Abstract
The rapid development of safe and effective vaccines against severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) is a necessary response to coronavirus outbreak. Here, we developed PRAK-03202, the world's first triple antigen virus-like particle vaccine candidate, by cloning and transforming SARS-CoV-2 gene segments into a highly characterized S. cerevisiae-based D-Crypt™ platform, which induced SARS CoV-2 specific neutralizing antibodies in BALB/c mice. Immunization using three different doses of PRAK-03202 induced an antigen-specific (spike, envelope, and membrane proteins) humoral response and neutralizing potential. Peripheral blood mononuclear cells from convalescent patients showed lymphocyte proliferation and elevated interferon levels suggestive of epitope conservation and induction of T helper 1-biased cellular immune response when exposed to PRAK-03202. These data support further clinical development and testing of PRAK-03202 for use in humans.
Keywords: Virus like particle, Vaccine, Humoral immune response, Convalescent COVID-19 patients, Electron microscopy
Highlights
-
•
We developed the world's first triple antigen VLP vaccine candidate-PRAK-03202.
-
•
PRAK-03202 can induce neutralizing antibodies against SARS CoV-2.
-
•
PRAK-03202 can induce an IFN-γ response in convalescent patient sera.
-
•
IgG antibody responses against the novel PRAK-03202 persisted for months.
Virus like particle; Vaccine; Humoral immune response; Convalescent COVID-19 patients; Electron microscopy.
1. Introduction
The coronavirus disease (COVID-19) outbreak was declared a public health emergency of international concern on January 30, 2020, and a pandemic on March 11, 2020, by the World Health Organization. As of June 2021, with more than ∼3,840,223 deaths in total and 408,990 new cases each day, it is considered a serious threat to global public health. Although several vaccine candidates have initiated clinical testing, very little is currently known about their long-term humoral response (Hasan et al., 2021). There are also currently no effective therapeutics (Ho et al., 2004), calling for the urgent development of safe and effective therapeutics against COVID-19.
Severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) is an enveloped virus with a positive-strand RNA of 29.9 kb that contains four structural proteins, including the spike, envelope, membrane, and nucleocapsid proteins. Currently, numerous efforts have focused on developing DNA and RNA vaccines to combat COVID-19. However, there are several challenges, including: I) poor immunogenicity; II) single target-oriented approach for the vaccines currently in clinical trials: receptor-binding domain (RBD) or spike protein; III) amounts and duration of protein production; IV) high mutation rate of the spike protein; and V) expenses for ultra-cold chain storage of the vaccines, which all create a bottleneck in the development of an effective COVID-19 vaccine.
While the spike protein has been well documented as a target for developing effective vaccines or drug-mediated therapies, mutations in the spike protein of new emerging variants encourage the inclusion of other structural proteins in vaccine candidates to provide a broader immune response against the variants of SARS CoV-2. Moreover, competition between neutralizing and non-neutralizing epitopes of the spike protein could greatly reduce the host immune response (Du et al., 2016) and increase the chances of failure of single-antigen targeting vaccines. Recent studies have reported the significance of the envelope and membrane proteins as potential vaccine targets against SARS CoV-2 (Bhattacharya et al., 2021; Lopandic et al., 2021).
This study aimed to establish approaches to overcome the abovementioned limitations by producing a virus-like particle (VLP)-based triple antigenic vaccine candidate, PRAK-03202, against COVID-19 to combat this emerging infectious disease. VLPs are composed of multiple viral proteins, but they lack the viral genome. VLPs are structurally identical to the native virus and can display pathogen-associated molecular patterns to the pattern recognition receptors of the host innate immune system to further activate the adaptive immune response (Kumar et al., 2011; Wang and Wang, 2013). Immunization with VLPs has been demonstrated as an effective strategy for vaccine development for respiratory viruses by several research groups, as they bring an apparent improvement in terms of biological safety (Kim et al., 2015; Naskalska et al., 2018; Quan et al., 2020; Syomin and Ilyin, 2019).
We used the D-crypt™ platform to produce PRAK-03202 because of its low risk of contamination by adventitious agents, low production costs, and the ability to produce VLPs with reliable quality and quantity (Arora, 2020). PRAK-03202 immunogenicity in viral neutralizing antibody assays was determined together with the adjuvant effect of alhydrogel (AH). Aluminum-based adjuvants have been widely used in more than 30 licensed vaccines (Di Pasquale et al., 2015) and are the only adjuvant in use for the last 70 years. Recent preclinical studies have shown that AH is associated with protection against SARS-CoV-2 (Gao et al., 2020; Liang et al., 2020).
2. Materials and methods
2.1. Mice
Pathogen-free 6-8 week-old BALB/c mice were maintained in DHITI Life Sciences, India. All animal protocols were approved by the Committee for the Purpose of Control and Supervision of Experiments on Animals (1931/PO/RcBi/S/16/CPCSEA). BALB/c mice (n = 40) were immunized intramuscularly three times with PRAK-03202 within a 14-day interval and categorized into the following eight groups: placebo (0 μg in physiological saline; N = 5), AH only (N = 5), and AH with PRAK-03202 (N = 5/dose; 5, 10, 20, 50, 100, and 150 μg/dose). All immunization experiments were performed using the high-performance liquid chromatography (HPLC)-purified form of PRAK-03202. In addition, the same purified lot of PRAK-03202 was used in all studies.
2.2. Clinical information and serological testing
Patient medical history was collected for information on demographic characteristics, clinical profile including blood biochemistry, lung profile, renal profile, liver profile, and subsequent outcome in case of any reported symptoms and signs. Blood from convalescent patients was fractionated into the sera and peripheral blood mononuclear cells (PBMCs). The study was approved by the Institutional Ethics Committee of Premas Biotech Pvt. Ltd.
2.3. 5-Bromo-2-deoxyuridine (BrDU) assay
PBMCs were separated from the blood of convalescent patients and stimulated with two doses of PRAK-03202 (2.5 μg and 5 μg). The lymphocyte proliferation rate was measured using the BrdU assay according to the manufacturer's instructions [cell proliferation enzyme-linked immunosorbent assay (ELISA) BrDU, Roche, USA].
2.4. Serum antibody measurements
This study measured PRAK-03202-specific immunoglobulin G (IgG)-mediated antibody titers in serum samples collected from immunized mice and patients by ELISA (Jackson et al., 2020). We also measured the spike, envelope, and membrane protein-specific IgG-mediated immune responses in mouse serum samples. For the PRAK-03202-specific IgG response, wells were coated with 0.25 μg of PRAK-03202, and for the antigen-specific IgG response, 96-well microtiter plates were coated with 0.025 μg of purified spike, envelope, and membrane proteins individually at 2–8 °C overnight. Then, the plates were blocked with 2% bovine serum albumin for 1 h at room temperature. Diluted sera (1:1000) of mice and convalescent patients were applied to each well and incubated at 37 °C for 2 h. Afterwards, the plates were respectively incubated with horseradish peroxidase (HRP)-conjugated goat anti-mouse antibodies (1:5000; A4416, Sigma-Aldrich, USA) and HRP-conjugated anti-human secondary antibodies (1:10000 dilution; A0170, Sigma-Aldrich, USA) at 37 °C for 1 h. The plates were developed using 3, 3′, 5, 5′-tetramethylbenzidine (TMB) and read at 450/570 nm using an ELISA plate reader.
2.5. SARS-CoV-2 neutralization assays
Neutralization experiments on serum samples from immunized animals and convalescent patients were performed according to the manufacturer's protocol (sVNT Kit, GenScript, USA). Briefly, the samples were pre-incubated with HRP-RBD to bind circulating neutralizing antibodies. The mixture was added to a human angiotensin-converting enzyme 2 (ACE2) pre-coated plate and incubated at 37 °C for 15 min. The wells were washed four times with phosphate-buffered saline, and the mixture was incubated with TMB at 20–25 °C in the dark for 15 min. The stop solution was added, and the plate was read at 450 nm using a microtiter plate reader. Mouse neutralization potential (NP) was plotted relative to the human NP (reference), taken as 100%.
2.6. Plaque reduction neutralization test (PRNT)
Vero E6 cells (1 × 105 cells/well) were seeded onto 24-well plates. The following day, 30 PFU of infectious wild-type SARS-CoV-2 was incubated with diluted serum (total volume of 150 μl) at 37 °C for 1 h. The virus-serum mixture was added to the pre-seeded Vero E6 cells and incubated at 37 °C for 1 h. Then, 1 ml of 2% modified Eagle's medium containing carboxymethyl cellulose was added to the infected cells. After 3 days of incubation, 1 ml of 3.7% formaldehyde was added and incubated at room temperature for 30 min. The formaldehyde solution from each well was discarded, and the cell monolayer was stained with a crystal violet solution for 60 min. After washing with water, the plaques were counted to calculate PRNT50, which indicates serum dilutions yielding 50% virus neutralization. The PRNT assay was performed at the biosafety level 3 (BSL-3) facility at THSTI, India.
2.7. Cytokine profiling
Healthy control and patient PBMCs (1 × 105 cells/well) were stimulated with two doses of PRAK-03202 (2.5 μg and 5 μg) at 37 °C in a humidified chamber containing 8% CO2 for 120 h. Supernatants were collected, and cytokine staining for interferon (IFN)-γ was performed according to the manufacturer's instructions [human IFN--g ELISA set (RUO), BD Biosciences, USA].
2.8. Vaccine safety evaluation
The safety of the SARS-CoV-2 vaccine was evaluated in immunized mice at week 5. Datasets of many safety-related parameters were collected during and after immunization, including clinical observation, body weight, organ weight (lung and spleen), and body temperature. Flow cytometric analysis of lymphocyte subset percentage was performed in the lungs, and blood was collected using commercially labeled CD4+ (Cat≠100412; Biolegend), CD8+ (Cat≠140410; Biolegend), CD11c (Cat≠117316; BioLegend), CD11b+ (Cat≠101224; Biolegend), B cells (Cat≠1115535; Biolegend), natural killer (NK Cat≠108905; Biolegend), and Ly6B (Cat≠127629; Biolegend) antibodies. Briefly, the lungs were initially treated with a collagenase solution and macerated. Both lung and blood cells were lysed in red blood cell lysis buffer (Biolegend) on ice for 15 min. The cells were centrifuged at 400 rpm and 4 °C for 5 min. Cell pellets were resuspended in flow cytometry staining (FACS) buffer containing a 1:100 dilution of target-specific antibodies and incubated at 4 °C in the dark for 20 min. Cells were then washed twice with FACS buffer, and data were acquired using a BD FACS Canto II and analyzed using FlowJo (TreeStar).
2.9. Long-term humoral immune response
Mice were kept alive beyond the recovery period under observation to assess the long-term immune response. Briefly, sera were collected from these mice at various time points (0, 21, 61, 66, 76, 86, 97, and 110 days). The total IgG response was evaluated by ELISA using a 1:5000 dilution of HRP-conjugated anti-mouse secondary antibody (A4416, Sigma-Aldrich, USA).
2.10. Statistical analysis
Results are presented as the mean ± standard error of the mean (SEM). The differences in antibody titers were evaluated using the non-parametric Kruskal-Wallis test. The differences in NP and the overall differences were tested using analysis of variance (ANOVA). Bonferroni-adjusted P-values were computed for all pairwise comparisons. The correlations between the methods were analyzed using the Spearman correlation test. All statistical analyses were performed using OriginPro software (Version, 2020b). Statistical significance was set at p < 0.05.
3. Results and discussion
3.1. Characterization and binding affinity of PRAK-03202 for novel coronavirus
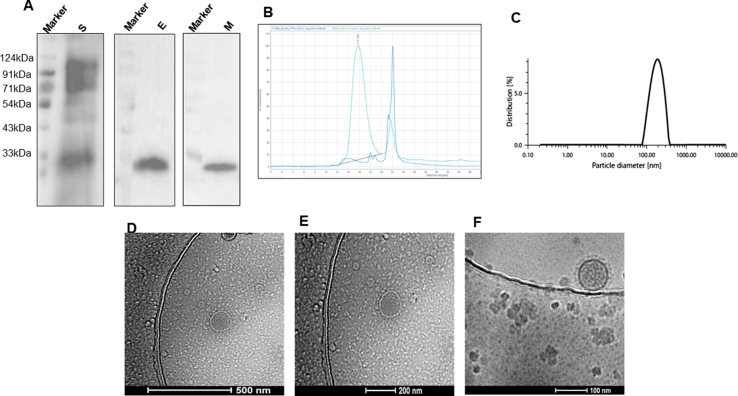
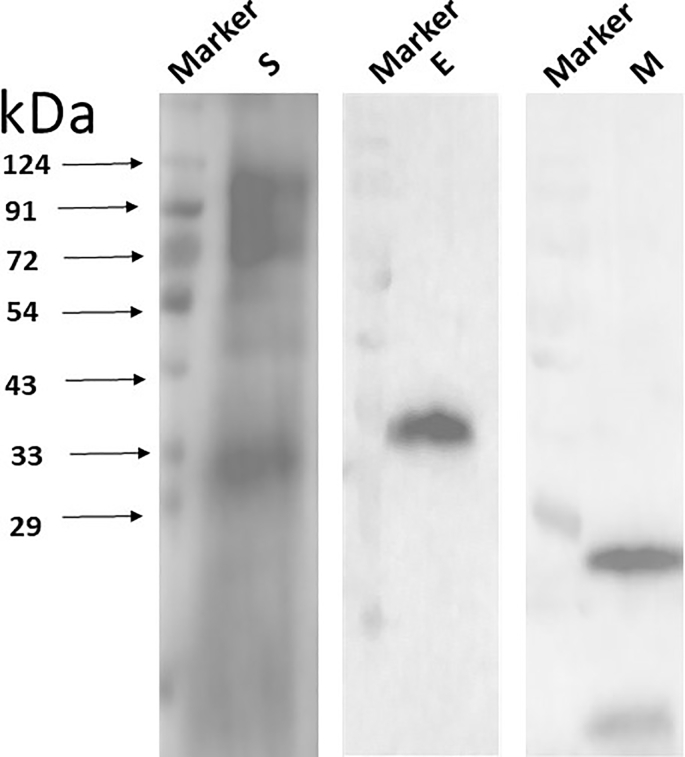
In the present study, we developed a VLP-based COVID-19 vaccine candidate, PRAK-03202, with triple antigenic efficacy. PRAK-03202 design and synthesis were initiated upon the release of the SARS CoV-2 genome sequences in February 2020 (Wu et al., 2020). The co-expression of the spike, envelope, and membrane proteins has been shown to form VLPs for SARS-CoV-2 in recent studies (Boson et al., 2020; Xu et al., 2020). The design and manufacture of the PRAK-03202 vaccine candidate represents a plug-and-play process, where we insert the three-target antigen sequence into a highly characterized S.cerevisiae-based D-Crypt™ platform (Premas Biotech). This system allows scalability of the drug product, and thus circumvents conventional vaccine production complexities in eggs or cell culture (Arora, 2020). PRAK-03202 was purified from cell lysates and analyzed for spike, envelope, and membrane protein expression. Immunoblot analysis using commercially available antibodies confirmed the expression of the three proteins (Figure 1A). The co-expression of the spike, envelope, and membrane proteins was further confirmed by mass spectrometry. Purified PRAK-03202 showed purity greater than 98% using size exclusion chromatography-HPLC (Figure 1B). PRAK-03202 was characterized by dynamic light scattering (DLS) and cryo-transmission electron microscopy (cryo-TEM). DLS analysis showed a mean particle size of 176 ± 18 nm with an 18% polydispersity index (Figure 1C). Additionally, cryo-electron microscopy analysis showed intact spherical bilayer particles (Turonova et al., 2020) with distinct crown-like spikes representing a prefusion virus state (Figure 1D-F).
Figure 1.
Characterization of the triple-antigenic PRAK-03202 as a vaccine candidate against SARS-CoV-2. A) Immunoblot analysis for co-expression of spike, envelope, and membrane proteins in the S. cerevisiae-based D-Crypt™ platform by using antigen-specific antibodies (Sigma Aldrich, USA). S: Spike protein, E: Envelope protein, M: Membrane protein (Refer: Supplementary Figure 1). B) HPLC profile of purified peak (left) from cytoplasmic extract of S. cerevisiae cells, co-expressing the spike, envelope, and membrane proteins at 48 h post-induction. The buffer peak on the right side was overlaid with the HPLC profile peak. C) DLS analysis of the purified VLP intercept g12 = 0.8116; polydispersity index = 18.5%; particle size = 176 ± 18 nm; baseline = 0.998. D-F) Cryo-TEM image of PRAK-03202 from yeast cell cytoplasmic lysate at the D) 500 nm, E) 200 nm, and F) 100 nm scale. The figure shows intact spherical-shaped bilayer particles with distinct spikes.
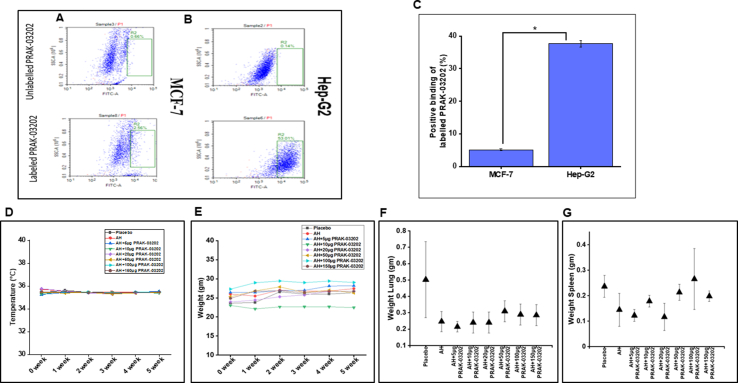
Binding of the RBD to the ACE2 receptor is the first step in SARS CoV-2 infection. Therefore, preventing the interaction between the spike RBD and the ACE2 receptor is considered a strong therapeutic strategy, and work with the SARS and Middle East respiratory syndrome (MERS) coronaviruses have demonstrated proof-of-concept for this approach (Davidson et al., 2020; Huang and Chai, 2020; Li, 2013). To assess the binding affinity of PRAK-03202 to the human ACE2 receptor, flow cytometric analysis was performed with Hep-G2 (high endogenous expression of ACE2 receptor) and MCF-7 (low endogenous expression of ACE2 receptor-negative control) cells. The data demonstrated that Hep-G2 cells bound preferentially to a higher extent (31 ± 9%) than MCF-7 cells, demonstrating the binding efficacy of PRAK-03202 with the ACE2 receptor (Figure 2A-C).
Figure 2.
Safety and specificity of PRAK-03202 for ACE2 receptor. A and B) Flow cytometric analysis to show PRAK-03202 binding to the ACE2 receptor in A) MCF-7 (left panel) and B) HEP-G2 cells (right panel). PRAK-03202 was labelled with CFSE dye (lower panel); unlabeled PRAK-03202 was taken as control (upper panel). Hep-G2 cells with high endogenous expression of ACE-2 and MCF-7 cells with marginal expression of ACE-2 were used as positive and negative controls, respectively. C) Graphical representation to show positive binding of labelled PRAK-03202 to Hep-G2 and MCF-7 cells. Percentage values are given as means ± SEM from n = 3. The amount of PRAK-03202 binding ranged within 31 ± 9%. ∗Indicates statistically significant difference (P < 0.05) from MCF-7 cells. D) Temperature and E) weight measurement of BALB/c mice immunized with 6 different doses of PRAK-03202 and AH for five consecutive weeks (N = 5/group; total number of mice = 45). Values are given as means ± SEM. F and G) Scatter graph depicting weight of F) lung and G) spleen of immunized mice at week 5. Values are given as means ± SEM.
3.2. PRAK-03202-specific humoral immune responses in mice
Serum neutralizing antibodies provide protection against several respiratory viruses and are therefore accepted as a functional biomarker of the in vivo humoral response. Therefore, to assess the immunogenicity of PRAK-03202, BALB/c mice (n = 45) were immunized with different doses (5, 10, 20, 50, 100, and 150 μg) of PRAK-03202 and categorized into eight groups: placebo (0 μg in physiological saline; N = 5), AH only (N = 5), and AH with PRAK-03202 (N = 5/dose; 5, 10, 20, 50, 100, and 150 μg). No visible changes in body temperature, organ/body weight (Figure 2D-G), or other clinical symptoms, such as an arched back and decreased response to external stimuli, were observed, even at high doses (150 μg). Therefore, this dose was considered to have no observed adverse effect levels (Nair and Jacob, 2016).
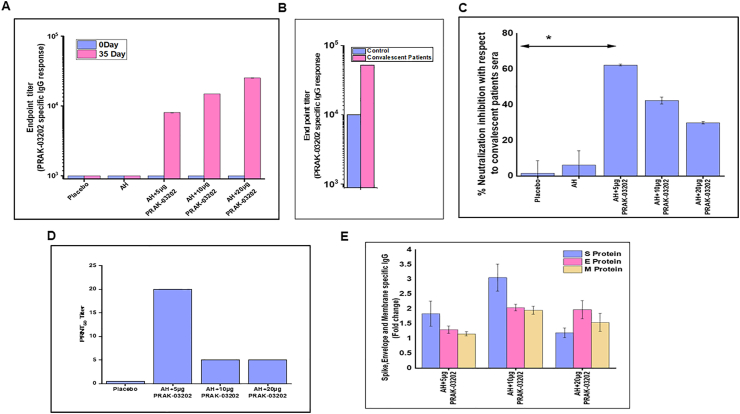
Optimal protection against SARS-CoV-2 is likely elicited by humoral and cell-mediated immune responses (Chowdhury et al., 2020). Since lower doses in animals are considered safe for humans (USFDA, 2005), the PRAK-03202-specific total IgG response was evaluated from the sera of mice immunized with 5, 10, and 20 μg doses of adjuvant PRAK-03202 at days 0 and 35. Briefly, 96-well microtiter plates were coated with 0.025 μg of PRAK-03202 at 2–8 °C overnight. Diluted sera of vaccinated mice and convalescent patients were applied to each well and incubated at 37 °C for 2 h. Next, the total IgG binding endpoint titers from all immunized mouse groups were measured against PRAK-03202 by ELISA. The results showed that all PRAK-03202-vaccinated groups elicited higher IgG-mediated responses than the controls. We observed a dose-dependent increase in titer throughout the study, with a maximum titer obtained at a 20 μg dose of PRAK-03202 (AH: titer value 1000 ± 0; AH+5 μg PRAK-03202: 8500 ± 50; AH+10 μg PRAK-03202: 14900 ± 36; AH+20 μg PRAK-03202: 25300 ± 65) (Figure 3A). Neutralizing antibody titers of PRAK-03202 closely matched the titers measured for the convalescent patient sera (51,714 ± 133), highlighting the potential of PRAK-03202 to induce a potent neutralizing immune response (Figure 3B).
Figure 3.
Humoral immune responses in immunized BALB/c mice (n = 5/group) and convalescent patient sera (N = 3). A and B) Five groups of BALB/c mice were immunized with the indicated doses of PRAK-03202 (n = 5/group). PRAK-03202-specific IgG antibody titers were analyzed by ELISA in mice (A) and in (B) healthy and convalescent patient sera. Bars represent the mean titer, with standard deviation indicated. C) Bar chart depicting the NP of PRAK-03202 in immunized mice relative to the NP of convalescent patients, which was taken as reference. Corrected NP (%) = (average NP of sera samples of immunized mice/average NP of sera samples from convalescent patients) X100. ∗Indicates statistically significant difference (P < 0.05). D) Vero E6 cells were infected with the 30 PFU of wild type SARS-CoV-2 and serum mixture at the indicated dilutions. PRNT50 titer was plotted for each group of immunized mice. E) Antigen-specific -fold changes in IgG responses (spike, envelope, and membrane proteins) of PRAK-03202 were measured by ELISA in immunized mice. PRAK-03202 was incubated with 0.25 μg of purified spike, envelope, and membrane protein-coated 96-well plates. The plates were read at 450/630 nm using an ELISA plate reader. Error bars indicate SEM.
RBD-specific neutralization inhibition was evaluated in sera from convalescent and immunized mice. The NP of convalescent patient sera was used as a reference and considered as 100%; data from mice were plotted relative to this standard. In the neutralization inhibition assay, sera from all the PRAK-03202-vaccinated groups showed significant NP by inhibiting the RBD and ACE2 interaction, compared with the control groups. However, maximum inhibition of RBD and ACE2 cell surface receptors was observed at the lowest (5 μg) dose of adjuvant PRAK-03202 (62.3 ± 0.50%), compared with the control groups (AH: 6.12 ± 8.06%; Figure 3C). Comparatively low total IgG values and high NP values at a 5 μg dose (NP: 62.3 ± 0.50%) suggested that immunization with 10 μg (NP: 42.3 ± 1.92%) and 20 μg (NP: 29.9 ± 0.69%) of adjuvant PRAK-03202 led to the generation of non-neutralizing epitopes in sera that did not engage in ACE2 receptor binding; therefore, lower NP was observed. These results were consistent with those of previous studies, which showed that non-neutralizing epitopes severely reduced vaccine efficacy by inducing strong non-neutralizing immune responses and distracting the host immune system from reacting with neutralizing epitopes on the RBM (Du et al., 2013, 2016).
Conventionally, neutralizing antibodies are measured using PRNT. PRNT is considered the gold standard for determining immune protection (Muruato et al., 2020). To validate the virus neutralization assay results, we performed conventional PRNT on all PRAK-03202-vaccinated groups. On day 3 post-challenge, wild-type PRNT50 virus–neutralizing activity against SARS-CoV-2 was detected in all PRAK-03202 vaccinated groups. The PRNT50 titers were higher in the AH+5 μg PRAK-03202 (1:20) groups than in the other adjuvant groups, where PRNT50 was observed at a dilution of 1:5. Moderate inhibition of plaque number was observed in all mice except those vaccinated with a lower dose (5 μg) of PRAK-03202, further confirming the protective potential of this dose. A strong correlation was observed between the virus neutralization assay and the PRNT results, with a correlation efficiency R2 of 0.78 (p = 0.003) (Figure 3D). The results demonstrate that when diagnosing patient specimens, the viral neutralization assay of PRAK-03202 should deliver results comparable to those of the PRNT assay. Compared to the PRNT assay, BSL-2 containment is required for the viral neutralization assay, instead of BSL3, which decreases the turnaround time and increases testing efficacy to high-throughput in case of SARS-CoV-2 infection.
3.3. Spike, envelope, and membrane protein-specific immune response
Previous studies have shown that novel coronaviruses can escape the host immune response either by exposing non-neutralizing epitopes to their RBDs or due to emerging mutations in their spike sequence that mediate escape from neutralizing antibody responses induced by immunogens designed using the Wuhan/WIV04/2019 sequence (Dong et al., 2020; Durmaz et al., 2020). Hence, other SARS-CoV-2 proteins may also play important roles in the development of suitable vaccine candidates (Bhattacharya et al., 2021; Lopandic et al., 2021).
Therefore, to measure the in vitro spike, envelope, and membrane-specific IgG response, 96-well microtiter plates were coated with 0.025 μg of purified spike, envelope, and membrane proteins individually at 2–8 °C overnight. Diluted sera of vaccinated mice were applied to each well and incubated at 37 °C for 2 h. Evaluation of immune response against the spike, envelope, and membrane proteins showed that the sera of mice vaccinated with 10 μg dose showed maximal immune response against the three antigens (spike-3.05 ± 0.45-fold, envelope-2.04 ± 0.11-fold, membrane-1.95 ± 0.13-fold; P=NS), whereas AH in combination with 5 μg PRAK-03202 showed a comparatively high response for spike protein compared with controls (AH+5 μg PRAK-03202: spike-1.83 ± 0.42-fold, envelope-1.35 ± 0.12-fold, membrane-1.3 ± 0.07-fold) (Figure 3E). This highlights the potential of PRAK-03202 to induce a strong and potent immune response by eliciting effective antibody responses for all three antigens. Therefore, PRAK-03202 may serve as an effective vaccine candidate for novel coronavirus infections.
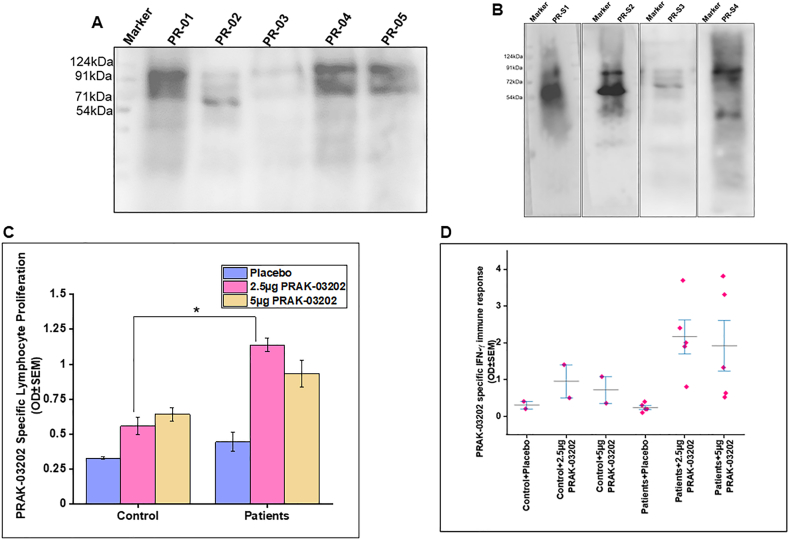
3.4. PRAK-03202 induced IFN-γ response in convalescent patients
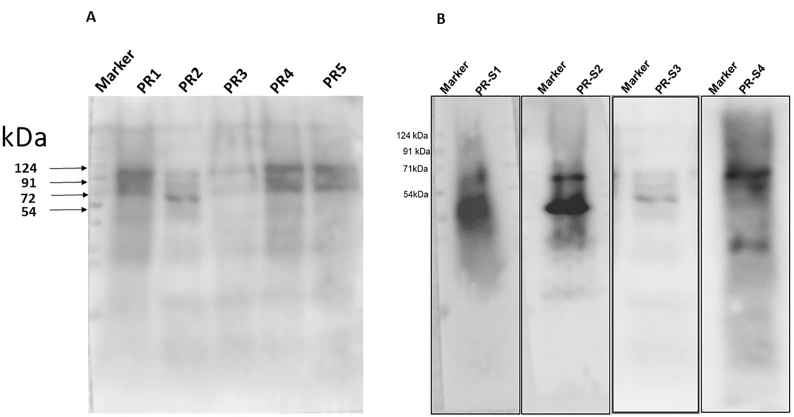
To further observe whether PRAK-03202 was recognized by the sera of convalescent patients (n = 7), immunoblotting analysis was performed. Our findings showed multiple protein bands, which suggest that certain components of PRAK-03202 were recognized by antibodies present in the sera of convalescent patients (Figure 4A-B).
Figure 4.
IFN-γ responses in convalescent patients. A) Immunoblot analysis of five different batches of PRAK-03202 (PR-01 to PR-05) when probed with sera from convalescent patients. M = marker, PR-01-PR-05: 5 batches of PRAK-03202 (Refer: Supplementary Figure 2A). B) Immunoblot analysis of PRAK-03202 when probed with sera from four convalescent patients (PR-S1 to PR-S4) (Refer: Supplementary Figure 2B). C) Lymphocyte proliferation in PRAK-03202 (2.5 μg and 5 μg)-stimulated PBMCs from controls (n = 2) and convalescent COVID-19 patients (n = 5). Samples were stimulated for 120 h, and the BrDU assay was performed (Cell Proliferation ELISA BrDU, Roche, USA). The plates were read at 450/690 nm using an ELISA plate reader. OD values represent means ± SEM. Significant differences between controls and patients were observed. ∗Indicates a statistically significant difference (p < 0.05). D) Cytokine staining for IFN-γ by ELISA in controls and convalescent patient samples stimulated with two different doses (2.5 μg and 5 μg) of PRAK-03202. Error bars indicate SEM.
In addition to humoral responses, cellular immune responses have also been associated with more favorable recovery from MERS-CoV infection and are likely an important factor in SARS-CoV infection as well (Zhao et al., 2017). To assess T cell responses and determine whether PRAK-03202 mimics the viral epitopes, PRAK-03202 was used in cytokine staining assays using healthy and convalescent human PBMCs. PRAK-03202-specific lymphocyte proliferation was evaluated by ELISA in convalescent patients (n = 5) and healthy control sera (n = 2).
In comparison with controls, higher lymphocyte proliferation was observed in PRAK-03202-stimulated patient sera at two doses (2.5 μg: 2-fold; 5μg: 1.45-fold) (Figure 4C). These findings suggest that PRAK-03202 induced lymphocyte proliferation in convalescent blood, indicating its recognition by antigen-presenting cells and presentation to immune cells.
Type I or type II immunity have been predominantly elicited by vaccines in previous studies (Hoft et al., 1999; Spellberg and Edwards, 2001). Therefore, we evaluated the IFN-γ response in the patient samples (Figure 4D). Experimental data showed elevated IFN-γ levels in patient PBMCs (2.16 ± 0.33) compared with healthy controls (0.95 ± 0.23), suggesting induction of T helper 1 (Th1)-biased cellular immune responses. Rapid cellular responses could potentially reduce the viral load and spread of SARS-CoV-2 and COVID-19.
Different strategies have been devised to enhance host immunity against viral diseases by inducing Th1-type immune responses and neutralizing antibodies against targeted proteins. Naïve T cells polarize immune responses into Th1 and Th2 cells. A recent study showed that patients mounting a Th2 response against SARS-CoV-2 required intensive care, compared with a Th1 response, which would keep the infection under IFN control (Roncati et al., 2020). IFNs, such as IFN-α and IFN-γ, are highly correlated with the SARS-CoV-2 viral load, suggesting that viral load may drive these cytokines (Lucas et al., 2020). Similarly, increased expression of toll-like receptor 3 (TLR3) after coronavirus infections has been reported to activate transcription factors, such as IFN regulatory transcription factor 3 and nuclear factor-κB, which are associated with increased production of type I IFNs (IFN-α and β), inflammatory cytokines (interleukin-6 and tumor necrosis factor), and IFN-γ (Allison et al., 2015). These results suggest that the virus evades the immune system by disabling IFNs during the early stages of infection. When a virus invades a cell, IFNs provoke an intense local response by unleashing various other proteins that inhibit viral replication and invade neighboring cells. Hence, successful vaccines are expected to polarize the T cell response towards type 1 immunity via IFNs and prevent the stimulation of cytokines that induce Th2 immunity.
In the present study, elevated IFN-γ levels in the patient samples supported the findings of previous studies demonstrating that intranasal IFN-γ is a viable treatment option for respiratory syncytial virus due to its ability to reduce viral titers in the lung with no detectable increase in CD4+ or CD8+ T cell infiltration (Empey et al., 2012). This indicates potential mimicking of the actual virus by PRAK-03202, which could induce a Th1 immune response.
3.5. PRAK-03202-specific IgG-mediated long-term humoral response
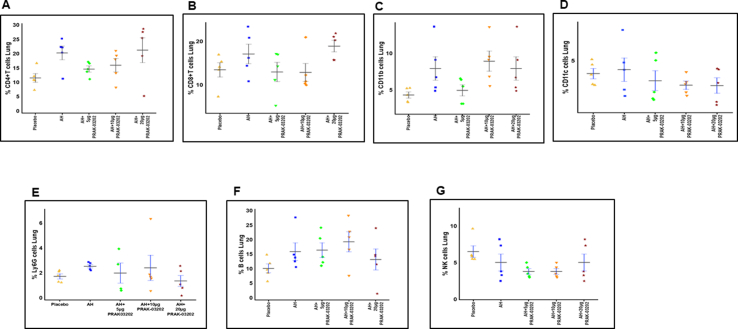
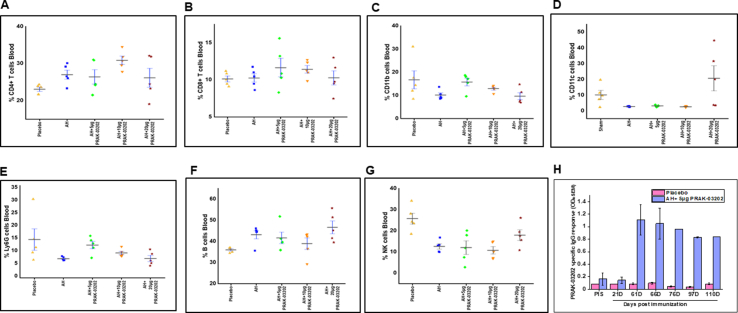
Safety and efficacy are essential for vaccine development in both preclinical and clinical trials. T cell infiltration can increase lung viral titers in the case of respiratory viruses and is considered a major part of vaccine development for respiratory diseases (Empey et al., 2012). We provide evidence for the safety of PRAK-03202 in mice and did not observe any visible changes in lymphocyte subset percentage (CD4+, CD8+, CD11b+, CD11c+, Ly6B, B cells, and NK cells) in either the lungs (Figure 5A-G) or blood (Figure 6A-G) of the PRAK-03202-vaccinated groups.
Figure 5.
Profile of immune cells in the lungs of BALB/c mice vaccinated with PRAK-03202. A-G) Lungs were initially treated with collagenase solution and macerated. Flow cytometric analysis of the lymphocyte subset percentage of A) CD4+, B) CD8+, C) CD11b+, D) CD11c+, E) Ly6G+, F) B cells, and G) NK cells in lung samples was performed by using the indicated antibodies at a 1:100 dilution. Error bars indicate means ± SEM.
Figure 6.
Profile of immune cells in the blood of mice vaccinated with PRAK-03202. A-G) Flow cytometric analysis of the lymphocyte subset percentage of A) CD4+, B) CD8+, C) CD11b+, D) CD11c+, E) Ly6G+, F) B cells, and G) NK cells in blood samples were performed by using the indicated antibodies at a 1:100 dilution. Error bars indicate means ± S.E.M. H) Sera from immunized mice were collected at various time points (0, 21, 61, 76, 86, 97, and 110 days). Total IgG response was evaluated using ELISA with a 1:5000 dilution of HRP-conjugated secondary antibodies (A4416, Sigma, USA). An IgG response was observed even after 110 days, suggesting long-term efficacy of PRAK-03202. Error bars indicate SEM.
Mice vaccinated with adjuvant PRAK-032025 were kept alive beyond the recovery period under observation for long-term humoral immune response; sera were collected at various time points. Total IgG responses could be seen even after 110 days (IgG: 5.25 ± 0.23-fold compared with placebo), suggesting a long-term humoral response induced by PRAK-03202 (Figure 6H).
The mortality and morbidity observed during the SARS-CoV-2 pandemic has created an imminent need for a prophylactic vaccine to prevent infection of approximately 7 billion people worldwide. Although several vaccine candidates have initiated clinical testing, very little is known about their long-term humoral response. Specifically, detailed descriptions and precise estimates of the magnitude and duration of immune responses are lacking.
We also observed IgG-mediated responses in all immunized mice for approximately 4 months (110 days). The observation that IgG and neutralizing antibody responses persist even up to 110 days is encouraging and suggests the development of systemic immune memory with PRAK-03202. While a long-term study may be necessary, the present findings support that the IgG antibody responses against the novel PRAK-03202 vaccine persist for months. However, we did not evaluate the protection level of PRAK-03202 in mice challenged with live SARS-CoV-2, which is important for future studies.
Our results indicate that, in comparison to other existing vaccine platforms against SARS-CoV-2, PRAK-03202 may provide several advantages: 1) resemblance with native SARS CoV-2; 2) non-replicative and non-infective nature, providing safe usage in immunocompromised populations (Nooraei et al., 2021); 3) scalability and commercialization using our D-crypt™ platform, which may circumvent conventional vaccine production complexities, and thus represent an attractive vaccine strategy against SARS-CoV-2 infection.
Limitations of the study
This study did not evaluate the protection level of PRAK-03202 in mice challenged with live SARS CoV-2. Furthermore, this study was based on mouse models; thus, it is important to call for research using non-human primates to evaluate the translational and pharmacological values of these findings.
Declarations
Author contribution statement
Saumyabrata Mazumder, Ruchir Rastogi, Kajal Arora, Nupur Mehrotra Arora: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Avinash Undale, Prabuddha Kumar Kundu: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data.
Biswa Pratim, Dilip Kumar, Abyson Joseph, Bhupesh Mali, Vidya Bhushan Arya, Sriganesh Kalyanaraman, Abhishek Mukherjee, Aditi Gupta, Swaroop Potdar, Sourav Singha Roy, Deepak Parashar, Jeny Paliwal, Sudhir Kumar Singh, Aelia Naqvi, Apoorva Srivastava, Manglesh Kumar Singh, Devanand Kumar, Sarthi Bansal, Satabdi Rautray, Manish Saini, Kshipra Jain: Performed the experiments.
Reeshu Gupta: Analyzed and interpreted the data; Wrote the paper.
Funding statement
This work was supported by Akers Biosciences and Premas Biotech Private Limited, India.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors thank Dr Manidipa Banerjee, IIT Delhi for TEM analysis, Dr. Deepak Rathore and Vishal Gupta at THSTI Faridabad for FACS analysis, Dr. Sankar Bhattacharyya, THSTI for PRNT assay, Dr. Nipendra Singh at RCB for mass spectrometry, Rakesh Jaswal and Abhishek Choudhary for logistics. We would also like to thank Dr. Manish Kumar, Nupur Pandey, Premas Biotech, for providing their assistance while performing ELISA, Abinash Patra, Amaresh Dutta, Arjun Singh Yadav, Premas Biotech for assisting in analytics, and Pankaj Fengade, Bibekanand Kumar and Indrajeet Singh in performing 5L fermentation scale-up studies.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
Supplementary Figure 1.
Non-adjusted Immunoblot image of Figure 1A
Supplementary Figure 2.
IFN-γ responses in convalescent patients. A) Non-adjusted image of Figure 4A demonstrating Immunoblot analysis of 5 different batches of PRAK-03202 (PR-01 to PR-05). B) Non-adjusted image Figure 4B demonstrating Immunoblot analysis of PRAK-03202 when probed with serum of 4 convalescent patient sera (PR-S1 to PR-S4).
References
- Allison L., Totura A.W., Agnihothram Sudhakar, Schäfer Alexandra, Katze Michael G., Heise Mark T., Baric Ralph S. Toll-like receptor 3 signaling via TRIF contributes to a protective innate immune response to severe acute respiratory syndrome coronavirus infection. mBio. 2015;6 doi: 10.1128/mBio.00638-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora K.e.a. Multi-Antigenic Virus-like Particle of SARS CoV-2 produced in Saccharomyces cerevisiae as a vaccine candidate. BioRxiv. 2020 [Google Scholar]
- Bhattacharya S., Banerjee A., Ray S. Development of new vaccine target against SARS-CoV2 using envelope (E) protein: an evolutionary, molecular modeling and docking based study. Int. J. Biol. Macromol. 2021;172:74–81. doi: 10.1016/j.ijbiomac.2020.12.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boson B., Legros V., Zhou B., Siret E., Mathieu C., Cosset F.L., Lavillette D., Denolly S. The SARS-CoV-2 envelope and membrane proteins modulate maturation and retention of the spike protein, allowing assembly of virus-like particles. J. Biol. Chem. 2020;296:100111. doi: 10.1074/jbc.RA120.016175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury M.A., Hossain N., Kashem M.A., Shahid M.A., Alam A. Immune response in COVID-19: a review. J. Infect. Public Health. 2020 doi: 10.1016/j.jiph.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson A.M., Wysocki J., Batlle D. Interaction of SARS-CoV-2 and other coronavirus with ACE (Angiotensin-Converting enzyme)-2 as their main receptor: therapeutic implications. Hypertension. 2020;76:1339–1349. doi: 10.1161/HYPERTENSIONAHA.120.15256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Pasquale A., Preiss S., Tavares Da Silva F., Garcon N. Vaccine adjuvants: from 1920 to 2015 and beyond. Vaccines. 2015;3:320–343. doi: 10.3390/vaccines3020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y., Dai T., Wei Y., Zhang L., Zheng M., Zhou F. A systematic review of SARS-CoV-2 vaccine candidates. Signal Transduct. Target Ther. 2020;5:237. doi: 10.1038/s41392-020-00352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du L., Kou Z., Ma C., Tao X., Wang L., Zhao G., Chen Y., Yu F., Tseng C.T., Zhou Y. A truncated receptor-binding domain of MERS-CoV spike protein potently inhibits MERS-CoV infection and induces strong neutralizing antibody responses: implication for developing therapeutics and vaccines. PLoS One. 2013;8 doi: 10.1371/journal.pone.0081587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du L., Tai W., Yang Y., Zhao G., Zhu Q., Sun S., Liu C., Tao X., Tseng C.K., Perlman S. Introduction of neutralizing immunogenicity index to the rational design of MERS coronavirus subunit vaccines. Nat. Commun. 2016;7:13473. doi: 10.1038/ncomms13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durmaz B., Abdulmajed O., Durmaz R. Mutations observed in the SARS-CoV-2 spike glycoprotein and their effects in the interaction of virus with ACE-2 receptor. Medeni Med. J. 2020;35:253–260. doi: 10.5222/MMJ.2020.98048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Empey K.M., Orend J.G., Peebles R.S., Jr., Egana L., Norris K.A., Oury T.D., Kolls J.K. Stimulation of immature lung macrophages with intranasal interferon gamma in a novel neonatal mouse model of respiratory syncytial virus infection. PLoS One. 2012;7 doi: 10.1371/journal.pone.0040499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Q., Bao L., Mao H., Wang L., Xu K., Yang M., Li Y., Zhu L., Wang N., Lv Z. Development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020;369:77–81. doi: 10.1126/science.abc1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan A., Al-Ozairi E., Al-Baqsumi Z., Ahmad R., Al-Mulla F. Cellular and humoral immune responses in covid-19 and immunotherapeutic approaches. ImmunoTargets Ther. 2021;10:63–85. doi: 10.2147/ITT.S280706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho Y., Lin P.H., Liu C.Y., Lee S.P., Chao Y.C. Assembly of human severe acute respiratory syndrome coronavirus-like particles. Biochem. Biophys. Res. Commun. 2004;318:833–838. doi: 10.1016/j.bbrc.2004.04.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoft D.F., Kemp E.B., Marinaro M., Cruz O., Kiyono H., McGhee J.R., Belisle J.T., Milligan T.W., Miller J.P., Belshe R.B. A double-blind, placebo-controlled study of Mycobacterium-specific human immune responses induced by intradermal bacille Calmette-Guerin vaccination. J. Lab. Clin. Med. 1999;134:244–252. doi: 10.1016/s0022-2143(99)90204-4. [DOI] [PubMed] [Google Scholar]
- Huang Z., Chai J. Door to the cell for COVID-19 opened, leading way to therapies. Signal Transduct. Target Ther. 2020;5:104. doi: 10.1038/s41392-020-00215-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson L.A., Anderson E.J., Rouphael N.G., Roberts P.C., Makhene M., Coler R.N., McCullough M.P., Chappell J.D., Denison M.R., Stevens L.J. An mRNA vaccine against SARS-CoV-2 - preliminary report. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2022483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K.H., Lee Y.T., Hwang H.S., Kwon Y.M., Kim M.C., Ko E.J., Lee J.S., Lee Y., Kang S.M. Virus-like particle vaccine containing the F protein of respiratory syncytial virus confers protection without pulmonary disease by modulating specific subsets of dendritic cells and effector T cells. J. Virol. 2015;89:11692–11705. doi: 10.1128/JVI.02018-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar H., Kawai T., Akira S. Pathogen recognition by the innate immune system. Int. Rev. Immunol. 2011;30:16–34. doi: 10.3109/08830185.2010.529976. [DOI] [PubMed] [Google Scholar]
- Li F. Receptor recognition and cross-species infections of SARS coronavirus. Antivir. Res. 2013;100:246–254. doi: 10.1016/j.antiviral.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Z., Zhu H., Wang X., Jing B., Li Z., Xia X., Sun H., Yang Y., Zhang W., Shi L. Adjuvants for coronavirus vaccines. Front. Immunol. 2020;11:589833. doi: 10.3389/fimmu.2020.589833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopandic Z., Protic-Rosic I., Todorovic A., Glamoclija S., Gnjatovic M., Cujic D., Gavrovic-Jankulovic M. IgM and IgG immunoreactivity of SARS-CoV-2 recombinant M protein. Int. J. Mol. Sci. 2021;22 doi: 10.3390/ijms22094951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas C., Wong P., Klein J., Castro T.B.R., Silva J., Sundaram M., Ellingson M.K., Mao T., Oh J.E., Israelow B. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature. 2020;584:463–469. doi: 10.1038/s41586-020-2588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muruato A.E., Fontes-Garfias C.R., Ren P., Garcia-Blanco M.A., Menachery V.D., Xie X., Shi P.Y. A high-throughput neutralizing antibody assay for COVID-19 diagnosis and vaccine evaluation. Nat. Commun. 2020;11:4059. doi: 10.1038/s41467-020-17892-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair A.B., Jacob S. A simple practice guide for dose conversion between animals and human. J. Basic Clin. Pharm. 2016;7:27–31. doi: 10.4103/0976-0105.177703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naskalska A., Dabrowska A., Nowak P., Szczepanski A., Jasik K., Milewska A., Ochman M., Zeglen S., Rajfur Z., Pyrc K. Novel coronavirus-like particles targeting cells lining the respiratory tract. PLoS One. 2018;13 doi: 10.1371/journal.pone.0203489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nooraei S., Bahrulolum H., Hoseini Z.S., Katalani C., Hajizade A., Easton A.J., Ahmadian G. Virus-like particles: preparation, immunogenicity and their roles as nanovaccines and drug nanocarriers. J. Nanobiotechnol. 2021;19:59. doi: 10.1186/s12951-021-00806-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan F.S., Basak S., Chu K.B., Kim S.S., Kang S.M. Progress in the development of virus-like particle vaccines against respiratory viruses. Expert Rev. Vaccines. 2020;19:11–24. doi: 10.1080/14760584.2020.1711053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncati L., Nasillo V., Lusenti B., Riva G. Signals of Th2 immune response from COVID-19 patients requiring intensive care. Ann. Hematol. 2020;99:1419–1420. doi: 10.1007/s00277-020-04066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spellberg B., Edwards J.E., Jr. Type 1/Type 2 immunity in infectious diseases. Clin. Infect. Dis. 2001;32:76–102. doi: 10.1086/317537. [DOI] [PubMed] [Google Scholar]
- Syomin B.V., Ilyin Y.V. Virus-like particles as an instrument of vaccine production. Mol. Biol. 2019;53:323–334. doi: 10.1134/S0026893319030154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turonova B., Sikora M., Schurmann C., Hagen W.J.H., Welsch S., Blanc F.E.C., von Bulow S., Gecht M., Bagola K., Horner C. In situ structural analysis of SARS-CoV-2 spike reveals flexibility mediated by three hinges. Science. 2020 doi: 10.1126/science.abd5223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X.W., Wang J.X. Pattern recognition receptors acting in innate immune system of shrimp against pathogen infections. Fish Shellfish Immunol. 2013;34:981–989. doi: 10.1016/j.fsi.2012.08.008. [DOI] [PubMed] [Google Scholar]
- Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G., Hu Y., Tao Z.W., Tian J.H., Pei Y.Y. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R., Shi M., Li J., Song P., Li N. Construction of SARS-CoV-2 virus-like particles by mammalian expression system. Front Bioeng. Biotechnol. 2020;8:862. doi: 10.3389/fbioe.2020.00862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Alshukairi A.N., Baharoon S.A., Ahmed W.A., Bokhari A.A., Nehdi A.M., Layqah L.A., Alghamdi M.G., Al Gethamy M.M., Dada A.M. Recovery from the Middle East respiratory syndrome is associated with antibody and T-cell responses. Sci. Immunol. 2017;2 doi: 10.1126/sciimmunol.aan5393. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supplementary material/referenced in article.