Abstract
Background
The COVID-19 pandemic has had a detrimental effect on the mental health of older adults living in nursing homes. Very few studies have examined the effects of Internet-based Cognitive Behavioral Therapy (ICBT) on older adults living in nursing homes during the pandemic. We conducted a feasibility study using a single-group design, to explore the effectiveness of ICBT on psychological distress in 137 older adults (without cognitive impairment) from 8 nursing homes in 4 southeast cities in China, between January and March 2020.
Methods
Symptoms of depression, anxiety, general psychological distress, and functional disability were measured at baseline, post-treatment (5 weeks) and at a 1-month follow-up. Mixed-effects model was used to assess the effects of ICBT.
Results
Statistically significant changes with large effect sizes were observed from pre- to post-treatment on the PHQ-9 (p < .001, Cohen's d = 1.74), GAD-7 (p < .001, d = 1.71), GDS (p < .001, d = 1.30), K-10 (p < .001, d = 1.93), and SDS (p < .001, d = 2.03). Furthermore, improvements in treatment outcomes were sustained at 1-month follow-up, and high levels of adherence and satisfaction were indicated.
Conclusion
ICBT was effective in reducing psychological distress in older adults without cognitive impairments living in nursing homes during the COVID-19 pandemic. Thus, it could be applied in improving the mental health of this vulnerable group during the pandemic.
Keywords: COVID-19, Internet-based cognitive behavioral therapy, Older adults, Psychological distress, Mental health, Feasibility study
Abbreviations: ICBT, Internet-based cognitive behavioral therapy; CBT, cognitive behavioral therapy; PHQ-9, Patient Health Questionnaire 9-item; GAD-7, Generalized Anxiety Disorder 7-item; DSM-IV, The Diagnostic and Statistical Manual of Mental Disorders-4th edition; GDS, Geriatric Depression Scale; K-10, 10-item Kessler Psychological Distress Scale; SDS, Sheehan Disability Scales; ITT, intention-to-treat; MMRM, mixed-effects model for repeated measure; LOCF, last observation carried forward; REML, restricted maximum likelihood; UN, unstructured; RCT, randomized controlled trials; SD, standard deviation; CIs, confidence intervals
Highlights
-
•
ICBT is effective in improving mental health in older adults without cognitive impairments in nursing homes during COVID-19
-
•
Results show improvement in symptoms of depression, anxiety, general psychological distress, and functional disability
-
•
Improvements in treatment outcomes were sustained at 1-month follow-up
-
•
Results reveal a low rate of attrition (17.32%), high adherence (87.4%) and high satisfaction (more than 80%) post-treatment.
-
•
Results highlight the potential of ICBT in improving access to online psychotherapy of isolated older adults during COVID-19
1. Introduction
The COVID-19 outbreak, which first emerged in Wuhan, China, and then rapidly spread worldwide, is the most widespread pandemic to have afflicted humanity in a century. Age remains a risk factor for mortality in patients with COVID-19 (Li et al., 2020; Rothan and Byrareddy, 2020). Hence, evidence for the pandemic's detrimental effect on the mental health of older adults is mounting (Livingston et al., 2020; Van Tilburg et al., 2020; Zhao et al., 2020). In addition, to lower the risk of disease transmission among older adults in nursing homes, who have a high risk of contracting the disease (Grabowski and Mor, 2020; McMichael et al., 2020), the Ministry of Civil Affairs of China formulated the “Guidelines on the Prevention and Control of the Pneumonia Epidemic caused by a Novel Coronavirus in Eldercare Institutions” on January 28, 2020 (Ministry of Civil Affairs of the People's Republic of China, Jan 28, 2020). As a result, all the nursing homes in China implemented closed management and completely suspended family visits after January 2020. The same measures were taken worldwide in the following months (Skoog, 2020; Van Tilburg et al., 2020). Consequently, older adults in nursing homes were isolated and unable to regularly visit psychiatric outpatient clinics, which considerably increased their mental health burden (Skoog, 2020; Yang et al., 2020).
To improve older adults' mental health during the COVID-19 pandemic situation, many researchers have called for the promotion of Internet-based psychotherapy (Gould and Hantke, 2020; Steinman et al., 2020). In fact, the pandemic has resulted in the widespread adoption of online mental health services, such as Internet-based cognitive behavioral therapy (ICBT) in China (Bao et al., 2020; Liu et al., 2020). In addition, earlier studies indicated that carefully developed clinician or self-guided ICBT interventions may significantly reduce mental health problems in older adults (Titov et al., 2016; Xiang et al., 2020). Furthermore, mental health professionals can play an important role in addressing psychological distress in older adults during the pandemic by reaching out to them through the Internet and screening them for psychological distress (Jawaid, 2020; Mukku and Sivakumar, 2020). A previous study also demonstrated that human support increases adherence to treatment through accountability to a coach, who is seen as a trustworthy expert (Mohr et al., 2011). Therefore, we chose a clinician-guided ICBT as the intervention in this study.
To date, several studies have explored the efficacy of Internet-based mental health interventions on people affected by the COVID-19 pandemic (Al-Alawi et al., 2021; Schlarb et al., 2021; Wei et al., 2020; Zhang et al., 2020; Zhou et al., 2020), while some smaller studies have focused on older adults (Shapira et al., 2021; Goodman-Casanova et al., 2020), especially those living in nursing homes, during the COVID-19 pandemic. In line with emerging research, we conducted a feasibility study to examine ICBT's effectiveness in the treatment of psychological distress in older adults without cognitive impairment living in nursing homes in China during the COVID-19 pandemic. This was the first study to explore the feasibility of ICBT intervention among older adults living in nursing homes in China during the COVID-19 pandemic, and to underscore its effectiveness for use in older adults.
It should be noted that nursing homes in China refer to public or private facilities providing nursing home care for older adults. Nursing home care in China is broadly divided into 4 categories: (1) Grade 3: independent in self-care; (2) Grade 2: semi-dependent in self-care; (3) Grade 1: inability in self-care; and (4) special nursing needs (Chu and Chi, 2008). In terms of ownership, nursing homes in China can be broadly characterized as government built and operated, government built and privately operated (mixed model), and privately built and operated (Feng et al., 2020). However, functional limitations and health status are not included as eligibility criteria for admission in any of these nursing homes, and cognitive and physical functioning of older adults living in them varies considerably.
The aim of this study was to test the following hypotheses
(1) Participants would demonstrate statistically significant improvements in measures of symptoms of depression, anxiety, general psychological distress, and functional disability, and those improvements would be sustained at follow-up. (2) Participants would show minor or major improvements in primary measures of symptoms of depression and anxiety. (3) Participants would show relatively high levels of adherence, response rate, acceptability, and treatment satisfaction.
2. Methods
2.1. Study design
This study conducted a single-group feasibility trial from 24 January 2020 to 31 March 2020, a period during which China witnessed the most serious stage of the COVID-19 pandemic. Standardized questionnaires were administered to participants before and after treatment, and at a 1-month follow-up. The study was promoted online through a WeChat official accounts platform. Older adults from eight nursing homes in four southeast cities in China participated in the study. Out of the eight nursing homes, four were government built and privately operated (Ningbo Guangan Nursing home, Ningbo YiLe Nursing home, Ningbo Yikang Nursing home, and Ningbo Fulin Nursing home) and the other four were privately built and operated (Songling Yada (Wuzhen) Nursing home, Shanghai Huixiangfu Nursing home, Hangzhou Suiyuan Nursing home, and Shanghai Yinkang Nursing home). Ten clinical psychologists from Ningbo First Hospital, Ningbo, China, ensured all clinical contact with the ICBT participants through a WeChat mini-program called the Healthy Psychological Station.
The study was approved by the Medical Ethics Committee of Ningbo First Hospital (approval number: 2020-R042) and the trial was registered in the Chinese Clinical Trials Registry (trial registration number: ChiCTR2000030697).
2.2. Participants and recruitment
A total of 231 older adults were consecutively recruited from January 24, 2020 to January 31, 2020. Among them, 127 met the study's inclusion criteria as described below.
With participants' permission, researchers examined the mental health information records of eligible older adults and informed the selected participants of their inclusion in the study.
With the help of researchers working in the same nursing homes, these participants were invited to sign an informed consent form online and were required to verbally confirm their consent in a telephonic interview. Selected participants were asked to login to the Healthy Psychological Station and fill out a series of questionnaires, including all measures, before treatment, immediately after treatment, and again 1 month after the treatment, as well as provide their sociodemographic data and their satisfaction with and acceptability of the treatment. Older adults who completed post-treatment and follow-up questionnaires received CNY 50 (approximately $7.50). To be eligible for participation in the study, the participants had to: (1) be residents of China, (2) be at least 60 years old, (3) have a smart device and internet access, (4) have a Patient Health Questionnaire 9-item (PHQ-9) score > 5 but not be currently experiencing severe depression (defined as a total score ≥ 19 or a score > 2 on question 9 on the PHQ-9) (Kroenke et al., 2001), and (5) have a Generalized Anxiety Disorder 7-item (GAD-7) score > 5, but not be currently experiencing severe GAD (defined as a total score ≥ 15) (Spitzer et al., 2006).
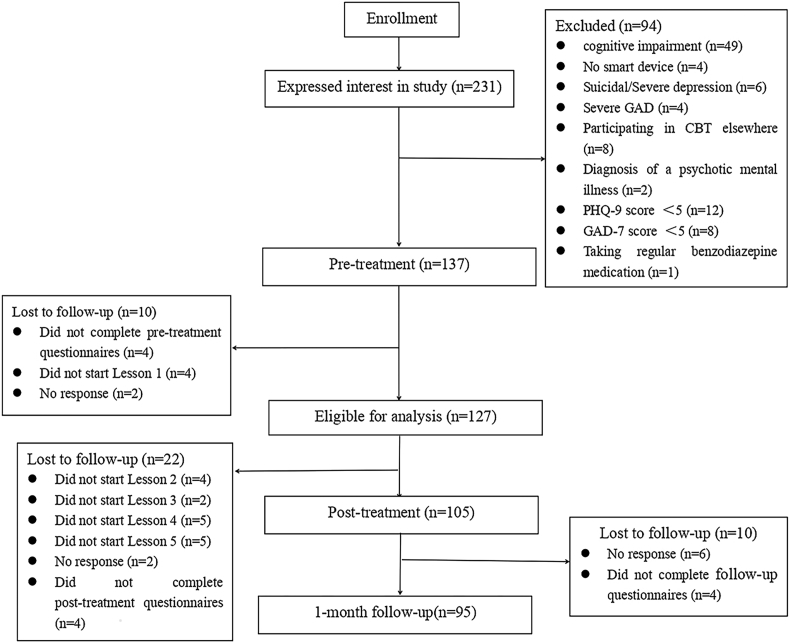
The exclusion criteria were as follows: (1) cognitive impairment with a score on a Mini-Mental State Examination ≤ 24 (Folstein et al., 1975), (2) participation in cognitive behavioral therapy (CBT) elsewhere, (3) use of illicit substances or consumption of more than three standard drinks a day, (4) diagnosis of a psychotic mental illness, and (5) taking regular benzodiazepine medication (i.e., more than once every 2 weeks) and, if taking a medication for anxiety or depression, not having been on a stable dose for at least a month. Fig. 1 depicts the details of participant flow.
Fig. 1.
Flowchart of participants.
2.3. The intervention
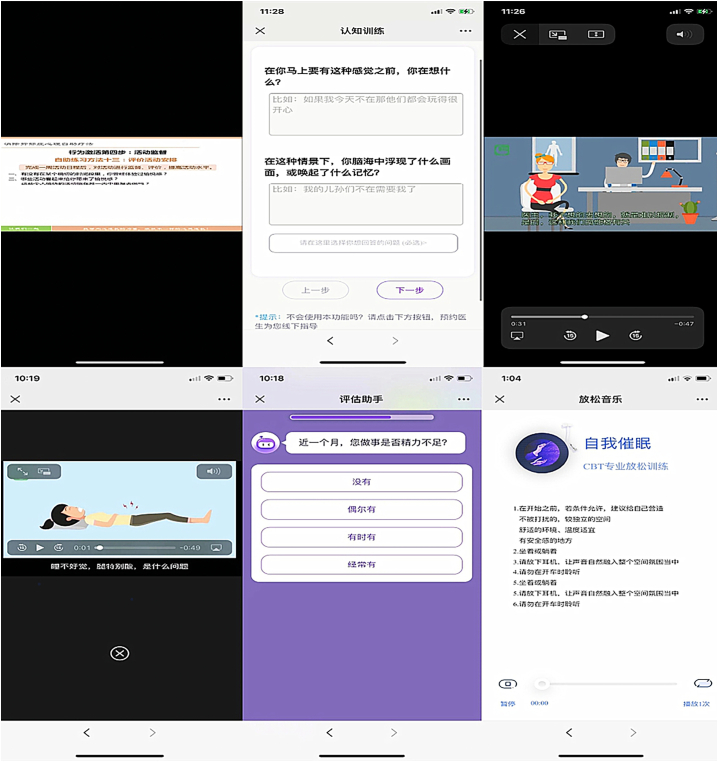
The Healthy Psychological Station comprised a 5-week long clinician-guided ICBT delivered through a WeChat mini-program. This program, which teaches practical CBT skills and comprises 5 lessons with corresponding case stories, is based on the Chinese version of the Handbook of Cognitive-Behavioral Therapies (Dobson et al., 2015). To make the lessons and case stories culturally appropriate for the Chinese, they were developed by clinical psychologists from Ningbo First Hospital and researchers from Ningbo College of Health Sciences in consultation with Chinese patients having a history of depression and anxiety, most of whom were over 55 years old. This was also the reason we chose this ICBT program for the participants. Fig. 2 provides a screenshot of the program.
Fig. 2.
A screen shot of an Internet-based cognitive behavioral therapy (ICBT) program called “Healthy Psychological Station”.
Table 1 depicts the descriptions of each lesson. Participants were instructed to read the lessons within five weeks according to the same treatment timetable. It was important that lessons were released sequentially based on completion of the prior lesson within five weeks. Without completing the previous lessons, the participants could not access the lessons for the next few weeks. The case stories corresponding to the lessons were based on real cases of Chinese patients who had undergone CBT and recovered from anxiety and depression. In addition to the five lessons, the Healthy Psychological Station (1) facilitated online communication with one of the clinicians who answered participants' questions about the treatment, provided technical assistance upon request, and encouraged them to use the program. All clinicians were trained to provide online communication before the start of the study, and all clinical contact with participants was recorded as the total clinical psychologist time; (2) provided a summary of each lesson, along with homework, to ensure participants' application of the skills taught in that lesson; (3) set an automated WeChat reminder to encourage adherence to the timetable and reinforce progress; and (4) made available additional WeChat mini-program resources on skills that were not described in the lessons, including communication skills, cognitive training, and sleep hygiene.
Table 1.
Lesson content of the Healthy Psychological Station.
| Lesson | Lesson content | Case story |
|---|---|---|
| Lesson 1 |
|
|
| Lesson 2 |
|
|
| Lesson 3 |
|
|
| Lesson 4 |
|
|
| Lesson 5 |
|
|
2.4. Measures
2.4.1. Primary outcome measures
2.4.1.1. Patient Health Questionnaire-9 Item
We employed the Chinese version of the PHQ-9 to assess the depressive symptoms in older adults. The PHQ-9 is a 9-item measure to assess the presence and severity of symptoms of depression, which is based on the Diagnostic and Statistical Manual of Mental Disorders-4th edition (DSM-IV) criteria for major depressive disorder (Kroenke et al., 2001). It has been widely used in China, and studies have demonstrated good reliability and validity of the Chinese version (Wang et al., 2014). The Cronbach's α was 0.91 in this study. Further, the presence of depressive symptoms was defined as a total score ≥ 5 points in the PHQ-9, according to earlier studies that were conducted during the COVID-19 pandemic (Liu et al., 2020; Ying et al., 2020).
2.4.1.2. Generalized Anxiety Disorder 7-Item
We employed the Chinese version of the GAD-7 to assess the anxiety symptoms in older adults. The GAD-7 is a seven-item measure to assess the presence and severity of symptoms of general anxiety and is based on the DSM-IV diagnostic criteria for GAD (Spitzer et al., 2006). It has been widely used in China, and studies have confirmed good reliability and validity of the Chinese version (Yu et al., 2018). The Cronbach's α was 0.92 in this study. The presence of an anxiety symptom was defined as a total score ≥ 5 points in the GAD-7, according to earlier studies that were conducted during the COVID-19 pandemic (Liu et al., 2020; Ying et al., 2020).
2.4.2. Secondary outcome measures
2.4.2.1. Geriatric Depression Scale
We employed the Chinese version of the Geriatric Depression Scale (GDS) to assess the depressive symptoms of older adults. The GDS is a 15-item short-form screening measure to assess and detect depression in older adults (Jerome et al., 1986). Studies have demonstrated good reliability and validity of its Chinese version (Chan, 1996). The Cronbach's α was 0.85 in this study.
2.4.2.2. Ten-Item Kessler Psychological Distress Scale
We employed the Chinese version of the 10-item Kessler Psychological Distress Scale (K-10) to assess the general psychological distress of older adults (Kessler et al., 2002). An earlier study found that the K-10 is useful in the diagnosis of anxiety and depressive disorders (Andrews and Slade, 2001). Studies have confirmed good reliability and validity of its Chinese version (Zhou et al., 2008). The Cronbach's α was 0.90 in this study.
2.4.2.3. Sheehan Disability Scales
We employed the Chinese version of the Sheehan Disability Scales (SDS) to assess the functional disability of older adults, in accordance with an earlier study that examined the ICBTs' effectiveness for older adults (Dear et al., 2013). It is 3-item scale measuring individuals' functional impairments in work and studies, social life, family life, and household responsibilities (Sheehan, 1983). Studies have confirmed good reliability and validity of its Chinese version (Leu et al., 2015). The Cronbach's α was 0.96 in this study.
2.4.2.4. Acceptability and satisfaction
Participants' satisfaction with and acceptability of treatment were assessed after treatment using the following two questions, which were taken from a similar study: (1) “Would you feel confident in recommending this program?” and (2) “Was it worth your time doing the program?” To these questions, participants responded with either “yes” or “no” (Dear et al., 2015).
2.5. Statistical analysis
All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). A two-tailed p-value <.05 was considered statistically significant.
Participants who did not start lesson 1 were not included in the analyses. An intention-to-treat (ITT) mixed-effects model for repeated measures (MMRM) (Gueorguieva and Krystal, 2004) was used to examine changes in the symptom measures over time. Missing data were handled using the last observation carried forward (LOCF) method. Furthermore, the effects were modelled using the restricted maximum likelihood (REML) estimation method with an unstructured (UN) covariance structure and participant characteristics as covariates. Model fit was evaluated using Schwarz's Bayesian criterion.
A standardized mean difference effect size (Cohen's d) was calculated using the observed pooled standard deviation (SD) as the denominator (Feingold, 2009) and then corrected for correlations between repeated measurement time points (Morris and DeShon, 2002). Furthermore, confidence intervals (CIs) for the effect size were calculated using the method described by Kelley (Kelley, 2007). Effect sizes were categorized as small, medium, and large for Cohen's d > 0.2, d > 0.5, and d > 0.8, respectively (Cohen, 1988).
Finally, the proportions of participants with deteriorating conditions (i.e., symptom deterioration ≥ 30%), no improvements (i.e., symptom deterioration ≤ 29% and symptom improvement ≤ 29%), minor improvements (i.e., symptom improvement ≥ 30% and ≤49%), and major improvements (i.e., symptom improvement ≥ 50%) were calculated. Minor and major improvements were defined as clinically meaningful improvements. This approach was used based on the findings of an earlier study (Dear et al., 2019).
3. Results
3.1. Participants' demographic characteristics
Table 2 depicts participants' demographic characteristics. As shown in Table 2, the median age of participants was 73.39 years (SD = 7.37, range 63-91 years). Of all the participants, 68.5% were women, and most were widowed (approximately 84.3%) and had more than 2 children (approximately 73.2%), respectively. In addition, only 3.9% of the participants had an educational qualification higher than a certificate/diploma/university degree. Most were independent in self-care or semi-dependent in self-care, and more than 90% had never taken prescription medication for anxiety or depression.
Table 2.
Participant characteristics.
| Variable | Total sample N = 127 |
|---|---|
| Gender, n (%) | |
| Women | 87 (68.50) |
| Men | 40 (31.50) |
| Age (years) | |
| Mean age (SD) | 73.39 (7.37) |
| Range | 61-92 |
| Marital status, n (%) | |
| Single/never married | 2 (1.57) |
| Married/de facto | 18 (14.17) |
| Separated/divorced/widowed | 107 (84.25) |
| Number of children, n (%) | |
| 0 | 2 (1.57) |
| 1 | 11 (8.67) |
| 2 | 21 (16.54) |
| 3 | 33 (25.98) |
| 4 | 31 (24.41) |
| More than 4 | 29 (22.83) |
| Education level, n (%) | |
| Junior school or below | 76 (59.84) |
| High school | 46 (36.22) |
| Certificate/diploma/university or above | 5 (3.94) |
| Employment status, n (%) | |
| Retired | 120 (94.49) |
| Employed | 5 (3.94) |
| Unemployed | 2 (1.57) |
| Nursing home, n (%) | |
| Ningbo YiLe Nursing home | 15 (11.81) |
| Ningbo Guangan Nursing home | 11 (8.67) |
| Ningbo Yikang Nursing home | 12 (9.45) |
| Ningbo Fulin Nursing home | 28 (22.05) |
| Songling Yada (Wuzhen) Nursing home | 21 (16.54) |
| Shanghai Yinkang Nursing home | 13 (10.24) |
| Shanghai Huixiangfu Nursing home | 14 (11.02) |
| Hangzhou Suiyuan Nursing home | 13 (10.24) |
| Care categories, n (%) | |
| Independent in self-care | 41 (32.28) |
| Semi-dependent in self-care | 75 (59.06) |
| Inability in self-care | 11 (8.66) |
| Special nursing needs | 0 (0.00) |
| History of taking prescription medication for anxiety/depression, n (%) | |
| No | 118 (92.91) |
| Yes | 9 (7.19) |
3.2. Primary outcome measures
Table 3 depicts the observed mean, SDs, and Cohen's d effect sizes for the primary outcome variables.
Table 3.
Primary and secondary outcome measures: observed mean and standard deviation, estimated change and within-group effect sizes (Cohen's d) based the estimates derived from the linear mixed model.
| Outcome | Observed mean (SDa) |
Estimated Change |
Cohen's d (95% CI) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | 1-month follow-up | Preb-postc | p value | Post-follow-up | p value | Pre-follow-up | p value | Pre-post | Post-follow-up | Pre-follow-up | |
| PHQ-9d | 10.57 (1.42) | 6.20 (2.62) | 6.46 (2.57) | -4.42 | <.001 | 0.26 | .190 | -4.16 | <.001 | 1.74 (1.62, 1.86) | 0.14 (0.07, 0.21) | 1.20 (1.10, 1.30) |
| GAD-7e | 9.51 (1.31) | 6.60 (2.28) | 6.18 (2.55) | -2.96 | <.001 | -0.42 | <.001 | -3.37 | <.001 | 1.71 (1.61, 1.81) | 0.29 (0.22, 0.36) | 1.27 (1.18, 1.36) |
| GDSf | 11.18 (1.06) | 8.00 (2.27) | 7.20 (2.65) | -3.24 | <.001 | -0.80 | <.001 | -4.04 | <.001 | 1.30 (1.19, 1.41) | 0.45 (0.38, 0.52) | 1.12 (1.02, 1.22) |
| K-10g | 29.76 (1.54) | 21.29 (4.86) | 21.47 (4.93) | -8.61 | <.001 | 0.18 | .601 | -8.43 | <.001 | 1.93 (1.80, 2.06) | 0.08 (0.01, 0.15) | 1.27 (1.16, 1.38) |
| SDSh | 15.68 (1.05) | 10.13 (3.13) | 10.81 (2.86) | -5.62 | <.001 | 0.68 | .002 | -4.94 | <.001 | 2.03 (1.90, 2.16) | 0.54 (0.47, 0.61) | 1.21 (1.11, 1.31) |
SD: standard deviation.
Pre: pre-treatment.
Post: post-treatment.
PHQ-9: Patient Health Questionnaire-9 Item.
GAD-7: Generalized Anxiety Disorder 7-Item Scale.
GDS: The Geriatric Depression Scale.
K-10: The 10-item Kessler Psychological Distress Scale.
SDS: Sheehan Disability Scales.
The mixed-effects model analyses comparing pre- and post-treatment scores revealed significant reductions with large effect sizes in both the PHQ-9 (p < .001, Cohen's d = 1.74, 95% CI 1.62-1.86) and GAD-7 (p < .001, d = 1.71, 95% CI 1.61-1.81).
Furthermore, the mixed-effects analysis comparing post-treatment and follow-up scores indicated significant reductions with small effect sizes in the GAD-7 (p < .001, d = 0.29, 95% CI 0.22-0.36), but no significant changes in the PHQ-9 (p = .190).
In addition, there were significant reductions with large effect sizes in both the PHQ-9 (p < .001, d = 1.20, 95% CI 1.10-1.30) and GAD-7 (p < .001, d = 1.27, 95% CI 1.18-1.36) from pre-treatment to follow-up.
3.3. Secondary outcome measures
Table 3 depicts the observed mean, SDs, and Cohen's d effect sizes for secondary outcome variables.
The mixed-effects model analyses comparing pre- and post-treatment scores revealed significant reductions with large effect sizes in the GDS (p < .001, d = 1.30, 95% CI 1.19-1.41), K-10 (p < .001, d = 1.93, 95% CI 1.80-2.06), and SDS (p < .001, d = 2.03, 95% CI 1.90-2.16).
The mixed-effects model analyses comparing post-treatment and follow-up scores indicated significant reductions with small effect sizes in the GDS (p < .001, d = 0.45, 95% CI 0.38 to 0.52) and improvements with medium effect sizes in the SDS (p = .002, d = 0.54, 95% CI 0.47-0.61), but no significant changes in the K-10.
Furthermore, there were significant reductions with large effect sizes in the GDS (p < .001, d = 1.12, 95% CI 1.02-1.22), K-10 (p < .001, d = 1.27, 95% CI 1.16-1.38), and SDS (p < .001, d = 1.21, 95% CI 1.11-1.31) from pre-treatment to follow-up.
3.4. Proportions of participants with deterioration, no improvements, minor improvements, and major improvements in treatment outcomes
Table 4 depicts the proportions of participants with deterioration, no improvements, minor improvements, and major improvements in treatment outcomes.
Table 4.
Proportions of participants with deterioration, no improvements, minor improvements, and major improvements in treatment outcomes.
| Outcome | Deteriorationa, n (%) |
No improvementsb, n (%) |
Minor improvementsc, n (%) |
Major improvementsd, n (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pree-postf | Post-follow-up | Pre-follow-up | Pre-post | Post-follow-up | Pre-follow-up | Pre-post | Post-follow-up | Pre-follow-up | Pre-post | Post-follow-up | Pre-follow-up | |
| PHQ-9 | 0 | 14 (14.74) | 0 | 10 (9.52) | 79 (83.16) | 8 (8.42) | 19 (18.10) | 1 (1.05) | 33 (34.74) | 76 (72.38) | 1 (1.05) | 54 (56.84) |
| GAD-7 | 1 (0.95) | 0 | 0 | 14 (13.33) | 86 (90.53) | 8 (8.42) | 74 (70.48) | 9 (9.47) | 38 (40.00) | 16 (15.24) | 0 | 49 (51.58) |
| GDS | 0 | 0 | 0 | 32 (30.48) | 83 (87.37) | 4 (4.21) | 60 (57.14) | 12 (12.63) | 47 (49.47) | 13 (12.38) | 0 | 44 (46.32) |
| K-10 | 0 | 2 (2.11) | 0 | 11 (10.48) | 93 (97.89) | 14 (14.89) | 94 (89.52) | 0 | 79 (84.04) | 0 | 0 | 1 (1.06) |
| SDS | 0 | 1 (1.05) | 0 | 7 (6.67) | 94 (98.95) | 7 (7.37) | 73 (69.52) | 0 | 84 (88.42) | 25 (23.81) | 0 | 4 (4.21) |
Deterioration was defined as a deterioration in symptoms ≥ 30%.
No improvements were defined as a deterioration in symptom ≤ 29% and an improvement in symptoms ≤ 29%.
Minor improvements were defined as an improvement in symptoms ≥ 30% to ≤49%.
Major improvements were defined as an improvement in symptoms ≥ 50%.
Pre: pre-treatment.
Post: post-treatment.
Post-treatment, 90.48%, 85.72%, 69.52%, 89.52%, and 93.33% of the participants reported clinically meaningful improvements in the PHQ-9, GAD-7, GDS, K-10 and SDS, respectively. Only one participant (0.95%) experienced deterioration in anxiety symptoms post-treatment.
Furthermore, at follow-up, 9.47% and 12.63% of the participants reported clinically meaningful improvements in the GAD-7 and GDS, respectively, whereas 14.74% experienced deteriorations in the PHQ-9. From pre-treatment to follow-up, more than 85% of the participants reported clinically meaningful improvements in all outcomes, while no participant experienced any deterioration.
3.5. Adherence, attrition, response rates, and treatment satisfaction
The 5 lessons in the Healthy Psychological Station were completed by 111 of 127 participants (87.4%) in 5 weeks. The average number of lessons completed was 4.74 (SD = 0.81), and the mean total clinical psychologist time spent with each participant for the entire program was 35.63 min (SD = 25.41). Furthermore, eight participants (6.3%) did not respond to and eight (6.3%) did not complete the post-treatment or follow-up questionnaires. Hence, post-treatment and 1-month follow-up data were collected from 105/127 (82.68%) and 95/127 (74.80%) participants, respectively. The participants who completed the post-treatment satisfaction questionnaires reported a high level of satisfaction. Further, 84 participants (80.00%) felt confident in recommending this mini-program to others, and 92 (87.62%) reported that it was worth doing.
4. Discussion
4.1. Principal findings
In this study, we explored the feasibility of clinician-guided ICBT on older adults without cognitive impairments living in nursing homes during the COVID-19 pandemic. The study revealed that the intervention was feasible with large effect sizes from pre- to post-treatment and at 1-month follow-up for symptoms of anxiety (measured by the GAD-7), depression (measured by the PHQ-9 and GDS), general psychological distress (measured by the K-10), and functional disability (measured by the SDS). In addition, more than 85% of participants reported clinically meaningful improvements in all outcomes from pre-treatment to follow-up, while none experienced any deterioration. Furthermore, 87.4% of participants completed all five lessons in the Healthy Psychological Station, and more than 80% of them reported a high degree of satisfaction. Overall, ICBT was found to be effective in reducing psychological distress in older adults without cognitive impairments living in nursing homes in China during the pandemic.
4.2. Comparisons with previous work
The results of this trial are comparable with those of other randomized controlled trials (RCTs) that investigated Internet-based mental health interventions among participants with symptoms of anxiety and depression during the COVID-19 pandemic (Al-Alawi et al., 2021; Wei et al., 2020) and a preliminary study that evaluated the effectiveness of WeChat-based individual counselling on suspected COVID-19 patients (Zhou et al., 2020). All the studies indicated that participants exhibited significantly decreased levels of depressive and anxiety symptoms after treatment and that Internet-based psychological interventions could play an important role in relieving the psychological burden on people who are isolated from society; including patients with COVID-19 as well as older adults living in nursing homes, during the pandemic. For this reason, online mental health services, particularly ICBT, were widely adopted in China during the pandemic (Bao et al., 2020; Liu et al., 2020; Mukku and Sivakumar, 2020). However, none of the aforementioned studies provide an effect size for the outcomes of mental health interventions. In addition, although some studies suggested good effectiveness of ICBT on sleep problems during the COVID-19 pandemic, they did not report an effect size of the improvement in mental health (Schlarb et al., 2021; Zhang et al., 2020). Thus, we could not directly compare the effectiveness of these interventions; future RCTs should be conducted to compare the effects of different psychological interventions implemented during the pandemic.
Compared to conventional face-to-face therapy, ICBT is advantageous because it can be flexibly applied, conducted independently of time and place, and implemented at lower costs and lower threshold accessibility (Andersson et al., 2019). These aspects of ICBT are particularly relevant for older adults isolated in nursing homes during the pandemic. To the best of our knowledge, this is the first study to provide detailed data on the effectiveness of ICBT on older people without cognitive impairments living in nursing homes during the pandemic. Although studies from different countries have reported on the pandemic's severe negative psychological effects on older adults and relevant mental health services, particularly those used by the older adults isolated in nursing homes (Gould and Hantke, 2020; Skoog, 2020; Steinman et al., 2020; Van Tilburg et al., 2020; Yang et al., 2020), only a few studies have examined the effects of online psychotherapy for community-dwelling older adults (Goodman-Casanova et al., 2020; Shapira et al., 2021), while no studies have focused on older persons living in nursing homes.
It is worth noting that the within-group effect size for depressive symptoms in this study was much higher than that of the community-dwelling older adults using the PHQ-9 (Shapira et al., 2021). We speculated that compared to older adults living in the community, participants with higher baseline severity of depressive symptoms in this study were more likely to obtain larger symptom reduction, according to the results of previous studies (Bower et al., 2013; Mathiasen et al., 2018). Moreover, in this study, within-group effect sizes, as well as the proportions of participants who reported reliable improvements in treatment outcomes, were both high; these values were as high as or even higher than those reported in earlier uncontrolled studies (pre-post design) on ICBT's effectiveness on older adults under non-pandemic conditions (Dear et al., 2013; Dear et al., 2015). There are several possible explanations for our findings. First, ICBT is likely to have the highest benefits in individuals with positive attitudes (Schröder et al., 2018). The adherence, response rates, and treatment satisfaction in this study were as high as or even higher than those observed in the aforementioned studies (Dear et al., 2013; Dear et al., 2015). This is understandable because the older adults who were isolated in nursing homes were more eager to improve their mental health during the pandemic than during non-pandemic conditions (Steinman et al., 2020). In addition, given the culture of obedience to the authority of doctors in China, clinician-guided ICBT may be more acceptable for Chinese older adults, compared to older adults of other races or from other ethnic backgrounds in the aforementioned studies. Further, although the older-adult population group usually tends to have lower levels of digital literacy, in this study, the participants could seek technical assistance from clinicians at any time. Moreover, the clinicians encouraged them to use the program. Such human support from clinicians can decrease participant attrition rate (Mohr et al., 2011). Second, in this study, clinicians answered participants' questions about the treatment. This kind of human support can enhance the effectiveness of eHealth interventions (Andersson and Cuijpers, 2009). There is compelling evidence which demonstrates that clinician-guided ICBT is more effective than unguided ICBT in mitigating psychological distress (Baumeister et al., 2014). A recent study also found that therapist-guided online therapy was superior to self-help online therapy during COVID-19 pandemic (Al-Alawi et al., 2021). Third, our program was developed based on conventional CBT, which has been shown to be effective in people affected by the pandemic (Cole et al., 2020). Lastly, although the ICBT program used in this study was not tailored for older adults, the lessons and case stories were developed in consultation with Chinese patients having a history of depression and anxiety, most of whom were more than 55 years old.
A statistically significant increase was observed in SDS scores alone at 1-month follow-up. This finding is inconsistent with the data indicating the follow-up effects of ICBT on SDS scores for older adults (Dear et al., 2013). One possible reason is that SDS measures functional impairment by focusing on individuals' social life, family life, and household responsibilities (Sheehan, 1983). The spread of the COVID-19 pandemic was almost brought under control in China by the end of this study's 1-month follow-up period. However, closed management and suspension of family visits continue to be strictly implemented in all nursing homes. Therefore, we speculate that older adults still suffer from a functional disability that results from insufficient family support, since they cannot physically meet their family members.
Pandemic conditions remain extremely serious outside China, and older people living in nursing homes have accounted for approximately 25-50% of documented deaths due to COVID-19 in the United States and some European countries including France and Ireland (Grabowski and Mor, 2020). A recent study demonstrated that older adults in nursing homes still experience psychological distress because of the burden of social isolation and containment measures (Greco et al., 2021). In the context of such a situation, our findings provide potential evidence for recommending the use of ICBT to manage psychological distress among isolated older adults without cognitive impairment living in nursing homes in other countries as well. Another important implication of this study is that it extends the findings of earlier studies by firstly examining ICBT's feasibility and effectiveness for use in older adults among Chinese populations. Furthermore, the results of this study are similar to those of studies evaluating ICBT's use for older adults of other races or from other ethnic backgrounds (Dear et al., 2015; Silfvernagel et al., 2018).
4.3. Strengths and limitations
This study has the following strengths: First, participants' mental health status was measured using well-validated measurement tools with good reliability and validity. Second, the attrition rates were relatively small at the 1-month follow-up. Moreover, assuming that the data of the participants who were lost-to-follow-up were randomly missing, the linear mixed model provides an unbiased estimation of the ITT effect.
Nevertheless, we acknowledge several limitations of our study. First, it was a feasibility trial that used a single-group design with no control group. Thus, the results of this study should be considered with caution. During the pandemic, ICBT's effectiveness may have been affected by other factors that cannot be controlled for with a single-group design. For instance, adjustment to the “new normal” of the pandemic through increased coping flexibility (Cheng et al., 2021), the positive role of the community in flattening mental health risks (Ahmed et al., 2020), and a reduction of pandemic-related information in the media (Depoux et al., 2020). However, due to the sudden and serious outbreak of COVID-19 in China in January 2020, we had no time to develop tailored interventions for participants in the intervention or control group because we needed to devise a solution focused on improving the mental health of older adults living in nursing homes at the earliest. Hence, further research involving direct comparison groups such as a waiting-list control group or participants in a control group receiving self-help to improve psychological distress associated with COVID-19 is required to draw conclusions on the effectiveness of ICBT in older adults.
Second, the results were based on self-reported scores of older adults collected through the Internet; hence, data collection might have resulted in selection bias. Additionally, clinician-rated scales of Hamilton Depression Scale (HAMD; Hamilton, 1967) and Hamilton Anxiety Scale (HAMA; Hamiltion, 1959) may be more appropriate to evaluate the clinical efficacy of the treatment of depression and anxiety in practice. However, we did not use these measurements because clinicians could not enter nursing homes due to COVID-19 restrictions. We suggest that HAMD and HAMA be used in future studies to examine the clinical efficacy of ICBT in improving depression and anxiety among older adults during the COVID-19 pandemic.
Third, our sample was not highly representative because all the respondents were from four southeast cities in China. However, because of the Chinese Lunar New Year holiday, the population outflows from Wuhan during the pandemic were concentrated in eastern China (Cheng et al., 2020). These four cities had the second, third, fourth, and seventh largest numbers of confirmed cases in East China, respectively, during the period of this study (Health Commission of Zhejiang Province, March 31, 2020). Thus, our sample was comparatively representative.
Fourth, it is unclear whether the current results were maintained beyond the 1-month follow-up period, because the pandemic situation was brought under control by early April 2020 in China. Fifth, most of the participants in this study were independent or semi-dependent in self-care. However, cognitive and physical functioning of older adults living in nursing homes varies considerably across countries. Therefore, the generalizability of our findings may be limited.
5. Conclusions
The study results provide evidence in support of ICBT's effectiveness in helping older adults without cognitive impairments living in nursing homes recover from mental health challenges during the COVID-19 pandemic. Although the study did not use a control group, the results indicated that ICBT interventions delivered during the pandemic period could result in similarly high or even higher treatment completion rates, levels of satisfaction, and larger effect sizes for older adults than those delivered during non-pandemic conditions. The findings of the current trial further highlight the considerable potential of ICBT programs, such as the Healthy Psychological Station, in improving access to online psychotherapy of isolated older adults living in nursing homes, who may otherwise never receive mental health services during the COVID-19 pandemic.
Role of the funding source
This study was supported by the Ningbo Philosophy and Social Planning Project [Grant No. G21-3-ZX94], Zhejiang Province Public Welfare Technology Application Research Project [Grant No. LGF21H090004], Ningbo Public Welfare Science and Technology Plan Project [Grant No. 202002N3180], General Scientific Research Project of Department of Education of Zhejiang Province [Grant No. Y201942547], Ningbo Health Branding Subject Fund [Grant No. PPXK2018-01], Medical and Health Science and Technology Plan Project of Zhejiang Province [Grant No. 2021KY335, 2017KY136, 2018KY671 and 2019KY564], Major Social Development Special Foundation of Ningbo [Grant No. 2017C510010], Science and Technology Innovation Activity Plan of Zhejiang University Student & XinMiao Talents Program [Grant No. 2021R464003]. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
CRediT authorship contribution statement
YY, YJ, LR, and ZL conceived and designed the experiments, YY, YJ, KF, QC, and YH performed the experiments, FK, LZ, ZL, PM, LY and LL analysed the data, YY, YJ, LR, ZL, WK, LW, and QC wrote the manuscript, YY, LR, LJ, XZ, XL, LX, YM, ZL, and LR reviewed and commented on the manuscript. All authors read and approved the final manuscript.
Declaration of competing interest
None.
Acknowledgements
We would like to thank all the older adults for participating, clinicians for providing clinician-assistance, and programmers for constructing the ICBT platform, and Editage (www.editage.cn) for English language editing. In addition, we express our heartfelt respect for all health care workers who are fighting against the COVID-19 pandemic.
Contributor Information
Zhongze Lou, Email: lorenzo_87@163.com.
Liemin Ruan, Email: 13805869162@163.com.
References
- Ahmed D., Buheji M., Merza Fardan S. Re-emphasising the future family role in ‘care economy’ as a result of Covid-19 pandemic spillovers. Am. J.Econ. 2020;10(6):332–338. doi: 10.5923/j.economics.20201006.03. [DOI] [Google Scholar]
- Al-Alawi M., McCall R.K., Sultan A., Al Balushi N., Al-Mahrouqi T., Al Ghailani A., Al Sinawi H. Efficacy of a six-week-long therapist-guided online therapy versus self-help internet-based therapy for covid-19-induced anxiety and depression: open-label, pragmatic, randomized controlled trial. JMIR Ment. Health. 2021;8(2) doi: 10.2196/26683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn. Behav. Ther. 2009;38(4):196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Andersson G., Titov N., Dear B.F., Rozental A., Carlbring P. Internet-delivered psychological treatments: from innovation to implementation. World Psychiatry. 2019;18(1):20–28. doi: 10.1002/wps.20610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Slade T. Interpreting scores on the kessler psychological distress scale (K10) Aust. N. Z. J. Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842X.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister H., Reichler L., Munzinger M., Lin J. The impact of guidance on internet-based mental health interventions—a systematic review. Internet Interv. 2014;1(4):205–215. doi: 10.1016/j.invent.2014.08.003. [DOI] [Google Scholar]
- Bower P., Kontopantelis E., Sutton A., Kendrick T., Richards D.A., Gilbody S., Liu E.T. Influence of initial severity of depression on effectiveness of low intensity interventions: meta-analysis of individual patient data. BMJ. 2013;346 doi: 10.1136/bmj.f540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A.C. Clinical validation of the Geriatric Depression Scale (GDS): Chinese version. J. Aging Health. 1996;8(2):238–253. doi: 10.1177/089826439600800205. [DOI] [PubMed] [Google Scholar]
- Cheng C., Zhang T., Song C., Shen S., Jiang Y., Zhang X. The coupled impact of emergency responses and population flows on the COVID-19 pandemic in China. Geohealth. 2020;4(12) doi: 10.1029/2020GH000332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C., Wang H., Ebrahimi O.V. Adjustment to a“New Normal:”coping flexibility and mental health issues during the COVID-19 pandemic. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.626197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu L.W., Chi I. Nursing homes in China. J. Am. Med. Dir. Assoc. 2008;9(4):237–243. doi: 10.1016/j.jamda.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Cohen J. second ed. Lawrence Erlbaum Associates; Mahwah: 1988. Statistical Power Analysis for the Behavioural Sciences. [Google Scholar]
- Cole C.L., Waterman S., Hunter E.C.M., Bell V., Greenberg N., Rubin G.J., Beck A. Effectiveness of small group cognitive behavioural therapy for anxiety and depression in ebola treatment Centre staff in Sierra Leone. Int. Rev. Psychiatry. 2020;17:1–9. doi: 10.1080/09540261.2020.1750800. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Zou J., Titov N., Lorian C., Johnston L., Spence J., Knight R.G. Internet-delivered cognitive behavioural therapy for depression: a feasibility open trial forolder adults. Aust. N. Z. J. Psychiatry. 2013;47(2):169–176. doi: 10.1177/0004867412466154. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Zou J.B., Ali S., Lorian C.N., Johnston L., Terides M.D., Titov N. Examining self guided internet-delivered cognitive behavior therapy for older adults withsymptoms of anxiety and depression: two feasibility open trials. Internet Interv. 2015;2:17–23. doi: 10.1016/j.invent.2014.11.002. [DOI] [Google Scholar]
- Dear B.F., Johnson B., Singh A., Wilkes B., Brkic T., Gupta R., Titov N. Examining an internet-delivered intervention for anxiety and depression when delivered as a part of routine care for university students: a phase IV trial. J. Affect Disord. 2019;256:567–577. doi: 10.1016/j.jad.2019.06.044. [DOI] [PubMed] [Google Scholar]
- Depoux A., Martin S., Karafillakis E., Preet R., Wilder-Smith A., Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J. Travel Med. 2020;27(3):taaa031. doi: 10.1093/jtm/taaa031/5775501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobson, Keith S., Li Z.J. third ed. People’s medical publishing house; Beijing: 2015. Chinese Version of Handbook of Cognitive-behavioral Therapies. [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol. Methods. 2009;14(1):43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z., Glinskaya E., Chen H., Gong S., Qiu Y., Xu J., Yip W. Long-term care system for older adults in China: policy landscape, challenges, and future prospects. Lancet. 2020;24;396(10259):1362–1372. doi: 10.1016/S0140-6736(20)32136-X. [DOI] [PubMed] [Google Scholar]
- Folstein M.F., Folstein S.E., McHugh P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Goodman-Casanova J.M., Dura-Perez E., Guzman-Parra J., Cuesta-Vargas A., Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: survey study. J. Med. Internet Res. 2020;22(5) doi: 10.2196/19434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould C.E., Hantke N.C. Promoting technology and virtual visits to improve older adult mental health in the face of COVID-19. Am. J. Geriatr. Psychiatry. 2020;28(8):889–890. doi: 10.1016/j.jagp.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski D.C., Mor V. Nursing home Care in Crisis in the wake of COVID-19. JAMA. 2020;324(1):23–24. doi: 10.1001/jama.2020.8524. [DOI] [PubMed] [Google Scholar]
- Greco G.I., Noale M., Trevisan C., Zatti G., Pozza M.D., Lazzarin M., Sergi G. Increase in frailty in nursing home survivors of Coronavirus disease 2019: comparison with noninfected residents. J. Am. Med. Dir. Assoc. 2021;22 doi: 10.1016/j.jamda.2021.02.019. S1525-8610(21)00233-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gueorguieva R., Krystal J.H. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the archives of general psychiatry. Arch. Gen. Psychiatry. 2004;61(3):310–317. doi: 10.1001/archpsyc.61.3.310. [DOI] [PubMed] [Google Scholar]
- Hamiltion M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959;32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. Br. J. Soc. Clin. Psychol. 1967;6(4):278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Health Commission of Zhejiang Province Report on the epidemic situation of COVID-19 in Zhejiang Province as of March 31, 2020. 2020. https://wsjkw.zj.gov.cn/art/2020/3/31/art_1202101_42435723.html (accessed Apr 4, 2021)
- Jawaid A. Protecting older adults during social distancing. Science. 2020;368(6487):145. doi: 10.1126/science.abb7885. [DOI] [PubMed] [Google Scholar]
- Jerome A., Yesavage M.D., Javaid I., Sheikh M.D. Geriatric depression scale (GDS) Clin. Gerontol. 1986;5(1–2):165–173. doi: 10.1300/J018v05n01_09. [DOI] [Google Scholar]
- Kelley K. Confidence intervals for standardized effect sizes: theory, application, and implementation. J. Stat. Softw. 2007;20:1–24. doi: 10.18637/jss.v020.i08. [DOI] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L., Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leu S.H., Chou J.Y., Lee P.C., Cheng H.C., Shao W.C., Hsien W.L., Chen V.C. Validity and reliability of the Chinese version of the Sheehan Disability Scale (SDS-C) Asia Pac. Psychiatry. 2015;7(2):215–222. doi: 10.1111/appy.12182. [DOI] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston G., Rostamipour H., Gallagher P., Kalafatis C., Shastri A., Huzzey L., Marston L. Prevalence, management, and outcomes of SARS-CoV-2 infections in older people and those with dementia in mental health wards in London, UK: a retrospective observational study. Lancet Psychiatry. 2020;7(12):1054–1063. doi: 10.1016/S2215-0366(20)30434-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathiasen K., Riper H., Andersen T.E., Roessler K.K. Guided internet-based cognitive behavioral therapy for adult depression and anxiety in routine secondary care: observational study. J. Med. Internet Res. 2018;20(11):e10927. doi: 10.2196/10927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael T.M., Currie D.W., Clark S., Pogosjans S., Kay M., Schwartz N.G., Duchin M.D. Public health–Seattle and King County, EvergreenHealth, and CDC COVID-19 investigation team. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N. Engl. J. Med. 2020;382(21):2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Civil Affairs of the People’s Republic of China . 1st edition. 2020. Guidelines on the Prevention and Control of the Pneumonia Epidemic caused by a Novel Coronavirus in Eldercare Institutions.http://www.mca.gov.cn/article/xw/mzyw/202001/20200100023683.shtml (accessed Mar 27, 2021) [Google Scholar]
- Mohr D.C., Cuijpers P., Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J. Med. Internet Res. 2011;13(1) doi: 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris S.B., DeShon R.P. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol. Methods. 2002;7(1):105–125. doi: 10.1037/1082-989X.7.1.105. [DOI] [PubMed] [Google Scholar]
- Mukku S.S.R., Sivakumar P.T.T. Mental health Care of Older Adults during coronavirus disease (COVID-19) pandemic: challenges and way ahead in India. Indian J. Psychol. Med. 2020;42(5):495–496. doi: 10.1177/0253717620944824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlarb A.A., Fründ J.P., Kovacevic T., Faber J. Modularized iCBT-I self-learn training for university staff-prevention and early intervention in the SARS-CoV-2 crisis: a pilot study. Somnologie (Berl) 2021;24:1–9. doi: 10.1007/s11818-021-00301-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schröder J., Berger T., Meyer B., Lutz W., Späth C., Michel P., Moritz S. Impact and change of attitudes toward Internet interventions within a randomized controlled trial on individuals with depression symptoms. Depress Anxiety. 2018;35(5):421–430. doi: 10.1002/da.22727. [DOI] [PubMed] [Google Scholar]
- Shapira S., Yeshua-Katz D., Cohn-Schwartz E., Aharonson-Daniel L., Sarid O., Clarfield A.M. A pilot randomized controlled trial of a group intervention via zoom to relieve loneliness and depressive symptoms among older persons during the COVID-19 outbreak. Internet Interv. 2021;24 doi: 10.1016/j.invent.2021.100368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D.V. Scribner; New York: 1983. [Google Scholar]
- Silfvernagel K., Westlinder A., Andersson S., Bergman K., Diaz Hernandez R., Fallhagen L., Andersson G. Individually tailored internet-based cognitive behaviour therapy for older adults with anxiety and depression: a randomised controlled trial. Cogn. Behav. Ther. 2018;47(4):286–300. doi: 10.1080/16506073.2017.1388276. [DOI] [PubMed] [Google Scholar]
- Skoog I. COVID-19 and mental health among older people in Sweden. Int. Psychogeriatr. 2020;32(10):1173–1175. doi: 10.1017/S104161022000143X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Steinman M.A., Perry L., Perissinotto C.M. Meeting the care needs of older adults isolated at home during the COVID-19 pandemic. JAMA Intern. Med. 2020;180(6):819–820. doi: 10.1001/jamainternmed.2020.1661. [DOI] [PubMed] [Google Scholar]
- Titov N., Fogliati V.J., Staples L.G., Gandy M., Johnston L., Wootton B., Dear B.F. Treating anxiety and depression in older adults: randomised controlled trial comparing guided v. self-guided internet-delivered cognitive-behavioural therapy. BJPsych. Open. 2016;2(1):50–58. doi: 10.1192/bjpo.bp.115.002139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Tilburg T.G., Steinmetz S., Stolte E., Van Der Roest H., De Vries D.H. Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. J. Gerontol. B. Psychol. Sci. Soc. Sci. 2020;5 doi: 10.1093/geronb/gbaa111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Bian Q., Zhao Y., Li X., Wang W., Du J., Zhao M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Wei N., Huang B.C., Lu S.J., Hu J.B., Zhou X.Y., Hu C.C., Hu S.H. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J. Zhejiang Univ. Sci. B. 2020;21(5):400–404. doi: 10.1631/jzus.B2010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang X., Wu S., Zuverink A., Tomasino K.N., An R., Himle J.A. Internet-delivered cognitive behavioral therapies for late-life depressive symptoms: a systematic review and meta-analysis. Aging Ment. Health. 2020;24(8):1196–1206. doi: 10.1080/13607863.2019.1590309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Li W., Zhang Q., Zhang L., Cheung T., Xiang Y.T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4) doi: 10.1016/S2215-0366(20)30079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying Y., Ruan L., Kong F., Zhu B., Ji Y., Lou Z. Mental health status among family members of health care workers in Ningbo, China, during the coronavirus disease 2019 (COVID-19) outbreak: across-sectional study. BMC Psychiatry. 2020;20(1):379. doi: 10.1186/s12888-020-02784-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu W., Singh S.S., Calhoun S., Zhang H., Zhao X., Yang F. Generalized anxiety disorder in urban China: prevalence, awareness, and disease burden. J. Affect. Disord. 2018;234:89–96. doi: 10.1016/j.jad.2018.02.012. [DOI] [PubMed] [Google Scholar]
- Zhang C., Yang L., Liu S., Xu Y., Zheng H., Zhang B. One-week self-guided internet cognitive behavioral treatments for insomnia in adults with situational insomnia during the COVID-19 outbreak. Front. Neurosci. 2020;14 doi: 10.3389/fnins.2020.622749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao S.Z., Wong J.Y.H., Luk T.T., Wai A.K.C., Lam T.H., Wang M.P. Mental health crisis under COVID-19 pandemic in Hong Kong, China. Int. J. Infect. Dis. 2020;100:431–433. doi: 10.1016/j.ijid.2020.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou C., Chu J., Wang T., Peng Q., He J., Zheng W.G., Xu L.Z. Reliability and validity of 10-item Kessler scale (K10) Chinese version in evaluation of mental health status of Chinese population. Chin. J. Clin. Psychol. 2008;16:627–629. [Google Scholar]
- Zhou L., Xie R.H., Yang X., Zhang S., Li D., Zhang Y., Wen S.W. Feasibility and preliminary results of effectiveness of social media-based intervention on the psychological well-being of suspected COVID-19 cases during quarantine. Can. J. Psychiatry. 2020;65(10):736–738. doi: 10.1177/0706743720932041. [DOI] [PMC free article] [PubMed] [Google Scholar]