Abstract
Broader phenotypes associated with genetic liability, including mild difficulties with pragmatic language skills, have been documented in mothers of children with autism spectrum disorder (ASD) and mothers of children with fragile X syndrome (FXS). This study investigated the relationship between pragmatic difficulties and indicators of maternal well-being and family functioning. Pragmatic difficulty was associated with loneliness in mothers of children with ASD or FXS, and with depression, decreased life satisfaction, and poorer family relationship quality in mothers of children with FXS only. Results inform subtle maternal pragmatic language difficulties as a risk factor that that may contribute to reduced health and well-being, informing tailored support services to better meet the unique needs of families of children with ASD or FXS.
Keywords: social communication, fragile X premutation, loneliness, fragile X syndrome, autism spectrum disorder, depression
Pragmatic language, or “social language,” reflects the ability to use language effectively in social contexts to convey meaning (Hyter, 2007; Prutting & Kirchner, 1983). Pragmatic skills include the ability to clarify misunderstandings, convey information succinctly, avoid redundant messages, and tailor one’s message to the listener’s expectations and background knowledge. These skills are essential skill for navigating social situations. Difficulty with pragmatics is associated with loneliness, social isolation, problems establishing social relationships, poor social-emotional adjustment, and psychological risk (Coplan & Weeks, 2009; Geurts et al., 2004; Jobe & White, 2007; Ketelaars, Cuperus, Jansonius, & Verhoeven, 2010; Laws, Bates, Feuerstein, Mason-Apps, & White, 2012; Skuse et al., 2009; Whitehouse, Watt, Line, & Bishop, 2009). Pragmatic language skills are impaired in many neurodevelopmental disorders, including autism spectrum disorder (ASD) and fragile X syndrome (FXS) (Klusek, Martin, & Losh, 2014a; Landa, 2000). Milder pragmatic language difficulties are also observed in a subset of mothers of children with ASD and FXS, due to shared genetic liability within the family. Pragmatic aptitude may be especially important for parents of children with disabilities, given that strong communication skills are important for maintaining social support networks, effectively advocating for one’s child, and structuring dyadic interactions with the child in ways that support development. Yet, the impact of maternal pragmatic difficulties on family and maternal outcomes within these disability groups is unknown, hindering the ability to tailor support services to the family’s specific needs. This study addresses this knowledge gap by delineating the relationship between pragmatic language difficulties in mothers of children with ASD and mothers of children with FXS and their association with several maternal and family outcomes: loneliness, life satisfaction, depression, and family relationship quality.
Pragmatic language difficulties have been well-documented among mothers of children with ASD as part of the broad autism phenotype. The broad autism phenotype consists of subtle personality and language traits that mirror the core features of ASD, including aloof and rigid personality styles and pragmatic language difficulties (Losh, Childress, Lam, & Piven, 2008; Piven, Palmer, Landa, Santangelo, Jacobi, et al., 1997). These features are observed at higher rates among unaffected relatives of individuals with ASD, including mothers, and are believed to reflect genetic liability to ASD (Losh et al., 2008; Piven, Palmer, Landa, Santangelo, Jacobi, et al., 1997). In terms of the pragmatic aspects of the phenotype, mothers of children with ASD are more likely to violate pragmatic norms during conversation such as by using pedantic word choice, including too many details, and having trouble staying on topic, relative to mothers of children with typical development and mothers of children with Down syndrome (Klusek, Losh, & Martin, 2014; Landa et al., 1992; Losh et al., 2008; Piven, Palmer, Landa, Santangelo, & Childress, 1997; Ruser et al., 2007; Whitehouse, Barry, & Bishop, 2007). Reduced narrative cohesion and quality has also been noted in mothers of children with ASD (Landa, Folstein, & Isaacs, 1991; Lee et al., 2020).
Similar pragmatic phenotypes have been observed in mothers of children with FXS who carry the FMR1 premutation. FXS is a single-gene disorder that shows significant behavioral overlap with ASD, with about 50% of children with FXS meeting diagnostic criteria for ASD (Abbeduto et al., 2019; Harris et al., 2008; Klusek, Martin, & Losh, 2014b). The condition is caused by an expansion of >200 repeats of the CGG trinucleotide sequence on the Fragile X Mental Retardation-1 (FMR1) gene on the X chromosome. This expansion causes hypermethylation of the gene and thus, reduced production of Fragile X Mental Retardation (FMRP), a protein that regulates synaptic plasticity and supports brain development (Darnell & Klann, 2013; Fernandez, Rajan, & Bagni, 2013). In most cases, FXS is inherited from mothers who carry a smaller trinucleotide expansion of 55–200 CGG repeats on FMR1, known as the FMR1 premutation (Maddalena et al., 2001). Mothers with the FMR1 premutation are at risk for a broad spectrum of clinical involvement including medical, cognitive-executive, and psychiatric problems (Klusek, Hong, Sterling, Berry-Kravis, & Mailick, 2020; Movaghar et al., 2019; Roberts et al., 2016; Shelton et al., 2016; Wheeler, Raspa, Hagerman, Mailick, & Riley, 2017). Elevated rates of ASD and the broad autism phenotype have also been documented in females with the FMR1 premutation, including differences in the pragmatic use of language (Clifford et al., 2007; Losh, Klusek, et al., 2012; Schneider et al., 2016). Compared to control mothers, mothers with the FMR1 premutation are more likely to violate pragmatic language conventions during conversation, such as speaking too quietly, introducing overly-personal topics, and dominating the conversation (Klusek, Fairchild, & Roberts, 2019; Losh, Klusek, et al., 2012). Reduced eye contact and atypical patterns of attention to social gaze are also observed in this group (Klusek, Ruber, & Roberts, 2018; Klusek, Schmidt, Fairchild, Porter, & Roberts, 2017).
The pragmatic language difficulties experienced by mothers of children with ASD or FXS are of relevance to the developmental outcomes of their children, consistent with social-interactionist theories of development (Bruner, 1974; Snow, 1994). For example, pragmatic difficulties in mothers with the FMR1 premutation are associated with less synchronous mother-child interactions and poorer receptive vocabulary, lower expressive syntax ability, and elevated ASD symptoms in children with FXS (Klusek, Mcgrath, Abbeduto, & Roberts, 2016; Losh, Martin, Klusek, Hogan-Brown, & Sideris, 2012; Moser, Mattie, Abbeduto, & Klusek, in press). Similar associations are observed among families of children with ASD; maternal pragmatic language difficulties are related to lower child receptive language scores and elevated ASD-related communication deficits (Klusek, Losh, et al., 2014; Nayar et al., 2020; Stern, Maltman, & Roberts, 2017).
While the relationship between maternal pragmatic language features and child outcomes has been a focus of prior research, few studies have addressed the potential consequences of these features for the outcomes of the mother herself. Indeed, because these maternal pragmatic features have been assumed to have little clinical relevance, given that they are generally mild in nature and do not rise to the level of Social (Pragmatic) Communication Disorder (American Psychiatric Association, 2013) in terms of severity. However, although the functional impact may be less obvious, these pragmatic deficits may still create a cascade of negative consequences. It is clear from the study of other clinical and non-clinical groups that even mild pragmatic language deficits do have negative consequences, including social isolation, difficulty managing social relationships, psychological risk, poor social-emotional adjustment, and loneliness (Coplan & Weeks, 2009; Faso, Corretti, Ackerman, & Sasson, 2015; Geurts et al., 2004; Jobe & White, 2007; Ketelaars et al., 2010; Laws et al., 2012; Skuse et al., 2009; Whitehouse et al., 2009). Thus, there is a need to better understand the implications of pragmatic language difficulties experienced by mothers of children with ASD or FXS, as they could have significant consequences for the ability of mothers to maintain the social support networks that are essential for successfully caring for a child with a developmental disability as well as for their ability to scaffold their child’s language development (Seeman, Lusignolo, Albert, & Berkman, 2001). Additionally, it is unclear whether the expression of pragmatic difficulties across mothers of children with ASD and mothers of children with FXS has similar implications, as the distinct characteristics of specific disability groups could lead to unique vulnerabilities and needs. Understanding of syndrome-specific patterns could inform the tailoring of services to better meet the needs of families of children with ASD or FXS.
The present study aimed to determine the relationship between maternal pragmatic language difficulties and outcomes for the mother herself and the family unit as a whole. We focused on depression, loneliness, life satisfaction as maternal outcomes of interest, as decreased psychological health and quality of life are observed in both mothers of children with FXS and mothers of children with ASD. This includes elevated depression symptoms (Abbeduto et al., 2004; Franke et al., 1996; Roberts et al., 2009; Roberts et al., 2016; Singer, 2006), with about 5–13% of mothers of children with FXS and 30% of mothers of children with ASD experiencing current depression symptoms in the clinical range (Abbeduto et al., 2004; Davis & Carter, 2008; Roberts et al., 2009; Roberts et al., 2015). Reduced life satisfaction and quality of life have also been well documented in mothers of children with ASD (Ekas, Lickenbrock, & Whitman, 2010; Lu et al., 2015; Vasilopoulou & Nisbet, 2016) and nearly a fourth of mothers of children with FXS report low or very low quality of life/life satisfaction, although, on average, mothers of children with FXS do not differ from the general population or other disability groups on these indicators (Bailey, Sideris, Roberts, & Hatton, 2008; Lewis et al., 2006; Wheeler, Skinner, Bailey, & Abbeduto, 2008). While the specific role of pragmatic language features in maternal well-being and quality of life has not been investigated, some work suggests that increased expression of broad autism phenotype features is associated with increased depression and loneliness, and poorer friendships (Ingersoll & Hambrick, 2011; Ingersoll, Meyer, & Becker, 2011; Jobe & White, 2007; Kunihira, Senju, Dairoku, Wakabayashi, & Hasegawa, 2006). Pragmatic language difficulties, in particular, may impact well-being and quality of life outcomes by making it more difficult for mothers to tap into social support networks thereby exacerbating feelings of loneliness, symptoms of depression, and lower levels of life satisfaction. Parents of children with disabilities already experience barriers in this area because the challenges of raising a child with a disability can make it difficult to fully participate in the community and access community-based social supports (Myers, Mackintosh, & Goin-Kochel, 2009; Raspa, Bailey, Bann, & Bishop, 2014; Sanders & Morgan, 1997); pragmatic language difficulties may compound this effect.
Finally, family relationship quality was also examined as an outcome that would presumably be impacted by communication difficulties and is particularly critical within families of children with disabilities. Family relationship quality is a predictor of child disability severity, child depression symptoms, and child outcomes such as employment and social activity in adulthood (Crossman, Warfield, Kotelchuck, Hauser-Cram, & Parish, 2018; Lewandowski, Palermo, Stinson, Handley, & Chambers, 2010; Loomis, Javornisky, Monahan, Burke, & Lindsay, 1997; Rice, Harold, Shelton, & Thapar, 2006). Reduced family relationship quality has been documented in both families of children with ASD and families of children with FXS relative to families of children with typical development or other disabilities (Fielding-Gebhardt, Warren, & Brady, 2020; Gau et al., 2012) and is associated with both child problem behaviors as well as maternal internalizing symptoms (Baker, Seltzer, & Greenberg, 2012; Timmons, Willis, Pruitt, & Ekas, 2016). Despite the importance of communication skills in social-emotional functioning (Carton, Kessler, & Pape, 1999; Eğeci & Gençöz, 2006; Riggio, Watring, & Throckmorton, 1993; Snow & Douglas, 2017; Whitehouse et al., 2009), no prior studies have examined the relationship between maternal pragmatic language difficulties and family relationship quality.
The limited data available regarding the relationship between maternal pragmatic phenotypes and individual and family outcomes is a barrier to the development of family-centered services that incorporate the needs of all family members. Failure to consider the potential consequences of genetically-mediated maternal characteristics hinders the development of intervention models that support the specific needs of mothers of children with ASD or FXS, which in term can have downstream negative effects on the diagnosed child and response to intervention (e.g., Karst & Van Hecke, 2012). The present study investigates maternal pragmatic language difficulties as features that may be relevant to the unmet service needs of families impacted by ASD or FXS. We posed the following research questions:
Are pragmatic language difficulties in mothers of children with FXS and mothers of children with ASD associated with individual and family outcomes? We hypothesized that maternal pragmatic difficulties would relate to loneliness, reduced life satisfaction, depression, and poorer family relationship quality across both groups. While we contrasted mothers of children with ASD and mothers of children with FXS to explore the potential for syndrome-specific patterns, we did not pose specific hypotheses regarding group-specific relationships given the lack of prior research in this area.
Can associations between maternal pragmatic difficulties and individual and family outcomes be better accounted for by the features of aloofness included within the broad autism phenotype? We hypothesized that these relationships would not be better accounted for by aloof features of the broad autism phenotype.
Methods
Participants
Participants were 55 women who were both carriers of the FMR1 premutation and mothers of children with FXS and 45 mothers who had a child diagnosed with ASD. The mothers’ ages ranged from 26–64 years (M = 45). All mothers spoke American English as their native language and were the biological parent to their child. Mothers in the ASD parent group had a child who had been clinically diagnosed with ASD, and the ASD was not associated with any known genetic syndrome, including FXS. Clinical ASD diagnoses of the children with ASD were confirmed via the Autism Diagnostic Observation Schedule-2 (Lord et al., 2012) by examiners who had achieved research reliability standards. FMR1 premutation status (55–200 CGG repeats on the 5’UTR of FMR1) was confirmed in the mothers of children with FXS through molecular genetic testing conducted as part of a larger research project (64%) or through tests reported in the medical records. Of those participants who participated in molecular genetic testing within the context of the present study, the average CGG repeat length was 96 (SD = 17, range 64–147). None of the mothers of children with FXS had been clinically diagnosed with Fragile X Associated Tremor Ataxia Syndrome, per self-report. Demographic information is presented in Table 1. The groups did not differ on maternal age, education level, race, or household income. The children in the FXS group were significantly older (mean age= 18 years) than the children from the ASD group (mean age = 13 years).
Table 1.
Group Characteristics
| Variable | Group |
||
|---|---|---|---|
| Mothers of children with FXS (n = 55) | Mothers of children with ASD (n = 45) | Test of group differences (p-value) | |
|
| |||
| Mother age in years | |||
| M (SD) | 46.32 (7.44) | 43.91 (8.45) | .133 |
| Range | 26.55–64.30 | 29.37–62.07 | |
| Child age in years | |||
| M (SD) | 18.19 (5.99) | 13.37 (6.79) | <.001* |
| Range | 3.15–35.81 | 2.02–29.47 | |
| Education level | |||
| Associate’s degree or lower | 53% | 39% | |
| Bachelor’s degree | 31% | 36% | .387 |
| Master’s degree | 16% | 23% | |
| Professional degree | 0% | 2% | |
| Race | |||
| African American | 2% | 14% | |
| American Indian/Alaskan Native | 2% | 0% | |
| Asian | 0% | 2% | .076 |
| Caucasian | 96% | 80% | |
| Native Hawaiian/Pacific Islander | 0% | 2% | |
| Other | 0% | 2% | |
| Household income | |||
| <40,000 | 15% | 22% | |
| 40,001–60,000 | 13% | 7% | |
| 60,001–80,000 | 17% | 25% | |
| 80,001–100,000 | 14% | 25% | .267 |
| 100,001–120,000 | 13% | 8% | |
| 120,001–140,000 | 11% | 8% | |
| >140,001 | 17% | 5% | |
p <.050
The participant sample was drawn from two linked studies: (1) a multi-site study focused on adolescents with FXS or ASD and their mothers conducted at the University of South Carolina and the MIND Institute at the University of California, Davis (e.g., Abbeduto et al., 2019) and (2) a study focused on social-communication phenotypes of mothers of children of FXS or ASD at the University of South Carolina, which included the mothers from the adolescent study who participated at the South Carolina site as well as supplementary recruitment of additional mothers (e.g., Klusek et al., 2019). Seventeen mothers of children with FXS and three mothers of children with ASD included in the present study were drawn from the MIND Institute site, whereas the remaining sample was recruited through the University of South Carolina. Recruitment was conducted through word of mouth, social media, flyers targeting families of children with FXS or ASD, referrals from an ongoing research study focused on FXS or ASD being conducted at the University of South Carolina (e.g., Roberts et al., 2020), and with the assistance of the National Fragile X Foundation and the IDDRC Research Participant Registries of the University of North Carolina at Chapel Hill and the MIND Institute
Procedures
All participants provided informed consent and the protocol was approved by the Institutional Review Boards of the participating university sites. As part of the larger studies in which they were enrolled, all mothers participated in assessments and in-person interviews at the respective university site. Two weeks prior to their appointment, mothers were mailed a packet of questionnaires and asked to complete the forms prior to their appointment. The packet included the informant version of the Broad Autism Phenotype Questionnaire (BAP-Q; Hurley, Losh, Parlier, Reznick, & Piven, 2007) and mothers were instructed to ask someone who “knew them well” to complete the form. A prepaid mailer was enclosed with instructions for the informant to return the completed questionnaire directly to the researchers.
Measures
Pragmatic language skills were measured with the pragmatic subscale of the Broad Autism Phenotype Questionnaire (BAPQ; Hurley et al., 2007; Sasson et al., 2013). The BAPQ is a 36-item questionnaire that was designed to evaluate personality and pragmatic language features associated with the broad autism phenotype. This questionnaire has good reliability, evidence supporting internal consistency, and the factor structure of its subscales has been validated (Hurley et al., 2007; Ingersoll, Hopwood, Wainer, & Donnellan, 2011; Sasson et al., 2013). The questionnaire provides subscale scores for rigid, aloof, and pragmatic language traits. The pragmatic subscale of the BAPQ captures social-language problems that may result in ineffective communication and difficulty maintaining a fluid, reciprocal conversation. The subscale consists of 12 items that inquire about features such as the ability to remain on-topic during conversation, remaining “in sync” with the conversational partner, and use of appropriate prosody and volume. Each item is scored on a scale of 1–6 according to the frequency that each pragmatic difficulty is exhibited. Select items are reverse-coded to minimize response bias. Items within each subscale are averaged, yielding continuous subscale scores than can range from 1–6, with higher scores indicating greater pragmatic difficulty. A cut-off score of 2.90 is recommended to identify females who are “positive” for pragmatic language features of the broad autism phenotype (Sasson et al., 2013). Two versions of the questionnaire, a self-report form and an informant-report form, were administered to each participant. A best-estimate score, which averages the scores from the self and informant reports, was computed. Best-estimate scores have increased sensitivity for identifying the presence of broad autism phenotype features relative to the use of informant-only or self-report-only scores (Hurley et al., 2007). When participants only had scores available from the self-report (n = 14) or the informant-report (n = 1) versions of the form, those scores were used as the best estimate, consistent with the methods used in prior reports (Hurley et al., 2007; Seidman, Yirmiya, Milshtein, Ebstein, & Levi, 2012). To confirm that the inclusion of cases involving only one data source did not influence the results, models were run omitting those cases; inference did not change and, therefore, these cases were retained in analyses. Self-report and informant-report scores were highly correlated with the best-estimate score (r’s = .82 and .86, respectively).
Life satisfaction was measured with the Satisfaction with Life Scale (Diener, Emmons, Larsen, & Griffin, 1985), a 5-item self-report tool that evaluates global judgements of one’s own life satisfaction. Items are rated on a 7-point scale indicating the degree to which one agrees with a series of statements describing overall satisfaction with life. Scores are summed, yielding a potential score range of 5–35, with high scores denoting increased satisfaction. The Satisfaction with Life Scale shows strong internal reliability, good discriminant validity from other emotional well-being scales, temporal stability, and its factor structure has been validated (Pavot & Diener, 2009).
Loneliness was indexed with the UCLA Loneliness Scale, version 3 (Russell, 1996), a self-report tool that measures perceived social isolation and loneliness. The scale consists of 20 items describing feelings related to loneliness, which are scored on a 4-point scale indicating the frequency that each feeling is experienced. Nine items are reverse scored to reduce response bias. Potential scores range from 20–80, with higher scores indicating increased feelings of loneliness. The scale has been shown to have high internal consistency and test-retest reliability, strong convergent validity with other loneliness measures, evidence of construct validity, and a validated factor structure (Russell, 1996). Due to time constraints, this measure was not collected on participants enrolled through the MIND Institute site (n’s available for each measure are presented in Table 2).
Table 2.
Descriptive Statistics
| Variable | Group |
Test of group differences (p-value) | |||
|---|---|---|---|---|---|
| Mothers of children with FXS |
Mothers of children with ASD |
||||
| n |
M±SD range |
n |
M±SD range |
||
|
| |||||
| BAPQ, Pragmatic Subscale Best Estimate Score | 55 | 2.27±0.59 1.21–4.63 |
45 | 2.14±0.62 1.21–3.75 |
.194 |
| BAPQ, Aloof Subscale Best Estimate Score | 55 | 2.84±0.78 1.63–4.54 |
45 | 2.54±0.59 1.25–4.00 |
.037* |
| Satisfaction with Life Scale, Total Score | 54 | 23.44±6.80 5.00–35.00 |
44 | 23.00±7.74 5.00–35.00 |
.763 |
| UCLA Loneliness Scale, Total Score | 38 | 41.05±11.34 20.00–70.00 |
41 | 41.54±11.74 20.00–63.00 |
.823 |
| Beck Depression Inventory, Total Score | 37 | 10.81±9.85 0–44.00 |
38 | 8.34±6.80 0–24.00 |
.210 |
| Family Environment Scale, Family Relationship Index | 53 | 18.60±4.10 8.00–25.00 |
39 | 19.03±4.31 5.00–24.00 |
.634 |
| Parenting Stress Index-4, Total Stress Percentile | 55 | 64.47±21.04 4.00–99.00 |
44 | 66.61±20.31 15.00–99.00 |
.611 |
p < .050
Depression symptoms were measured with the Beck Depression Inventory-II (Beck, Steer, & Brown, 1996). This 21-item self-report questionnaire captures the severity of depression symptoms experienced over the prior two weeks. Items are summed, yielding a continuous score reflecting depression symptom severity. Scores of ≥14 are considered indicative of clinical depression. Evidence supports high test-retest reliability, internal consistency, and validity estimates (e.g., Osman, Kopper, Barrios, Gutierrez, & Bagge, 2004; Sprinkle et al., 2002; Storch, Roberti, & Roth, 2004). This questionnaire was not collected on the participants enrolled through the MIND Institute site for a variety of logistical reasons (see Table 2 for n’s available for each measure).
Family relationship quality was evaluated with the Family Relationship Index of the Family Environment Scale, Form R (Moos & Moos, 1986). The Family Environment Scale consists of 90 self-report true/false statements that measure the social and interpersonal climate of the family. The Family Relationship Index is a composite standard score comprised of 27 items that reflects family cohesion (the degree of commitment and support family members provide each other), expressiveness (the degree to which family members openly communicate with each other), and level of conflict. Higher scores reflect a more positive perception of family interactions. The Family Environment Scale is a well-established tool with evidence supporting discriminant, construct, and predictive validity, and high internal consistency (Moos, 1990)
Parenting stress was indexed with the Total Stress Percentile of the Parenting Stress Inventory-4 Short Form (Abidin, 2013). This variable was collected as a covariate to account for the potential influence of parenting-related stress on the outcome variables.
Data Analysis
Analyses were conducted using SAS software, version 9.4, Copyright © 2013, SAS Institute Inc., Cary, NC, USA. First, variables were examined to confirm normal distribution. Descriptive statistics were examined within each group and group differences on each of the variables of interest were tested with general linear models to inform differences in levels of endorsement across the groups. A Pearson correlation matrix was computed to inform the relationship among study variables and model specification (see Table 3). Child age was not significantly associated with any variable of interest within or across the groups and therefore was not covaried in the statistical models. Parenting stress level, indexed with the Total Stress Percentile of the Parenting Stress Inventory-4 Short Form (Abidin, 2013), was significantly correlated with several variables of interest was included as a covariate in the models. A series of general linear models tested pragmatic language difficulty as a predictor of the life satisfaction, loneliness, and family environment outcomes. Group membership and its interaction with pragmatic difficulty were included in the models to test for potential group-specific effects. Significant interaction terms were followed by interaction contrasts to determine the effect of pragmatic skills on the outcome at each level of group. Next, to address whether patterns could be better accounted for by aloof features of the broad autism phenotype, the general linear model for each outcome was repeated adding terms for the aloof BAPQ subscale and its interaction with group. FDR correction was applied at the level of the model F to correct for multiple comparisons (Benjamini & Hochberg, 1995). Partial eta squared (η2p) effect sizes were computed for all models, with effects at 0.01, 0.06, and 0.14 generally indicative of “small”, “medium”, and “large”, respectively (Cohen, 1988).
Table 3.
Correlation Matrix among Time 1 Variables
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1. BAPQ, Pragmatic Subscale Best Estimate Score | 1.00 | |||||||
| 2. BAPQ, Aloof Subscale Best Estimate Score | .42* | 1.00 | ||||||
| 3. Satisfaction with Life Scale, Total Score | −.14 | −.11 | 1.00 | |||||
| 4. UCLA Loneliness Scale, Total Score | .51* | .19 | −.32* | 1.00 | ||||
| 5. Beck Depression Inventory-II, Total Score | .40* | .30* | −.45* | .60* | 1.00 | |||
| 6. Family Environment Scale, Family Relationship Index | −.19 | −.11 | .42* | −.33* | −.48* | 1.00 | ||
| 7. Parenting Stress Index-4, Total Stress Percentile | .14 | .23* | −.41* | .45* | .39* | −.30* | 1.00 | |
| 8. Child Age (Years) | .02 | .09 | −.16 | −.15 | −.06 | −.09 | .02 | 1.00 |
p < .050
Results
Descriptive Statistics
Group means, standard deviations, and ranges for each variable are reported in Table 2, along with the tests of group differences. Mothers of children with FXS and mothers of children with ASD did not differ statistically in the extent of pragmatic language difficulties, life satisfaction ratings, loneliness, the quality of the family relationship, or parenting stress levels. Aloof features of the broad autism phenotype, indexed with the BAPQ aloof subscale, were significantly elevated in the mothers of children with FXS relative to the mothers of children with ASD. Using the revised BAPQ cut-offs reported by Sasson et al. (2013) to describe the percentage of participants who scored “positive” for each features of the broad autism phenotype, five (11%) mothers of children with ASD and nine (16%) mothers of children with FXS exceeded cut-offs for pragmatic features; rates across the groups were not statistically different, χ2 (1, N=100) = .567, p = .451. Ten (22%) mothers of children with ASD and 21 (38%) mothers of children with FXS exceeded cut-offs for aloof features; the rates across the groups did not differ significantly, χ2 (1, N=100) = 2.94, p = .086. Eight (18%) mothers of children with ASD and 12 (22%) mothers of children with FXS obtained a score of 14 or higher on the Beck Depression Inventory-II data, which is considered indicative of clinical depression; the rates did not differ significantly across groups χ2 (1, N=100) = 253, p = .615.
Pragmatic Difficulty as a Predictor of Individual and Family Outcomes
Loneliness.
The overall model testing the combined influence of group, pragmatic difficulty, group-by-pragmatics, and parenting stress level as predictors of concurrent loneliness was statistically significant (F [4, 74] = 13.31, FDR-corrected p < .001, R2 = .42), see Table 4. A main effect for pragmatics was detected, with a large effect size (p < .001, η2p = .27), with increased pragmatic difficulty associated with increased loneliness. The group-by-pragmatics interaction term was not significant, indicating that the relationship between pragmatics and loneliness was similar across both parent groups (p = .574, η2p < .01); see Figure 1.
Table 4.
Model Results: Relationship Between Maternal Pragmatic Features and Individual and Family Outcomes
| Outcome Variable |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | Loneliness | Life Satisfaction | Depression | Family Relationship Quality | ||||||||
|
|
|
|
||||||||||
| F | p | η 2 p | F | p | η 2 p | F | p | η 2 p | F | p | η 2 p | |
|
| ||||||||||||
| Pragmatic Difficulty | 27.03 | <.001* | .27 | 0.77 | .384 | <.01 | 17.85 | <.001* | .20 | 1.62 | .207 | .02 |
| Group | 0.03 | .584 | <.01 | 4.08 | .046* | .04 | 8.35 | .005* | .11 | 3.61 | .061 | .04 |
| Pragmatic-by-Group Interaction | 0.32 | .574 | <.01 | 4.09 | .046* | .04 | 12.03 | .009* | .15 | 4.56 | .036* | .05 |
| Parenting Stress | 18.58 | <.001* | .20 | 14.62 | .002* | .14 | 12.30 | .008* | .15 | 5.93 | .017* | .06 |
p < .050
Figure 1. Relationship between pragmatic language difficulty and loneliness across groups.
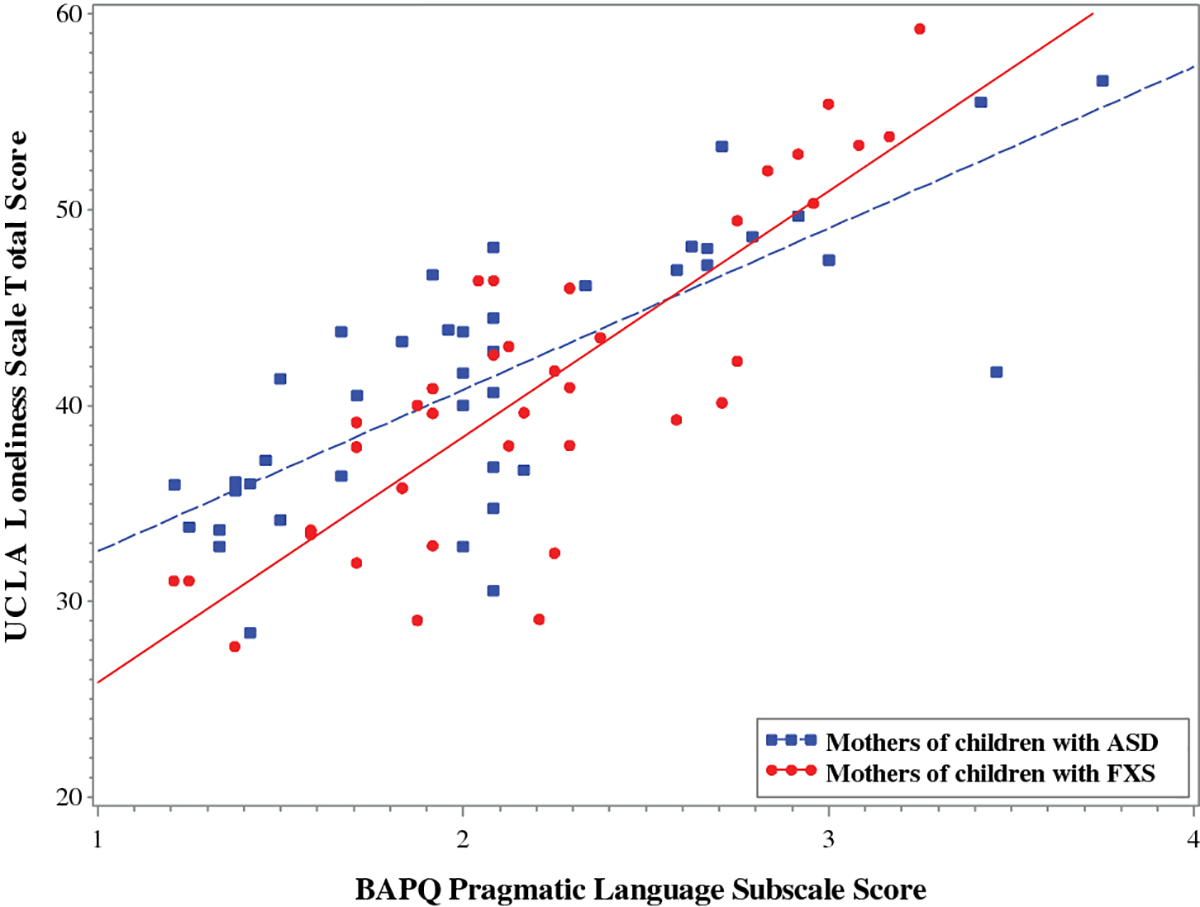
Note. Higher scores on the BAPQ Pragmatic Language Subscale indicate greater pragmatic language difficulty. Higher scores on the UCLA Loneliness Scale indicate increased feelings of loneliness. Model-predicted values are shown, controlling for parenting stress level.
To determine whether the observed associations were better accounted for by aloof features of the broad autism phenotype, the model was repeated adding terms for aloof personality style and its interaction with group. Even after accounting for aloof features, pragmatic language difficulties significantly predicted loneliness symptoms in both groups, with a large effect size (p < .001, η2p = .30). A significant interaction group-by-aloofness interaction term indicated that the effect of aloof features on life satisfaction varied by group (p = .008, η2p = .09). Interaction contrasts indicated that aloofness was significantly associated with loneliness in the mothers of children with ASD (F [1, 72] = 7.87, p = .007, η2p = .10), but not in the mothers of children with FXS (F [1, 72] = 0.61, p = .438, η2p < .01).
Life Satisfaction.
The overall model testing the combined influence of group, pragmatics, group-by-pragmatics, and parenting stress level as predictors of concurrent life satisfaction was statistically significant (F [4, 93] = 6.20, FDR-corrected p < .001, R2 = .21). A significant group-by-pragmatics interaction term was observed (p =.046, η2p < .04). Interaction contrasts indicated that increased pragmatic difficulty was significantly associated with lower life satisfaction among the mothers of children with FXS (F [1, 93] = 4.39, p = .039, η2p = .05), but not among mothers of children with ASD (F [1, 93] = 0.64, p = .436, η2p < .01); see Figure 2. Model results are presented in Table 4.
Figure 2. Relationship between pragmatic language difficulty and life satisfaction across groups.
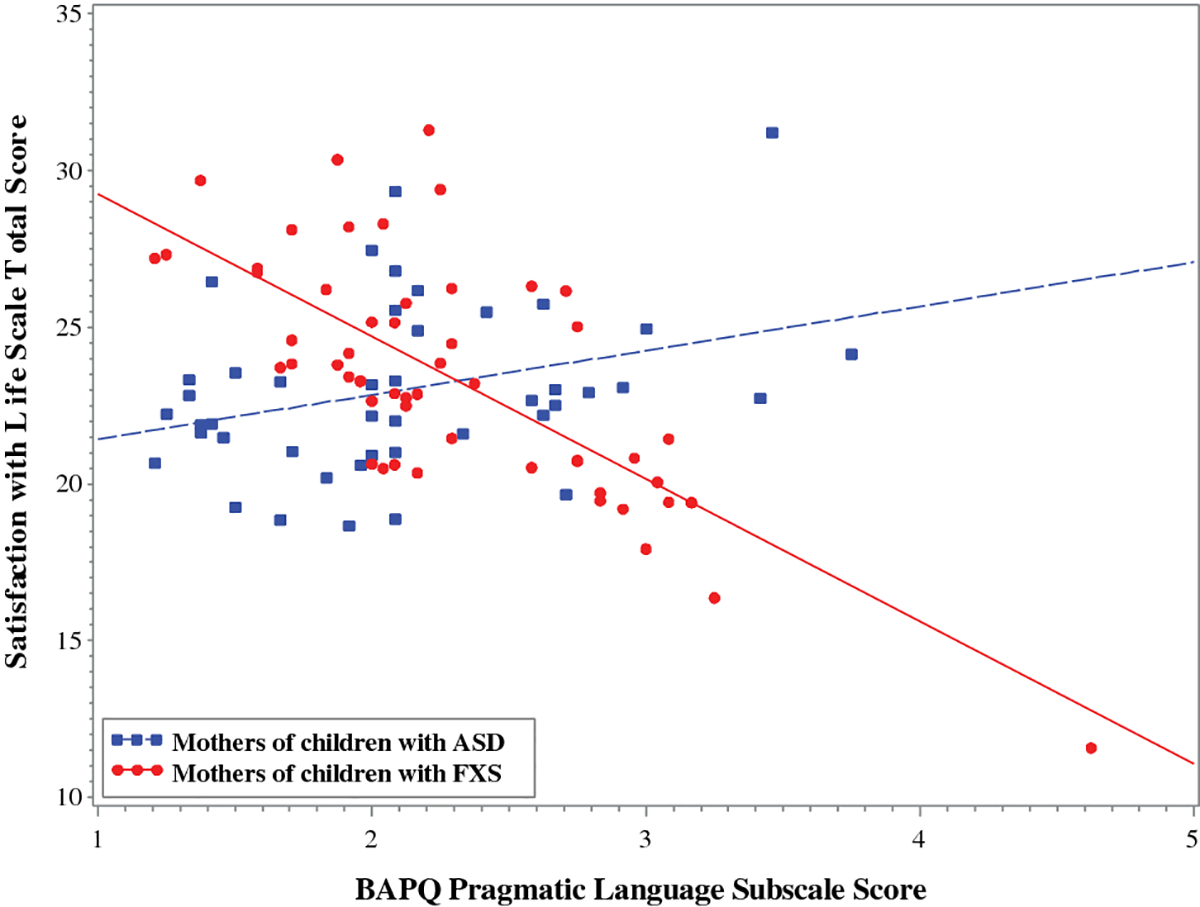
Note. Higher scores on the BAPQ Pragmatic Language Subscale indicate greater pragmatic language difficulty. Higher scores on the Satisfaction with Life Scale indicate increased life satisfaction. Model-predicted values are shown, controlling for parenting stress level.
To determine whether the observed associations were better accounted for by the aloof features of the broad autism phenotype, the model was repeated adding terms for aloof personality style and its interaction with group. The terms for aloofness (F [1, 91] = 0.16, p = .694, η2p < .01) and the aloof-by-group interaction (F [1, 91] = 0.16, p = .688, η2p < .01) were not statistically significant. With the addition of new terms to the model and loss of degrees of freedom, the group-by-pragmatics interaction term that was significant in the primary model was no longer significant (F [1, 91] = 2.93, p = .090, η2p = .03).
Depression Symptoms.
The combined influence of group, pragmatics, group-by-pragmatics, and parenting stress level accounted for significant variance in concurrent depression, F(4, 70) = 12.09, FDR-corrected p < .001, R2 = .41. A significant group-by-pragmatic difficulty interaction term indicated that the effect of pragmatic difficulty on depression symptoms differed across the parent groups (p <.001, η2p < .15). Interaction contrasts indicated that elevated pragmatic difficulty was significantly associated with greater depression symptoms for the mothers of children with FXS with a large effect size (F [1, 70] = 24.80, p < .001, η2p = .24), but not for the mothers of children with ASD (F [1, 70] = 0.37, p = .548, η2p < .01); see Figure 3. See Table 4 for full model results.
Figure 3. Relationship between pragmatic language difficulty and depression symptoms across groups.
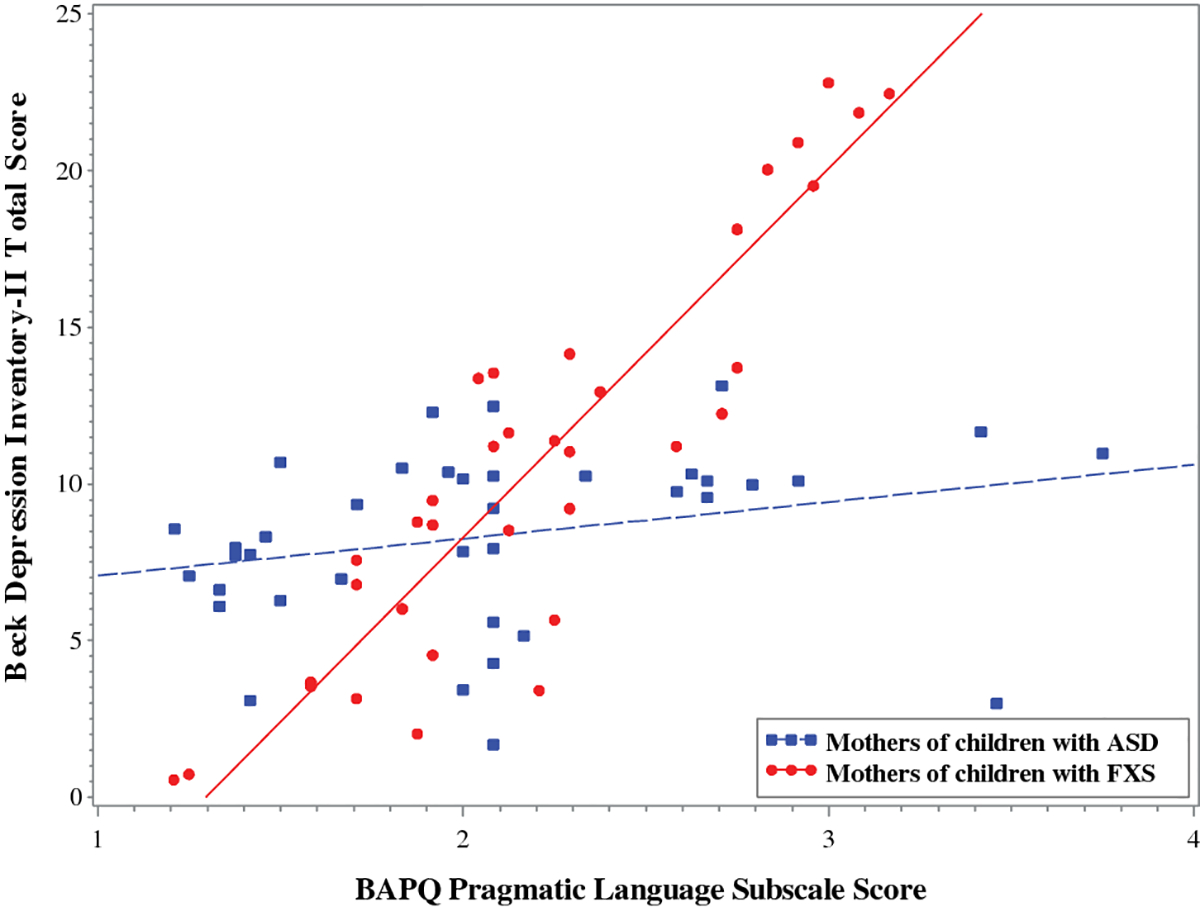
Note. Higher scores on the BAPQ Pragmatic Language Subscale indicate greater pragmatic language difficulty. Higher scores on the Beck Depression Inventory-II indicate increased depression symptoms. Model-predicted values are shown, controlling for parenting stress level.
Accounting for the aloof features of the broad autism phenotype did not change the model results. The terms involving aloofness did not account for significant variance in depression symptoms (F [1, 68] = 0.00, p = .993, η2p < .01), and neither did the group-by-aloof interaction term (F [1, 68] = 2.63, p = .110, η2p = .12). The group-by-pragmatics interaction terms remained significant, with pragmatic features associated with depression in the mothers of children with FXS but not in the mothers of children with ASD (F [1, 68] = 6.61, p = .012, η2p = .09).
Family Relationship Quality.
The overall model testing the combined influence of group, pragmatics, group-by-pragmatics, and parenting stress level as predictors of family relationship quality was statistically significant, F(4, 87) = 4.12, FDR-corrected p = .004, R2 = .16. A significant group-by-pragmatic difficulty interaction term indicated that the effect of pragmatic difficulty on family relationship quality differed across the groups (p =.036, η2p = .05). Increased maternal pragmatic difficulty was significantly associated with reduced family relationship quality in the FXS parent group (F [1, 87] = 6.18, p = .015, η2p = .07), but not in the ASD parent group (F [1, 87] = 0.36, p = .548, η2p < .01); see Figure 4. Model results are presented in Table 4.
Figure 4. Relationship between pragmatic language difficulty and family relationship quality across groups.
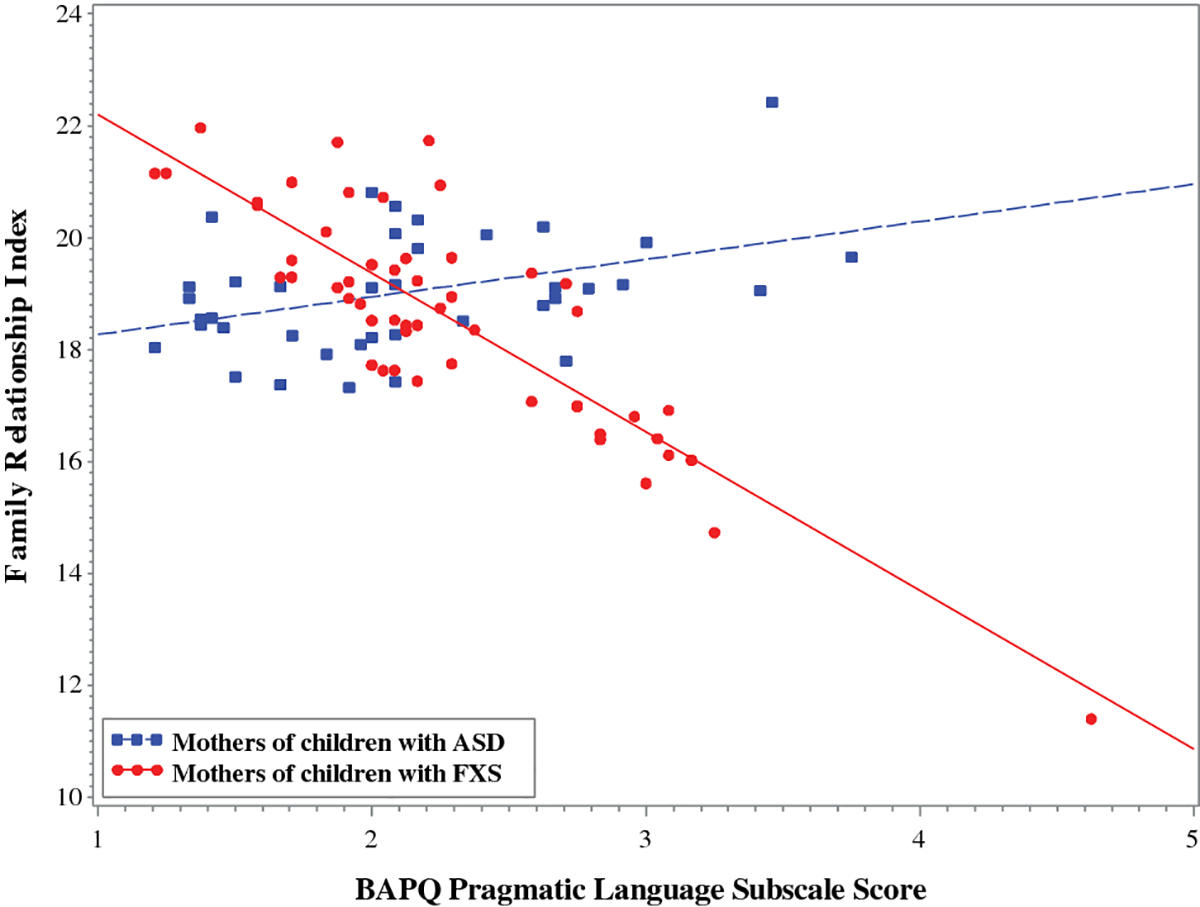
Note. Higher scores on the BAPQ Pragmatic Language Subscale indicate greater pragmatic language difficulty. Higher Family Relationship Index scores reflect more positive perceptions of family interactions. Model-predicted values are shown, controlling for parenting stress level.
Repeating the model to determine whether the observed associations could be better accounted for by the aloofness trait, the group-by-pragmatics interaction term remained significant with pragmatic features associated with family relationship quality in the mothers of children with FXS but not in the mothers of children with ASD (F [1, 85] = 4.99, p = .028, η2p = .06). The aloof features did not account for significant variance in family relationship quality (F [1, 85] = 0.00, p = .993, η2p < .01), and neither did the group-by-aloofness interaction term (F [1, 85] = 0.43, p = .513, η2p < .01).
Discussion
The heritable nature of both ASD and FXS is such that genetic risk within the family is not unique to the child who is affected by ASD or FXS; parents of children with these neurodevelopmental conditions are also at heightened genetic susceptibility for adverse phenotypes. Broader phenotypes, including mild difficulties with pragmatic language skills, have been documented in both mothers of children with ASD and mothers of children with FXS. This study investigated the consequences of maternal pragmatic difficulties within these parent groups, with a focus on implications for maternal well-being and family relationship quality. Results indicated that loneliness was elevated among mothers who displayed pragmatic language deficits, which is consistent with the view of pragmatic language as a fundamental skill for navigating social relationships and building social support networks. The association between pragmatics and loneliness was of a large effect size even after controlling for parenting stress and was not explained by other social features of the broad autism phenotype (i.e., features of aloofness). Pragmatic language difficulty was also linked to depression, lower life satisfaction, and reduced family relationship quality, but interestingly these associations were unique to the mothers of the youth with FXS. Thus, the negative consequences of pragmatic language difficulties appear to be more pervasive among mothers of children with FXS. Although more research is needed to understand the source of these syndrome-specific patterns, this study contributes to a more comprehensive understanding of pragmatic language phenotypes associated with the broad autism phenotype and the FMR1 premutation. These findings may help tailor support services to better meet the unique needs of families of children living with ASD and FXS.
Pragmatic Language Difficulty is Associated with Loneliness
This study is the first to show that loneliness is related to the expression of pragmatic language phenotypes in mothers of children with ASD and mothers of children with FXS who carry the FMR1 premutation. Effects were large in size, even after accounting for parenting stress levels, and were not accounted for by the presence of socially aloof features of the broad autism phenotype. This robust relationship between pragmatics and loneliness is notable considering that the majority of participants did not exhibit gross pragmatic language deficits. Only 11% of the ASD group and 16% of the FXS group exhibited sufficient pragmatic language features to be considered “positive” for pragmatic features of the broad autism phenotype on the BAPQ. Therefore, findings suggest that even mildly expressed pragmatic language features in mothers of children with ASD and mothers of children with FXS can influence social relationships and contribute to perceived social isolation. This finding is consistent with prior reports demonstrating that “normal” variation in pragmatic language competence influences social functioning, such as evidence that the pragmatic language skills of college students affect the quality of their relationships (Faso et al., 2015; Jobe & White, 2007). Such findings have important clinical implications for identifying at-risk individuals and developing clinical practices that better support long-term health and quality of life in mothers of children with ASD or FXS. Indeed, the consequences of loneliness are not insignificant. Chronic loneliness is a major risk factor for increased morbidity and mortality (Hawkley & Cacioppo, 2010; Heinrich & Gullone, 2006) that is associated with health-related problems ranging from cardiovascular disease (Caspi, Harrington, Moffitt, Milne, & Poulton, 2006; Thurston & Kubzansky, 2009), stroke (Cacioppo, Capitanio, & Cacioppo, 2014), sleep problems (Cacioppo et al., 2002), cognitive decline (Boss, Kang, & Branson, 2015; Cacioppo & Hawkley, 2009), and aberrant physiological stress reactivity across the autonomic, endocrine, and immune systems (Hawkley & Cacioppo, 2003). Thus, the present study sheds new light on how the expression of genetic liability in mothers of children with ASD or FXS may represent a risk factor for reduced health and well-being.
Loneliness is defined by perceived social isolation, with one’s social needs not being met by the quantity or quality of one’s relationships (Hawkley et al., 2008; Peplau & Perlman, 1982). Presumably, pragmatic language deficits lead to perceived social isolation through their well-documented negative impact on the ability to establish and maintain social relationships (Faso et al., 2015; Lamport & Turner, 2014; Leonard, Milich, & Lorch, 2011; Whitehouse et al., 2009). Our findings align with current theoretical frameworks suggesting that loneliness is maintained through a self-reinforcing feedback loop (see Cacioppo & Hawkley, 2009; Cacioppo, Hawkley, et al., 2006). In this loop, lonely individuals develop cognitive biases such that they attend more closely to negative social information and begin to expect negative social interactions. Negative expectations in turn elicit negative social responses, confirming the lonely individual’s expectations and reinforcing the feedback loop. Pragmatic language deficits could contribute to this cycle by causing communication breakdowns that result in more frequent negative social interactions.
Additional research is needed to determine whether the negative impact of subtle pragmatic language difficulties is amplified within the context of families of children with neurodevelopmental disorders. The social support networks of these families are often already weakened because the challenges of raising a child with a disability can make it difficult to participate in the community and obtain community-based social support (Myers et al., 2009; Raspa et al., 2014; Sanders & Morgan, 1997). It is possible that the impact of subtle communication difficulties on social relationships may be more pronounced within the context of an already weak social support network, and therefore the consequences of subtle maternal pragmatic language features may be more substantial within families of children with ASD or FXS.
The tie between pragmatic language difficulty and loneliness may have particular relevance for the promotion of healthy aging in mothers of children with ASD or FXS. Longitudinal and experimental studies suggest that loneliness plays a causal role in cognitive decline (Boss et al., 2015; Cacioppo & Cacioppo, 2014; Cacioppo & Hawkley, 2009), with some estimates suggesting that lonely older adults experience cognitive decline approximately 20% faster than their non-lonely counterparts (Donovan et al., 2017). Mothers of children with developmental disabilities are already at risk for accelerated cognitive aging, as the stressors of parenting a child with a disability over a prolonged period of time have been shown to jeopardize cognitive function (Song, Mailick, Greenberg, Ryff, & Lachman, 2015). Mothers of children with FXS are believed to be doubly vulnerable for age-related decline, as the FMR1 premutation itself is a genetic risk factor for accelerated aging and decline in cognitive-executive and cognitive-linguistic skills, such as inhibitory control and language fluency (Bredin-Oja et al., 2021; Goodrich-Hunsaker, Wong, Mclennan, Srivastava, et al., 2011; Goodrich-Hunsaker, Wong, Mclennan, Tassone, et al., 2011; Klusek et al., 2020; Moser, Schmitt, Schmidt, Fairchild, & Klusek, 2021; Sterling, Mailick, Greenberg, Warren, & Brady, 2013), which is then compounded by the stressors of parenting a child with FXS (Allen et al., 2007; Seltzer et al., 2012). Therefore, the implications of pragmatic language difficulties in mothers of children with ASD and mothers of children with FXS, and their relationship with loneliness, may become more salient as mothers approach middle and later adulthood. Strategies to mitigate risk for loneliness may be of potential utility to improve the long-term outcomes of mothers of children with ASD or FXS and their families, such as social cognitive training interventions that have been shown to effectively combat loneliness (Masi, Chen, Hawkley, & Cacioppo, 2011).
The Impact of Pragmatic Difficulty May be More Pervasive in Mothers of Children with FXS
Mothers of children with ASD and mothers of children with FXS did not differ in the severity of pragmatic features, nor did they differ in loneliness, life satisfaction, depression, or family relationship quality. Despite these similar profiles, maternal pragmatic language difficulties were associated with depression, reduced life satisfaction, and lower family relationship quality only in the mothers of youth with FXS. It is unclear why pragmatic language difficulties did not have the same impact for the mothers of children with ASD. However, the finding that the pragmatic language phenotype of mothers of children with ASD was not linked to indicators of well-being or family functioning is consistent with the conceptualization of the broad autism phenotype as a subclinical phenomenon—a “forme fruste” that reflects ASD genetic liability and is not associated with functional impairment (Losh et al., 2008; Losh et al., 2017; Piven, Palmer, Jacobi, Childress, & Arndt, 1997).
But why did these same pragmatic language features relate to poorer individual and family outcomes when expressed in mothers of children with FXS? We considered the possibility that other social features of the broad autism phenotype, such aloof personality features, could be differentially expressed across groups and could confound the observed associations with pragmatics. However, our data did not support this hypothesis. After accounting for pragmatic language features, social aloofness did not account for significant variance in depression, life satisfaction, or family relationship quality in either group of mothers. One possibility is that the group-specific patterns reflect differences in the clinical manifestations of the broad autism phenotype and the FMR1 premutation. In parents of children with ASD, the broad autism phenotype is a relatively isolated set of characteristics that are not typically accompanied by clinical risk. Additionally, evidence suggests that the features of the broad autism phenotype co-segregate in relatives of children with ASD (Happe & Ronald, 2008), which means that parents often exhibit features corresponding to just one or two subdomains of the ASD triad, further minimizing the scope of involvement. In contrast, mothers with the FMR1 premutation are at risk for a broader constellation of clinical problems that extend far beyond pragmatic language features, including risk for executive dysfunction, autoimmune disorders, psychiatric involvement, fertility problems, and neurodegenerative disease (Wheeler et al., 2017; Wheeler et al., 2014). Therefore, it is possible that pragmatic language difficulty in mothers of children with FXS represents a single symptom occurring as part of a broader clinical phenomena and this collective risk profile leads to reduced well-being and family relationship quality. Child-related stressors (e.g., severity of intellectual disability and other child symptoms, number of affected children in the family) may also be heightened in mothers of children with FXS, relative to mothers of children with ASD, and could contribute to cumulative risk. However, additional research is needed to test this hypothesis. In any case, the results of this study demonstrate that pragmatic language difficulties represent a significant risk factor for reduced well-being and family functioning for mothers with the FMR1 premutation, with robust relationships observed across multiple indicators.
Group-Specific Associations with Depression
Eighteen percent of mothers of children with FXS and 22% of mothers of children with ASD in the present study reported current depression symptoms within the clinical range, which is in line with rates of current depression previously reported in the literature (Abbeduto et al., 2004; Davis & Carter, 2008; Piven et al., 1991; Roberts et al., 2009; Roberts et al., 2015). Although both groups exhibited similar levels of current depression symptoms, these symptoms were associated with pragmatic difficulties only within the FXS parent group. This finding is consistent with Piven and Palmer (1999), who also did not detect an association between the presence of major depressive disorder and pragmatic language competence among parents of children with ASD (Piven & Palmer, 1999). Although the reason for these syndrome-specific patterns is unclear, it is possible that the association between pragmatic language difficulties and depression is moderated by other factors that vary across etiological groups and were not accounted for here. Social support is one such potential moderator that deserves additional attention, as pragmatic language difficulties could make it more difficult to obtain social support and low levels of social support have been consistently shown to be related to depression risk in mothers of children with ASD (Boyd, 2002; Smith, Greenberg, & Seltzer, 2012). Levels of social support may differ across ASD and FXS parent groups, or the potential buffering effect of social support may be weakened in mothers of children with FXS. In fact, some reports have failed to detect a relationship between social support and stress in mothers of children with FXS (Mccarthy, Cuskelly, Van Kraayenoord, & Cohen, 2006) and mothers who carry midrange FMR1 premutation CGG repeats may be less able to derive benefit from positive emotional support (Hartley, Dawalt, Hong, Greenberg, & Mailick, 2019). Additional research is needed to explore the potential moderating role of social support across the two groups of parents. Child-related stressors may also vary in severity across these parent groups and are known to contribute to depression risk (Abbeduto et al., 2004; Falk, Norris, & Quinn, 2014; Roberts et al., 2009; Zablotsky, Anderson, & Law, 2013). Because we measured only current symptoms of depression, it is also possible that differences in lifetime histories of depression between the two groups of mothers may also have differentially shaped their social networks and set into motion different developmental cascades of phenotypic features and relationships.
Strengths, Weaknesses, and Directions
This study has both strengths and weaknesses. In terms of measurement, our use of well-validated instruments that are widely used in the literature supports validity and facilitates comparison with the extant literature. Another strength is the use of combined informant and self-report scores to derive the best-estimate pragmatic language subscale score of the BAPQ. The best-estimate scores have increased sensitivity and specificity compared to self-report or informant-report only and have been validated against direct-assessment measures of communication and personality features of the broad autism phenotype (Hurley et al., 2007). The inclusion of large samples of 55 mothers of children with FXS and 45 mothers of children with ASD is also a strength, although participant numbers were lower for some measures. Finally, although the sample was diverse in terms of educational attainment and economic status, racial diversity was relatively limited, particularly within the FXS parent group.
We adopted a statistical approach that tested pragmatics as a predictor of each outcome of interest individually. This method allowed us to address our primary research focused on the relationship between pragmatic language difficulties and indicators of well-being and family functioning. However, we acknowledge that the relationship between the study variables is likely more complex, with potential intercorrelations among the outcomes. For example, depression and loneliness are often correlated with evidence of bidirectional effects (Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006). Our focus was on the relationship between pragmatic language deficits and outcomes, and because this is a new area of study, we thought it was critical to first establish predictive relationships at a more individual level before attempting to tease apart mediating or moderating effects among the outcome variables.
We are unable to infer causality from this correlational study, which limits understanding of the directionality of the associations. It is plausible that features such as loneliness or depression also reciprocally impact pragmatic language skills, such as a situation where depression causes an individual to be less engaged in conversational interactions. Future studies that follow participants longitudinally will be better able to tease apart reciprocal associations and the evolution of features over time. Longitudinal work following mothers through midlife and older adulthood will be particularly important for understanding the long-term implications of pragmatic language difficulties in mothers of children with ASD or FXS across the adult lifespan.
Conclusion
This study suggests that subtle maternal pragmatic language difficulties represent a risk factor for loneliness in mothers of children with ASD and mothers of children with FXS. Moreover, pragmatic language difficulties in mothers of children with FXS were linked with depression, reduced life satisfaction, and poorer family relationship quality. Results provide a more comprehensive understanding of the implications of subtle pragmatic language difficulty experienced by parents of children with ASD or FXS, which have been traditionally conceptualized as a subclinical trait of negligible clinical relevance. By informing risk factors that may contribute to reduced health and well-being in mothers, findings may help tailor support services to better meet the unique needs of families of children living with ASD or FXS.
Acknowledgments
Funding
This research was supported by National Institutes of Health grants F32DC013934, R21DC017804, and R03HD098291 awarded to Jessica Klusek; R01HD024356 and U54HD079125 awarded to Leonard Abbeduto; R01MH107573 awarded to Jane Roberts; by the Research Participant Registry Core of the Carolina Institute for Developmental Disabilities (U54HD079124). Support was also provided by an ASPIRE-I grant awarded by the Office of the Vice President for Research at the University of South Carolina.
Funding: This research was supported by National Institutes of Health grants F32DC013934, R21DC017804, and R03HD098291 awarded to Jessica Klusek; R01HD024356 and P50HD103526 awarded to Leonard Abbeduto; R01MH107573 awarded to Jane Roberts; by the Research Participant Registry Core of the Carolina Institute for Developmental Disabilities (U54HD079124). Support was also provided by an ASPIRE-I grant awarded by the Office of the Vice President for Research at the University of South Carolina.
Conflict of interest: Leonard Abbeduto has received funding to develop and implement outcome measures for clinical trials from F. Hoffman-LaRoche, Ltd., Roche TCRC, Inc., and Neuren Pharmaceuticals Limited, Inc. No other authors have conflicts or financial disclosures to declare. Angela John Thurman has received funding to develop and implement outcome measures from Fulcrum Therapeutics.
Footnotes
Conflict of Interest
Compliance with Ethical Standards
Ethical Approval
All procedures were performed in accordance with the standards laid out by the Declaration of Helsinki and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Boards of the University of University of South Carolina and the University of California Davis Health.
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained for all participants included in the study.
Bibliography
- Abbeduto L, Seltzer MM, Shattuck P, Krauss MW, Orsmond G, Murphy MM, & Floyd F (2004). Psychological well-being and coping in mothers of youths with autism, down syndrome, orfragile X syndrome. American Journal on Mental Retardation, 109(3), 237–254. [DOI] [PubMed] [Google Scholar]
- Abbeduto L, Thurman AJ, McDuffie A, Klusek J, Feigles RT, Brown WT, … Dobkins C (2019). ASD comorbidity in fragile X syndrome: symptom profile and predictors of symptom severity in adolescent and young adult males. Journal of Autism and Developmental Disorders, 49(3), 960–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abidin RR (2013). Parenting Stress Index, Fourth Edition Short Form (PSI-4-SF). In. Lutz, FL: PAR, Inc. [Google Scholar]
- Allen E, Sullivan A, Marcus M, Small C, Dominguez C, Epstein M, … Sherman S (2007). Examination of reproductive aging milestones among women who carry the FMR1 premutation. Human Reproduction, 22(8), 2142–2152. doi: 10.1093/humrep/dem148 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5 ed.): American Psychiatric Publishing, Incorporated. [Google Scholar]
- Bailey DB, Sideris J, Roberts J, & Hatton D (2008). Child and genetic variables associated with maternal adaptation to fragile X syndrome: A multidimensional analysis. American Journal of Medical Genetics Part A, 146A, 720–729. doi: 10.1002/ajmg.a.32240 [DOI] [PubMed] [Google Scholar]
- Baker JK, Seltzer MM, & Greenberg JS (2012). Behaviour problems, maternal internalising symptoms and family relations in families of adolescents and adults with fragile X syndrome. Journal of intellectual disability research : JIDR, 56(10), 984–995. doi: 10.1111/j.1365-2788.2012.01580.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck Depression Inventory-II. In (pp. b9). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological), 57(1), 289–300. doi:https://www.jstor.org/stable/2346101 [Google Scholar]
- Boss L, Kang D-H, & Branson S (2015). Loneliness and cognitive function in the older adult: a systematic review. International Psychogeriatrics, 27(4), 541–553. [DOI] [PubMed] [Google Scholar]
- Boyd BA (2002). Examining the relationship between stress and lack of social support in mothers of children with autism. Focus on Autism and Other Developmental Disabilities, 17(4), 208–215. doi: 10.1177/10883576020170040301 [DOI] [Google Scholar]
- Bredin-Oja SL, Warren SF, Romine RES, Fleming KK, Brady N, & Berry-Kravis E (2021). Word retrieval difficulty in adult females with the FMR1 premutation: Changes over time and across contexts. Brain and Cognition, 148, 105694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruner JS (1974). From communication to language—A psychological perspective. Cognition, 3(3), 255–287. [Google Scholar]
- Cacioppo JT, & Cacioppo S (2014). Older adults reporting social isolation or loneliness show poorer cognitive function 4 years later. Evidence-Based Nursing, 17(2), 59–60. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, & Hawkley LC (2009). Perceived social isolation and cognition. Trends in cognitive sciences, 13(10), 447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, & Hobson JA (2002). Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science, 13(4), 384–387. doi: 10.1111/1467-9280.00469 [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, & Spiegel D (2006). Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality, 40(6), 1054–1085. [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, & Thisted RA (2006). Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and Aging, 21(1), 140. [DOI] [PubMed] [Google Scholar]
- Cacioppo S, Capitanio JP, & Cacioppo JT (2014). Toward a neurology of loneliness. Psychological Bulletin, 140(6), 1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carton JS, Kessler EA, & Pape CL (1999). Nonverbal decoding skills and relationship well-being in adults. Journal of Nonverbal Behavior, 23(1), 91–100. [Google Scholar]
- Caspi A, Harrington H, Moffitt TE, Milne BJ, & Poulton R (2006). Socially isolated children 20 years later: risk of cardiovascular disease. Archives of Pediatrics and Adolescent Medicine, 160(8), 805–811. [DOI] [PubMed] [Google Scholar]
- Clifford S, Dissanayake C, Bui QM, Huggins R, Taylor AK, & Loesch DZ (2007). Autism spectrum phenotype in males and females with fragile X full mutation and premutation. Journal of Autism and Developmental Disorders, 37(4), 738–747. doi: 10.1007/s10803-006-0205-z [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: L. Erlbaum Associates. [Google Scholar]
- Coplan RJ, & Weeks M (2009). Shy and soft-spoken: shyness, pragmatic language, and socio-emotional adjustment in early childhood. Infant and Child Development, 18(3), 238–254. Retrieved from 10.1002/icd.622 [DOI] [Google Scholar]
- Crossman MK, Warfield ME, Kotelchuck M, Hauser-Cram P, & Parish SL (2018). Associations Between Early Intervention Home Visits, Family Relationships and Competence for Mothers of Children with Developmental Disabilities. Maternal and Child Health Journal, 22(4), 599–607. doi: 10.1007/s10995-018-2429-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnell JC, & Klann E (2013). The translation of translational control by FMRP: Therapeutic targets for FXS. Nature Neuroscience, 16(11), 1530–1536. doi: 10.1038/nn.3379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis NO, & Carter AS (2008). Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. Journal of Autism and Developmental Disorders, 38(7), 1278. doi: 10.1007/s10803-007-0512-z [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, & Griffin S (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. [DOI] [PubMed] [Google Scholar]
- Donovan NJ, Wu Q, Rentz DM, Sperling RA, Marshall GA, & Glymour MM (2017). Loneliness, depression and cognitive function in older US adults. International Journal of Geriatric Psychiatry, 32(5), 564–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eğeci İS, & Gençöz T (2006). Factors associated with relationship satisfaction: Importance of communication skills. Contemporary Family Therapy, 28(3), 383–391. [Google Scholar]
- Ekas NV, Lickenbrock DM, & Whitman TL (2010). Optimism, social support, and well-being in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 40(10), 1274–1284. [DOI] [PubMed] [Google Scholar]
- Falk NH, Norris K, & Quinn MG (2014). The factors predicting stress, anxiety and depression in the parents of children with autism. Journal of Autism and Developmental Disorders, 44(12), 3185–3203. [DOI] [PubMed] [Google Scholar]
- Faso DJ, Corretti CA, Ackerman RA, & Sasson NJ (2015). The broad autism phenotype predicts relationship outcomes in newly formed college roommates. Autism, 20(4), 412–424. doi: 10.1177/1362361315585733 [DOI] [PubMed] [Google Scholar]
- Fernandez E, Rajan N, & Bagni C (2013). The FMRP regulon: from targets to disease convergence. Frontiers in Neuroscience, 7(191). doi: 10.3389/fnins.2013.00191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielding-Gebhardt H, Warren SF, & Brady NC (2020). Child challenging behavior influences maternal mental health and relationship quality over time in fragile X syndrome. Journal of Autism and Developmental Disorders, 50(3), 779–797. doi: 10.1007/s10803-019-04308-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke P, Maier W, Hautzinger M, Weiffenbach O, Gänsicke M, Iwers B, … Froster U (1996). Fragile‐X carrier females: Evidence for a distinct psychopathological phenotype? American Journal of Medical Genetics Part A, 64(2), 334–339. [DOI] [PubMed] [Google Scholar]
- Gau SS-F, Chou M-C, Chiang H-L, Lee J-C, Wong C-C, Chou W-J, & Wu Y-Y (2012). Parental adjustment, marital relationship, and family function in families of children with autism. Research in Autism Spectrum Disorders, 6(1), 263–270. doi: 10.1016/j.rasd.2011.05.007 [DOI] [Google Scholar]
- Geurts HM, Verté S, Oosterlaan J, Roeyers H, Hartman CA, Mulder EJ, … Sergeant JA (2004). Can the Children’s Communication Checklist differentiate between children with autism, children with ADHD, and normal controls? Journal of Child Psychology and Psychiatry, 45(8), 1437–1453. [DOI] [PubMed] [Google Scholar]
- Goodrich-Hunsaker NJ, Wong LM, McLennan Y, Srivastava S, Tassone F, Harvey D, … Simon TJ (2011). Young adult female fragile X premutation carriers show age- and genetically-modulated cognitive impairments. Brain and Cognition. doi: 10.1016/j.bandc.2011.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodrich-Hunsaker NJ, Wong LM, McLennan Y, Tassone F, Harvey D, Rivera SM, & Simon TJ (2011). Adult female fragile X premutation carriers exhibit age- and CGG repeat length-related impairments on an attentionally-based enumeration task. Frontiers in Human Neuroscience, 5. doi: 10.3389/fnhum.2011.00063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Happe F, & Ronald A (2008). The ‘fractionable autism triad’: A review of evidence from behavioral, genetic, cognitive, and neural research. Neuropsychological Review, 18(4), 287–304. [DOI] [PubMed] [Google Scholar]
- Harris SW, Hessl D, Goodlin-Jones BL, Ferranti J, Bacalman S, Barbato I, … Abbeduto L (2008). Autism profiles of males with fragile X syndrome. American Journal on Mental Retardation, 113(6), 427–438. doi: 10.1352/2008.113:427-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley SL, DaWalt LS, Hong J, Greenberg JS, & Mailick MR (2019). Positive emotional support in premutation carrier mothers of adolescents and adults with fragile X syndrome: Gene by environment interactions. American Journal on Intellectual and Developmental Disabilities, 124(5), 411–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2003). Loneliness and pathways to disease. Brain, Behavior, and Immunity, 17(1), 98–105. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness Matters: A Theoretical and Empirical Review of Consequences and Mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, & Cacioppo JT (2008). From social structural factors to perceptions of relationship quality and loneliness: the Chicago health, aging, and social relations study. The journals of gerontology. Series B, Psychological sciences and social sciences, 63(6), S375–S384. doi: 10.1093/geronb/63.6.s375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich LM, & Gullone E (2006). The clinical significance of loneliness: A literature review. Clinical Psychology Review, 26(6), 695–718. doi: 10.1016/j.cpr.2006.04.002 [DOI] [PubMed] [Google Scholar]
- Hurley RS, Losh M, Parlier M, Reznick JS, & Piven J (2007). The broad autism phenotype questionnaire. Journal of Autism and Developmental Disorders, 37(9), 1679–1690. doi: 10.1007/s10803-006-0299-3 [DOI] [PubMed] [Google Scholar]
- Hyter YD (2007). Pragmatic language assessment: A pragmatics-as-social practice model. Topics in Language Disorders, 27(2), 128–145 Retrieved from http://journals.lww.com/topicsinlanguagedisorders/Fulltext/2007/04000/Pragmatic_Language_Assessment__A.5.aspx [Google Scholar]
- Ingersoll B, & Hambrick DZ (2011). The relationship between the broader autism phenotype, child severity, and stress and depression in parents of children with autism spectrum disorders. Research in Autism Spectrum Disorders, 5(1), 337–344. doi: 10.1016/j.rasd.2010.04.017 [DOI] [Google Scholar]
- Ingersoll B, Hopwood CJ, Wainer A, & Donnellan MB (2011). A comparison of three self-report measures of the broader autism phenotype in a non-clinical sample. Journal of Autism and Developmental Disorders, 41(12), 1646–1657. [DOI] [PubMed] [Google Scholar]
- Ingersoll B, Meyer K, & Becker MW (2011). Increased rates of depressed mood in mothers of children with ASD associated with the presence of the broader autism phenotype. Autism Research, 4(2), 143–148. [DOI] [PubMed] [Google Scholar]
- Jobe LE, & White SW (2007). Loneliness, social relationships, and a broader autism phenotype in college students. Personality and Individual Differences, 42(8), 1479–1489. doi: 10.1016/j.paid.2006.10.021 [DOI] [Google Scholar]
- Karst JS, & Van Hecke AV (2012). Parent and family impact of autism spectrum disorders: A review and proposed model for intervention evaluation. Clinical Child and Family Psychology Review, 15(3), 247–277. doi: 10.1007/s10567-012-0119-6 [DOI] [PubMed] [Google Scholar]
- Ketelaars MP, Cuperus J, Jansonius K, & Verhoeven L (2010). Pragmatic language impairment and associated behavioural problems. International Journal of Language and Communication Disorders, 45(2), 204–214. [DOI] [PubMed] [Google Scholar]
- Klusek J, Fairchild AJ, & Roberts JE (2019). Vagal tone as a putative mechanism for pragmatic competence: An investigation of carriers of the FMR1 premutation Journal of Autism and Developmental Disorders, 49, 197–208. doi: 10.1007/s10803-018-3714-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Hong J, Sterling A, Berry-Kravis E, & Mailick MR (2020). Inhibition deficits are modulated by age and CGG repeat length in carriers of the FMR1 premutation allele who are mothers of children with fragile X syndrome. Brain and Cognition, 139, 105511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Losh M, & Martin G (2014). Sex differences and within-family associations in the broad autism phenotype. Autism: International Journal of Research and Practice, 18, 106–116. doi: 10.1177/1362361312464529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Martin GE, & Losh M (2014a). A comparison of pragmatic language in boys with autism and fragile X syndrome . Journal of Speech, Language, and Hearing Research, 57, 1692–1707. doi: 10.1044/2014_JSLHR-L-13-0064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Martin GE, & Losh M (2014b). Consistency between research and clinical diagnoses of autism among boys and girls with fragile X syndrome. Journal of Intellectual Disability Reasearch, 58, 940–952. doi: 10.1111/jir.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, McGrath SE, Abbeduto L, & Roberts JE (2016). Pragmatic language features of mothers with the FMR1 premutation are associated with the language outcomes of adolescents and young adults with fragile X syndrome. Journal of Speech, Language, and Hearing Research, 59, 49–61. doi: 10.1044/2015_JSLHR-L-15-0102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Ruber A, & Roberts JE (2018). Impaired eye contact in the FMR1 premutation is not associated with social anxiety or the broad autism phenotype. The Clinical Neuropsychologist, 32, 1337–1352. doi: 10.1080/13854046.2017.1384063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Schmidt J, Fairchild AJ, Porter A, & Roberts JE (2017). Altered sensitivity to social gaze in the FMR1 premutation and pragmatic language competence. Journal of Neurodevelopmental Disorders, 9, 31. doi: 10.1186/s11689-017-9211-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunihira Y, Senju A, Dairoku H, Wakabayashi A, & Hasegawa T (2006). ‘Autistic’traits in non-autistic Japanese populations: relationships with personality traits and cognitive ability. Journal of Autism and Developmental Disorders, 36(4), 553–566. [DOI] [PubMed] [Google Scholar]
- Lamport D, & Turner LA (2014). Romantic Attachment, Empathy, and the Broader Autism Phenotype among College Students. The Journal of Genetic Psychology, 175(3), 202–213. doi: 10.1080/00221325.2013.856838 [DOI] [PubMed] [Google Scholar]
- Landa R (2000). Social language use in Asperger syndrome and high-functioning autism. In Ami K, Volkmar F, & Sparrow SS (Eds.), Asperger Syndrome (pp. 403–417). New York: Guilford Press. [Google Scholar]
- Landa R, Folstein SE, & Isaacs C (1991). Spontaneous narrative-discourse performance of parents of autistic individuals. Journal of Speech and Hearing Research, 34(6), 1339–1345. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1787716 [DOI] [PubMed] [Google Scholar]
- Landa R, Piven J, Wzorek MM, Gayle JO, Chase GA, & Folstein SE (1992). Social language use in parents of autistic individuals. Psychological Medicine, 22(1), 245–254. [DOI] [PubMed] [Google Scholar]
- Laws G, Bates G, Feuerstein M, Mason-Apps E, & White C (2012). Peer acceptance of children with language and communication impairments in a mainstream primary school: Associations with type of language difficulty, problem behaviours and a change in placement organization. Child Language Teaching and Therapy, 28(1), 73–86. doi: 10.1177/0265659011419234 [DOI] [Google Scholar]
- Lee M, Nayar K, Maltman N, Hamburger D, Martin GE, Gordon PC, & Losh M (2020). Understanding social communication differences in autism spectrum disorder and first-degree relatives: A study of looking and speaking. Journal of Autism and Developmental Disorders, 50(6), 2128–2141. doi: 10.1007/s10803-019-03969-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard MA, Milich R, & Lorch EP (2011). The role of pragmatic language use in mediating the relation between hyperactivity and inattention and social skills problems. Journal of Speech Language and Hearing Research, 54(2), 567–579. Retrieved from http://jslhr.asha.org/cgi/content/abstract/54/2/567 [DOI] [PubMed] [Google Scholar]
- Lewandowski AS, Palermo TM, Stinson J, Handley S, & Chambers CT (2010). Systematic Review of Family Functioning in Families of Children and Adolescents With Chronic Pain. The Journal of Pain, 11(11), 1027–1038. doi: 10.1016/j.jpain.2010.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis P, Abbeduto L, Murphy M, Richmond E, Giles N, Bruno L, … Orsmond G (2006). Psychological well‐being of mothers of youth with fragile X syndrome: Syndrome specificity and within‐syndrome variability. Journal of Intellectual Disability Research, 50(12), 894–904. [DOI] [PubMed] [Google Scholar]
- Loomis JW, Javornisky JG, Monahan JJ, Burke G, & Lindsay A (1997). Relations between family environment and adjustment outcomes in young adults with spina bifida. Developmental Medicine and Child Neurology, 39(9), 620–627. doi: 10.1111/j.1469-8749.1997.tb07498.x [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, & Bishop SL (2012). Autism Diagnostic Observation Schedule, Second Edition (ADOS-2). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Losh M, Childress D, Lam K, & Piven J (2008). Defining key features of the broad autism phenotype: A comparison across parents of multiple- and single-incidence autism families. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 147B(4), 424–433. doi: 10.1002/ajmg.b.30612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losh M, Klusek J, Martin GE, Sideris J, Parlier M, & Piven J (2012). Defining genetically meaningful language and personality traits in relatives of individuals with fragile X syndrome and relatives of individuals with autism. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 159B(6), 660–668. doi: 10.1002/ajmg.b.32070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losh M, Martin GE, Klusek J, Hogan-Brown AL, & Sideris J (2012). Social communication and theory of mind in boys with autism and fragile X syndrome. Frontiers in Psychology, 3, 1–12. doi: 10.3389/fpsyg.2012.00266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losh M, Martin GE, Lee M, Klusek J, Sideris J, Barron S, & Wassink T (2017). Developmental Markers of Genetic Liability to Autism in Parents: A Longitudinal, Multigenerational Study. Journal of Autism and Developmental Disorders, 47(3), 834–845. doi: 10.1007/s10803-016-2996-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu M, Yang G, Skora E, Wang G, Cai Y, Sun Q, & Li W (2015). Self-esteem, social support, and life satisfaction in Chinese parents of children with autism spectrum disorder. Research in Autism Spectrum Disorders, 17, 70–77. [Google Scholar]
- Maddalena A, Richards CS, McGinniss MJ, Brothman A, Desnick RJ, Grier RE, … Popovich B (2001). Technical standards and guidelines for fragile X: the first of a series of disease-specific supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics. Genetics in Medicine, 3(3), 200–205. doi: 10.1097/00125817-200105000-00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi CM, Chen H-Y, Hawkley LC, & Cacioppo JT (2011). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy A, Cuskelly M, van Kraayenoord CE, & Cohen J (2006). Predictors of stress in mothers and fathers of children with fragile X syndrome. Research in Developmental Disabilities, 27(6), 688–704. doi: 10.1016/j.ridd.2005.10.002 [DOI] [PubMed] [Google Scholar]
- Moos RH (1990). Conceptual and Empirical Approaches to Developing Family-Based Assessment Procedures: Resolving the Case of the Family Environment Scale. Family Process, 29(2), 199–208. doi: 10.1111/j.1545-5300.1990.00199.x [DOI] [PubMed] [Google Scholar]
- Moos RH, & Moos BS (1986). The Family Environment Scale: the manual Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Moser C, Mattie L, Abbeduto L, & Klusek J (in press). The FMR1 premutation phenotype and mother-child synchrony in fragile X syndrome. American Journal of Intellectual and Developmental Disabilities. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser C, Schmitt L, Schmidt J, Fairchild A, & Klusek J (2021). Response inhibition deficits in women with the FMR1 premutation are associated with age and fall risk. Brain and Cognition, 148, 105675. doi: 10.1016/j.bandc.2020.105675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Movaghar A, Page D, Brilliant M, Baker MW, Greenberg J, Hong J, … Mailick MR (2019). Data-driven phenotype discovery of FMR1 premutation carriers in a population-based sample. Science Advances, 5(8), eaaw7195. doi: 10.1126/sciadv.aaw7195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers BJ, Mackintosh VH, & Goin-Kochel RP (2009). “My greatest joy and my greatest heart ache:” Parents’ own words on how having a child in the autism spectrum has affected their lives and their families’ lives. Research in Autism Spectrum Disorders, 3(3), 670–684. [Google Scholar]
- Nayar K, Sealock JM, Maltman N, Bush L, Cook EH, Davis LK, & Losh M (2020). Elevated polygenic burden for autism spectrum disorder Is associated with the broad autism phenotype in mothers of individuals with autism spectrum disorder. Biological Psychiatry. doi: 10.1016/j.biopsych.2020.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Kopper BA, Barrios F, Gutierrez PM, & Bagge CL (2004). Reliability and validity of the Beck depression inventory--II with adolescent psychiatric inpatients. Psychological Assessment, 16(2), 120. [DOI] [PubMed] [Google Scholar]
- Pavot W, & Diener E (2009). Review of the satisfaction with life scale. In D. E. (Ed.), Assessing well-being (pp. 101–117). Dordrecht: Springer. [Google Scholar]
- Peplau LA, & Perlman D (1982). Perspectives on loneliness. In Peplau LA & Perman D (Eds.), Loneliness: A source-book of current thoery, research and therapy (pp. 1–8). New York: NY: Wiley. [Google Scholar]
- Piven J, Chase GA, Landa R, Wzorek M, Gayle J, Cloud D, & Folstein S (1991). Psychiatric disorders in the parents of autistic individuals. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 471–478. [DOI] [PubMed] [Google Scholar]
- Piven J, & Palmer P (1999). Psychiatric disorder and the broad autism phenotype: evidence from a family study of multiple-incidence autism families. American Journal of Psychiatry, 156(4), 557–563. [DOI] [PubMed] [Google Scholar]
- Piven J, Palmer P, Jacobi D, Childress D, & Arndt S (1997). Broader autism phenotype: Evidence from a family history study of multiple-incidence autism families. American Journal of Psychiatry, 154(2), 185–190. [DOI] [PubMed] [Google Scholar]
- Piven J, Palmer P, Landa R, Santangelo S, Jacobi D, & Childress D (1997). Personality and language characteristics in parents from multiple-incidence autism families. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 74(4), 398–411. [PubMed] [Google Scholar]
- Piven J, Palmer P, Landa R, Santangelo SJ,D, & Childress D (1997). Personality and language characteristics in parents from multiple-incidence autism families. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 74(4), 398–411. [PubMed] [Google Scholar]
- Prutting C, & Kirchner D (1983). Applied pragmatics. In Prutting CA (Ed.), Pragmatic assessment and intervention issues in language (pp. 29–64). San Diego, CA: College-Hill Press. [Google Scholar]
- Raspa M, Bailey DB Jr, Bann C, & Bishop E (2014). Modeling family adaptation to fragile X syndrome. American Journal on Intellectual and Developmental Disabilities, 119(1), 33–48. doi: 10.1352/1944-7558-119.1.33 [DOI] [PubMed] [Google Scholar]
- Rice F, Harold GT, Shelton KH, & Thapar A (2006). Family Conflict Interacts With Genetic Liability in Predicting Childhood and Adolescent Depression. Journal of the American Academy of Child and Adolescent Psychiatry, 45(7), 841–848. doi: 10.1097/01.chi.0000219834.08602.44 [DOI] [PubMed] [Google Scholar]
- Riggio RE, Watring KP, & Throckmorton B (1993). Social skills, social support, and psychosocial adjustment. Personality and Individual Differences, 15(3), 275–280. [Google Scholar]
- Roberts JE, Bailey DB, Mankowski J, Ford A, Weisenfeld LA, Heath TM, & Golden RN (2009). Mood and anxiety disorders in females with the FMR1 premutation. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 150B(1), 130–139. doi: 10.1002/ajmg.b.30786 [DOI] [PubMed] [Google Scholar]
- Roberts JE, Bradshaw J, Will E, Hogan AL , McQuillin S, & Hills K (2020). Emergence and rate of autism in fragile X syndrome across the first years of life. Development and Psychopathology, 32(4), 1335–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE, Tonnsen BL, McCary LM, Ford AL, Golden RN, & Bailey DB (2015). Trajectory and Predictors of Depression and Anxiety Disorders in Mothers with the FMR1 Premutation. Biological Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE, Tonnsen BL, McCary LM, Ford AL, Golden RN, & Bailey DB (2016). Trajectory and Predictors of Depression and Anxiety Disorders in Mothers with the FMR1 Premutation. Biological Psychiatry, 79(10), 850–857. doi: 10.1016/j.biopsych.2015.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruser TF, Arin D, Dowd M, Putnam S, Winklosky B, Rosen-Sheidley B, … Folstein S (2007). Communicative competence in parents of children with autism and parents of children with specific language impairment. Journal of Autism and Developmental Disorders, 37, 1323–1336. [DOI] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66(1), 20. Retrieved from https://auth.lib.unc.edu/ezproxy_auth.php?url=http://search.ebscohost.com/login.aspx?direct=true&db=s3h&AN=6380089&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Sanders JL, & Morgan SB (1997). Family stress and adjustment as perceived by parents of children with autism or Down syndrome: Implications for intervention. Child & Family Behavior Therapy, 19(4), 15–32. [Google Scholar]
- Sasson NJ, Lam KS, Childress D, Parlier M, Daniels JL, & Piven J (2013). The Broad Autism Phenotype Questionnaire: Prevalence and Diagnostic Classification. Autism Research, 6(2), 134–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider A, Johnston C, Tassone F, Sansone S, Hagerman R, Ferrer E, … Hessl D (2016). Broad autism spectrum and obsessive–compulsive symptoms in adults with the fragile X premutation. The Clinical Neuropsychologist, 30(6), 929–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Lusignolo TM, Albert M, & Berkman L (2001). Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging. Health Psychology, 20(4), 243. [DOI] [PubMed] [Google Scholar]
- Seidman I, Yirmiya N, Milshtein S, Ebstein RP, & Levi S (2012). The Broad Autism Phenotype Questionnaire: Mothers Versus Fathers of Children with an Autism Spectrum Disorder Journal of Autism and Developmental Disorders, 42, 837–846. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Barker ET, Greenberg JS, Hong J, Coe C, & Almeida D (2012). Differential sensitivity to life stress in FMR1 premutation carrier mothers of children with fragile X syndrome. Health Psychology, 31(5), 612–622. doi: 10.1037/a0026528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton AL, Cornish KM, Kraan CM, Lozano R, Bui M, & Fielding J (2016). Executive dysfunction in female FMR1 premutation carriers. The Cerebellum, 15(5), 565–569. [DOI] [PubMed] [Google Scholar]
- Singer GH (2006). Meta-analysis of comparative studies of depression in mothers of children with and without developmental disabilities. American Journal of Mental Retardation, 111(3), 155–169. doi: 10.1352/0895-8017(2006)111[155:Mocsod]2.0.Co;2 [DOI] [PubMed] [Google Scholar]
- Skuse DH, Mandy W, Steer C, Miller LL, Goodman R, Lawrence K, … Golding J (2009). Social communication competence and functional adaptation in a general population of children: preliminary evidence for sex-by-verbal IQ differential risk. Journal of the American Academy of Child and Adolescent Psychiatry, 48(2), 128–137. [DOI] [PubMed] [Google Scholar]
- Smith LE, Greenberg JS, & Seltzer MM (2012). Social support and well-being at mid-life among mothers of adolescents and adults with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(9), 1818–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snow CE (1994). Beginning from baby talk: Twenty years of research on input and interaction. In Gallaway C & Richards BJ (Eds.), Input and interaction in language acquisition (pp. 3–12). Cambridge, MA: Cambridge University Press. [Google Scholar]
- Snow P, & Douglas J (2017). Psychosocial aspects of pragmatic disorders. In Research in clinical pragmatics (pp. 617–649): Springer. [Google Scholar]
- Song J, Mailick MR, Greenberg JS, Ryff CD, & Lachman ME (2015). Cognitive aging in parents of children with disabilities. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 71, 821–830. doi: 10.1093/geronb/gbv015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprinkle SD, Lurie D, Insko SL, Atkinson G, Jones GL, Logan AR, & Bissada NN (2002). Criterion validity, severity cut scores, and test-retest reliability of the Beck Depression Inventory-II in a university counseling center sample. Journal of Counseling Psychology, 49(3), 381. [Google Scholar]
- Sterling AM, Mailick M, Greenberg J, Warren SF, & Brady N (2013). Language dysfluencies in females with the FMR1 premutation. Brain and Cognition, 82(1), 84–89. doi: 10.1016/j.bandc.2013.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern YS, Maltman N, & Roberts MY (2017). The influence of maternal pragmatics on the language skills of children with autism. Journal of Developmental and Behavioral Pediatrics, 38(5), 339–344. doi: 10.1097/DBP.0000000000000445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Roberti JW, & Roth DA (2004). Factor structure, concurrent validity, and internal consistency of the beck depression inventory—second edition in a sample of college students. Depression and Anxiety, 19(3), 187–189. doi: 10.1002/da.20002 [DOI] [PubMed] [Google Scholar]
- Thurston RC, & Kubzansky LD (2009). Women, loneliness, and incident coronary heart disease. Psychosomatic Medicine, 71(8), 836–842. doi: 10.1097/PSY.0b013e3181b40efc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmons L, Willis KD, Pruitt MM, & Ekas NV (2016). Predictors of daily relationship quality in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(8), 2573–2586. doi: 10.1007/s10803-016-2799-0 [DOI] [PubMed] [Google Scholar]
- Vasilopoulou E, & Nisbet J (2016). The quality of life of parents of children with autism spectrum disorder: A systematic review. Research in Autism Spectrum Disorders, 23, 36–49. doi: 10.1016/j.rasd.2015.11.008 [DOI] [Google Scholar]
- Wheeler A, Raspa M, Hagerman R, Mailick M, & Riley C (2017). Implications of the FMR1 premutation for children, adolescents, adults, and their families. Pediatrics, 139, S172–S182. doi: 10.1542/peds.2016-1159D [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler AC, Bailey DB Jr, Berry-Kravis E, Greenberg J, Losh M, Mailick M, … Hagerman R (2014). Associated features in females with an FMR1 premutation. Journal of Neurodevelopmental Disorders, 6(30). doi:: 10.1186/1866-1955-6-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler AC, Skinner DG, Bailey DB, & Abbeduto L (2008). Perceived quality of life in mothers of children with fragile X syndrome. American Journal on Mental Retardation, 113(3), 159–177. doi: 10.1352/0895-8017(2008)113[159:PQOLIM]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Whitehouse A, Watt H, Line E, & Bishop D (2009). Adult psychosocial outcomes of children with specific language impairment, pragmatic language impairment and autism. International Journal of Language and Communication Disorders, 44(4), 511–528. Retrieved from 10.1080/13682820802708098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehouse AJO, Barry JG, & Bishop DVM (2007). The broader language phenotype of autism: a comparison with specific language impairment. Journal of Child Psychology and Psychiatry, 48(8), 822–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zablotsky B, Anderson C, & Law P (2013). The association between child autism symptomatology, maternal quality of life, and risk for depression. Journal of Autism and Developmental Disorders, 43(8), 1946–1955. [DOI] [PubMed] [Google Scholar]


