Abstract
A 66‐year‐old woman was hospitalized for recurrent pneumonia twice in 1 year. After treatment for pneumonia, chronic coughing, sputum and low‐grade fever continued, so she was referred and admitted to our hospital for investigation. Chest computed tomography revealed a lung infiltrative shadow and diffuse centrilobular micronodules. Histological findings from transbronchial lung biopsy showed chronic inflammation and giant cells in the bronchiole. These findings were compatible with diffuse aspiration bronchiolitis (DAB), which is characterized by chronic inflammation of the bronchioles caused by recurrent aspiration of foreign bodies. Oesophagogastroduodenoscopy revealed stenosis of the oesophageal entrance, which was thought to be caused by radiation therapy for hypopharyngeal cancer 20 years before. Antibiotic treatment ameliorated the centrilobular nodule shadow. After discharge, there was no recurrence. This is the first case report of DAB resulting from oesophageal stenosis associated with hypopharyngeal cancer and will serve as an educational case.
Keywords: aspiration pneumonia, diffuse aspiration bronchiolitis, oesophageal stenosis, pharyngeal cancer, radiation therapy
Here, we report a case of diffuse aspiration bronchiolitis (DAB) with oesophageal stenosis after radiation therapy for hypopharyngeal cancer. To the best of our knowledge, this is the first report of DAB due to oesophageal stenosis after radiation therapy, highlighting the importance of late‐onset chronic aspiration after radiation therapy for head and neck cancer.

INTRODUCTION
Diffuse aspiration bronchiolitis (DAB) is characterized by chronic inflammation of the bronchioles from recurrent aspiration of foreign particles. Macroscopic findings of DAB are similar to diffuse panbronchiolitis.1 Dysphagia is detected in almost all DAB cases, regardless of the patient background.2 DAB is more prevalent among patients who have been lying in bed in the long term, especially in elderly poor consciousness patients with gastro‐oesophageal reflux disease (GERD) and achalasia.3 Here, we report a DAB case with oesophageal stenosis after radiation therapy for hypopharyngeal cancer. To the best of our knowledge, this is the first report of DAB due to oesophageal stenosis after radiation therapy, highlighting the importance of late‐onset chronic aspiration after radiation therapy for head and neck cancer.
CASE REPORT
A 66‐year‐old woman had a low‐grade fever and productive cough, 1 year before visiting our hospital. She was hospitalized for pneumonia in an acute care hospital, twice in the previous year. After discharge, the patient was being managed as an outpatient by a general practitioner. However, her symptoms continued and she was referred to our tertiary hospital. She had a history of hypopharyngeal cancer that had been treated with radiation therapy 20 years ago. She had never smoked or consumed alcohol. She had a family history of pulmonary tuberculosis (younger brother). On admission, the patient's temperature was 37.3°C, her heart rate was 72 bpm and her blood pressure was 112/68 mmHg. She was underweight; her height was 143 cm, her weight was 29 kg and her body mass index was 14.2 kg/m2. Laboratory data revealed elevated C‐reactive protein (1.6 mg/dl). The partial pressure of arterial oxygen was 85 mmHg. Coarse crackles were heard bilaterally in the lower lung fields on inspiration. A chest x‐ray showed bilateral infiltrates and micronodular changes in the lower lung fields (Figure 1A). Chest computed tomography (CT) showed diffuse micronodules and lung infiltration in the left lower lobe and right middle lobe, and bronchiectasis in the right middle lobe (Figure 1B,C). On day 6 after admission, she underwent bronchoscopy for bronchoalveolar lavage (BAL) and transbronchial lung biopsy (TBLB) because the clinical course and imaging findings suggested the possibility of tuberculosis or metastatic tumours as differential diagnoses. The BAL fluid (right B5a) revealed an increased total cell count (2.1 × 106/ml) with 90% neutrophils. TBLB from the right lower lobe showed inflammatory infiltrate and giant cells in the bronchiole (Figure 1E). Klebsiella pneumoniae 3+ and Acinetobacter baumannii 2+ were identified in the BAL fluid, and the test for mycobacteria was negative. Pathological examination showed no evidence of malignancy. Therefore, we diagnosed DAB.
FIGURE 1.
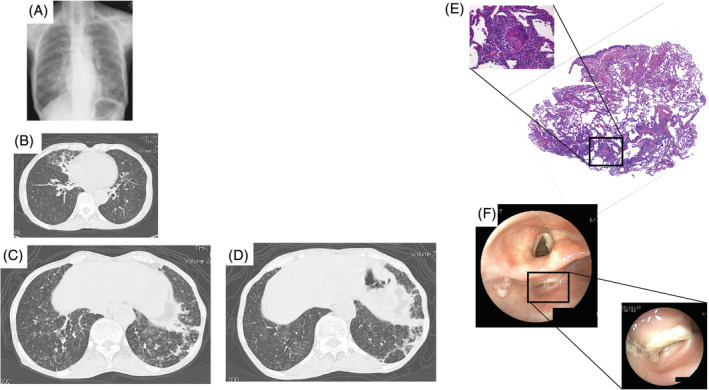
Chest images on admission. (A) The chest x‐ray shows lung infiltration and bilateral micronodular changes in the lower lung field. (B, C) Chest computed tomography (CT) shows diffuse micronodules, lung infiltration in the left lower lobe and right middle lobe, and bronchiectasis in the right middle lobe. Chest images 28 days after administration. (D) Chest CT shows improved diffuse micronodules in the bilateral lung field. Transbronchial lung biopsy from the right lower lobe (E). Photomicrograph shows chronic inflammation and giant cells in the bronchiole (haematoxylin–eosin staining; original magnification, ×40; inset magnification, ×400). Oesophagogastroduodenoscopy shows oesophageal stenosis (F)
After bronchoscopy, cefotaxime (2 g/day) was administered. On day 8, the inflammatory reaction worsened. According to a drug sensitivity test, we changed to meropenem (1 g/day) on day 10, which significantly improved the inflammatory reaction. On day 17, oesophagogastroduodenoscopy was performed to identify the cause of aspiration. An ulcer scar from behind the hypopharynx to the entrance of the oesophagus was detected (Figure 1F). Stenosis of the oesophagus, associated with radiation therapy for hypopharyngeal cancer 20 years before, was thought to be the cause of the repeated aspiration. On day 18, we changed the antibiotic to oral moxifloxacin (400 mg), and the treatment was completed on day 24. The patient refused balloon catheter dilatation. Therefore, the patient's diet was altered to include only semisolid foods. On day 28, lung infiltrates were not improved, but the bilateral micronodular shadow was significantly improved (Figure 1D). On day 35, she was discharged. Follow‐up chest images after discharge confirmed the absence of recurrence.
DISCUSSION
DAB is defined as chronic inflammation of the bronchioles caused by recurrent aspiration of foreign bodies.1 Chest CT typically reveals centrilobular micronodules. The differential diagnosis includes mycobacterial pneumonia, diffuse panbronchiolitis and DAB. In the present case, there was a family history of pulmonary tuberculosis. However, tuberculosis was not detected with BAL and TBLB. Histological findings from the right lower lobe were characterized by the location of chronic inflammation with a foreign body in the bronchioles, leading to a DAB diagnosis. DAB is characterized by chronic inflammation caused by reactions to foreign bodies in the bronchioles.4 The patient had no GERD symptoms. We performed oesophagogastroduodenoscopy to investigate the cause of DAB and detected stenosis of the oesophagus. According to her history, the cause of DAB was radiation therapy for hypopharyngeal cancer 20 years before. Endoscopic balloon dilation is a form of therapy available for stenosis after radiation therapy.5 Treatment of DAB with cricopharyngeal myotomy was also reported.6 However, this patient declined invasive treatments, including endoscopic balloon dilatation and cricopharyngeal myotomy. To avoid aspiration, the patient's meal consistency was changed to include only semisolid food. Thereafter, the deterioration of DAB was not observed. Although the mechanism responsible for DAB due to oesophageal stenosis 20 years after radiation therapy is unclear, dysphagia caused by sarcopenia in the swallowing muscles because of age and malnutrition may have contributed to the development of DAB.
To the best of our knowledge, this is the first report of DAB resulting from stenosis after radiation therapy for hypopharyngeal cancer. Aspiration‐related lung diseases are common; however, the causes are rarely investigated properly and adequately. Only 25% of DAB patients were clinically suspected.2 DAB should be considered as a differential diagnosis in the case of a diffuse centrilobular micronodular shadow in chest CT.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTION
Kazuhide Horimoto and Yoshiro Kai wrote the manuscript. All authors contributed to the editing of the manuscript and approved the final version of the manuscript.
ETHICS STATEMENT
The authors declare that appropriate written informed consent was obtained for the publication of this case report and accompanying images.
ACKNOWLEDGMENT
The authors would like to thank Enago (www.enago.jp) for the English language review.
Horimoto K, Kai Y, Fukuoka A, Tamaki S, Yoshikawa M, Hamada K, et al. A case of diffuse aspiration bronchiolitis due to oesophageal stenosis after radiation therapy. Respirology Case Reports. 2021;9:e0855. 10.1002/rcr2.855
Associate Editor: Yet Hong Khor
REFERENCES
- 1.Fukuchi Y, Matsuse T, Kida K. Infection – clinico‐pathological profile of diffuse aspiration bronchiolitis (DAB). Nihon Kyobu Shikkan Gakkai Zasshi. 1989;27:571–7. [PubMed] [Google Scholar]
- 2.Hu X, Yi ES, Ryu JH. Diffuse aspiration bronchiolitis: analysis of 20 consecutive patients. J Bras Pneumol. 2015;41:161–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Teramoto S, Yamamoto H, Yamaguchi Y, Tmoita T, Ouchi Y. Diffuse aspiration bronchiolitis due to achalasia. Chest. 2004;125:349–50; author reply 350. [DOI] [PubMed] [Google Scholar]
- 4.Matsuse T, Oka T, Kida K, Fukuchi Y. Importance of diffuse aspiration bronchiolitis caused by chronic occult aspiration in the elderly. Chest. 1996;110:1289–93. [DOI] [PubMed] [Google Scholar]
- 5.Laurell G, Kraepelien T, Mavroidis P, Lind BK, Fernberg JO, Beckman M, et al. Stricture of the proximal esophagus in head and neck carcinoma patients after radiotherapy. Cancer. 2003;97:1693–700. [DOI] [PubMed] [Google Scholar]
- 6.Inoue T, Oida K, Kohri Y, Taguchi Y, Tomii K, Matsumura Y, et al. Successful treatment of diffuse aspiration bronchiolitis by cricopharyngeal myotomy. Nihon Kyobu Shikkan Gakkai Zasshi. 1996;34:926–30. [PubMed] [Google Scholar]


