Jan 16];13(1). Available from: http://bmcpregnancychildbirth.biomedcentral.com/articles/https://doi.org/10.1186/1471-2393-13-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vanthuyne K, Meloni F, Ruiz-Casares M, Rousseau C, Ricard-Guay A. Health workers’ perceptions of access to care for children and pregnant women with precarious immigration status: health as a right or a privilege? Soc Sci Med. 2013;93:78–85. [DOI] [PubMed] [Google Scholar]
- 78.Reitmanova S, Gustafson DL. “They can’t understand it”: maternity health and care needs of immigrant muslim women in St. John’s, Newfoundland. Matern Child Health J 2008;12(1):101–11. [DOI] [PubMed] [Google Scholar]
- 79.Alaggia R, Regehr C, Rishchynski G. Intimate partner violence and immigration laws in Canada: how far have we come? Int J Law Psychiatry. 2009;32(6):335–41. [DOI] [PubMed] [Google Scholar]
- 80.Higginbottom GMA, Safipour J, Yohani S, O’Brien B, Mumtaz Z, Paton P. An ethnographic study of communication challenges in maternity care for immigrant women in rural Alberta. Midwifery. 2015;31(2):297–304. [DOI] [PubMed] [Google Scholar]
- 81.Merry L, Semenic S, Gyorkos TW, Fraser W, Gagnon AJ. Predictors of unplanned cesareans among low-risk migrant women from low- and middle-income countries living in Montreal, Canada. Birth. 2016;43(3):209–19. [DOI] [PubMed] [Google Scholar]
- 82.Khadilkar A, Chen Y. Rate of cervical cancer screening associated with immigration status and number of years since immigration in Ontario, Canada. J Immigr Minor Health [Internet]. 2012. [cited 2019 Mar 7]; Available from: http://link.springer.com/https://doi.org/10.1007/s10903-012-9711-6 [DOI] [PubMed] [Google Scholar]
- 83.O’Mahony JM, Donnelly TT. How does gender influence immigrant and refugee women’s postpartum depression help-seeking experiences? J Psychiatr Ment Health Nurs. 2013;20(8):714–25. [DOI] [PubMed] [Google Scholar]
- 84.Siriwardhana C, Ali SS, Roberts B, Stewart R. A systematic review of resilience and mental health outcomes of conflict-driven adult forced migrants. Confl Health. 2014;8:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Oram S, Stöckl H, Busza J, Howard LM, Zimmerman C. Prevalence and risk of violence and the physical, mental, and sexual health problems associated with human trafficking: systematic review. PLOS Med. 2012;9(5):e1001224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Boerleider AW, Wiegers TA, Manniën J, Francke AL, Devillé WLJM. Factors affecting the use of prenatal care by non-western women in industrialized western countries: a systematic review. BMC Pregnancy Childbirth. 2013;13:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bollini P, Pampallona S, Wanner P, Kupelnick B. Pregnancy outcome of migrant women and integration policy: a systematic review of the international literature. Soc Sci Med. 2009;68(3):452–61. [DOI] [PubMed] [Google Scholar]
- 88.Heaman M, Bayrampour H, Kingston D, Blondel B, Gissler M, Roth C, et al. Migrant women’s utilization of prenatal care: a systematic review. Matern Child Health J. 2013;17(5):816–36. [DOI] [PubMed] [Google Scholar]
- 89.International Organization for Migration. Social determinants of migrant health [Internet]. International Organization for Migration. 2017. [cited 2019 Feb 6]. Available from: https://www.iom.int/social-determinants-migrant-health [Google Scholar]
- 90.Ganann R, Sword W, Black M, Carpio B. Influence of maternal birthplace on postpartum health and health services use. J Immigr Minor Health. 2012;14(2):223–9. [DOI] [PubMed] [Google Scholar]


