Abstract
Background
Suicide is the second leading cause of death among U.S. college students. Past pandemics have been linked to increases in suicide risk, but little is known about how suicide risk relates to COVID-19 symptoms or hospitalizations.
Methods
We analyzed data from the Fall cohort of the 2020-2021 Healthy Minds Study, a cross-sectional, web-based survey of undergraduate and graduate students in the U.S. (N = 16,315). Logistic regression was used to test for associations between COVID-19 infections, hospitalizations, and symptoms severity, and suicide-related outcomes.
Results
Suicidal ideation was reported by n = 2190 (13.4%), plans by n = 885 (5.4%), and attempts by n = 209 (1.3%). The prevalence of each suicide-related outcome measure was greater among those reporting COVID-19 symptoms/diagnosis and among those with greater COVID-19 symptom severity, with a drastically greater prevalence of suicide attempts among those who were hospitalized for COVID-19, odds ratio (95% confidence interval) = 9.43 (3.87-22.95). Among respondents with suicidal ideation, 53.8% of those hospitalized for COVID-19 also made a suicide attempt, compared to 8.9% of non-infected respondents with past-year ideation.
Limitations
Limitations include the use of cross-sectional data and retrospective self-report measures, which may be subject to recall biases. The response rate was low but typical of online surveys conducted during the COVID-19 pandemic.
Conclusions
Hospitalization for COVID-19 may be an underestimated risk factor for suicide attempts. While mechanisms remain unclear, these data suggest that college students hospitalized for COVID should be screened for suicidal thoughts and behaviors subsequent to discharge, particularly if they have pre-existing suicidal ideation.
Keywords: Suicide, Attempts, COVID-19, Coronavirus, Ideation to action
1. Introduction
Suicide is the second leading cause of death among college students in the U.S. Significant physical illness, such as COVID-19, can potentially contribute to suicidal ideation by increasing hopelessness and social isolation (Banerjee and Rai, 2020; Twenge and Joiner, 2020), or through purported neurological and psychiatric effects of the illness (Leonardi et al., 2020; Montalvan et al., 2020; Ritchie et al., 2020; Werner et al., 2020). Therefore, the effects of COVID-19 would be expected to increase risk for suicidal ideation and behavior with increasing symptom severity, as greater severity would entail a commensurate level of physical and social consequences. Further, hospitalization and the risk of imminent mortality associated with more severe acute illness can potentially affect one's acquired capability for suicide by making one more familiar with and less fearful of death, while increasing pain tolerance (Klonsky and May, 2015; Van Orden et al., 2010). If so, hospitalization may be categorically linked to suicide attempts, regardless of the presence or absence of associations with COVID-19 symptoms.
Past pandemics, including Spanish Flu and HIV/AIDS, have been linked to increases in suicide risk (Glass, 1988; Wasserman, 1992), while studies are just emerging on suicide during the COVID-19 pandemic (Leaune et al., 2020). Suicidal ideation is reportedly prevalent on college campuses during the pandemic in the US (Wang et al., 2020), but little is known about how suicide risk directly relates to COVID-19 symptoms or hospitalizations. In this study, we sought to examine COVID-19 symptoms/diagnosis, symptom severity, and hospitalization as potential risk factors for suicidal thoughts and behaviors among college students in the United States. We further tested whether COVID-19 or COVID-19 severity statistically differentiated those with ideation alone from those with attempts, following an ideation-to-action framework.
2. Methods
2.1. Sample
We analyzed data from the Fall semester cohort of the 2020-2021 Healthy Minds Study (HMS), a cross-sectional, web-based survey examining mental health and related factors in undergraduate and graduate student populations (Healthy Minds Network, 2021). The survey was administered between September through December of 2020 at 28 universities. At each university, a random sample of 8000 students was invited by e-mail to participate, except at smaller universities (<8,000 students) where all students were invited to participate. The response rate was 14%, which is typical of online surveys of university populations (Lipson et al., 2019). Sample probability weights were used to adjust for non-response using the following administrative data on full student populations: gender, race/ethnicity, academic level, and GPA. The HMS was approved by the Institutional Review Boards at all participating campuses.
2.2. COVID-19 measurement
COVID-19 infection was measured using the item: “Have you had COVID-19 (the novel coronavirus disease)? Responses of “yes,” “probably,” and “maybe” were combined to form a binary variables indicating likely COVID symptoms or diagnosis. COVID-19 hospitalization was measured using the dichotomous item: Were you hospitalized because of your COVID-19 symptoms (yes/no)? COVID-19 severity was measured using the item: How severe were any symptoms that you experienced? Respondents could answer: Severe (e.g., difficulty breathing or speaking, low blood pressure, high fever of 103 F (39.4 C) or higher); Moderate (e.g., some shortness of breath, cough, fever of 100.4 F (38 C) or higher); Mild (e.g., cold-like symptoms); No symptoms (asymptomatic).
2.3. Suicidal ideation and behaviors
Binary variables indicated past-year ideation, plans, and attempts. Respondents were asked: “In the past year, did you ever seriously think about attempting suicide?” Respondents who stated ‘yes’ were then asked two additional items: “In the past year, did you make a plan for attempting suicide?” and “In the past year, did you attempt suicide?”
2.4. Sociodemographic covariates
Respondents self-reported sociodemographic characteristics, including gender identity, sexual orientation, race, ethnicity, age, and international student status.
2.5. Analysis
Of a total sample of 36,875 college students, 16,382 completed the COVID module and 32,811 completed the suicide module, leaving an analytic sample of N = 16,315. Remaining missing data for individual variables was handled using listwise deletion, which is appropriate for these survey data given the low frequency of missingness (1.2%, n = 186, missing data). Separate fixed effects logistic regression analyses were used to test for associations between COVID and suicide-related outcomes, and for associations between COVID symptom severity and suicide-related outcomes. Associations between COVID history and suicidal ideation and behavior are presented as odds ratios, adjusted for age, gender identity, sexual orientation, race/ethnicity, international status, and school. Additional analyses were conducted among the sub-sample with suicidal ideation, in order to explore whether COVID history and symptom severity were associated with suicide attempts among those with ideation, when conceptualized within an “ideation-to-action” framework (Klonsky and May, 2015).
3. Results
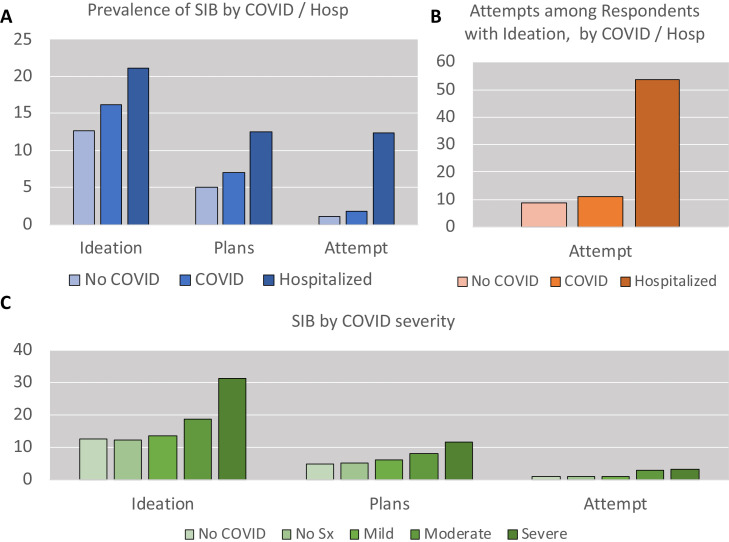
Respondent demographics, past year prevalence of suicidal ideation, plans, and attempts, and history of COVID-19 symptoms and hospitalization are presented in Table 1 . Suicidal ideation was reported by n = 2190 (13.4%), suicide plans by n = 885 (5.4%), and attempts by n = 209 (1.3%). The prevalence of all suicide-related outcome measures was greater among those reporting COVID-19 symptoms/diagnosis, and among those with greater COVID-19 symptom severity, with a particularly pronounced increase in suicide attempt prevalence among those who were hospitalized (Fig. 1 ). Past-year suicidal ideation was significantly associated with COVID symptoms OR(95% CI)=1.24(1.11-1.38), but not COVID-19 hospitalization, OR(95% CI)=1.57(0.81-3.05). Suicide plans were similarly associated only with COVID-19 symptoms/diagnosis, OR(95% CI)=1.34(1.15-1.57), but not hospitalization, OR(95% CI)=0.97-5.20). Prevalence of suicide attempts was likewise associated with COVID symptoms/diagnosis, OR(95% CI)=1.47(1.08-2.01). However, unlike suicidal ideation and suicide plans, the past-year prevalence of suicide attempts was drastically greater among those who were hospitalized for COVID, OR(95% CI)=9.43(3.87-22.95). Odds of suicidal ideation, OR(95% CI)=1.13(1.09-1.18), suicide plans OR(95% CI)=1.15(1.08-1.22), and suicide attempts, OR(95% CI)=1.27(1.14-1.41), were all modestly but significantly increased with increasing severity of COVID-19 symptoms.
Table 1.
Demographics of included participants.
| N = 16315 | N | % |
|---|---|---|
| Sex at birth | ||
| Male | 6726 | 41.2 |
| Female | 9563 | 58.6 |
| Intersex | 11 | 0.1 |
| Missing | 15 | 0.1 |
| Gender identity | ||
| Male | 6549 | 40.1 |
| Female | 9212 | 56.5 |
| Trans or other | 540 | 3.3 |
| Missing | 13 | 0.1 |
| Sexual Orientation | ||
| Heterosexual | 12809 | 78.5 |
| LGBTQ+1 | 3342 | 20.5 |
| Missing | 164 | 1.0 |
| Race | ||
| White, non-Latino | 11387 | 69.8 |
| Black, non-Latino | 1284 | 7.9 |
| Latino | 2289 | 14.0 |
| Asian/Pacific Islander, non-Latino | 987 | 6.1 |
| Other, non-Latino | 344 | 2.1 |
| Missing | 23 | 0.1 |
| Age | ||
| Years, Mean (SD) | 24.75 | 8.60 |
| International | ||
| Yes | 540 | 3.3 |
| No | 15768 | 96.7 |
| Missing | 7 | 0.0 |
| 12-month Suicide Ideation | ||
| Yes | 2190 | 13.4 |
| No | 14125 | 86.6 |
| 12-month Suicide Plans | ||
| Yes | 885 | 5.4 |
| No | 15395 | 94.4 |
| Missing | 34 | 0.2 |
| 12-month Suicide Attempts | ||
| Yes | 209 | 1.3 |
| No | 16062 | 98.4 |
| Missing | 45 | 0.3 |
| COVID-19 History | ||
| No symptoms/diagnosis | 12706 | 77.9 |
| COVID-19 symptoms or diagnosis | 3552 | 21.8 |
| Hospitalized | 57 | 0.3 |
| COVID-19 Severity | ||
| No COVID-19 | 12706 | 77.9 |
| No symptoms | 367 | 2.3 |
| Mild symptoms | 1857 | 11.4 |
| Moderate symptoms | 1141 | 7.0 |
| Severe symptoms | 239 | 1.5 |
| Missing | 4 | 0.0 |
Note: Variables without a “missing” row did not have missing data in our sample.
LGBTQ+ = Lesbian, gay, bisexual, transgender, queer, and other sexual minorities.
Fig. 1.
Suicidal ideation and behavior (SIB) by COVID status. (A) The past-year prevalence of suicidal ideation, plans, and attempts, by presence/absence of COVID-19 symptoms and hospitalization. (B) 12-month suicide attempts among respondents that reported suicidal ideation. (C) Suicidal ideation, plans, and attempts by COVID-19 symptom severity level (including non-infected, indicated as “no COVID,” and asymptomatic, indicated as “no sx”).
To test whether COVID distinguishes individuals with ideation alone from those who act upon that ideation, additional regression analyses were conducted specifically among respondents with past-year ideation. Among this sub-group (n = 2145), COVID-19 hospitalization was associated with a substantially greater prevalence of suicide attempts, OR(95% CI)=11.66(3.44-39.52); specifically, 53.8% (n = 7) of respondents with suicidal ideation that were hospitalized for COVID-19 also made a suicide attempt, compared to 8.9% (n = 139) of non-infected respondents with past-year ideation.
4. Discussion
4.1. Main findings
This study of US college students found that the presence of COVID-19 symptoms/diagnosis was significantly associated with suicidal ideation, suicide plans, and suicide attempts, with odds of each suicide measure increasing modestly with increasing COVID-19 symptom severity. Notably, COVID-19 hospitalization was associated with a substantially greater risk for suicide attempt. Specifically, 12.3% (7 out of n = 57) of hospitalized respondents reported a past-year attempt, and this jumped to more than 50% when focusing on respondents with underlying suicidal ideation (7 out of n = 13). Our findings call attention to an overlooked danger among college students hospitalized for COVID-19, which may potentially generalize others with severe COVID-19 as well.
4.2. Potential mechanisms
Several leading theories of suicidal behavior implicate a mechanism, variably labelled as “acquired capability” or “capacity,” which is indicative of an acquired pain tolerance and increased acceptance of the possibility of death. This appears to be critical for the transition from suicidal ideation to suicidal behavior. Being treated for an acutely life-threatening illness such as COVID-19 may also increase short-term capacity for suicide, especially if respondents experienced symptoms that were painful and required extreme life-preserving measures (e.g., ventilators), thereby reducing sensitivity to pain. Being hospitalized may also contribute towards recognizing death as an immediate possibility, thus weakening the barriers to suicidal behavior following hospitalization.
Prior studies have also suggested that COVID may affect the nervous system, similar to other coronavirus variants (Iadecola et al., 2020; Paterson et al., 2020). Individuals with COVID-19 have complained of memory loss, difficulty concentrating, and confusion even after recovering from the virus (Z9), and case reports have identified suicide-related symptoms (e.g., command hallucinations to attempt suicide) that appear to be specifically linked to COVID (Mirza et al., 2020). In addition to biological factors, several psychosocial influences (e.g., loneliness, hopelessness, or the stigma of COVID-19) may similarly increase in a linear fashion with increasing COVID-19 severity (Banerjee and Rai, 2020; Twenge and Joiner, 2020), and may mediate associations with suicide outcomes.
4.3. Limitations
Data were cross-sectional and did not allow us to determine the temporal order of events, although there is little conceptual reason expect prior suicide attempt to increase likelihood of contracting or being hospitalized for COVID-19. Second, the response rate for the survey was 14%, which is low but within the normal range for online surveys, and higher than reported in other studies on college students during the pandemic. Third, all measures were retrospective and self-report and therefore susceptible to social desirability or recall biases, although written self-report tends to yield more valid responses for stigmatized behaviors such as suicide (Turner et al., 1998). Finally, we did not have measures of potential mechanisms linking COVID-19 symptoms or hospitalization to suicide outcomes, which remains an open question.
4.4. Implications and conclusions
Recovering from COVID-19 symptoms does not necessarily signify the end of the virus's effects; our findings raise the possibility that COVID-19 infection increases risk for suicidal thoughts and behaviors among college students, and possibly other groups. While COVID-19 death rates are higher among older adults, suicide is the second leading cause of death among college students. Hospitalization for COVID-19, and possibly other medical conditions, may be an underestimated risk factor for suicide attempts. While mechanisms remain unclear, these data suggest that college students hospitalized for COVID should be screened for suicidal thoughts and behaviors subsequent to discharge, particularly if they have pre-existing suicidal ideation.
Conflict of Interest
None.
Acknowledgments
Author Statement
JD developed the study hypothesis, conducted the primary analyses, and wrote the initial draft of the manuscript. SZ contributed to data analysis and contributed to revisions of the manuscript. HO contributed to the development of the study concept and revised drafts of the manuscript.
Acknowledgments
None.
Role of funding
No external funding was used for this project.
References
- Banerjee D, Rai M. Social isolation in Covid-19: The impact of loneliness. Int. J. Soc. Psychiatry. 2020:525–527. doi: 10.1177/0020764020922269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass RM. AIDS and suicide. JAMA. 1988;259(9):1369–1370. [PubMed] [Google Scholar]
- Health Minds Network, retrieved from: https://healthymindsnetwork.org/hms/, February 12, 2021.
- Iadecola C., Anrather J., Kamel H. Effects of COVID-19 on the nervous system. Cell. 2020 doi: 10.1016/j.cell.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, May AM. The three-step theory (3ST): a new theory of suicide rooted in the “ideation-to-action” framework. Int. J. Cognit. Ther. 2015 Jun;8(2):114–129. [Google Scholar]
- Leaune E, Samuel M, Oh H, Poulet E, Brunelin J. Suicidal behaviors and ideation during emerging viral disease outbreaks before the COVID-19 pandemic: A systematic rapid review. Prev. Med. 2020 doi: 10.1016/j.ypmed.2020.106264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonardi M, Padovani A, McArthur JC. Neurological manifestations associated with COVID-19: a review and a call for action. J. Neurol. 2020;267:1573–1576. doi: 10.1007/s00415-020-09896-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipson S.K., Lattie E.G., Eisenberg D. Increased rates of mental health service utilization by US college students: 10-year population-level trends (2007-2017) Psychiatric services. 2019;70(1):60–63. doi: 10.1176/appi.ps.201800332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montalvan V., Lee J., Bueso T., De Toledo J., Rivas K. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin. Neurol. Neurosurg. 2020;194 doi: 10.1016/j.clineuro.2020.105921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson R.W., Brown R.L., Benjamin L., Nortley R., Wiethoff S., Bharucha T., Jayaseelan D.L., Kumar G., Raftopoulos R.E., Zambreanu L., Vivekanandam V. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 2020;143(10):3104–3120. doi: 10.1093/brain/awaa240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie K., Chan D., Watermeyer T. The cognitive consequences of the COVID-19 epidemic: collateral damage? Brain Commun. 2020;2(2) doi: 10.1093/braincomms/fcaa069. fcaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner C.F., Ku L., Rogers S.M., Lindberg L.D., Pleck J.H., Sonenstein F.L. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Joiner TE. Mental distress among US adults during the COVID-19 pandemic. J. Clin. Psychol. 2020;76(12):2170–2182. doi: 10.1002/jclp.23064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner Jr TE. The interpersonal theory of suicide. Psychol. Rev. 2010;117(2):575. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman IM. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life Threat. Behav. 1992;22(2):240–254. [PubMed] [Google Scholar]
- Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J. Med. Internet Res. 2020;22(9):e22817. doi: 10.2196/22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner C, Scullen T, Mathkour M, Zeoli T, Beighley A, Kilgore MD, Carr C, Zweifler RM, Aysenne A, Maulucci CM, Dumont AS. Neurological impact of coronavirus disease (COVID-19): practical considerations for the neuroscience community. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.04.222. [DOI] [PMC free article] [PubMed] [Google Scholar]