Highlights
-
•
Mixed functional/organic tremor has longer duration to diagnosis than other tremors.
-
•
Electrophysiologic studies guide the diagnosis in clinically indeterminate tremors.
-
•
Variability on electrophysiologic testing is associated with a change in diagnosis.
Keywords: Electrophysiology, Functional tremor, Distractibility, Entrainment
Abstract
Objective
To determine the utility of tremor electrophysiology testing in differentiating clinically indeterminate tremor due to organic, functional, and mixed tremor types.
Background
Prior studies have shown that electrophysiological studies increase diagnostic sensitivity of tremor syndromes; however, few have examined mixed organic and functional tremors.
Methods
Patients referred for tremor to the Mayo Clinic, Rochester movement disorders lab were consecutively selected and retrospectively reviewed. Surface electromyography (EMG) recordings of upper limb muscles were performed at rest, posture, with action and distractibility tasks.
Results
Of 116 patients, all were clinically described as having either a resting tremor, postural tremor, action tremor, postural and action tremor, mixed resting, postural, and action tremor, or nonspecific tremulousness. Based on electrophysiological features, patients were diagnosed with organic tremor (parkinsonian, essential, mixed, rubral, cerebellar, non-specific tremulousness), functional tremor, or mixed functional and organic tremors. The median disease duration at electrophysiological confirmation of diagnosis was shorter for functional tremor at 1.5 years (IQR 1–9.3), and organic tremor at 3 years (IQR 1–15), versus mixed organic and functional tremor at 11 years (IQR 2–15) (p = 0.0422). The electrophysiology study clarified the referral/clinical diagnosis in 87 patients (75%), 26 (29.5%) of whom had functional tremor, and 61 (70.1%) had organic tremor or mixed organic/functional tremor. Variability of tremor during electrophysiology testing was associated with a change in diagnosis (p = 0.0286).
Conclusion
Our findings show that electrophysiological assessment of tremor can be helpful in the clinical diagnosis of patients with both organic and functional tremor.
1. Introduction
Tremor is a characterized by a rhythmic involuntary oscillation along a fixed point [1]. While various clinical features can aid in the classification of different tremor types, bedside examination can be unreliable and carries inherent limitations. Commonly encountered diagnostic challenges include difficulty distinguishing multiple tremor types in the same individual and difficulty distinguishing organic versus functional tremor disorder. However, even in patients with a single tremor disorders such as essential tremor, clinical misdiagnosis rates are estimated around 37%, as these patients are sometimes later diagnosed with Parkinson’s disease, or mixed Parkinson’s disease and essential tremor [2].
In patients with functional tremor, early recognition and management are critical to guide appropriate management strategies and avoid excessive testing or unnecessary medications [3].
Electrophysiological testing can be helpful in objectively analyzing selected tremor disorders [3], [4].
Prior studies have validated laboratory supported criteria for diagnosis of functional tremor, which emphasize entrainment, distractibility, co-contraction pattern, amplitude increase with loading, and variability of tremor frequency during contralateral finger tapping, with high sensitivity and specificity (89.5% and 95.9% respectively) [5], [6]. Studies have also shown how tremor frequencies produced by one or multiple oscillators are fixed, and can be differentiated by comparing frequencies of oscillations in different limbs with coherence analysis [3], [7]. However, few studies have demonstrated clinical utility of electrophysiology in clinically indeterminate tremor disorders, and how this data can aid accurate and prompt tremor-specific diagnosis, especially amongst patients with mixed tremor disorders.
We sought to describe the clinical and electrophysiological features of tremor in a large consecutively selected retrospective cohort of patients and determine how electrophysiological features aid in diagnosis and management of different tremor disorders.
2. Methods
2.1. Study design
This study was approved by the Mayo Clinic Institutional Review Board before the patients were selected for analysis. All included patients had previously signed a general informed consent form allowing their medical records to be used for research purposes. 116 consecutively sampled patients with clinically indeterminate tremor who were referred to the Mayo Clinic, Rochester, MN movement disorders lab for electrophysiological testing of upper limb tremor in 2018 were retrospectively reviewed. Indeterminate tremor was defined as: 1) tremor noted on clinical exam that did not meet clinical criteria for any clearly defined syndrome, 2) if there was concern for an underlying functional tremor, or 3) two clinically distinct tremor types on examination concerning for multiple tremor diagnoses. In patients who were referred for testing, the referral diagnosis code listed in the test order was obtained and considered the “referral diagnosis”. All patients underwent tremor electrophysiology studies within 3 months of the neurologic consultation. Tremors were categorized based on clinical phenotype and electrophysiological features based on established criteria, and the criteria for tremor diagnosis used in the Movement Disorders Laboratory at Mayo Clinic Rochester are listed as Supplementary Material [3], [7]. Other variables such as demographics, time to diagnosis, and family history were collected. Imaging was reviewed in all patients on whom it was obtained.
2.2. Tremor electrophysiology testing
A standardized tremor protocol was performed, and electrophysiology data was obtained via surface electromyography (EMG) electrodes placed on biceps, wrist extensors, wrist flexors, and first dorsal interosseous muscles bilaterally. Tremor was assessed in various positions; rest, cognitive distraction, posture (arms outstretched, and hands held near the face), and action such as finger-nose-finger or holding a cup. Time-frequency analysis was performed to determine the tremor frequency and variation over time. Variability was defined as a change in the frequency of tremor during the recording by more than 2 Hz; this threshold was selected as tremor frequencies less than 2 Hz were considered fixed and within expectation for organic tremor caused by a central nervous system oscillator [7]. Patients were asked to tap their fingers with the contralateral limb at different fixed frequencies with a metronome to assess for distraction or entrainment. Weight loading and response to ballistic movements were not consistently performed in all patients and not included for analysis. Final diagnoses were obtained from the electrophysiology report by the movement disorder neurologist which were made based on published diagnostic criteria in regards to functional versus organic tremor [1], [3], [6]. Essential tremor, parkinsonian tremor, rubral tremor, enhanced physiologic tremor, and intention tremor were diagnosed based on a combination of clinical phenotype and electrophysiologic characteristics including frequency, amplitude change with posture, component, and coherence (FA, AH, JHB, BTK, JYM, EAC) (see Supplementary material) [1], [3], [6].
2.3. Statistical analysis
JMP statistical software was used to perform statistical analyses, with statistical significance set at p < 0.05. Categorical data was analyzed using χ2 testing; continuous variables analyzed using the Student’s t-test.
3. Results
3.1. Demographics
Over the last 15 years, on average 3% (n = 1752) of patients seen at Mayo Clinic, Rochester, MN Neurology clinic for tremor were referred for movement electrophysiology testing. Patients are often referred for electrophysiological assessment if tremor type is not definitively clear on clinical exam, more than one tremor type exists, or in some cases of suspected functional tremor. Of the 116 patients consecutively sampled who were referred to the laboratory for tremor assessment, 54% were females (n = 63). The median age of onset was 44 (interquartile range 31–57). Out of all the patients with tremor, anxiety was diagnosed in 29% (n = 34), and depression was present in 41%, (n = 48). Twenty-one patients (18%) in the group were referred for a movement study as part of a pre-operative evaluation for Deep Brain Stimulation (DBS) to confirm tremor type. A family history of essential tremor was present in 21% (n = 24) and Parkinson Disease was present in 9% (n = 10).
3.2. Clinical features
All 116 patients’ tremor phenotypes were classified based on the initial clinical impression of the evaluating neurologist as follows: resting tremor 11% (n = 13), postural tremor 9% (n = 10), action tremor 3% (n = 4), postural/action tremor 41% (n = 48), mixed resting and postural/action tremor 29% (n = 34), non-specific tremulousness 6% (n = 7).
Both anxiety and depression were more likely to be present in patients with functional tremor (50%, n = 13 and 65%, n = 17) as compared to patients with organic tremor (23%, n = 19, and 33%, n = 28) (p = 0.0068 and p = 0.0027 respectively). Patients with mixed functional and organic tremors had no significant difference in history of anxiety or depression (29%, n = 2) as compared to those with organic tremor (43%, n = 3) (p = 0.977 and p = 0.881). Median time duration between symptom onset and diagnosis was the longest for mixed functional and organic tremor being 11 years, (IQR 2–15), as compared to 1.5 years (IQR 1.-9.3) for functional tremor and 3 years (IQR 1–15) for organic tremor (p = 0.042). See Table 1 for further information.
Table 1.
Patient demographics and clinical characteristics.
| Organic tremor (79/116) | Functional tremor (26/116) | Mixed functional/organic tremor (7/116) | |
|---|---|---|---|
| Gender (male) | 43 (54) | 7 (27) | 4 (57) |
| Age of onset (y) | 46 (31–59) | 37 (31–48) | 40 (20–56) |
| Duration of symptoms (y) | 3 (1–15) | 1.5 (1–9) | 11 (2–15) |
| Anxiety | 19 (24) | 13 (50) | 2 (29) |
| Depression | 28 (35) | 17 (65) | 3 (43) |
| MRI completed | 41 (51) | 10 (38) | 4 (57) |
Categorical variables are shown as number (percentage, or interquartile range). Four patients had no tremor on testing and were not included.
3.3. Tremor diagnosis
Final electrophysiological diagnoses were as follows: parkinsonian tremor (n = 16), essential tremor (n = 23), mixed parkinsonian and essential tremor (n = 9), functional tremor (n = 26), non-specific tremulousness (n = 7), rubral tremor (n = 2), postural tremor (n = 1), mixed parkinsonian tremor and functional tremor (n = 1), mixed functional tremor and essential tremor (n = 6), cerebellar tremor (n = 10), enhanced physiologic tremor (n = 11), and no tremor was detected in some (n = 4).
Patients who were ultimately diagnosed with parkinsonian tremor had minimal features of parkinsonism such as bradykinesia, rigidity, or postural instability based on clinical examination making the clinical diagnosis alone less uncertain thus likely prompting the referral for testing [10]. Of the patients who were diagnosed with essential tremor, one patient also had ataxia; and three patients had a resting tremor component on examination; none of the other patients met criteria for essential tremor plus syndrome [1].
Of the 116 patients who underwent tremor electrophysiology testing, the final electrophysiologic report was considered to add diagnostic value to the referral diagnosis in 75% (n = 87), which was defined as: 1) if a second previously unidentified tremor etiology was revealed by electrophysiology testing (18%, n = 16), 2) if a change in the previously suspected clinical diagnosis was made as a result of testing (10%, n = 9), or 3) if the final diagnosis based on electrophysiology was more specific than the referral impression (72%, n = 62). Of note, the referral diagnosis code for patients in group 3 was “tremor not otherwise specified”, thus the degree of clinical suspicion of functional or organic tremor prior to referral was less certain. The final diagnosis was made at a follow-up visit after testing was complete and took into consideration all prior imaging and medication challenges prior to determining the diagnosis. The clinician referral diagnosis and electrophysiology diagnosis matched in 25% of cases (n = 29). Based on the above, the final electrophysiological testing was considered to add diagnostic value in the assessment of 26% of essential tremor patients (n = 7), 69% in parkinsonian tremor patients (n = 11), and 88% of functional tremor patients (n = 23), and all patients with mixed tremor syndromes, non-specific tremulousness, rubral, cerebellar, and enhanced physiologic tremors.
Of the patients where a change in diagnosis was made based on electrophysiological testing, one was referred for orthostatic tremor and found to have parkinsonian tremor (low frequency subclinical resting tremor of both legs with no evidence of orthostatic tremor observed on electrophysiology), two were referred for non-specific tremulousness and found to have functional tremor, one thought to have orthostatic tremor was found to have functional tremor, and one with postural tremor not otherwise specified was found to have functional tremor. One patient referred for a suspected parkinsonian tremor without any additional features of parkinsonism on examination was diagnosed with nonspecific tremulousness. One patient was referred for essential tremor and found to have cerebellar tremor. Another patient was referred for non-specific tremulousness and found to have enhanced physiologic tremor. One patient was referred for parkinsonian tremor and diagnosed with essential tremor on electrophysiology. This patient had an outside diagnosis of Parkinson disease and resting tremor on exam without other features of parkinsonism and was ultimately thought to have a predominant postural/kinetic tremor upon clinical examination.
Sixteen patients underwent [123I] N-ω-fluoropropyl-2β-carbomethoxy-3β-(4-iodophenyl) nortropane (123I-FP-CIT SPECT, or DAT) imaging within the 3 months of their work up with a movement laboratory study; 8 of which were abnormal. Out of the patients DAT scans, 41% (n = 7) were found to change management. This was determined if a patient’s subsequent medication or surgical management was changed because of the imaging, and was also considered after electrophysiology testing when determining the final diagnosis. For example, if a patient was found to have a mixed organic postural kinetic tremor and resting tremor that could not be differentiated from long-standing essential tremor or essential tremor with a parkinsonian tremor, then a subsequent DAT scan was found to be helpful as this could clarify whether or that there was an underlying parkinsonian component to the tremor.
3.4. Electrophysiology features
Frequency of tremor was recorded in 0.1 Hz (Hz) increments and assigned to categorical groups of 3 Hz increments, for example 1–3 Hz, 4–6 Hz and so on up to a maximum of 13 Hz. Tremor was defined as being variable and hence less likely to be organic, if the frequency varied more than 2 Hz in range [7]. Table 2 summarizes the predominant tremor frequencies in each tremor type. Example surface electromyography and time frequency graphs of common tremor types are illustrated in Fig. 1, Fig. 2.
Table 2.
Frequencies of different tremor types.
| 1–3 Hz | 4–6 Hz | 7–10 Hz | 11–13 Hz | Variable Hz | |
|---|---|---|---|---|---|
| Cerebellar (10) | 4 (40%) | 6 (60%) | |||
| Parkinsonian (16) | 16 (100%) | ||||
| Essential (23) | 17 (73%) | 6 (26%) | |||
| Functional (26) | 6 (23%) | 3 (12%) | 17 (65%) | ||
| Non-specific tremulousness (7) | 7 (100%) | ||||
| Enhanced physiologic (11) | 2 (18%) | 5 (45%) | 4 (36%) | ||
| Rubral tremor (2) | 2 (100%) |
Categorical variables are shown as number (percentage).
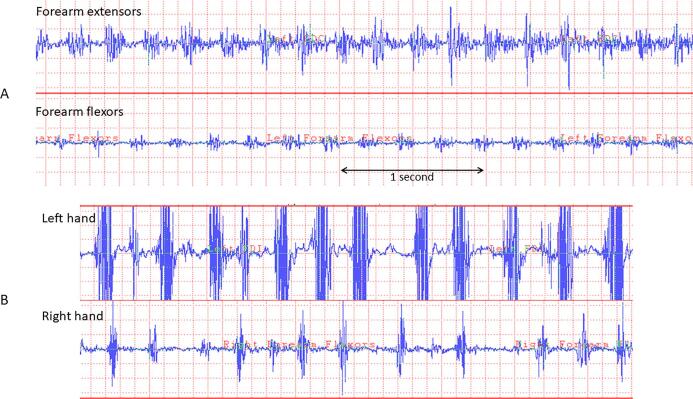
Fig. 1.
Surface EMG of organic and functional tremor. A: Alternating rhythmic EMG bursts are recorded over the wrist extensor and flexor muscles. Rest or postural tremor may have a similar electrophysiologic appearance and will be characterized by limb position during recording. B: Patient performs finger tapping at pre-set frequencies with the left hand (LH). The tremor in the right hand (RH) becomes variable in frequency.
Fig. 2.
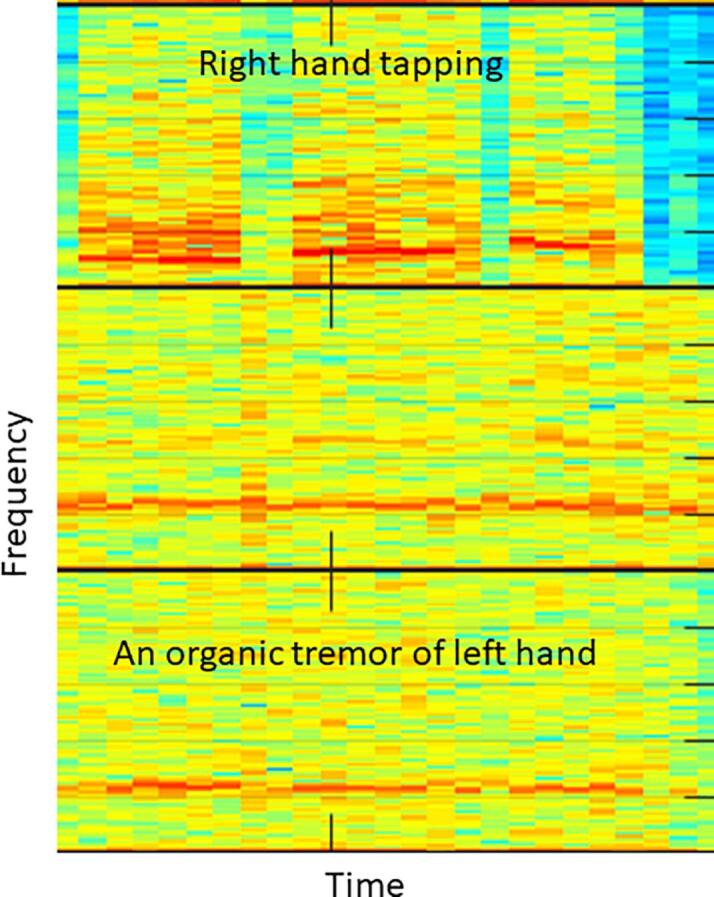
Time frequency analysis of organic tremor: Organic tremor will have a fixed frequency that persists during contralateral finger tapping.
Contralateral motor distration maneuvers were performed in 85% of patients. This is done by contralateral finger tapping at 2, 2.5 and 3 Hz. Accuracy of timed tapping was considered adequate in 85% of the patients who performed tapping.
Tremor frequency was fixed in 93% of those with parkinsonian tremor (n = 15), 100% essential tremor (n = 23), 8% functional tremor (n = 2), 100% cerebellar tremor (n = 10), and 100% enhanced physiologic tremor (n = 11). Tremor was distractible with contralateral finger tapping in 88% with functional tremor (n = 21), 50% rubral tremor (n = 1), and in 50% with mixed essential tremor/functional tremor (n = 3). Three patients diagnosed with functional tremor or mixed essential tremor and functional tremor demonstrated entrainment. Variation during tapping tasks was noted in functional tremors (n = 13, 54%), mixed essential tremor and parkinsonian tremor (n = 1, 11%), and mixed essential tremor and functional tremor (n = 3, 50%).
Of the patients who had a change in diagnosis as a result of electrophysiology testing, 66% (n = 6) had varability (p = 0.0286), 50% had distractibilty (p = 0.097), and none had entrainment (p = 0.46) on electrophysiology testing.
4. Discussion
Patients with tremor may have a variable presentation and clinical phenomenology does not always match characteristic clinical descriptions. Electrophysiological testing of tremor can be valuable in distinguishing organic from functional tremor, or mixed tremor disorders [3], [4], [7]. The objective information regarding frequencies and patterns can sometimes facilitate early diagnosis, assess need for advanced neuroimaging, and select a therapeutic direction to pursue. In our patient population, patients who had mixed tremor had a significantly longer time to diagnosis (11 years) as compared to functional tremor (1.5 years) and organic tremor (3 years). Tremor electrophysiology may be especially useful in cases of mixed tremor where the phenotype is more difficult to determine on clinical exam alone. Although DAT or MRI imaging may still be needed in some cases, patients could be selected more judiciously based on tremor electrophysiology data before pursuing more costly neuroimaging. Electrophysiological assessment of tremor is also a relatively simple, and well tolerated test making it patient friendly [3].
Tremor electrophysiology can advance our understanding of tremor disorders by objectively capturing tremor characteristics and heterogeneity across organic and functional tremor syndromes. In this cohort, distractibility and variability were noted in all functional or mixed organic/functional tremors except for two patients. The first patient had a history of traumatic brain injury and was diagnosed with organic rubral tremor based on having regular rhythmic EMG burst activity of the arm muscles at 4z frequency, though did have distractibility with finger tapping. This patient had significant dysexecutive function which was thought to have contributed to functional overlay. The second patient was diagnosed with mixed parkinsonism and essential tremor but was noted to have variable frequency of tremor during testing; however, this was thought to be secondary to altered stance position and only noted in the leg. Patients with an organic postural tremor may demonstrate variability in tremor based on limb position that may account for apparent distractibility noted in some cases of organic postural tremor and should be interpreted carefully.
Electrophysiology testing guided the clinical diagnosis in 75% of patients with organic, functional, and mixed tremor syndromes. Variability on electrophysiology testing was significantly associated with a change in the referral diagnosis, suggesting that this characteristic is especially important in tremor protocols. This demonstrates that electrophysiology testing can play a vital role in determining the diagnosis which may change medical and surgical management in patients with tremor disorders. In patients with functional tremor, electrophysiological data can also be helpful in facilitating patient counseling, and lead to ultimate acceptance of the diagnosis and effectiveness of therapy [5], [6], [7], [8].
In addition, most patients who underwent neuroimaging ultimately were diagnosed based on electrophysiological testing and imaging did not alter the treatment plan. However, presynaptic dopamine transport imaging is indicated in patients when it is necessary to differentiate tremor related to parkinsonism from other tremor syndromes [11].
Interestingly, we also found that in patients who had mixed functional and organic tremor that there was not an increased risk of associated anxiety and depression, suggesting that there may be less clinical suspicion upon initial evaluation that these patients have a functional component to the tremor.
Strengths of this study include the large tremor cohort and multiple tremor types that were included in analysis. Previous studies have described electrophysiological characteristics of the main tremor syndromes; however few studies have described clinical utility of such testing demonstrated by how frequently electrophysiologic testing can identify functional and mixed tremor syndromes which are missed in clinic and could theoretically reduce diagnostic delay and the need for more expensive diagnostic testing [3], [4], [7], [8], [9].
Limitations include the retrospective nature of the study. Data was not collected on long-term outcomes and symptom evolution after initial diagnosis given the tertiary referral nature and lack of sustained follow-up among patients. The lack of long-term outcomes limits what we can definitively say about the extent of the role of electrophysiology testing in the diagnosis of tremor, which can be clarified in future prospective studies. Also, the time from symptom onset to diagnosis in patients with tremor syndromes likely varied as a consequence of referral bias at a specialized movement disorders center. In addition, there may be a tertiary referral bias towards more complex tremor patients which may limit the generalizability of this study to all patients with tremor. Although there are validated criteria for electrophysiologic diagnosis of functional tremor, other forms of tremor have less objective diagnostic criteria which have been validated and thus accuracy is less certain in comparison to the gold standard of clinical diagnosis.
Future directions should include a larger prospective longitudinal cohort to assess electrophysiological heterogeneity in tremor disorders such as essential tremor plus, and dystonic tremor. In addition, future studies could explore the diagnostic utility of tremor electrophysiology in clinical practice, and development of potential electrophysiological biomarkers such as tremor signatures in tremor disorders.
5. Sponsors
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Lauren Jackson: Conceptualization, Investigation, Methodology, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Bryan T. Klassen: Data curation, Formal analysis, Writing – review & editing. Anhar Hassan: Data curation, Formal analysis, Writing – review & editing. James H. Bower: Data curation, Formal analysis, Writing – review & editing. Joseph Y. Matsumoto: Data curation, Formal analysis. Elizabeth A. Coon: Data curation, Formal analysis, Writing – review & editing. Farwa Ali: Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.prdoa.2021.100108.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Bhatia K.P., Bain P., Bajaj N., Elble R.J., Hallett M., Louis E.D., Raethjen J., Stamelou M., Testa C.M., Deuschl G. Consensus Statement on the classification of tremors. from the task force on tremor of the International Parkinson and Movement Disorder Society. Mov. Disord. 2018;33(1):75–87. doi: 10.1002/mds.27121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jain S., Lo S.E., Louis E.D. Common misdiagnosis of a common neurological disorder. Arch. Neurol. 2006;63:1100. doi: 10.1001/archneur.63.8.1100. [DOI] [PubMed] [Google Scholar]
- 3.Vial F., Kassavetis P., Merchant S., Haubenberger D., Hallett M. How to do an electrophysiological study of tremor. Clin. Neurophysiol. Pract. 2019;4:134–142. doi: 10.1016/j.cnp.2019.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wardt J.V.d., van der Stouwe A.M.M., Dirkx M., Elting J.W.J., Post B., Tijssen M.AJ., Helmich R.C. Systematic clinical approach for diagnosing upper limb tremor. J. Neurol. Neurosurg. Psychiatry. 2020;91(8):822–830. doi: 10.1136/jnnp-2019-322676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gelauff J., Stone J., Edwards M., Carson A. The prognosis of functional (psychogenic) motor symptoms: a systematic review. J. Neurol. Neurosurg. Psychiatry. 2014;85(2):220–226. doi: 10.1136/jnnp-2013-305321. [DOI] [PubMed] [Google Scholar]
- 6.Schwingenschuh P., Deuschl G. Functional tremor. Handb. Clin. Neurol. 2016;139:229–233. doi: 10.1016/B978-0-12-801772-2.00019-9. [DOI] [PubMed] [Google Scholar]
- 7.Kamble N.L., Pal P.K. Electrophysiological evaluation of psychogenic movement disorders. PRD. 2016;22(1):153–158. doi: 10.1016/j.parkreldis.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 8.Schwingenschuh P., Saifee T.A., Katschnig-Winter P., Macerollo A., Koegl-Wallner M., Culea V., Ghadery C., Hofer E., Pendl T., Seiler S., Werner U., Franthal S., Maurits N.M., Tijssen M.A., Schmidt R., Rothwell J.C., Bhatia K.P., Edwards M.J. Validation of laboratory supported criteria for functional (psychogenic) tremor. Mov. Disord. 2016;31(4):555–562. doi: 10.1002/mds.26525. [DOI] [PubMed] [Google Scholar]
- 9.Zeuner K.E., Shoge R.O., Goldstein S.R., Dambrosia J.M., Hallett M. Accelerometry to distinguish psychogenic from essential or parkinsonian tremor. Neurology. 2003;61(4):548–550. doi: 10.1212/01.wnl.0000076183.34915.cd. [DOI] [PubMed] [Google Scholar]
- 10.Postuma R.B., Berg D., Stern M., Poewe W., Olanow C.W., Oertel W., Obeso J., Marek K., Litvan I., Lang A.E., Halliday G., Goetz C.G., Gasser T., Dubois B., Chan P., Bloem B.R., Adler C.H., Deuschl G. MDS clinical diagnostic criteria for parkinson’s disease. Mov. Disord. 2015;30(12):1591–1601. doi: 10.1002/mds.26424. [DOI] [PubMed] [Google Scholar]
- 11.Perlmutter J.S., Eidelberg D. To scan or not to scan dat is the question. Neurology. 2012;78(10):688–689. doi: 10.1212/WNL.0b013e3182494c72. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.