Highlights
-
•
Aspirin use among adults in the US has slightly declined over the last decade.
-
•
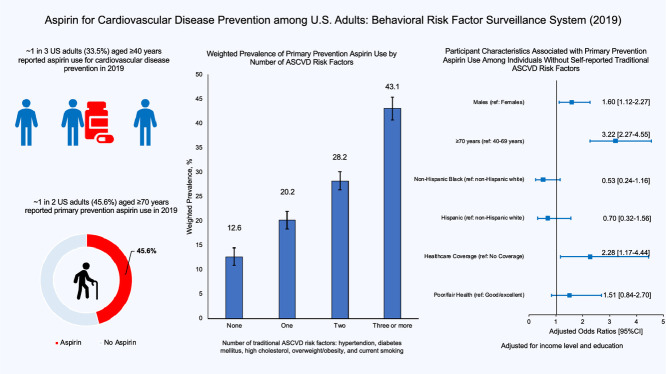
1 in 3 US adults aged ≥40 years reported aspirin use for ASCVD prevention in 2019.
-
•
Approximately 45.6% of adults ≥70 years reported primary prevention aspirin use in 2019.
-
•
Females were less likely than men to report secondary prevention aspirin use.
Keywords: Aspirin, Primary prevention, Secondary prevention, Trends
Abstract
Objective
: Aspirin has been widely utilized over several decades for atherosclerotic cardiovascular disease (ASCVD) prevention among adults in the United States. We examined trends in aspirin use among adults aged ≥40 years from 1998 to 2019 and assessed factors associated with its use for primary and secondary ASCVD prevention.
Methods
: Using 1998–2019 Behavioral Risk Factor Surveillance System data, we obtained weighted prevalence of aspirin use among adults aged ≥40 years for each year and examined trends in use over this period. Using multivariable logistic regression and utilizing data from 54,388 respondents aged ≥40 years in the 2019 data, we assessed factors associated with aspirin use for secondary prevention and for primary prevention stratified by the number of traditional ASCVD risk factors reported (hypertension, diabetes mellitus, high cholesterol, overweight/obesity, and cigarette smoking).
Results
: Aspirin use prevalence increased from 29.0%(95%CI, 27.9%-30.2%) in 1998 to 37.5%(36.9%-38.0%) in 2009. However, use has slightly declined over the last decade: 35.6%(34.6%-36.6%) in 2011 to 33.5%(32.5%-34.6%) in 2019. In 2019, among respondents without cardiovascular disease (CVD), 27.5%(26.4%-28.6%) reported primary prevention aspirin use while 69.7%(67.0%-72.2%) of respondents with CVD reported secondary prevention aspirin use. Of concern, 45.6%(43.5%-47.7%) of adults aged ≥70 years without CVD reported primary prevention aspirin use. Additionally, among individuals without any self-reported traditional ASCVD risk factor, males (adjusted odds ratio(aOR):1.60, 95%CI:1.12–2.27), persons aged ≥70 years (aOR:3.22, 95%CI:2.27–4.55), and individuals with healthcare coverage (aOR:2.28, 95%CI:1.17–4.44) had higher odds of primary prevention aspirin use compared to females, persons aged 40–69 years, and individuals without healthcare coverage, respectively. Females were less likely than males to report secondary prevention aspirin use (aOR:0.64, 95%CI:0.50–0.82).
Conclusion
: Aspirin use has slightly declined over the last decade. A significant proportion of adults aged ≥70 years reported primary prevention aspirin use in 2019. Since current guidelines do not recommend primary prevention aspirin use among adults aged ≥70 years, such use should be discouraged.
Graphical abstract
Cardiovascular diseases (CVD), including coronary artery disease (CAD) and stroke, remain the leading cause of death in the United States (US), accounting for approximately 870,000 deaths in 2018 [1]. CVD prevention strategies over the years have included antiplatelet therapy and effective management of atherosclerotic cardiovascular disease (ASCVD) risk factors such as hypertension, diabetes mellitus, and cigarette smoking. Due to its antithrombotic properties, aspirin, a low-cost antiplatelet medication that is over-the-counter in the US, has been used to reduce the incidence of cardiovascular events among individuals with a high ASCVD risk factor burden (primary prevention) and to reduce recurrent events and mortality among individuals with preexisting CVD (secondary prevention) [2].
While evidence for its role in secondary prevention has remained robust [3], [4], [5], [6], aspirin use for primary prevention, though supported by earlier trials and recommended in past guidelines, is now discouraged, particularly among low- and intermediate-risk persons as well as adults aged >70 years [7], [8], [9], [10], [11]. Recent trials such as the Aspirin to Reduce Risk of Initial Vascular Events (ARRIVE) and the Aspirin in Reducing Events in the Elderly (ASPREE), with low CVD risk trial populations (incidence of thrombotic events in placebo group <1% per year), failed to show significant benefits of primary prevention aspirin use, particularly when used in addition to other evidence-based primary prevention therapies such as lipid-lowering medications [12,13]. Indeed, in these recent trials, not only was there a lack of benefit with primary prevention aspirin use in reducing major adverse cardiovascular events, but there was also a significant increase in bleeding risk [12,13]. The American College of Cardiology and the American Heart Association (ACC/AHA) 2019 Primary Prevention of Cardiovascular Disease Guideline, therefore, does not recommend the routine use of aspirin for primary prevention, particularly among low- and intermediate-risk individuals, persons at increased risk of bleeding, and individuals >70 years since such use may result in net harm [14].
Despite the widespread use of aspirin for atherosclerotic cardiovascular disease (ASCVD) prevention in the US, few studies have examined in detail trends in use over the last 2 decades. Additionally, with the current AHA/ACC primary prevention guidelines, it is crucial to assess aspirin use patterns to inform intervention needed to incorporate new recommendations into clinical practice. We, therefore, aimed to 1) examine trends in aspirin use over the last 2 decades, 2) present updated prevalence estimates of aspirin use for primary and secondary prevention, and 3) assess the factors associated with aspirin use for primary and secondary prevention.
1. Methods
1.1. Study design, data sources, and study sample
We analyzed data from 1998 to 2019 Behavioral Risk Factor Surveillance (BRFSS) to obtain yearly prevalence estimates of aspirin use among adults aged ≥40 years and to examine trends in usage over this period. Using the 2019 data, we examined the associations between participant characteristics and aspirin use for primary and secondary prevention. The BRFSS is a health-related nationally representative telephone survey of non-institutionalized adults conducted by all 50 states, the District of Columbia, and participating US territories, with assistance from the Centers for Disease Control and Prevention [15]. In 2011, the BRFSS weighting methodology was changed from simple post-stratification to iterative proportional fitting to improve sample representativeness [16]. While this limits the direct comparison of 2011 estimates to previous years, the shape of trend lines is unlikely to be affected [16].
The cardiovascular module containing questions on aspirin in the BRFSS is optional, giving states the flexibility to include this module in their state survey. Therefore, the number of states providing data on aspirin use varied from year to year and is presented in Supplementary Table 1, together with the analytic sample size for each year. In 2019, 8 states (Alaska, Florida, Iowa, Maine, Minnesota, Mississippi, Nebraska, and Texas) provided data on aspirin use. The median survey response rate for all states, territories, and Washington, DC, in 2019 was 49.4 and ranged from 37.3 to 73.1. Response rates for states and territories included in this analysis had a median of 52.5 and ranged from 44.3 to 60.1 [15].
Our study was exempted from review by an institutional review board since it uses de-identified publicly available BRFSS data. We followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines in reporting our findings [17].
1.2. Aspirin use
Aspirin use was previously assessed with the question, “Do you take aspirin daily or every other day?” We classified participants who responded in the affirmative as aspirin users. In 2019, aspirin use was specified for the prevention of CVD with the question, “How often do you take aspirin to prevent or control heart disease, heart attacks, or stroke?” We classified participants who responded “daily” or “some days” as aspirin users. Participants who answered “used to take it but had to stop due to side effects” or “do not take it” were classified as non-users. We regarded aspirin users who reported ever being diagnosed with stroke, myocardial infarction, or coronary heart disease as taking aspirin for secondary prevention and those who did not report any of these as taking it for primary prevention [18].
1.3. Covariate assessment
Sex (male, female), age (40–69, ≥70 years), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Other), healthcare coverage (yes, no), and education (less than high school, high school/some college, college graduate) were self-reported. Participants who had any form of healthcare coverage, including health insurance, prepaid plans, or government plans such as Medicare, were classified as having healthcare coverage. Annual family income was adjusted using federal poverty guidelines for each state and categorized as: below, within 100–200%, or >200% of the federal poverty line [19].
Health indicators such as self-reported general health status (poor/fair, good/excellent) and BMI (kg/m2), calculated from self-reported weight and height (non-overweight/obese, overweight/obese), were included in our analyses. Traditional ASCVD risk factors including combustible cigarette smoking (never, former, or current), diabetes mellitus(yes, no), hypertension(yes, no), and high cholesterol(yes, no) were also self-reported. We assigned each participant a score of 0 to 5 based on the number of traditional ASCVD risk factors reported (hypertension, diabetes mellitus, high cholesterol, overweight/obesity, and current combustible cigarette use) [20].
1.4. Statistical analysis
To examine the trends in the prevalence of aspirin use for ASCVD prevention from 1998 to 2019, we calculated the weighted prevalence estimate of aspirin use for each year, first overall, and then stratified by the purpose of use (primary or secondary ASCVD prevention). We tested trends in the prevalence of aspirin use across years using linear regression with survey year as a continuous variable. Due to changes in the BRFSS weighting methodology in 2011, we examined temporal trends in aspirin use pre-and post-2011.
For 2019, in addition to the purpose of use, aspirin use prevalence was stratified by key participant characteristics. Using multivariable logistic regression models with complete case analyses and utilizing data from 2019, we examined the factors associated with aspirin use for primary prevention among groups stratified by self-reported traditional ASCVD risk factor burden (absence of self-reported conventional ASCVD risk factors and presence of ≥3 self-reported conventional ASCVD risk factors) and for secondary prevention.
The survey command “svy” was used in all analyses to account for the complex weighting methodology used by the BRFSS. We performed all analyses in 2020 with Stata version 16 (StataCorp, College Station, TX) and used a 2-sided alpha(α) level of <0.05 to determine the statistical significance.
2. Results
Trends in Aspirin Use Pre- and Post-2011:
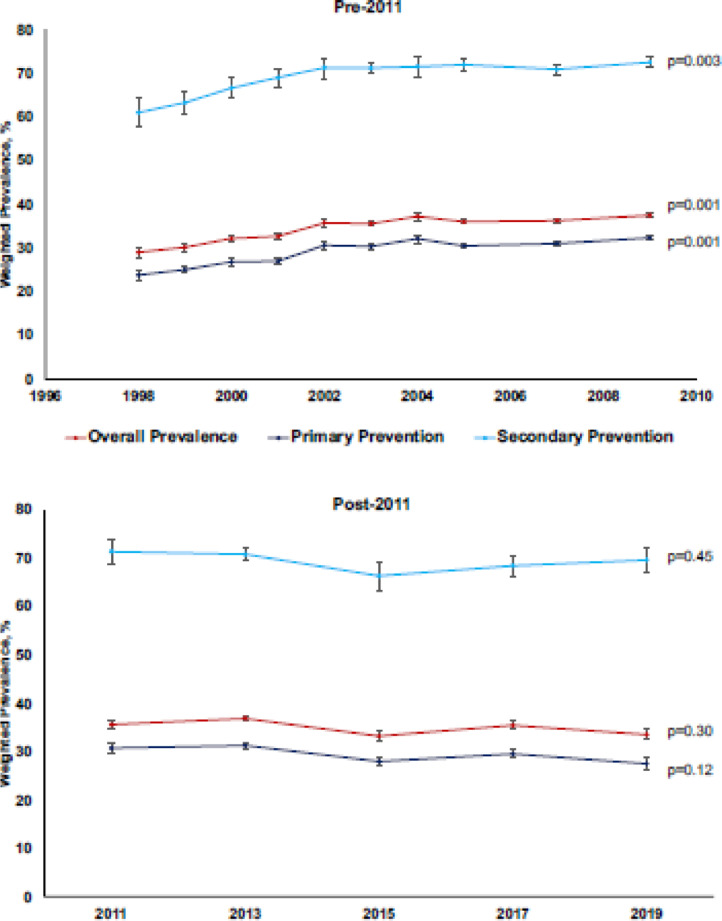
Fig. 1 shows the trends in aspirin use for ASCVD prevention among adults ≥40 years from 1998 to 2019. Between 1998 and 2009, the overall prevalence of aspirin use increased from 29.0% (27.9%−30.2%) to 37.5% (36.9%−38.0%; p-value 0.001). This observed increase was seen for both primary (23.8% to 32.3%; p-value 0.001) and secondary prevention aspirin use (61.0% to 72.5%; p-value 0.003). However, between 2011 and 2019, the overall prevalence of aspirin use declined from 35.6% (34.6%−36.6%) to 33.5% (32.5%−34.6%) although this was not statistically significant (p-value 0.30). Similarly, declines in primary (30.7% to 27.5%; p-value 0.12) and secondary (71.4% to 69.7%; p-value 0.45) prevention aspirin use over this period were not significant.
Fig. 1.
Trends in aspirin use among adults ≥40 years in the united states, behavioral risk factor surveillance system (1998–2019).
2.1. Characteristics of study participants (BRFSS 2019)
Of the 54,388 participants aged ≥40 years who responded to questions on aspirin use in 2019, the majority were aged 40–69 years (73.9%), female (53.1%), non-Hispanic White (64.8%), had income >200% of the federal poverty level (66.7%), and healthcare coverage (87.9%). The majority reported good/excellent health (75.6%), with no diabetes (82.1%), no hypertension (52.8%), no high cholesterol (56.7%), no history of combustible cigarette smoking (55.3%), or no CVD (86.1%). About 73.1% of respondents had BMI in the overweight/obese range (Table 1).
Table 1.
Characteristics of study participants stratified by aspirin use, behavioral risk factor surveillance system (2019)*.
| Characteristics | Overall Unweighted n = 54,388 (Weighted%) | Aspirin Use Unweighted n = 20,115 (Weighted%) | No Aspirin Use Unweighted n = 34,273 (Weighted%) |
|---|---|---|---|
| Sex | |||
| Male | 23,659 (46.9) | 9751 (51.8) | 13,908 (44.4) |
| Female | 30,729 (53.1) | 10,364 (48.2) | 20,365 (55.6) |
| Age, years | |||
| 40–69 | 35,144 (73.9) | 10,247 (59.5) | 24,897 (81.1) |
| ≥70 | 19,244 (26.1) | 9868 (40.5) | 9376 (18.9) |
| Race/Ethnicity | |||
| Non-Hispanic White | 44,819 (64.8) | 16,613 (67.5) | 28,206 (63.4) |
| Non-Hispanic Black | 3327 (10.8) | 1497 (14.0) | 1830 (9.3) |
| Hispanic | 3197 (19.8) | 919 (14.8) | 2278 (22.3) |
| Other | 2074 (4.6) | 703 (3.7) | 1371 (5.0) |
| Education | |||
| Less than high school | 4014 (15.3) | 1735 (17.2) | 2279 (14.5) |
| High school/Some college | 30,807 (57.6) | 12,233 (60.0) | 18,574 (56.3) |
| College graduate | 19,435 (27.1) | 6103 (22.8) | 13,332 (29.2) |
| Income, poverty line | |||
| Below | 4024 (11.9) | 1576 (12.1) | 2448 (11.8) |
| Within 100–200% | 12,121 (21.4) | 5070 (24.7) | 7051 (19.8) |
| >200% | 38,071 (66.7) | 13,422 (63.2) | 24,649 (68.4) |
| Healthcare coverage | |||
| No | 3862 (12.1) | 1006 (8.4) | 2856 (13.9) |
| Yes | 50,377 (87.9) | 19,057 (91.6) | 31,320 (86.1) |
| General Health Status | |||
| Poor/fair | 12,086 (24.4) | 5735 (32.0) | 6351 (20.6) |
| Good/excellent | 42,173 (75.6) | 14,322 (68.0) | 27,851 (79.4) |
| Combustible Cigarette Smoking | |||
| Never | 29,091 (55.3) | 9854 (49.4) | 19,237 (58.3) |
| Former | 17,519 (30.0) | 7419 (36.5) | 10,100 (26.7) |
| Current | 7394 (14.7) | 2694 (13.1) | 4700 (15.0) |
| Diabetes | |||
| No | 44,718 (82.1) | 14,347 (70.3) | 30,371 (88.1) |
| Yes | 9571 (17.9) | 5730 (29.7) | 3841 (11.9) |
| Hypertension | |||
| No | 27,221 (52.8) | 6779 (34.9) | 20,432 (61.8) |
| Yes | 26,995 (47.2) | 13,264 (65.1) | 13,731 (38.2) |
| High cholesterol | |||
| No | 29,219 (56.7) | 8620 (43.9) | 20,599 (63.4) |
| Yes | 22,975 (43.3) | 10,961 (56.1) | 12,014 (36.6) |
| Overweight/Obesity | |||
| No | 14,795 (26.9) | 4666 (23.0) | 10,129 (28.8) |
| Yes | 36,644 (73.1) | 14,483 (77.0) | 22,161 (71.2) |
| CVD | |||
| No | 45,323 (86.1) | 13,936 (71.0) | 31,387 (93.7) |
| Yes | 8422 (13.9) | 5839 (29.0) | 2583 (6.3) |
The numbers represent actual number of participants. All percentages are weighted to reflect the final survey weights
CVD: Cardiovascular disease
p < 0.001 for all variables comparing aspirin users and non-users.
Compared to individuals who did not use aspirin, those who used aspirin were more likely to be males (51.8% vs 44.4%), older (age ≥70 years: 40.5% vs 18.9%), overweight/obese (77.0% vs 71.2%), and former smokers (36.5% vs 26.7%). Those who used aspirin were also more likely to report poor/fair health (32.0% vs 20.6%), diabetes (29.7% vs 11.9%), hypertension (65.1% vs 38.2%), and high cholesterol (56.1% vs 36.6%) (Table 1).
2.2. Weighted prevalence of aspirin use by participant characteristics (BRFSS 2019)
In 2019, the weighted prevalence of aspirin use for ASCVD prevention among adults ≥40 years was 33.5% (32.5−34.6%). Among respondents without CVD, 27.5% (26.4−28.6%) reported primary prevention aspirin use, while 69.7% (67.0−72.2%) of those with preexisting CVD reported aspirin use for secondary prevention (Table 2). For respondents with preexisting CVD who did not report secondary prevention aspirin use, 15.2% cited “used to take but stopped due to side effects” as the reason for aspirin nonuse.
Table 2.
Weighted Prevalence of Aspirin Use Stratified by Participant Characteristics, Behavioral Risk Factor Surveillance System (2019).
| Characteristics | Overall Unweighted n = 54,388 | No CVD (Primary Prevention) Unweighted n = 45,323 |
CVD (Secondary Prevention) Unweighted n = 8422 |
||
|---|---|---|---|---|---|
| % [95%CI] | % [95%CI] | p-value* | % [95%CI] | p-value* | |
| Overall | 33.5 (32.5–34.6) | 27.5 (26.4–28.6) | 69.7 (67.0–72.2) | ||
| Sex | <0.001 | <0.001 | |||
| Male | 37.0 (35.4–38.7) | 30.0 (28.3–31.7) | 73.9 (70.5–77.0) | ||
| Female | 30.4 (29.1–31.8) | 25.4 (24.1–26.8) | 64.9 (60.8–68.7) | ||
| Age, years | <0.001 | 0.19 | |||
| 40–69 | 27.0 (25.8–28.2) | 22.1 (21.0–23.4) | 68.1 (64.0–72.0) | ||
| ≥70 | 52.0 (50.2–53.8) | 45.6 (43.5–47.7) | 71.4 (68.4–74.3) | ||
| Race/Ethnicity | <0.001 | 0.57 | |||
| Non-Hispanic White | 35.0 (33.9–36.0) | 28.8 (27.7–29.8) | 70.2 (67.7–72.7) | ||
| Non-Hispanic Black | 43.3 (39.2–47.4) | 37.0 (32.7–41.6) | 73.8 (64.8–81.2) | ||
| Hispanic | 25.1 (22.0–28.4) | 20.0 (17.1–23.2) | 65.1 (54.2–74.7) | ||
| Other | 27.5 (22.7–32.9) | 22.7 (17.7–28.5) | 67.5 (57.9–75.8) | ||
| Income, poverty line | <0.001 | 0.23 | |||
| Below | 34.1 (30.2–38.1) | 25.5 (21.9–29.6) | 68.1 (59.9–75.2) | ||
| Within 100–200% | 38.7 (36.3–41.1) | 31.9 (29.3–34.7) | 67.0 (61.6–72.0) | ||
| >200% | 31.8 (30.7–33.0) | 26.5 (25.4–27.7) | 71.8 (68.7–74.7) | ||
| Healthcare coverage | <0.001 | 0.08 | |||
| No | 23.4 (20.3–26.8) | 19.1 (16.1–22.6) | 60.6 (48.7–71.3) | ||
| Yes | 35.0 (33.9–36.1) | 28.7 (27.6–29.9) | 70.5 (67.9–73.1) | ||
| General health status | <0.001 | 0.78 | |||
| Poor/fair | 43.8 (41.3–46.2) | 33.5 (30.8–36.3) | 69.9 (65.9–73.5) | ||
| Good/excellent | 30.1 (29.0–31.2) | 26.0 (24.9–27.1) | 69.1 (65.5–72.5) | ||
| Education | <0.001 | 0.39 | |||
| Less than high school | 37.5 (33.8–41.4) | 31.2 (27.3–35.5) | 65.5 (57.8–72.4) | ||
| High school/Some college | 35.0 (33.7–36.3) | 28.4 (27.1–29.8) | 70.8 (67.5–73.9) | ||
| College graduate | 28.2 (26.7–29.8) | 23.9 (22.3–25.4) | 70.4 (66.1–74.4) | ||
| Combustible Cigarette Smoking | <0.001 | 0.15 | |||
| Never | 30.0 (28.6–31.4) | 25.7 (24.3–27.1) | 67.9 (63.7–71.8) | ||
| Former | 40.8 (38.9–42.6) | 33.1 (31.2–35.2) | 72.5 (68.8–76.0) | ||
| Current | 32.1 (29.4–34.8) | 23.6 (21.2–26.2) | 66.7 (59.2–73.4) | ||
| Diabetes | <0.001 | 0.003 | |||
| No | 28.7 (27.7–29.8) | 23.7 (22.7–24.9) | 66.9 (63.6–70.1) | ||
| Yes | 55.7 (53.0–58.4) | 48.7 (45.5–51.9) | 74.8 (70.7–78.5) | ||
| Hypertension | <0.001 | 0.033 | |||
| No | 22.2 (20.9–23.5) | 19.0 (17.8–20.3) | 64.4 (58.2–70.2) | ||
| Yes | 46.2 (44.6–47.8) | 38.9 (37.1–40.7) | 71.4 (68.6–74.1) | ||
| High cholesterol | <0.001 | 0.001 | |||
| No | 26.5 (25.2–27.8) | 22.8 (21.6–24.1) | 63.8 (59.2–68.1) | ||
| Yes | 44.4 (42.7–46.1) | 36.4 (34.5–38.4) | 72.6 (69.3–75.7) | ||
| Overweight/Obesity | <0.001 | 0.014 | |||
| No | 29.0 (27.1–30.9) | 23.5 (21.6–25.5) | 63.7 (57.6–69.3) | ||
| Yes | 35.6 (34.3–36.9) | 29.3 (28.0–30.7) | 71.5 (68.6–74.3) | ||
| Number of traditional ASCVD risk factors † | <0.001 | <0.001 | |||
| 0 | 14.7 (12.9–16.8) | 12.6 (10.9–14.5) | 53.9 (40.8–66.4) | ||
| 1 | 22.6 (20.8–24.4 | 20.2 (18.4–22.0) | 58.7 (49.6–67.1) | ||
| 2 | 33.7 (31.9–35.6) | 28.2 (26.4–30.1) | 69.5 (64.7–73.8) | ||
| ≥ 3 | 50.9 (48.8–52.9) | 43.1 (40.7–45.4) | 73.2 (69.9–76.3) | ||
p-values for bivariate analyses.
ASCVD Risk Factors: hypertension, diabetes, high cholesterol, overweight/obesity, and current combustible cigarette smoking
ASCVD: atherosclerotic cardiovascular disease.
Primary prevention aspirin use was relatively more prevalent among males, persons who reported poor/fair health, individuals who were overweight/obese, and those with diabetes, hypertension, or high cholesterol, compared to their respective comparison groups. It was also more prevalent among adults ≥70 years, with 45.6% reporting aspirin use for primary prevention. Additionally, the prevalence of aspirin use for primary prevention increased with increasing ASCVD risk factor burden, with 12.6% (10.9%−14.5%) of persons with none of the five traditional ASCVD risk factors reporting primary prevention aspirin use (Table 2). Aspirin use for secondary prevention was similarly more prevalent among males, overweight/obese persons, and individuals with diabetes, hypertension, or high cholesterol (Table 2).
The prevalence estimates of primary and secondary prevention aspirin use by sex, age, and race/ethnicity are reported in supplementary Table 2. Among males aged 40–69 years, Hispanic individuals had a lower prevalence of aspirin use overall and for primary prevention than non-Hispanic White and non-Hispanic Black persons (Supplementary Table 2).
2.3. Factors associated with primary and secondary prevention aspirin use
Statistically significant determinants of primary prevention aspirin use among individuals with no self-reported traditional ASCVD risk factor were sex, age, and healthcare coverage (Table 3). Among individuals who did not report any of the five conventional ASCVD risk factors, males had higher odds of primary prevention aspirin use compared to females (aOR; 1.60, 95%CI; 1.12–2.27), and adults ≥70 years had higher odds compared to those aged 40–69 years (aOR; 3.22, 95%CI; 2.27–4.55). Similarly, individuals who had healthcare coverage had higher odds of primary prevention aspirin use than those without (aOR; 2.28, 95%CI; 1.17–4.44) (Table 3).
Table 3.
Factors Associated with Secondary and Primary Prevention Aspirin Use Stratified by Number of Traditional ASCVD Risk Factors, Behavioral Risk Factor Surveillance System (2019).
| Characteristics | No CVD Primary Prevention |
CVD Secondary Prevention |
||||
|---|---|---|---|---|---|---|
| Absence of self-reported ASCVD risk factors |
Presence of ≥3 self-reported ASCVD risk factors |
|||||
| aOR [95% CI] | p-value* | aOR [95% CI] | p-value* | aOR [95% CI] | p-value† | |
| Sex | ||||||
| Female | Ref | Ref | Ref | |||
| Male | 1.60 [1.12–2.27] | 0.009 | 1.12 [0.91–1.37] | 0.28 | 1.56 [1.23–1.99] | <0.001 |
| Age, years | ||||||
| 40–69 | Ref | Ref | Ref | |||
| ≥70 | 3.22 [2.27–4.55] | <0.001 | 1.88 [1.53–2.30] | <0.001 | 1.17 [0.93–1.48] | 0.19 |
| Race/ethnicity | ||||||
| Non-Hispanic White | Ref | Ref | Ref | |||
| Non-Hispanic Black | 0.53 [0.24–1.16] | 0.11 | 1.44 [1.03–2.02] | 0.035 | 1.22 [0.77–1.94] | 0.40 |
| Hispanic | 0.70 [0.32–1.56] | 0.38 | 0.64 [0.44–0.92] | 0.017 | 0.96 [0.60–1.53] | 0.86 |
| Other | 0.49 [0.20–1.24] | 0.13 | 0.91 [0.56–1.48] | 0.70 | 0.93 [0.58–1.48] | 0.76 |
| Income, poverty line | ||||||
| Below | Ref | Ref | Ref | |||
| Within 100–200% | 1.44 [0.50–4.16] | 0.50 | 1.13 [0.73–1.73] | 0.58 | 0.88 [0.57–1.36] | 0.56 |
| >200% | 1.13 [0.47–2.71] | 0.78 | 0.93 [0.63–1.36] | 0.69 | 1.11 [0.73–1.69] | 0.63 |
| Healthcare coverage | ||||||
| No | Ref | Ref | Ref | |||
| Yes | 2.28 [1.17–4.44] | 0.015 | 1.14 [0.73–1.77] | 0.58 | 1.34 [0.82–2.19] | 0.24 |
| Education | ||||||
| Less than high school | Ref | Ref | Ref | |||
| High school/Some college | 0.92 [0.39–2.18] | 0.85 | 0.83 [0.58–1.20] | 0.33 | 1.25 [0.86–1.82] | 0.24 |
| College graduate | 0.85 [0.34–2.13] | 0.73 | 0.88 [0.61–1.29] | 0.52 | 1.24 [0.82–1.89] | 0.31 |
| General health status | ||||||
| Good/excellent | Ref | Ref | Ref | |||
| Poor/fair | 1.51 [0.84–2.70] | 0.17 | 1.09 [0.88–1.36] | 0.42 | 1.08 [0.83–1.40] | 0.56 |
| ASCVD Risk Factors | ||||||
| 0 | – | – | Ref | |||
| 1 | 1.19 [0.64–2.19] | 0.58 | ||||
| 2 | 2.03 [1.13–3.65] | 0.017 | ||||
| ≥3 | 2.33 [1.33–4.10] | 0.003 | ||||
ASCVD Risk Factors: hypertension, diabetes, high cholesterol, overweight/obesity, and current combustible cigarette smoking.
ASCVD: atherosclerotic cardiovascular disease.
aOR: adjusted odds ratio.
CI: confidence interval.
CVD: cardiovascular disease.
Adjusted for age, sex, race, income, healthcare coverage, education, and self-reported health status.
Additionally adjusted for the number of ASCVD risk factors.
Among individuals who reported ≥3 of the traditional ASCVD risk factors, Hispanic individuals were less likely to report primary prevention aspirin use than non-Hispanic White persons (aOR; 0.64, 95%CI; 0.44–0.92) (Table 3). Sex and the number of traditional ASCVD risk factors were significantly associated with aspirin use for secondary prevention. Females were less likely to report aspirin use for secondary prevention than males (aOR; 0.64, 95%CI; 0.50–0.82) (Table 3).
3. Discussion
We found that while there was an upward trend in aspirin use before 2011, usage has slightly declined over the last decade, albeit not significant. In 2019, approximately 1 in 3 adults aged ≥40 years reported aspirin use for ASCVD prevention. Of concern, we found that a substantial proportion of adults aged ≥70 years reported regular aspirin use for primary prevention. Among individuals without any self-reported conventional ASCVD risk factor, males, adults ≥70 years, and individuals with healthcare coverage were more likely to report primary prevention aspirin use. In contrast, Hispanic individuals were less likely to report primary prevention aspirin use despite high ASCVD risk factor burden. Additionally, females were less likely than males to report aspirin use for secondary prevention.
Earlier studies describing trends in aspirin use among different population cohorts reported increasing aspirin use prevalence before 2011, similar to our findings [20], [21], [22], [23]. However, this upward trend has not been observed over the last decade, with most studies, like ours, reporting a slight decline in use, consistent with changing guidelines [24,25]. Until 2019, most professional medical societies recommended the routine use of low-dose aspirin for primary prevention [9,10,26,27]. However, following the publication in 2018 of 3 pivotal primary prevention aspirin trials which showed that primary prevention aspirin use had little or no benefit in preventing incident cardiovascular events while demonstrating a significant increase in bleeding risk, the ACC/AHA 2019 Primary Prevention Guideline does not recommend routine use of aspirin for primary prevention particularly among older adults, low- or intermediate-risk persons, and individuals at increased risk of bleeding [[12], [13], [14],28].
In 2019, approximately 1 in 4 US adults aged ≥40 years without stroke, myocardial infarction, or coronary heart disease reported primary prevention aspirin use. Of concern, almost half of adults aged ≥70 years without preexisting CVD reported primary prevention aspirin use, similar to reports from the National Health Interview Survey (NHIS) and National Health and Nutrition Examination Survey [24,29,30]. Given that the 2019 ACC/AHA guidelines explicitly advise against aspirin use for primary prevention among adults aged ≥70 years, such use should be discontinued and discouraged. Persons aged ≥70 years are at an increased risk of bleeding and hence may have a less favorable benefit-risk ratio with primary prevention aspirin use [14]. Additionally, 12.6% of respondents in our study with none of the traditional ASCVD risk factors reported aspirin use for primary prevention. This is similar to findings from the 2012–2015 NHIS, which showed that a significant proportion of adults with no modifiable ASCVD risk factor reported aspirin use for primary prevention [25]. Furthermore, we found that such inappropriate use of aspirin was more likely among males, persons ≥70 years, and individuals with healthcare coverage. In agreement with these findings, another study found male sex and old age to be associated with aspirin overutilization for primary prevention among low-risk populations [31]. The discordance between current guideline recommendations and these findings could be that the guidelines did not have much time to influence aspirin use behavior in participants who responded to survey questions in 2019. As such, more contemporary studies are needed to examine the effects of the 2019 AHA/ACC primary prevention guidelines on aspirin use patterns.
Unlike aspirin use for primary prevention, its routine use for secondary prevention is widely recommended due to its demonstrated benefits in reducing vascular mortality [32], [33], [34]. Approximately 69.7% of respondents with preexisting CVD in our study reported secondary prevention aspirin use, with 15.2% of the remaining eligible respondents citing side effects as the reason for aspirin nonuse. Aspirin use for secondary prevention in our study should be cautiously interpreted. The reasons for aspirin nonuse among the remaining eligible respondents could be related to under-prescription or non-adherence. It could also be due to the usage of other non-aspirin antiplatelet medications such as clopidogrel or contraindication in persons at increased bleeding risk, particularly those taking anticoagulation therapy for other indications. Also, the BRFSS does not account for persons with hemorrhagic stroke, in whom secondary prevention aspirin use may be inappropriate.
Sex differences in aspirin use for secondary prevention have also been reported in other studies [23,[35], [36], [37]]. The reasons that may account for the lower observed use of secondary prevention aspirin use among women than men include under-prescription, poor long-term -compliance, and preference of other non-aspirin antiplatelet medications among women [38]. Under-prescription of evidence-based secondary prevention therapies such as aspirin among women may be because women are more likely than men to have nonobstructive CAD [39]. Evidence suggests that persons with nonobstructive CAD are less likely to receive secondary prevention therapies such as aspirin at hospital discharge than those with obstructive CAD [40]. These, coupled with the documented sex disparities in the in-hospital management of acute cardiovascular events, may contribute to poorer outcomes observed among women following myocardial infarction and stroke [41], [42], [43], [44].
Observations in our current study may have important implications for healthcare providers. First, given the current ACC/AHA primary prevention guideline recommendations, clinicians should discontinue and discourage primary prevention aspirin use among adults aged ≥70 years due to the potential for net harm in this population. Also, healthcare providers should be selective in recommending aspirin for primary prevention and should assess risks and benefits on a case-by-case basis. Additionally, since aspirin is over-the-counter and a significant proportion of people take aspirin without physician advice [29], clinicians should inquire about aspirin use and discuss benefits and risks with patients. Lastly, factors contributing to the sex differences in secondary prevention aspirin use need to be explored.
3.1. Strengths and limitations
A unique strength of our study is the use of the BRFSS, which unlike clinical registries such as the PINNACLE [45], is nationally representative of the general population and not restricted to outpatients. However, our study had some limitations. First, the information used, including past medical history, was self-reported and could have resulted in recall bias and misclassification. ASCVD risk factors may be underdiagnosed in study participants who do not patronize healthcare services and underreported by those with low health literacy. Secondly, before 2019, questions on aspirin use were not specified for ASCVD prevention. Therefore, some respondents reporting aspirin use may have taken it for pain relief, potentially overestimate the prevalence estimates of aspirin use for ASCVD prevention, particularly primary prevention. However, we found that in most years in which further questions were asked to ascertain the purpose of use (e.g., 1998, 1999, 2000, etc.), respondents reporting aspirin use for only pain relief were in the minority.
Also, important information was unavailable regarding other conditions for which aspirin may be indicated, such as peripheral artery disease, revascularization, and high coronary artery calcium. Additionally, information on aspirin dose and whether aspirin was prescribed by a healthcare provider or obtained over the counter was lacking. Finally, not all states provided data on aspirin use for each year under consideration, and in 2019, only eight states provided data on aspirin use, limiting the generalizability of our results.
4. Conclusion
Despite the slight declines in use over the last decade, aspirin is still widely utilized for ASCVD prevention among US adults. A significant proportion of older adults aged ≥70 years reported using aspirin for primary ASCVD prevention. Given that such use may result in net harm, clinicians should endeavor to discuss the risks of primary prevention aspirin use among older adults and discontinue where appropriate. Also, future studies are needed to assess the impact of the 2019 AHA/ACC primary prevention guidelines on aspirin prescription and use patterns.
Funding
None.
CRediT authorship contribution statement
Ellen Boakye: Conceptualization, Methodology, Formal analysis, Writing – original draft. S.M. Iftekhar Uddin: Methodology, Formal analysis, Writing – review & editing. Olufunmilayo H. Obisesan: Methodology, Formal analysis, Writing – review & editing. Albert D. Osei: Visualization, Formal analysis, Writing – review & editing. Omar Dzaye: Writing – review & editing, Visualization. Garima Sharma: Writing – review & editing, Visualization. John William McEvoy: Writing – review & editing, Visualization. Roger Blumenthal: Writing – review & editing, Visualization. Michael J. Blaha: Conceptualization, Visualization, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2021.100256.
Appendix. Supplementary materials
References
- 1.Virani S.S., Alonso A., Aparicio H.J. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021;143:254–743. doi: 10.1161/cir.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 2.Montinari M.R., Minelli S., De Caterina R. The first 3500 years of aspirin history from its roots – a concise summary. Vascul Pharmacol. 2019;113:1–8. doi: 10.1016/j.vph.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Elwood P.C., Sweetnam P.M. Aspirin and secondary mortality after myocardial infarction. Lancet. 1979;314(8156–8157):1313–1315. doi: 10.1016/S0140-6736(79)92808-3. [DOI] [PubMed] [Google Scholar]
- 4.Altman R., Carreras L., Diaz R. Collaborative overview of randomised trials of antiplatelet therapy - I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Br Med J. 1994;308(6921):81–106. [PMC free article] [PubMed] [Google Scholar]
- 5.Edney P., Jackson P., Burrell B. Antiplatelet treatment reduces the risk of non-fatal vascular events and, to a lesser extent, vascular death. Br Med J. 1988;296(6618):320–331. doi: 10.1136/bmj.296.6618.320. [DOI] [Google Scholar]
- 6.Jacobsen A.P., Raber I., McCarthy C.P. Lifelong aspirin for all in the secondary prevention of chronic coronary syndrome: still sacrosanct or is reappraisal warranted? Circulation. 2020;142:1579–1590. doi: 10.1161/CIRCULATIONAHA.120.045695. [DOI] [PubMed] [Google Scholar]
- 7.Final report on the aspirin component of the ongoing physicians’ health study. N Engl J Med. 1989;321(3):129–135. doi: 10.1056/NEJM198907203210301. [DOI] [PubMed] [Google Scholar]
- 8.Ridker P.M., Cook N.R., Lee I.-.M. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352(13):1293–1304. doi: 10.1056/NEJMoa050613. [DOI] [PubMed] [Google Scholar]
- 9.Bibbins-Domingo K. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: u.s. preventive services task force recommendation statement. Ann Intern Med. 2016;164(12):836. doi: 10.7326/M16-0577. [DOI] [PubMed] [Google Scholar]
- 10.Pearson T.A., Blair S.N., Daniels S.R. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. Circulation. 2002;106(3):388–391. doi: 10.1161/01.CIR.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 11.Raber I., Mccarthy C.P., Vaduganathan M. The rise and fall of aspirin in the primary prevention of cardiovascular disease. Lancet. 2019;393(10186):2155–2167. doi: 10.1016/S0140-6736(19)30541-0. [DOI] [PubMed] [Google Scholar]
- 12.Gaziano J.M., Brotons C., Coppolecchia R. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet. 2018;392(10152):1036–1046. doi: 10.1016/S0140-6736(18)31924-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McNeil J.J., Wolfe R., Woods R.L. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379(16):1509–1518. doi: 10.1056/NEJMoa1805819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arnett D.K., Blumenthal R.S., Albert M.A. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2020;141:e774. doi: 10.1016/j.jacc.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC). Behavioral risk factor surveillance system survey data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, [2019]. Accessed March 31, 2021. https://www.cdc.gov/brfss/data_documentation/index.htm
- 16.Centers for Disease Control and Prevention (CDC). Methodologic Changes in the Behavioral Risk Factor Surveillance System in 2011 and Potential Effects on Prevalence Estimates. Published June 8, 2012. Accessed April 16, 2021. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6122a3.htm [PubMed]
- 17.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 18.Tchwenko S., Fleming E., Perry G.S. Aspirin use for the primary prevention of myocardial infarction among men in north Carolina, 2013. Prev Chronic Dis. 2015;12(11) doi: 10.5888/pcd12.150342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. Poverty Guidelines | ASPE. Accessed December 17, 2020. https://aspe.hhs.gov/poverty-guidelines
- 20.Ajani U.A., Ford E.S., Greenland K.J., Giles W.H., Mokdad A.H. Aspirin use among U.S. adults: behavioral risk factor surveillance system. Am J Prev Med. 2006;30(1):74–77. doi: 10.1016/j.amepre.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 21.Luepker R.V., Steffen L.M., Duval S., Zantek N.D., Zhou X., Hirsch A.T. Population trends in aspirin use for cardiovascular disease prevention 1980-2009: the minnesota heart survey. J Am Heart Assoc. 2015;4(12) doi: 10.1161/JAHA.115.002320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou Y., Boudreau D.M., Freedman A.N. Trends in the use of aspirin and nonsteroidal anti-inflammatory drugs in the general U.S. population. Pharmacoepidemiol Drug Saf. 2014;23(1):43–50. doi: 10.1002/pds.3463. [DOI] [PubMed] [Google Scholar]
- 23.Persell S.D., Baker D.W. Aspirin use among adults with diabetes: recent trends and emerging sex disparities. Arch Intern Med. 2004;164(22):2492–2499. doi: 10.1001/archinte.164.22.2492. [DOI] [PubMed] [Google Scholar]
- 24.Rhee T.G., Kumar M., Ross J.S., Coll P.P. Age-related tragectories of cardiovascular risk and use of aspirin and statin among adults aged 50 or older, 2011-2018. J Am Geriatr Soc. 2021:jgs.17038. doi: 10.1111/jgs.17038. Published online February 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stuntz M., Bernstein B. Recent trends in the prevalence of low-dose aspirin use for primary and secondary prevention of cardiovascular disease in the United States, 2012–2015. Prev Med Reports. 2017;5:183–186. doi: 10.1016/j.pmedr.2016.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Graham I., Atar D., Borch-Johnsen K. European guidelines on cardiovascular disease prevention in clinical practice: executive summary - Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by. Eur Heart J. 2007;28(19):2375–2414. doi: 10.1093/eurheartj/ehm316. [DOI] [PubMed] [Google Scholar]
- 27.Wood D., Wray R., Poulter N. JBS 2: joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005;91(Suppl. 5):v1–v52. doi: 10.1136/hrt.2005.079988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.ASCEND Study Collaborative Group, Bowman L., Mafham M. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529–1539. doi: 10.1056/nejmoa1804988. [DOI] [PubMed] [Google Scholar]
- 29.O'Brien C.W., Juraschek S.P., Wee C.C. Prevalence of aspirin use for primary prevention of cardiovascular disease in the United States: results from the 2017 National Health Interview Survey. Ann Intern Med. 2019;171(8):596–598. doi: 10.7326/M19-0953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu E.Y., Al-Sofiani M.E., Yeh H.-.C., Echouffo-Tcheugui J.B., Joseph J.J., Kalyani R.R. Use of preventive aspirin among older us adults with and without diabetes. JAMA Netw Open. 2021;4(6) doi: 10.1001/JAMANETWORKOPEN.2021.12210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.VanWormer J.J., Miller A.W., Rezkalla S.H. Aspirin overutilization for the primary prevention of cardiovascular disease. Clin Epidemiol. 2014;6:433–440. doi: 10.2147/CLEP.S72032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17 187 cases of suspected acute myocardial infarction: ISIS-2. Lancet. 1988;332(8607):349–360. doi: 10.1016/S0140-6736(88)92833-4. [DOI] [PubMed] [Google Scholar]
- 33.Baigent C., Sudlow C., Collins R., Peto R. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. Br Med J. 2002;324(7329):71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith S.C., Benjamin E.J., Bonow R.O. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124(22):2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 35.Ansa B., Hoffman Z., Lewis N. Aspirin use among adults with cardiovascular disease in the United States: implications for an intervention approach. J Clin Med. 2019;8(2):264. doi: 10.3390/jcm8020264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Opotowsky A.R., McWilliams J.M., Cannon C.P. Gender differences in aspirin use among adults with coronary heart disease in the United States. J Gen Intern Med. 2007;22(1):55–61. doi: 10.1007/s11606-007-0116-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fang J., George M.G., Hong Y., Loustalot F. Use of aspirin for prevention of recurrent atherosclerotic cardiovascular disease among adults — 20 states and the district of Columbia, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(27):733–737. [PMC free article] [PubMed] [Google Scholar]
- 38.Newby L.K., Allen LaPointe N.M., Chen A.Y. Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation. 2006;113(2):203–212. doi: 10.1161/CIRCULATIONAHA.105.505636. [DOI] [PubMed] [Google Scholar]
- 39.Waheed N., Elias-Smale S., Malas W. Sex differences in non-obstructive coronary artery disease. Cardiovasc Res. 2020;116(4):829–840. doi: 10.1093/cvr/cvaa001. [DOI] [PubMed] [Google Scholar]
- 40.Maddox T.M., Ho P.M., Roe M., Dai D., Tsai T.T., Rumsfeld J.S. Utilization of secondary prevention therapies in patients with nonobstructive coronary artery disease identified during cardiac catheterization: insights from the national cardiovascular data registry cath-PCI registry. Circ Cardiovasc Qual Outcomes. 2010;3(6):632–641. doi: 10.1161/CIRCOUTCOMES.109.906214. [DOI] [PubMed] [Google Scholar]
- 41.Reeves M.J., Bushnell C.D., Howard G. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7(10):915–926. doi: 10.1016/S1474-4422(08)70193-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barakat K., Wilkinson P., Suliman A., Ranjadayalan K., Timmis A. Acute myocardial infarction in women: contribution of treatment variables to adverse outcome. Am Heart J. 2000;140(5):740–746. doi: 10.1067/mhj.2000.110089. [DOI] [PubMed] [Google Scholar]
- 43.Scirica B.M., Moliterno D.J., Every N.R. Differences between men and women in the management of unstable angina pectoris (the Guarantee Registry) Am J Cardiol. 1999;84(10):1145–1150. doi: 10.1016/S0002-9149(99)00525-1. [DOI] [PubMed] [Google Scholar]
- 44.Jneid H., Fonarow G.C., Cannon C.P. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118(25):2803–2810. doi: 10.1161/CIRCULATIONAHA.108.789800. [DOI] [PubMed] [Google Scholar]
- 45.Quality Improvement for Institutions. Outpatient Registries. Accessed April 1, 2021. https://cvquality.acc.org/NCDR-Home/registries/outpatient-registries
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.