Abstract
Objective:
To examine the association of the volume and intensity of daily walking at baseline with the risk of knee replacement (KR) over five years in adults with advanced structural knee osteoarthritis.
Design:
Prospective, longitudinal, and multi-center observational study.
Setting:
Osteoarthritis Initiative study with follow-up from 2008 to 2015.
Participants:
Community-dwelling adults with or at risk of knee OA were recruited from four sites in the United States. We included participants with advanced structural disease, without KR and had valid daily walking data (quantified using Actigraph GT1M), at baseline.
Intervention:
Not applicable.
Main outcomes:
KR. Walking volume was measured as steps/day and intensity as minutes/day spent not walking (0 steps/min), and walking at very-light (1–49 steps/min), light (50–100 steps/min), or moderate (>100 steps/min) intensities. To examine the relationship of walking volume and intensity with the risk of KR, we calculated hazard ratios (aHR) and 95% confidence intervals (CI) adjusting for covariates.
Results:
Of 516 adults with advanced structural disease ([mean±sd] age: 67.7±8.6 years, BMI: 29.3±4.7 kg/m2, 52% female), 88 (17%) received a KR over five years. Walking an additional 1,000 steps/day was not associated with the risk of KR (adjusted HR 0.95, 95% CI [0.84, 1.04]). Statistically replacing 10 minutes/day of very-light and light walking with 10 minutes/day of moderate walking reduced the risk of KR incidence by 35% and 37%, respectively (adjusted HR 0.65, 95% CI [0.45 to 0.94] for very light, and adjusted HR 0.63, 95%CI [0.40 to 1.00] for light).
Conclusion:
Daily walking volume and intensity did not increase KR risk over five years, and may be protective in some cases in adults with advanced structural knee OA.
Keywords: knee replacement, daily walking, moderate-to-vigorous physical activit
Reference to the published conference abstracts:
Master H, Thoma L, Christiansen M, Mathews D, Macri E, Ziegler M, Stefanik JJ, White D. Friend or Foe: Does Walking at Higher Intensities Increase or Decrease the Risk of Total Knee Arthroplasty over Five Years? [abstract]. Arthritis & Rheumatology 2018; 70 (suppl 10).
Master, H., Thoma, L., Christiansen, M., Stefanik, J., Mathews, D., & White, D. K. (2018). Association of daily walking with the risk of total knee replacement over 5 years: an observational study. Osteoarthritis and Cartilage, 26, S237-S238.
Physical activity offers health benefits, including protection from cardiovascular disease, diabetes, and cancer1,2, enhanced psychological health3, and increased muscle strength4 and physical function5–8. Daily walking is the most common type of physical activity older adults employ for exercise9. Walking produces load on cartilage, which promotes nutrient exchange with synovial fluid10, an important mechanism for knee joint health. The frequency of daily walking can be measured by volume (total steps/day) and intensity (faster steps). For adults with knee osteoarthritis (OA) who have existing damage to cartilage and underlying bone, excessive volume and/or intensity of daily walking may have deleterious effects11–14, which may in turn, increase the risk of knee replacement (KR). Adults with knee OA have expressed the belief that exercise will only damage their knee and increase pain15. To date, however, studies of physical activity provide conflicting results showing that greater activity is associated with an increase16–19, decrease20, or has no relationship21,22 with KR. These conflicting results may be attributed to the employment of patient-reported and not objective measurement instruments of physical activity, and the absence of distinguishing between different intensities of physical activity.
Little is known about the association of daily walking, both in terms of volume and intensity, with the risk of KR among adults with knee OA. This is a major need given the increase in KR utilization in the United States23. One study using data from 1082 community-dwelling older adults in Tasmania reported greater walking volume was related to a small increase in the risk of KR, though walking intensity was not measured16. Studying the relationship of intensity with study outcomes is methodologically challenging. This is because the total time each day is fixed at 24 hours and increasing time at one intensity comes at the cost of decreasing time at another intensity. Hence, there is a need to simultaneously calculate the effects of added time at one intensity while accounting for less time at the other24. To overcome this challenge, we employed a statistical model, i.e., isotemporal substitution,25 to estimate the simultaneous effects of reallocating or replacing very-light and light intensity walking for an equal amount of time walking at a moderate intensity on the risk of KR incidence.
The purpose of this study was to investigate two aspects of daily walking, i.e., 1) volume and 2) intensity, with KR risk in adults with advanced structural knee OA. Given that daily walking has a positive relationship with physical function5–8 which, by extension, may lessen the risk of KR, we hypothesize that greater daily walking volume and higher intensity will not increase risk of KR in adults with advanced structural knee OA, but in fact may be protective and decrease risk.
Methods:
Study Design
The Osteoarthritis Initiative (OAI) is a large, multicenter, longitudinal cohort study of community-dwelling people with or at high risk of knee OA. Detailed descriptions of the study protocol and eligibility criteria have been published elsewhere26. Briefly, study participants were recruited from four clinical sites located in the United States (Maryland, Pennsylvania, Rhode Island, and Ohio). All participants consented to participate in the OAI study. People with rheumatoid or inflammatory arthritis, bilateral end-stage disease defined as severe joint space narrowing or total knee replacement in both knees, and those who used ambulatory aids other than a cane were excluded. Institutional review board approval was obtained from all OAI sites.
This study focused on a subset of the OAI cohort. We considered the 48-month visit as our analytic baseline, as this was the first visit in which objectively measured physical activity was collected. Other participants were not eligible because they completed the 48-month follow-up visit before the accelerometry study was initiated, were lost to follow-up, died, or withdrew from the study27. Of the 2712 OAI participants that were eligible for accelerometry study, 2172 consented to participate in the accelerometry study. We included participants who had valid accelerometry data and excluded those who had a KR at or before the 48-month follow-up visit or did not have advanced structural knee OA at the 48-month follow-up visit. (Figure 1). We defined adults with advanced structural knee OA as having Kellgren–Lawrence (KL) grade 3 or 4 on x-ray in one or both knees.
Figure 1:
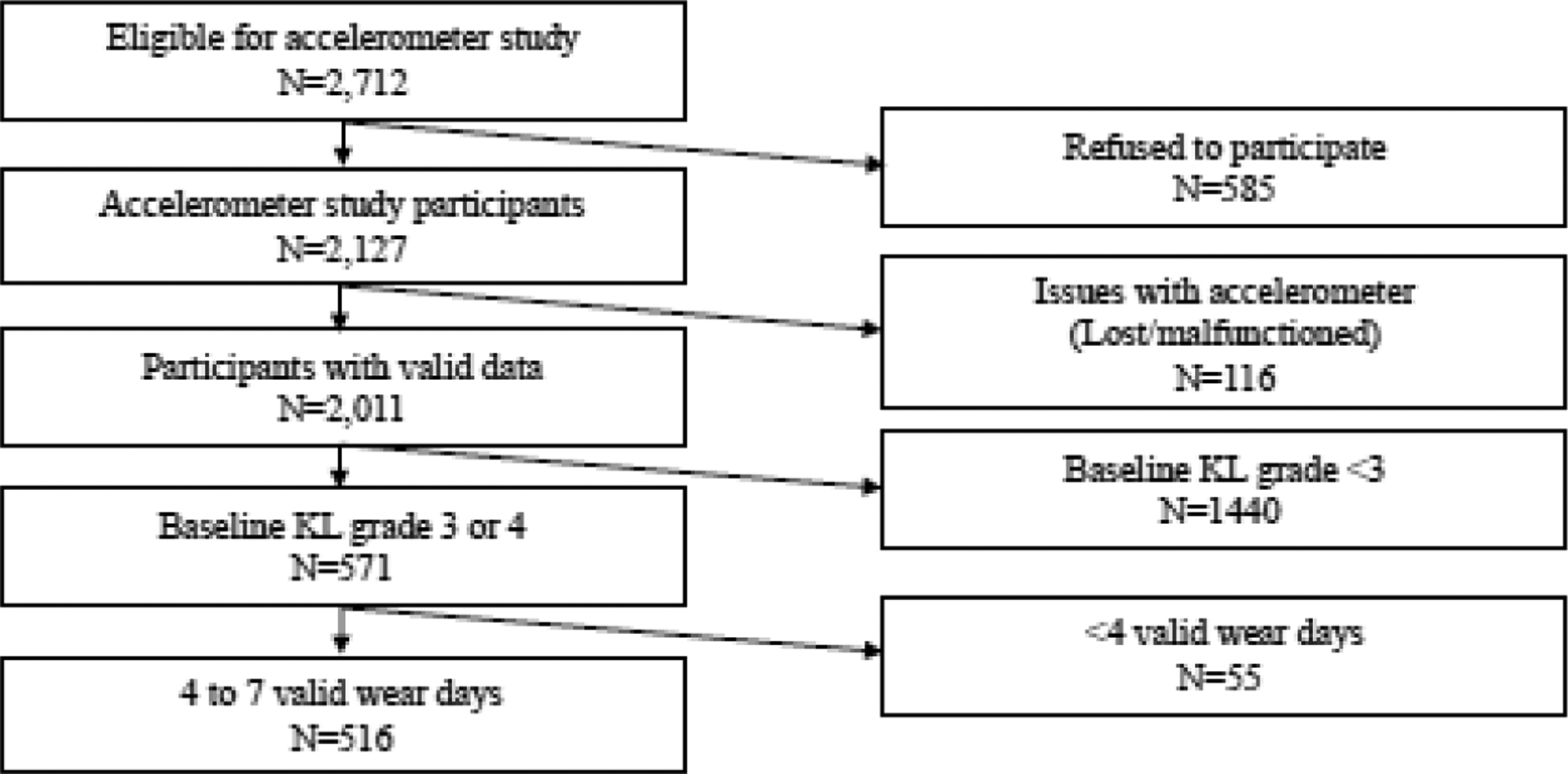
Data reduction from accelerometry OAI sample to the eligible analytical sample of study participants with advanced structural knee OA (KL grade 3 or 4) at baseline. (N=516)
Study Outcome
Time to KR was quantified in months from our study baseline visit date (conducted between 2008–2010) to the date of KR. Date of KR, when applicable, was collected through the 108-month clinic visit (conducted between 2013–2015). The date for KR was confirmed through adjudicated medical records when available. We censored participants without KR at the 108-month visit, or who were lost to follow-up or died during the 5-year study period (between 2008–2010 and 2013–2015).
Study Exposures
Daily walking was measured using a uniaxial accelerometer (Actigraph GT1M, Pensacola, FL, USA). The Actigraph GT1M is a device that validly quantifies physical activity in free-living conditions28–30. Subjects were fitted with the Actigraph GT1M above the right hip and were instructed to wear it during waking hours for seven consecutive days. We employed previously published methods to determine valid records31. In order to account for valid wear time, we identified and eliminated non-wear time, i.e., time the Actigraph was not worn, using a validated algorithm32. Specifically, non-wear time was identified if the accelerometer had registered >90 min of consecutive activity of <100 counts per min. We defined a valid wear day as ≥ 10 hours of valid wear time after eliminating non-wear time. We included participants with ≥ 4 valid wear days, which is the minimum number of days needed to reliably estimate free-living physical activity31.
We characterized daily walking as follows:
Volume.
Steps/day were averaged across the available valid days. As well, we categorized walking below or equal/above 4,000 to 10,000 steps/day in 1,000 step increments. Different cut points have been identified in previous studies to be associated with health outcomes in older adults (at least 4400 steps/day)33 and adults with knee OA (at least 6000 steps/day)7. Thus use employed a range of cut points to systematically study the association of volume with the risk of KR.
Intensity.
We measured minutes/day spent at different intensities of walking based on the number of steps/minute (i.e., step cadence)34. We defined 0 step/min as not walking, 1–49 steps/min as very-light walking, 50–100 steps/min as light walking, and >100 steps/min as moderate walking. Time spent walking at a vigorous intensity (>130 steps/min) was very rare in this sample. Therefore, we categorized >100 steps/min as moderate walking.
Potential Confounders
We considered the following factors that were measured at our analytic baseline, i.e., the 48-month OAI clinic visit, or at enrollment into OAI as potential confounders based on their association with daily walking and KR35,36: age, sex (female versus male), race/ethnicity (white versus non-white), education (no college or some college versus at least college graduate), body mass index (BMI, kg/m2) computed from standardized weight and height assessments, comorbidity using the modified Charlson comorbidity index (>1 versus none)37, index knee pain (determined using a 0–10 visual analog scale on the most painful knee), and history of knee injury or knee surgery, i.e., arthroscopy ligament repair, and meniscectomy (yes or no).
Statistical Analysis
We described the study sample using means and standard deviations for continuous variables and frequencies for categorical variables. We compared the demographic characteristics of participants with advanced structural knee OA who were included in the analytic sample versus those who were excluded using independent t-tests for continuous measures and Chi-square tests for categorical variables. To assess the association between walking volume and risk of KR, we calculated hazard ratios (HR) with 95% confidence intervals (CI) from Cox regression adjusted for potential confounders. Specifically, we executed separate models to investigate the relation of steps/day (i) continuous (i.e., per 1,000 steps/day) and (ii) categorical (< or ≥ different cut point of steps/day ranging from 4,000 to 10,000 steps/day) with the risk of KR over five years. To assess the association of walking at greater intensities with the risk of KR, we examined statistically replacing time walking at very-light walking and light walking with moderate walking using isotemporal substitution25. Isotemporal substitution was conducted within Cox regression models adjusted for potential confounders. 10 min/day was chosen as the duration of walking since this threshold is commonly used in the literature for people with knee OA,5,38,39 and represents a practical duration of walking in daily life.
We repeated analyses in adults with symptomatic knee OA since the presence of knee OA and/or symptoms may affect daily walking40 and the decision for a KR41. Adults with symptomatic knee OA were defined as the presence of KL grade ≥ 2 on x-ray in one or both knees, and pain, aching, or stiffness on most days of a month during the previous year in one or both knees. To account for competing events such as deaths and to confirm the direction of the effect estimates42, we repeated all analyses using competing risk analysis, i.e., Fine-Gray subdistribution hazard model instead of Cox regression model42,43. All analyses were adjusted for the potential confounders listed above and were conducted in SAS 9.4 (Cary, NC).
Results:
Of the 2,127 OAI participants who wore accelerometers at the 48-month visit, 571 had advanced structural disease and did not have a KR. Of these participants, 90% (516/571) had at least 4 valid wear days and were included in the analytic dataset (Figure 1). The analytic sample was 67.7±8.6 years of age (mean ± sd) with a BMI of 29.3±4.7 kg/m2 and over half were women (52%). The majority were white (81%) and had at least a college education (63%). Compared to those excluded (n=55), included participants (n=516) were older, more likely to be white, and graduate from college. 17% of the analytic sample (88/516) received a KR over five years (Table 1). The participants with symptomatic knee OA who were included in the sensitivity analysis had similar characteristics as described for those with advanced structural knee OA (Supplemental Table 1).
Table 1:
Characteristics of participants with advanced structural knee OA (Kellgren and Lawrence grade ≥3 in one or both knees) who were included and those who were excluded from the study
| Characteristics | Included | Excluded | p-value† |
|---|---|---|---|
| Sample size | 516 | 55 | |
| Age in years (Mean±SD) | 67.7±8.6 | 65.3±9.3 | 0.05 |
| Women (n (%)) | 268 (52) | 27 (49) | 0.69 |
| Race, white (n (%)) | 418 (81) | 36 (65) | 0.01 |
| Education, more than college | 323 (63) | 26 (47) | 0.03 |
| Body mass index in kg/m2 (Mean±SD) | 29.3±4.7 | 30.7±5.9 | 0.10 |
| VASˠ pain on a 0–10 scale (Mean±SD) | |||
| Right | 3.0±2.9 | 3.2±3.2 | 0.63 |
| Left | 2.7±2.8 | 2.6±2.9 | 0.77 |
| Index kneeˠˠ | 3.9±2.9 | 3.8±3.3 | 0.88 |
| Comorbidity (n (%)) | 174 (34) | 16 (29) | 0.49 |
| Presence of previous knee injuries/surgeries (n (%)) | 297 (58) | 37 (67) | 0.16 |
| People who had KR (n (%)) | 88 (17) | 8 (15) | 0.64 |
| Steps/day (Mean±SD) | 5,569±2,753 | - | - |
| Time spent in mins/day (Mean±SD) | |||
| not walking, 0 steps/min | 462.6±91.3 | - | - |
| very-light walking, 1–49 steps/min | 395.5±90.3 | - | - |
| light walking, 50–100 steps/min | 16.5±15.2 | - | - |
| moderate walking, >100 steps/min | 5.9±9.4 | - | - |
Visual analog scale
Index knee was the most painful knee identified using the VAS scale
p-value was obtained from independent t-test for continuous variables and Chi-square test for categorical variables to compare the characteristics of participants who included vs. those who were excluded.
Walking volume was not associated with the risk of KR. Walking an additional 1,000 steps/day did not change the risk of KR (adjusted HR 0.95, 95%CI [0.84, 1.04]). We found similar findings that did not meet statistical significance for cut points ranging from 4,000 steps/day to 10,000 steps/day (Table 2). We found similar results that did not reach statistical significance when repeating analyses for adults with symptomatic knee OA (Supplemental Tables 2 and 3). Applying a Fine-Gray sub-distribution hazard model to account for the competing risk of death produced similar effect estimates.
Table 2:
Summary of association of steps/day cut points to the risk of KR over five years in adults with advanced structural knee OA (Kellgren and Lawrence grade ≥3 in one or both knees) using unadjusted and adjusted Cox regression models (N=516).
| Daily walking cut points | Number of participants | KR n (%) | Unadjusted HR [95% CI] | Adjusted HR [95% CI]† |
|---|---|---|---|---|
| 4,000 steps/day | Below (n=168) | 31 (18) | 1.0 [Reference] | 1.0 [Reference] |
| Equal/Above (n=348) | 57 (16) | 0.83 [0.53, 1.28] | 0.97 [0.58, 1.61] | |
| 5,000 steps/day | Below (n=255) | 47 (18) | 1.0 [Reference] | 1.0 [Reference] |
| Equal/Above (n=261) | 41 (16) | 0.79 [0.52, 1.20] | 0.85 [0.51, 1.39] | |
| 6,000 steps/day | Below (n=322) | 58 (18) | 1.0 [Reference] | 1.0 [Reference] |
| Equal/Above (n=194) | 30 (15) | 0.80 [0.51, 1.24] | 0.83 [0.48, 1.41] | |
| 7,000 steps/day | Below (n=372) | 70 (19) | 1.0 [Reference] | 1.0 [Reference] |
| Equal/Above (n=144) | 18 (13) | 0.62 [0.37, 1.03] | 0.60 [0.34, 1.06] | |
| 8,000 steps/day | Below (n=421) | 74 (18) | 1.0 [Reference] | 1.0 [Reference] |
| Equal/Above (n=95) | 14 (15) | 0.79 [0.45, 1.40] | 0.74 [0.40, 1.39] | |
| 9,000 steps/day | Below (n=459) | 80 (17) | 1.0 [Reference] | 1.0 [Reference] |
| Equal/Above (n=57) | 8 (14) | 0.47 [0.37, 1.59] | 0.70 [0.33, 1.51] | |
| 10,000 steps/day | Below (n=478) | 85 (18) | 1.0 [Reference] | 1.0 [Reference] |
| Equal/Above (n=38) | 3 (8) | 0.42 [0.13, 1.32] | 0.38 [0.12, 1.23] |
HR=hazard ratio CI=confidence interval
Adjusted for age, BMI, sex, education, race, index knee pain defined using most painful knee on visual analog scale, comorbidities, and previous knee injuries/surgeries
Walking at moderate intensity was associated with less risk of KR (Table 3). Statistically replacing 10 mins/day of very-light and light walking with 10 mins/day of moderate walking was associated with 35% and 37% less risk of KR, respectively, which met statistical significance (adjusted HR 0.65, 95% CI [0.45, 0.94] for replacing very-light with moderate walking, and adjusted HR 0.63, 95% CI [0.40, 1.00] for replacing light with moderate walking). We found similar protective effect estimates that did not meet statistical significance when restricting our analyses to adults with symptomatic knee OA (Supplemental Table 4). Similar effect estimates for walking intensity were observed when we repeated the analyses using a Fine-Gray sub-distribution hazard model to account for the competing risk of death.
Table 3:
Effects of replacing lighter intensities with equal periods of walking at a moderate intensity on risk for KR over five years in adults with advanced structural knee OA (Kellgren and Lawrence grade ≥3 in one or both knees) (N=516).
| Walking intensity | Unadjusted HR [95%CI] | Adjusted HR [95%CI]† |
|---|---|---|
| Replacing 10 mins/day of very-light walking‡ with 10 mins/day of | ||
| Moderate walking‡‡ | 0.62 [0.42, 0.92]* | 0.65 [0.45, 0.94]* |
| Replacing 10 mins/day of light walking‡‡‡ with 10 mins/day of walking at | ||
| Moderate walking‡‡ | 0.57 [0.35, 0.92]* | 0.63 [0.40, 1.00]* |
HR=hazard ratio CI=confidence interval
Adjusted for age, BMI, sex, education, race, index knee pain defined using most painful knee on VAS scale, comorbidities, and previous knee injuries/surgeries
Very-light walking is defined as time spent in 1–49 steps/min
Moderate walking is defined as time spent in 50–100 steps/min
Denotes statistical significance, i.e., p-value<0.05 and 95%CI does not cross 1
Light walking is defined as time spent in >100 steps/min
Discussion:
Daily walking volume and intensity did not increase the risk of KR over five years in adults with advanced structural knee OA. In fact, we observed some protective effects of daily walking. In particular, more time spent walking at a moderate intensity instead of very-light or light intensities had modest protective effects that reached statistical significance. We found similar results in samples of adults with symptomatic knee OA. Our study findings provide preliminary evidence that daily walking may not increase KR risk, rather there is the possibility of decreasing risk over 5 years in adults with advanced structural knee OA.
One reason why daily walking may not have accelerated KR risk is the unsound relationship between daily walking and accelerated structural worsening. For example, adults with knee OA receiving an exercise intervention over 18 months as part of the Intensive Diet and Exercise for Arthritis (IDEA) trial, which included three 15 minute walking sessions per week, had similar joint space width loss and cartilage loss measured using MRI over the 18-month as those who received a diet intervention without the exercise intervention44. A systematic review and meta-analysis of five prospective cohort studies reported very limited and low-quality evidence to support a causal link between knee loading during walking and structural progression from MRI in adults with knee OA progression over 12 to 72 months45. One study did report greater walking volume (≥ 10,000 steps/day) to be related to structural worsening, i.e., increased the risk of worsening bone marrow lesions, meniscal pathology scores, and cartilage defects, which was especially true among those with pre-existing structural abnormalities, though worsening symptoms and KR were not recorded as clinical endpoints14.
One potential reason why daily walking may protect against KR is its known relationship with physical function in knee OA5,7,8. Limited physical function is one reason for KR,46 and those who walk more may better preserve functional ability than those who walk less. Greater total step/day7 and brisk steps5 are protective against poor physical function by preserving lower-extremity muscle strength4 and mitigating knee pain47. However, it is important to note that KR is elected for reasons other than limitations in physical function, such as evidenced by the growing number of replacements in younger adults who wish to maintain high levels of physical activity associated with recreational activities23. A major limitation to our study is the potential for confounding, that is, adults who walked more also had less structural disease and pain, and were consequently less likely to have KR. Given the observational nature of our study, we are unable to completely prevent the possibility of confounding by disease severity and/or knee pain. However, we attempted to limit this confounding by selecting a sample that had advanced structural disease, i.e., KL grade 3 or 4, and statistically adjusting for knee pain. As well, we repeated our analyses and found similar results in samples of adults with symptomatic knee OA.
Study Limitations
Our study has several additional limitations. Caution should be taken when generalizing our results beyond our study. Namely, our study follow-up time, i.e., 5 years, is less than the average time from diagnosis of knee OA to KR, which is 13 years48. As well, the definition of advanced structural disease was not related to knee pain intensity, thus it is unclear how well our findings generalize to those with mild, moderate, and severe knee pain. We did find similar results in adults with symptomatic knee OA, which was defined as pain, aching, or stiffness on most days of a month during the previous year in one or both knees in addition to KL ≥ 2 on x-ray in one or both knees. It is noteworthy that our analytic sample was predominantly white, overweight, and college-educated which may limit generalizability to the general population of adults with knee OA. We did not distinguish specific reasons for KR since these were not collected in the OAI. Lastly, we did not account for intercurrent events such as hospitalization or hip replacement, which may have occurred during follow-up. Despite these limitations, our study has several strengths, which include the use of longitudinal data from an existing large cohort, measurement of daily walking volume and intensity using an accelerometer, and employment of an analytic technique, isotemporal substitution, to estimate the effects of reallocating very-light or light walking with moderate walking.
Clinical implications and future directions
Our study findings are important and encouraging given that exercise is recommended as a first-line treatment strategy for knee OA by OA-related medical societies49,50 and walking is the most common type of physical activity older adults employ for exercise9. One preliminary goal for daily walking volume is 6,000 steps/day, which was found to distinguish between those who did and did not develop functional limitation over two years among 1,788 adults with or at high risk of knee OA from the Multicenter Osteoarthritis (MOST) study7. For intensity, we previously reported that 90% of adults from MOST self-selected a moderate intensity of walking, i.e., ≥ 100 steps/min, during a 20-meter walk test51. Thus, most adults with knee OA are capable of walking at a moderate intensity. Using a pedometer or activity tracker to measure daily walking paired with daily step goals is an effective strategy to increase daily walking52. Patient education about the benefits of exercise is critical, as misinformation about exercise for knee OA is common, i.e., that exercise-based interventions will only cause damage15. One potential strategy to increase daily walking is to consider referral to a physical therapist, who are experts in prescribing exercise for adults with chronic disease, and can educate patients about the benefits of exercise while addressing knee pain and limitations in physical function47. Physical Therapy is likely underutilized for knee OA. One study of health claims data from 11 million patients found that < 10% of adults with knee OA were prescribed Physical Therapy 5 years prior to a KR53. Future research should be geared towards exploring promising delivery models that may help bolster Physical Therapy utilization for OA. For instance, one model is telehealth because recent studies have shown this mode being acceptable to patients54, and effective to improve physical function for adults with knee OA55. Additonally, further research is needed to explore the impact of physical activity, in terms of volume and intensity, with other strucutral outcomes, relevant for knee OA population.
Conclusion:
Daily walking, both in terms of volume and intensity, did not accelerate the need for KR over 5 years, and in some cases, tended to decrease the risk of KR. Given the observational nature of this study, we cannot definitely conclude that daily walking volume and intensity at a moderate intensity led to a lower risk of knee replacement. Nevertheless, our findings support the recommendation to employ daily walking for exercise, and adds that daily walking, both in terms of volume and intensity, is unlikely to accelerate the need for future KR in adults with advanced knee OA.
Supplementary Material
Highlights.
Walking volume and intensity did not expedite knee replacement risk over 5 years.
More steps/day was not associated with risk of knee replacement over 5 years.
Walking at a moderate intensity was related to a small decrease in knee replacement risk.
Acknowledgment of financial support:
The study was supported in part by the University Doctoral fellowship award from Unidel Foundation, R21-AR071079-01A1, K12HD055931-01, K23AR070913, T32-HD007490, F32AR073090, K24-AR070892, and U54 GM104941. We have used publicly available data from the Osteoarthritis Initiative (OAI). The OAI is a public-private partnership composed of five contracts (N01-AR-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health (NIH), a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the NIH. This manuscript was prepared using an OAI public use dataset and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Acknowledgment of any presentation of this material:
Some parts of the manuscript were presented at the following conferences:
American College of Rheumatology/Association of Rheumatology Health Professionals Annual Meeting, and Osteoarthritis Research Society International World Congress.
List of abbreviations:
- OA
osteoarthritis
- KR
knee replacement
- OAI
Osteoarthritis Initiative
- KL
Kellgren–Lawrence
- BMI
Body mass index
- HR
hazard ratios
- CI
confidence interval
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Explanation of any conflicts of interest: There are no competing interests for any author. Also, all authors have no disclosures.
References:
- 1.O’Grady M, Fletcher J, Ortiz S. Therapeutic and physical fitness exercise prescription for older adults with joint disease: an evidence-based approach. Rheumatic Disease Clinics of North America. 2000;26(3):617–646. [DOI] [PubMed] [Google Scholar]
- 2.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. [DOI] [PubMed] [Google Scholar]
- 3.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28(1):1–8. [DOI] [PubMed] [Google Scholar]
- 4.Foong YC, Chherawala N, Aitken D, Scott D, Winzenberg T, Jones G. Accelerometer‐determined physical activity, muscle mass, and leg strength in community‐dwelling older adults. Journal of cachexia, sarcopenia and muscle. 2016;7(3):275–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fenton SAM, Neogi T, Dunlop D, et al. Does the intensity of daily walking matter for protecting against the development of a slow gait speed in people with or at high risk of knee osteoarthritis? An observational study. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunlop DD, Song J, Semanik PA, Sharma L, Chang RW. Physical activity levels and functional performance in the osteoarthritis initiative: a graded relationship. Arthritis & Rheumatism. 2011;63(1):127–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White DK, Tudor‐Locke C, Zhang Y, et al. Daily walking and the risk of incident functional limitation in knee osteoarthritis: an observational study. Arthritis care & research. 2014;66(9):1328–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunlop DD, Song J, Hootman JM, et al. One Hour a Week: Moving to Prevent Disability in Adults With Lower Extremity Joint Symptoms. Am J Prev Med. 2019;56(5):664–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yusuf HR, Croft JB, Giles WH, et al. Leisure-time physical activity among older adults: United States, 1990. Arch Intern Med. 1996;156(12):1321–1326. [PubMed] [Google Scholar]
- 10.Sun HB. Mechanical loading, cartilage degradation, and arthritis. Annals of the New York Academy of Sciences. 2010;1211:37–50. [DOI] [PubMed] [Google Scholar]
- 11.Lin W, Alizai H, Joseph GB, et al. Physical activity in relation to knee cartilage T2 progression measured with 3 T MRI over a period of 4 years: data from the Osteoarthritis Initiative. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2013;21(10):1558–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stehling C, Lane NE, Nevitt MC, Lynch J, McCulloch CE, Link TM. Subjects with higher physical activity levels have more severe focal knee lesions diagnosed with 3 T MRI: analysis of a non-symptomatic cohort of the osteoarthritis initiative. Osteoarthritis and cartilage. 2010;18(6):776–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar D, Souza RB, Singh J, et al. Physical activity and spatial differences in medial knee T1rho and t2 relaxation times in knee osteoarthritis. J Orthop Sports Phys Ther. 2014;44(12):964–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dore DA, Winzenberg TM, Ding C, et al. The association between objectively measured physical activity and knee structural change using MRI. Ann Rheum Dis. 2013;72(7):1170–1175. [DOI] [PubMed] [Google Scholar]
- 15.Bunzli S, O’Brien BhealthSci P, Ayton D, et al. Misconceptions and the Acceptance of Evidence-based Nonsurgical Interventions for Knee Osteoarthritis. A Qualitative Study. Clinical orthopaedics and related research. 2019;477(9):1975–1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Munugoda IP, Wills K, Cicuttini F, et al. The association between ambulatory activity, body composition and hip or knee joint replacement due to osteoarthritis: a prospective cohort study. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2018;26(5):671–679. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Simpson JA, Wluka AE, et al. Is physical activity a risk factor for primary knee or hip replacement due to osteoarthritis? A prospective cohort study. The Journal of rheumatology. 2011;38(2):350–357. [DOI] [PubMed] [Google Scholar]
- 18.Leung YY, Bin Abd Razak HR, Talaei M, Ang LW, Yuan JM, Koh WP. Duration of physical activity, sitting, sleep and the risk of total knee replacement among Chinese in Singapore, the Singapore Chinese Health Study. PLoS One. 2018;13(9):e0202554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnsen MB, Hellevik AI, Baste V, et al. Leisure time physical activity and the risk of hip or knee replacement due to primary osteoarthritis: a population based cohort study (The HUNT Study). BMC musculoskeletal disorders. 2016;17:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richey PA, Johnson KC, Neiberg RH, et al. Association of the Intensive Lifestyle Intervention With Total Knee Replacement in the Look AHEAD (Action for Health in Diabetes) Clinical Trial. J Arthroplasty. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ageberg E, Engstrom G, Gerhardsson de Verdier M, Rollof J, Roos EM, Lohmander LS. Effect of leisure time physical activity on severe knee or hip osteoarthritis leading to total joint replacement: a population-based prospective cohort study. BMC musculoskeletal disorders. 2012;13:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skou ST, Wise BL, Lewis CE, Felson D, Nevitt M, Segal NA. Muscle strength, physical performance and physical activity as predictors of future knee replacement: a prospective cohort study. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2016;24(8):1350–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94(3):201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pelclová J, Štefelová N, Dumuid D, et al. Are longitudinal reallocations of time between movement behaviours associated with adiposity among elderly women? A compositional isotemporal substitution analysis. International journal of obesity (2005). 2020;44(4):857–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. American journal of epidemiology. 2009;170(4):519–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Riddle DL, Kong X, Jiranek WA. Two-year incidence and predictors of future knee arthroplasty in persons with symptomatic knee osteoarthritis: preliminary analysis of longitudinal data from the osteoarthritis initiative. The Knee. 2009;16(6):494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dunlop DD, Song J, Semanik PA, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis and rheumatism. 2011;63(11):3372–3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 Suppl):S531–S543. [DOI] [PubMed] [Google Scholar]
- 29.Berlin JE, Storti KL, Brach JS. Using activity monitors to measure physical activity in free-living conditions. Phys Ther. 2006;86(8):1137–1145. [PubMed] [Google Scholar]
- 30.Matthews CE, Ainsworth BE, Thompson RW, Bassett DR Jr. Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34(8):1376–1381. [DOI] [PubMed] [Google Scholar]
- 31.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181. [DOI] [PubMed] [Google Scholar]
- 32.Song J, Semanik P, Sharma L, et al. Assessing physical activity in persons with knee osteoarthritis using accelerometers: data from the osteoarthritis initiative. Arthritis care & research. 2010;62(12):1724–1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee I-M, Shiroma EJ, Kamada M, Bassett DR, Matthews CE, Buring JE. Association of Step Volume and Intensity With All-Cause Mortality in Older Women. JAMA Intern Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tudor-Locke C, Camhi SM, Leonardi C, et al. Patterns of adult stepping cadence in the 2005–2006 NHANES. Prev Med. 2011;53(3):178–181. [DOI] [PubMed] [Google Scholar]
- 35.Sharma L, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis and rheumatism. 2003;48(12):3359–3370. [DOI] [PubMed] [Google Scholar]
- 36.Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. Am J Public Health. 1990;80(8):945–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996:73–84. [DOI] [PubMed] [Google Scholar]
- 38.Wallis J, Webster K, Levinger P, Singh P, Fong C, Taylor N. The maximum tolerated dose of walking for people with severe osteoarthritis of the knee: a phase I trial. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2015;23(8):1285–1293. [DOI] [PubMed] [Google Scholar]
- 39.Song J, Dunlop DD, Semanik PA, et al. Reallocating time spent in sleep, sedentary behavior and physical activity and its association with pain: a pilot sleep study from the Osteoarthritis Initiative. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2018;26(12):1595–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Song J, Chang AH, Chang RW, et al. Relationship of knee pain to time in moderate and light physical activities: Data from Osteoarthritis Initiative. Semin Arthritis Rheum. 2018;47(5):683–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carr AJ, Robertsson O, Graves S, et al. Knee replacement. Lancet. 2012;379(9823):1331–1340. [DOI] [PubMed] [Google Scholar]
- 42.Austin PC, Fine JP. Practical recommendations for reporting Fine-Gray model analyses for competing risk data. Stat Med. 2017;36(27):4391–4400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. [Google Scholar]
- 44.Hunter DJ, Beavers DP, Eckstein F, et al. The Intensive Diet and Exercise for Arthritis (IDEA) trial: 18-month radiographic and MRI outcomes. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2015;23(7):1090–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Henriksen M, Creaby MW, Lund H, Juhl C, Christensen R. Is there a causal link between knee loading and knee osteoarthritis progression? A systematic review and meta-analysis of cohort studies and randomised trials. BMJ open. 2014;4(7):e005368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zeni JA, Axe MJ, Snyder-Mackler L. Clinical predictors of elective total joint replacement in persons with end-stage knee osteoarthritis. BMC musculoskeletal disorders. 2010;11(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med. 2015;49(24):1554–15574. [DOI] [PubMed] [Google Scholar]
- 48.Losina E, Paltiel AD, Weinstein AM, et al. Lifetime medical costs of knee osteoarthritis management in the United States: impact of extending indications for total knee arthroplasty. Arthritis care & research. 2015;67(2):203–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis & Rheumatology. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2019;27(11):1578–1589. [DOI] [PubMed] [Google Scholar]
- 51.White DK, Tudor-Locke C, Felson DT, et al. Do radiographic disease and pain account for why people with or at high risk of knee osteoarthritis do not meet physical activity guidelines? Arthritis and rheumatism. 2013;65(1):139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–2304. [DOI] [PubMed] [Google Scholar]
- 53.Dhawan A, Mather RC 3rd, Karas V, et al. An epidemiologic analysis of clinical practice guidelines for non-arthroplasty treatment of osteoarthritis of the knee. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2014;30(1):65–71. [DOI] [PubMed] [Google Scholar]
- 54.Lawford BJ, Delany C, Bennell KL, Hinman RS. “I Was Really Pleasantly Surprised”: Firsthand Experience and Shifts in Physical Therapist Perceptions of Telephone-Delivered Exercise Therapy for Knee Osteoarthritis-A Qualitative Study. Arthritis care & research. 2019;71(4):545–557. [DOI] [PubMed] [Google Scholar]
- 55.Hinman RS, Campbell PK, Lawford BJ, et al. Does telephone-delivered exercise advice and support by physiotherapists improve pain and/or function in people with knee osteoarthritis? Telecare randomised controlled trial. British journal of sports medicine. 2019:bjsports-2019–101183. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


