Abstract
Autism spectrum disorders are an issue of increasing public health significance. The incidence of autism spectrum disorders has been increasing in recent years, and they are associated with significant personal and financial impacts for affected persons and their families. In recent years, a large number of scientific studies have been undertaken, which investigate genetic and environmental risk factors for autism, with more studies underway. At present, much remains unknown regarding autism spectrum disorder risk factors, but the emerging picture of causation is in many cases complex, with multiple genes and gene–environment interactions being at play. The complexity and uncertainty surrounding autism spectrum disorder risk factors raise a number of questions regarding the ethical considerations that should be taken into account when undertaking autism spectrum disorder risk communication. At present, however, little has been written regarding autism spectrum disorder risk communication and ethics. This article summarizes the findings of a recent conference investigating ethical considerations and policy recommendations in autism spectrum disorder risk communication, which to the authors’ knowledge is the first of its kind. Here, the authors discuss a number of issues, including uncertainty; comprehension; inadvertent harm; justice; and the appropriate roles of clinicians, scientists, and the media in autism spectrum disorder risk communication.
Keywords: autism, ethics, risk communication
Introduction
Research examining the etiology of autism spectrum disorders (ASDs) is increasingly focused on complex genetic and environmental mechanisms (Berkel et al., 2010; Croen et al., 2011; Deth et al., 2008; Hallmeyer et al., 2011; IOM, 2008; Rutter, 2011). Findings from major new initiatives now underway have the potential to enrich the understanding of the etiology of ASD. Given the intensity of public debate about causes for ASD—both contemporary and historical—the communication of scientific findings relating to its etiology presents significant challenges.
Scientific understanding of autism etiology has been both transformed and disputed since the naming of the diagnosis by the child psychiatrist Leo Kanner (1943). Beginning in the middle of the twentieth century, the “refrigerator mother” hypothesis, a psychogenic explanation for autism etiology, laid blame for a child’s autism diagnosis on mothers for more than a generation. In addition, more recent claims that vaccination or vaccine preservatives are the primary etiologic factor in ASDs highlight just some of the ways in which the communication of scientific findings and etiologic risk for the disorder have been accompanied by controversy and strife (Baker, 2008; Silverman and Brosco, 2007). Given this history, the ways stakeholders communicate etiologic findings have enormous implications for this area of research; for public health; for biomedical ethics; and, of course, for the children, adults, and families affected by the disorder. There is, therefore, a fundamental need for a more robust understanding of the ethical and risk communication issues associated with scientific findings on autism.
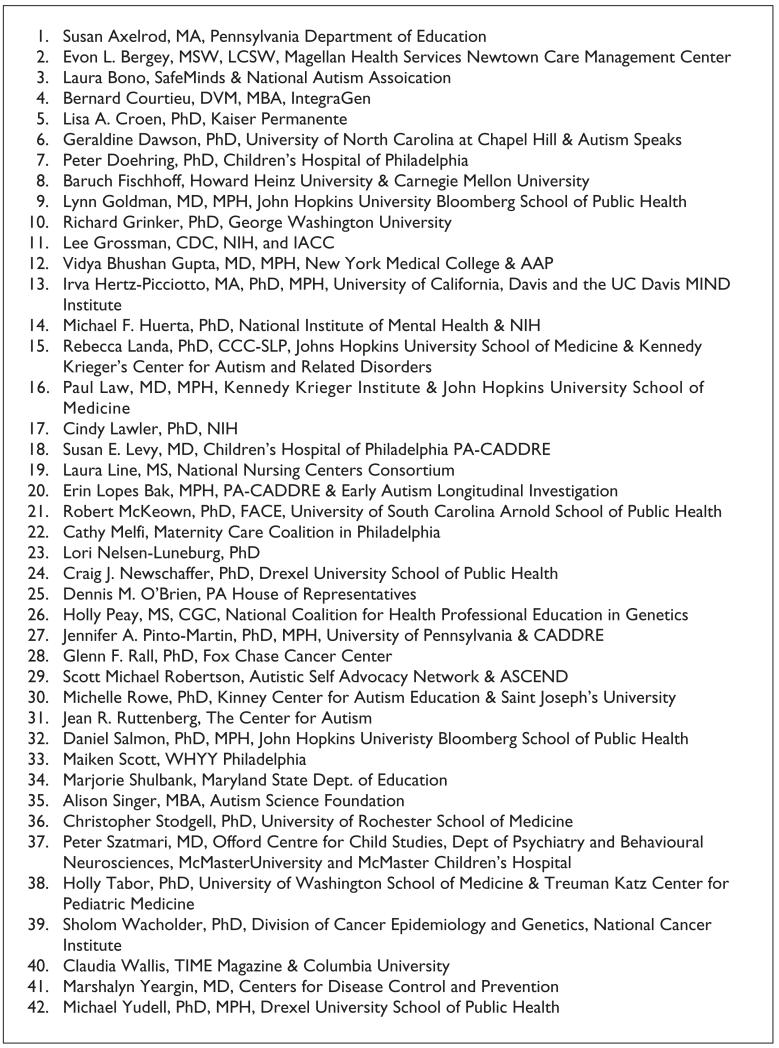
To address emerging challenges in autism risk communication and ethics, a meeting was held in October 2009 with ASD stakeholders from diverse autism stakeholder communities (see Figure 1). The purpose of the meetings was to examine the ethical and risk communication issues involved in ASD research and its dissemination and to foster this research by building new partnerships by including a diverse set of stakeholders in our process.
Figure 1.
Participants in October 2009 meeting including speakers and invited stakeholders (Affiliations listed are as of the meeting date).
This article offers a brief exploration of ethical and risk communication challenges in autism and provides a summary of the four policy proposal areas that emerged from the meeting discussions. These areas were as follows: (a) the role that clinicians and service providers play in disseminating and translating findings in autism research; (b) the roles for researchers and the media in balancing the communication of scientific advances and continuing uncertainty; (c) the importance of tailoring risk communication for autism to different communities and populations, and the role of advocacy organizations in these efforts; and (d) the dissemination of research results to autism research study participants.
Autism, ethics, and risk communication
Despite the explosion of research on autism’s natural history, biologic underpinnings, and etiology, there remains only a small literature on the ethics of autism research and its dissemination. Several papers provide an initial assessment of the field (Chen et al., 2003; Jordan and Tsai, 2010; McMahon et al., 2006; Miller et al., 2010), but focus on genetic risk factors almost exclusively. Some authors have warned, for example, that the complexity of ASD genetic etiology will result in a convergence of significant ethical and scientific challenges around issues, including, but not limited to, culturally sensitive genetic counseling, complex genetic test results and their uncertainty, appropriate descriptions of potential harms from autism research, genetic discrimination, insurance eligibility criteria, and direct-to-consumer marketing of genetic tests for ASD (Chen et al., 2003; McMahon et al., 2006; Tabor, 2011).
Similarly, the field of risk communication has only recently begun to focus on the challenges associated with communicating ASD risk, motivated by a rapid rise in the magnitude of ASD prevalence estimates, the perceived association between vaccination and autism risk, and the highly public fallout that this has had on perception of the safety and efficacy of vaccines (Downs et al., 2008). The field of risk communication is relatively new, spanning only a few decades, but has grown considerably in this short time. Its focus not only includes attention to the communication of disease risk to patients and populations but also extends to other contexts, such as the communication of risk around potential technological and environmental hazards. The theory and practice of risk communication raise numerous and significant ethical issues, which apply to the discussion and dissemination of disease risk information to patients, families, autism research participants, and the wider community.
Risk communication, like bioethics and public health ethics, draws its expertise from multiple fields, including psychology, public health, medicine, and risk assessment and management. Risk communication experts are interested in how to improve the communication about the risks individuals face in their lives. This requires attention to how risk messages are formulated; how individuals understand risk information; how risk messages are socially amplified or attenuated; and what goals, values, and trade-offs are implicit in risk messages. Successful risk communication may be defined in a number of ways. Early in the field’s history in the 1970s and 1980s, success was defined as the ability to “get one’s message across” to an audience, with the measure of this success being reflected by an audience’s understanding and acceptance of the message risk communicators intended (National Research Council (NRC), 1989). This orientation subsequently led to a large body of empirical research in risk perception (e.g. Slovic, 1987), sometimes marshaled in support of figuring out why laypersons’ “subjective” risk estimates differed from technical experts’ “objective” risk estimates (Finkel, 2008; Hansson, 1993). However, for a number of reasons, this approach to risk communication has evolved toward an approach focused on two-way dialogues, where “risk communication is successful only to the extent that it raises the level of understanding of relevant issues or actions and satisfies those involved that they are adequately informed within the limits of available knowledge” (NRC, 1989: 21). While it is true that both technical experts and nonexperts may display biases in probabilistic reasoning, it is also true that definitions of risk, the way risk information is framed, and “rational” or “appropriate” responses to risk are all influenced by philosophical assumptions and moral values (Douglas and Wildavsky, 1982; Hansson, 1993; NRC, 1989; Shrader-Frechette, 1991). Furthermore, in a democratic society, the public expects to participate in discussions about risk and to have their viewpoints heard. While political legitimacy may require some degree of public participation, at a practical level, risk communication will not be successful if message recipients feel marginalized or disenfranchised.
As concerns risk communication in general, and certainly as applied to autism, ethical issues include the following: value judgments involved in risk messaging; procedural constraints governing the risk communication process; how risk communication might lead to ethically salient outcomes such as benefit or harm; and the consideration given such outcomes in terms of norms such as respect for autonomy, nonmaleficence, beneficence, and justice. The concept of risk presupposes a bad or harmful outcome to be avoided. While value judgments implicit in risk communication may sometimes be uncontroversial (e.g. that developing cancer is a harm), in other cases, they may be both rationally contestable and politically controversial. As regards ASDs, there is a need for more nuanced discussion in the sciences as to whether “risk” is an appropriate descriptor for all ASD-related phenotypes. Arguably, the most important value judgment presupposed by risk communication for ASDs is that ASDs are harmful outcomes to be avoided. For individuals severely affected by ASDs, the judgment that ASDs are harmful may not be controversial. However, given the broad phenotype of the disorder, questions have been raised, particularly by self-advocates, as to whether all such phenotypes are harmful outcomes to be avoided. The nature of our stakeholder group, including an autism self-advocate and parents of children and adults with ASDs, sought to address these concerns by having an inclusive discussion of these matters.
Some of the extant literature relating to risk communication touches upon these ethical issues, for example, the way in which the framing of risk information is value-laden, or how the formulation of risk messages intersects with questions of democratic representation and political legitimacy (Johnson, 1999; NRC, 1989). However, overall, little has been written about risk communication and ethics concerning autism, and there is a need to further explore the ethical issues involved in risk communication and, where possible, to develop recommendations regarding ethically defensible risk communication practice for ASDs.
Furthermore, autism risk communication, in particular, raises a number of more specific ethical issues and questions. These include the following: ‘How should autism risk be communicated in an atmosphere of controversy and uncertainty around the etiology and diagnosis of the disorder?’ ‘When and what information from scientific studies should researchers communicate to clinicians, parents, the media, and the public?’ and ‘How should stakeholders involved in the communication of autism risk tailor messages of risk to the myriad subpopulations affected by autism?’ This may include tailored communication to communities that have historically suffered from diagnostic and treatment disparities of ASD, families with adult children with ASD, and families whose children are diagnosed at different points on the autism spectrum. These communication issues are closely associated with what can be characterized as more traditional bioethics concerns involving autism, including the challenges of working with pediatric research participants, the return of results to study participants, and protecting vulnerable populations in research (Tabor, 2011). Therefore, the consideration of ethical issues in autism risk communication presents a unique challenge: the distinct literatures around risk communication, ethics, and autism must be synthesized, and the early stage of ethical inquiry relating to risk communication likely means that much work will be needed in this area.
Three separate, but related, factors underscore the importance of addressing ethical and risk communication issues as they pertain to autism. First, recently updated prevalence statistics from the Centers for Disease Control and Prevention (CDC) suggest that ASDs affect, on average, 1 in 88 children in the United States (Baio, 2012). Between 2002 and 2008, CDC data show that prevalence rates for autism have risen, on average, 78%. The fact that autism is now a commonly diagnosed disorder with largely unknown etiology has made it a public health priority, and as such, it is imperative that we understand how to communicate the diagnosis and the risk of developing an ASD to the growing population of affected families in an ethical manner. Second, this dramatic increase in prevalence has led to robust debate about what accounts for this change (Newschaffer et al., 2005). Some cite the change in diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, while others point to environmental factors, genetics, or the complex interplay of both (Charman et al., 2009; Geschwind and Levitt, 2007; King and Bearman, 2009). Still others have blamed specific vaccines, vaccine preservatives, or the number of pediatric vaccines for the increase in autism prevalence. Communicating risk in this time of uncertainty creates significant challenges that must be addressed in a scientific and scholarly manner. Third, and finally, this era of changing prevalence and great uncertainty has provoked considerable controversy, confusion, and hostility within the autism stakeholder community. The intensity of the debates over autism etiology, full of blame and accusation, and with measurable impacts on public health practice and policy in the form of a decrease in vaccination rates for certain vaccines that seem to be related to the vaccine/autism controversy, demands attention to improved risk communication and ethical issues concerning autism.
Building consensus in autism risk communication and ethics
With funding from both the National Institute of Environmental Health Sciences and the nonprofit science and advocacy organization Autism Speaks, the Drexel University School of Public Health convened a 2-day workshop in Philadelphia, Pennsylvania, designed to facilitate, through a series of presentations, panel discussions, and breakout sessions, a consensus approach to ethical and risk communication challenges facing autism research. By bringing together leading ASD stakeholders, the workshop sought to build consensus and make recommendations about ethically approaching ASD research and its dissemination in a manner that can secure the public’s trust. A smaller follow-up meeting in Seattle, Washington, in November 2010, funded by Autism Speaks, continued to examine these ethical and risk challenges.
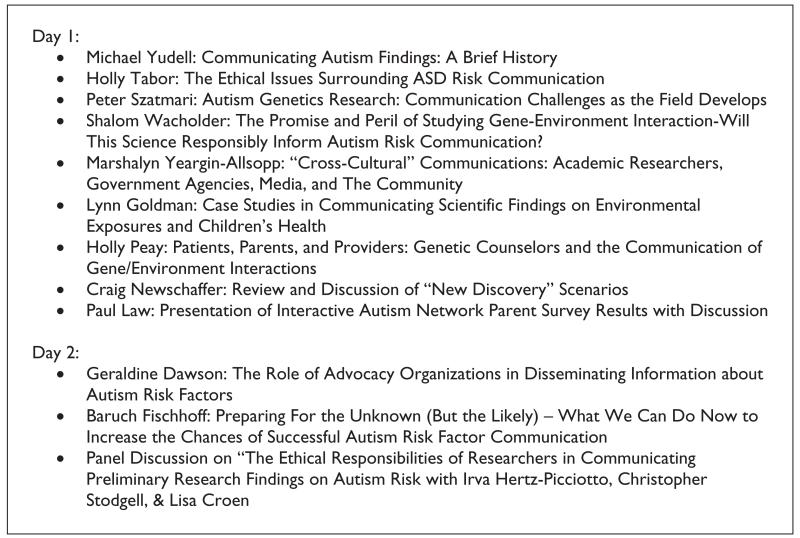
In developing the workshop agenda, the organizers were careful to include participants with diverse opinions from the spectrum of autism stakeholders. Participants included autism self-advocates, parents of children and adults with autism, autism genetic researchers, epidemiologists and other scientists, and science journalists. The conference took place over a 2-day period where participants attended presentations by experts in ASD research and were invited to participate in case study discussions (see Figure 2).
Figure 2.
Talk topics.
Each of the invited stakeholders was assigned to a discussion group based on his/her role or possible role in autism ethics and risk communication. Group members were charged with discussing both the barriers to effective and ethical risk communication they personally face as well as barriers and projected barriers to the larger group of stakeholders each represented. Discussions of the four priority areas below are not intended to be comprehensive summaries of all barriers and challenges facing the diverse stakeholders involved in autism ethics and risk communication research. Rather, they should be viewed as first steps toward moving the autism field forward as research efforts and understanding continue to develop. All stakeholders were invited to be part of the Working Group in Autism Risk Communication and Ethics.
Priority area 1: the role of clinicians and other service providers in disseminating and translating findings in autism research
There was strong consensus among workshop participants that clinical, educational, and other professionals providing diagnostic, assessment, and intervention services to children with autism and their families need to play a pivotal role in the communication of information about autism risk factors. Casiday (2010) has posited that trust is the key ingredient in situations where parents’ “chief concern is to protect their own children from harm but uncertainty about the nature and likelihood of different harms meant that parents had to turn to other sources for information and interpretations.” Given the complexity of autism etiology and the challenges of conducting risk factor research as well as the historical context, this characterization will certainly apply to future emerging autism risk factors. One survey showed that parents were far more likely to turn to the media (71%–73%), conferences or workshops (42%), or other parents (42%) than health-care or other professionals (15%–20%) (Rhoades et al., 2007). Furthermore, data collected by the Interactive Autism Network (IAN), which used an online survey of 278 respondents on autism knowledge and the role of the media, supported the important role these individuals play. Results from the IAN survey suggested that nonphysician intervention service providers, followed by physicians, are the most relied-upon source of information among professionals (Law, 2009). In the wake of the autism–vaccine controversy, some risk communications researchers have noted further strain in parents’ trust of professionals (Austin et al., 2008; Raithatha et al., 2003), a phenomenon tied to contradictory messages received from the professional community throughout the vaccine controversy plus a perception that there was a lack of reciprocation of trust in these encounters, with some parents believing that physicians were reluctant to acknowledge their intention to act in the best interest of their children (Casiday, 2007). One means of building trust has been the use of narrative in the exchange of information about health risks (Earle and Cvetkovich, 1995), and the dialogue between provider and parent is one place where narrative can be built. Narrative accounts of patients’ experiences during medical encounters help to provide differing “frames” for the story of such encounters, inasmuch as patients may perceive a series of events or the importance of specific events differently than physicians. Narrative approaches to physician–patient interactions have been used extensively in bioethics as a means of uncovering morally salient considerations that otherwise would have been ignored (e.g. Chambers, 1999; Fiester, 2007). Narrative can similarly be used as a tool for the exploration of families’ perspectives when interacting with physicians or other service providers in the context of autism.
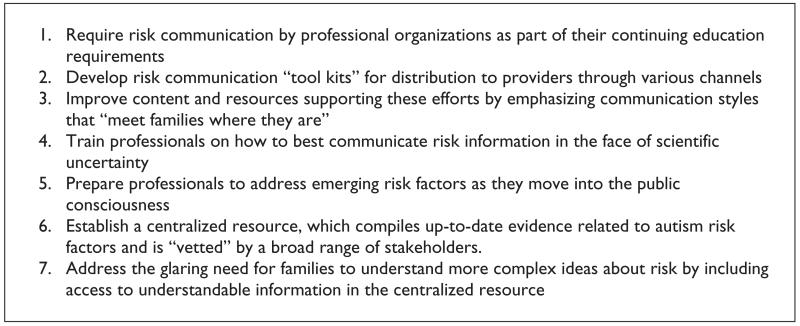
The working group recognized, however, that there are barriers to effective communication around risk factors between parents and service providers that need to be surmounted to better create opportunities for dialogue and the construction of trust-building narrative (see Figure 3). Barriers raised generally fell into three groups: (a) institutional/organizational issues within the providers’ setting; (b) providers’ lack of risk communication skills and savvy; and (c) provider’s impaired access to, and understanding of, the most appropriate autism risk factor information suitable for risk communication (as opposed to professional knowledge or research) purposes.
Figure 3.
Summary of recommendations in priority area 1.
Finally, one additional major barrier discussed that fell outside these three areas was a perception that there was also a lack of parental comfort in asking questions about risk. This could well be related to some of institutional/organizational issues (e.g. insufficient time during clinical encounters) but also could be connected to worry that raising these questions might not be well received (perhaps a consequence in part of erosion in trust). From a survey of the literature, little seems known about this barrier and further research in this area could be helpful.
With respect to institutional/organizational issues, the working group noted time pressure faced by providers during service encounters and lack of reimbursement for efforts related to risk communication during service visits. Working group participants agreed that even among the most qualified providers, there was still a lack of skill and experience directly related to risk communication. Consequently, there was substantial support for finding ways to enhance risk communication training for service providers across a range of disciplines ranging from physician specialists, to general pediatricians, nurses, and early intervention providers. The working group believed that relevant professional organizations, including American Academy of Pediatrics, the American Medical Association, the American Psychological Association, and the American Psychiatric Association, among others, should require risk communication training as part of their continuing education requirements and that both general and specific to autism “risk communication toolkits” could be developed for distribution to providers through various channels. However, the working group also acknowledged that for these efforts to be effective, improved content and resources supporting such efforts likely needed to be developed. It was recommended that these resources and content emphasize communication styles that are family-friendly, show empathy, and stress that risk communication begin by “meeting families where they are” in terms of their level of concern. Moreover, given that considerable scientific uncertainty is likely to be part of the landscape around data on emerging autism risk factors, training on how to best communicate information in the face of uncertainty was also anticipated to be crucial. This working group stressed that communication around emerging risk factors should be proactive; instead of waiting for families to raise concerns themselves, the consensus was that providers need to be ready and be able to approach risk factor topics with individual families soon after they move into the public consciousness.
In addition, participants felt quite strongly that there was much room for improvement in access to information about emerging autism risk factors presented in a manner that will be most relevant when conveyed to families. There was support for the establishment of a centralized resource, which compiles up-to-date evidence related to autism risk factors and is “vetted” by a broad range of stakeholders. After establishment, the resource should then be made widely known and accessible to service providers. It is possible that, as discussed above, advocacy organizations can help fill this need. Such a central resource could also house ready-to-distribute supporting materials that providers could use in their practice and could also negotiate ways to speed the flow of clinically useful information from researchers to service providers. Among the significant challenges associated with such an effort would be the creation of buy-in from a diverse group of stakeholders, to balance competing stakeholder interests and scientific evidence, and finding funding.
It was also recognized that, aside from the logistical challenges of timeliness and consensus in the vetting process, such a central resource should also address some of the issues related to optimizing content in a manner that best facilitates effective risk communication. While quantitative information will undoubtedly be desired by professionals, many persons may have difficulties understanding quantitative probabilistic information, and there is disagreement about which kinds of quantitative formats (e.g. frequencies vs. percentages) are most understandable (Condit and Shen, 2011; Gigerenzer et al., 2005; Hampel, 2006; Slovic, 1987, 1997; Smith et al., 2010). However, qualitative descriptions of risk may be interpreted very variably and thus be even more problematic. For example, one recent study (French and Maule, 2010) demonstrated a 40-fold difference between regulators and laypersons in what was meant by the term “low risk” (Berry et al., 2002).
Even more sobering is the glaring need in autism risk communication for families to understand complex nuances of risk. For example, a relative risk of 2.0 (“doubling of risk associated with exposure”) may seem quite large and is often a convention used to define “large associations” in epidemiology (Carruth and Goldstein, 2001), but if reconstructed as a risk difference (say, the small absolute difference in the 2% risk for the exposed group vs. 1% in the unexposed), the same data may have quite a different impact for families (Rothman, 2002a). Similarly, when research suggests that a risk factor may account for “ten percent” of autism cases, which sounds quite large, the interpretation of this may be quite different if families can be helped to understand that, for a complex multifactorial disease like autism, attributable risk percentages will not be bounded at 100% (Rothman, 2002b).
Efforts to make risk information more comprehensible may come at the cost of accuracy or neutrality. The notion that someone bears “twice the risk of the average person” may be more intuitively understandable than an absolute risk or risk difference, but as already discussed, relative risks may be misleading. In addition, risk communicators may employ so-called “risk ladders” to help contextualize the magnitude of a risk. Risk ladders present the risk of interest alongside of risks of larger and smaller magnitudes, and are particularly useful for conveying risks of small magnitude. However, it is easy to give the impression that a risk of interest is more or less acceptable than another risk to which it is compared (NRC, 1989). Having said this, obstacles in achieving understanding among a target audience may be due not to the audience’s inability to understand quantitative information, but rather to the risk communicators’ inability to provide relevant information in a comprehensible format (Fischhoff, 2007). Risk communicators have a responsibility to make their messages as understandable as possible and not to automatically blame an audience’s lack of understanding on their inability to understand.
Priority area 2: the roles of researchers and the media in balancing the communication of scientific advances and continuing uncertainty
Providing the public with accurate, comprehensible, timely, and relevant autism risk information presents special challenges to scientists and the media. Scientists may feel most comfortable when communicating risk in quantitative terms, but as already discussed many persons may have difficulty understanding risk information expressed quantitatively. The same difficulties involved in making risk information comprehensible, accurate, and not misleading in the clinical context also apply to research scientists’ communication with the public. In addition, information contained in the primary scientific literature and intended for consumption by other scientists should be a focus for risk communication. For example, Tabor and Cho (2007) found that studies reporting genetic risk information for autism tended to make causal claims using inconsistent criteria, and sometimes when such claims are not warranted. Inasmuch as information contained in the primary scientific literature may be used by genetic counselors, clinicians, and other risk communicators, misleading claims—even if unintentional and subtle—can have magnified downstream effects.
University press offices also play a large role in communicating autism risk, insofar as they disseminate summarized research findings to the scientific media, the popular media, and the public directly. Press releases are typically less technical than the primary scientific literature upon which they are based, and qualifications and nuances present in an original scientific publication may not be reflected in a press release (Woloshin et al., 2009). Individuals staffing press offices may not be trained in the relevant science or in risk communication. Furthermore, part of the function of university press offices is to bring attention and prestige to a university by highlighting the important and impactful research being done there. While there is nothing wrong with this, some possible tension should be acknowledged between this goal and that of providing clear and accurate risk information. It is easy to inadvertently “hype” a scientific finding on autism risk beyond what is supported by the primary scientific literature.
When risk information is misleading, through simplification, framing, or unintentional “hyping,” harms (of omission, of poorly communicated risk, and of poorly understood risk) to message recipients may result. Individuals and populations might act on this information in ways they otherwise would not had they understood the information correctly. Care should be taken to provide individuals with risk information relevant to their values and interests, while avoiding—to the greatest degree possible—misunderstanding, anxiety, blame, or other bad outcomes. It is recognized that this ideal may be challenging to achieve in practice.
The existence of uncertainty in risk information, particularly preliminary risk information, exacerbates this ethical tension. Where risk information is not robustly supported by evidence, or where the implications of this risk information are not fully understood, it becomes more likely that individuals may act inappropriately, or that scientists or media outlets communicating risk information may draw unwarranted conclusions. For example, scientists may present preliminary research findings at an academic conference, where such findings are not yet ready for publication and are shared for the purposes of providing a “progress report” and to stimulate scholarly collaboration. Nonetheless, members of the media or other stakeholder groups may be present at the conference and gain access to this information (Schwartz et al., 2002). Given the rapid pace of autism research, the intense interest of the general public on this subject, and the continued dissemination of both preliminary and published findings, as we recommend below, clear guidelines for reporting preliminary findings are needed for ASD research.
Even published scientific information comes with varying degrees of evidential support. For example, a recent survey-based study found a statistically significant association between acetaminophen use and ASDs (Schultz et al., 2008), but questions were raised regarding recall bias and the validity of the findings (Cox and Mcdowell, 2009). While the gradual accretion of evidence and debates over the robustness of evidence are part of normal scientific process, from a risk communication standpoint, it should be emphasized that the degree of evidential support for a risk factor has major ethical implications (Pellicano and Stears, 2011). As concerns the present example, acetaminophen is a commonly used anti-inflammatory in infants and young children, and parents’ disuse of this drug on account of concerns about ASD development, if not warranted, may leave children worse-off in light of the lack of alternatives. Thus, it is important to carefully consider the degree of evidential support for autism risk information that is appropriate prior to actively communicating such information. Finally, the notion of “sufficient” or “appropriate” evidential support involves value judgments, and the adequacy of standard scientific conventions governing the acceptance or rejection of claims may at times be subject to reasonable debate, particularly as concerns risk (Cranor, 1997; Shrader-Frechette, 1991).
Further increasing the stakes of autism risk communication is the fact that families affected by autism remain desperate for answers in light of the absence of a comprehensive biological profile of the disorder and an understanding of its etiology for the vast majority of cases. Hence, mistakes in risk communication made by scientists, press offices, or other media professionals may have a greater impact than they would in other contexts, because the audience in question may “latch onto” risk information more strongly than in other contexts. While scientists and risk communicators have obligations to prevent or minimize inadvertent harm, they should not have sole authority in making decisions about the design or timing of ASD risk communication. A number of treatments of risk analysis and risk communication have emphasized the importance of broad stake-holder participation (Kusch, 2007; NRC, 1989; Shrader-Frechette, 1991), and we echo these recommendations, particularly as concerns ASD risk communication. Risk communicators may not be able to know in advance what risk information is relevant to message recipients, nor may they be able to anticipate the comprehensibility of their messages without consulting their intended audience in some capacity. Furthermore, since judgments of “sufficient evidence” are value-laden, there is no good reason to exclude the voices of the broader autism community when considering them.
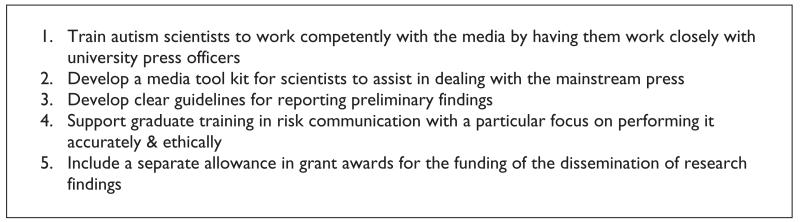
To address these ethical concerns in risk communication, the working group proposed the following five action items and additional areas for further investigation (see Figure 4). First, with little to no media training, scientists can find themselves involved in communicating their results in an unfamiliar medium, which can lead to miscommunications and misunderstandings (Garrett and Bird, 2000). University press officers should work closely with autism scientists for training on interacting with the media. Second, the working group also encouraged the development of a media tool kit—a reference and practical tool that would help scientists navigate the often unfamiliar terms of communicating their findings in nonscientific media.
Figure 4.
Summary of recommendations in priority area 2.
Third, clear guidelines must be developed for reporting preliminary findings. Too often, published studies include forward-looking statements that are far beyond the scope of the published research and are readily misinterpreted by the media and public as being more certain or explanatory of a complex phenomenon than it actually is. As an example, a 2009 genome-wide association study (GWAS) offers a cautionary tale on this matter. The study identified CDH9 and CDH10 as candidate genes that may be associated with ASD etiology. The authors of that study hypothesized that single-nucleotide polymorphisms on these two genes may be “involved in shaping the physical structure and functional connectivity of the brain that leads to the clinical manifestations of ASDs” (Wang et al., 2009). While such GWAS studies reveal important etiologic clues about ASD, the complex phenotype of ASD creates significant obstacles in establishing causality. The article concludes with a forward-looking statement about the potential application of the study’s findings, which the article suggests “can be better integrated to improve our understanding of the molecular basis of ASDs, and foster the development of early preventive and corrective treatment” (Wang et al., 2009).
Somehow, the forward-looking statements from the Science article became an overstatement of the study’s findings in mainstream media. A BBC News Online (2009) story, published the day the Wang study was released, made two unsubstantiated claims: first, that the article had produced “the most compelling evidence to date that genetics play a key role in autism” and that if one common genetic variant identified in the study were corrected, it “would cut cases of autism by 15%.” The original Wang et al.’s article did not directly make this claim. The source most likely was the press release issued by the sponsoring institution that said in its opening paragraph that the study “pin-points a gene region that may account for as many as 15 percent of autism cases …” It is unclear how this estimate was derived, and, consequently, it raises more questions about whether and how this percentage should be reported. Given the wide popular impact that this finding had in both making claims about the genetic nature of ASDs and about the ability to intervene in the natural history of the disorder, the communication of preliminary findings should be more prudent.
Fourth, the working group believed that the National Institutes of Health and other funders of autism research must devote additional resources to training graduate students in risk communication, including ethical issues related to risk communication. Fifth and finally, grant awards should make separate allowance to support engagement of risk communication and ethical issues at every stage of the research process, including, most importantly, for the dissemination of research findings, which would allow scientists to more effectively meet the challenges outlined in this document.
Priority area 3: the importance of tailoring risk communication for autism to different communities and populations, and the role of advocacy organizations
The goal of effective risk communication is to enable people to participate meaningfully in decision-making about their own health and health care, or that of their patients or family members. Parents, service providers, individuals with ASDs, and the general public have a stake in understanding information about risk for autism. However, the populations to whom risk information is targeted differ widely in their needs, perspectives, attitudes, developmental levels, and experiences. Thus, it is important to consider how to tailor risk communication to different individuals and communities in a way that takes into account differences at the individual, familial, cultural, and societal levels.
A number of factors bear upon the consideration of how best to tailor ASD risk information to a particular audience. These include, but need not be limited to, how individuals and populations may differ in their ability to access ASD risk information or to receive a timely diagnosis; how individuals and populations may differ in their ability to understand ASD risk information, their information preferences, or their concerns over time; and how individuals and populations may differ in their beliefs about the causation, categorization, or appropriate treatment of ASDs.
Parents’ experiences with the health-care system or their ability to finance care can influence their access to risk information, as well as their ability to develop a trusting relationship with a health-care provider who is communicating risk information. Based on a national survey of children with special health-care needs, Kogan et al. (2008) found that parents identifying their children as having an ASD were significantly more likely to report problems accessing health care and have unmet needs for family support services, referrals, and coordinated care. Parents from ethnic minority backgrounds reported even greater challenges in obtaining appropriate assessments for their affected child, thereby limiting access to risk information, which is often provided in the context of a diagnostic evaluation (Kogan et al., 2008). Children who are Black, Hispanic, or of other race/ethnicity are less likely than White children to receive a diagnosis (Mandell et al., 2009), require more visits before an assessment is made, and receive a diagnosis at a later age (Mandell et al., 2002). These experiences and the frustration that results from them can influence parents’ ability and willingness to establish a strong relationship with a health-care provider. The presence of such a relationship may enhance the effectiveness of risk communication, while the absence may prevent discussion entirely.
Access to ASD risk information may vary across the international setting. Most prevalence studies to date have been conducted in the United States and United Kingdom. There is very little information about how the genetics, biology, risk factors, treatment, and course of ASD differ across continents, countries, or ethnic groups (Grinker et al., 2011). Meeting the information needs of populations at a global level will ultimately require that population-specific information be available. Efforts to expand data available on diverse US and international populations are currently underway, but face a number of obstacles, including the development of “efficient and affordable diagnostic assessments that are reliable and valid in multiple languages and societies” (Grinker et al., 2011).
Individuals and populations may differ not just in their access to ASD risk information, but in their ability to understand that information, their information preferences, and/or their concerns over time. When autism is diagnosed, questions arise regarding cause, associated health risks, availability and access to intervention and support, and implications for parenting. Many individuals will have low literacy and some will not be capable of reading. In Europe, for example, it is not uncommon for educational and advocacy agencies to provide “easy read” information, which is specifically designed for people whose first language is not English, who may have a reading difficulty, or who would like simplified information about ASD. Other individuals with autism, especially those with impaired receptive language skills, may be helped by the use of photos, visual stories, and cartoons. For many individuals, it will be necessary to involve a legal guardian in the process of communication of risk information. Decision aids, such as pamphlets and videos that describe risk information, have been shown to help individuals understand their options and participate in decision-making, regardless of the intellectual or communication ability of the individual (O’Conner et al., 2009).
Because risk information is often complex, there is a need for repetition of information and an opportunity for questions and follow-up. The kinds of questions that will be relevant are likely to change with the individual’s age, experiences, and current circumstances. Questions about risks associated with autism may be especially pertinent during times when the individual is transitioning from one life stage to another, such as the questions about increased risk for seizures during adolescence or genetic risk during adulthood if and when parenting is considered. This kind of careful, individualized, and developmental approach to risk communication with persons with ASD requires patience, time, and, ideally, an ongoing trusted relationship with a knowledgeable person.
Another important consideration relating to the tailoring of ASD risk information is that individuals and populations may differ in their beliefs about the causation, categorization, or appropriate treatment of ASDs. Parental attitudes and beliefs about what may have caused their child’s autism will influence how risk information is understood, accepted, and used. Such attitudes and beliefs can be influenced by the age of the affected child, his or her developmental history, and the severity and nature of the child’s symptoms and challenges. For example, the results of a parent survey conducted on the IAN (http://www.ianproject.org; Law, 2009) indicated that, whereas the majority (79%) of parents believed that autism was caused by both genetic and environmental factors, parents whose child had a history of regression were much more likely to believe that vaccines cause autism. Such beliefs, rooted strongly in personal experience, may influence parents’ openness and trust toward different ideas and perspectives. Other factors that shape parental attitudes and beliefs about risk factors for autism include their prior experiences with the health-care system, religious, ethnic, and racial backgrounds, media influences, and the historical context, as discussed above (Elder, 1994; Hebert and Koulouglioti, 2010; Ravindran and Myers, 2012).
Just the same, beliefs about the causality of ASDs can differ between cultures more broadly (Grinker et al., 2011; Mandell and Novak, 2005; Ravindran and Myers, 2012). For example, while beliefs about the etiology of ASDs in the United States and United Kingdom focus increasingly on biological causes,
French health professionals generally view autism as a problem that lies within family social relationships and with the mother-child relationship in particular, [and] there are only a few psychiatric or medical centers with expertise on autism as a genetic or brain disorder. (Grinker et al., 2011)
Differing views about the causality of ASDs may manifest in differing views about appropriate treatment, as where behavioral and school-based interventions for ASDs have been generally resisted in France. Even the very recognition of ASDs as such varies between cultures (Grinker et al., 2011). Sensitivity to these individual factors that can influence communication about risk can increase the likelihood that the information conveyed is understood and perceived as credible by parents.
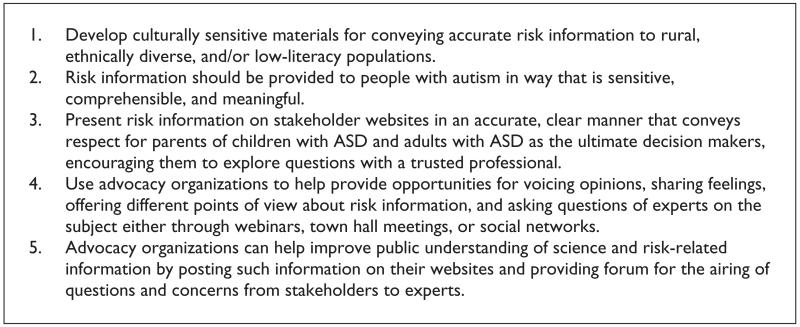
Addressing the various issues raised here is likely to be time-consuming, resource-intensive, and logistically and ethically complex. In particular, individual and cultural variability in belief as concerns the categorization and causality of ASDs raises questions about value judgments and rationality that cannot be explored here. However, working group members identified a number of action items that may be feasible for prioritization in the immediate future (see Figure 5). First, there is a great need for novel strategies and culturally sensitive materials for conveying accurate risk information to rural, ethnically diverse, and/or low-literacy populations. Some efforts in this area have already been made (see, for example, Mackert et al., 2009), but given the profound influence of health literacy, ethnicity, and culture on risk beliefs and attitudes, more attention is needed. Barriers to accessing accurate risk information by parents from ethnic minority backgrounds include lack of training for health-care professionals in autism and risk communication, financial barriers in paying for diagnostic and counseling services, and differing cultural interpretations of the meaning and causes of autism and its symptoms. Parents frequently develop their own beliefs about the causes of their child’s condition; cultural beliefs and attitudes have a significant influence on these beliefs, which will ultimately shape how the information that the health-care provider offers is perceived and accepted.
Figure 5.
Summary of recommendations in priority area 3.
Second, individuals with autism have the right to self-determination and direct involvement in decisions affecting their lives; such a right requires that information be provided to people with autism in way that is sensitive, comprehensible, and meaningful. It is, therefore, important to involve persons with ASD and their families in the discussion concerning how best to convey risk information to persons with ASD and to respectfully consider their concerns that scientific findings pertaining to both genetic and environmental risk factors could lead to discrimination. This call for greater stakeholder participation in ASD risk communication echoes other recommendations as concerns risk assessment and communication more generally (Johnson, 1999; Meghani, 2009; NRC, 1989; Shrader-Frechette, 1991).
Third, advocacy organizations can and should play an important role in risk communication. Such organizations, especially those that are also involved in funding research and supporting legislative reform, are uniquely positioned at the interface of the scientific, government, and stake-holder communities. Their role involves representing the needs and perspectives of families and deciphering and synthesizing the vast amount of complex scientific knowledge in a way that is understandable, trustworthy, and useful for stakeholders.
As mentioned above, a recent survey suggests that parents are increasingly turning to the Internet to access information about autism. Thus, one important role of an advocacy organization is to provide accurate and clear summary information about risk factors. Today, the web is the principal means for conveying such information because of growing ease of access and the ability for the organization to change content easily. Almost all disease-focused advocacy organizations provide such information on their websites, but it can range in depth from the very general statements regarding risk factors to very specific, detailed, and actionable information. Some organizations provide risk information that is specifically intended to influence decision-making and actions, such as information about how to reduce the risk of a disease by avoiding certain exposures (Needleman, 1987). Other organizations provide tools for interpreting risk information, such as how to interpret a medical test related to a disease. Many organizations provide ratings on the empirical validity of certain claims about risk information.
While these tools and types of information are certainly useful for families and affected individuals, effective risk communication is an interactive process requiring opportunities to exchange opinions, ask questions, and discuss risk and methods of managing risk (NRC, 1989). Best practices in risk communication (Covello, 2003) include accepting and involving stakeholders as legitimate partners by demonstrating respect and including them in the decision-making process; listening to people to find out what they know, think, feel, and want done, and letting people know that what they think and feel is valid and has been understood; communicating in a way that is truthful, frank, open, and compassionate; discussing data and information uncertainties, strengths, and weaknesses; and being accessible to reporters and other in the media.
Advocacy organizations can help implement these best practices in risk communication that complement our above-outlined action items by providing on their website, accurate, clear information that conveys respect for the parent as the ultimate decision-maker and encourages parents and affected individuals to further explore their questions and concerns about risk in the context of a trusted relationship with a professional, such as their physician. Advocacy groups should also develop opportunities for give-and-take, offering different points of view, and sharing feelings and concerns about risk information and related research through town hall meetings, webinars that offer time for questions and answers, and through social networks, such as Facebook and blogs, which allow an opportunity for posing questions and airing of different perspectives. Many advocacy organizations also provide a mechanism for direct one-on-one contact (e.g. “Autism Response Team” toll-free number at Autism Speaks), which allows people to discuss their concerns and questions with a knowledgeable person.
When new scientific findings are published, advocacy organizations can also improve the public’s understanding of such findings by posting statements on their website that help interpret the implications of such findings and by responding to queries from the media with clear, accurate information. Increasingly, advocacy organizations are providing scientists an opportunity to post blogs about their new findings that can help provide more detail and context than can typically be offered by the media, as well as an opportunity for airing of questions and perspectives from the stakeholders who read the blog.
Priority area 4: the dissemination of research results to autism research study participants
There is a longstanding and ongoing debate in biomedical research about whether research results should be returned to participants (Fernandez et al., 2004; National Bioethics Advisory Commission (NBAC), 1999; Shalowitz and Miller, 2005). In recent years, much of this debate has focused on the return of genetic results (Bookman et al., 2006; Fabsitz et al., 2010; Ravitsky and Wilfond, 2006). The dilemmas about return of results have been a challenge for genetic studies of autism in the past and present, and will become even more significant as both genetic and environmental studies identify possible causal factors in the future.
The working group discussed several arguments in support of returning of individual research results that are especially relevant in autism research. The first is beneficence, that individual results may provide important benefits to participants. There are three main kinds of direct benefits that are possible from return of results: (1) return of clinically significant and/or actionable results that will affect the treatment of the affected participant, (2) the return of results that provide explanatory or diagnostic information, and (3) return of results to demonstrate reciprocity and trust to research participants, and to provide information and knowledge about the progress of the research study. It is worth noting that Miller et al. (2010) recently documented that autism research participants believed that genetic results that could explain the cause of autism and provide an answer as to “why” a child developed autism should be disclosed to participants, even if they were not fully validated, immediately actionable, or able to provide direct clinical benefit. Another study found that parents of children with autism who were enrolled in genetic research study were interested in results for potential future benefit for reproductive decision-making for themselves, their children, and other family members (Tabor, 2011). These findings support a potentially greater obligation to return results to participants in autism research, as compared to other disease research contexts.
The working group also identified several potential harms that might arise from return of individual research results. Most of these harms arise from the fact that many results may be returned that are not yet validated, or for which the meaning and clinical utility have not been characterized. These potential harms include the following: (a) the potential risk of therapeutic misconception or research participants misunderstanding the goals of research as being synonymous with the goals of clinical care; (b) the potential for misunderstanding and misinterpretation of results, leading to unnecessary diagnostic odysseys or therapeutic choices; and (c) the potential damage to the trust relationship between researchers and research participants, both within the specific study and more broadly in the research enterprise, if results are later found to be incorrect.
The working group discussed the balance between these potential benefits and harms of return of results in the context of autism research. The lack of understanding about the etiology of autism creates unusual challenges both for the potential benefits and potential harms. Researchers may feel obligated to demonstrate reciprocity to participants, providing any possibly useful or personally meaningful results when possible. However, the lack of certainty or validity around research results, as well as the lack of possible clinical utility, may limit the potential benefit of the return of results.
In addition, the pace of autism research has led to a rapid increase in findings, particularly in genetic causes of autism. It is likely that research on environmental causes of autism may also yield substantive findings in the near future. As the aggregate findings of these studies are reported in the media, researchers and participants may have increased expectations about the return of individual research results and about the meaning of those results.
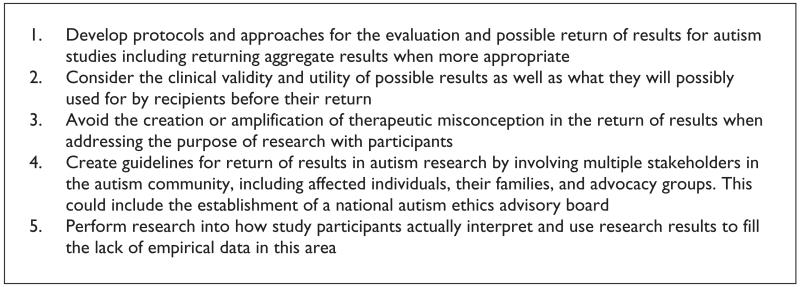
Given these challenges, the working group developed five recommendations (see Figure 6) surrounding the return of results in autism research. First, researchers should develop protocols and approaches for the evaluation and possible return of results for autism studies. These protocols should consider the impact of results on the individuals and families in the studies, and how these families will use this risk information, if at all. They should include a time line for when possible results will be communicated to study participants. The working group also agreed that researchers should develop plans for communicating aggregate, as well as individual, results to research participants, as there may be situations where return of aggregate results is more appropriate.
Figure 6.
Summary of recommendations in priority area 4.
Second, when considering results for return, researchers should consider the clinical validity and utility of possible results. Because so little is understood about the etiology of autism, there may be a potential to prematurely return results to participants in the name of reciprocity, even if the results are preliminary and not validated or incompletely understood. Researchers need to consider what participants will do with results, and whether the results actually provide adequate benefit to participants to merit return.
Third, researchers should avoid the creation or amplification of therapeutic misconception in the return of results. In autism, because many research studies are conducted in academic medical centers, parents of participants may believe that research is expected to provide direct clinical benefits to their children, rather than generate generalizable knowledge. In this context, the return of results may increase this potential therapeutic misconception and increase the likelihood that participants will misunderstand the meaning of results.
Fourth, multiple stakeholders in the autism community, including affected individuals, their families, and advocacy groups, should be involved in the creation of guidelines for return of results in autism research. One possible strategy for achieving this is to establish a national autism ethics advisory board, composed of multiple stakeholders, that could create guidelines and serve as a consult service for ethical issues and planning related to the return of results.
Fifth and finally, the working group acknowledged that there are little if any empirical data about how study participants actually interpret and use research results and that there is a need for research in this area. The working group recommends that autism researchers who are returning results partner with researchers who can empirically study the process and short- and long-term impacts of return of results on participants. These data can be used to inform return of results guidelines, as well as future studies and researchers facing these issues.
Conclusions
There currently remains a lack of understanding of the mechanisms of autism etiology. The increasing volume of research in this area may bring rapid change to our understanding of this complex disorder. At a follow-up meeting held at Seattle Children’s Hospital and the University of Washington, a smaller group began to plan for the process of developing research projects examining some of the challenges of autism risk communication and ethics and the challenges inherent in disseminating novel findings in autism science. Several working group members are collaborating on projects that will hopefully begin to clarify the complexities examined in this article. In addition, researchers around the world are also beginning to pay closer attention to these issues (Pellicano and Stears, 2011). Without rigorous attention to risk communication and ethics regarding the dissemination of these findings, the benefits of such findings may lead to poor risk communication and general misunderstanding of the disorder. Our field and those for whom this research is done will benefit from closer attention to these issues. Scientists need to be proactive on matters of risk and ethics. If the history of autism is any guide, failure to do so would be irresponsible.
Acknowledgement
The authors wish to thank Aaron Pankiewicz, MPH, for his research assistance on this paper.
Funding
This research received support from Autism Speaks and The National Institutes of Health, Grant 1R13ES017394-01.
Contributor Information
Michael Yudell, Drexel University, USA.
Holly K Tabor, University of Washington, USA; Seattle Children’s Research Institute, USA.
Geraldine Dawson, University of North Carolina; Autism Speaks, USA.
John Rossi, Drexel University, USA.
Craig Newschaffer, Drexel University, USA.
References
- Austin H, Campion-Smith C, Thomas S, et al. Parents’ difficulties with decisions about childhood immunisation. Community Practitioner. 2008;81(10):32–35. [PubMed] [Google Scholar]
- Baio J. Prevalence of autism spectrum disorders—autism and development disabilities monitoring network, 14 sites, United States, 2008. MMWR Surveillance Summaries. 2012;61(SS03):1–19. [PubMed] [Google Scholar]
- Baker J. Mercury, vaccines, and autism: one controversy, three histories. American Journal of Public Health. 2008;98(2):244–253. doi: 10.2105/AJPH.2007.113159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC News ÒGenes have key role in autismÓ. BBC News Online. 2009 Apr 28; 2009. http://news.bbc.co.uk/2/hi/health/8020837.stm.
- Berkel S, Marshall CR, Weiss B, et al. Mutations in the SHANK2 synaptic scaffolding gene in autism spectrum disorder and mental retardation. Nature Genetics. 2010;42(6):489–491. doi: 10.1038/ng.589. [DOI] [PubMed] [Google Scholar]
- Berry DC, Raynor DK, Knapp PR, et al. Official warnings on thromboembolism risk with oral contraceptives fail to inform users adequately. Contraception. 2002;66:305–307. doi: 10.1016/s0010-7824(02)00386-4. [DOI] [PubMed] [Google Scholar]
- Bookman EB, Langehorne AA, Eckfeldt JH, et al. Reporting genetic results in research studies: summary and recommendations of an NHLBI working group. American Journal of Medical Genetics, Part A. 2006;140:1033–1040. doi: 10.1002/ajmg.a.31195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carruth RS, Goldstein BD. Relative risk greater than two in proof of causation in toxic tort litigation. Jurimetrics. 2001;41:195. [Google Scholar]
- Casiday R. Children’s health and the social theory of risk: insights from the British MMR controversy. Social Science & Medicine. 2007;65:1059–1070. doi: 10.1016/j.socscimed.2007.04.023. [DOI] [PubMed] [Google Scholar]
- Casiday R. Risk communication in the British pertussis and MMR vaccine controversies. In: Bennett P, Calman K, Curtis S, et al., editors. Risk Communication and Public Health. Oxford University Press; New York: 2010. pp. 129–146. [Google Scholar]
- Chambers T. The Fiction of Bioethics. Routledge; New York: 1999. [Google Scholar]
- Charman T, Pickles A, Chandler S, et al. Commentary: effects of diagnostic thresholds and research vs service and administrative diagnosis on autism prevalence. International Journal of Epidemiology. 2009;38(5):1234–1238. doi: 10.1093/ije/dyp256. author reply 1243-1244. [DOI] [PubMed] [Google Scholar]
- Chen DT, Miller FG, Rosenstein DL. Ethical aspects of research into the etiology of autism. Mental Retardation and Developmental Disabilities Research Reviews. 2003;9(1):48–53. doi: 10.1002/mrdd.10059. [DOI] [PubMed] [Google Scholar]
- Condit CM, Shen L. Public understanding of risks from gene-environment interaction in common diseases: implications for public communications. Public Health Genomics. 2011;14(2):115–124. doi: 10.1159/000314915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covello VT. Best practices in public health risk and crisis communication. Journal of Health Communication. 2003;8:5–8. doi: 10.1080/713851971. [DOI] [PubMed] [Google Scholar]
- Cox AR, Mcdowell S. A response to the article on the association of paracetamol/acetaminophen use and autism by Stephen T. Schultz. Autism. 2009;13(1):123–125. doi: 10.1177/1362361308101816. [DOI] [PubMed] [Google Scholar]
- Cranor CF. The normative nature of risk assessment: features and possibilities. Risk: Health, Safety, and Environment. 1997;8:123–136. [Google Scholar]
- Croen L, Grether JK, Yoshida CK, et al. Antidepressant use during pregnancy and childhood autism spectrum disorders. Archives of General Psychiatry. 2011 doi: 10.1001/archgenpsychiatry.2011.73. Epub ahead of print 4 July 2011. DOI: 10.1001/archgenpsychiatry.2011.73. [DOI] [PubMed] [Google Scholar]
- Deth R, Muratore C, Benzecry J. How environmental and genetic factors combine to cause autism: a redox/methylation hypothesis. Neurotoxicology. 2008;29(1):190–201. doi: 10.1016/j.neuro.2007.09.010. [DOI] [PubMed] [Google Scholar]
- Douglas M, Wildavsky A. Risk and Culture: An Essay on the Selection of Technical and Environmental Dangers. University of California Press; Berkeley, CA: 1982. [Google Scholar]
- Earle TC, Cvetkovich GT. Social Trust: Toward a Cosmopolitan Society. Praeger Publishing; Westport, CT: 1995. [Google Scholar]
- Elder JH. Beliefs held by parents of autistic children. Journal of Child and Adolescent Psychiatric Nursing. 1994;7(1):9–16. doi: 10.1111/j.1744-6171.1994.tb00184.x. [DOI] [PubMed] [Google Scholar]
- Fabsitz RR, McGuire A, Sharp RR, et al. Ethical and practical guidelines for reporting genetic research results to study participants: updated guidelines from a National Heart, Lung and Blood Institute working group. Circulation: Cardiovascular Genetics. 2010;3:574–580. doi: 10.1161/CIRCGENETICS.110.958827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez CV, Skedgel C, Weijer C. Considerations and costs of disclosing study findings to research participants. Canadian Medical Association Journal. 2004;170:1417–1419. doi: 10.1503/cmaj.1031668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiester A. Viewpoint: why the clinical ethics we teach fails patients. Academic Medicine. 2007;82:684–689. doi: 10.1097/ACM.0b013e318067456d. [DOI] [PubMed] [Google Scholar]
- Finkel A. Perceiving others’ perceptions of risk: still a task for Sisyphus. Annals of the New York Academy of Sciences. 2008;1125:121–137. doi: 10.1196/annals.1399.013. [DOI] [PubMed] [Google Scholar]
- Fischhoff B. Nonpersuasive communication about matters of greatest urgency: climate change. Environmental Science & Technology. 2007;41(21):7204–7208. doi: 10.1021/es0726411. [DOI] [PubMed] [Google Scholar]
- French S, Maule J. Exploring and communicating risk: scenario-based workshops. In: Bennett P, Calman K, Curtis S, et al., editors. Risk Communication and Public Health. Oxford University Press; New York: 2010. pp. 299–316. [Google Scholar]
- Garrett JM, Bird SJ. Ethical issues in communicating science. Science and Engineering Ethics. 2000;6(4):435–442. doi: 10.1007/s11948-000-0001-7. [DOI] [PubMed] [Google Scholar]
- Geschwind DH, Levitt P. Autism spectrum disorders: developmental disconnection syndromes. Current Opinion in Neurobiology. 2007;17(1):103–111. doi: 10.1016/j.conb.2007.01.009. [DOI] [PubMed] [Google Scholar]
- Gigerenzer G, Hertwig R, Van den Broek E, et al. “A 30% chance of rain tomorrow”: how does the public understand probabilistic weather forecasts? Risk Analysis. 2005;25:623–629. doi: 10.1111/j.1539-6924.2005.00608.x. [DOI] [PubMed] [Google Scholar]
- Grinker RR, Yeargin-Allsopp M, Doyle C. Culture and autism spectrum disorders: the impact on prevalence and diagnosis. In: Amaral A, Geschwind D, Dawson G, editors. Autism Spectrum Disorders. Oxford University Press; Oxford: 2011. pp. 112–136. [Google Scholar]
- Hallmeyer J, Cleveland S, Torres A, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Archives of General Psychiatry. 2011 doi: 10.1001/archgenpsychiatry.2011.76. Epub ahead of print 4 July 2011. DOI: 10.1001/archgenpsychiatry.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampel J. Different concepts of risk—a challenge for risk communication. International Journal of Medical Microbiology. 2006;296(Suppl. 40):5–10. doi: 10.1016/j.ijmm.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Hansson SO. The false promises of risk analysis. Ratio. 1993;6(1):16–26. [Google Scholar]
- Hebert EB, Koulouglioti C. Parental beliefs about cause and course of their child’s autism and outcomes of their beliefs: a review of the literature. Issues in Comprehensive Pediatric Nursing. 2010;33(3):149–163. doi: 10.3109/01460862.2010.498331. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) Autism and the Environment: Challenges and Opportunities for Research; Workshop Proceedings; Washington, DC: National Academies Press. 2008. [Google Scholar]
- Johnson BB. at. Risk Analysis. 1999;19(3):335–348. doi: 10.1023/a:1007084108903. [DOI] [PubMed] [Google Scholar]
- Jordan BR, Tsai DFC. Whole-genome association studies for multigenic diseases: ethical dilemmas arising from commercialization—the case of genetic testing for autism. Journal of Medical Ethics. 2010;36:440–444. doi: 10.1136/jme.2009.031385. [DOI] [PubMed] [Google Scholar]
- Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217–250. [PubMed] [Google Scholar]
- King M, Bearman P. Diagnostic change and the increased prevalence of autism. International Journal of Epidemiology. 2009;38(5):1224–1234. doi: 10.1093/ije/dyp261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan MD, Strickland BB, Blumberg SJ, et al. A national profile of the health care experiences and family impact of autism spectrum disorders among children in the United States, 2005-2006. Pediatrics. 2008;122:1149–1158. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- Kusch M. Towards a political philosophy of risk. In: Lewens T, editor. Risk: Philosophical Perspectives. Routledge; New York: 2007. [Google Scholar]
- Law P. Presentation of interactive autism network parent survey results with discussion; Presentation at the 2009 meeting on ethics of communicating scientific findings of autism risk; Philadelphia, PA. 6-7 October 2009.2009. [Google Scholar]
- Mackert M, Kahlor L, Tyler D, et al. Designing e-health interventions for low-health-literate culturally diverse parents. Telemedicine Journal and e-Health. 2009;15:672–677. doi: 10.1089/tmj.2009.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon WM, Baty BJ, Botkin J. Genetic counseling and ethical issues for autism. American Journal of Medical Genetics Part C-Seminars in Medical Genetics. 2006;142(1):52–57. doi: 10.1002/ajmg.c.30082. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Novak M. The role of culture in families’ treatment decisions for children with autism spectrum disorders. Mental Retardation and Developmental Disabilities Research Reviews. 2005;11(2):110–115. doi: 10.1002/mrdd.20061. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Listerud J, Levy SE, et al. Race differences in the age of diagnosis among medicaid-eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1447–1453. doi: 10.1097/00004583-200212000-00016. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Wiggins LD, Carpenter LA, et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health. 2009;99:493–498. doi: 10.2105/AJPH.2007.131243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meghani Z. The US food and drug administration, normativity of risk assessment, GMOs, and American democracy. Journal of Agricultural & Environmental Ethics. 2009;22:125–139. [Google Scholar]
- Miller FA, Hayeems RZ, Bytautas JP. What is a meaningful result? Disclosing the results of genomic research in autism to research participants. European Journal of Human Genetics. 2010;18:867–871. doi: 10.1038/ejhg.2010.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bioethics Advisory Commission (NBAC) Research Involving Human Biological Materials: Ethical Issues and Policy Guidance. National Bioethics Advisory Commission; Rockville, MD: 1999. [Google Scholar]
- National Research Council (NRC) Improving Risk Communication. National Academy Press; Washington, DC: 1989. [Google Scholar]
- Needleman C. Ritualism in communicating risk information. Science Technology & Human Values. 1987;12(3-4):20–25. [Google Scholar]
- Newschaffer CJ, Falb MD, Gurney JG. National autism prevalence trends from United States special education data. Pediatrics. 2005;115(3):277–282. doi: 10.1542/peds.2004-1958. [DOI] [PubMed] [Google Scholar]
- O’Connor AM, Bennett CL, Stacey D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews. 2003;1:1–94. doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- O’Conner AM, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD001431.pub2. published online, http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001431/frame.html. [DOI] [PubMed] [Google Scholar]
- Pellicano E, Stears M. Bridging autism, science, and society: moving toward an ethically informed approach to autism research. Autism Research. 2011;4(4):271–282. doi: 10.1002/aur.201. [DOI] [PubMed] [Google Scholar]
- Raithatha N, Holland R, Gerrard S, et al. A qualitative investigation of vaccine risk perception amongst parents who immunize their children: a matter of public health concern. Journal of Public Health Medicine. 2003;25(2):161–164. doi: 10.1093/pubmed/fdg034. [DOI] [PubMed] [Google Scholar]
- Ravindran N, Myers BJ. Cultural influences on perceptions of health, illness, and disability: a review and focus on autism. Journal of Child and Family Studies. 2012;21:311–319. [Google Scholar]
- Ravitsky V, Wilfond BS. Disclosing individual genetic results to research participants. American Journal of Bioethics. 2006;6:8–17. doi: 10.1080/15265160600934772. [DOI] [PubMed] [Google Scholar]
- Rhoades RA, Scarpa A, Salley B. The importance of physician knowledge of autism spectrum disorder: results of a parent survey. BMC Pediatrics. 2007;7:37–47. doi: 10.1186/1471-2431-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman KJ. Chapter 3: measuring disease occurrence and causal effects. In: Rothman KJ, editor. Epidemiology: An Introduction. Oxford University Press; New York: 2002a. pp. 46–49. [Google Scholar]
- Rothman KJ. Chapter 2: what is causation. In: Rithman KJ, editor. Epidemiology: An Introduction. Oxford University Press; New York: 2002b. pp. 12–13. [Google Scholar]
- Rutter ML. Progress in understanding autism: 2007-1010. Journal of Autism and Developmental Disorders. 2011;41:395–404. doi: 10.1007/s10803-011-1184-2. [DOI] [PubMed] [Google Scholar]
- Schultz ST, Klonoff-Cohen HS, Wingard DL, et al. Acetaminophen (paracetamol) use, measles-mumps-rubella vaccination, and autistic disorder: the results of a parent survey. Autism. 2008;12(3):293–307. doi: 10.1177/1362361307089518. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S, Baczek L. Media coverage of scientific meetings: too much, too soon? Journal of the American Medical Association. 2002;287(21):2859–2863. doi: 10.1001/jama.287.21.2859. [DOI] [PubMed] [Google Scholar]
- Shalowitz DI, Miller FG. Disclosing individual results of clinical research: implications of respect for participants. Journal of the American Medical Association. 2005;294(6):737–740. doi: 10.1001/jama.294.6.737. [DOI] [PubMed] [Google Scholar]
- Shrader-Frechette KS. Risk and Rationality: Philosophical Foundations for Populist Reforms. University of California Press; Los Angeles, CA: 1991. [Google Scholar]
- Silverman C, Brosco J. Understanding autism: parents and pediatricians in historical perspective. Archives of Pediatrics & Adolescent Medicine. 2007;161(4):392–398. doi: 10.1001/archpedi.161.4.392. [DOI] [PubMed] [Google Scholar]
- Slovic P. Perception of risk. Science. 1987;236(4799):280–285. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- Slovic P. Public perception of risk. Journal of Environmental Health. 1997;59(9):22–24. [Google Scholar]
- Smith SG, Wolf MS, von Wagner C. Socioeconomic status, statistical confidence, and patient-provider communication: an analysis of the Health Information National Trends Survey. Journal of Health Communication. 2010;15:169–185. doi: 10.1080/10810730.2010.522690. [DOI] [PubMed] [Google Scholar]
- Tabor H. Commentary: bioethical considerations in autism research and translation—present and future. In: Amaral D, Dawson G, Geschwind DH, editors. Autism Spectrum Disorders. Oxford University Press; New York: 2011. pp. 1337–1342. [Google Scholar]
- Tabor H, Cho M. Ethical implications of array comparative genomic hybridization in complex phenotypes: points to consider in research. Genetics in Medicine. 2007;9(9):626–631. doi: 10.1097/GIM.0b013e3181485688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K, Zhang H, Ma D, et al. Common genetic variants on 5p14.1 associated with autism spectrum disorder. Nature. 2009;459:528–533. doi: 10.1038/nature07999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woloshin S, Schwartz LM, Casella SL, et al. Press releases by academic medical centers: not so academic? Annals of Internal Medicine. 2009;150(9):613–618. doi: 10.7326/0003-4819-150-9-200905050-00007. [DOI] [PubMed] [Google Scholar]