Abstract
Mycobacterium tuberculosis (Mtb), the main etiology of tuberculosis (TB), is predominantly an intracellular pathogen that has caused infection, disease and death in humans for centuries. Lipid droplets (LDs) are dynamic intracellular organelles that are found across the evolutionary tree of life. This review is an evaluation of the current state of knowledge regarding Mtb-LD formation and associated Mtb transcriptome directly from sputa.
Based on the LD content, Mtb in sputum may be classified into three groups: LD positive, LD negative and LD borderline. However, the clinical and evolutionary importance of each state is not well elaborated. Mounting evidence supports the view that the presence of LD positive Mtb bacilli in sputum is a biomarker of slow growth, low energy state, towards lipid degradation, and drug tolerance. In Mtb, LD may serve as a source of chemical energy, scavenger of toxic compounds, prevent destruction of Mtb through autophagy, delay trafficking of lysosomes towards the phagosome, and contribute to Mtb persistence. It is suggest that LD is a key player in the induction of a spectrum of phenotypic and metabolic states of Mtb in the macrophage, granuloma and extracellular sputum microenvironment. Tuberculosis patients with high proportion of LD positive Mtb in pretreatment sputum was associated with higher rate of poor treatment outcome, indicating that LD may have a clinical application in predicting treatment outcome.
The propensity for LD formation among Mtb lineages is largely unknown. The role of LD on Mtb transmission and disease phenotype (pulmonary TB vs extra-pulmonary TB) is not well understood. Thus, further studies are needed to understand the relationships between LD positivity and Mtb lineage, Mtb transmission and clinical types.
Keywords: Mycobacterium, Sputum, Tuberculosis, Lipid droplet, Transcriptome, Host-pathogen interaction, Transmission, Treatment outcome, Lineage
Introduction
Mycobacterium tuberculosis
The genus Mycobacterium encompassed over 170 species and the pathogenic species are classified in to three: Mycobacterium tuberculosis complex (MTBC: Mycobacterium tuberculosis, Mycobacterium africanum, Mycobacterium bovis, Mycobacterium microti, Mycobacterium canettii, Mycobacterium caprae), Mycobacterium leprae and M. ulcerans. Among the species in MTBC, Mycobacterium tuberculosis (Mtb) is the main etiological agent of tuberculosis (TB) and is an intracellular pathogen that has ravaged humanity for centuries [1]. The evolutionary success of Mtb is attributed to its ability to flip-flop between different metabolic/phenotypic states, adaptation to diverse microenvironments, inhibition of phagolysosome fusion, and formation of necrotic granuloma [2, 3]. More than 24.8% of the global human population may harbor Mtb [4] in different fatty tissues [5] in the form of latent TB. Ten million active infections and 1.4 million deaths were reported in 2019 [6]. The lipid-rich sputum, and its source pulmonary granuloma microenvironment carries phenotypically heterogeneous population of Mtb [7].
Lipid and lipid droplet in M. tuberculosis
Lipid is an inclusive term for fats and lipoids. Lipids include all of the alcohol ether soluble constituents of protoplasm such as fats, oils, waxes and several complex lipids (phospholipids, glycolipids, sulfolipids, aminolipids, chromolipids, and fatty acids) [8, 9]. Mycobacteria contain different types of structural [10, 11] and nonstructural [12] lipids. Lipids are a major source of energy [13] and play a vital role in virulence, pathogenicity, and persistence [3]. Unlike other prokaryotes, 60% of Mtb cell-wall constituents are lipids, mainly mycolic acids. Moreover, 40% of the dry weight of mycobacteria is derived from lipids. Mtb stores its chemical energy in the form of neutral lipids by forming emulsion vesicles inside the aqueous phase cytoplasm [14]. In general, lipids are the rations, attire and armor of Mtb [15]; as such, the diagnosis, treatment, drug resistance [16] and immunological lifecycle of Mtb [17] is heavily relies on membrane and/or cytoplasmic lipids.
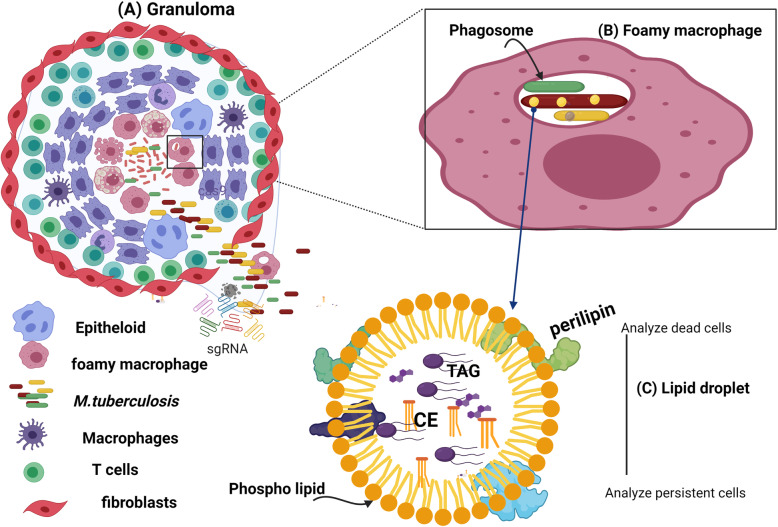
Cells store excess lipids inside the cytoplasm and this stored lipid is known by different names depending on the type of cells and tissue. These names includes lipid droplet (LD), lipid body (LB), intracellular lipid inclusions (ILI), oil body (OB), adiposome, spherosome and oleosome. Lipid droplets are pervasive and dynamic subcellular organelles of diverse morphological and functional diversity [18–21] across evolutionary tree of life. Lipid droplets comprised of a hydrophobic core of neutral lipids (triacylglycerol, TAG and cholesterol ester, CE) surrounded by a phospholipid monolayer of phosphatidylcholine (PC), phosphatidylethanolamine (PE), phosphatidylinositol (PI) and lyso-phospholipids; decorated with different types of proteins such as Perilipins (PLIN) [22, 23] (Fig. 1). For a detailed understanding regarding the (cell) biology and biophysics of LD, readers are advised to refer these excellent reviews [26, 27].
Fig. 1.
A:Necrotic granuloma, B: Foamy macrophages that contain LD-positive Mtb in granuloma tissue, phagocytosed Mtb C: Lipid droplet. A: The necrotic granuloma is a cryptic infectious immunopathological architecture and compacted collection phagocytic cells. It is the hallmark of tuberculosis [24]. Evidence showed that, except macrophages which serve as a feeder for new Mtb infection, innate immunity has only a little role in the initiation of granuloma formation and bacterial virulence factors such as trehalosdimycolate and ESX-1 are the driving factors for priming granuloma formation [25]. Once it is primed, dendritic cells migrate to regional lymph nodes, activate Th cells making the granuloma mature through layering of cells (macrophage, foamy macrophage, epithelioid, T cells and fibroblasts) [25]. The macrophage is the predominant phagocytic cell which occurs in differentiated forms. These are epithelioid, multinucleated giant cells, foamy macrophages and ruffled membrane macrophages [24]. Mtb might be found in the granuloma microenvironment due to rupture of phagosome and foamy macrophages. When the granuloma ruptures Mtb will be seeded to the environment through coughing, sneezing and talking. The metabolism and the level of stress in each microenvironment is different, driving Mtb into at least three distinct phenotypic and metabolic states; actively replicating (green), Lipid droplets (LD) loaded persister phenotype (red) and borderline between the two states (yellow). B: A macrophage that ingests Mtb through phagocytosis may harbor multiple Mtb phenotypes and may become a warehouse of lipid and serving as an energy reserve. These lipid-loaded macrophages are called foamy macrophages). C: Lipid droplets are composed of a hydrophobic core of neutral lipids (triacylglycerol, TAG and cholesterol ester, CE) surrounded by a phospholipid monolayer (phosphatidylcholine (PC), phosphatidylethanolamine (PE), phosphatidylinositol (PI) and lyso-phospholipids) decorated with different proteins. LD is an efficient energy storage organelle, as the most compacted and efficient means to store excess lipid in cells. Figures are created with BioRender.com
It was demonstrated that the LD of Mtb is derived from host fatty acids and that isocitrate lyase (encoded by icl) is the responsible enzyme that catabolizes fatty acids (FA) through glyoxylate cycle. Triacylglycerol synthase 1 (coded by tgs1) is the primary enzyme involved in triacylglycerol (TAG) synthesis and that the deletion of the tgs1 gene led to complete loss of TAG accumulation by Mtb [28]. The role of sputum derived LD positive Mtb in treatment outcome and transmission has been demonstrated [29]. The presence of LD-positive Mtb bacilli in sputum is a biomarker of slow growth, low energy state, lipid degradation, anaerobic metabolism, and non-mutational drug tolerance. Sputum-derived LD-positive Mtb transcriptome data reveals distinct patterns of gene expression; displaying up- and down-regulation of specific metabolic pathways in sputum microenvironment. In general, the LD profile and transcriptome of Mtb directly from sputa are real-time metabolic, phenotypic and physiological markers of the Mtb population diversity and dynamics. However, the relationships between Mtb LD with Mtb lineages, Mtb transmission capacity and clinical pathology (i.e., pulmonary TB vs extra pulmonary TB) are not well studied or understood. We hypothesize that LD-loaded Mtb cells in sputum are like “rocket blast off for planned orbital mission”. Thus, this review synthesized the current state of Mtb LD knowledge and showed gaps for fueling future areas of research.
Advent of M. tuberculosis lipid droplet research
The presence of fatty material inside the cytoplasm of prokaryotic cells was first demonstrated in 1946 by Burdon using the technique of Sudan black intracellular staining [30]. According to this classic experiment, noticeable amounts of LD were found in the majority of studied bacteria [30]. At that time, more LDs were observed in saprophytic and Mycobacterium leprae than in Mtb species [30]. With the aim of determining the precise organization of lipids in the envelope domain of living Mycobacteria, Christensen et al 1999 [31] developed an improved (fluorescent lipophilic probes) technique that is less disruptive than detergents [32] or ultra-sonication [33]. After probe labeling of cultivated Mtb, cells were observed by phase-contrast and epifluorescence microscopy. Using this technique, distinct lipid domains of Mycobacteria were visualized, including the envelope and LDs [31]. Generally, the lipid domains of Mycobacteria are comprised of three parts; the annular envelope, internal peripheral deposits contiguous with the envelope, and distinct LDs that are not associated with the envelope [31].
Following Burdon [30] and Christensen et al [31], Garton and colleagues [29] advanced the field through biochemically characterizing LD in M. smegmatis and Mtb, and by analyzing factors affecting lipid formation, and the synthesis pathways in these mycobacterial species. The effects of various chemicals and growth conditions on LD were examined using Youmans’ and Middle brook 7H10 culture medias. Cells were stained with Auramine-O followed by Nile red and then stained regions were detected by epifluorescence microscope. Images were captured using a microcomputer controlled CCD camera [29]. The findings showed that, in low-carbon Youmans’ broth (YB), M. smegmatis showed high annular pattern and low level of LD. In contrast, in low-nitrogen YB, the annular labelling was lost and prominent LDs were observed. In addition, this study proved that LDs were formed during stationary-phase of growth. Furthermore, this study confirmed apparent indifference to carbon sources such as glucose vs glycerol on LDs formation. However, addition of exogenous fatty acids (oleic or palmitic) promoted the formation of LD, confirming the decisive role of fatty acids for Mtb energy systems and structural carbon sources. Further analysis identified the chemical composition of LD in M. smegmatis. For this, the non-polar lipids were extracted and analyzed using thin layer chromatography, Proton Nuclear Magnetic Resonance (NMR) and gas chromatography-mass spectrometry (GC-MS). The results showed that TAG was the principal component. Extending the M. smegmatis research above into pathogenic Mtb isolated from TB patients’ sputa confirmed the presence of LD in Mtb from sputum, and from stationary phase of cultured Mtb [29]. LD synthesis pathway analysis showed that TAG might be imported directly from macrophages or synthesized de novo [12, 13]. For a detailed understanding of LD nucleation, readers are advised to refer to excellent reviews elsewhere [34–36].
Lipid droplets in macrophage and Mtb evolutionary arms race
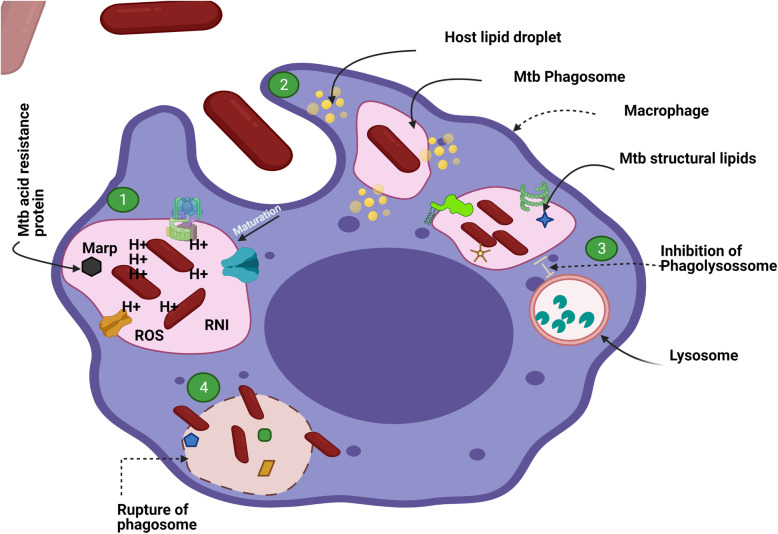
Mtb can exist extracellularly in the granuloma microenvironments, or in the cytoplasm or phagosome of (foamy) macrophages (FM). Several hypotheses have been proposed regarding the survival strategies of Mtb inside the acidic phagosome of macrophage [37]. From these, the majority of studies support the view that Mtb survives inside the hostile phagosome environment by avoiding the fusion of lysosome with phagosome [38–41]. Briefly, Mtb avoids phagolysosome amalgamation through retaining immature phagosome markers (Rab5, Rab11 and Coronin1/TACO) and blocking the recruitment of mature endosome markers (Rab7, CD63 and Cathepsin D) at phagosome surfaces [37].
A second view suggests that phagolysosome fusion occurs, but that Mtb resides inside the hostile phagosome environment through upregulation of serine proteases such as Mycobacterial acid resistance Protease (MarP) [42]. MarP is an acid tolerance and virulence factor. The seminal experiment was carried out by Botella et al. (2017) to differentiate whether Mtb survival is via acid tolerance or phagolysosome fusion avoidance. To resolve this issue, two transposon mutants were prepared; marP::Tn (acid susceptible) and ptpA::Tn (↑lysosomal trafficking for enhancing lysosomal action). The study confirmed that, marP::Tn mutants became hypersusceptible to lysosomal content and growth attenuation occurred. Furthermore, 25 times higher attenuation rate was observed among marP::Tn (acid susceptibility) than ptpA::Tn (phagolysosome fusion) mutants. This showed that lysosomal acid tolerance was a more significant determinant than avoidance of phagosome-lysosome fusion [42]. Botella and colleagues further elaborated the mechanism of action of MarP. Accordingly, RipA, a peptidoglycan hydrolase is a substrate for MarP and acid tolerance is achieved when MarP cleaves RipA for its biological function [43].
The third hypothesis suggests that Mtb survives inside the phagosome through its interaction with host LD. Host LD helps Mtb-phagosome evading the macrophage’s defense systems [44]. In this survival pathway, the different Mtb cell wall components are participated. For instance, lipoarabinomannan (LAM) block endosome maturation and phosphatidylinositol mannosides (PIM) nourish the pathogen [44]. Additionally, the LucA protein from Mtb forms a complex with Mce1 and Mce4 fatty acid transporters to scavenge cholesterol and fatty acids from the cytoplasm of the macrophage [45]. The conclusion is that two or more of these survival strategies are employed by Mtb. Figure 2 below illustrates these Mtb survival strategies.
Fig. 2.
Survival strategies of M. tuberculosis inside the phagosome environment. This figure illustrates the mechanisms proposed to allow Mtb to survive inside the phagosome or Mtb escaping mechanisms from host defense. (1) Mtb survives inside the hostile phagosome by expressing Mycobacterial acid resistance Protein (MarP), a protein that buffers the acidic milieu. (2) Mtb survives inside the phagosome and evades the host immune response by residing apposition to the host lipid droplet. (3) Mtb avoids phagosome maturation and phagolysosome fusion by tagging early endosome markers (Rab5, Rab11, coronin1/TACO) and avoiding attachment and activation of several others (Rab7, CD63, lysosomal hydrolase, cathepsin D), which inhibits the proton–ATPase activity. Mtb accomplishes this by expressing various virulent factor lipoproteins (Man LAM, secreted phosphatase, lipid phosphatidylinositol 3 phosphate, phosphatase ptpA, TDM). (4) Mtb exits the phagosome and replicates inside the cytoplasm by rupturing the phagosome expressing ESX-1, DIM/PDIM, and phospho lipase A2 [46]. This phagosomal escape is advantageous to the pathogen for acquiring essential amino acids (arginine, methionine, or leucine), replication and dissemination [47]. Mtb: M. tuberculosis; Man LAM: Mannosylated lipoarabinomannan; TDM: Trehalose-6,6′-dimycolate; ESX-1: Early secretary antigenic target 6 (ESAT6) secretion system like protein; TACO: tryptophan aspartate containing coat protein, also named P57, Coronin1; DIM/PDIM: phthiocerol dimycocerosates. Figure is created with BioRender.com
Whether macrophage LD formation is in favor of pathogen survival or part of the host defense is a subject of on-going debate. Some studies suggest that host LD gives an evolutionary advantage to the bacilli by serving as depot of chemical energy [28, 44, 48] and shelter [49, 50]. In Barisch et al (2017) review, host LD is found in close apposition to the Mtb phagosome, serving as a lipid supply for Mtb LD formation via fusion, coalescence or lipophagy-dependent internalization [48]. Peyron et al (2008) supported this hypothesis [51], showing that FM formation is a unique feature of pathogenic Mycobacteria (Mtb, M. avium) and oxygenated mycolic acid played a role in the differentiation of macrophages into FM. Peyron and colleagues infect macrophages with Mtb and scanned the formation of the granuloma at days 3 and 11 using electron microscopy. At 3-days after infection, Mtb was found only inside the phagosome or around the granuloma microenvironment but not inside the cytoplasm of FM. At 11-days post infection, the FM population increased from 9% (day− 3 post infection) to 41%, the size of LD of FM were also increased (> 5 LD/FM), and 1–20 phagocytosed Mtb were observed. While 60% of phagosomes were evenly distributed in the cytoplasm of FM, nearly 21% of phagosomes were stationed in close proximity to the FM-LD and progressive engulfment was observed. This study also noted that only Mtb that transferred from the phagosome to FM-LD became LD positive, thereby proposing that Mtb LD may be derived from FM-LD [51]. According to Daniel et al. (2011), hypoxia is also another key factor for macrophage LD formation, where host LD in the form of TAG were incorporated into Mtb LD [28]. Taken together, these studies support the view that, host and Mtb LDs benefit the evolutionary success of the pathogen.
In apparent contradiction to the above research, a study by Knight et al. (2017) suggested that host LD formation is entirely dependent on IFN-γ/HIF-1α activation and few LDs are observed without these cytokines. For instance, when primary murine bone marrow derived macrophages were infected with Mtb, very few, (average of < 1) LD were formed by macrophages. However, a large number of LD (average of > 10 LDs/macrophage) were formed when these Mtb-infected macrophages were treated with IFN-γ; 100% of macrophages accumulated LD. Additionally, the authors showed that Mtb can extricate different types of lipid from the host. Knight et al. concluded that Mtb LD and host LD formation are two opposing and uncoupled phenomena; where Mtb LD are synthesized as means of Mtb survival, whereas host LD synthesis is a mechanism of host defense [52]. Other studies have also reported that the accumulation of LD in the macrophage cytoplasm is part of a coordinated host defense mechanism [52–54].
The up-regulation of Mtb genes (hspX, icl1, tgs1, dosR, lipY, pckA) related to LD metabolism and hypoxia in the granuloma and inside the phagosome environment confirmed the rescue function of Mtb-LD [55]. Taken together, the evidence supports the view that Mtb LD formation serves the pathogen, and may act as a source of chemical energy [12, 56], shelter of genomic DNA [50], scavenger of toxic free fatty acids [12], creating non-mutational phenotypic heterogeneity [7] such as formation of antibiotic tolerance [55, 57–59] and evading host immune cells by hiding its pathogen associated molecular patterns (PAMP) [60, 61]. The host LD and the Mtb cell wall lipid components are also essential for Mtb survival by avoiding autophagy and delaying lysosomal trafficking towards the phagosome [62, 63].
Clinical relevance of M. tuberculosis lipid droplets
Dynamics and role of LD positive Mtb during TB treatment
Sloan et al 2015 hypothesized that the proportion of LD-positive Mtb in sputum influences the outcome of TB treatment. To address this, sputum culture and Auramine-LipidTox staining of sputum smears were carried out on consecutively collected samples through the treatment period and the treatment outcome was recorded as good or bad [64]. The study found a higher proportion of LD-positive Mtb among patients with poor treatment outcome [64]. Kayigire et al (2015) assessed the dynamics of LD positive Mtb in sputum over treatment period. The study identified three types of Mtb in TB patients; vegetative cells that stained positively with Auramine-O (green), LD-positive Nile-red stained Mtb (red) and Mtb cells stained by both (cream cells; that were borderline between the two), whose relative proportions changed over the course of treatment. Prior to the start of anti-TB treatment, green cells predominate and LD-positive cells (red) shared a small proportion of all Mtb. As treatment proceeded, there was a clear shift towards fewer replicating/green Mtb cells and more borderline and red LD-positive cells [65]. Taken together, these data suggested the value of LD staining techniques for monitoring treatment outcomes. Since LD-positive Mtb appear to be drug-tolerant (or drug-resistant) and refractory to staining with Auramine O, techniques targeting these phenotypes might have higher resolution and become a sensitive biomarker for treatment monitoring and predicting treatment outcome. Moreover, such studies may combine with drug discovery programs that target drug-tolerant populations of Mtb [66–68].
The role of Mtb-LD in TB transmission
The role of LD in Mtb transmission is a controversial issue that warrants further scrutiny [29, 69]. Jones-López and colleagues determined the variation in Mtb transmission from infected households to their close contacts. The finding showed significant heterogeneity of Mtb transmission among human living together in a single household. This study classified isolates into Mtb high transmission (Mtb-HT) and Mtb low transmission (Mtb-LT) strains [69]. According to this study, Mtb-LT isolates showed an increased LD accumulation than Mtb-HT isolates. Moreover, in Animal model study by Verma et al, Mtb-LT isolates showed high growth rate. Furthermore, diffused inflammatory lung pathology, high CD8+ T cells, high inflammatory response and high mortality rate were observed among TB patients infected with Mtb-LT isolates. On the contrary, well defined circumscribed lesions, high degree of granuloma, caseous necrosis, cavitary lesion and high transmission rate were found among patients infected with Mtb-HT isolates. Hence, this study suggest that the presence of LD per se does not confer a specific transmission fitness and transmission phenotype [70], a result in contrast with the Garton et al study [29]. Collectively, TB transmission rate is deduced to be driven by several factors and TB transmission study should consider clinical presentation, host immunity, pathogen and environmental axis. Since sputum derived Mtb are phenotypically and metabolically heterogeneous, which phenotypes (containing differing proportions of LD positive Mtb, LD negative, border line or all types) are more transmissible is unknown and further study is required.
LD-positive Mtb in pulmonary and extra pulmonary TB
Little is known about the relationship between Mtb-LD formation and clinical manifestation of disease as pulmonary TB (PTB) versus extra-pulmonary TB (EPTB). Lung is the primary site of TB disease initiation and lymph node is the primary site of adaptive immune initiation. Initiation of an adaptive immune response to Mtb depends on the transport of live bacteria from the lung to the mediastinal lymph nodes, and delay of this process may be advantageous for the pathogen [71]. Ganchua et al (2018) suggested that the lymph node (LN) provides an ecological niche for Mtb, based on evidence of higher survival of Mtb in the LN than in lung granuloma. This may be because granulomas that form in LNs lack B cell-rich tertiary lymphoid structures. With this, LNs are not only sites of antigen presentation and immune activation during infection, but also a niche that is protected from adaptive immune-mediated responses [72]. Severe diseases like EPTB is the outcome of a co-evolutionary mismatch [73]. The pathogen’s fitness depends on its ability to cause a high level of damage to its human host [73, 74]. Little is known about relative proportions of LD-positive Mtb in pulmonary parenchymal and lymph node tissue. In this regard, Maji and colleagues analyzed the transcriptome of tubercular lymphadenitis tissue and observed downregulation of host lipid metabolism related genes, in contrast to pulmonary tissue. This study confirmed the differential expression of lipid metabolic signatures between TB lymphadenitis and PTB [75]. However, the Mtb-LD related transcriptome and the proportion of LD positive Mtb among PTB and EPTB was not determined. The observation of a shift from predominant pulmonary TB to predominant LN-associated TB in certain geographic regions like Ethiopia, is provocative. The link between Mtb lineages and type of TB (PTB Vs EPTB) is unclear [76, 77] and some association between Mycobacterium africanum (MAF) and EPTB [78–80] have been reported. In general, LD formation profiling among Mtb and MAF isolates disaggregated by types of TB (EPTB Vs PTB) might narrow the existing knowledge gap.
Lipid droplets formation and Mtb lineages
The Beijing lineage (lineage 2) of Mtb appears to be the slowest in time to culture conversion after the start of anti-TB treatment [81]. A study comparing the phenolic glycolipid (PGL), TAG and dosR regulon of Beijing lineages with lineage 3 and lineage 4 showed striking variation among lineages [82]. Briefly, while 10, 60 and 80% isolates under Beijing lineages (groups 3, 4 and 5 respectively) contain PGL, other strains from Beijing and non-Beijing lineages did not produce PGL. Additionally, while all the 36 isolates from Beijing lineages included in the analysis produced TAG, the 18 non-Beijing lineages included in the analysis failed to synthesize detectable amounts of TAG during in vitro aerobic culture [82]. However, while the authors reported 100% TAG production in Beijing lineage (L2 strains), they reported no accumulation of TAG in L3 and L4 Mtb isolates, a result that seems very unlikely. The culture conditions might be one factor leading to this discrepancy.
Diarra et al (2018) conducted a prospective cohort study to determine whether M. africanum (MAF, L6) responds faster to TB treatment more quickly than Mtb-L4, using Auramine O and Fluorescein Diacetate (FDA) viability stains. The authors found that MAF responded better to TB treatment but time kill kinetics was slower for MAF than L4 [81]. One would predict that slow smear conversion might lead to more transmission and drug resistance, however, based on clustering and drug resistance data, rates of transmission and drug resistance were not higher for MAF compared with Mtb [83, 84]. The link between poor treatment outcome, drug tolerance and LDs is well explained elsewhere [28, 64, 65]. The slow growth rate [79, 81, 85] and slow clinical recovery rate associated with MAF strains among TB cases has also been reported elsewhere [86]. Similar to MAF, Mtb lineage 7, which is restricted to Ethiopia and the Horn of Africa, grew more slowly in vitro and produced smaller colonies on solid media [87] in comparison to other Mtb strains. It is not known whether any of these characteristics correlate with LD. Collectively, the propensity of Mtb LD formation among lineages is known and a simple LD comparative analysis might provide insight regarding the differential LD formation among Mtb lineages.
The proportion of LD-positive Mtb in sputum
The clinical relevance of LD-positive Mtb bacilli in sputum was first elucidated by Garton and colleagues [29, 88]. These studies concluded that the proportion of LD-positive Mtb in sputum lies between 3 and 86%, with 2–8 LDs/bacilli [29]. Growth rate is significantly associated with the proportion of LD-positive Mtb bacilli in sputum [29]. Garton and colleagues concluded that the replicating phenotypes of Mtb in sputum were a minor component, and LD-positive Mtb bacilli were predominant. This report contrasted with that of the cell culture study by Daniel et al [28]. Daniel et al characterized dynamic of Mtb LD formation inside the hypoxic FMs incubated under 1% O2. After 0, 3, and 5 days of incubation from this hypoxic state, Mtb recovered from FMs were stained with dual Auramine-O and Nile red staining techniques. It was found that the fraction of the Mtb population positive for Auramine O staining decreased from ~ 86% at day-0 to ~ 40% at day-5, while Nile Red-positive LD-positive cells increased with time from ~ 35% prior to hypoxic treatment to ~ 81% at day-5 of 1% O2 (hypoxia) treatment, more than two-fold increment [28]. Taken together, studies which could determine the Mtb population (LD positive, LD negative, borderline) dynamic is desirable.
Transcriptome profile of M. tuberculosis from patient sputa
The spectrum of Mtb metabolic reprogramming is better studied through transcriptome profiling. This is because the transcriptome of sputum-derived Mtb provides genome-wide information on the real time metabolic state of Mtb populations. In addition, the state of Mtb metabolic reprogramming is more readily ascertained from transcriptome data than from genomic data, through quantifying the changing expression levels of Mtb transcripts in distinct physiological conditions. Hence, evidences on this subtopic are synthesized from the transcriptome of sputum-derived Mtb in comparison with the transcriptomes of Mtb grown in vitro culture and over the course of TB treatment. This section reviewed only original articles and the methodology of the studies are summarized in Table 1.
Table 1.
Transcriptome profiling and validation techniques used for Mtb sputum transcriptomics
| Comparative transcriptomics of SMtb | RNA profiling method | Validation | #Transcript | Reference |
|---|---|---|---|---|
| SMtb vs culture with 7H10 agar /7H9 broth/Dubos a | Microarray | qRT-PCR | 516 | [29] |
| SMtb vs culture | Microarray | qRT-PCR | 557 | [89] |
| SMtb vs MAF/Mtb | qRT-PCR | 2179 | [90] | |
| SMtb vs Exponential phase of liquid culture | Dual RNA seq | Nano String | 198 | [91] |
| SMtb vs Stationary phase of liquid culture | Dual RNA seq | Nano String | 392 | [91] |
| Sputum vs MGIT 460 culture | Microarray | qRT-PCR | 1083 | [92] |
| SMtb at Day 3 vs SMtb at day0 treatment | Microarray | qRT-PCR | 109 | [92] |
| SMtb at Day7/14 vs day 0 treatment | Microarray | qRT-PCR | 39 | [92] |
| Lipid rich Dubos brothb vs Dextrose rich Dubos brothb | RNA seq | qRT-PCR | – | [60] |
| SMtb/ BAL-Mtb vs 7H9/ DTAc culture | qRT-PCR | – | [93] | |
| SMtb before Rx vs SMtb after Rx | qRT-PCR | qRT-PCR | 2411 | [94] |
| Sputum Mtb vS culture H37Rv | Microarray | qRT-PCR | – | [95] |
a7H10 agar with oleic acid-albumin-dextrose-catalase supplement or in 7H9 broth with albumin-dextrose-catalase supplement, 0.2% glycerol and 0.05% Tween-80. Hypoxic (non-replicating persistence) cultures M. tuberculosis strains H37Rv and CH were grown in Dubos Tween albumin broth. bDubos broth (Difco), without glycerol, containing 0.5% albumin, supplemented with either 0.2% dextrose or a lipid mixture (oleic acid, palmitic acid, stearic acid, at final concentration of 0.001% each, plus 0.01% cholesterol). c7H9 media (0.05% Tween 80, 0.2% glycerol, 10% ADC supplement)/ DTA: Dubos Tween albumin; for the NRP-2 model was grown in 100 mL Dubos Tween albumin (DTA). SMtb sputum-derived M. tuberculosis, Mtb Mycobacterium tuberculosis, vs versus, Rx treatment, MAF Mycobacterium africanum, L4 Lineage 4, qRT-PCR Real-Time Quantitative Reverse Transcription PCR, RNA seq RNA-sequencing, DTA Dubos Tween, BAL Broncho alveolar lavage
The key findings of the individual studies referred in Tables 2. The transcriptome data showed distinct transcriptome profiles which might be explained by differences in the technique, study populations and number of genes targeted. The sputum-derived Mtb transcriptome relatively mirrored the lung/ broncho alveolar lavage (BAL) derived Mtb transcript profile. The slight differences between the two (sputum and BAL) might be due to the higher hypoxic state of the lung than upper respiratory tracts such as bronchi and oral cavity. Hence, sputum Mtb transcriptome profiling might be a substitute for the BAL transcriptome for assessing Mtb pathogenesis and treatment conditions [93]. Comparing the Mtb transcriptome in lipid and dextrose rich medium did not showed significant differential expression [60]. The sputum-derived Mtb transcriptome is quite different from exponentially growing Mtb in animal models and in-vitro.
Table 2.
The summary of transcriptomes of M. tuberculosis in sputum versus other conditions, 2021
| Transcriptome condition | In vitro comparator | URG in sputum Mtb | DRG in sputum Mtb | Ref |
|---|---|---|---|---|
| SMtb vs Culture | 7H10 agar /7H9 broth/Dubosa | dosR, icl1, hspX, narK2, tgs1, PE/PPE | nuoB, qcrC, and ctaD | [29] |
| SMtb Vs Culture | No information | Conserved Hypotheticals. mprAB: dosR is stable |
pks15/1, pks10 Pks12, phoP, ESX 1-ESX-5 |
[89] |
| SMtb Vs Culture | Liquid culture | ACOD1/IRG1, GLUT1, MCT4, ESX-3, Rv0106, Rv2990c, ESX-3, mprA | TCA cycle, ETC, NADH dehydrogenase, pentose phosphate pathway (PPP), NAPDH, ROS. PhoP, small RNA mcr7, pks12, esat-6 and cfp-10, phoP | [91] |
| SMtb Vs Culture | MGIT 460 | Glyoxylate shunt, methylcitrate cycle (icl, prpC and rv1129c), catabolism of cholesterol and fatty acids, and tgs; Nitrate reduction (narK2/3). dosR nrdZ, narK2, rv1738, pfkB, hspX, hrp1,rv3126c and rv3128c | gltA2, kgd, mdh, korA/B, sucC, rv0247c/48c, fumC and mqo), FAS-1 (fas), FAS-II, mmaA2/3/4, cmaA2, pcaA, fadD32 and pks13, NADH dehydrogenase, cytochrome C reductase | [92] |
| SMtb Vs culture | 7H9/ DTAc | sputum and BAL had significant up-regulation of the dosR regulon | Ribosomal genes and primary metabolism genes | [93] |
| Day 7–14 days Vs day0 | None applicable | Anaerobic respiration, PE/PPE genes, is, dosR,transcriptional factors, oxidative stress, sigma factors, toxin-antitoxin modules, | TCA cycle, ATP synthesis, ribosomal proteins, pks, ESX, replication, efflux pumps, drug-activating enzymes & drug targets | [94] |
| SMtb at day 3/7/14 Vs day 0 Rx | None applicable | Mtb responses at 7 and 14 daysduring chemotherapy were most similar to that of bacillibefore drug therapy had begun | methylcitrate | [92] |
| Day14 Vs day2 | None applicable | tgs, and ATP-binding cassette transporter and toxin. Rv1258c, bacA, and mmr, rpoB. TA modules, sigma factors | ESX and ribosomal genes, drug-activating enzymes katG, pncA, and ethA, gyrase, bedaquiline target atpE | [94] |
| BAL vs sputum | 7H9/ DTAc | dosR regulon expression was higher in BAL than in sputum | BAL had lower expression of ribosome proteins | [93] |
| Lipid-NRP1 Vs Dextrose-NRP1 | Dubos brothb | Higher virulence, detoxification & adaptation, lipid metabolism, intermediary metabolism& respiration, regulatory protein | Insertion sequences & phages | [60] |
| In NRP-2 state | 7H9/ DTAc | dosR regulon, oxidative stress responses, anaerobic respiration | Growth and metabolism | [93] |
The list of genes up /down regulated is not exhaustive, only common genes listed
a7H10 agar with oleic acid-albumin-dextrose-catalase supplement or in 7H9 broth with albumin-dextrose-catalase supplement, 0.2% glycerol and 0.05% Tween-80. Hypoxic (non-replicating persistence) cultures M. tuberculosis strains H37Rv and CH were grown in Dubos Tween albumin broth. bDubos broth (Difco), without glycerol, containing 0.5% albumin, supplemented with either 0.2% dextrose or a lipid mixture (oleic acid, palmitic acid, stearic acid, at final concentration of 0.001% each, plus 0.01% cholesterol). c7H9 media (0.05% Tween 80, 0.2% glycerol, 10% ADC supplement)/ DTA: Dubos Tween albumin; for the NRP-2 model was grown in 100 mL Dubos Tween albumin (DTA). SMtb Sputum Mtb, Mtb Mycobacterium tuberculosis, URG Up regulated genes, DRG Down regulated genes, BAL Broncho alveolar lavage, NRP None replicating persistent state, Vs versus, Rx treatment, dosR Dormancy survival regulator, hspX a-crystallin homologue, narK2 nitrate/ nitrite transporter, qcrC cytochrome bc1 complex, ctaD aa3-type cytochrome c oxidase, icl1 isocitrate lyase gene, nuoB type-I NADH dehydrogenase, Pks12 Polyketide synthase, PDIMs Phthiocerol dimycocerosates, PGLs phenolic glycolipids
Relative to pretreatment expression, the mRNA abundance decreased by 50% over 12 h during the first 2 days of anti-TB treatments shots [94]. Over the course of anti-TB treatment, genes encoding drug activating enzymes such as a catalase peroxidase (katG), nicotinamidase/pyrazinamidase (pncA), and Ethionamide activator (ethA) showed repression, indicating that majority of the Mtb populations are dying and entered into drug related stress tolerance state [94]. Genes related to persister phenotypes such as triacylglycerol synthases and, ATP-binding cassette transporter and toxin molecules were induced [94].
In terms of energy utilization, the ATP synthase operon in sputum was downregulated and the transcriptome of sputum-derived Mtb was more similar to the transcriptome of Mtb during stationary phase growth than during exponential growth of Mtb in-vitro. Decrease in abundance of phoP and esx transcripts indicated a switch to lipolysis and decreased virulence [91]. PhoPR a two-component system is essential for virulence through its secretary function and its mutation leads to a loss of virulence [96]. Because the Mtb in sputum has originated from a granuloma rich in lipid, it is not unexpected that the transcriptome of sputum-derived Mtb microenvironment is enriched for transcripts involved in lipid metabolism [91, 92], microaerophilic respiration, low energy state, and persistence [29, 94].
The DosR regulon (dosR) which constitutes over 50 genes [4] is activated by low oxygen tension [97] and accumulation of oxygen byproducts such as H2O2, CO, NO, and ethanol [98]. The dosR regulon is over expressed in sputum and during anti-TB treatment [92, 94] compared with log phase in vitro culture [92, 93]. The expression of the dosR regulon is likely a general indicator of bacteria’s tolerance to oxygen and may have no direct role in LD metabolism. Hence, while expression of the dosR regulon is observed in both growing and persister populations of Mtb [29, 99], its expression is dependent on the degree of the hypoxic state. Comparatively upregulation of dosR regulon was observed among Lineage 2 Mtb than Lineage 4 Mtb from sputum [91] and among Mtb-L4 than among MAF-L6 [90]. These results suggest that upregulation of the dosR regulon is an indicator of the aerophilic state of Mtb/MAF rather than a marker of metabolic states linked to LD.
M. tuberculosis genes such as dosR regulon, hspX, mprAB and PE/PPE and those involved in the glyoxylate shunt, methylcitrate cycle, cholesterol catabolism, nitrate reduction metabolism were upregulated relative to log phase control H37Rv cells grown in vitro [29, 89, 91, 92]. In contrast, the tricarboxylic acid (TCA) cycle, electron transport chain (ETC), polyketide synthase, ESX secretion apparatus, mycolic acid synthesis, NADH dehydrogenase and cytochrome c reductase were downregulated in sputum-derived Mtb compared to log phase aerobic in vitro culture [91, 92]. During treatment, downregulation of ESX secretion and anti-TB drug activating enzymes were noticed compared with pre-treatment sputum Mtb [94]. When under extreme stress, NRP-2 state, anaerobic respiration and dosR were upregulated and genes involved in growth and metabolism were repressed [93] (Table 2). Garcia et al concluded that the transcriptomes of BAL and sputum-derived Mtb reflect a moderate level of hypoxia approximately midway on a spectrum of the hypoxic state between aerobic growth and NRP-2 [93]. En masse, the majority of genes from the information pathway, cell wall and cell processes, virulence, detoxification, adaptation, secretion, transport, intermediary metabolism and respiration [89] are repressed in Mtb from direct sputum.
Anti-TB treatment is typically monitored by microscopy and culture conversion. However, such techniques are inadequate for the detecting non-replicating drug-tolerant Mtb, which is important for predicting treatment duration, treatment outcome and drug resistance. Techniques measuring 16 s rRNA or pre-rRNA promise to add new depth to our understanding of the efficacy of drug combinations in patients [100, 101]. Demirci and colleagues assessed the diagnostic accuracy of Mtb-mRNA-based RT-qPCR technique, with the BACTEC MGIT 960 method used as the gold standard. The findings were encouraging, in that the mRNA-based method appeared to be more sensitive and specific than other methods [102]. However, additional information is needed before this technique can be translated into clinical practice. In particular, questions with regard to Mtb persistence and dormancy need to be addressed and defined [12, 29, 103–105].
Study strength and limitations
This review summarized pertinent information regarding the role of Mtb LD on host-pathogen interactions, diagnosis, treatment and transmission. As such, the review highlighted conflicting reports and advised future research areas. However, our literature search strategy is not complete and the quality of included articles were not appraised.
Conclusions
The role of LD in the co-evolutionary arms race, granuloma formation, and treatment outcome of TB must be recognized. The power of LD in determining the distinct metabolic, physiological, phenotypic state from sputum-derived Mtb is described. The presence of LD is observed universally in prokaryotes including Mtb. However, LD are more common and more abundant: 1) in BAL-derived Mtb than in sputum-derived Mtb, 2) after anti-TB drug therapy, and 3) during stationary phase than exponential phase of growth in vitro culture.
LD are a source of chemical energy and phenotypic heterogeneity. They can also delay lysosomal trafficking towards phagosomes, block autophagy, promote immune cell evasion and scavenge toxic metabolites and signaling. The influence of LD on transmissibility and virulence of Mtb is less well understood. Multiple factors from the pathogen, host and environment axis might influence Mtb transmission, however some evidence links overproduction of LD in the Mtb Beijing lineage 2 and some Mtb lineage 4 isolates with higher transmissibility/virulence.
Several different transcriptome profiles were detected in LD-positive Mtb, which could reflect sample-to-sample variation, differences in methodology or other experimental conditions. Nevertheless, we conclude that Mtb in sputum exists in a variable phenotypic and metabolic states. The dynamics of gene expression in LD-positive Mtb from sputum provides clinically-important information on the evolution and pathogenicity of Mtb. Further studies are needed to investigate the relationships between intracellular LDs and Mtb lineages, Mtb transmission capacity, clinical phenotype and Mtb pathophysiology.
Transcriptomic analysis of sputum-derived LD-positive Mtb cells could prove to be useful in clinical and research settings. For instance, lipophilic staining targeting LD-positive Mtb might be more sensitive and specific than current methods, such as ZN/ FM microscopy, which only detects actively growing Mtb. Finally, lipid metabolism-associated genes are upregulated in LD-positive Mtb. Based on this observation, it may be possible to develop an mRNA based diagnostic test that is sensitive and specific for the detection of LD-positive Mtb. Such a test could be valuable for TB diagnostics and to monitor treatment of TB. This exciting possibility will be explored in future research.
Acknowledgements
The authors would like to thank Institute of Biotechnology staffs for their encouragement and support during the review process. The review is part of a mega project funded by Institute of Biotechnology, Bahir Dar University under the project PI of Endalkachew Nibret.
Abbreviations
- BAL
Broncho alveolar lavage
- CE
Cholesterol ester
- DIM/PDIM
Phthiocerol dimycocerosates.
- DTA
Dubos Tween
- EPTB
Extra-pulmonary TB
- ESAT6
Early secretary antigenic target 6
- ESX-1
ESAT6 secretion system like protein
- ETC
Electron transport chain
- FDA
Fluorescein Diacetate
- FM
Foamy Macrophages
- GC-MS
Gas chromatography-mass spectrometry
- ILI
Intracellular lipid inclusions
- L4
Lineage 4
- LAM
Lipoarabinomannan
- LB
Lipid body
- LD
Lipid droplet
- LDs
Lipid droplets
- LN
Lymph node
- MAF
Mycobacterium africanum
- MAF
Mycobacterium africanum
- Man LAM
Mannosylated lipoarabinomannan
- MarP
Mycobacterial acid resistance Protease
- Mtb
Mycobacterium tuberculosis
- MTBC
Mycobacterium tuberculosis complex
- NMR
Proton Nuclear Magnetic Resonance
- OB
Oil body
- PC
Phosphatidylcholine
- PE
Phosphatidylethanolamine
- PGL
Phenolic glycolipid
- PI
Phosphatidylinositol
- PIM
Phosphatidylinositol mannosides
- PTB
Pulmonary TB
- qRT-PCR
Real-Time Quantitative Reverse Transcription PCR;
- RNA seq
RNA-sequencing
- Rx
Treatment
- SMtb
Sputum-derived M. tuberculosis
- TACO
Tryptophan aspartate containing coat protein
- TAG
Triacylglycerol
- TB
Tuberculosis
- TCA
Tricarboxylic acid cycle,
- TDM
Trehalose-6,6′-dimycolate
- vs
versus
- YB
Youmans’ broth
Authors’ contributions
DM: Conceived the review topic, did the literature search, and drafted the manuscript; AD, AM, SAY, TT EN, AM: contributed to writing and editing, BA, SJW, AA: helped conceive the study topic, and edit the review. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gagneux S. Ecology and evolution of Mycobacterium tuberculosis. Nat Rev Microbiol. 2018;16(4):202–213. doi: 10.1038/nrmicro.2018.8. [DOI] [PubMed] [Google Scholar]
- 2.Gengenbacher M, Kaufmann SH. Mycobacterium tuberculosis: success through dormancy. FEMS Microbio Rev. 2012;36(3):514–532. doi: 10.1111/j.1574-6976.2012.00331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fieweger RA, Wilburn KM, VanderVen BC. Comparing the metabolic capabilities of bacteria in the Mycobacterium tuberculosis complex. Microorganisms. 2019;7(6):177. doi: 10.3390/microorganisms7060177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen A, Mathiasen VD, Schön T, Wejse C. The global prevalence of latent tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2019;54(3). 10.1183/13993003.00655-2019. [DOI] [PubMed]
- 5.Neyrolles O, Hernández-Pando R, Pietri-Rouxel F, Fornès P, Tailleux L, Payán JAB, Pivert E, Bordat Y, Aguilar D, Prévost MC, Petit C, Gicquel B. Is adipose tissue a place for Mycobacterium tuberculosis persistence? PLoS One. 2006;1(1):e43. doi: 10.1371/journal.pone.0000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO . Global tuberculosis report 2020. In: WHO, editor. Global tuberculosis report 2020. Geneva: WHO; 2020. [Google Scholar]
- 7.Dhar N, Mckinney J, Manina G. Phenotypic heterogeneity in Mycobacterium tuberculosis. Microbiol Spectrum. 2016;4(6):671–697. doi: 10.1128/microbiolspec.TBTB2-0021-2016. [DOI] [PubMed] [Google Scholar]
- 8.Brown HA, Marnett LJ. Introduction to lipid biochemistry, metabolism, and signaling. Chem Rev. 2011;111(10):4–5820. doi: 10.1021/cr200363s. [DOI] [PubMed] [Google Scholar]
- 9.Fahy E, Subramaniam S, Brown HA, Glass CK, Merrill AH, Jr, Murphy RC, et al. A comprehensive classification system for lipids. Eur J Lipid Sci Technol. 2005;107(5):337–364. doi: 10.1002/ejlt.200405001. [DOI] [PubMed] [Google Scholar]
- 10.Singh P, Rameshwaram NR, Ghosh S, Mukhopadhyay S. Cell envelope lipids in the pathophysiology of Mycobacterium tuberculosis. Future Microbiol. 2018;13(06):689–710. doi: 10.2217/fmb-2017-0135. [DOI] [PubMed] [Google Scholar]
- 11.Ghazaei C. Mycobacterium tuberculosis and lipids: insights into molecular mechanisms from persistence to virulence. J Res Med Sci. 2018;23(1):63. doi: 10.4103/jrms.JRMS_904_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maurya RK, Bharti S, Krishnan MY. Triacylglycerols: Fuelling the hibernating mycobacterium tuberculosis. Front Cell Infect Microbiol. 2019;8:450. doi: 10.3389/fcimb.2018.00450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilburn KM, Fieweger RA, VanderVen BC. Cholesterol and fatty acids grease the wheels of Mycobacterium tuberculosis pathogenesis. Pathog Dis. 2018;76(2). 10.1093/femspd/fty021. [DOI] [PMC free article] [PubMed]
- 14.Chiaradia L, Lefebvre C, Parra J, Marcoux J, Burlet-Schiltz O, Etienne G, Tropis M, Daffé M. Dissecting the mycobacterial cell envelope and defining the composition of the native mycomembrane. Sci Rep. 2017;7(1):1–12. doi: 10.1038/s41598-017-12718-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Russell DG, VanderVen BC, Lee W, Abramovitch RB. Kim M-j, Homolka S et al: Mycobacterium tuberculosis wears what it eats. Cell Host Microbe. 2010;8(1):68–76. doi: 10.1016/j.chom.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pal R, Hameed S, Kumar P, Singh S, Fatima Z. Comparative lipidomics of drug sensitive and resistant Mycobacterium tuberculosis reveals altered lipid imprints. 3 Biotech. 2017;7(5):1–10. doi: 10.1007/s13205-017-0972-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ernst JD. The immunological life cycle of tuberculosis. Nat Rev Immunol. 2012;12(8):581–591. doi: 10.1038/nri3259. [DOI] [PubMed] [Google Scholar]
- 18.Beller M, Herker E, Füllekrug J. Grease on—perspectives in lipid droplet biology. Semin Cell Dev Biol. 2020;108:94–101. doi: 10.1016/j.semcdb.2020.06.017. [DOI] [PubMed] [Google Scholar]
- 19.Walther TC, Farese RV., Jr The life of lipid droplets. Biochim Biophys Acta. 2009;1791(6):459–466. doi: 10.1016/j.bbalip.2008.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang C, Liu P. The lipid droplet: a conserved cellular organelle. Protein Cell. 2017;8(11):796–800. doi: 10.1007/s13238-017-0467-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chi X, Ogunsade OO, Zhou Z, Li Z, Li X, Zhang M, et al. Lipid droplet is an ancient and inheritable organelle in bacteria. bioRxiv. 2020. 10.1101/2020.05.18.103093.
- 22.Herker E, Ott M. Emerging role of lipid droplets in host/pathogen interactions. J Biol Chem. 2012;287(4):2280–2287. doi: 10.1074/jbc.R111.300202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lundquist PK, Shivaiah K-K, Espinoza-Corral R. Lipid droplets throughout the evolutionary tree. Prog Lipid Res. 2020:101029. 10.1016/j.plipres.2020.101029. [DOI] [PubMed]
- 24.Pagán AJ, Ramakrishnan L. The formation and function of granulomas. Annu Rev Immunol. 2018;36(1):639–665. doi: 10.1146/annurev-immunol-032712-100022. [DOI] [PubMed] [Google Scholar]
- 25.Ehlers S, Schaible UE. The granuloma in tuberculosis: dynamics of a host–pathogen collusion. Front Immunol. 2013;3:411. doi: 10.3389/fimmu.2012.00411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thiam AR, Farese RV, Jr, Walther TC. The biophysics and cell biology of lipid droplets. Nat Rev Mol Cell Biol. 2013;14(12):775–786. doi: 10.1038/nrm3699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farese RV, Walther TC. Lipid droplets finally get a little R-E-S-P-E-C-T. Cell. 2009;139(5):855–860. doi: 10.1016/j.cell.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daniel J, Maamar H, Deb C, Sirakova TD, Kolattukudy PE. Mycobacterium tuberculosis uses host triacylglycerol to accumulate lipid droplets and acquires a dormancy-like phenotype in lipid-loaded macrophages. PLoS Pathog. 2011;7(6). 10.1371/journal.ppat.1002093. [DOI] [PMC free article] [PubMed]
- 29.Garton NJ, Waddell SJ, Sherratt AL, Lee SM, Smith RJ, Senner C, Hinds J, Rajakumar K, Adegbola RA, Besra GS, Butcher PD, Barer MR. Cytological and transcript analyses reveal fat and lazy persister-like bacilli in tuberculous sputum. PLoS Med. 2008;5(4):0634–0645. doi: 10.1371/journal.pmed.0050075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burdon KL. Fatty material in bacteria and fungi revealed by staining dried, fixed slide preparations. J Bacteriol. 1946;52(6):665–678. doi: 10.1128/jb.52.6.665-678.1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Christensen H, Garton NJ, Horobin RW, Minnikin DE, Barer MR. Lipid domains of mycobacteria studied with fluorescent molecular probes. Mol Microbiol. 1999;31(5):1561–1572. doi: 10.1046/j.1365-2958.1999.01304.x. [DOI] [PubMed] [Google Scholar]
- 32.Rastogi N, Frehel C, David HL. Triple-layered structure of mycobacterial cell wall: evidence for the existence of a polysaccharide-rich outer layer in 18 mycobacterial species. Curr Microbiol. 1986;13(5):237–242. doi: 10.1007/BF01568645. [DOI] [Google Scholar]
- 33.Nikaido H, Kim SH, Rosenberg EY. Physical organization of lipids in the cell wall of Mycobacterium chelonae. Mol Microbiol. 1993;8(6):1025–1030. doi: 10.1111/j.1365-2958.1993.tb01647.x. [DOI] [PubMed] [Google Scholar]
- 34.Thiam AR, Ikonen E. Lipid droplet nucleation. Trends Cell Biol. 2020;31(2):108–118. doi: 10.1016/j.tcb.2020.11.006. [DOI] [PubMed] [Google Scholar]
- 35.Thiam AR, Forêt L. The physics of lipid droplet nucleation, growth and budding. Biochim Biophys Acta. 2016;1861(8):715–722. doi: 10.1016/j.bbalip.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 36.Queval CJ, Brosch R, Simeone R. The macrophage: a disputed fortress in the battle against Mycobacterium tuberculosis. Front Microbiol. 2017;8:2284. doi: 10.3389/fmicb.2017.02284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Walther TC, Farese RV., Jr Lipid droplets and cellular lipid metabolism. Annu Rev Biochem. 2012;81(1):687–714. doi: 10.1146/annurev-biochem-061009-102430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ehrt S, Schnappinger D. Mycobacterial survival strategies in the phagosome: defence against host stresses. Cell Microbiol. 2009;11(8):1170–1178. doi: 10.1111/j.1462-5822.2009.01335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sturgill-Koszycki S, Schlesinger PH, Chakraborty P, Haddix PL, Collins HL, Fok AK, Allen R, Gluck S, Heuser J, Russell D. Lack of acidification in Mycobacterium phagosomes produced by exclusion of the vesicular proton-ATPase. Science. 1994;263(5147):678–681. doi: 10.1126/science.8303277. [DOI] [PubMed] [Google Scholar]
- 40.MacMicking JD, Taylor GA, McKinney JD. Immune control of tuberculosis by IFN-γ-inducible LRG-47. Science. 2003;302(5645):654–659. doi: 10.1126/science.1088063. [DOI] [PubMed] [Google Scholar]
- 41.Armstrong J, Hart PDA. Response of cultured macrophages to Mycobacterium tuberculosis, with observations on fusion of lysosomes with phagosomes. J Exp Med. 1971;134(3):713–740. doi: 10.1084/jem.134.3.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Levitte S, Adams KN, Berg RD, Cosma CL, Urdahl KB, Ramakrishnan L. Mycobacterial acid tolerance enables phagolysosomal survival and establishment of tuberculous infection in vivo. Cell Host Microbe. 2016;20(2):250–258. doi: 10.1016/j.chom.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Botella H, Vaubourgeix J, Lee MH, Song N, Xu W, Makinoshima H, Glickman MS, Ehrt S. Mycobacterium tuberculosis protease MarP activates a peptidoglycan hydrolase during acid stress. EMBO J. 2017;36(4):536–548. doi: 10.15252/embj.201695028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roque NR, Lage SL, Navarro R, Fazolini N, Maya-Monteiro CM, Rietdorf J, Melo RCN, D'Avila H, Bozza PT. Rab7 controls lipid droplet-phagosome association during mycobacterial infection. Biochim Biophys Acta Mol Cell Biol Lipids. 2020;1865(8):158703. doi: 10.1016/j.bbalip.2020.158703. [DOI] [PubMed] [Google Scholar]
- 45.Teng O, Ang CKE, Guan XL. Macrophage–bacteria interactions—a lipid-centric relationship. Front Immunol. 2017;8:1836. doi: 10.3389/fimmu.2017.01836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Houben D, Demangel C, Van Ingen J, Perez J, Baldeón L, Abdallah AM, et al. ESX-1-mediated translocation to the cytosol controls virulence of mycobacteria. Cell Microbiol. 2012;14(8):1287–1298. doi: 10.1111/j.1462-5822.2012.01799.x. [DOI] [PubMed] [Google Scholar]
- 47.Tiwari S, Casey R, Goulding CW, Hingley-Wilson S, Jacobs WR Jr. Infect and inject: how Mycobacterium tuberculosis exploits its major virulence-associated type VII secretion system, ESX-1. Bacteria Intracell. 2019:113–26. 10.1128/9781683670261.ch8. [DOI] [PMC free article] [PubMed]
- 48.Barisch C, Soldati T. Breaking fat! How mycobacteria and other intracellular pathogens manipulate host lipid droplets. Biochimie. 2017;141:54–61. doi: 10.1016/j.biochi.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 49.Mattos KA, Lara FA, Oliveira VG, Rodrigues LS, D'Avila H, Melo RC, et al. Modulation of lipid droplets by Mycobacterium leprae in Schwann cells: a putative mechanism for host lipid acquisition and bacterial survival in phagosomes. Cell Microbiol. 2011;13(2):259–273. doi: 10.1111/j.1462-5822.2010.01533.x. [DOI] [PubMed] [Google Scholar]
- 50.Zhang C, Yang L, Ding Y, Wang Y, Lan L, Ma Q, et al. Bacterial lipid droplets bind to DNA via an intermediary protein that enhances survival under stress. Nat Commun. 2017;8(1):1–15. doi: 10.1038/s41467-016-0009-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peyron P, Vaubourgeix J, Poquet Y, Levillain F, Botanch C, Bardou F, et al. Foamy macrophages from tuberculous patients’ granulomas constitute a nutrient-rich reservoir for M. tuberculosis persistence. PLoS Pathog. 2008;4(11):e1000204. doi: 10.1371/journal.ppat.1000204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Knight M, Braverman J, Asfaha K, Gronert K, Stanley S. Lipid droplet formation in Mycobacterium tuberculosis infected macrophages requires IFN-γ/HIF-1α signaling and supports host defense. PLoS Pathog. 2018;14(1):e1006874. doi: 10.1371/journal.ppat.1006874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Monson EA, Crosse KM, Das M, Helbig KJ. Lipid droplet density alters the early innate immune response to viral infection. PLoS One. 2018;13(1):e0190597. doi: 10.1371/journal.pone.0190597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Welte MA. Expanding roles for lipid droplets. Curr Biol. 2015;25(11):R470–R481. doi: 10.1016/j.cub.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kaur G, Kaur J. Multifaceted role of lipids in Mycobacterium leprae. Future Microbiol. 2017;12(4):315–335. doi: 10.2217/fmb-2016-0173. [DOI] [PubMed] [Google Scholar]
- 56.Santucci P, Johansen MD, Point V, Poncin I, Viljoen A, Cavalier JF, Kremer L, Canaan S. Nitrogen deprivation induces triacylglycerol accumulation, drug tolerance and hypervirulence in mycobacteria. Sci Rep. 2019;9(1):8667. doi: 10.1038/s41598-019-45164-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hammond RJ, Baron VO, Oravcova K, Lipworth S, Gillespie SH. Phenotypic resistance in mycobacteria: is it because I am old or fat that I resist you? J Antimicrob Chemother. 2015;70(10):2823–2827. doi: 10.1093/jac/dkv178. [DOI] [PubMed] [Google Scholar]
- 58.Zhang Y, Yew WW, Barer MR. Targeting persisters for tuberculosis control. Antimicrob Agents Chemother. 2012;56(5):2223–2230. doi: 10.1128/AAC.06288-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sebastian J, Swaminath S, Nair RR, Jakkala K, Pradhan A, Ajitkumar P. De novo emergence of genetically resistant mutants of Mycobacterium tuberculosis from the persistence phase cells formed against antituberculosis drugs in vitro. Antimicrob Agents Chemother. 2017;61(2). 10.1128/AAC.01343-16. [DOI] [PMC free article] [PubMed]
- 60.Aguilar-Ayala DA, Tilleman L, Van Nieuwerburgh F, Deforce D, Palomino JC, Vandamme P, et al. The transcriptome of Mycobacterium tuberculosis in a lipid-rich dormancy model through RNAseq analysis. Sci Rep. 2017;7(1):1–13. doi: 10.1038/s41598-017-17751-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arbues A, Lugo-Villarino G, Neyrolles O, Guilhot C, Astarie-Dequeker C. Playing hide-and-seek with host macrophages through the use of mycobacterial cell envelope phthiocerol dimycocerosates and phenolic glycolipids. Front Cell Infect Microbiol. 2014;4:173. doi: 10.3389/fcimb.2014.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guerrini V, Gennaro ML. Foam cells: One size doesn’t fit all. Trends Immunol. 2019;40(12):1163–1179. doi: 10.1016/j.it.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Choi AM, Ryter SW, Levine B. Autophagy in human health and disease. NEJM. 2013;368(7):651–662. doi: 10.1056/NEJMra1205406. [DOI] [PubMed] [Google Scholar]
- 64.Sloan DJ, Mwandumba HC, Garton NJ, Khoo SH, Butterworth AE, Allain TJ, Heyderman RS, Corbett EL, Barer MR, Davies GR. Pharmacodynamic modeling of bacillary elimination rates and detection of bacterial lipid bodies in sputum to predict and understand outcomes in treatment of pulmonary tuberculosis. Clin Infect Dis. 2015;61(1):1–8. doi: 10.1093/cid/civ195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kayigire XA, Friedrich SO, van der Merwe L, Donald PR, Diacon AH. Simultaneous staining of sputum smears for acid-fast and lipid-containing Myobacterium tuberculosis can enhance the clinical evaluation of antituberculosis treatments. Tuberculosis. 2015;95(6):770–779. doi: 10.1016/j.tube.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 66.Bhaskar A, Dwivedi VP, Nandicoori VK. Pathogenicity and drug resistance of human pathogens: mechanisms and novel approaches. 2020. Eliminating mycobacterial persistence: Novel targets for anti-tb therapy; pp. 57–79. [Google Scholar]
- 67.Vilchèze C, Jacobs WR., Jr The isoniazid paradigm of killing, resistance, and persistence in Mycobacterium tuberculosis. J Mol Biol. 2019;431(18):3450–3461. doi: 10.1016/j.jmb.2019.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mandal S, Njikan S, Kumar A, Early JV, Parish T. The relevance of persisters in tuberculosis drug discovery. Microbiol. 2019;165(5):492–499. doi: 10.1099/mic.0.000760. [DOI] [PubMed] [Google Scholar]
- 69.Jones-López EC, Kim S, Fregona G, Marques-Rodrigues P, Hadad DJ, Molina LPD, et al. Importance of cough and M. tuberculosis strain type as risks for increased transmission within households. PloS One. 2014;9(7):e100984. doi: 10.1371/journal.pone.0100984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Verma S, Bhatt K, Lovey A, Ribeiro-Rodrigues R, Durbin J, Jones-López EC, Palaci M, Vinhas SA, Alland D, Dietze R, Ellner JJ, Salgame P. Transmission phenotype of Mycobacterium tuberculosis strains is mechanistically linked to induction of distinct pulmonary pathology. PLoS Pathog. 2019;15(3):e1007613. doi: 10.1371/journal.ppat.1007613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wolf AJ, Desvignes L, Linas B, Banaiee N, Tamura T, Takatsu K, Ernst JD. Initiation of the adaptive immune response to Mycobacterium tuberculosis depends on antigen production in the local lymph node, not the lungs. J Exp Med. 2008;205(1):105–115. doi: 10.1084/jem.20071367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ganchua SKC, Cadena AM, Maiello P, Gideon HP, Myers AJ, Junecko BF, Klein EC, Lin PL, Mattila JT, Flynn JAL. Lymph nodes are sites of prolonged bacterial persistence during Mycobacterium tuberculosis infection in macaques. PLoS Pathog. 2018;14(11):e1007337. doi: 10.1371/journal.ppat.1007337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kodaman N, Sobota RS, Mera R, Schneider BG, Williams SM. Disrupted human–pathogen co-evolution: a model for disease. Front Genet. 2014;5:290. doi: 10.3389/fgene.2014.00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nuismer SL, Thompson JN. Coevolutionary alternation in antagonistic interactions. Evolution. 2006;60(11):2207–2217. doi: 10.1111/j.0014-3820.2006.tb01858.x. [DOI] [PubMed] [Google Scholar]
- 75.Maji A, Misra R, Mondal AK, Kumar D, Bajaj D, Singhal A, et al. Expression profiling of lymph nodes in tuberculosis patients reveal inflammatory milieu at site of infection. Sci Rep. 2015;5(1):1–10. doi: 10.1038/srep15214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mekonnen D, Derbie A, Chanie A, Shumet A, Biadglegne F, Kassahun Y, et al: Molecular epidemiology of M. tuberculosis in Ethiopia: A systematic review and meta-analysis. Tuberculosis 2019, 118:101858, DOI: 10.1016/j.tube.2019.101858. [DOI] [PMC free article] [PubMed]
- 77.Mekonnen D, Derbie A, Abeje A, Shumet A, Kassahun Y, Nibret E, Munshea A, Bobosha K, Wassie L, Biadglegne F, Aseffa A, Sack U. Genomic diversity and transmission dynamics of M. tuberculosis in Africa: a systematic review and meta-analysis. IJTLD. 2019;23(12):1314–1326. doi: 10.5588/ijtld.19.0127. [DOI] [PubMed] [Google Scholar]
- 78.Sharma A, Bloss E, Heilig CM, Click ES. Tuberculosis caused by Mycobacterium africanum, United States, 2004–2013. Emerg Infect Dis. 2016;22(3):396–403. doi: 10.3201/eid2203.151505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ates LS, Dippenaar A, Sayes F, Pawlik A, Bouchier C, Ma L, Warren RM, Sougakoff W, Majlessi L, van Heijst JWJ, Brossier F, Brosch R. Unexpected genomic and phenotypic diversity of Mycobacterium africanum lineage 5 affects drug resistance, protein secretion, and immunogenicity. Genome Biol Evol. 2018;10(8):1858–1874. doi: 10.1093/gbe/evy145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Coscolla M, Gagneux S. Consequences of genomic diversity in Mycobacterium tuberculosis. Semin Immunol. 2014;26(6):431–444. doi: 10.1016/j.smim.2014.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Diarra B, Kone M, Togo ACG, Sarro YDS, Cisse AB, Somboro A, et al. Mycobacterium africanum (lineage 6) shows slower sputum smear conversion on tuberculosis treatment than Mycobacterium tuberculosis (lineage 4) in Bamako, Mali. PloS One. 2018;13(12):e0208603. doi: 10.1371/journal.pone.0208603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Reed MB, Gagneux S, DeRiemer K, Small PM, Barry CE. The W-Beijing lineage of Mycobacterium tuberculosis overproduces triglycerides and has the DosR dormancy regulon constitutively upregulated. J Bacteriol. 2007;189(7):2583–2589. doi: 10.1128/JB.01670-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ejo M, Gehre F, Barry MD, Sow O, Bah NM, Camara M, Bah B, Uwizeye C, Nduwamahoro E, Fissette K, Rijk PD, Merle C, Olliaro P, Burgos M, Lienhardt C, Rigouts L, de Jong BC. First insights into circulating Mycobacterium tuberculosis complex lineages and drug resistance in Guinea. Infect Genet Evol. 2015;33:314–319. doi: 10.1016/j.meegid.2015.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chisompola NK, Streicher EM, Muchemwa CMK, Warren RM, Sampson SL. Molecular epidemiology of drug resistant Mycobacterium tuberculosis in Africa: a systematic review. BMC Infect Dis. 2020;20(1):1–16. doi: 10.1186/s12879-020-05031-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gehre F, Otu J, DeRiemer K, de Sessions PF, Hibberd ML, Mulders W, Corrah T, de Jong BC, Antonio M. Deciphering the growth behaviour of Mycobacterium africanum. PLoS Negl Trop Dis. 2013;7(5):e2220. doi: 10.1371/journal.pntd.0002220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tientcheu LD, Bell A, Secka O, Ayorinde A, Otu J, Garton NJ, Sutherland JS, Ota MO, Antonio M, Dockrell HM, Kampmann B, Barer MR. Association of slow recovery of Mycobacterium africanum-infected patients posttreatment with high content of Persister-like bacilli in pretreatment sputum. Int J Mycobacteriol. 2016;5(5):99–S100. doi: 10.1016/j.ijmyco.2016.09.033. [DOI] [PubMed] [Google Scholar]
- 87.Yimer SA, Norheim G, Namouchi A, Zegeye ED, Kinander W, Tønjum T, Bekele S, Mannsåker T, Bjune G, Aseffa A, Holm-Hansen C. Mycobacterium tuberculosis lineage 7 strains are associated with prolonged patient delay in seeking treatment for pulmonary tuberculosis in Amhara region, Ethiopa. J Clin Microbiol. 2015;53(4):1301–1309. doi: 10.1128/JCM.03566-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Garton NJ, Barer MR. Mycobacterial lipid bodies and the chemosensitivity and transmission of tuberculosis. In: Goldfine H, editor. Health Consequences of Microbial Interactions with Hydrocarbons, Oils, and Lipids. Switzerland: Springer Nature; 2020. pp. 109–132. [Google Scholar]
- 89.Sharma S, Ryndak MB, Aggarwal AN, Yadav R, Sethi S, Masih S, Laal S, Verma I. Transcriptome analysis of mycobacteria in sputum samples of pulmonary tuberculosis patients. PLoS One. 2017;12(3):e0173508. doi: 10.1371/journal.pone.0173508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ofori-Anyinam B, Dolganov G, Van T, Davis JL, Walter ND, Garcia BJ, et al. Significant under expression of the DosR regulon in M. tuberculosis complex lineage 6 in sputum. Tuberculosis. 2017;104:58–64. doi: 10.1016/j.tube.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lai RP, Cortes T, Marais S, Rockwood N, Burke ML, Garza-Garcia A, et al. Transcriptomic characterization of tuberculous sputum reveals a host Warburg effect and microbial cholesterol catabolism. bioRxiv. 2020. 10.1101/2020.03.09.983163. [DOI] [PMC free article] [PubMed]
- 92.Honeyborne I, McHugh TD, Kuittinen I, Cichonska A, Evangelopoulos D, Ronacher K, et al. Profiling persistent tubercule bacilli from patient sputa during therapy predicts early drug efficacy. BMC Med. 2016;14(1):1–13. doi: 10.1186/s12916-016-0609-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Garcia BJ, Loxton AG, Dolganov GM, Van TT, Davis JL, de Jong BC, et al. Sputum is a surrogate for bronchoalveolar lavage for monitoring Mycobacterium tuberculosis transcriptional profiles in TB patients. Tuberculosis. 2016;100:89–94. doi: 10.1016/j.tube.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Walter ND, Dolganov GM, Garcia BJ, Worodria W, Andama A, Musisi E, Ayakaka I, van TT, Voskuil MI, de Jong BC, Davidson RM, Fingerlin TE, Kechris K, Palmer C, Nahid P, Daley CL, Geraci M, Huang L, Cattamanchi A, Strong M, Schoolnik GK, Davis JL. Transcriptional adaptation of drug-tolerant Mycobacterium tuberculosis during treatment of human tuberculosis. J Infect Dis. 2015;212(6):990–998. doi: 10.1093/infdis/jiv149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bukka A, Price CT, Kernodle DS, Graham JE. Mycobacterium tuberculosis RNA expression patterns in sputum bacteria indicate secreted Esx factors contributing to growth are highly expressed in active disease. Front Microbiol. 2012;2:266. doi: 10.3389/fmicb.2011.00266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ryndak M, Wang S, Smith I. PhoP, a key player in Mycobacterium tuberculosis virulence. Trends Microbiol. 2008;16(11):528–534. doi: 10.1016/j.tim.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 97.Leistikow RL, Morton RA, Bartek IL, Frimpong I, Wagner K, Voskuil MI. The Mycobacterium tuberculosis DosR regulon assists in metabolic homeostasis and enables rapid recovery from nonrespiring dormancy. J Bacteriol. 2010;192(6):1662–1670. doi: 10.1128/JB.00926-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chen T, He L, Deng W, Xie J. The Mycobacterium DosR regulon structure and diversity revealed by comparative genomic analysis. J Cell Biochem. 2013;114(1):1–6. doi: 10.1002/jcb.24302. [DOI] [PubMed] [Google Scholar]
- 99.Rodríguez JG, Hernández AC, Helguera-Repetto C, Aguilar Ayala D, Guadarrama-Medina R, Anzóla JM, et al. Global adaptation to a lipid environment triggers the dormancy-related phenotype of Mycobacterium tuberculosis. mBio. 2014;5(3):e01125–e01114. doi: 10.1128/mBio.01125-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Honeyborne I, Mtafya B, Phillips PP, Hoelscher M, Ntinginya EN, Kohlenberg A, et al. The molecular bacterial load assay replaces solid culture for measuring early bactericidal response to antituberculosis treatment. J Clin Microbiol. 2014;52(8):3064–3067. doi: 10.1128/JCM.01128-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Walter ND, Born SE, Robertson GT, Reichlen M, Dide-Agossou C, Ektnitphong VA, et al. Mycobacterium tuberculosis precursor rRNA as a measure of treatment-shortening activity of drugs and regimens. Nat Commun. 2021;12(1):1–11. doi: 10.1038/s41467-021-22833-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Demirci M, Saribas S, Ozer N, Toprak S, Caglar E, Ortakoylu G, Yuksel P, Ayaz G, Tokman HB, Uysal O, Dinc HO, Ziver T, Kocazeybek B. Diagnostic performance of the RT-qPCR method targeting 85B mRNA in the diagnosis of pulmonary Mycobacterium tuberculosis infection. J Infect Public Health. 2018;11(5):662–666. doi: 10.1016/j.jiph.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 103.Mukamolova GV, Turapov O, Malkin J, Woltmann G, Barer MR. Resuscitation-promoting factors reveal an occult population of tubercle bacilli in sputum. Am J Respir Crit Care Med. 2010;181(2):174–180. doi: 10.1164/rccm.200905-0661OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lipworth S, Hammond R, Baron V, Hu Y, Coates A, Gillespie S. Defining dormancy in mycobacterial disease. Tuberculosis. 2016;99:131–142. doi: 10.1016/j.tube.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 105.Colangeli R, Gupta A, Vinhas SA, Venkata UDC, Kim S, Grady C et al: Mycobacterium tuberculosis progresses through two phases of latent infection in humans. Nat Commun 2020, 11(1):1–10, DOI: 10.1038/s41467-020-18699-9. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.