Highlights
-
•
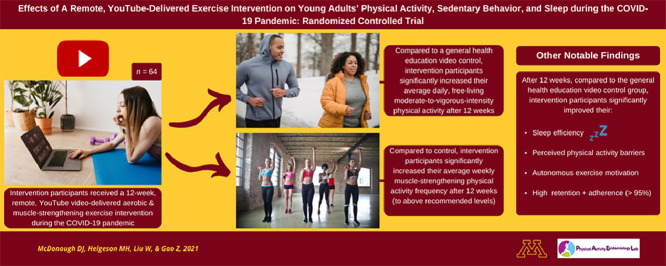
A 12-week, remote, YouTube video-delivered intervention improves free-living physical activity.
-
•
Muscle-strengthening activity improved after the 12-week, home-based, exercise intervention.
-
•
Home-based high-intensity interval training and resistance-training workouts improved autonomous exercise motivation.
-
•
The intervention improved sleep quality (sleep efficiency) during the COVID-19 pandemic.
-
•
A remote, video-delivered exercise program improved perceived physical activity and exercise barriers.
Keywords: High-intensity interval training, Resistance-training, Self-determination theory, Social media, Video
Abstract
Background
Public health guidelines have called for innovative and flexible physical activity (PA) intervention strategies to promote PA and health amid the coronavirus disease 2019 (COVID-19) pandemic. Therefore, this study's purpose was to examine the effects of a home-based, YouTube-delivered PA intervention grounded in self-determination theory on young adults’ free-living PA, sedentary behavior, and sleep quality (NCT04499547).
Methods
Sixty-four young adults (48 females; age = 22.8 ± 3.4 years, mean ± SD; body mass index = 23.1 ± 2.6 kg/m2) were randomized (1:1) into the intervention group, which received weekly aerobic and muscle-strengthening PA videos, or control group, which received weekly general health education videos, for 12 weeks. Our primary outcome was free-living moderate-to-vigorous PA (MVPA) and our secondary outcomes were sedentary behavior, light PA, and sleep quality (measured using ActiGraph accelerometers) along with muscle-strengthening PA frequency, self-determination theory-related motivation (non-regulation, external regulation, introjected regulation, identified regulation, integrated regulation, and intrinsic regulation), and perceived PA barriers (assessed using validated questionnaires). Repeated measures analysis of variances (ANOVAs) examined between-group differences at an adjusted significance level of 0.004 and effect sizes as partial eta-squared (ηp2).
Results
We observed statistically significant interaction effects for MVPA, sleep efficiency, muscle-strengthening PA frequency, non-regulation, integrated regulation, intrinsic regulation, and perceived PA barriers (F(1, 62) = 10.75–77.67, p < 0.001–0.002, ηp2 = 0.15–0.56) with all outcomes favoring the intervention group. We observed no statistically significant differences in either group for sedentary behavior, light PA, sleep duration, or external, introjected, and identified regulations after 12 weeks (F(1, 62) = 1.11–3.64, p = 0.06–0.61).
Conclusion
With national COVID-19 restrictions still in place and uncertainty regarding post-pandemic PA environments and behaviors, a remote, YouTube-delivered PA intervention may help foster clinically meaningful improvements in young adults’ free-living MVPA, muscle-strengthening PA frequency, sleep efficiency, PA-related intrinsic motivation, and perceived PA barriers.
Graphical Abstract
1. Introduction
To optimize health, the World Health Organization recommends adults engage in a minimum of 150 min per week of moderate-to-vigorous physical activity (MVPA) and at least 2 days per week of muscle-strengthening physical activities (PAs) targeting all major muscle groups.1 However, recent population-level surveillance data indicate that over 80% of U.S. adults fail to meet the minimum recommendations for aerobic and muscle-strengthening PAs.2 This pandemic of physical inactivity3,4 has become a major public health challenge, given that physical inactivity greatly increases the risk of developing non-communicable diseases and premature mortality5 and that physical inactivity-related morbidities now account for approximately 85% of total health care costs in the United States annually.4 Additionally, high levels of physical inactivity have been observed to adversely affect individuals’ sleep quality6 (i.e., sleep duration and efficiency7), which contributes to the incidence of hypokinetic diseases8 and all-cause mortality9 and further burdens the economy indirectly by decreasing daytime productivity.10
With the outbreak of the coronavirus disease 2019 (COVID-19) pandemic and the enacted regulations to reduce its transmission (e.g., physical distancing, gym and recreation center closures, home quarantine11, 12, 13, 14), we are currently facing an infectious disease pandemic that has compounded the preexisting physical inactivity pandemic.3,15 While all demographics have been affected by these regulations, U.S. young adults in particular have been forced to make extraordinary changes to their lifestyle and behavioral patterns,16 which has created exceptional barriers to their PA participation and has further exacerbated the issue of poor sleep quality in this population.16,17 Further, with the home environment emerging as the only viable indoor opportunity for PA, the inaccessibility of commercial exercise equipment has decreased young adults’ autonomous motivation to engage in PAs.18 Accordingly, the American College of Sports Medicine has released a call to action for health professionals to develop novel and flexible approaches to PA that account for these unprecedented circumstances.19 Thus, there is an urgent need to develop innovative and enjoyable home-based PA promotion interventions that minimize human contact, are cost-effective, and have a wide reach in order to help mitigate the compounding effects of the COVID-19 pandemic on physical inactivity and poor sleep quality among U.S. young adults.
One PA promotion intervention strategy that fulfills the preceding criteria is delivery by social media. Indeed, over 90% of U.S. young adults use online social media regularly20 and have demonstrated high interest in receiving health-related information on these platforms, thereby widening access to health behavior change interventions in this population.21 Further, social media platforms are cost-effective methods of increasing user interaction and providing peer-to-peer support,21 which may be especially beneficial to young adults during the COVID-19 pandemic considering their increased levels of anxiety and depression during this time.16 Thus, it stands to reason that social media would be an effective medium by which to disseminate a home-based PA intervention during the COVID-19 pandemic, especially among young adults who are the primary consumers.20 However, a meta-analysis of randomized controlled trials (RCTs) observed social media-based health behavior change interventions to be ineffective in promoting PA in this population.22 Notably, the PA interventions included in this analysis were delivered via Facebook groups, Twitter, or custom websites with social components (e.g., forums)—text-based platforms wherein participants were instructed to read PA-related information and apply it in their daily lives. However, eye-tracking studies23,24 have indicated that text-based media consumption on the Internet is primarily nonlinear (i.e., time is primarily spent browsing, keyword spotting, and/or scanning), thereby limiting information processing and the likelihood that participants will put the provided information into action. Further, global consumer Internet video traffic now accounts for over 80% of all consumer Internet traffic,25 and Internet-based video consumption is on track to surpass television for consuming video-based content,26 demonstrating a recent shift in preferred media consumption. Indeed, unlike text, online videos minimize the cognitive effort required to process information,27 thereby leading to improved comprehension, and have shown to be more engaging than content-identical, text-delivered content.27,28 That said, it is not surprising that YouTube—a video-based social media platform—is now the most used social media platform and is regularly used by over 94% of U.S. young adults.29,30 Therefore, the use of video-based social media platforms like YouTube to disseminate a remote, home-based PA promotion intervention warrants investigation.
Interestingly, despite the preceding statistics demonstrating the preference for, and benefits of, Internet-based video consumption over content-identical, text-based media consumption, the research empirically examining its utility for disseminating remote PA interventions is scant. Limited pilot trials28,31,32 with small sample sizes have demonstrated Internet-based, video-delivered PA content to be more effective than text-delivered content for promoting PA in adults. However, these trials were underpowered and were further limited by self-reported PA measures and short intervention durations. Interestingly, a large-scale RCT33 that addressed the preceding limitations found that Internet-delivered PA videos were not more effective than content-identical PA information delivered via text for increasing adults’ MVPA. However, this trial had notable limitations, which we believe hindered the effectiveness of utilizing video to increase individuals’ PA levels: (1) Attrition was very high (49% at 12 weeks) primarily from loss of intervention interest—likely due to low frequency of video dissemination (only 8 videos were disseminated over 12 weeks); (2) Too many behavior change theories were used when meta-analyses34,35 have shown multi-theory-based interventions to be less effective for PA behavior change compared to single-theory-based interventions; (3) Content within the videos was not guided by empirically-based content analyses and principles of health-based video quality;36 and (4) Example footage (i.e., “B-roll”)—one of the inherent benefits of using remotely-disseminated video—was not optimally utilized to demonstrate on-screen aerobic and muscle-strengthening PAs that participants could follow along to, thereby missing the opportunity to promote physical literacy, which is a major barrier to PA in young adults,37,38 especially with the recent confinement to the home without access to familiar exercise equipment.
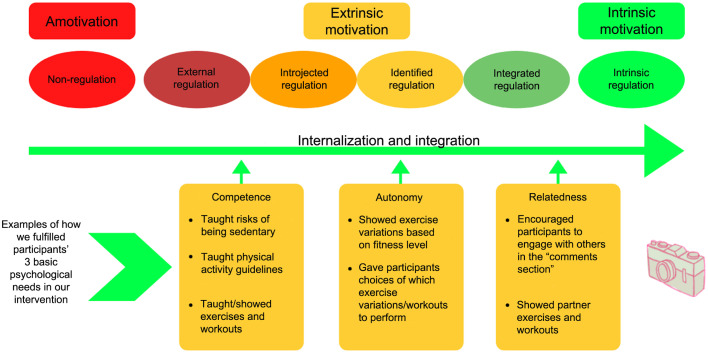
Taken together, in response to the preceding COVID-19-related barriers to young adults’ PA participation and the resulting decrease in autonomous motivation for engaging in home-based PA,16, 17, 18 a timely health behavior change intervention should aim to promote more intrinsically-regulated forms of PA motivation among this population. Thus, given the seamless integration of health behavior change theory in social media-based PA interventions,39,40 the intervention should be grounded in a behavior change theory that fosters more internally-regulated forms of motivation for PA. Self-determination theory (SDT) is a widely-used health behavior change theory that has demonstrated effectiveness for improving young adults’ intrinsic motivation for PA and exercise.41 Briefly, SDT postulates that by fulfilling 3 basic human psychological needs—competency (i.e., experience of mastery and effectiveness), autonomy (i.e., experience of willingness and volition), and relatedness (i.e., experience of connecting to others)—one's motivation will progress along a continuum to more internally-regulated forms ranging from amotivation (i.e., no motivation) to extrinsic motivation and then to intrinsic motivation, which helps foster long-term PA adherence.41
Therefore, this study's purpose was to examine the effects of a remote, home-based, YouTube video-delivered aerobic and muscle-strengthening PA intervention grounded in SDT as compared to a YouTube video-delivered general health education control intervention on young adults’ free-living MVPA (primary outcome) and sedentary behavior (SB), light PA (LPA), muscle-strengthening PA frequency, self-determined PA motivation, and perceived PA barriers (secondary outcomes). We hypothesized a priori that, compared to the control group, intervention participants would significantly improve their daily MVPA, SB, and LPA levels, muscle-strengthening PA frequency, intrinsic PA motivation, and perceived PA barriers after 12 weeks. Findings from this study may better inform clinicians and other health professionals of the utility of Internet-based video platforms to disseminate PA promotion interventions suitable for improving young adults’ aerobic and muscle-strengthening PA and sleep quality at scale to help attenuate the compounding effects of the COVID-19 pandemic on the preexisting pandemic of physical inactivity.
2. Materials and methods
We followed the CONSORT guidelines42 (Supplementary Table 1) while drafting this manuscript. Further, this study was approved by the University of Minnesota Institutional Review Board (STUDY00010444) in November 2020, and we registered the trial with ClinicalTrials.gov (NCT04499547). All study questionnaires were distributed to participants using Qualtrics (Qualtrics; Provo, UT, USA)—an online survey software. Notably, for all survey questions within this software, we applied the “force response” function to ensure a 100% survey response and completion rate.
2.1. Study design and sample
We employed a prospective, 12-week, parallel RCT wherein participants were randomized (1:1) into either the experimental group (received weekly YouTube video-delivered aerobic and muscle-strengthening PA videos grounded in SDT) or the control group (received weekly YouTube video-delivered general health education videos with no PA-related content). In detail, 64 participants from the University of Minnesota took part during Fall 2020–Winter 2021, and all participants started the study concurrently. Given national COVID-19-related campus closures, we only recruited participants via email communications, using various university email servers to sample from a variety of disciplines. We included participants who were between the ages of 18 years and 35 years, were enrolled or employed at/by the study university, had a body mass index (BMI) ≥ 18.5 kg/m2, had PA levels below national recommendations1 over the last month (verified by questionnaire), possessed no self-reported diagnosed physical/mental disability and had no contraindications to PA participation (assessed by the PA Readiness Questionnaire), had Internet access and a device capable of accessing YouTube, and were willing to be randomized into either study group. Participants were excluded from participation if they were younger than 18 years or older than 35 years, had a BMI < 18.5 kg/m2, met or were above the PA recommendations over the last month, answered “yes” to at least 1 question on the PA Readiness Questionnaire, did not have access to the Internet and/or YouTube, or were not willing to be randomized into either study group. We obtained Institutional Review Board approval from the University of Minnesota and written informed consent (digitally signed) from participants prior to recruitment and data collection. Further, all participant-involved procedures were performed in accordance with the ethical standards of the institution and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.43 Participants were paid USD30 for successful study completion.
2.2. Procedures
Interested participants were instructed to respond directly to the recruitment email, after which the project manager (MAH) responded with an email link containing the online consent form and questionnaires to determine whether they met the preceding inclusion criteria. Participants who qualified were emailed another link containing a battery of online baseline surveys to obtain demographic information and assess psychosocial and other self-reported study outcomes. The same psychosocial and self-report questionnaires were re-distributed at 12 weeks for post-intervention assessments. Additionally, at baseline and 12 weeks, participants who qualified for the study were mailed an ActiGraph accelerometer GT9X+ (ActiGraph, LLC., Pensacola, FL, USA) with an adjustable wrist strap, the associated wear instructions, and a sleep log; they were also provided a self-addressed stamped envelope to return the accelerometer and sleep log after the 7-day wear periods. Notably, the wear log was only utilized as a wear-compliance strategy, given that our analysis of raw accelerometer data did not require sleep log input. All accelerometers were disinfected based on World Health Organization guidelines44 as well as study university policies before being distributed to participants. Accelerometers were mailed back by participants in the supplied envelopes with pre-paid postage, and the returned accelerometers were left untouched (i.e., quarantined) for ≥14 days to rid them of any potential COVID-19 contamination.44
Following the 7-day baseline testing period, the project manager (MAH) informed participants of their group allocation. To preserve participants’ privacy and to blind the study investigators (DJM, WL, and ZG) to participants’ group allocation, participants were instructed by the project manager (MAH) to create a new YouTube account that was linked to their university email under a pseudo username (i.e., a creative username other than their given name) so they could not be identified (e.g., “YouTube Study Participant 2021”). Participants were then instructed to subscribe to the YouTube channel for their respective study group and turn on upload notifications by clicking the “bell” icon. Turning on upload notifications was used as an intervention adherence strategy as it ensured that participants would be immediately notified via email when each video was uploaded to the study channel. As a part of our intervention fidelity protocol, participants were encouraged to contact the project manager (MAH) with questions and were also contacted every 3 weeks during the study with standardized emails encouraging continued intervention adherence. Lastly, to prevent intervention contamination, we asked participants to refrain from sharing their group allocation and/or content from their group videos with friends/peers who were enrolled in the study.
2.3. Interventions
We used YouTube as the delivery vehicle for our intervention videos to maximize ecological validity as our formative testing among young adults at the study university revealed this platform to be the primary place of consumption for Internet-based video, which is consistent with statistics demonstrating YouTube to be the top social media platform both globally and in the United States, particularly among young adults (used by 94%).30 Additionally, social media platforms like YouTube are cost-effective methods of increasing user interaction and providing peer-to-peer support16,21 through interactions in the “comments section” of the videos, which our formative testing revealed to be an enjoyable intervention component.
We conducted formative testing in the Spring and Fall of 2020 among young adults around the university by distributing surveys and conducting small focus groups to help identify preferred PA-based video content (e.g., preferred video lengths and upload frequencies, preferred PA- and SB-related content, workout interests, etc.). Based on our findings, to achieve high intervention adherence and make the study videos enjoyable for both groups, we adhered to the American Medical Association's video quality guidelines45 for video and sound recording and best practices for video editing (e.g., utilizing “jump-cuts” for conciseness). Also based on feedback from our formative testing, we utilized “A-roll” (i.e., primary footage of the main subject (MAH) wherein the main content was taught interview-style) and overlaid the A-roll footage during post-production editing with “B-roll” (i.e., supplemental video footage) to visually demonstrate what was being talked about and show how to properly execute the information in order to facilitate participants’ physical literacy.36 To further increase video quality and participants’ comprehension of the intervention content, during post-production editing we overlaid our video footage with text using dynamic motion graphics titles, relevant stock images and video footage (Shutterstock.com; Shutterstock, New York, NY, USA), copyright-free music, and utilized multiple camera angles to demonstrate the proper biomechanics of the exhibited exercises. To track intervention adherence (i.e., watching all study videos in their entirety), we instructed both groups to reply to “in-video response questions” (embedded randomly within the videos) within the comments section of each video. We also tracked adherence using watch-time metrics provided by YouTube's Creator Analytics and informed participants that if we deemed video adherence too low, they may be removed from the study. Lastly, to improve ecological validity and facilitate SDT-related social support, we encouraged participants to interact with one another and to provide feedback on their replies to the response questions within the comments section of each video.
2.3.1. Experimental intervention
In addition to our formative testing, our videos were informed by an empirically-based content analysis36 examining the best practices for disseminating PA and SB information via video (e.g., emphasis should be placed more on increasing PA rather than reducing SB). Moreover, given research demonstrating young adults’ decreased autonomous motivation for engaging in home-based PAs,18 the intervention group videos were grounded in SDT.41 We demonstrated SDT and how we grounded our intervention group videos in SDT in Fig. 1.
Fig. 1.
Self-determination theory-grounded intervention videos.
The intervention group received 1 YouTube video per week (duration = 6.3 ± 3.9 min, mean ± SD) and were asked not to consume other PA-related YouTube videos during the duration of the 12-week intervention. In detail, the videos contained SB-related content (e.g., the negative effects of prolonged SB and different strategies for how to break up daily SB), PA-related content (e.g., taught participants the aerobic and muscle-strengthening PA guidelines1 and various strategies to increase their daily MVPA and muscle-strengthening PAs), and/or home-based aerobic and muscle-strengthening workouts that participants could follow along to on-screen. Regarding the home-based workout videos, in the absence of commercial gym equipment, high-intensity interval training has been observed as a feasible and effective option for home-based aerobic PA with limited space.46 Briefly, we leveraged pre-recorded video and edited in on-screen countdown timers (green timers indicated work intervals and red timers indicated rest intervals), so participants could follow along and workout during the video and we added in up-tempo music during the workout intervals to increase enjoyment and workout intensity. Likewise, muscle-strengthening exercise (e.g., resistance-training) could effectively be achieved in the home setting using one's own bodyweight and by manipulating various resistance-training variables (e.g., focusing on eccentric muscle actions, shortening between-set rest intervals, etc).46 Additionally, because the muscle-strengthening exercises were more difficult to follow along to on-screen (identified during formative testing), we demonstrated all exercises within each video and created high-quality PDF files (e.g., Supplementary Figs. 1 and 2) containing written versions of the workouts and then linked them directly under the YouTube videos so participants could download and readily access them any time they wanted to re-visit the workouts, ideally helping them to meet the weekly muscle-strengthening PA guideline. Lastly, given only 1 video per week was uploaded, we encouraged participants to re-visit the previous study videos and PDF workout files and to perform the provided workouts multiple times per week to further increase MVPA and muscle-strengthening PA levels. Full access to the control group's videos was provided after successful completion of the 12-week intervention.
2.3.2. Control condition
The control group also received 1 video per week during the 12-week intervention and participants were asked not to consume other health-related YouTube videos during the 12-week intervention. In detail, these videos were delivered on the same days/times as the intervention group videos but contained no PA-related content. Rather, the video content within the control group covered a variety of general health education topics relevant to young adults (e.g., nutrition, anxiety, mental health). As an additional incentive for intervention fidelity in the control group, full access to the intervention group's videos was provided after successful completion of the 12-week intervention.
2.4. Outcomes
We conducted the following tests to measure free-living MVPA (primary outcome) and sleep quality, adherence to the muscle-strengthening PA guidelines, SDT-related motivation, and perceived PA barriers (secondary outcomes). All study outcomes were determined a priori.
2.4.1. Baseline demographics and anthropometric measures
We used the online survey software to collect participants’ self-reported demographic information (e.g., age, sex, previous YouTube use/experience, COVID-19-related effects on their PA levels, etc.) using a variety of response types (e.g., multiple-choice, short answer). Full demographic information for our sample by study group is provided in Table 1. Given the fully remote nature of our study, baseline anthropometric measures (e.g., height (cm), weight (kg)) were also self-reported, and BMI was calculated as weight (kg)/height (m2). These data were collected at baseline and analyzed descriptively to characterize our sample.
Table 1.
Baseline group comparisons (self-reported).
| Intervention (n = 32) | Control (n = 32) | |
|---|---|---|
| Sex | ||
| Male Female |
9 23 |
7 25 |
| Race/ethnicity | ||
| Non-Hispanic Caucasian African American Asian Hispanic |
26 3 3 0 |
24 2 3 3 |
| Age (year) | 22.69 ± 3.06 | 22.91 ± 3.68 |
| PA level | ||
| MVPA/day (min) LPA/day (min) SB/day (min) |
8.28 ± 6.47 183.11 ± 42.19 688.02 ± 88.58 |
9.16 ± 7.01 192.17 ± 48.79 675.86 ± 65.38 |
| Sleep quality | ||
| Sleep duration (h/night) | 7.99 ± 0.82 | 8.07 ± 0.74 |
| Sleep efficiency (%) | 84.62 ± 7.12 | 86.69 ± 5.99 |
| Muscle-strengthening PA | ||
| Days/week | 0.81 ± 0.86 | 0.94 ±1.06 |
| Met guideline | 7 | 7 |
| Did not meet guideline | 25 | 25 |
| Psychosocial variable | ||
|
SDT-related intrinsic motivation Non-regulation External regulation Introjected regulation Identified regulation Integrated regulation Intrinsic regulation |
0.42 ± 0.43 1.30 ± 0.95 2.68 ± 0.94 2.96 ± 0.63 2.21 ± 0.92 2.48 ± 0.96 |
0.51 ± 0.53 1.18 ± 0.98 2.50 ± 0.97 2.98 ± 0.61 2.32 ± 0.60 2.38 ± 0.83 |
| Perceived PA barriers | 2.33 ± 0.39 | 2.25 ± 0.40 |
| Internet/YouTube use | ||
| Previous experience using YouTube | 32 | 32 |
|
Device most used to consume YouTube Phone Laptop Tablet |
26 4 2 |
24 5 3 |
| Anthropometric variable | ||
| Height (cm) | 171.29 ± 8.56 | 168.94 ± 10.04 |
| Weight (kg) | 67.29 ± 10.24 | 66.12 ± 10.07 |
| BMI (kg/m2) | 22.90 ± 2.74 | 23.34 ± 2.45 |
Notes: All categorical variable values are frequency or n. All continuous variable values are mean ± SD.
Abbreviations: BMI = body mass index; LPA = light physical activity; MVPA = moderate-to-vigorous physical activity; PA = physical activity; SB = sedentary behavior; SDT = self-determination theory.
2.4.2. Free-living PA, SB, and sleep quality
We measured daily minutes in MVPA, LPA, SB, and sleep quality using the wrist-worn ActiGraph Link GT9X accelerometer (ActiGraph)—a small (3.5×3.5×100 mm), lightweight (14 g) device that captures one's movement along the 3 orthogonal axes. We instructed participants to snugly and comfortably fit the accelerometers on the wrist of their non-dominant arm using the provided strap and to remove any other health wearable device(s) for the duration of the wear periods.47 To allow for the collection of PA and sleep data, we asked participants to wear the accelerometer all day and night for a period of 7 days with the only exception being during activities of prolonged deep-water submersion (e.g., swimming). Data were sampled at a frequency of 30 Hz, and we turned the screens off to disable PA-related feedback and prevent performance bias. We defined sleep quality as sleep duration (i.e., total true sleep time) and sleep efficiency (i.e., the ratio of time sleeping divided by total time in bed).7 We considered accelerometer data valid if the device was worn for at least 4 days, including at least 1 weekend day, and for at least 16 h each day.48
We processed the raw accelerometer data into 5-s epochs using the R Studio-package GGIR (Version 1.2.1335)49 in R Version 4.0.4 (the R Foundation, Vienna, Austria). Briefly, GGIR calculates PA intensities and detects non-wear time by converting all raw acceleration values into a single omnidirectional acceleration value. Specifically, the raw accelerometer data were auto-calibrated and converted into gravity-corrected vector magnitude units called Euclidian norm minus one with negative values set to zero. For valid wear days, we calculated PA intensities (i.e., MVPA, LPA, SB) based on previously established cut-points in milligravity (mg) for Euclidian norm minus one with negative values set to zero values: SB (0–56.2 mg), LPA (56.3–191.6 mg), and MVPA (>191.6 mg).50 For detection of participants’ sleep quality, we used GGIR to estimate change(s) in arm angle relative to the horizontal plane while sleeping, with a change in arm angle of <5° over a 5-min period considered as a possible sleep period.51 We calculated the following sleep variables: sleep duration (h/night) and sleep efficiency (total sleep time (h)/time in bed (h)×100%). Mean values for PA, SB, and sleep quality outcomes were calculated at baseline and 12 weeks.
2.4.3. Muscle-strengthening PA frequency
We assessed muscle-strengthening PA frequency using an item from the Behavioral Risk Factor Surveillance System survey—a valid and reliable self-report assessment of adults’ habitual participation in muscle-strengthening PAs.52 The full script for this item has been published elsewhere.53 Notably, participants reported their muscle-strengthening PA frequency as times per week or per month. For those who reported times per month, we divided this number by 4 to provide estimates of weekly muscle-strengthening PA frequency.52 Further, we a priori decided to truncate weekly frequency of muscle-strengthening PA at 14 times/week to limit the possibility of unrealistic responses.53 Mean changes in days/week of muscle-strengthening PA were used as the study outcome and were measured at baseline and 12 weeks.
2.4.4. SDT-related motivation
Participants’ SDT-related PA motivation was evaluated using the 24-item Behavioral Regulation in Exercise Questionnaire-3 (BREQ-3) survey54—a version of the BREQ-2 survey that is amended to include an assessment for integrated regulation, which has demonstrated good validity and reliability for measuring self-determined motivation for PA in U.S. young adults. Briefly, the BREQ-3 survey is used to quantify the continuum of behavioral regulation types in PA applications by evaluating 3 levels of motivation, progressing from amotivation to extrinsic motivation and then to intrinsic motivation, with 6 subscales progressing along this continuum: (1) non-regulation; (2) external regulation; (3) introjected regulation; (4) identified regulation; (5) integrated regulation; and (6) intrinsic regulation.55 In detail, using a 5-point Likert-type scale (1 = not true for me; 5 = always true for me), the BREQ-3 required participants to determine how true different statements were, such as “I don't see why I should have to exercise” (for non-regulation), and “I exercise because it's fun” (for intrinsic regulation). We used the mean score for each of the 6 subscales as the outcome, with higher scores indicating a greater regulation type. Participants’ SDT-related motivation was assessed at baseline and 12 weeks. Internal consistency (Cronbach's α) for this measure was good among our sample (α = 0.84).56
2.4.5. Perceived PA barriers
Participants’ perceived PA barriers were evaluated using the 14-item Perceived Barriers Scale, which has demonstrated good reliability and validity among adults.57 In detail, this scale required participants to rate the agreement between their own perceived PA barriers and hypothetical PA barriers using a 4-point Likert-type scale (1 = strongly disagree; 4 = strongly agree) for statements such as “Physical activity takes too much of my time” and “There are too few places to be physically active”. Mean scores were used as the study outcome, with higher scores indicating greater perceived barriers to PA. Participants’ perceived PA barriers were assessed at baseline and 12 weeks. Internal consistency for this measure was good among our sample (α = 0.81).56
2.5. Sample size calculation, randomization, and blinding
We used G*Power (G*Power; Brunsbüttel, Germany) to determine the necessary sample size for this study based on changes in free-living MVPA, which was our primary study outcome. Based on average (small) effect sizes for changes in young adults’ MVPA (d = 0.30) according to previous social media-delivered PA promotion interventions of the same duration,22,58 it was estimated that 60 participants (30 per group) were necessary to detect a significant between-group difference and give 80% power with a two-sided significance level of 0.05. Assuming 15% attrition, our goal was to enroll 69 participants. No interim analysis was planned.
Randomization, participant enrollment, and group allocation were completed by our project manager (MAH), who was blinded to the study questions and outcomes. Specifically, our random allocation sequence was completed using the “randomize” package in R Studio with no block restrictions applied. Given the use of pseudo usernames within the intervention YouTube channels to preserve participants’ privacy, all other investigators were blinded to participants’ group allocation; the blinding was not broken until the primary and secondary analyses were completed.
2.6. Statistical analysis
All data were collected and organized using an online spreadsheet. Prior to our main analysis, we extracted the raw accelerometer PA and sleep data from the associated ActiLife accelerometer software (Version 6.13.3; ActiGraph, LLC.) and analyzed these data using the GGIR package in R Studio (the R Foundation). Missing data were handled and analyzed under the intent-to-treat principle (i.e., based on original random allocation) using multiple imputation on a missing at random assumption and multiple imputation was completed with chained equations (MICE) using the MICE package in R Studio. Following that, we conducted our main analysis using SPSS Statistics (Version 27.0; IBM Corp., Armonk, NY, USA). First, we used histograms and Shapiro-Wilks’ statistics to examine the assumptions of normality and outliers for our repeated measures ANOVAs. We then conducted two-way (time × group) repeated measures analysis of variances (ANOVAs) for all outcomes, with time as the within-subject factor and group as the between-subject factor. We set the significance level to α = 0.05, and to account for potential bias from multiple comparisons, we applied the Bonferroni correction for our 13 dependent variables. Thus, our adjusted familywise error rate was 0.004 (α = 0.05/13) at the individual outcome level. Lastly, for statistically significant outcomes, we reported effect sizes as partial eta-squared (ηp2) with small, medium, and large effect sizes classified as 0.01, 0.06, and 0.14, respectively.59 We reported means and associated standard deviations for all outcomes. Notably, we a priori decided to report any clinically meaningful imbalances we observed between groups and perform sensitivity analyses with these variable(s) as covariate(s) in our ANOVAs.
3. Results
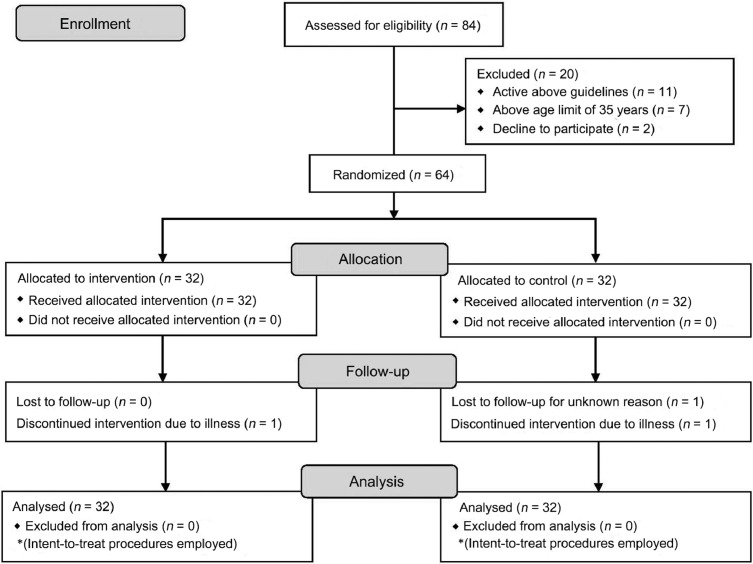
3.1. Participant flow through the trial
Participant flow through the trial is shown in Fig. 2. Briefly, 84 young adults expressed interest and were screened for study participation, 64 of whom were deemed eligible (reasons for ineligibility at each stage of recruitment are shown in Fig. 2). Thus, 64 participants completed baseline testing and randomization. Retention was 96.9% in the experimental group and 93.8% in the comparison group. One experimental group participant dropped out for reasons unrelated to the study (illness) and 2 dropouts from the control group were due to loss of contact and illness.
Fig. 2.
CONSORT flow diagram.
3.2. Baseline participant characteristics
Descriptive statistics for participants’ baseline characteristics by group are shown in Table 1. We observed no clinically meaningful baseline differences between groups for participant demographics and therefore determined our randomization procedures to be robust. Accordingly, we did not perform any covariate analyses. Additionally, we determined dropouts’ baseline data were not materially different from completers’ baseline data and, thus, proceeded with the planned imputation procedures. Overall, the sample was healthy (X̅BMI = 23.1 kg/m2), 100% used YouTube prior to the study, and the primary device used for consuming YouTube was a smart phone (78.1%). Notably, 56.2% of participants reported using YouTube very often (i.e., daily), 34.4% reported often (i.e., a few times per week), 7.8% reported sometimes (i.e., a few times per month), and 1.6% reported rarely (i.e., a few times per year). The primary recruitment strategy was email (90.6%), followed by word of mouth. Lastly, 62.5% and 68.8% of intervention and control participants, respectively, reported that COVID-19 had made them “less active”, 9.4% and 12.5% reported “more active”, and 28.1% and 18.7% reported “no difference”.
3.3. Primary outcome
All assumptions for ANOVA were met for our outcomes. We therefore proceeded with the planned analysis. Table 2 shows the descriptive statistics for our primary outcome at baseline and 12-week follow-up. Notably, all outcomes were analyzed at the adjusted p < 0.004 level. Briefly, our primary analysis showed a significant interaction effect (group × time) for MVPA (F(1, 62) = 21.65, p < 0.001, ηp2 = 0.26) such that the intervention group's MVPA significantly increased after 12 weeks as compared to that of the control group.
Table 2.
Primary and secondary outcomes by groups at baseline and 12 weeks.
| Group | Baseline | 12 weeks | p | ηp2 | |
|---|---|---|---|---|---|
| Primary outcome | |||||
| MVPA (min/day)* | Intervention Control |
8.28 ± 6.47 9.16 ± 7.01 |
22.75 ± 9.32 7.75 ± 6.83 |
<0.001 | 0.26 |
| Secondary outcome | |||||
| LPA (min/day) | Intervention Control |
183.11 ± 42.19 192.17 ± 48.79 |
203.28 ± 43.33 193.47 ± 39.11 |
0.16 | |
| SB (min/day) | Intervention Control |
688.02 ± 88.58 675.86 ± 65.38 |
658.92 ± 71.82 696.16 ± 114.55 |
0.16 | |
| Sleep duration (h/night) | Intervention Control |
7.99 ± 0.82 8.07 ± 0.74 |
8.07 ± 0.75 7.84 ± 1.41 |
0.30 | |
| Sleep efficiency (%)* | Intervention Control |
84.62 ± 7.12 86.69 ± 5.99 |
88.44 ± 4.83 85.88 ± 6.68 |
<0.001 | 0.25 |
| Muscle-strengthening PA (day/week)* | Intervention Control |
0.81 ± 0.86 0.94 ± 1.06 |
3.28 ± 1.33 0.81 ± 0.86 |
<0.001 | 0.56 |
| SDT-related intrinsic motivation | |||||
| Non-regulation* | Intervention Control |
0.42 ± 0.43 0.51 ± 0.53 |
0.18 ± 0.40 0.63 ± 0.55 |
<0.001 | 0.17 |
| External regulation | Intervention Control |
1.30 ± 0.95 1.18 ± 0.98 |
1.18 ± 0.82 1.35 ± 0.93 |
0.61 | |
| Introjected regulation | Intervention Control |
2.68 ± 0.94 2.50 ± 0.97 |
2.46 ± 1.00 2.58 ± 0.86 |
0.13 | |
| Identified regulation | Intervention Control |
2.96 ± 0.63 2.98 ± 0.61 |
3.18 ± 0.49 3.00 ± 0.61 |
0.06 | |
| Integrated regulation* | Intervention Control |
2.21 ± 0.92 2.32 ± 0.60 |
2.55 ± 0.96 2.19 ± 0.54 |
0.002 | 0.15 |
| Intrinsic regulation* | Intervention Control |
2.48 ± 0.96 2.38 ± 0.83 |
3.05 ± 0.88 2.09 ± 0.73 |
<0.001 | 0.37 |
| Perceived PA barriers* | Intervention Control |
2.33 ± 0.39 2.25 ± 0.40 |
1.58 ± 0.31 2.40 ± 0.29 |
<0.001 | 0.70 |
Notes: We applied the Bonferroni correction to account for possible bias from multiple comparisons. Significance level was set to p < 0.05, and the adjusted familywise error rate at the individual outcome level for 13 comparisons was p < 0.004. All categorical variable values are frequency or n. All continuous variable values are mean ± SD.
* p < 0.004, statistically significantly difference between groups in favor of the intervention group.
Abbreviations: BMI = body mass index; LPA = light physical activity; MVPA = moderate-to-vigorous physical activity; PA = physical activity; SB = sedentary behavior; SDT = self-determination theory.
3.4. Secondary outcomes
Table 2 shows the descriptive statistics for our secondary outcomes at baseline and 12-week follow-up. We observed a significant interaction effect for sleep efficiency (F(1, 62) = 21.06, p < 0.001, ηp2 = 0.25), which indicated that intervention group participants significantly increased their sleep efficiency after 12 weeks compared to the control group. Further, we observed a significant interaction effect for muscle-strengthening PA frequency (F(1, 62) = 77.67, p < 0.001, ηp2 = 0.56), which indicated intervention group participants significantly increased their frequency at the 12-week follow-up compared to the control group. We observed no statistically significant between-group differences after 12 weeks for SB, LPA, and sleep duration (F(1, 62) = 1.11–2.04, p = 0.16–0.30). Regarding the 6 subgroups of SDT-related PA motivation, we observed statistically significant interaction effects for non-regulation (F(1, 62) = 13.06, p < 0.001, ηp2 = 0.17), integrated regulation (F(1, 62) = 10.75, p = 0.002, ηp2 = 0.15), and intrinsic regulation (F(1, 62) = 35.59, p < 0.001, ηp2 = 0.37), such that intervention group participants’ motivational states significantly decreased in amotivation and increased in integrated and intrinsic regulation states after 12 weeks compared to the control group. Lastly, we observed a statistically significant interaction effect for perceived PA barriers (F(1, 62) = 146.60, p < 0.001, ηp2 = 0.70), such that only participants in the intervention group significantly decreased their perceived PA barriers after 12 weeks. We observed no statistically significant between-group differences after 12 weeks for external and identified regulations (F(1, 62) = 3.61–3.64, p = 0.06–0.61).
3.5. Adverse events
No adverse events related to the intervention were reported in either study group during the study. However, 1 participant dropped out mid-intervention due to contracting COVID-19.
4. Discussion
Our study examined the effectiveness of a home-based, YouTube video-delivered PA promotion intervention grounded in SDT for improving young adults’ free-living aerobic and muscle-strengthening PA, SB, sleep quality, SDT-related PA motivation, and perceived PA barriers. We observed statistically significant improvements in free-living MVPA, muscle-strengthening PA frequency, sleep efficiency, SDT-related PA motivation, and perceived PA barriers after 12 weeks in the intervention group. We observed no statistically significant interaction effects for LPA, SB, or sleep duration after 12 weeks, and we observed no statistically significant main effects for time for any outcome in the control group.
Congruent with our hypothesis, participants in the intervention group significantly improved their free-living MVPA after 12 weeks. We believe the intervention group's post-intervention increases in MVPA were a result of their more internally-regulated motivational states (e.g., significantly decreased non-regulation and increased integrated and intrinsic regulation) as well as their significantly decreased perceived PA barriers. Regarding SDT-related motivation, as postulated by SDT,41 we methodically embedded video components that aimed to progress participants’ motivational states from less to more internally-regulated forms by targeting this group's 3 basic psychological needs: (1) competence (e.g., videos taught participants the risks of high SB and low PA levels and the benefits of achieving the PA guidelines with B-roll visually demonstrating how to achieve these guidelines); (2) autonomy (e.g., videos used B-roll to visually demonstrate more and less intense exercise varieties to allow participants to choose which version to perform based on their level of physical fitness); and (3) relatedness (e.g., videos overlaid the A-roll with B-roll that visually demonstrated partner exercises, thereby encouraging participants to perform these exercises/workouts with a friend or family member who they felt safe to exercise around). Given that young adults have been observed to be less intrinsically motivated to perform PA in the home setting without commercial exercise equipment,46 we purport that SDT's well-documented ability to improve habitual PA behaviors60 facilitated the observed changes in MVPA among the intervention group. Notably, although not statistically significant at the adjusted significance level, SB decreased by an average of 30 min per day in the intervention group after 12 weeks, which we believe is practically significant. Because we observed significant changes in MVPA but no significant changes in LPA, we believe that intervention participants replaced some of their SB time with MVPA, shifts which both have clinically meaningful implications independent of one another.1 Additionally, we leveraged our videos to create pre-recorded high-intensity interval training workouts focusing on full-body exercises that participants could seamlessly follow along to on-screen and perform with the study investigators. Indeed, high-intensity interval training requires maximal or near-maximal effort and has demonstrated effectiveness in an RCT61 to improve adults’ cardiorespiratory fitness in only 4 weeks. Therefore, we believe performing these workouts weekly greatly contributed to the increased MVPA levels among the intervention group.
Likewise, we observed that participants in the intervention group significantly improved their muscle-strengthening PA frequency after 12 weeks, whereas those in the control group demonstrated no changes in this outcome. Notably, participants in the intervention group increased their average muscle-strengthening PA frequency from less than 1 day per week (i.e., below the recommended guideline of ≥2 days per week) to over 3 days per week (i.e., exceeding the recommended guideline). Again, we believe the use of video, and particularly B-roll within the intervention videos, helped improve participants’ physical literacy—a major barrier to muscle-strengthening PA in this population.37,38,62 Also contributing to improved physical literacy was the videos’ use of different camera angles and exercise variations based on one's muscular fitness level, which allowed participants to see how to properly perform these exercises. Being confined to the home during the COVID-19 pandemic without familiar commercial exercise equipment not only affects autonomous motivation to engage in muscle-strengthening activities like resistance-training,46 but was likely also a perceived muscle-strengthening PA barrier. However, assuming exercise intensity is near-maximal, one's own bodyweight is sufficient to induce favorable musculoskeletal adaptations (e.g., muscular strength and hypertrophy).63,64 Therefore, our muscle-strengthening-oriented videos promoted various methods of enhancing resistance-training workout intensity like adding general household items to exercises to increase the working load (e.g., wearing a loaded backpack during squats to train the legs, holding filled laundry soap containers to perform lateral raises for the shoulders) and introducing various resistance-training techniques like eccentric-focused training, wherein the emphasis is placed on muscle lengthening (or eccentric muscle actions) for longer periods of time. Moreover, not only did we teach the intervention participants the muscle-strengthening recommendations and provide on-screen demonstrations of full-body resistance-training workouts employing various training techniques to increase workout intensity, but we also encouraged participants to perform these activities multiple times per week and provided them with high-quality PDF files with the written workouts so they could download and readily access them when they planned to perform the resistance-training workout(s) later in the week. Thus, in the absence of commercial gym equipment in the home setting, pre-recorded YouTube videos that teach the muscle-strengthening PA guidelines and demonstrate exercises and workouts using the above strategies could effectively improve muscle-strengthening PA participation, which has a myriad of physical and mental health benefits independent of aerobic PA participation,65,66 including improved depressive symptoms,67 which may be especially important for young adults during the COVID-19 pandemic.16
Also in line with our hypotheses, only the intervention participants significantly improved their sleep efficiency despite no changes in either group for total sleep duration. The observed increases in sleep efficiency were likely attributed to the observed decreases in this group's SB and increases in aerobic and muscle-strengthening PA levels. These findings are consistent with other findings among young adults demonstrating that there is an inverse relationship between SB and sleep efficiency.68 Likewise, a growing body of research has demonstrated that increased PA levels improve adults’ sleep quality. Thus, the concurrent decreases in SB and increases in PA among the intervention group—especially that of moderate- and vigorous-intensities—lead to significantly improved sleep efficiency. Interestingly, despite the preceding improvements in sleep efficiency among the intervention group, we observed no differences in sleep duration in either group. Also to our surprise, average sleep duration in both groups was high (about 8 h/night) despite research demonstrating poor sleep behaviors among this population during the pandemic.16,17 We believe that because the majority of our sample were college students, the winter break—and therefore lack of school responsibilities—was responsible for the high sleep durations in both groups. Nevertheless, the ability for participants in the intervention group to fall asleep faster and, thus, get more quality sleep, may have great public health implications7 regarding their physical health,8,9 as well as daytime productivity and being able to contribute to society.10 Therefore, the use of video to deliver remote, home-based PA, SB, and aerobic and muscle-strengthening information/workouts not only directly improves participants’ PA behaviors but also indirectly affects individuals’ sleep quality, both of which have major public health implications during the COVID-19 pandemic and beyond.
Our study had several strengths. First, our sufficiently-powered RCT allowed us to examine causal relationships between the independent and dependent outcome variables between homogonous groups of young adults. Second, we employed device-based measurements for our primary PA and sleep quality outcomes as well as valid and reliable questionnaires for our muscle-strengthening PA and psychosocial outcomes. Lastly, our intervention videos were based on formative assessments among young adults, an empirically-based content analysis and principles of health videos,36 and were grounded in a single behavior change theory (SDT), which has been observed to be more effective for PA behavior change than multi-theory interventions.34,35 However, despite the preceding strengths, our study had some limitations that must be addressed.
First, we employed a self-reported muscle-strengthening PA assessment, which may have been prone to response bias. Nevertheless, this item has demonstrated good validity and reliability among adults and is currently the only viable option for this assessment given objective, device-based assessments for muscle-strengthening PA are not available. Second, we were unable to employ long-term follow-up assessments and examine the long-term effectiveness of this intervention. Third, in an effort to maximize ecological validity (i.e., have participants consume the intervention YouTube videos as they would in the real world), internal validity may have been compromised insofar as we did not directly assess intervention adherence. Fourth, given our sample was primarily female, this may have influenced the results to some degree and, therefore, future studies should aim to recruit an equal distribution of male and female participants. Lastly, our study was conducted in the middle of the COVID-19 pandemic wherein participants were facing enacted regulations to reduce the transmission of COVID-19 (e.g., home quarantine) and, thus, it remains unknown if this intervention will effectively improve PA behaviors during the post-pandemic era with lifted restrictions (e.g., no home confinement, access to commercial fitness centers). Similarly, given these special circumstances, participants may have had more time on their hands than usual, and it remains unknown if the observed results would be replicated during pre-pandemic conditions. Likewise, our intervention was conducted in the state of Minnesota during the winter season wherein temperatures are consistently freezing. Participants in both groups may have been more motivated to engage in outdoor PA during the warmer spring/summer months. Thus, post-pandemic research should employ similar interventions in warmer climate regions and/or during warmer seasons and with longer follow-up periods and more representative samples.
5. Conclusion
Our findings indicated that a remote, home-based, YouTube video-delivered PA intervention grounded in SDT significantly improved young adults’ free-living MVPA, muscle-strengthening PA, and sleep efficiency, which was likely a result of the intervention's positive effects on participants’ self-determined motivation for PA and decreased perceived barriers to PA. Thus, with COVID-19 still prevalent in the United States and with uncertainty regarding young adults’ preferred PA behaviors and environments in the post-pandemic era, remote, home-based interventions utilizing SDT-grounded, pre-recorded videos demonstrating PA promotion, SB reduction, and aerobic and muscle-strengthening exercise routines have emerged as an effective intervention strategy for reducing PA barriers and facilitating more autonomous forms of PA motivation to help combat the compounding effects of the COVID-19 pandemic on the preexisting pandemic of PA and poor sleep quality in the United States.
Also noteworthy is that these interventions are cost-effective for both researchers (e.g., content can be filmed using a smart phone and uploaded for free to YouTube) and participants (e.g., YouTube content is free to consume) and have mass-reach capabilities. Indeed, additional video-based PA platforms like YouTube are rapidly emerging, including Apple's “Apple Fitness +” and video-delivered exercise routines through commercial gyms. Therefore, we encourage qualified health professionals to utilize these findings and remotely disseminate video-based PA interventions using high-traffic video platforms like YouTube.
Acknowledgments
This study was funded by DJM's Doctoral Dissertation Fellowship through the University of Minnesota as well as DJM's Professional Development Grant through the University of Minnesota's School of Kinesiology.
Authors’ contributions
DJM conceived the study idea, conducted statistical analyses, drafted the manuscript, and created/edited the study videos; MAH was the subject for all talking-head (“A-roll”) video clips for the intervention and control groups, performed randomization and group allocation, created content for the general health education control group, and oversaw all other managerial tasks; WL facilitated the analyses for raw PA and sleep data and edited and revised the manuscript; ZG helped conceive the study idea, edited and revised the manuscript, and provided the accelerometers. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Acknowledgments
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2021.07.009.
Supplementary materials
References
- 1.Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bennie JA, De Cocker K, Teychenne MJ, Brown WJ, Biddle SJH. The epidemiology of aerobic physical activity and muscle-strengthening activity guideline adherence among 383,928 U.S. adults. Int J Behav Nutr Phys Act. 2019;16:34. doi: 10.1186/s12966-019-0797-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kohl 3rd HW, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: Global action for public health. The Lancet. 2012;380:294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- 4.Ding D, Lawson KD, Kolbe-Alexander TL, et al. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. The Lancet. 2016;388:1311–1324. doi: 10.1016/S0140-6736(16)30383-X. [DOI] [PubMed] [Google Scholar]
- 5.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. The Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: A meta-analytic review. J Behav Med. 2015;38:427–449. doi: 10.1007/s10865-015-9617-6. [DOI] [PubMed] [Google Scholar]
- 7.Falck RS, Stamatakis E, Liu-Ambrose T. The athlete's sleep paradox prompts us to reconsider the dose–response relationship of physical activity and sleep. Br J Sports Med. 2021;55:887–888. doi: 10.1136/bjsports-2020-103835. [DOI] [PubMed] [Google Scholar]
- 8.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15:42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gallicchio L, Kalesan B. Sleep duration and mortality: A systematic review and meta-analysis. J Sleep Res. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 10.Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J. The economic burden of insomnia: Direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32:55–64. [PMC free article] [PubMed] [Google Scholar]
- 11.Jurak G, Morrison SA, Leskošek B, et al. Physical activity recommendations during the coronavirus disease-2019 virus outbreak. J Sport Health Sci. 2020;9:325–327. doi: 10.1016/j.jshs.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9:103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu W. Should, and how can, exercise be done during a coronavirus outbreak? An interview with Dr. Jeffrey A. Woods. J Sport Health Sci. 2020;9:105–107. doi: 10.1016/j.jshs.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sallis JF, Adlakha D, Oyeyemi A, Salvo D. An international physical activity and public health research agenda to inform coronavirus disease-2019 policies and practices. J Sport Health Sci. 2020;9:328–334. doi: 10.1016/j.jshs.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis. 2021;64:108–110. doi: 10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huckins JF, daSilva AW, Wang W, et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. J Med Internet Res. 2020;22:e20185. doi: 10.2196/20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marelli S, Castelnuovo A, Somma A, et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2021;268:8–15. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaushal N, Keith N, Aguiñaga S, Hagger MS. Social cognition and socioecological predictors of home-based physical activity intentions, planning, and habits during the COVID-19 Pandemic. Behav Sci (Basel) 2020;10:133. doi: 10.3390/bs10090133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Denay KL, Breslow RG, Turner MN, Nieman DC, Roberts WO, Best TM. ACSM call to action statement: COVID-19 considerations for sports and physical activity. Curr Sports Med Rep. 2020;19:326–328. doi: 10.1249/JSR.0000000000000739. [DOI] [PubMed] [Google Scholar]
- 20.Pew Research. Share of U.S. adults using social media, including Facebook, is mostly unchanged since 2018. Available at: https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018/. [accessed 21.12.2019].
- 21.Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15:e85. doi: 10.2196/jmir.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams G, Hamm MP, Shulhan J, Vandermeer B, Hartling L. Social media interventions for diet and exercise behaviours: A systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2013-003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alley S, Jennings C, Persaud N, Plotnikoff RC, Horsley M, Vandelanotte C. Do personally tailored videos in a web-based physical activity intervention lead to higher attention and recall? An eye-tracking study. Front Public Health. 2014;2:13. doi: 10.3389/fpubh.2014.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vandelanotte C, Alley S, Persaud N, Horsely M. In: Current trends in eye tracking research. Horsley M, Toon N, Knight BA, Reilly R, editors. Springer; Cham: 2014. Comparing personally tailored video- and text-delivered web-based physical activity interventions—the medium and the message: An eye-tracking study. [Google Scholar]
- 25.Vernon J. Video marketing stats every business should know for 2018. Available at: https://marketinghy.com/2017/09/video-marketing-stats-every-business-know-2018/. [accessed 26.03. 2019].
- 26.Zenith. Global Intelligence Issue 05 2018. Available at: https://www.zenithmedia.com/insights/global-intelligence-issue-05-2018/. [accessed 11.03.2021].
- 27.Sweller J. Cognitive load theory, learning difficulty, and instructional design. Learn Instr. 1994;4:295–312. [Google Scholar]
- 28.Soetens KC, Vandelanotte C, de Vries H, Mummery KW. Using online computer tailoring to promote physical activity: A randomized trial of text, video, and combined intervention delivery modes. J Health Commun. 2014;19:1377–1392. doi: 10.1080/10810730.2014.894597. [DOI] [PubMed] [Google Scholar]
- 29.Smith A, Anderson M. Social media use in 2018. Available at: https://www.pewinternet.org/2018/03/01/social-media-use-in-2018/. [accessed 26.03. 2019].
- 30.Smith C. 160 YouTube statistics and facts (2019). Available at: https://expandedramblings.com/index.php/youtube-statistics/. [accessed 26.03.2019].
- 31.Walthouwer MJ, Oenema A, Lechner L, de Vries H. Use and effectiveness of a video- and text-driven web-based computer-tailored intervention: Randomized controlled trial. J Med Internet Res. 2015;17:e222. doi: 10.2196/jmir.4496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walthouwer MJ, Oenema A, Lechner L, de Vries H. Comparing a video and text version of a web-based computer-tailored intervention for obesity prevention: A randomized controlled trial. J Med Internet Res. 2015;17:e236. doi: 10.2196/jmir.4083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vandelanotte C, Short CE, Plotnikoff RC, et al. Are web-based personally tailored physical activity videos more effective than personally tailored text-based interventions? Results from the three-arm randomised controlled TaylorActive trial. Br J Sports Med. 2021;55:336–343. doi: 10.1136/bjsports-2020-102521. [DOI] [PubMed] [Google Scholar]
- 34.Gourlan M, Bernard P, Bortolon C, et al. Efficacy of theory-based interventions to promote physical activity. A meta-analysis of randomised controlled trials. Health Psychol Rev. 2016;10:50–66. doi: 10.1080/17437199.2014.981777. [DOI] [PubMed] [Google Scholar]
- 35.Prestwich A, Sniehotta FF, Whittington C, Dombrowski SU, Rogers L, Michie S. Does theory influence the effectiveness of health behavior interventions? Meta-analysis. Health Psychol. 2014;33:465–474. doi: 10.1037/a0032853. [DOI] [PubMed] [Google Scholar]
- 36.Bopp T, Vadeboncoeur JD, Stellefson M, Weinsz M. Moving beyond the gym: A content analysis of YouTube as an information resource for physical literacy. Int J Environ Res Public Health. 2019;16:3335. doi: 10.3390/ijerph16183335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilson OWA, Papalia Z, Duffey M, Bopp M. Differences in college students' aerobic physical activity and muscle-strengthening activities based on gender, race, and sexual orientation. Prev Med Rep. 2019;16 doi: 10.1016/j.pmedr.2019.100984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fairchild Saidi G, Branscum P. Gender differences for theory-based determinants of muscle-strengthening physical activity in college-aged students: A moderation analysis. Transl Behav Med. 2020;10:781–791. doi: 10.1093/tbm/ibz058. [DOI] [PubMed] [Google Scholar]
- 39.Korda H, Itani Z. Harnessing social media for health promotion and behavior change. Health Promot Pract. 2013;14:15–23. doi: 10.1177/1524839911405850. [DOI] [PubMed] [Google Scholar]
- 40.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12:e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 42.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother. 2010;1:100–107. doi: 10.4103/0976-500X.72352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.World Medical Association World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organization. Cleaning and disinfection of environmental surfaces in the context of COVID-19: Interim guidance. Available at: https://www.who.int/publications/i/item/cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19. [accessed 09.04.2021].
- 45.Journal of the American Medical Association. Instructions for authors. Guidelines for optimal video quality. Available at: https://jamanetwork.com/journals/jama/pages/instructions-for-authors. [accessed 09.04.2021].
- 46.Schwendinger F, Pocecco E. Counteracting physical inactivity during the COVID-19 pandemic: Evidence-based recommendations for home-based exercise. Int J Environ Res Public Health. 2020;17:3909. doi: 10.3390/ijerph17113909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McDonough DJ, Su X, Gao Z. Health wearable devices for weight and BMI reduction in individuals with overweight/obesity and chronic comorbidities: Systematic review and network meta-analysis. Br J Sports Med. 2021;55:917–925. doi: 10.1136/bjsports-2020-103594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dillon CB, Fitzgerald AP, Kearney PM, et al. Number of days required to estimate habitual activity using wrist-worn GENEActiv accelerometer: A cross-sectional study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0109913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Migueles J, Rowlands A, Huber F, et al. GGIR: A research community-driven open source R package for generating physical activity and sleep outcomes from multi-day raw accelerometer data. J Meas Phys Behav. 2019;2:188–196. [Google Scholar]
- 50.Hildebrand M, VAN Hees VT, Hansen BH, Ekelund U. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med Sci Sports Exerc. 2014;46:1816–1824. doi: 10.1249/MSS.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 51.van Hees VT, Sabia S, Anderson KN, et al. A novel, open access method to assess sleep duration using a wrist-worn accelerometer. PLoS One. 2015;10 doi: 10.1371/journal.pone.0142533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dankel SJ, Loenneke JP, Loprinzi PD. The individual, joint, and additive interaction associations of aerobic-based physical activity and muscle strengthening activities on metabolic syndrome. Int J Behav Med. 2016;23:707–713. doi: 10.1007/s12529-016-9570-y. [DOI] [PubMed] [Google Scholar]
- 53.Bennie JA, Lee DC, Khan A, et al. Muscle-strengthening exercise among 397,423 U.S. adults: Prevalence, correlates, and associations with health conditions. Am J Prev Med. 2018;55:864–874. doi: 10.1016/j.amepre.2018.07.022. [DOI] [PubMed] [Google Scholar]
- 54.Wilson PM, Rodgers WM, Loitz CC, Scime G. “It's who I am…really!” The importance of integrated regulation in exercise contexts. J Biobehav Res. 2006;11:79–104. [Google Scholar]
- 55.Mullan E, Markland D, Ingledew DK. A graded conceptualisation of self-determination in the regulation of exercise behaviour. Pers Individ Differ. 1997;23:745–752. [Google Scholar]
- 56.Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sechrist KR, Walker SN, Pender NJ. Development and psychometric evaluation of the exercise benefits/barriers scale. Res Nurs Health. 1987;10:357–365. doi: 10.1002/nur.4770100603. [DOI] [PubMed] [Google Scholar]
- 58.Pope ZC, Barr-Anderson DJ, Lewis BA, Pereira MA, Gao Z. Use of wearable technology and social media to improve physical activity and dietary behaviors among college students: A 12-week randomized pilot study. Int J Environ Res Public Health. 2019;16:3579. doi: 10.3390/ijerph16193579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Richardson JTE. Eta squared and partial eta squared as measures of effect size in educational research. Rev Educ Res. 2011;6:135–147. [Google Scholar]
- 60.Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: A systematic review. Int J Behav Nutr Phys Act. 2012;9:78. doi: 10.1186/1479-5868-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Menz V, Marterer N, Amin SB, Faulhaber M, Hansen AB, Lawley JS. Functional vs. running low-volume high-intensity interval training: Effects on VO2max and muscular endurance. J Sports Sci Med. 2019;18:497–504. [PMC free article] [PubMed] [Google Scholar]
- 62.Rhodes RE, Lubans DR, Karunamuni N, Kennedy S, Plotnikoff R. Factors associated with participation in resistance training: A systematic review. Br J Sports Med. 2017;51:1466–1472. doi: 10.1136/bjsports-2016-096950. [DOI] [PubMed] [Google Scholar]
- 63.Schoenfeld BJ, Grgic J, Ogborn D, Krieger JW. Strength and hypertrophy adaptations between low- vs. high-load resistance training: A systematic review and meta-analysis. J Strength Cond Res. 2017;31:3508–3523. doi: 10.1519/JSC.0000000000002200. [DOI] [PubMed] [Google Scholar]
- 64.Schoenfeld BJ, Peterson MD, Ogborn D, Contreras B, Sonmez GT. Effects of low- vs. high-load resistance training on muscle strength and hypertrophy in well-trained men. J Strength Cond Res. 2015;29:2954–2963. doi: 10.1519/JSC.0000000000000958. [DOI] [PubMed] [Google Scholar]
- 65.Maestroni L, Read P, Bishop C, et al. The benefits of strength training on musculoskeletal system health: Practical applications for interdisciplinary care. Sports Med. 2020;50:1431–1450. doi: 10.1007/s40279-020-01309-5. [DOI] [PubMed] [Google Scholar]
- 66.El-Kotob R, Ponzano M, Chaput JP, et al. Resistance training and health in adults: An overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(Suppl. 2):S165–S179. doi: 10.1139/apnm-2020-0245. [DOI] [PubMed] [Google Scholar]
- 67.Gordon BR, McDowell CP, Hallgren M, Meyer JD, Lyons M, Herring MP. Association of efficacy of resistance exercise training with depressive symptoms: Meta-analysis and meta-regression analysis of randomized clinical trials. JAMA Psychiatry. 2018;75:566–576. doi: 10.1001/jamapsychiatry.2018.0572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu W, Yuan Q, Zeng N, et al. Relationships between college students’ sedentary behavior, sleep quality, and body mass index. Int J Environ Res Public Health. 2021;18:3946. doi: 10.3390/ijerph18083946. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.