Abstract
Background:
To describe the first case of Coronavirus disease-2019 (COVID-19) vision loss from an acute outer retinopathy.
Methods:
A retrospective case report from a tertiary referral center using multimodal retinal imaging and clinical examination findings
Findings:
A 40-year-old female developed significant vision loss in her right eye shortly after developing fever and myalgias. She was found to be COVID positive, while her systemic laboratory evaluation was otherwise unremarkable. Multimodal imaging was consistent with a white-dot-like outer retinopathy and she was started on systemic prednisone. Within ten days of starting steroids, her vision, symptoms, and outer retinal changes on multimodal imaging were improving.
Interpretation:
While exceedingly rare, COVID-19 can cause inflammatory-associated changes of the outer retina and significant vision loss.
Keywords: COVID, coronavirus, outer retinopathy, vision loss
Introduction
Coronavirus disease-2019 (COVID-19) can affect nearly every organ system resulting in flu-like symptoms, diarrhea, loss of smell and taste, and in the worst cases, strokes, acute respiratory distress, multi-organ failure, and death.1 With ocular involvement, there are few reports of viral conjunctivitis and incidental, visually-insignificant retinal findings,2,3 but no reported cases of vision-threatening complications associated with COVID-19 as described herein.
Results
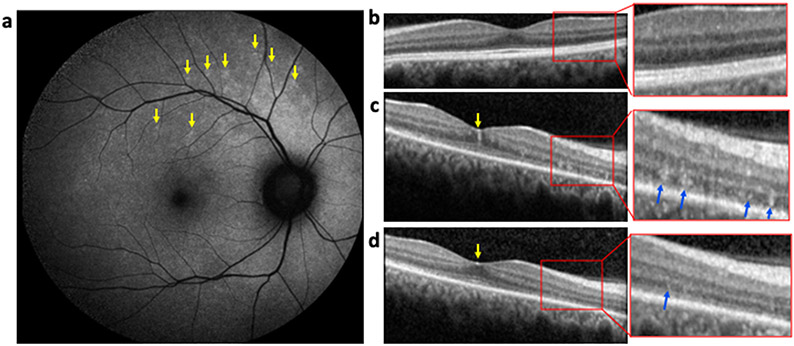
A 40-year-old woman with history of ulcerative colitis in remission developed low grade fevers and myalgias. Two days later, she developed acute vision loss in the right eye with positive visual photopsias followed by a loss of taste and smell. Subsequent PCR testing was positive for SARS-CoV-2. On ocular examination three weeks later, she was found to have severe visual impairment with a visual acuity of 20/1250 in the affected eye, no afferent pupillary defect, and peripapillary hyperautofluorescence indicative of sickened retinal pigment epithelial and/or the overlying photoreceptors (Figure 1a, yellow arrows). Her left eye was normal on examination and multimodal imaging with visual acuity of 20/20 at the time (Figure 1b). Optical coherence tomography (OCT) identified hyperreflective foci at the fovea (yellow arrows) and within the thinned outer nuclear layer (blue arrows) and ellipsoid zone disruption (Figure 1c), similar to changes seen with non-infectious inflammatory chorioretinopathies. A focused serological evaluation for both infectious and non-infectious etiologies and MRI of the brain showed IgG antibodies against SARS-CoV-2 but was otherwise unremarkable. The patient developed flickering photopsias in her left eye and was started on oral prednisone (60 mg/day) due to concern of further vision loss. Re-evaluation ten days later showed symptom and anatomic improvement (Figure 1d, yellow and blue arrows). Three weeks after starting prednisone, her visual acuity recovered to 20/600, and aqueous humor PCR for SARS-CoV-2 was negative. She would unfortunately develop macular edema while tapering systemic steroids and was started on oral methotrexate due to concern of developing inflammatory complications in her left eye. The symptoms in her left eye have completely resolved and the vision in her right eye remains severely impaired but stable (20/200). She remains on 20 milligrams of methotrexate orally and has completed her systemic steroid taper with continued improvement in her ellipsoid zone on OCT six months later.
Figure 1: Imaging Results in a Patient with COVID19-Associated Retinopathy.
(a) Fundus autofluorescence imaging noted patchy peripapillary autofluorescence extending into the macula (yellow arrows). (b) A normal OCT of the left eye at presentation. (c) An OCT of the right eye at presentation that showed multiple hyperreflective lesions at the level of the inner fovea (yellow arrows) and in thinned, outer nuclear layer with ellipsoid zone disruption (blue arrows, inset). (d) Ten days after starting systemic prednisone, the inner foveal lesion (yellow) and the outer retinal lesions (blue arrow) had nearly completed resolved.
Discussion
To our knowledge, this report represents the first case of retinal inflammation with vision loss associated with COVID-19 and is highly suggestive due to the temporal relationship of the various patient symptoms. The outer retinopathy described herein is similar to an inflammatory choroidopathy known as multiple evanescent white dot syndrome (MEWDS) that is likely the result of post-viral inflammation.4 However, our patient’s clinical course differs from typical cases of MEWDS there is near-to-complete visual recovery unlike in our patient.5 Surprisingly, there have been only a few other ocular inflammatory events associated with COVID-19 reported in the literature, mainly optic nerve complications, despite significant neurological complications and inflammatory microvascular changes of the brain seen in many patients with severe COVID-19 infections.6-9 In contrast, there have been multiple reports of patients developing retinal vascular complications related to COVID-19 including paracentral acute middle maculopathy and central retinal vein occlusions and similar to the vascular complications known to occur with the disease in other tissues.10-12
While we cannot entirely exclude direct infection of the retina, our findings support an inflammatory etiology, evident by improvement of the OCT lesions on systemic steroid therapy alone, the presence of seroconversion to SARS-CoV-2, and negative PCR from intraocular fluid. Unfortunately, we were unable to obtain the aqueous fluid at time of presentation due to logistics and SARS-CoV-2 protocols and would have ideally be obtained at the time of symptom onset. While her improvement in vision and resolution of outer retinal lesions are encouraging, vision loss is profound and further recovery uncertain. As some epidemiological models estimate that 1.7 billion people worldwide are at risk of developing SARS-CoV-2 infection, identification of vision-threatening sequelae, including infectious and potentially rare, post-infectious inflammatory conditions, is imperative.13 Due to limitations in access to ocular care during the ongoing pandemic, we hypothesize that ocular complications from SARS-CoV-2 infection will become more apparent in the coming months as more patients seek care for vision loss.
Acknowledgements
This research was supported by the National Eye Institute (R01EY030989 to R.C.R), and Research to Prevent Blindness (to the University of Michigan Kellogg Eye Center and R.C.R.). R.C.R. received funding from the Beatrice & Reymont Paul Foundation, March Hoops to Beat Blindness, the Taubman Institute, the Leonard G. Miller Endowed Professorship and Ophthalmic Research Fund at the Kellogg Eye Center, and the Grossman, Elaine Sandman, Marek and Maria Spatz (endowed), Greenspon, Dunn, Avers, Boustikakis, Sweiden, and Terauchi research funds to R.C.R. C.D.C. was supported in part by the Heed Ophthalmic Foundation. The funding agencies had no role in the design or conduct of this study.
Footnotes
Declaration of Interests
None of the authors has any conflicts of interest to disclose.
Bibliography
- 1.Huang R, Zhu L, Xue L, et al. Clinical findings of patients with coronavirus disease 2019 in Jiangsu province, China: A retrospective, multi-center study. PLOS Neglected Tropical Diseases. 2020;14(5):e0008280. doi: 10.1371/journal.pntd.0008280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu P, Duan F, Luo C, et al. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. Published online March31, 2020. doi: 10.1001/jamaophthalmol.2020.1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marinho PM, Marcos AAA, Romano AC, Nascimento H, Belfort R. Retinal findings in patients with COVID-19. The Lancet. 2020;395(10237):1610. doi: 10.1016/S0140-6736(20)31014-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quillen DA, Davis JB, Gottlieb JL, et al. The white dot syndromes. Am J Ophthalmol. 2004;137(3):538–550. doi: 10.1016/j.ajo.2004.01.053 [DOI] [PubMed] [Google Scholar]
- 5.Jampol LM, Sieving PA, Pugh D, Fishman GA, Gilbert H. Multiple evanescent white dot syndrome. I. Clinical findings. Arch Ophthalmol. 1984;102(5):671–674. doi: 10.1001/archopht.1984.01040030527008 [DOI] [PubMed] [Google Scholar]
- 6.François J, Collery AS, Hayek G, et al. Coronavirus Disease 2019–Associated Ocular Neuropathy With Panuveitis: A Case Report. JAMA Ophthalmology. Published online December17, 2020. doi: 10.1001/jamaophthalmol.2020.5695 [DOI] [PubMed] [Google Scholar]
- 7.Zhou S, Jones-Lopez EC, Soneji DJ, Azevedo CJ, Patel VR. Myelin Oligodendrocyte Glycoprotein Antibody–Associated Optic Neuritis and Myelitis in COVID-19. Journal of Neuro-Ophthalmology. 2020;40(3). https://journals.lww.com/jneuro-ophthalmology/Fulltext/2020/09000/Myelin_Oligodendrocyte_Glycoprotein.16.aspx [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Helms J, Kremer S, Merdji H, et al. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med. 2020;382(23):2268–2270. doi: 10.1056/NEJMc2008597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee M-H, Perl DP, Nair G, et al. Microvascular Injury in the Brains of Patients with Covid-19. N Engl J Med. Published online December30, 2020. doi: 10.1056/NEJMc2033369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Invernizzi A, Pellegrini M, Messenio D, et al. Impending Central Retinal Vein Occlusion in a Patient with Coronavirus Disease 2019 (COVID-19). null. 2020;28(8):1290–1292. doi: 10.1080/09273948.2020.1807023 [DOI] [PubMed] [Google Scholar]
- 11.Virgo J, Mohamed M. Paracentral acute middle maculopathy and acute macular neuroretinopathy following SARS-CoV-2 infection. Eye. 2020;34(12):2352–2353. doi: 10.1038/s41433-020-1069-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y, Li M, Wang M, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc Neurol. 2020;5(3):279. doi: 10.1136/svn-2020-000431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clark A, Jit M, Warren-Gash C, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. The Lancet Global Health. 2020;0(0). doi: 10.1016/S2214-109X(20)30264-3 [DOI] [PMC free article] [PubMed] [Google Scholar]