Supplemental Digital Content is available in the text.
Introduction:
The transition from high school to postsecondary education can be challenging for adolescents and young adults (AYAs) with chronic health conditions. AYAs with hemoglobinopathies, including sickle cell disease, are a particularly vulnerable group whose academic performance is impacted by unpredictable disease symptoms. AYA with hemoglobinopathies may require academic accommodations to promote postsecondary success; however, accessing appropriate supports can be complicated.
Methods:
Given these complexities, a multidisciplinary team in a pediatric outpatient clinic designed and implemented a standardized intervention to support AYA with hemoglobinopathies in navigating the transition to postsecondary education. A quality improvement (QI) project was initiated to support the referral of all eligible patients with hemoglobinopathies to postsecondary accessibility offices. This article will describe the development of the intervention and present key findings from qualitative interviews with patients (ages 18−19) and postsecondary accessibility office staff about the implemented resources as an initial step of an ongoing QI project. We used thematic analysis to identify themes across interviews with both groups of stakeholders.
Results:
Key themes across both groups of interviews highlighted the benefits of the intervention, including (1) knowledge of available services, (2) registering early with appropriate documentation, and (3) self-advocacy.
Conclusions:
The preliminary qualitative findings validate the importance of embedding discussions about the transition to postsecondary education into routine clinic appointments for AYA with chronic health conditions. Clinical implications of this ongoing QI project for health care providers working with AYA with chronic health conditions will be shared.
INTRODUCTION
The transition from high school to postsecondary education for adolescents and young adults (AYAs) with chronic health conditions occurs during a developmental period associated with psychosocial issues, mental health concerns, and poor health outcomes.1–3 AYAs with chronic health conditions experience multiple life transitions simultaneously, including transferring from pediatric to adult health services.4 AYAs with hemoglobinopathies, including sickle cell disease (SCD), are a particularly vulnerable group due to the unpredictable nature of symptoms and increased morbidity and mortality rates around the transfer to adult services.5,6
SCD-related complications, including pain episodes, cognitive impairment, and frequent hospitalizations, have been shown to impact academic performance and attendance.7–9 At the juncture of transition from high school to postsecondary education, poor school performance can be particularly stressful for AYA if adequate planning has not occurred.10 In one study, 60% of 12-20 year olds with SCD reported that the disease interfered with school, and 40% had repeated a grade.11 Additionally, adolescents with SCD who experienced more frequent hospitalizations reported lower grades.11 In the same study, 57% of participants endorsed that they would be interested in obtaining educational support interventions, including college application assistance.11
To support AYA in transitioning from pediatric to adult health care, centers have developed transition programs for various chronic health conditions that offer holistic, person-centered interventions.12 Given that enrollment in postsecondary education/training is an indicator of a successful transition, Betz and Smith13 recommended that these programs offer vocational/educational resources. However, there is a lack of literature on how health care providers (HCPs) can operationalize these concepts in busy clinical settings.
Individuals with chronic health conditions in Canada have the right to receive academic accommodations to ensure that their health does not impede their ability to succeed in achieving their goals.14 Every publicly funded postsecondary institution in Ontario has an accessibility office (AO) whose mandate is to support students with disabilities.14 Accessibility includes ensuring that those with absenteeism due to chronic health issues are given supports to obtain access to educational material and are not penalized for absenteeism due to their health-related concern.15 In Canada, the Charter of Rights and Freedoms governs the accommodation of students with disabilities/chronic conditions. However, each postsecondary institution is responsible for developing its process for delivering services and meeting its students’ needs.14
Although postsecondary institutions must accommodate students with disabilities, the process for accessing supports can be complicated.14 Registration often consists of multiple steps that can be challenging to navigate, particularly for those whose diagnoses impact executive functioning.16 Additionally, AOs may not have an in-depth understanding of symptoms or clinical implications of rare genetic disorders, such as SCD, on academic performance.
The implications of disease-related complications on academic performance for AYA with SCD underscore the importance of patients understanding and accessing accommodations in postsecondary institutions to maximize their opportunities for success.8,9 To our knowledge, limited research is available on the postsecondary experiences of AYA with hemoglobinopathies, specifically related to how they access and utilize accommodations and the role of HCPs in facilitating this access. This article will utilize qualitative interview data to describe key stakeholders’ perceptions of an intervention aimed at providing education to patients with hemoglobinopathies about postsecondary accommodations. It is novel and resource-intensive for a pediatric outpatient clinic to systematically deliver this type of patient education and facilitate proactive registration with AO for every patient attending postsecondary education. Qualitative feedback was essential to determine the utility of the intervention in meeting patients’ needs during their first year of postsecondary education, given the resource-intensive nature of this process.
METHODS
Description of Intervention
This quality improvement (QI) project took place within an outpatient hemoglobinopathy clinic at a pediatric tertiary hospital in Ontario, Canada. The clinic provides care to patients aged 0−18 years with hemoglobinopathies, with approximately 55 patients transferring to adult services each year. The multidisciplinary team consists of hematologists, nurse practitioners, clinical nurse specialists, a social worker, and a Transition Navigator (TN). The TN is a masters-educated clinician cross-appointed between pediatric and adult care sites supporting AYA aged 12−20 years with the development of self-management skills and transitioning to adult services.
HCPs in the hemoglobinopathy clinic piloted an intervention to systematically inform AYA with SCD about postsecondary supports during their final pediatric clinic appointments. This intervention was designed using a Plan-Do-Study-Act (PDSA) cycle framework to test, refine, and improve its quality over time.17 Feedback was obtained from 2 groups of stakeholders using qualitative interviews, and the intervention was refined based on this input to improve clinical care. Figure 1 provides an overview of the timeline of the development of the intervention and PDSA cycle.
Fig. 1.
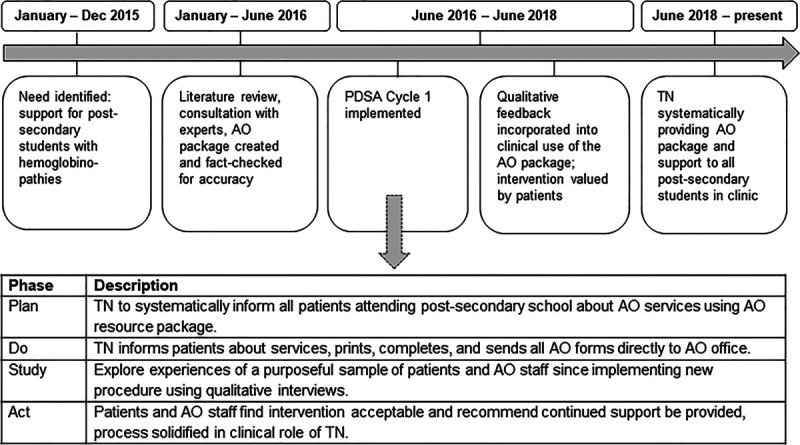
Timeline of quality improvement implementation.
After identifying a clinical need to address postsecondary accessibility in patients with hemoglobinopathies, HCPs with expertise in health care transition conducted an environmental scan. Subsequently, they developed an information package consisting of educational handouts. The package was used to inform AYA with hemoglobinopathies about their rights, documentation requirements for academic accommodations, and financial aid information. A template letter describing the complications of hemoglobinopathies, implications on academic performance, and suggested accommodations was also developed with input from a neuropsychologist and AO advisor. This template letter would supplement all AO registration forms to inform postsecondary institutions about the nature of these chronic health conditions. A physician would sign it.
During the first PDSA cycle (June 2016 to June 2018), the information package and option for postsecondary AO registration support was offered to all patients ages 16−18 years in the hemoglobinopathy clinic. The TN met with each patient entering a postsecondary institution in the next 6−8 months to provide education about relevant resources, assist patients in navigating AO websites, support patients in completing paperwork, and facilitate the delivery of documentation directly to postsecondary AO staff. We modeled this initiative after a similar intervention, which provided systematic screening and referrals to address social determinants of health in brief clinical encounters.18
The intervention’s goal was to reduce barriers for AYA with hemoglobinopathies in connecting with postsecondary supports and obtain feedback from patients and AO staff about the resources. During the “Study” phase of the PDSA cycle, we conducted individual interviews to provide insights about the experience and process of registering for AO services from the patient and staff perspective.
Approval to conduct this qualitative project was obtained following the institution’s QI procedures, including ethical oversight of Quality Improvement Projects. Research ethics board approval was not required.
Participant Recruitment
Purposeful sampling19 was used to recruit patients who had been offered the intervention by the TN and AO staff for interviews about their perceptions of the information package and experiences utilizing it. Recruitment took place from May to July 2018.
Patients
Patients aged 18−19 years with SCD or thalassemia attending postsecondary education were approached at their final pediatric hemoglobinopathy clinic appointment by a clinical team member about the QI evaluation. We invited eligible patients to participate in an interview about their postsecondary experience. Patients completed and signed an agreement to be contacted form, indicating their interest in participating.
Postsecondary AO Staff
Postsecondary AO staff in Ontario were invited via email to participate in an interview about their intake processes, commonly provided accommodations, and to provide feedback on the template letter. We informed staff by email that their participation in this project was voluntary to obtain feedback to better support patients in registering for accommodations.
Data Collection
Semistructured telephone interviews lasting 30−40 minutes were conducted using separate interview guides for each sample of participants, between May and June 2018. Two members of the research team with experience in the transition and disability sectors developed these guides. All interviews were conducted by 1 member of the research team who was not involved in patient care. The team reviewed the study information and obtained verbal consent before proceeding with the interviews.
Data Analysis
The interviews were transcribed, and data analysis was conducted concurrently by 2 members of the research team. The AO staff and patient interviews were analyzed simultaneously; however, codes and themes were extrapolated separately based on the interview participant’s background. We used an inductive approach to thematic analysis to analyze the data.20 The research team read and reread interview transcripts to familiarize themselves with the data. Memos were used to capture striking findings, and the research team began assigning codes to specific pieces of interview data and broader themes emerging from the transcripts. The team collated codes across interview transcripts and categorized them according to overarching themes. We reviewed these themes to ensure an accurate representation of staff and patient perspectives. Themes were further refined across the 2 sets of interviews and discussed among the research team to consolidate the findings. Themes will be described below, with illustrative quotes to exemplify concepts from both sets of participants. Additional supporting quotations from the qualitative interviews with patients and AO staff are available in Table 1, Supplementary Digital Content, http://links.lww.com/PQ9/A209.
Table 1.
Patient Demographics
| Yes % (N) | No % (N) | |
|---|---|---|
| Taking a full course load | 80 (8) | 20 (2) |
| Living in family home | 70 (7) | 30 (3) |
| Experienced health issue during school year | 70 (7) | 30 (3) |
| Hospitalized during school year | 40 (4) | 60 (6) |
| Used accommodations during school year | 50 (5) | 50 (5) |
| Applied for government bursary for students with disabilities | 90 (9) | 10 (1) |
| Received government bursary for students with disabilities | 90 (9) | 10 (1) |
RESULTS
Patient Demographics
A total of 9 young adults with SCD and 1 with thalassemia who had completed at least 1 year of postsecondary education were interviewed. Seventy percent of patients were attending university, and 30% attended college. Further demographic information is given in Table 1.
Staff Demographics
Thirteen AO staff from 11 Ontario colleges/universities were interviewed. Staff caseloads ranged from 100 to 450 students per counselor, and experience levels ranged from 6 months to 30 years. Further demographic characteristics are highlighted in Table 2.
Table 2.
Staff Demographics
| % (N) | |
|---|---|
| Staff education | |
| Masters | 77 (10) |
| Bachelors | 23 (3) |
| Employment status | |
| Full time | 90 (12) |
| Part time | 10 (1) |
| Professional background | |
| Social work | 23 (3) |
| Occupational therapy | 15 (2) |
| Psychology | 15 (2) |
| Education | 15 (2) |
| Other | 32 (4) |
Theme 1: Knowledge of Available Services
Both staff and patient participants highlighted the importance of knowing what services are available for students with chronic conditions and which supports they are eligible for in the postsecondary setting. One staff member stated “It is beneficial for students to know their rights about accommodations, the college has a duty to accommodate legally” (S05). Patients discussed how connecting with the AO allowed them to learn about the services for which they were eligible. One young adult stated “when I had my accessibility office interview they gave me a lot of information and resources about accessibility services and managing health issues at [my school], and I felt like I had a lot more support after the interview than I did before” (P04).
Theme 2: Early Registration with Appropriate Documentation
Participants discussed how registering with the AO in postsecondary institutions requires that a medical professional complete appropriate intake forms to verify an individual's health condition. They discussed the importance of having the correct documentation and registering as early as possible for services. Patients articulated that support with registering with the AO before commencing postsecondary studies was helpful. Ninety percent of patients agreed that registering with the AO alleviated some of the worries they had about starting school with a chronic condition. Furthermore, all 10 patients stated that the TN was the one who informed them of the AO and supported them in completing the medical documentation required for registration.
Regarding the template letter, most AO staff found it “detailed and comprehensive.” Participant S05 stated she would use it “as a jumping-off point for discussion.” Other staff requested “more information as to how this disability is impacting each unique student” (S08). Opinions on the comfort level in supporting students with hemoglobinopathies were mixed. Some staff advocated for “more professional development on [these conditions]” (S02). In contrast, others felt “comfortable meeting with students with all disability types [given they] do [their] research on particular health conditions and focus on the functional impacts” (S04).
Theme 3: Self-advocacy Skills
Developing self-advocacy skills in the postsecondary setting emerged as a common theme. One staff participant discussed the importance of a student’s ability to “describe a day in their life, and describe within the last year, for example, what your condition looks like, what supports were helpful for you” (S09). When asked for advice for future patients with a chronic health condition, 1 patient stated “Self-advocacy—if you feel like you need help, don’t be afraid to ask for it” (P08). Another patient recommended to “use your resources wisely if you get them, use them… don’t use your chronic illness negatively” (P06).
DISCUSSION
This article described key stakeholders’ feedback on an intervention aimed at supporting the referral of all eligible patients with hemoglobinopathies to postsecondary AOs in a tertiary care outpatient clinic. Interviews with staff and patients validated the importance of the information package, the value of providing anticipatory guidance to patients in the pediatric environment, and the template letter’s utility in informing AO staff about complicated medical conditions and their implications on academics.
Patients and AO staff highlighted the benefits of registering proactively for postsecondary accommodations for young people with chronic conditions. This project highlighted that HCPs have an essential “gatekeeper” role to play in this process, given that medical documentation is required for registration and that patients do not necessarily routinely hear about AO from other sources. Registering for accommodations consists of multiple steps and requires an intake meeting with appropriate documentation. Therefore, both stakeholder groups noted the value of an information package, provision of appropriate forms with the opportunity to obtain physician signatures onsite, and step-by-step instructions by a HCP.
AO staff described the consequences of students failing to apply for accommodations early should they experience health crises. They identified that undue stress arises when students apply following a health crisis, as gathering relevant documentation promptly can be challenging. For example, financial and academic consequences can ensue. Our intervention sought to prevent this by proactively assisting patients with completing paperwork and sending the documentation directly to the postsecondary institution. The concept of addressing social determinants of health at routine clinic appointments has been proven effective in facilitating connection to community resources for vulnerable populations.18 In our study, AYA voiced that merely being aware of how to access services should they fall ill during the school year reduced feelings of worry. Stakeholders expressed that self-advocacy skills and patient education about rights were essential, and patients valued having postsecondary discussions with HCPs. These findings align with other studies wherein students with SCD requested postsecondary support from HCPs.11
Given the feedback from patients and staff regarding the importance of early registration with AO, we refined the intervention using the PDSA cycle framework.17 The intervention is now considered one of the core pillars of the TN role rather than a small transition care component. During our first PDSA cycle, it became apparent that patients may have already started school when receiving the intervention, depending on the timing of their final pediatric clinic appointment. Therefore, the TN is actively seeking information by phone/email from eligible patients between appointments about which school they plan to attend so that the appropriate paperwork can be completed in advance. The TN places further emphasis on preparing AYA to communicate with others about how their condition could impact academic performance should complications arise unexpectedly. The template letter is also tailored for patients with complex or specific needs. The TN reviews specific AO websites with patients to highlight essential information that may differ by school and actively monitors changes to application processes for financial aid. This level of specificity was not present before the first PDSA cycle. The TN serves as a bridge and provides patients and staff information about relevant policies, procedures, and accommodations in the postsecondary setting, which may change over time across schools. Subsequently, the TN continues to build professional relationships with AO staff at colleges and universities to maximize collaboration.
A strength of this evaluation was the integration of feedback from both patients and staff. This project is the first to explore the connection between outpatient specialty clinic staff and AO staff to optimize outcomes for a particular patient population. When effective intersectoral collaboration occurs, youth with disabilities have been shown to achieve positive postsecondary education and employment outcomes.21,22 Thus, this project serves as an essential step toward developing role clarity and strengthening partnerships between the health, community, and education sectors to support seamless educational transition planning for youth with chronic conditions. The TN role has been identified as a critical factor in the transition process. It supports patients in navigating multiple life transitions, including the move to adult services and postsecondary education.
Limitations
Interview participant recruitment took place over 2 months. Thus, our sample sizes for both stakeholder groups were small. It was not possible with resourcing available to collect information and report on characteristics of those who were not interviewed to contrast and compare. We interviewed staff from only Ontario postsecondary institutions for this project; thus, processes may differ from other provinces or countries. Given the focus of this preliminary phase of an ongoing QI project on perceptions of the intervention from patients and staff, we did not collect or analyze pre- and postintervention quantitative data, limiting our ability to conclude the effectiveness of the intervention on patient outcomes.
Concluding Summary
This project validated the utility of an intervention intended to improve the process of registering patients with hemoglobinopathies with AOs using qualitative interviews. Quantitative data on patient outcomes pre- and postintervention are needed to determine the impact of this intervention. However, our preliminary findings reveal that this intervention can inform the development of future interventions in similar clinics to support AYAs with hemoglobinopathies as they navigate postsecondary education. It can prevent adverse long-term penalties in academic settings for a population with high rates of morbidity known to interfere with academic performance.11
The hemoglobinopathy team will continue to embed postsecondary accommodation support into routine clinical practice. As this QI project is ongoing, further data collection focused on patient academic outcomes, registration with AO offices, and receipt of financial support, comparing patients before and following the intervention’s implementation, is needed to demonstrate impact. The next steps of this project include a retrospective chart review and prospective data collection to compare outcomes pre- and postintervention across patient cohorts. We recommend that pediatric clinics consider incorporating discussions about postsecondary education into clinical care to support patients with chronic conditions based on positive patient and staff feedback in our qualitative interviews. Further research is needed on AYAs’ experiences with chronic conditions in the postsecondary education setting and intersectoral collaboration throughout this transition.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
ACKNOWLEDGMENTS
The authors acknowledge all of the interview participants for their contributions to this project. The authors thank the patients and staff who took part in interviews and their colleagues in the Good 2 Go Transition Program (Dr. Miriam Kaufman, Dr. Khush Amaria, and Geraldine Cullen-Dean) and the hemoglobinopathy clinics at both the Hospital for Sick Children (Dr. Melanie Kirby, Dr. Isaac Odame, Dr. Suzan Williams, Karen Charpentier, Melina Cheong, Amanda Wagner, Emily Clarke, Manuela Merelles-Pulcini, Marcia Palmer, Carly Nishimura, and Jennifer Davies) and at Toronto General Hospital (Dr. Richard Ward, Dr. Jacob Pendergrast, Dr. Kevin Kuo, Kate Uchendu, Colleen Johnson, and Heather Gordon) for their support, feedback, and guidance throughout this process.
Supplementary Material
Footnotes
Published online September 25, 2020
Preliminary data from this study was presented as a poster at the Chronic Illness and Disability Conference: October 24, 2018, Houston, Tex., as a micro-oral presentation at the Qualitative Health Research Conference: October 29, 2019, Vancouver, British Columbia, Canada, and as an oral presentation at the 4th Biennial Canadian Sickle Cell Conference: November 8, 2018, Ontario, Canada.
This project received grant funding to support a summer nursing student through the Garron Family Cancer Centre Nursing and Allied Health Summer Student Program, Hospital for Sick Children.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Allemang BA, Bradley J, Leone R, Henze M. Transitions to Postsecondary Education in Young Adults with Hemoglobinopathies: Perceptions of Patients and Staff. Pediatr Qual Saf 2020;5:e349.
REFERENCES
- 1.American Diabetes Association. Children and adolescents. Diabetes Care. 2016; 39S86–S93. [DOI] [PubMed] [Google Scholar]
- 2.Klein K, Wheeler M, Yonkaitis CF. College-bound: transition planning strategies for students with type 1 diabetes. NASN Sch Nurse. 2019; 34:17–20. [DOI] [PubMed] [Google Scholar]
- 3.Stollon NB, Paine CW, Lucas MS, et al. Transitioning adolescents and young adults with sickle cell disease from pediatric to adult health care: provider perspectives. J Pediatr Hematol Oncol. 2015; 37:577–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnett JJ. Emerging adulthood: what is it, and what is it good for? Child Dev Perspect. 2007; 1:68–73. [Google Scholar]
- 5.Blinder MA, Vekeman F, Sasane M, et al. Age-related treatment patterns in sickle cell disease patients and the associated sickle cell complications and healthcare costs. Pediatr Blood Cancer. 2013; 60:828–835. [DOI] [PubMed] [Google Scholar]
- 6.Brousseau DC, Owens PL, Mosso AL, et al. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010; 303:1288–1294. [DOI] [PubMed] [Google Scholar]
- 7.Berkelhammer LD, Williamson AL, Sanford SD, et al. Neurocognitive sequelae of pediatric sickle cell disease: a review of the literature. Child Neuropsychol. 2007; 13:120–131. [DOI] [PubMed] [Google Scholar]
- 8.Quinn CT, McKinstry RC, Dowling MM, et al. Acute silent cerebral ischemic events in children with sickle cell anemia. JAMA Neurol. 2013; 70:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwartz LA, Radcliffe J, Barakat LP. Associates of school absenteeism in adolescents with sickle cell disease. Pediatr Blood Cancer. 2009; 52:92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eckes SE, Ochoa TA. Students with disabilities: transitioning from high school to higher education. Am Second Educ J. 2005; 33:6–20. [Google Scholar]
- 11.Crosby LE, Joffe NE, Irwin MK, et al. School performance and disease interference in adolescents with sickle cell disease. Phys Disabil. 2015; 34:14–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stinson J, Kohut SA, Spiegel L, et al. A systematic review of transition readiness and transfer satisfaction measures for adolescents with chronic illness. Int J Adolesc Med Health. 2014; 26:159–174. [DOI] [PubMed] [Google Scholar]
- 13.Betz C, Smith K. Measuring health care transition planning outcomes: challenges and issues. Int J Child Adolesc Health. 2011; 3:463–472. [Google Scholar]
- 14.Ontario Human Rights Commission. The opportunity to succeed: achieving barrier-free education for students with disabilities. Consultation report. http://www.ohrc.on.ca/en/opportunity-succeed-achieving-barrier-free-education-students-disabilities/post-secondary-education. Published 2003. Accessed September 15, 2019.
- 15.Ontario Human Rights Commission. Policy on ableism and discrimination based on disability. http://www.ohrc.on.ca/sites/default/files/Policy%20on%20ableism%20and%20discrimination%20based%20on%20disability_accessible_2016.pdf. Published 2016. Accessed September 15, 2019.
- 16.National Educational Association of Disabled Students. Landscape of accessibility and accommodation in post-secondary education for students with disabilities. https://www.neads.ca/en/about/media/AccessibilityandAccommodation%202018-5landscapereport.pdf. Published in 2018. Accessed September 20, 2019.
- 17.Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014; 23:290–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garg A, Toy S, Tripodis Y, et al. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015; 135:e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palinkas LA, Horwitz SM, Green CA, et al. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015; 42:533–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006; 3:77–101. [Google Scholar]
- 21.Haber MG, Mazzotti VL, Mustian AL, et al. What works, when, for whom, and with whom: a meta-analytic review of predictors of post-secondary success for students with disabilities. Rev Educ Res. 2016; 86:123–162. [Google Scholar]
- 22.Mazzotti VL, Rowe DA, Sinclair J, et al. Predictors of post school success: a systematic review of NLTS2 secondary analyses. Career Dev Transit Except Individ. 2015; 39:196–215. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


