Abstract
With the continued spread of the COVID-19 pandemic and the strict implementation of quarantine policy, the levels of anxiety among university students surged in the lockdown period. Previous studies confirmed the effectiveness of social support in mitigating anxiety, so offering social support should be of high priority in COVID-19, especially in quarantine. However, various coping strategies against the pandemic may explain the link between social support and anxiety. The purpose of this study was to investigate the associations of social support, coping strategy against COVID-19, and anxiety, identifying the potential mediating effect of coping strategy between social support and anxiety during the COVID-19 quarantine. Home-quarantined Chinese university students (N = 2640; 68.79% female) completed online ratings of social support, coping, and anxiety from February 21st to 24th, 2020, when they had been confined to their homes in the peak of the pandemic. Sex and academic attainment being covariates, path analysis with parallel mediation were conducted using “lavaan” package in R environment. Anxiety was significantly negatively related to subjective support and counselor support, while family support did not demonstrate substantive associations with anxiety. The mediating role of cognitive coping was found between all the three social support sources and anxiety. Emotional coping and behavioral coping were found to partially mediate the relationship between subjective support and anxiety, fully mediate the associations of family support and anxiety. However, the impact of counselor support on anxiety was not found to be mediated by emotional coping and behavioral coping. This large-scale online study provides initial evidence that various coping strategies may mediate the relationship between three sources of social support and anxiety in quarantine to some extent. Given that coping against COVID-19 is a valuable reasearch goal upon the global ongoing challenge, the findings will shed more light on the mechanism in the link between coping, social support, and anxiety.
Keywords: Coping strategy, Social support, Anxiety, Path analysis model, COVID-19 quarantine
Background
The COVID-19 pandemic has escalated into a global crisis currently, and over 50 thousand confirmed cases were reported from the previous day, with total 4,424,330 confirmed cases and 1.45% of fatal cases, as of July 30, 2021 (World Health Organization, 2021). Considering the high transmission rate of this disease, many governments have implemented national policies to reduce social contact, such as requirement for quarantine at home, prohibition of outdoor activities, extension of national holidays, and closure of schools (Yue et al., 2020). With increasing numbers of COVID-19 infections at the outbreak, China extended the lockdown policy imposed on Wuhan on 23 January to all the other cities, leading to a nationwide home quarantine period (Wang et al., 2020b). However, the quarantine policy which forced residents to stay indoors and regulate physical interaction amplifies psychological and social burdens. Greek students reported that their mental health was greatly impacted by the closure of universities and the subsequent transition to distance learning (Karasmanaki & Tsantopoulos, 2021). Moreover, a majority of students interviewed in the United States demonstrated the elevated sense of social isolation (Son et al., 2020).
Particularly, some studies called for the attention on the age-based differences in the negative anxious emotion. By definition, anxiety is a feeling of apprehension, dread, or foreboding with autonomic signs and symptoms, in the presence or absence of a stressful situation (Zhou et al., 2016). A global survey of 1653 participants from 63 countries observed high levels of stress and anxiety regardless of the number of COVID-19 cases, and further found age as moderator between the pandemic stress and anxiety, indicating that younger groups were more vulnerable to stress (Varma et al., 2020). A corresponding study of 1297 samples during the COVID-19 confinement found high anxiety among French university students (Vigouroux et al., 2021). An Ecuadorian study found that social isolation affected the mental health of the public, and students tended to be more anxious than nonstudents (Mautong et al., 2021). Anxiety was also found among Indonesian, Taiwanese and Thai university students in a comparative study in which Thai students presented the highest levels of anxiety (Pramukti et al., 2020). These studies suggested age-specific interventions for the vulnerable individuals (Bruffaerts et al., 2018). Therefore, coping strategies to reduce anxiety among university students should arouse great attention of the researchers.
Among the interacting factors that have been shown to influence anxiety, social support has been identified as one of the most valuable predictors of anxiety. There is considerable evidence that social support is an effective factor to alleviate anxiety (Zhu et al., 2020). A Chinese study in February 2020 demonstrated that medical students who possessed medium or low level of social support were inclined to elicit an elevated possibility of mild to severe anxiety than those with high level of social support (Yin et al., 2021), anxiety being associated with reduced likelihood of seeking social support. More importantly, lack of social support in home quarantine period may elicit anxiety. Study among French students during lockdown identified tensions at home, difficulties isolating, and not direct outdoor access as the risk factors for anxiety, while family and friend support were protective factors (Bourion-Bedes et al., 2021). Study on home-quarantined nursing students in China found insufficient social support was one of the risk factors for anxiety (Li et al., 2021b). Lack of adaptive functioning in the relationships among the family members during the lockdown period may cause mental disorders, especially regarding younger students. The prolonged confinement at home may elicit frustration and boredom, lack of physical contact with classmates, desire for personal space, which can trigger subsequent problematic interactions among families (Wang et al., 2020b). Besides, social distancing (e.g., confinement to unsupportive home environments and isolation from closed social networks) may result in more stressors (Fish et al., 2020). Result of thematic analysis of the interviewed students in Australia viewed social support as one dominant theme the students were concerned about (Brett et al., 2021). Therefore, social support is urgently needed to avoid exacerbating existing anxiety in quarantine.
Apart from social support, the literature proposed the significance of utilizing accurate coping strategies against COVID-19 in mitigating anxiety. Study on general health has found that COVID-19 anxiety was negatively related with COVID-19 coping (Yildirim et al., 2021). Prior study also found the availability of updated health information and precautionary behaviors were associated with lower levels of anxiety (Wang et al., 2020a). Similarly, it was reported that health care professionals who had no COVID-19 update were almost 5 times more likely to elicit anxiety than those who had an update (Teshome et al., 2020). Furthermore, Chinese nursing students reported various degrees of fear, anger, and anxiety, and fear emotion was moderately and positively associated with anxiety during the lockdown period (Huang et al., 2020). Hence, the importance of gauging coping strategies toward COVID-19 and their potential influences on anxiety has been highlighted in the extant literature. Although the construct of coping embraced social support in a broad sense (Kassam, 2019), social support should be tailored as one separate variable apart from coping for the sake of the specific role of social support in the pandemic-related coping mechanism. Consequently, while it is clear that social support affects anxiety and that coping strategy impacts anxiety, it is unclear as to whether different coping strategies, such as cognitive coping, emotional coping, and behavioral coping, would explain associations between various social support sources and anxiety.
Social Support and Anxiety in the Pandemic
The significant role of social support in coping with COVID-19 deserves great attention. One American study surveyed the types of coping that 1086 Americans employed to manage stressors online in early April 2020 and encouraged frequent use of emotional support-seeking strategies (Park et al., 2020). Indeed, numerous studies on students documented the relationship between social support and anxiety in the COVID-19 context. Specifically, studies have probed into the anxious problem during the COVID-19 confinement on a variety of university populations. A Chinese study sampled on 7143 college-level medical students found a negative association between social support and anxiety (Cao et al., 2020). A cross-sectional study of 3454 vocational college students found that perceived social support was negatively correlated with general anxiety as well (Mai et al., 2021). Survey from 506 university students in Turkey also justified the negative relationship between social support and quarantine-related anxiety (Yalcin et al., 2021). The empirical study conducted in the lockdown in China observed the negative correlation between social support and trait anxiety, and social support was negatively associated with state anxiety (Ao et al., 2020). Despite these findings, the majority of research examining the associations between social support and anxiety in COVID-19 has focused on the general social support, rather than specific social support from various sources. Therefore, additional research covering diversified sources of social support is needed to fully characterize the relationship between social support and anxiety in quarantine.
Social support is normally defined as the individual’s perceived availability of potentially supportive social ties (Cohen & Hoberman, 1983). Based on the typologies of Chinese version of the Social Support Rating Scale (SSRS) (Duan et al., 2019; Xiao, 1994, 1998), social support can be classified into two categories, namely, subjective support and objective support. The former is a broader measure of perceived availability of support from family and friends, labelled as subjective support, indicating the perceived satisfaction, and feeling of being supported and understood of the individual, while the latter is objective and practical support in terms of frequency of contacts, referring to the relationship-specific actual support directly from social networks (such as family, colleagues, and other group relationships) (Duan et al., 2019). Most of the existing studies were concerned about the perceived support. One comparative study found that perception of more satisfactory support contributed to higher levels of anxiety for Indonesian and Thai students (Pramukti et al., 2020). Given the mixed findings concerning social support and anxiety, subjective support was identified as an overarching parameter in this study. In other words, the role of subjective support should be further analyzed, especially in conjunction with other types of support. Given that the perception of resources may not represent resources actually possessed (Chwaszcz et al., 2021), and people tend to use available resources to cope effectively with difficulties, the constructs of subjective support and objective support were reasonable in the COVID-19 situation. Objective support was further categorized into family support and counselor support to highlight the situational nature of social support in COVID-19 pandemic. There is a need for the distinction of the sources of objective support in that Chinese students regarded support from family and friends as the most used support and support from teachers as the least used one (Mai et al., 2021). Family support referred to the availability of objective support from family and counselor support tapped the utilization of support from psychological counselors when individual met mental stress. The multiple sources of objective support invoked the specific exploration of their roles in the pandemic-related coping system. The study based on Chinese Weibo users revealed that the public were more worried about their families than friends and tended to seek emotional support from their families in the pandemic (Li et al., 2020b), since seeking family support could satisfy emotional needs and thus reduce stress in an emergency (Chwaszcz et al., 2021). Keeping good interpersonal relationships with family members could reduce the anxiety of Spanish university students (Garvey et al., 2021). Moreover, offering online counseling was another source of psychological support. Previous studies have made recommendations that experts should provide sufficient mental healthcare services including preventive support and counseling to vulnerable young students while monitoring their anxiety levels (Karasmanaki & Tsantopoulos, 2021). From this viewpoint, counselor support could be an important source of social support in the pandemic.
Coping Strategies as Mediators of the Link Between Social Support and Anxiety
Coping strategies are defined as certain cognitive, emotional, or behavioral actions employed in the face of stressors beyond personal resources, which are normally classified as either positive or negative (Vinothkumar et al., 2016). Positive coping, namely, problem solving or looking for advice, was supposed to decrease stress, while negative coping, such as self-blame, avoidance, and wishful thinking, was found to be related to higher levels of stress (Vinothkumar et al., 2016). Patients with negative coping suffered more anxious emotions in contrast to the corresponding parts using constructive coping strategies (Jankowska-Polanska et al., 2020).
The unprecedented COVID-19 has stimulated much of research on the mediating role of coping in the relationship of social support and mental system. A COVID-19 related study on individuals who had participated in a psychological support project in Poland found that coping strategies exerted a mediating role both in the association between resource gains and the quality life, and between resource losses and the quality of life, which included the domain of psychological health (Chwaszcz et al., 2021). In specific, resource gain reduced helplessness-based coping, while resource loss increased helplessness which in turn reduced the quality of life. Previous studies have proved the inter-related associations of social support, coping and wellbeing, while some literature highlighted the mediating effect of coping between social support and anxiety. Positive refocusing, which was an adaptive coping strategy in COVID-19, was pursued as a mediator among elderly population so that higher perceived social support led to higher positive refocusing, which in turn resulted in less incidence of anxiety (Labadi et al., 2021). One empirical study in China demonstrated the mediating effect of coping style between social support and anxiety during COVID-19. By use of the Self-rated Anxiety Scale, Social Support Rate Scale, and Trait Coping Style Scale, the study surveyed Chinese medical staff and found that social support had direct and negative effect on anxiety. Further, social support also exerted indirect effect on anxiety through the partial mediating role of positive coping and negative coping. This COVID-19-related study provided preliminary evidence that the impact of social support on anxiety may operate through coping (Zhu et al., 2020). Although how different social support sources influence coping strategies against COVID-19 is unclear, previous disaster-related study which demonstrated a positive association between social support and problem-focused coping under typhoon circumstances proved an evidence on the link between social support and coping strategies (Chao, 2017). To be more specific, a COVID-19 related study in Taiwan found that lower perceived social support was significantly associated with higher active coping (Li et al., 2021a). Again, Chinese students with high levels of social support from family and friends tended to adopt more positive coping strategies (Mai et al., 2021). These studies have proposed the potential mediating role of coping between social support and anxiety in the pandemic context.
Therefore, the present study focused on the potential mediating roles of three coping strategies in the relationship of various social support and anxiety under the COVID-19 pandemic context. The impact of coping strategies on anxiety can be understood in the context of Lazarus and Folkman’s theory of psychological stress, which posits that the dynamic interactions between individuals and their environment provoke stress, and individuals address the stressor by appraising the significance of stressors and utilizing their perceived resources (Lazarus & Folkman, 1984). Although pandemic-related research has consistently shown the effect of positive coping and negative coping on the anxiety, the classic categorization of positive coping and negative coping cannot unravel the associations between the internal construct of coping and mental disorders in the pandemic, which indicates a contextual gap. According to the existing theory of coping, coping is defined as cognitive and behavioral efforts employed to manage the external or internal demands of stressful events (Folkman & Lazarus, 1984). Meanwhile, the coping process is deeply related to the emotional mechanism (Belhaj et al., 2016), and Roseman (2013) addresses emotion as “a coherent, integrated system of general-purpose coping strategies, guided by appraisal, for responding to situations of crisis”. Coping strategies are also defined as “efforts to regulate emotions, behaviors, cognitions, psychophysiology, and environmental aspects in response to the stress of everyday events” (Morales-Rodriguez & Perez-Marmol, 2019). Further, coping strategies are situation-based, and the effectiveness of the same strategy can be varied depending on the specific situation (Carver et al., 1989; Lazarus & Folkman, 1984). Hence, emotion can be examined as a coping strategy against the pandemic on an exploratory basis. In fact, a recent study has employed the construct of emotional and cognitive responses, and behavioral coping in the COVID-related study (Cai et al., 2020). Given the lack of COVID-related theorizing of coping strategies, the present study constructed a pandemic-specific framework of coping strategies, namely, cognitive, emotional, and behavioral coping, on the basis of the stress and coping model to highlight the eminently situational nature of the functionality of coping strategies. Coping strategies in this study was defined as individual’s response to the threat of COVID-19 in the aspects of cognition, emotion, and behavior. To be specific, cognitive coping indicated the appraise and awareness of the current crisis and the way pandemic news was handled. Appropriate acquisition of COVID-19-related information would lead to lower levels of anxiety (Wang et al., 2020a), while other study found Chinese students who eagerly updated the pandemic information might develop anxiety symptoms (Huang & Zhao, 2020). The classic emotional-focused coping drawn by the Cognitive-Motivational-Relational Theory of emotion pertained to the emotional adaptive actions, including the search for emotional support, emotional suppression, avoidance, etc. (Lazarus, 1999). According to Taylor’s (2019) psychological conclusions of the pandemic, a moderate level of fear and anxiety facilitated people to cope with health threats, while severe distress hindered coping. Besides, the management of emotions resulted in effective coping with stress (Cabanach et al., 2016). In this sense, individual’s emotional response promoted coping, and moderate emotional reactions could be deemed as positive and adaptive emotional coping, resulting in constructive functions. The impact of emotional coping can be assumed based on an early research on the onset of the pandemic in Poland that has found the emotional reactions to the perceived threats served an instrumental role in motivating individuals to cope proactively (Cypryanska & Nezlek, 2020). In this view, emotional coping thereby referred to moderate and reasonable COVID-19 specific emotional reactions to the perceived threats of COVID-19. Herein, the construct of emotional reactions was a broader use of emotion models, which was more adaptive and oriented to the practical research needs. Evidence of Chinese local and overseas university students proved that fear of infection and insecurity were significant predictors of anxiety (Feng et al. 2021). In addition, worry about the influence of COVID-19 had a highly positive effect on the level of anxiety (Dhar et al., 2020). Again, healthcare workers who had COVID-19 related worry were more likely to elicit severe anxiety (Teshome et al., 2020). Behavioral coping signified the activities to alter the stressful encounter (Lazarus & Folkman, 1984), indicating the preventive measures in the pandemic specifically, namely, masking-wearing, hygiene practice, control of social distancing, and avoidance of potential infectious circumstance (Kim et al., 2021). Personal preventive measures including handwashing, social distancing, and wearing face masks were found to be related to fewer psychiatric symptoms (Tan et al., 2020; Wang et al., 2020a). Given that coping plays a mediating role in the relationship between social support and anxiety, there is a reason to hypothesize that coping strategies would be a mediator between social support and anxiety in the pandemic-related context. This novel model would broaden the perception of the coping mechanism in COVID-19.
The Present Study
The ultimate goal of the present study was to bring awareness of the effect of social support and pandemic-related coping of university students in response to the anxiety in COVID-19 quarantine. To the best of our knowledge, previous studies did not untangle the complex associations among the above variables in the pandemic context, neither the relationship between specific social support sources and anxiety, nor the potential mediating roles of various coping strategies between specific social support sources and anxiety. Whilst most research has estimated the mediation model of coping under the construct of positive and negative coping strategies, few researchers have considered the potentiality of other competing models and probed into the intermediary role of coping between social support and anxiety under alternative constructs of coping and social support.
Accordingly, the purpose of the current study was to evaluate the relationship between social support, coping strategy, and anxiety using the sample of home-quarantined Chinese university students at the height of COVID-19. The present study sought to answer the following questions:
- Q1
- Are the three sources of social support (i.e., subjective support, family support, and counselor support) associated with anxiety among Chinese university students?
- Q2
- Do coping strategy (i.e., cognitive coping, emotional coping, and behavioral coping, respectively) mediate the association between the three sources of social support and anxiety?
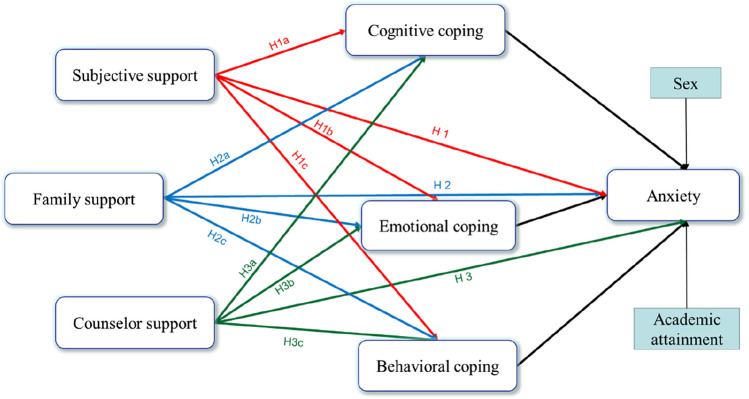
Considering previous studies and the hypothesized associations concerning social support, coping strategy, and anxiety, the following hypotheses were formed specifically:
H1
Subjective support and anxiety are significantly negatively correlated.
H1a
The relationship between subjective support and anxiety is mediated by cognitive coping.
H1b
Emotional coping has a mediating effect on the relationship between subjective support and anxiety.
H1c
Behavioral coping plays a mediating role in the relationship between subjective support and anxiety.
H2
Family support is related to anxiety significantly and negatively.
H2a
The relationship between family support and anxiety is mediated by cognitive coping.
H2b
Emotional coping has a mediating effect on the relationship between family support and anxiety.
H2c
Behavioral coping plays a mediating role in the relationship between family support and anxiety.
H3
Counselor support and anxiety are significantly negatively correlated.
H3a
The relationship between counselor support and anxiety is mediated by cognitive coping.
H3b
Emotional coping has a mediating effect on the relationship between counselor support and anxiety.
H3c
Behavioral coping plays a mediating role in the relationship between counselor support and anxiety.
The conceptual model is presented as follows (Fig. 1):
Fig. 1.
Conceptual model of the relationship between social support, coping strategy, and anxiety
Materials and methods
Participants and Procedure
This large-scale study was implemented under the context of psychological counseling service whose aim was to gauge the psychological status and initiate counseling assistance during COVID-19 quarantine. The study was approved by the Human Research Ethics Committee of City University of Macau (EA2001025). Participants include 2640 young adults (out of 2680 recruited) aged 18 to 25 from a comprehensive university in an developed economic zone in China. Adopting stratified random sampling represented in terms of students’ sex, age, and academic attainment, recruitment occurred through the school email platform during February 21st to 24th of 2020, when the students had been confined at home with their families for at least one month since the outbreak of COVID-19 in Wuhan. After granting informed consent via the guidelines at the beginning of the survey, the respondents completed three online questionnaires concerning social support, coping strategy, and anxiety anonymously. Before the formal questionnaires, students’ sociodemographic data were collected, including sex, major, academic attainment (graduate or undergraduate), current location (Hubei Province, the pandemic zone or not), self-perceived health status, and isolation condition (medically observed or not), by which it meant that residents were required to stay indoors and self-monitor their temperatures if they showed common cold symptoms.
Measures
Social Support Questionnaire (SSQ)
The Social Support Questionnaire (SSQ) derived from the Chinese version of the Social Support Rating Scale (SSRS) to evaluate the respondent’s availability of different social support sources under pandemic context (Duan et al., 2019; Xiao, 1994, 1998). The revised SSQ adopted the typologies of the SSRS, which contained subjective support and objective support originally, and categorized objective support to family support and counselor support to highlight the situational nature of social support in COVID-19 pandemic. Hence, the present SSQ was divided into three dimensions, including subjective support (items 1–2), family support (items 3–4) and counselor support (items 5–6). Subjective support evaluated the individual’s emotional experience of being supported and understood by the outer social networks, and the items were listed as “I can rely on my families and friends when I meet mental stress in the COVID-19 pandemic” and “I feel being supported by my families and friends”. Family support referred to the availability of objective support from family when individual meets mental stress and the example of item was “I talk to my families in face of mental stress in the epidemic”. Item like “I talk to my counselors in face of mental stress in the epidemic” represented the dimension of counselor support, which accessed the degree of utilization of support from counselors when individual meets mental stress. Items were rated on a 1 (“strongly disagree”) to 5 (“strongly agree”) point Likert scale, with higher scores indicating greater availability of support in the pandemic. The mean value of each dimension was viewed as the level of the corresponding social support status. In the present sample, the results of Pearson’s correlations for the subjective support (r = 0.922, p < 0.01), family support (r = 0.647, p < 0.01), and counselor support subscales (r = 0.932, p < 0.01) were satisfactory.
Coping Strategy Questionnaire (CSQ)
Given the lack of pandemic-related coping instrument, the researchers designed a COVID-19 situational coping questionnaire. Guided by the theory of psychological stress (Lazarus & Folkman, 1984), the Coping Strategy Questionnaire was framed to evaluate coping strategies against the COVID-19 pandemic, including dimensions of cognitive coping (CC; items 1–3), emotional coping (EC; items 4–6) and behavioral coping (BC; items 7–10). This 5-point Likert scale ranged from 1 (“strongly disagree”) to 5 (“strongly agree”). The subscale of emotional coping was reversely coded, with higher scoring indicating higher tendencies of utilizing appropriate emotional response. The means of the item scores were used as a measurement of the coping status. The 10 items were listed as follows:
I understand the preventive information regarding COVID-19.
I have paid close attention to the news about the COVID-19 epidemic.
I believe that the COVID-19 epidemic can be under effective control.
I am worried about being infected with COVID-19.
I am afraid that everyone could be the infected with COVID-19.
I feel unsafe even if I wear mask outside.
I wear mask when I go outside.
I have paid more attention to personal health than before.
I have cancelled outing schedules and social gathering.
I have tried to avoid going to the hospital to keep away from infection.
Factor structure was verified using principal component analyses, with a total of three factors accounting for 61.396% of the variance, and factors of CC, EC, and BC accounting for 24.540%, 18.674%, and 18.183%, respectively. This scale exhibited satisfactory validity with an index of 0.795 in the Kaiser–Meyer–Olkin test, and a significant result in the Bartlett’s test of sphericity. The fit indices of factor analysis were acceptable (χ2/df = 5.324, GFI = 0.987, CFI = 0.979, NFI = 0.975, RMSEA = 0.040, RMR = 0.018). The Cronbach’s alpha coefficient was 0.83 with 0.70, 0.67, and 0.77 of it and 0.67, 0.67, and 0.76 of omega alpha coefficient for each subscale dimension (CC, EC, BC), respectively.
Self-rating Anxiety Scale (SAS)
Participants completed the Self-rating Anxiety Scale (SAS), a 20-item questionnaire with items measured on a 4-point scale (1 = rarely, 2 = sometimes, 3 = frequently, and 4 = always) developed by Zung (1971) that assessed the anxiety level of the students. Some item examples evaluating the anxious symptoms were: “I feel more nervous and anxious than usual”; “I get upset easily or feel panicky”; “My arms and legs shake and tremble.” The aggregate score of the SAS questionnaire was computed as the sum of the 20 items multiplied by 1.25, with higher scores representing more symptoms of anxiety. The scale had been proved reliable and valid, with a Cronbach’s alpha coefficient of 0.76 in the Chinese context (Tang et al., 2010) and 0.89 in this research. According to the recommended anxiety index (Dunstan & Scott, 2020; Zung, 1980), the levels of anxiety were assessed as follows: values below 45 indicating “Anxiety within normal range”; values between 45 and 59 indicating “Mild to moderate anxiety”; values in the range of 60–74 indicating “Marked to severe anxiety”; values of 75 or above indicating “Most extreme anxiety”.
Statistical Analyses
All the analyses were computed under R environment (Version 4.0.2). First, preliminary analyses were performed to extract the reliability and descriptive statistics, consisting of the factor analysis, mean, and standard deviations of the variables under study. Next, correlation matrix among all variables was conducted in R using the “corrplot” package. Then, the hypothesized model (see Fig. 1) was examined by means of path analysis with parallel mediation using the “lavaan” package (Rosseel, 2012). In this multivariate theoretical assumptions, three sources of social support (i.e., subjective support, family support and counselor support) were used as predictors, coping strategies (i.e., cognitive coping, emotional coping, and behavioral coping) were used as mediators, and anxiety was used as outcome variable. Sex and academic attainment were included as covariates in the model. Path analysis modeling was performed using Maximum Likelihood (ML) as the estimator. For direct and indirect effects, significance was considered to be indicated by p values under 0.05. Model fit statistics included comparative fit index (CFI; 0.95 or above indicative of good fit), Tuker-Lewis index (TLI; 0.90 or above indicative of good fit), root mean square error of approximation (RMSEA; 0.05 or below indicative of good fit), and standardized root mean square residual (SRMR; 0.05 or below indicative of good fit) (Bollen, 1989; Browne & Cudeck, 1993).
Results
Descriptive Statistics and Correlations
A total of 2640 Chinese university students who were quarantined at home living with their families participated in this study with 68.79% female and 31.21% male participants (Table 1). The students surveyed were composed of graduates (14.51%) and undergraduates (85.49%), with the age ranging from 18 to 25 years, including 677 freshmen, 616 sophomores, 545 juniors, 588 seniors, 83 First-year graduate students, 69 s-year graduate students, and 62 third-year graduate students, specifically. All the participants were required to stay at home with their families at the height of the pandemic in China, and the students (0.91%) who showed common cold symptoms (i.e., runny nose, sore throat, but not headache) were demanded to be medically observed (i.e., self-monitoring of body temperature at home). The students’ current perception on health were also assessed and 98.52% of participants claimed that they were very healthy or healthy.
Table 1.
Sociodemographic and descriptive characteristics of the participants (n = 2640)
| Sociodemographic characteristics | N | % |
|---|---|---|
| Gender | ||
| Male | 824 | 31.21 |
| Female | 1816 | 68.79 |
| Academic attainment | ||
| Graduate student | 383 | 14.51 |
| Undergraduate | 2257 | 85.49 |
| Current location | ||
| Hubei Province (the epicenter) | 62 | 2.35 |
| Other provinces | 2578 | 97.65 |
| Isolation condition | ||
| Medically observed | 24 | 0.91 |
| Not medically observed | 2616 | 99.09 |
| Self-perceived health status | ||
| Very healthy | 2136 | 80.91 |
| Healthy | 465 | 17.61 |
| Not sure | 37 | 1.4 |
| Not healthy | 2 | 0.08 |
| Anxiety | ||
| Normal | 2525 | 95.64 |
| Mild to moderate | 108 | 4.09 |
| Marked to severe | 6 | 0.23 |
| Most extreme | 1 | 0 |
| Variable | Mean | SD |
|---|---|---|
| Social support | ||
| Subjective support | 4.70 | 0.52 |
| Family support | 4.62 | 0.57 |
| Counselor support | 4.44 | 0.82 |
| Coping strategy | ||
| Cognitive coping | 4.53 | 0.47 |
| Emotional coping | 2.76 | 0.87 |
| Behavioral coping | 4.76 | 0.37 |
| Anxiety | 36.25 | 4.57 |
The students showed significantly higher anxiety during the COVID-19 outbreak than the normal period (MCOVID-19 = 36.25, SDCOVID-19 = 4.57; MChinese norm = 29.78, SDChinese norm = 0.46; t = 72.815, p = 0.000) (Li et al., 2004), though anxiety levels remained in the normal range for 95.64% of students. To be specific, 108 students (4.09%) experienced mild to moderate level of anxiety, 6 students (0.23%) were identified as marked to severe level of anxiety, and only 1 student experienced most extreme level of anxiety (Table 1). Ratings of subjective support, cognitive coping, and behavioral Coping were high (MSS = 4.70, SDSS = 0.52; MCC = 4.53, SDCC = 0.47; MBC = 4.76, SDBC = 0.37), while the mean of emotional coping was comparatively low (MEC = 2.76, SDEC = 0.87) (Table 1). Correlation matrix among all variables is depicted in Fig. 2. Specifically, increased anxiety was associated with decreased subjective support (r = − 0.29, p < 0.01), family support (r = − 0.26, p < 0.01), and counselor support (r = − 0.30, p < 0.01). Anxiety was also negatively correlated with cognitive coping (r = − 0.19, p < 0.01), emotional coping (r = − 0.14, p < 0.01), and behavioral coping (r = − 0.12, p < 0.01).
Fig. 2.
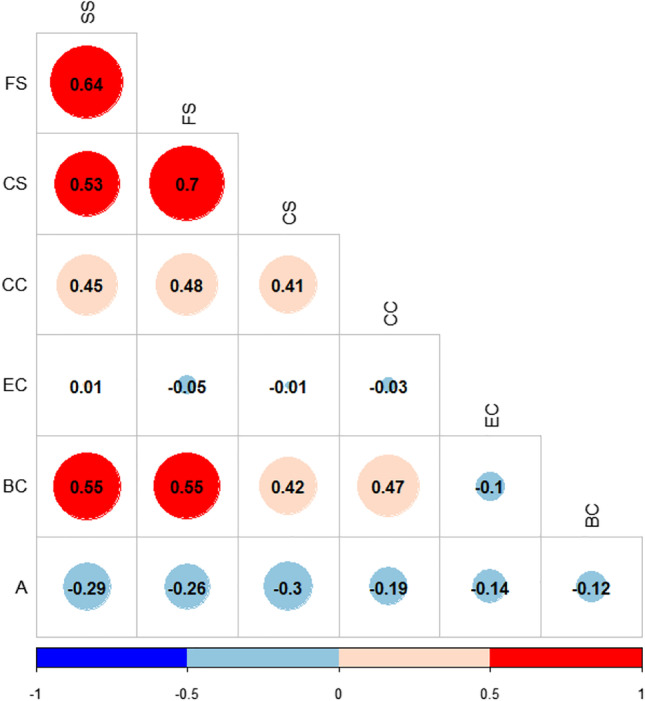
Correlation matrix among all variables. SS subjective support, FS family support, CS counselor support, CC cognitive coping, EC emotional coping, BC behavioral coping, A anxiety. Matrix was created in R using the “corrplot” package
Hypothesis Testing
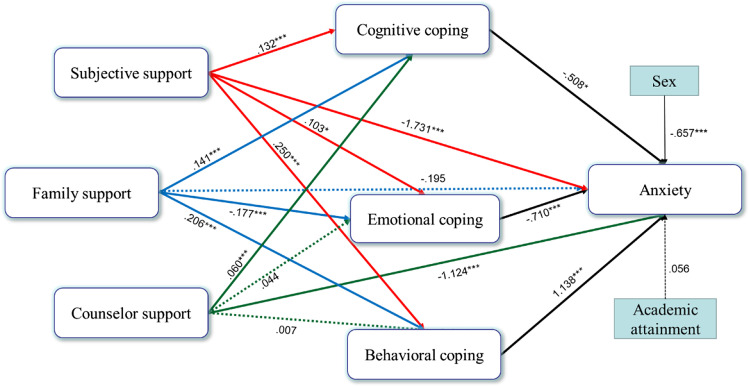
The path analysis model was conducted to measure the associations of social support, coping and anxiety among home-quarantined students. Sex and academic attainment were entered as covariates in the model to control for the potential effect of predictors in the analyses. Overall fitness of the path model was acceptable (χ2(8) = 73.284, p < 0.01; RMSEA = 0.056; CFI = 0.976; TLI = 0.921; SRMR = 0.020). Standardized regression coefficients of the hypothesized model are depicted in Fig. 3, and Table 2 demonstrates the mediation results.
Fig. 3.
Path analysis model depicting the relationship between social suppor, coping strategy, and anxiety. All the coefficients are standardized; dashed lines indicate the insignificant path effect; *p < .05, **p < .01, ***p < .001
Table 2.
The mediation analysis of coping in the relationship between social support and anxiety
| Pathway1 | Β | SE | P | Conclusion |
|---|---|---|---|---|
| Direct effect | ||||
| Subjective support → Anxiety | − 1.731 | .223 | .000 | |
| Indirect effect | ||||
| Subjective support → Cognitive coping → Anxiety | − .067 | .030 | .024 | Partial |
| Subjective support → Emotional coping → Anxiety | − .073 | .032 | .023 | Partial |
| Subjective support → Behavioral coping → Anxiety | .284 | .073 | .000 | Partial |
| Pathway2 | Β | SE | P | Conclusion |
|---|---|---|---|---|
| Direct effect | ||||
| Family support → Anxiety | − .195 | .236 | .408 | |
| Indirect effect | ||||
| Family support → Cognitive coping → Anxiety | − .072 | .032 | .024 | Full |
| Family support → Emotional coping → Anxiety | .126 | .037 | .001 | Full |
| Family support → Behavioral coping → Anxiety | .234 | .061 | .000 | Full |
| Pathway3 | Β | SE | P | Conclusion |
|---|---|---|---|---|
| Direct effect | ||||
| Counselor support → Anxiety | − 1.124 | .142 | .000 | |
| Indirect effect | ||||
| Counselor support → Cognitive coping → Anxiety | − .030 | .014 | .033 | Partial |
| Counselor support → Emotional coping → Anxiety | − .031 | .021 | .136 | Na |
| Counselor support → Behavioral coping → Anxiety | .008 | .011 | .500 | Na |
N = 2640. Pathway1 is from the subjective support model, Pathway2 is from the family support model, and Pathway3 is from the counselor support model
As can be seen in Fig. 3, higher subjective support (β = − 1.731, p = 0.000) and counselor support (β = − 1.124, p = 0.000) were significantly associated with lower anxiety, providing support for H1 and H3, while higher family support was not significantly associated with lower anxiety (β = − 0.195, p = 0.408), which did not support H2. The largest standardized regression coefficient was from subjective support to anxiety (β = − 1.731), suggesting that increases in subjective support by one standard deviation decreased anxiety by almost two standard deviations.
In the mediation Pathway1 from subjective support to anxiety, subjective support was positively related to cognitive coping (β = 0.132, p = 0.000), which in turn was negatively related to anxiety (β = − 0.508, p = 0.016); subjective support disposed greater use of emotional coping (β = 0.103, p = 0.017) and lower anxiety (β = − 0.710, p = 0.000); subjective support was also positively related to behavioral coping (β = 0.250, p = 0.000), which in turn was positively related to anxiety (β = 1.138, p = 0.000). Higher subjective support was associated with lower anxiety (β = − 1.731, p = 0.000), and this effect was partially mediated through cognitive coping (indirect effect β = − 0.067, p = 0.024), emotional coping (indirect effect β = − 0.073, p = 0.023), and behavioral coping (indirect effect β = 0.284, p = 0.000). Therefore, cognitive coping, emotional coping and behavioral coping acted as partial mediators of the relationship between subjective support and anxiety, which supported H1a, H1b, and H1c, and the largest indirect effect of behavioral coping indicated that behavioral coping had the largest meditating effect between subjective support and anxiety.
In Pathway2 from family support to anxiety, family support increased cognitive coping (β = 0.141, p = 0.000) and behavioral coping (β = 0.206, p = 0.000), and decreased emotional coping (β = − 0.177, p = 0.000). Given that the direct effect of family support on anxiety in the model was nonsignificant (β = − 0.195, p = 0.408), cognitive coping, emotional coping and behavioral coping fully significantly mediated the relationship between family support and anxiety (magnitude of indirect effect: βCC = − 0.072, p = 0.024; βEC = 0.126, p = 0.001; βBC = 0.234, p = 0.000). This result provided support for H2a, H2b, and H2c.
In Pathway3 from counselor support to anxiety, counselor support increased cognitive coping (β = 0.060, p = 0.000), but the effect of counselor support on the emotional coping (β = 0.044, p = 0.128) and behavioral coping (β = 0.007, p = 0.494) were not significant. Higher counselor support was also significantly associated with lower anxiety (β = − 1.124, p = 0.000), and this effect was significant when adding cognitive coping (magnitude of indirect effect: β = − 0.030, p = 0.033), but not significant when adjusting for scores on emotional coping (magnitude of indirect effect: β = − 0.031, p = 0.136) and behavioral coping (magnitude of indirect effect: β = 0.008, p = 0.500). This result suggested that cognitive coping partially significantly mediated the effect of counselor support on anxiety, supporting H3a, while there was no significant mediation effect observed in emotional coping and behavioral coping, which did not support H3b and H3c.
Discussion
The foremost intention of the present study was to clarify the associations between social support, coping strategies, and anxiety. In response to the first research question, subjective support, and counselor support were significantly and negatively associated with anxiety, while family support did not demonstrate substantive associations with anxiety. Regarding the second research question, the further mediation analysis found mediating effects of cognitive coping, emotional coping, and behavioral coping respectively on the relationship between subjective support, family support, and anxiety, while cognitive coping, but not emotional coping and behavioral coping, played a partial intermediary role in the relationship between counselor support and anxiety.
First, the current study indicated that the level of anxiety during the COVID-19 outbreak was higher than the normal period before the pandemic. However, it was much lower than the Chinese medical staff (36.25 ± 4.57 vs 46.1 ± 10.4) (Zhu et al., 2020). In the same vein, the anxiety level of the college students was lower than the suspected infectious cases who were required to be self-isolated at home in the Chinese epicenter (Xiao et al., 2020). These differences could be attributed to the distinctions in the residence of the respondents, confirming a previous finding that the psychological symptoms of individuals working in the epicenter were higher than those working outside the epicenter (Lai et al., 2020). The current study found that 4.09% of the students experienced mild to moderate level of anxiety, with 0.27% having severe to extreme levels. Comparing to the COVID-related studies using the Zung self-rating anxiety scale, 35% of the students in Saudi Arabia experienced moderate to extreme levels of anxiety (Khoshaim et al., 2020), while 25.3% of the students in Pakistan exhibited mild to moderate level of anxiety (Baloch et al., 2021). Looking at students in China, Cao et al. (2020) argued approximate 24% of college medical students experienced mild to moderate level of anxiety, with 0.9% having severe anxiety during the COVID-19 outbreak. In contrast, a study during the lockdown reported a much higher anxiety level (34% for severe anxiety and 28.5% for mild to moderate anxiety) among Spanish students (Diaz-Jimenez et al., 2020). Likewise, 66.1% of the American counterparts revealed mild to severe anxiety (Guo et al., 2021). These findings indicated that the levels of anxiety among university students, regardless of nation and major, were affected during the confinement. The main reason for the comparative low levels of anxiety of Chinese students could be the timely reactions of Chinese government to restrict the spread of COVID-19 which controlled the fatal influence of the pandemic.
As a response to H1, H1a, H1b, and H1c, subjective support had a negative direct and indirect impacts on anxiety. Consistent with H1, the finding of a strong negative effect of subjective support on anxiety in the direct path did not mirror the path analysis on sample of Indonesian students which revealed that greater perceived satisfactory support explained higher levels of anxiety (Pramukti et al., 2020). The considerably difference in the result may be attributed to the cultural variety. Further, cognitive coping, family coping, and behavioral coping were partial mediators between subjective support and anxiety, which indicated that other potential mediating variables existed in the path through subjective support and anxiety. In addition, this finding supported the position that subjective support can be understood as an overarching coping style distinguished from established conceptualizations of coping (Dawson & Golijani-Moghaddam, 2020). The finding of Thai students, stating that the lack of resource (including sufficiency of psychological support) and the low confidence in pandemic control may explain the high level of anxiety, could possibly explain the mediating role of cognitive coping between subjective support and anxiety (Pramukti et al., 2020). This finding suggested that cognitive coping strengthened the positive effect of subjective support on anxiety. In the first half of the path, subjective support functioned as the positive predictor of all the three coping strategies, indicating that individuals who experienced more subjective support tended to utilize more cognitive coping, emotional coping, and behavioral coping.
Considering H2, H2a, H2b, and H2c, family support had an indirect effect on anxiety, but not a direct effect. The unexpected finding of the insignificant effect of family support on anxiety contradicted many early studies emphasizing the prevailing role of family support on anxiety. A study of Spanish student majoring in social work argued that higher perceived social support from families significantly reduced the moderate to severe levels of anxiety symptoms during the COVID-19 lockdown (Diaz-Jimenez et al., 2020). In parallel, living with parents was found to be a favorable factor for decreasing anxiety among university students in Bangladesh (Dhar et al., 2020). On the contrary, Thai students reported that receiving more information from family significantly explained higher levels of anxiety (Pramukti et al., 2020). Specifically in the indirect path, cognitive coping, emotional coping, and behavioral coping were full mediators between family support and anxiety. Their full mediating roles suggested that living with families was possibly not a significant factor to reduce anxiety, but only by applying proper coping strategies can the conductive effect of family support be stimulated, which subsequently abated anxiety. In the first half of the path, family support was significantly positively associated with cognitive coping and behavioral coping. Interestingly, this study found family support was negatively related to emotional coping which denoted moderate emotional reactions towards the pandemic threat. In other words, the more family support individuals received, the greater excessive emotional response, such as worries and fear, they might reveal. This can be interpreted that sharing pandemic information repeatedly in a small social network, such as the family may result in increased anxiety (Pramukti et al., 2020). Further, the echo chamber effects may amplify the dissemination of information, wherein individuals with close relationship showed more trust in the information shared (Chou et al. 2018). Thus, the extreme information shared within families may subsequently lead to excessive emotional response.
Regarding H3, H3a, H3b, and H3c, counselor support significantly negatively predicted anxiety, with an indirect effect through cognitive coping. A systematic review of mobile app-based college counseling services found preliminary evidence of efficacy of cognitive behavioral therapy on anxiety (Oliveira et al., 2021). Similarly, an Italian study of 53 subjects verified the versatility and usefulness of a single online counseling session in reducing state anxiety during the lockdown (Carbone et al., 2021). These findings are in line with the effect of counselor support on anxiety found in the present study. Support from online counselor or social media group should be advocated to alleviate the anxiety of the students (Feng et al., 2021). The indirect effects of counselor support on anxiety were significant through cognitive coping, which supported H3a, indicating that counseling interventions that enhanced cognitive coping may therefore mitigate anxiety. Moreover, the finding that the mediating impact of emotional coping and behavioral coping did not exist in counselor support and anxiety, which contradicted H3b and H3c, could be interpreted in light of the fact that emotional coping and behavioral coping did not play a dominant role in the mechanism between counselor support and anxiety. There may be other potential intermediating variables to be identified in the future study. The partial mediating role of cognitive coping between counselor support and anxiety may be explained by the characteristics of the existing counseling approach. Most interventions are delivered via verbal means and thus the pandemic-related cognitive appraise of the students may be effectively changed, while less impact can be expected on the emotional and behavioral components of coping, giving a partial explanation of why emotional and behavioral coping did not mediate the effect of counselor support on anxiety. Hence, interventions other than cognitive approach may be taken into consideration. Given the variety of the students’ demographic background, school counselors should avail themselves of the optimal interventions to empower students. At this point, technique such as dialectical behavior therapy (DDT) which involves more mindfulness self-regulation or emotion regulation may be more suitable for adolescents (Karaman et al., 2021).
In the second half of the mediation path, cognitive coping and emotional coping were found to be conductive to reducing anxiety, while behavioral coping had a large positive association with anxiety. As for the impact of cognitive coping on anxiety, it is reasonable that the more students kept in pace with the relevant psychological and physical information from medias, the more comprehensions they acquired about the pandemic, which in turn buffered the anxious symptoms. The finding that cognitive coping was moderately and negatively correlated with the level of anxiety also concurs with the findings from a Chinese survey stating that regular updating the latest information about the pandemic was significantly associated with lower anxiety score (Wang et al., 2020a). This might be explained by the perception that more availability of the information may enhance individuals’ confidence in fighting against COVID-19 which has been found to be associated with more adaptive psychological responses in face of the pandemic (Li et al., 2020a, 2020b; Lin & Cheng, 2020). However, this finding was not similar to that of another study on the Thai students, which found that higher anxiety levels were highly affected by receiving COVID-19 information from the internet (Pramukti et al., 2020). This different result may be resulted from the accuracy and quality of the pandemic-related information. For instance, a study on a sample of Iranian students found that the use of problematic social media was significantly positively associated with psychological distress regarding anxiety and depression (Lin et al., 2020). Hence, one cognitive coping to decrease anxiety was to seek accurate information, but not to constantly update the latest information regardless of the quality. Additionally, emotional coping which indicated adaptive and moderate COVID-19 specific emotional reactions was found to be negatively associated with anxiety in the current study. This is consistent with the previous findings that fear of infection and COVID-19 related worry were prone to result in anxiety in the pandemic (Dhar et al., 2020; Teshome et al., 2020). An interesting result to emerge from this study was that behavioral coping was highly positively associated with higher levels of anxiety, which is inconsistent with most of the earlier studies. To our common knowledge, appropriate implementation of precaution measures, such as washing hands immediately after coughing, avoiding the sharing of utensils, high frequency of wearing masks regardless of the presence or absence of symptoms, predicted lower scores in anxiety (Wang et al., 2020a). In contrast, a study on Australian undergraduate paramedicine students found a positive and significant correlation between behavioural disengagement and anxiety (Brett et al., 2021). While the proactive behaviors are reckoned to positively impact mental health, the potential destructive impact of maladaptive coping behaviors such as disengagement and excessive engagement might be overlooked. Given that appropriate engagement in preventive behaviors is recommended, the curvilinear association of behavioral coping with anxiety leaves room for future research.
Limitations
However, there are some limitations in the present study. First, the generalizability of the findings is restricted in the consideration that students in China tend to be more disciplined regarding to the restrictive measures decreed by the authorities, so more diverse samples, especially Western populations, should be investigated concerning these relationships. Second, since the cross-sectional study has the limitation of providing the causal relationships among variables, more relative longitudinal studies are needed to confirm the associations in between. Nevertheless, this short interval study, which was conducted shortly after the COVID-19 outbreak, was reckoned to be the optimal method by the authors in order to reflect the immediate psychological response of the students. Going forward, evidence from Chinese quarantined students showed that the prevalence of anxiety raised from 19% in February 2020 to 36.7% in April 2020 (Chen et al., 2021), suggesting the needs for longitudinal further testing of these relationships over time. Third, the current measures were designed to apply to the novel situation of the pandemic and more research is needed to refine measures of this sort. For example, to disentangle the contribution of emotional reactions and emotion regulation strategies in emotional coping. Finally, the general biases of the self-report method, such as social desirability and perfunctory reports, could influence the veracity of the result.
Conclusion
This study proposed a model to investigate the relationships of social support, coping strategy, and anxiety of university students who were quarantined at home for more than one month in the peak of the COVID-19 pandemic in China from January to February 2020, exploring the mediating roles of coping strategies between various social support sources and anxiety particularly. These findings provided new perspectives for social support and coping strategies on alleviating anxiety in the COVID-19 pandemic.
This empirical study will shed light on the mental support of the current global crisis for two core reasons. First, this study detected the facilitating effect of subjective support and counselor support on decreasing anxiety in quarantine. Second, the specific mediating power of cognitive coping, emotional coping, and behavioral coping between social support (especially for subjective support and family support) and anxiety should arouse attention of the students and school administrators in the lockdown period. Given the insights detected from this study, it is recommended to provide students with COVID-19-specific social support and detailed advice on how to cope with emergency, and thus manage anxiety in the quarantine.
Acknowledgements
The authors appreciate the study participants and the funders of this project.
Author Contributions
YL conducted the conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, validation, wrote and revised the manuscript; JP administered, supervised the project, reviewed and revised the manuscript; YQT analyzed the data in the revised version. All authors have read and approved the final version of the manuscript.
Funding
This study was funded by the key project of Physical and Psychological Health and Artistic Expression Studio, and mental health education projects, launched by Shenzhen University (Grant Number 19XSZ03; 21MSZX08; Y20210607). Also, it was supported by the Higher Education Fund of the Macao SAR Government (OTH-2002-03). The views expressed in this article are those of the authors and do not necessarily reflect the position of the funders.
Data Availability
The data that support the findings of this study has been deposited to dryad and the doi is available from the corresponding author on reasonable request (may require data use agreements to be developed).
Declarations
Conflict of Interest
The authors have no potential conflicts of interest to disclose.
Ethical Approval
This study was granted ethics approval by the Human Research Ethics Committee of City University of Macau (EA2001025). All the respondents granted permission for inclusion by reading the introductions for the investigation and provided voluntary response.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ao Y, Zhu H, Meng F, Wang Y, Ye G, Yang L, Dong N, Martek I. The impact of social support on public anxiety amidst the COVID-19 pandemic in China. International Journal of Environmental Research and Public Health. 2020 doi: 10.3390/ijerph17239097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baloch GM, Kamaludin K, Chinna K, Sundarasen S, Nurunnabi M, Khoshaim HB, Hossain SFA, Sukayt AA, Baloch LG. Coping with COVID-19: The strategies adapted by Pakistani students to overcome implications. International Journal of Environmental Research and Public Health. 2021 doi: 10.3390/ijerph18041799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belhaj M, Kebair F, Ben Said L. Modeling and simulation of coping mechanisms and emotional behavior during emergency situations. In: Jezic G, Chen-Burger YH, Howlett R, Jain L, editors. Agent and multi-agent systems: Technology and applications. Smart innovation systems and technologies. Cham: Springer; 2016. [Google Scholar]
- Bollen KA. Structural equations with latent variables. Wiley; 1989. [Google Scholar]
- Bourion-Bedes S, Tarquinio C, Batt M, Tarquinio P, Lebreuilly R, Sorsana C, Legrand K, Rousseau H, Baumann C. Psychological impact of the COVID-19 outbreak on students in a French region severely affected by the disease: Results of the PIMS-CoV 19 study. Psychiatry Research. 2021;295:113559. doi: 10.1016/j.psychres.2020.113559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett W, King C, Shannon B, Gosling C. Impact of COVID-19 on paramedicine students: A mixed methods study. International Emergency Nursing. 2021;56:100996. doi: 10.1016/j.ienj.2021.100996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; 1993. pp. 136–162. [Google Scholar]
- Bruffaerts R, Mortier P, Kiekens G, Auerbach RP, Cuijpers P, Demyttenaere K, Green JG, Nock MK, Kessler RC. Mental health problems in college freshmen: Prevalence and academic functioning. Journal of Affective Disorders. 2018;225:97–103. doi: 10.1016/j.jad.2017.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabanach RG, Souto-Gestal A, González L, Souto S. Efectos diferenciales de la atención y la claridad emocional sobre la percepción de estresores académicos y las respuestas de estrés de estudiantes de fisioterapia [Differential effects of attention and emotional clarity on the perception of academic stressors and stress response in physiotherapy students] Fisioterapia. 2016;38:271–279. doi: 10.1016/j.ft.2015.11.003. [DOI] [Google Scholar]
- Cai Z, Zheng S, Huang Y, Zhang X, Qiu Z, Huang A, Wu K. Emotional and cognitive responses and behavioral coping of Chinese medical workers and general population during the pandemic of COVID-19. International Journal of Environmental Research and Public Health. 2020 doi: 10.3390/ijerph17176198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbone GA, Zarfati A, Nicoli MS, Paulis A, Tourjansky G, Valenti G, Valenti EM, Massullo C, Farina B, Imperatori C. Online psychological counselling during lockdown reduces anxiety symptoms and negative affect: Insights from Italian framework. Clinical Psychology Psychotherapy. 2021 doi: 10.1002/cpp.2608. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–287. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Chao SF. Social support, coping strategies and their correlations with older adults’ relocation adjustments after natural disaster. Geriatrics & Gerontology International. 2017;17(6):1006–1014. doi: 10.1111/ggi.12807. [DOI] [PubMed] [Google Scholar]
- Chen X, Qi H, Liu R, Feng Y, Li W, Xiang M, Xiang YT. Depression, anxiety and associated factors among Chinese adolescents during the COVID-19 outbreak: A comparison of two cross-sectional studies. Translational Psychiatry. 2021;11(1):148. doi: 10.1038/s41398-021-01271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou WS, Oh A, Klein WMP. Addressing health-related misinformation on social media. JAMA. 2018;320(23):2417–2418. doi: 10.1001/jama.2018.16865. [DOI] [PubMed] [Google Scholar]
- Chwaszcz J, Palacz-Chrisidis A, Wiechetek M, Bartczuk RP, Niewiadomska I, Wosko P, Slawska-Jaroszewska P. The quality of life, resources, and coping during the first weeks of the COVID19 pandemic in people seeking psychological counselling before the pandemic. International Journal of Occupational Medicine and Environmental Health. 2021;34(2):275–287. doi: 10.13075/ijomeh.1896.01700. [DOI] [PubMed] [Google Scholar]
- Cohen, S., & Hoberman, H. M. (1983). Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology, 13(2), 99–125. 10.1111/j.1559-1816.1983.tb02325.x
- COVID-19 Situation in WHO. World Health Organization—Western Pacific. URL: https://experience.arcgis.com/experience/e1a2a65fe0ef4b5ea621b232c23618d5 [Accessed July 30, 2021]
- Cypryanska M, Nezlek JB. Anxiety as a mediator of relationships between perceptions of the threat of covid-19 and coping behaviors during the onset of the pandemic in poland. PLoS ONE. 2020;15(10):e0241464. doi: 10.1371/journal.pone.0241464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DL, Golijani-Moghaddam N. COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science. 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhar BK, Ayittey FK, Sarkar SM. Impact of COVID-19 on psychology among the university students. Global Challenges. 2020 doi: 10.1002/gch2.202000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Jimenez RMPD, Caravaca-Sanchez FPD, Martin-Cano MCPD, De la Fuente-Robles YMPD. Anxiety levels among social work students during the COVID-19 lockdown in Spain. Social Work in Health Care. 2020;59(9–10):681–693. doi: 10.1080/00981389.2020.1859044. [DOI] [PubMed] [Google Scholar]
- Duan X, Ni X, Shi L, Zhang L, Ye Y, Mu H, Li Z, Liu X, Fan L, Wang Y. The impact of workplace violence on job satisfaction, job burnout, and turnover intention: The mediating role of social support. Health and Quality of Life Outcomes. 2019;17(1):93–93. doi: 10.1186/s12955-019-1164-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20(1):90. doi: 10.1186/s12888-019-2427-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng S, Zhang Q, Ho SMY. Fear and anxiety about COVID-19 among local and overseas Chinese university students. Health & Social Care in the Community. 2021 doi: 10.1111/hsc.13347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN, McInroy LB, Paceley MS, Williams ND, Henderson S, Levine DS, Edsall RN. “I’m kinda stuck at home with unsupportive parents right now”: LGBTQ youths' experiences with COVID-19 and the importance of online support. Journal of Adolescent Health. 2020;67(3):450–452. doi: 10.1016/j.jadohealth.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey AM, Garcia IJ, Otal Franco SH, Fernandez CM. The psychological impact of strict and prolonged confinement on business students during the COVID-19 pandemic at a Spanish university. International Journal of Environmental Research and Public Health. 2021 doi: 10.3390/ijerph18041710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo AA, Crum MA, Fowler LA. Assessing the psychological impacts of COVID-19 in undergraduate medical students. International Journal of Environmental Research and Public Health. 2021 doi: 10.3390/ijerph18062952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L, Lei W, Xu F, Liu H, Yu L. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: A comparative study. PLoS ONE. 2020;15(8):e0237303. doi: 10.1371/journal.pone.0237303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankowska-Polanska B, Polanski J, Chabowski M, Rosinczuk J, Mazur G. Influence of coping strategy on perception of anxiety and depression in patients with non-small cell lung cancer. Advances in Experimental Medicine and Biology. 2020;1251:57–70. doi: 10.1007/5584_2019_448. [DOI] [PubMed] [Google Scholar]
- Karaman MA, Esici H, Tomar IH, Aliyev R. COVID-19: Are School counseling services ready? Students’ psychological symptoms, school counselors’ views, and solutions. Frontiers in Psychology. 2021;12:647740. doi: 10.3389/fpsyg.2021.647740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karasmanaki E, Tsantopoulos G. Impacts of social distancing during COVID-19 pandemic on the daily life of forestry students. Child and Youth Service Review. 2021;120:105781. doi: 10.1016/j.childyouth.2020.105781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam S. Understanding experiences of social support as coping resources among immigrant and refugee women with postpartum depression: An integrative literature review. Issues in Mental Health Nursing. 2019;40:999–1011. doi: 10.1080/01612840.2019.1585493. [DOI] [PubMed] [Google Scholar]
- Khoshaim HB, Al-Sukayt A, Chinna K, Nurunnabi M, Sundarasen S, Kamaludin K, Baloch GM, Hossain SFA. Anxiety level of university students during COVID-19 in Saudi Arabia. Frontiers in Psychology. 2020;11:579750. doi: 10.3389/fpsyt.2020.579750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Shim Y, Choi I, Choi E. The role of coping strategies in maintaining well-being during the COVID-19 outbreak in South Korea. Social Psychological and Personality Science. 2021 doi: 10.1177/1948550621990595. [DOI] [Google Scholar]
- Labadi B, Arato N, Budai T, Inhof O, Stecina DT, Sik A, Zsido AN. Psychological well-being and coping strategies of elderly people during the COVID-19 pandemic in Hungary. Aging & Mental Health. 2021 doi: 10.1080/13607863.2021.1902469. [DOI] [PubMed] [Google Scholar]
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RSH. An emotion and a vital coping resource against despair. Social Research. 1999;66:653–678. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; 1984. [Google Scholar]
- Li DJ, Ko NY, Chang YP, Yen CF, Chen YL. Mediating effects of risk perception on association between social support and coping with COVID-19: An online survey. International Journal of Environmental Research and Public Health. 2021 doi: 10.3390/ijerph18041550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D, Ko N, Chen Y, Wang P, Chang Y, Yen C. Confidence in coping with COVID-19 and its related factors among the public in Taiwan. Psychiatry and Clinical Neurosciences. 2020;74(11):608–610. doi: 10.1111/pcn.13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D, Zou L, Zhang Z, Zhang P, Zhang J, Fu W, Mao J, Cao S. The psychological effect of COVID-19 on home-quarantined nursing students in China. Frontiers in Psychiatry. 2021;12:652296. doi: 10.3389/fpsyt.2021.652296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: A study on active Weibo users. International Journal of Environmental Research and Public Health. 2020 doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li XL, LiZhang XLL. Stress of SARS and psychological health: An investigation of response to SARS stress and anxiety level of nurse students in SARS prevalence period. Journal of West China Medical. 2004;19:596–598. [Google Scholar]
- Lin CY, Brostrom A, Griffiths MD, Pakpour AH. Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interventions—the Application of Information Technology in Mental and Behavioural Health. 2020;21:100345. doi: 10.1016/j.invent.2020.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin M, Cheng Y. Policy actions to alleviate psychosocial impacts of COVID-19 pandemic: Experiences from Taiwan. Social Health Behavior. 2020;3(2):72. doi: 10.4103/shb.shb_18_20. [DOI] [Google Scholar]
- Mai Y, Wu YJ, Huang Y. What type of social support is important for student resilience during COVID-19? A latent profile analysis. Frontiers in Psychology. 2021;12:646145. doi: 10.3389/fpsyg.2021.646145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mautong H, Gallardo-Rumbea JA, Alvarado-Villa GE, Fernandez-Cadena JC, Andrade-Molina D, Orellana-Roman CE, Cherrez-Ojeda I. Assessment of depression, anxiety and stress levels in the Ecuadorian general population during social isolation due to the COVID-19 outbreak: A cross-sectional study. BMC Psychiatry. 2021;21(1):212. doi: 10.1186/s12888-021-03214-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales-Rodriguez FM, Perez-Marmol JM. The role of anxiety, coping strategies, and emotional intelligence on general perceived self-efficacy in university students. Frontiers in Psychology. 2019;10:1689. doi: 10.3389/fpsyg.2019.01689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira C, Pereira A, Vagos P, Nobrega C, Goncalves J, Afonso B. Effectiveness of mobile App-based psychological interventions for college students: A systematic review of the literature. Frontiers in Psychology. 2021;12:647606. doi: 10.3389/fpsyg.2021.647606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL, Russell BS, Fendrich M, Finkelstein-Fox L, Hutchison M, Becker J. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. Journal of General Internal Medicine. 2020 doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pramukti I, Strong C, Sitthimongkol Y, Setiawan A, Pandin MGR, Yen CF, Lin C-Y, Griffiths MD, Ko NY. Anxiety and suicidal thoughts during the COVID-19 pandemic: Cross-country comparative study among Indonesian, Taiwanese, and Thai university students. Journal of Medical Internet Research. 2020;22(12):e24487. doi: 10.2196/24487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roseman, I. J. (2013). Appraisal in the emotion system: coherence in strategies for coping. Emotion Review, 5(2), 141–149. 10.1177/1754073912469591
- Rosseel Y. Lavaan: An R package for structural equation modeling and more Version 0.5–12 (BETA) Journal of Statistical Software. 2012;48:37. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research. 2020;22(9):e21279. doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, Zhao X, Zou Y, Hu Y, Luo X, Zhang Z, Lai A, Ho R, Tran B, Ho C, Tam W. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang J, Yu Y, Du Y, Ma Y, Zhu H, Liu Z. Association between actual weight status, perceived weight and depressive, anxious symptoms in chinese adolescents: a cross-sectional study. BMC Public Health. 2010;10(1):1–8. doi: 10.1186/1471-2458-10-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing; 2019. [Google Scholar]
- Teshome A, Glagn M, Shegaze M, Tekabe B, Getie A, Assefa G, Getahun D, Kanko T, Getachew T, Yenesew N, Temtmie Z, Tolosie K. Generalized anxiety disorder and its associated factors among health care workers fighting COVID-19 in Southern Ethiopia. Psychology Research and Behavior Management. 2020;13:907–917. doi: 10.2147/PRBM.S282822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during covid-19 pandemic: A global cross-sectional survey. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2020;109:110236. doi: 10.1016/j.pnpbp.2020.110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigouroux SL, Goncalves A, Charbonnier E. The psychological vulnerability of French university students to the covid-19 confinement. Health Education & Behavior. 2021;48(2):123–131. doi: 10.1177/1090198120987128. [DOI] [PubMed] [Google Scholar]
- Vinothkumar M, Arathi A, Joseph M, Nayana P, Jishma EJ, Sahana U. Coping, perceived stress, and job satisfaction among medical interns: The mediating effect of mindfulness. Industrial Psychiatry Journal. 2016;25(2):195–201. doi: 10.4103/ipj.ipj_98_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17:1–25. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945–947. doi: 10.1016/s0140-6736(20)30547-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the Coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Medical Science Monitor. 2020;26:e923921. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao S. Theory and application research on social support rate scale. Journal of Clinic Psychiatry. 1994;4(2):98–100. [Google Scholar]
- Xiao S. Psychological health scale: Social support questionnaire. Beijing: The Journal of Chinese Psychological Press; 1998. [Google Scholar]
- Yalcin I, Can N, Mance Calisir O, Yalcin S, Colak B. Latent profile analysis of COVID-19 fear, depression, anxiety, stress, mindfulness, and resilience. Current Psychology. 2021 doi: 10.1007/s12144-021-01667-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildirim M, Akgul O, Gecer E. The effect of COVID-19 anxiety on general health: The role of COVID-19 coping. International Journal of Mental Health Addiction. 2021 doi: 10.1007/s11469-020-00429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin Y, Yang X, Gao L, Zhang S, Qi M, Zhang L, Tan Y, Chen J. The association between social support, COVID-19 exposure, and medical students' mental health. Frontiers in Psychiatry. 2021;12:555893. doi: 10.3389/fpsyt.2021.555893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue XG, Shao XF, Li RYM, Crabbe MJC, Mi L, Hu S, Baker JS, Liang G. Risk management analysis for Novel Coronavirus in Wuhan, China. Journal of Risk Financial Management. 2020;13:22. doi: 10.3390/jrfm13020022. [DOI] [Google Scholar]
- Zhou J, Yang Y, Qiu X, Yang X, Pan H, Ban B, Qiao Z, Wang L, Wang W. Relationship between anxiety and burnout among Chinese physicians: A moderated mediation model. PLoS ONE. 2016;11(8):e0157013. doi: 10.1371/journal.pone.0157013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu W, Wei Y, Meng X, Li J. The mediation effects of coping style on the relationship between social support and anxiety in Chinese medical staff during COVID-19. BMC Health Services Research. 2020;20(1):1007. doi: 10.1186/s12913-020-05871-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zung WW. A rating instrument for anxiety disorders. Psychosom. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- Zung WWK. How normal is anxiety? Current concepts. Durham: Upjohn; 1980. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study has been deposited to dryad and the doi is available from the corresponding author on reasonable request (may require data use agreements to be developed).