Abstract
Background. Burgeoning evidence suggests that loneliness during the COVID-19 pandemic is tied to high levels of depression and anxiety. The current study is unique, though, in examining which facets of social behavior and perceived social quality are most tied to internalizing symptoms using longitudinal data, including a pre-pandemic baseline, collected from a community sample of adults with pre-existing mental health concerns (analyzed n = 144). Methods. Participants completed measures of depressive and anxious symptoms pre-pandemic, followed by three weekly surveys during the pandemic. We distinguished four social variables: in-person social engagement, remote social engagement, social disruption, and social distress. OLS and mixed-effects regression models examined 1) pre-pandemic baseline symptoms as predictors of social functioning during the pandemic and 2) time-lagged associations between symptoms and social functioning during the pandemic. Results. Social behavior and social perceptions were dissociable. Baseline depressive, but not anxious, symptoms predicted greater social distress during the pandemic. Both anxious and depressive symptoms were predicted by social variables, but the specific associations differed: depressive symptoms were related to perceived social quality, whereas anxious symptoms were more tied to reported social behavior. Limitations. We relied on self-report indices, and causality should not be inferred directly from these correlational data. Conclusions. Overall, our results indicate that it is possible to follow social guidelines and even to spend relatively few hours socializing with close others, while still feeling connected and rewarded; however, people who struggle with depression and anhedonia were particularly vulnerable to distressing feelings of social disconnection amid the pandemic.
Keywords: COVID-19, Internalizing symptoms, Social functioning
Longitudinal associations between internalizing symptoms, social behavior, and social perceptions in the initial months of the COVID-19 pandemic: Findings from a transdiagnostic community sample
A rapidly emerging literature is documenting the global mental health challenges presented by the COVID-19 pandemic (e.g., Salari et al., 2020; Torales et al., 2020). In particular, there is considerable interest in identifying risk and protective factors associated with psychological and behavioral adjustment amid the pandemic (see Holmes et al., 2020; Van Bavel et al., 2020).
One of the most striking features of the COVID-19 pandemic has been an extraordinary shift in everyday human social behavior (Masters et al., 2020). Consistent with a broad raft of empirical evidence documenting the profound effects of social relationships and connectedness on adjustment to stressful life events and chronic stressors, psychological wellbeing, and physical health (e.g., Cacioppo and Cacioppo, 2014; Hawkley and Cacioppo, 2010; Rico-Uribe et al., 2018), social functioning amid the pandemic has been identified by researchers and policymakers as a critical domain of investigation and intervention (e.g., Killgore et al., 2020; Smith and Lim, 2020),
Emerging research indicates that the COVID-19 pandemic and associated social distancing behavior have contributed to increases in loneliness for many people (e.g., Killgore et al., 2020; Li and Wang, 2020; Tull et al., 2020), although findings have been heterogenous. More to the point, individual differences in loneliness, social distance, and perceived social support have consistently been found to be robust correlates of psychological adjustment amidst the COVID-19 pandemic, particularly for internalizing symptoms of depression and anxiety (e.g., Creese et al., 2020; Marroquin, Vine, and Morgan, 2020; Palgi et al., 2020). There is some evidence that these associations are bidirectional, such that individuals whose initial affective response to the COVID-19 pandemic was more negative were at greater risk of subsequently experiencing feelings of social disconnection and vice versa (Okruszek et al., 2020).
Nevertheless, much remains to be understood about how changes in social behavior, social connectedness, and internalizing symptoms are woven together over time, specifically in the context of the COVID-19 pandemic. First, considerable evidence shows that social behavior and social perceptions are correlated, but dissociable (e.g., Cacioppo et al., 2011; de Jong Gierveld, van Tilburg, and Dykstra, 2018; Haber et al., 2007). This observation underscores the need to consider behavior and subjective experience concurrently to identify more specific correlates of internalizing symptoms, yet these have often been assessed in isolation. Second, most of the available studies have relied on cross-sectional rather than longitudinal data or have not had access to pre-COVID baseline data, which limits the conclusions that can be drawn regarding temporal precedence. Third, few studies have focused specifically on individuals with a history of mental health difficulties, who may be particularly vulnerable to worsening mental health amid the high stress environment of the pandemic. Our goal was to respond to these three gaps.
A central aim of the current study was to identify unique associations of social behavior and perceived social quality with internalizing symptoms. Accordingly, we sought to disentangle four distinct social variables: 1) in-person social engagement (i.e., weekly hours spent interacting face-to-face with non-cohabiting close others); 2) remote social engagement (e.g., by phone, video chat); 3) perceptions of social disruption related to the pandemic (e.g., lower quality of social interactions as a result of social distancing); and 4) social distress (e.g., feelings of social disconnection or social anhedonia).
We examined links between our key variables across two timescales. First, we examined the extent to which pre-pandemic baseline measures of internalizing symptoms predicted in-person or remote social engagement, perceived social disruption, or perceived social distress during the pandemic. Second, we examined the time-lagged associations between internalizing symptoms and these same social variables in the weekly data gathered during COVID. We predicted that 1) higher pre-pandemic internalizing symptoms would predict greater social distress and disruption amid the pandemic and 2) that internalizing symptoms and social distress would be reciprocally and positively associated throughout the repeated assessments gathered during the pandemic.
Method
Participants and procedure
For the present study we capitalized on a well-characterized transdiagnostic community sample (n = 191) of US residents living in metropolitan areas who had completed baseline measures of internalizing symptoms pre-pandemic. To gage social behavior, perceived social functioning and internalizing symptoms during the early phase of the COVID-19 pandemic, these participants were invited to complete up to three additional once-weekly follow-up assessments. Baseline and follow-up procedures are described in more detail below.
Baseline procedures
Participants were originally recruited as part of a dual-site study investigating transdiagnostic mechanisms of mental illness. Participants were recruited via flyers posted in community locations, outreach to treatment centers, as well as via online advertisements (e.g., on Craigslist). Inclusion and exclusion criteria were assessed via phone interview and during the first face-to-face interviews. To meet inclusion criteria, participants were required to be between ages 18 and 55 and currently receiving or seeking mental health treatment, experiencing functional impairment due to mental health concerns (Sheehan Disability Scale score > 5) (Williams, 2008), or receiving government disability benefits for mental health reasons. Participants were ineligible if they reported daily use of marijuana, antipsychotic medication, or sedating medications; met diagnostic criteria for current (past 6 month) alcohol or substance use disorder or lifetime psychosis or mania on the SCID; had a lifetime history of head trauma resulting in loss of consciousness for at least five minutes or resulting in lasting effects; showed problems with memory or concentration (unweighted Orientation Memory Concentration test score < 7); reported any medical conditions or treatments that might interfere with psychiatric diagnosis (e.g., untreated endocrine disorders, HIV, syphilis, treatment for cancer); reported any neurological disorders; had received electroshock treatment within the past year; had language or vision problems that would interfere with ability to independently complete study tasks; and for the majority of Site A participants, MRI contraindications (e.g., ferrous metal in the body, seizure disorders, pregnancy, inability to stay in small spaces for extended periods of time).
After eligibility was determined, participants who consented to participate attended three or four in-person study sessions consisting of a structured clinical interview, questionnaires, behavioral tasks, and, for a subset, neuroimaging tasks. Baseline data were collected between March 01, 2017 and April 11, 2020.2 Six participants were excluded from follow-up due to failure to pass at least half of the 10 attention check items (e.g., choose D as your response for this item) in the questionnaires and/or poor behavioral task performance. Participants who passed catch trials and showed adequate performance on the baseline behavioral tasks (N = 190) were invited to take part in the online COVID follow-up study. All participants completed urine toxicology tests to rule out substance use on the day of behavioral assessments; none were excluded for failing these tests.
COVID follow-up procedures
Participants who enrolled in the COVID follow-up completed up to three online surveys at approximately one-week intervals on Qualtrics. The week 1 COVID follow-up assessments were conducted between April 20 and June 18, 2020, spanning the first two to five months of the pandemic (M days after March 11, 2020 = 48.12, SD = 6.17). On average, participants completed the first COVID follow-up survey 474.70 days after participating in the baseline assessment (SD = 314.95, range = 13 to 1149 days). The Week 1 survey took about 30 min, whereas the Week 2 and Week 3 surveys took about 15 min. To ensure data quality, data were flagged for review and potentially excluded from further follow-up, if participants: 1) missed three or more attention check items out of three to four checks total depending on wave (e.g., please choose “d” as your response to this item), 2) completed the survey in under five minutes, 3) lacked response variance (i.e., provided the same response across two or more scales), or 4) demonstrated inconsistent/randomized response patterns (i.e., a low correlation between even and odd items).
Of the 190 participants invited to complete the COVID follow-up surveys, 22 did not complete the first COVID survey and 15 were excluded due to data checks, leaving 153 valid responses at Week 1. 143 participants remained at Week 2 (93.5% of the week 1 sample), and 137 at Week 3 (95.8% of the Week 2 sample). Attrition between COVID weekly batteries was attributable to a combination of random experimenter error (i.e., failure to send participants timely follow-up surveys), late survey completion (which did not allow time for additional follow-ups), and participant drop-out. Of the 153 individuals with otherwise valid Week 1 COVID follow-up data, nine were excluded from analyses due to missing data (5-missing pre-COVID internalizing symptoms, 2-missing social engagement data during COVID, 2-missing data on whether they lived with their partner during COVID).
The final sample (N = 144) consisted of 107 women, 34 men, and 3 non-binary people, with ages ranging from 18 to 55 years old (Mage = 28.51 yrs.). 51% of participants identified as White, 22% as Asian, 13% as Black/African American, 11% as other/multiple, and 4% unknown; additionally, 24% of the sample identified as Hispanic/Latinx. On average, participants reported 15.70 years of education (SD = 2.33, range = 8 to 21 years) and a median household income level of $40,000 to $50,000 per year.
Measures
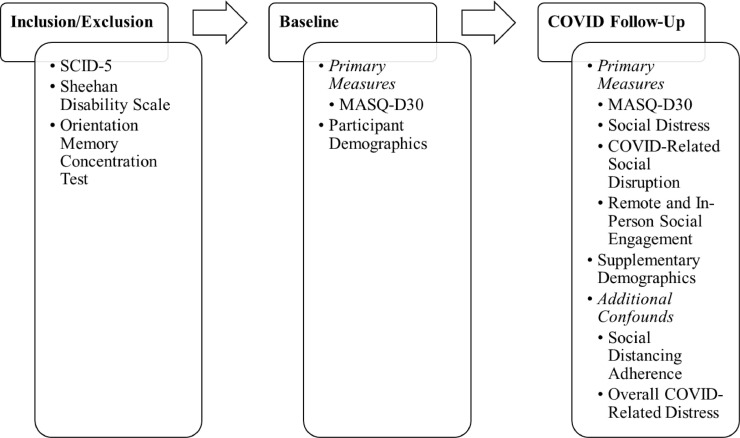
Participants completed several measures to assess their eligibility to participate, including selected modules from the Structured Clinical Interview for DSM-5, the Sheehan Disability Scale, and the Orientation Memory Concentration Test, during the phone screen and the first interview. As part of the baseline battery, participants provided demographic information and completed the Mood and Anxiety Symptoms Questionnaire (30 Item Short Form). During the COVID-19 follow-up phase, participants provided supplementary demographic information and completed the Mood and Anxiety Symptoms Questionnaire (30 Item Short Form), as well as measures of social distress, COVID-related social disruption, remote and in-person social engagement, adherence to social distancing, and overall COVID-related distress. For a visual breakdown of the measures that were administered and the timing of administration, see Fig. 1 . See below for more detailed information about each of the measures.
Fig. 1.
Visual breakdown of measure administration timing. Note. MASQ-D30 = Mood and Anxiety Symptoms Questionnaire (30 Item Short Form); SCID-5 = Structured Clinical Interview for DSM-5.
Measures of inclusion/exclusion
Psychological Diagnoses. The Structured Clinical Interview for DSM-5 (SCID-5) (First et al., 2015) is a commonly used and well-validated semi-structured interview designed to assess psychological diagnoses. Interviewers underwent didactive and interactive training (e.g., roleplaying, practicing coding with recorded training tapes) and were required to demonstrate sufficient inter-rater reliability before conducting clinical interviews with study participants. Throughout the study, reliability meetings were held to protect against rater drift. The average kappa (between the rater and gold standard diagnostic score) was 0.82.
Functional and Cognitive Impairment. The Sheehan Disability Scale (Leon et al., 1997) is a well-validated measure of functional impairment across three domains: work/school, social life, and family life. Potential participants were asked to pick, from the past six months, the worst month in terms of their mental health symptoms. Then, they rated how much these symptoms interfered with their lives, across each of the three domains, on a scale of 0–10, with verbal anchors provided: no (0), mild (1–3), moderate (4–6), severe (7–9), or very severe interference (10).
The Orientation Memory Concentration Test (Katzman et al., 1983) is a well-validated assessment of cognitive impairment. Total scores (range 0 to 12) reflect the number of errors across six items.
Baseline measures
Participants provided demographic information at baseline, specifically including their age, gender, race, ethnicity, and years of education.
Internalizing Symptoms. We used the 30-item short version of the Mood and Anxiety Symptoms Questionnaire (MASQ-D30), which shows similar psychometric properties to the full questionnaire, good internal consistency, and adequate construct validity between its subscales and other established dimensional measures of internalizing psychopathology (Wardenaar et al., 2010). For the sake of parsimony, we focused on the two subscales designed to differentiate depression (i.e., the anhedonic depression subscale) and anxiety (i.e., the anxious arousal subscale) and not on the general distress subscale, which reflects symptoms common to both depression and anxiety. Each subscale consists of ten items. Participants were asked to rate the degree to which they experienced various thoughts, feelings, and sensations within the past week on a scale from 1 (Not at all) to 5 (Extremely). Exemplar items from the anxious arousal subscale included: “Startled easily”, “Felt nauseous”, and “Was trembling or shaking”; items from the anhedonic depression subscale included: “Felt optimistic”, “Felt like I had a lot of energy”, “Felt really good about myself” (all reverse scored). Subscale scores were based on item totals. As shown in Table 1 , internal consistency was high for both subscales.
Table 1.
Means, standard deviations, and internal consistencies (omega) for repeated measures variables (N = 144).
| Baseline | COVID Week 1 | COVID Week 2 | COVID Week 3 | ||||||||||||
| Measures | M | SD | ω | M | SD | ω | M | SD | ω | M | SD | ω | |||
| MASQ | |||||||||||||||
| Anhedonic Depression | 35.99 | 6.83 | .92 | 35.74 | 7.36 | .92 | 35.39 | 8.11 | .94 | 36.36 | 8.33 | .94 | |||
| Anxious Arousal | 16.01 | 5.29 | .86 | 17.89 | 6.80 | .89 | 17.17 | 6.60 | .89 | 16.54 | 6.04 | .87 | |||
| Social Distress | 18.98 | 4.49 | .83 | 18.68 | 4.89 | .86 | 18.43 | 5.05 | .84 | ||||||
| Social Disruption | 15.63 | 3.63 | .72 | 16.12 | 4.15 | .81 | 16.08 | 3.71 | .80 | ||||||
| Social Engagement | |||||||||||||||
| Hours In-Person | 7.04 | 15.73 | 6.71 | 15.74 | 9.71 | 20.45 | |||||||||
| Hours Remote | 14.14 | 13.41 | 11.80 | 12.91 | 11.44 | 14.79 | |||||||||
| Social Distancing Adherence | 6.03 | 1.16 | 5.99 | 1.23 | 5.92 | 1.21 | |||||||||
| Overall COVID Distress | 3.54 | 1.04 | 3.22 | 1.02 | 3.18 | 1.11 | |||||||||
COVID follow-up measures
In the Week 1 COVID survey, participants indicated whether they lived with a spouse or romantic partner (dummy-coded as 0 = No, 1 = Yes) and rated their household income on an ordinal scale from 0 (Less than $10,000) to 12 (More than $150,000). In the Week 2 and 3 COVID assessments, these questions were only repeated if the participant indicated a change in their living situation or employment status.
Participants completed the measures listed below at each weekly assessment. Table 1 provides means, standard deviations, and internal consistencies (Revelle and Zinbarg, 2009) for each of these measures, broken out by time-point.
Internalizing Symptoms. As in the baseline assessment, participants completed the MASQ-D30 anxious arousal and anhedonic depression subscales at each COVID assessment timepoint (Wardenaar et al., 2010). Items within each subscale demonstrated strong internal consistency at each timepoint.
Social Distress. Participants completed a six-item measure assessing their social distress within the past week. Items were adapted from existing measures of loneliness, social disconnection, and social anhedonia (e.g., De Jong Gierveld and Kamphuis, 1985; Russell et al., 1980). Exemplar items included: “I felt lonely”, “I missed being around people,” and “My relationships with my friends, family, and/or romantic partners were rewarding” (reverse scored). Responses were rated on a scale from 1 (Strongly disagree) to 5 (Strongly agree), and showed high internal consistency. Scoring was the sum of item scores, where higher scores reflect greater social distress.
COVID-Related Social Disruption. Participants answered five face-valid items comparing their social interactions over the past week (e.g., quality, frequency) to those before COVID. Each of the five items shared a common stem: “As a result of COVID-19 and social distancing…” Participants rated statements such as “I am having social interactions…”, “I am having conflict with friends, family, romantic partners, and/or coworkers…” (reverse scored), and “The quality of my social interactions is…”, on a scale from 1 (Much more/better) to 5 (Much less/worse). Scoring was the sum of the items, where higher scores reflect greater social disruption due to COVID; items showed acceptable-to-good internal consistency.
Remote and In-Person Social Engagement. Participants indicated the number of hours in the past week they spent (1) remotely and (2) in-person with friends, family, and romantic partners with whom they did not live. Two participants reported socializing 24/7 (i.e., 168 h) at various timepoints, and so their entries were winsorized to the second highest number of remote or in-person hours reported for the corresponding assessment period.
Social Distancing. Participants completed two items regarding their awareness of and adherence to social distancing recommendations (e.g., to stay six feet apart from everyone except members of their household). At Week 1, 100% of participants indicated their awareness of social distancing recommendations. Therefore, we only included the latter item (i.e., adherence) in analyses. The adherence item was rated on a scale from 1 (None of the time) to 7 (All of the time).
Overall COVID-Related Distress. Participants were asked to indicate their overall level of distress regarding COVID-19 on a scale from 1 (No distress) to 6 (So much distress that it is almost unbearable to cope with).
Data analysis
Prior to testing our hypotheses, we examined potential sample and attrition biases; adherence to social distancing guidelines; and univariate and bivariate descriptive statistics, including zero-order, intraclass, and repeated measures correlations between key and demographic variables (Bakdash and Marusich, 2017). More specifically, to detect potential attrition biases, we used chi-square and t-tests to evaluate whether participant demographics (i.e., age, gender, race, Hispanic/Latinx status, and level of education) or baseline MASQ depression and anxiety scores predicted taking part in the COVID follow-up assessments.
To ascertain the degree to which pre-pandemic internalizing symptoms (i.e., MASQ depression and anxiety scores) longitudinally predicted social adjustment to the COVID-19 pandemic (Hypothesis 1), we computed four parallel multiple regression models to assess social distress, remote social engagement, in-person social engagement, and COVID-related social disruption at Week 1 of the COVID follow-up. In each of these models, we adjusted for potential confounds of age, gender, income, living with a significant other (cf. Okabe-Miyamoto et al., 2021), self-reported adherence to social distancing guidelines, and the number of days (1) between the baseline timepoint and the first COVID timepoint and (2) between the WHO COVID pandemic declaration on March 11, 2020 and the first COVID timepoint.
Next, we examined time-lagged associations between social functioning and internalizing symptoms within the weekly follow-ups (Hypothesis 2) in three parallel random-intercept mixed effects models. The dependent variables for these models were social distress, depression symptoms, and anxiety symptoms. Independent variables were past-week anxiety and depression symptoms, social engagement, COVID-related social disruption, and social distress. As before, we adjusted for potential confounds. Although our focus was on these time-lagged relationships, random-intercept mixed effects models to estimate same-week (i.e., within-timepoint) associations in the repeated measures data are reported in the online supplement for completeness.
All analyses were conducted in R version 4.0.2 (R Core Team, 2020). Repeated measures correlations were implemented with the rmcorr package (Bakdash and Marusich, 2017). Mixed effects models were implemented with the lme4 package using restricted maximum likelihood (REML) estimation (Bate et al., 2015). Corresponding p-values were estimated with the lmertest and pbkrtest packages using the Kenward-Roger approximation (Halekoh and Højsgaard, 2014; Kenward and Roger, 1997; Kuznetsova et al., 2017). Pseudo-r 2 values were computed for the mixed effects models with the MuMIn package (Bartoń, 2009; Nakagawa and Schielzeth, 2013).
Results
Attrition
Whereas attrition was unrelated to depression symptom scores and most demographic variables, the participants who completed at least one COVID follow-up assessment had significantly lower baseline MASQ anxiety scores (M = 15.95, t(304.14) = 2.39, p = .02) and significantly more years of education (M = 15.61, t(316.70)= 2.69, p = .008) relative to participants who did not complete any COVID follow-up surveys (Manx = 17.52, Medu = 14.93).
Within the COVID subsample, we observed no significant differences in demographics or MASQ anxiety and depression subscales between those who completed all three surveys and those who were lost to follow-up after completing the Week 1 COVID survey.
Adherence to social distancing guidelines and Covid-related distress
At the first weekly assessment, 100% of participants indicated that they were aware of guidelines instructing people to maintain at least 6 feet of distance from other people, and 93.5% of participants reported that they were adhering to this recommendation at least half of the time (≥ 4 on a 7-point scale). 53.6% of participants reported at Week 1 that they were currently at least moderately distressed regarding COVID-19 (≥ 4 on a 6-point scale), and only 2% reported that they were experiencing no distress (1 on a 6-point scale).
Associations between key variables
As one would expect, pre-pandemic symptoms of depression were correlated with depression symptoms at the first COVID timepoint, and this was also true for anxiety symptoms, as shown in Table 2 . On the other hand, pre-pandemic depression symptoms were not significantly correlated with Week 1 anxiety symptoms, nor did pre-pandemic anxiety symptoms predict Week 1 depression symptoms. Likewise, repeated measures of depression symptoms during the three weekly follow-ups were only modestly correlated on a same-week basis with anxiety symptoms, indicating substantial separability of depression and anxiety symptoms.
Table 2.
Zero-order, repeated measures, and intraclass correlations for key and demographic variables (N = 144).
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | ICCs | |
| (1) Pre-Pandemic MASQ Depression | – | .21* | .45*** | .11 | .30* | .04 | .02 | .11 | .04 | −0.05 | −0.02 | −0.04 | −0.03 | – |
| (2) Pre-Pandemic MASQ Anxiety | – | .12 | .62*** | .17* | −0.02 | .08 | −0.01 | −0.11 | −0.17* | −0.18* | −0.08 | −0.04 | – | |
| (3) COVID MASQ Depression | – | .12* | .31*** | −0.05 | .10 | .24*** | .06 | −0.11 | −0.10 | −0.01 | −0.05 | .67 | ||
| (4) COVID MASQ Anxiety | – | .20*** | .04 | .11 | .10 | .03 | −0.18* | −0.15 | −0.07 | −0.02 | .73 | |||
| (5) Social Distress | – | .05 | −0.07 | .26*** | .17** | .14 | −0.18* | .00 | −0.35*** | .65 | ||||
| (6) Social Engagement - Remote | – | −0.06 | .03 | −0.03 | .03 | −0.19* | −0.04 | −0.20* | .49 | |||||
| (7) Social Engagement - In-Person | – | .12 | −0.09 | −0.04 | .02 | −0.08 | .00 | .73 | ||||||
| (8) Social Disruption | – | .10 | .11 | −0.03 | −0.02 | −0.07 | .69 | |||||||
| (9) Social Distancing Adherence | – | −0.08 | .13 | .17** | .03 | .55 | ||||||||
| (10) Gender (107 female, 34 male) | – | .19* | .07 | −0.11 | – | |||||||||
| (11) Age | – | .03 | .17* | – | ||||||||||
| (12) Income | – | .17* | .92 | |||||||||||
| (13) Lives with SO (101 no, 43 yes) | – |
Note. Repeated measures correlations were computed to estimate associations between pairs of variables that were assessed at multiple timepoints (#3, 4, 5, 6, 7, 8, 9). Zero-order correlations were computed to estimate associations between pairs of variables that were assessed only once (#1, 2, 10, 11, 12, 13) or between baseline and repeated measures variables. In the latter case, repeated measures variables were aggregated across timepoints, within individuals.
Consistent with our aim of concurrently examining multiple social indices, social distress was only modestly associated with COVID-related social disruption, and all other correlations between social distress, disruption, and engagement were low and nonsignificant (see Table 2). Social distress was moderately, negatively correlated with living with a significant other, but only modestly, positively correlated with self-reported adherence to social distancing guidelines. Weekly depression symptoms were significantly correlated with same-week perceived social distress and perceived COVID-related social disruption but were not significantly correlated with in-person or remote social engagement. Anxiety symptoms were significantly, but modestly correlated with social distress and were not significantly correlated with either COVID-related social disruption, remote social engagement, or in-person social engagement.
Also shown in Table 2, intraclass correlations for the repeated assessments of each of our key variables were moderate to high, ranging from 0.49–0.73, indicating that individuals were relatively stable over time on these measures throughout our data collection window (i.e., that the preponderance of the variability across these measures was between-persons). As illustrated by Figure S1, though, both absolute levels and patterns of change over time for our key variables differed significantly between participants.
Tests of hypotheses
With regard to Hypothesis 1, we found that higher pre-pandemic depression symptoms—but not pre-pandemic anxiety symptoms—predicted higher Week 1 social distress, as shown in Table 3 . By contrast, neither pre-pandemic depression symptoms nor pre-pandemic anxiety symptoms significantly predicted remote or in-person social engagement or COVID-related social disruption. All results for key variables were substantively identical regardless of whether covariates were included or not.
Table 3.
Parameter estimates for four OLS regression models predicting social adjustment during the pandemic (social distress, remote social engagement, in-person social engagement, social disruption) from pre-pandemic internalizing symptoms (N = 144).
| Social Distress | Social Engagement – Remote |
Social Engagement – In-Person |
Social Disruption | ||||||||||
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | ||
| Pre-Pandemic MASQ Depression | .20 | .04, 0.36 | .02 | .06 | −0.11, 0.22 | .49 | .04 | −0.13, 0.21 | .67 | .16 | −0.01, 0.33 | .06 | |
| Pre-Pandemic MASQ Anxiety | .13 | −0.04, 0.30 | .14 | −0.17 | −0.34, 0.00 | .052 | .11 | −0.07, 0.29 | .22 | −0.06 | −0.24, 0.12 | .50 | |
| Gender | .37 | −0.01, 0.76 | .06 | .07 | −0.33, 0.47 | .73 | −0.07 | −0.48, 0.33 | .72 | .02 | −0.40, 0.43 | .94 | |
| Age | −0.07 | −0.24, 0.10 | .44 | −0.25 | −0.43, −0.07 | .01 | .07 | −0.11, 0.26 | .42 | .01 | −0.17, 0.19 | .91 | |
| Income | −0.01 | −0.17, 0.15 | .86 | −0.18 | −0.34, −0.01 | .04 | .12 | −0.05, 0.29 | .15 | .07 | −0.10, 0.24 | .40 | |
| Living with Significant Other | −0.34 | −0.71, 0.03 | .07 | −0.32 | −0.69, 0.04 | .08 | −0.01 | −0.40, 0.39 | .98 | .21 | −0.18, 0.60 | .29 | |
| Social Distancing Adherence | .10 | −0.06, 0.26 | .24 | −0.13 | −0.29, 0.03 | .12 | −0.22 | −0.39, −0.05 | .01 | .12 | −0.05, 0.28 | .18 | |
| Days Since Baseline | −0.08 | −0.24, 0.08 | .33 | −0.14 | −0.31, 0.03 | .10 | .07 | −0.11, 0.24 | .45 | .02 | −0.16, 0.19 | .86 | |
| Days Since Pandemic Declaration | .11 | −0.06, 0.27 | .20 | −0.08 | −0.25, 0.09 | .34 | .05 | −0.12, 0.23 | .53 | .17 | −0.00, 0.35 | .054 | |
| R2/Adjusted R2 | .14/0.08 | .5/0.09 | .09/0.02 | .08/0.02 | |||||||||
With regard to Hypothesis 2, we found that social distress was significantly predicted by past week depression symptoms and COVID-related social disruption, but not by anxiety symptoms, in-person social engagement, or remote social engagement, such that higher past week depression symptoms and higher perceived social disruption were both related to greater social distress the following week (see Table 4 ).
Table 4.
Parameter estimates for time-lagged (next-week) mixed-effects regression models (N = 138; k = 268).
| Social Distress | Depression Symptoms | Anxiety Symptoms | |||||||
| b | 95% CI | p | b | 95% CI | p | b | 95% CI | p | |
| Social Distress | – | – | – | .11 | −0.02, 0.24 | .09 | .01 | −0.10, 0.12 | .81 |
| Depression Symptoms | .25 | .13, 0.37 | < 0.001 | – | – | – | −0.00 | −0.12, 0.11 | .96 |
| Anxiety Symptoms | .04 | −0.08, 0.16 | .47 | −0.04 | −0.17, 0.09 | .57 | – | – | – |
| Social Disruption | .23 | .10, 0.35 | < 0.001 | .17 | .04, 0.29 | .01 | .07 | −0.04, 0.19 | .19 |
| Remote Social Engagement | −0.10 | −0.22, 0.03 | .14 | −0.12 | −0.25, 0.01 | .08 | −0.10 | −0.20, 0.01 | .08 |
| In-Person Social Engagement | −0.05 | −0.20, 0.10 | .50 | −0.06 | −0.22, 0.10 | .46 | −0.18 | −0.31, −0.04 | .01 |
| Living with Significant Other | −0.69 | −0.99, −0.39 | < 0.001 | −0.14 | −0.50, 0.21 | .43 | −0.12 | −0.46, 0.23 | .51 |
| Social Distancing Adherence | −0.07 | −0.22, 0.08 | .38 | −0.13 | −0.29, 0.02 | .10 | −0.16 | −0.28, −0.03 | .01 |
| Age | −0.10 | −0.24, 0.03 | .13 | −0.00 | −0.16, 0.15 | .98 | −0.07 | −0.22, 0.09 | .40 |
| Gender | .39 | .07, 0.71 | .02 | −0.24 | −0.61, 0.13 | .21 | −0.48 | −0.84, −0.12 | .01 |
| Income | −0.06 | −0.18, 0.07 | .38 | −0.04 | −0.18, 0.11 | .63 | −0.18 | −0.32, −0.04 | .01 |
| Days since COVID Declaration | −0.10 | −0.23, 0.03 | .13 | −0.06 | −0.19, 0.07 | .37 | −0.14 | −0.24, −0.03 | .01 |
| Marginal R2/Conditional R2 | .31/0.63 | .05/0.67 | .12/0.80 | ||||||
In the time-lagged models predicting internalizing symptoms, only past-week social disruption significantly predicted depression symptoms, such that greater past-week social disruption was related to higher depression symptoms. In contrast, anxiety symptoms were significantly predicted by past-week in-person social engagement and past-week social distancing, such that greater adherence to social distancing and greater in-person social engagement were related to lower anxiety scores. As above, all results for key variables were substantively identical regardless of whether covariates were included or not. Further, as shown in Table S1, results of the cross-sectional (same week) mixed effect models were substantially similar to those of the time-lagged models, albeit not all of the significant cross-sectional effects remained significant in time-lagged analyses.
Discussion
The COVID-19 pandemic is an extraordinary global stressor that has produced unprecedented shifts in social behavior and prompted widespread concerns about loneliness and psychological adjustment. Here, we aimed to characterize links between internalizing symptoms, social behavior, and social functioning through the initial months of the pandemic in a transdiagnostic community sample of adults living in the United States. Our sample was clearly cognizant of and impacted by the COVID-19 pandemic, in that all participants reported awareness of social distancing guidelines and that a majority reported considerable adherence to those guidelines and moderate or greater distress regarding COVID-19.
In line with hypotheses, our results support a robust, but complex set of reciprocal associations between social engagement, social disruption, social distress, and internalizing symptoms. Consistent with prior research on the dissociability of objective and perceived social isolation, social distress, disruption, and engagement were highly distinct from each other and from self-reported adherence to social distancing guidelines. This finding underscores the need for specificity in the dimensions of social functioning that are measured, as it cannot be taken for granted, for example, that greater adherence to social distancing necessarily equates with greater loneliness.
Perhaps of more import, these social variables showed remarkably distinct links with internalizing symptoms. Neither anxiety nor depressive symptoms at baseline predicted how much time participants reported spending socializing with others, nor the degree of COVID-related social disruption endorsed. Despite this, participants who reported more severe depression symptoms before the pandemic tended to report greater social distress at follow-up relative to those who reported lower depression levels. That is, baseline depression symptoms predicted greater feelings of social dissatisfaction amid the pandemic, despite the lack of evidence that depression was tied to the amount of time spent with non-household members. Baseline anxiety symptoms, on the other hand, did not significantly predict any of our social variables. Consistent with these effects, the weekly data likewise suggested that past-week depression symptoms, but not past-week anxiety symptoms, predicted increases in next-week social distress. In line with recent findings reported by Okabe-Miyamoto et al. (2021), participants who were living with a significant other were less liable to experience high levels of social distress than those who were not.
The weekly data also allowed us to examine the extent to which our key social variables of distress, remote engagement, in-person engagement, and disruption predicted changes in anxiety and depression over time. In these time-lagged analyses, social disruption—and not social distress, remote social engagement, or in-person social engagement—uniquely predicted next-week depression symptoms. In contrast, lower past week in-person social engagement—but not remote social engagement, social distress, or social disruption—predicted higher next-week anxiety symptoms, whereas higher adherence to social distancing guidelines predicted lower next-week anxiety symptoms. This finding highlights the need for opportunities for in-person social engagement activities that conform to public health guidelines to facilitate coping with anxiety.
As with all studies, this investigation had important strengths and limitations. Notable strengths include: careful characterization of a transdiagnostic community sample, pre-pandemic baseline data, and collection of repeated measures data during the pandemic. Observed effects held when models were adjusted for an array of potential confounds, and results were substantively identical when confounds were not included in the model. Our sample size, however, was modest in terms of the number of participants and the number of timepoints. As well, we observed evidence of a small but significant attrition bias in that participants with lower baseline anxiety scores and more years of education were slightly more likely to have participated in our COVID follow-up. The mean difference in education between those who did vs. did not participate in the COVID follow-up was less than a year (0.69 yrs.). Additionally, participants reported elevated levels of anxious arousal (MFollow-up = 15.95, MBaseline-only = 17.52) relative to a large non-clinical reference sample (M = 11.9, Q1 = 10, Q3 = 13) but substantially below that of a clinical reference sample (M = 31.3, Q1 = 26, Q3 = 37; reference values from Schulte-van Maaren et al., 2012). These data were collected during a particular interval during the pandemic and in a single country; as such, these findings may not generalize to other periods of the pandemic or to those living in other geographic regions. We relied on participant self-report, including of adherence to social distancing guidelines and remote social engagement, which may be difficult to estimate accurately and without bias. Finally, given the potential for third variables to be operative, causality should not be inferred from these data notwithstanding our attempts to statistically adjust for potential confounds.
Considered collectively, these data suggest several important points. Depressive symptoms, but not anxious symptoms, predicted social adjustment during the pandemic. Increases in depressive and anxious symptoms were predicted by social variables, but the nature of the social variables differed. Depression symptoms were more closely tied to perceptions of social disconnection and disruption than to the more behavioral indices of social engagement or social distancing. In contrast, weekly anxiety symptoms were predicted by indices of social behavior, specifically past-week in-person social engagement and adherence to social distancing. Perhaps most critically, these data indicate that it is possible to follow social guidelines and even to spend relatively few hours socializing with close others, while still feeling connected and rewarded, in line with prior research on quantity versus quality (e.g., Ellis et al., 2020; Hawkley et al., 2008). At the same time, these data highlight the relative vulnerability of those who struggle with depression and anhedonia to distressing feelings of social disconnection amid the pandemic.
Author statement
BS contributed to study conceptualization and design, formulated the specific hypotheses, conducted core analyses, and wrote the first draft of the manuscript. SL and KT jointly developed and designed the overarching study, directed the project, and provided extensive feedback on all drafts of the manuscript. PP managed the data, conducted preliminary analyses, and wrote portions of the Method and Results sections. AD coordinated the study and wrote portions of the Method sections. BS, SL, KT, and PP were engaged in the interpretation of the data. All authors contributed to and approved the final manuscript.
Role of the funding source
Funding for this work was provided by NIMH 5R01MH110477–05 (PIs: Sheri L. Johnson and Kiara R. Timpano) and the University of California, Berkeley; however, these funding sources had no role in study design or execution, analysis or interpretation of the data, or the decision to submit these results.
Acknowledgements
The authors would like to thank Kiana Modavi, Jamie Port, Jennifer Pearlstein, Manon Ironside, and Devon Sandel for their contributions to the management and execution of the study, as well as all of the participants without whom this study would not have been possible.
Footnotes
Baseline data for four participants was collected after the WHO classified the COVID-19 outbreak as a pandemic on March 11, 2020.
References
- Bakdash J.Z., Marusich L.R. Repeated measures correlation. Front. Psychol. 2017;8:456. doi: 10.3389/fpsyg.2017.00456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartoń K. 2009. MuMIn: Multi-Model Inference. [Google Scholar]
- Bates D., Mächler M., Bolker B., Walker S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015;67(1):1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Cacioppo J.T., Cacioppo S. Social relationships and health: the toxic effects of perceived social isolation. Soc. Personal. Psychol. Compass. 2014;8(2):58–72. doi: 10.1111/spc3.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Hawkley L.C., Norman G.J., Berntson G.G. Social isolation. Ann. N. Y. Acad. Sci. 2011;1231(1):17. doi: 10.1111/j.1749-6632.2011.06028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creese B., Khan Z., Henley W., O'Dwyer S., Corbett A., Da Silva M.V., Ballard C. Loneliness, physical activity and mental health during COVID-19: a longitudinal analysis of depression and anxiety in adults over 50 between 2015 and 2020. Int. Psychogeriatric. 2020:1–21. doi: 10.1017/S1041610220004135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jong Gierveld J., Van Tilburg T.G., Dykstra P.A. In: The Cambridge Handbook of Personal Relationships. Vangelisti A.L., Perlman D., editors. Cambridge University Press; 2018. New ways of theorizing and conducting research in the field of loneliness and social isolation; pp. 391–404. [DOI] [Google Scholar]
- De Jong Gierveld J., Kamphuis F. The development of a Rasch-type loneliness scale. Appl. Psychol. Meas. 1985;9(3):289–299. doi: 10.1177/014662168500900307. [DOI] [Google Scholar]
- Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canad. J. Behav. Scie./Revue Canadienne des Sci. du Comport. 2020;52(3):177. doi: 10.1037/cbs0000215. [DOI] [Google Scholar]
- First M.B., Williams J.B.W., Karg R.S., Spitzer R.L. Structured Clinical Interview for DSM-5. American Psychiatric Association; Arlington, VA: 2015. [Google Scholar]
- Haber M.G., Cohen J.L., Lucas T., Baltes B.B. The relationship between self-reported received and perceived social support: a meta-analytic review. Am. J. Commun. Psychol. 2007;39(1):133–144. doi: 10.1007/s10464-007-9100-9. [DOI] [PubMed] [Google Scholar]
- Halekoh U., Højsgaard S. A Kenward-Roger approximation and parametric bootstrap methods for tests in linear mixed models–the R package pbkrtest. J. Stat. Softw. 2014;59(9):1–30. doi: 10.18637/jss.v059.i09. [DOI] [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Annal. Behav. Med. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L.C., Hughes M.E., Waite L.J., Masi C.M., Thisted R.A., Cacioppo J.T. From social structural factors to perceptions of relationship quality and loneliness: the Chicago health, aging, and social relations study. J. Gerontol. Ser. B. 2008;63(6):S375–S384. doi: 10.1093/geronb/63.6.S375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. https://doi.org/10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzman R., Brown T., Fuld P., Peck A., Schechter R., Schimmel H. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am. J. Psychiatry. 1983;140(6):734–739. doi: 10.1176/ajp.140.6.734. 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- Kenward M.G., Rogers J.H. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. doi: 10.2307/2533558. [DOI] [PubMed] [Google Scholar]
- Killgore W.D., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D., Cloonan S.A., Taylor E.C., Miller M.A., Dailey N.S. Three months of loneliness during the COVID-19 lockdown. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuznetsova A., Brockhoff P.B., Christensen R.H. lmerTest package: tests in linear mixed effects models. J. Stat. Softw. 2017;82(13):1–26. doi: 10.18637/jss.v082.i13. [DOI] [Google Scholar]
- Leon A.V., Olfson M., Portera L., Farber L., Sheehan D.V. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int. J. Psychiatry Med. 1997;27(2):93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- Li L.Z., Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marroquín B., Vine V., Morgan R. Mental health during the COVID-19 pandemic: effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters N.B., Shih S.F., Bukoff A., Akel K.B., Kobayashi L.C., Miller A.L., Wagner A.L. Social distancing in response to the novel coronavirus (COVID-19) in the United States. PLoS ONE. 2020;15(9) doi: 10.1371/journal.pone.0239025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa S., Schielzeth H. A general and simple method for obtaining R2 from generalized linear mixed-effects models. Method. Ecol. Evol. 2013;4:133–142. doi: 10.1111/j.2041-210x.2012.00261.x. [DOI] [Google Scholar]
- Okabe-Miyamoto K., Folk D., Lyubomirsky S., Dunn E.W. Changes in social connection during COVID-19 social distancing: it’s not (household) size that matters, it’s who you’re with. PLoS ONE. 2021;16(1) doi: 10.1371/journal.pone.0245009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okruszek Ł., Aniszewska-Stańczuk A., Piejka A., Wiśniewska M., Żurek K. Safe but lonely? Loneliness, anxiety, and depression symptoms and COVID-19. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.579181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y., Hoffman Y. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A Language and Environment for Statistical Computing.https://www.R-project.org/ [Google Scholar]
- Revelle W., Zinbarg R.E. Coefficients alpha, beta, omega, and the glb: comments on Sijtsma. Psychometrika. 2009;74(1):145–154. doi: 10.1007/s11336-008-9102-z. [DOI] [Google Scholar]
- Rico-Uribe L.A., Caballero F.F., Martín-María N., Cabello M., Ayuso-Mateos J.L., Miret M. Association of loneliness with all-cause mortality: a meta-analysis. PLoS ONE. 2018;13(1) doi: 10.1371/journal.pone.0190033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D., Peplau L.A., Cutrona C.E. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J. Pers. Soc. Psychol. 1980;39(3):472–480. doi: 10.1037/0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte-van Maaren Y.W.M., Carlier I.V.E., Zitman F.G., van Hemert A.M., de Waal M.W.M., van Noorden M.S., Giltay E.J. Reference values for generic instruments used in routine outcome monitoring: the leiden routine outcome monitoring study. BMC Psychiatry. 2012;12(1):203. doi: 10.1186/1471-244X-12-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.J., Lim M.H. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res. Pract. 2020;30(2) doi: 10.17061/phrp3022008. [DOI] [PubMed] [Google Scholar]
- Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nature Hum. Behav. 2020;4(5):460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Wardenaar K.J., van Veen T., Giltay E.J., de Beurs E., Penninx B.W., Zitman F.G. Development and validation of a 30-item short adaptation of the Mood and Anxiety Symptoms Questionnaire (MASQ) Psychiatry Res. 2010;179(1):101–106. doi: 10.1016/j.psychres.2009.03.005. [DOI] [PubMed] [Google Scholar]
- Williams J.B.W. In: Handbook of psychiatric measures. 2nd. Rush A.J., First M.B., Blacker D., editors. American Psychiatric Association; Washington, DC: 2008. Mental health status, functioning, and disabilities measures; pp. 83–105. [Google Scholar]