Abstract
Introduction
Breast cancer survivors are faced with several psychological issues. We report the influence on self-efficacy by a holistic orientated training schedule based on the “Kyusho Jitsu” martial art and explore the effects on self-efficacy, distress, fear, and depression.
Methods
Breast cancer survivors (N = 51) were randomly assigned to an intervention (n = 30) or control group (n = 21). The intervention group participated in a Kyusho Jitsu intervention twice a week over a period of 6 months, the control group received no intervention. Patients from both groups were measured at baseline, 3 and 6 months on level of self-efficacy (German General-Self-Efficacy Scale, SWE), stress (Perceived Stress Questionnaire, PSQ20), and fear and depression (Hospital Anxiety and Depression Scale, HADS).
Results
Analysis of the original data showed a significant difference between both groups regarding the subscale “joy” (P = .018). Several significant results within the intervention group were seen in self-efficacy (P = .014), fear (P = .009) and the overall score for fear and depression (P = .043). Both groups improved significantly within “worries” (intervention P = .006, control P = .019) and the PSQ20 overall score (both P = .005). The control group also significantly improved in the subscale for “demands” (P = .019).
Conclusion
To summarize, our pilot study showed that Kyusho Jitsu training is safe and feasible. Though, the intervention alone cannot be considered as being effective enough to help breast cancer survivors regarding relevant psychological issues, but might be an important supplement offer within follow-up care.
Keywords: breast neoplasm, exercise intervention, martial arts, self-efficacy, anxiety, depression, stress
Introduction
Breast cancer is the leading cause of cancer-related death among females worldwide.1,2 With approximately 69 000 new cases per year in Germany, breast cancer is the most common cancer among women.3 The absolute 5-year survival rate for 2015/2016 was 79%.3 A diagnosis of a life threatening disease such as cancer can challenge a patient’s ability to cope4 and the stress associated with the diagnosis and treatment of cancer can cause significant psychiatric morbidities.5 In addition to the struggles of cancer treatment (eg, unexpected body changes caused by breast cancer surgery or hair loss from chemotherapy), systemic side effects such as “arthralgia” which is commonly triggered by aromatase inhibitors,6 foster distress, which can lead to a large psychological burden for the patient. 25% to 50% of patients have psychological problems, with at least 25% meeting the criteria for either major depressive disorder or adjustment disorder with depressed mood.5 Furthermore, a combination of mood disorders occur in 30% to 40% of oncological patients in hospital settings.7
Self-efficacy refers to the ability of an individual to control their motivation, behavior, and environment, and essentially boils down to be the belief of an individual to succeed in a given situation.8 Obviously, this belief is shaken after a cancer diagnosis, and self-efficacy will play an important role in the recovery process. Interestingly enough, Tai Chi (a form of Chinese martial arts/mediative practice) has been shown to have a beneficial effect on self-efficacy in a variety of patient groups,9,10 including breast cancer survivors.11
However, more than one third of all breast cancer survivors experience distress even after completing medical therapy.12 This distress leads to a higher risk of psychological illness in breast cancer survivors. For example, a significant number of women still had elevated anxiety and depression symptoms 18 months following treatment.13 Moreover, the majority of the literature indicates that the experience of stress impairs efforts to be physically active.14 This is especially true for those who receive a diagnosis of breast cancer, as simply receiving the diagnosis itself can reduce the level of physical activity.15 This leads to a vicious cycle of impaired movement and negative side effects, as those who do exercise suffer from less depression,16 anxiety,17 fatigue,18,19 and cognitive impairments.20,21
Previous research indicates that physical activity and exercise can directly benefit an individual upon the completion of cancer treatment.22-24 This applies in particular for depression, with both cancer patients22 and clinicians23 reporting lower levels of depression among patients who completed exercise training. Conversely, physical inactivity can contribute to worsening health in breast cancer survivors.24
While many modalities of exercise have been studied with the goal of improving the quality of life of cancer patients, one that has received markedly less attention, is martial arts. However, in recent years both martial arts and Tai Chi have been the focus of various studies, to increasingly positive results.25,26 One such as of yet under researched type of martial arts is Kyusho Jitsu. Kyusho Jitsu focuses on the so-called vital points of the body, and how the manipulation of these vital points can be used to produce neurological or physiological effects. While originally developed to be used in hand-to-hand combat, traditional Chinese medicine has applied the same principles with the goal of alleviating a variety of ailments.
It is for this reason, that Kyusho Jitsu could be a feasible physical activity modality to improve the mental well-being of breast cancer patients; while at the same time increasing their overall levels of physical activity, and thus all of the previously discussed positive benefits of exercise in general. Therefore, it is the goal of this study to assess the impact that a Kyusho Jitsu martial arts training program on the distress experienced by cancer patients, more specifically its influence on self-efficacy, fear, and depression.
Methods
This pilot study was a prospective, randomized-controlled 2-armed intervention study, which ran for 24 weeks with 51 female breast cancer survivors participating. The participants were randomly assigned to the intervention group or the control group by an uninvolved third-party using Microsoft Excel. The intervention group received their exercise intervention from weeks 1 to 24, while the control group received no such intervention, and only had contact with the researchers at their assessment appointments. The exercise intervention consisted of a 24-week holistic training program, which was based on “Kyusho Jitsu” martial arts, also known as “the art of vital points.” Participants were asked to attend 2 exercise sessions per week for 90 minutes each. The primary outcome was feasibility, which has been analyzed and published elsewhere within the publication of the main study.27
This exploratory analysis focused on the modification of distress in the intervention group. Further secondary outcomes were self-efficacy, fear, and depression. All outcomes were measured at baseline (t0), at the end of week 12 (t1), and 24 (t2).
The study was conducted under consideration of the Declaration of Helsinki. It was approved by the human research ethical committee of the German University of Sports Cologne and was registered retrospectively in the German Clinical Trials Register (DRKS-ID: DRKS00011245).
Participants and Procedures
Participants were recruited via local newspaper advertisement between 16th of June 2014 and 9th of September 2014. Inclusion criteria were: female breast cancer survivors aged 18 years or older, and having completed medical treatment (excluding hormone treatment) within the 6 months before enrollment. All participants had to provide written consent before they were enrolled into the study. Exclusion criteria were: metastasis, if the last chemotherapy or surgery was completed more than 6 months ago, or if physical and/or psychological functions that would impair the participation within the trial were present.
Assessments
Patients of both groups had to fill in an anthropometric questionnaire, which was comprised of clinical and sociodemographic data. Additional information about tumor stage, chemotherapy, and radiation were collected from patient medical records. All questionnaires were administered by a member of the research team.
The measurement of the secondary outcome self-efficacy was tested using the German SWE (“Allgemeine Selbst-Wirksamkeits-Erwartung”) questionnaire.28 It is a one-dimensional scale of 10 items. The range of the items is from 1 is “not true,” 2 is “hardly correct,” 3 is “more true” to 4 is “accurate.” Each item expresses an internal-stable attribution of the success expectation. The individual test value results from the summation of all 10 responses, so a score between 10 and 40 is possible.
The level of distress was evaluated using the PSQ-20 (Perceived Stress Questionnaire).29 The questionnaire analyses the subjective perception, evaluation and further processing of stressors. Whilst the original PSQ contains 30 items, the PSQ-20 is the short-form version of the original, and is comprised of 20 items. The range of the items is from 1 for “almost never,” 2 indicating “sometimes,” 3 for “frequently,” and 4 for “mostly” and should indicate certain stress events in a defined period of time. The period was set to the last 4 weeks, but the short form still contains a variant, which inquires for the last 2 years. The shortened version includes the following 4 scales, each with 5 items: worries, tension, joy, and demands.30
The level of fear and depression was quantified using the HADS (Hospital Anxiety and Depression Scale).31 The questionnaire consists of 14 questions that are presented alternately regarding the subdomains “anxiety” and “depression,” each with 7 items. For each answer, there are scores of 0 to 3. By adding the individual scores, both an anxiety- and a depression scale can be formed. The values are interpreted as: 0 to 7 inconspicuous, 8 to 10 suspect, >10 conspicuous.
Intervention
The therapeutic intervention consisted of a 24-week holistic orientated exercise training based on “Kyusho Jitsu—the art of vital points.” The training was performed 2 times a week for 90 minutes per session. The training included several aspects of martial arts, self-defense, and pain cognition, plus stretching, and physical invigoration. Kyusho Jitsu uses different techniques from Tai Chi and Qi Gong, such as breathing exercises and meditation to improve mental health. All training sessions were specially designed for post breast cancer patients, and focused on providing a positive environment for the participants. The training was split into 2 main parts: the first part included a physical training session, beginning with a warmup phase (for about 45 minutes). It consisted of different physical and psychological elements: coordination, mobilization (upper body focus), strength and endurance, but also self-efficacy and dependence training for psychological stabilization and handling of fear (such as blindly walking through the gym). Every training session started and ended with a short round of feedback about feelings, thoughts and whether it was considered a personal success.
The second main part was divided in 3 phases: Kyusho Jitsu training (20 minutes), Katha (continuous fight sequence for approximately 5 minutes) and meditation (15 minutes). In the first phase, the Kyusho Jitsu training, the patients were able to learn new elements (in the group) and review previously learnt movement patterns. The exercise time varied for every individual, and additionally when problems arose regarding the physical capability of an individual, different variations on the movement or exercise were provided. The Kyusho Jitsu training was also accompanied by Tai Chi breathing exercises. In the second phase, the fighting sequence was performed with relaxing music as a group. The goal was to learn one complete Katha by the end of the study. The third and last phase was the mediation for relaxing and strengthening the vital points (based on body “Meridians” from Traditional Chinese medicine).
The training took place at the German Sport University Cologne and was supervised by sport scientists and professional Kyusho Jitsu instructors who built up the movement patterns from simple to complex routines.
During the training duration of 24 weeks, the control group received no kind of intervention.
Statistical Analysis
Patient characteristics were described using mean ± standard deviation (SD). Potential baseline differences between groups in age, time since diagnosis and cancer treatments (surgery, chemotherapy, radiation, hormone treatment, antibodies) were analyzed using Mann–Whitney U-Tests and Chi-square tests, as appropriate. Outcome results were analyzed per protocol and presented as mean ± SD and median. For the between-group comparison of the delta we used the Mann–Whitney U-Test, for the within group comparison from baseline to 6 months the Wilcoxon Test, with a 2-sided significance level of α = 5%. A P-value ≤.05 was considered statistically significant. Furthermore, missing outcome data were imputed by Last Observation Carried Forward (LOCF) for an intention-to-treat analysis. All analyses were done using SPSS Statistics, Version 27 (IBM Corp., Armonk, NY, USA).
Results
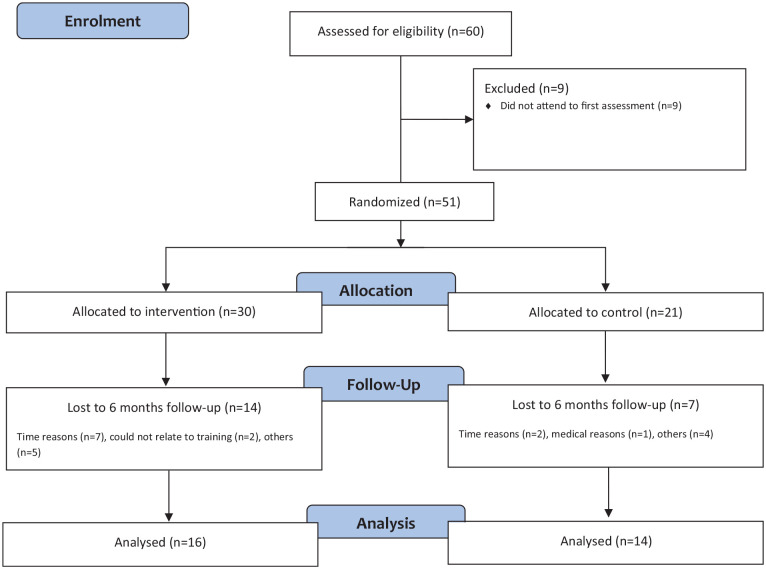
Between June 2014 and September 2014, 60 breast cancer survivors were enrolled in the study. However, because 9 patients did not attend to first assessment session, in total 51 patients were randomized, with 30 patients in the intervention group and 21 patients in the control group (Figure 1).
Figure 1.
CONSORT flow diagram.
Both groups were comparable with regards to the most relevant clinical and socio-demographic data. All patients had completed medical treatment within the previous 6 months before inclusion into the study. With study entry the time since diagnosis of breast cancer was 48.3 ± 44.4 months in the intervention group and 39.8 ± 34.5 months in the control group (Table 1).
Table 1.
Characteristics of Patients at Baseline.
| Intervention group (N = 30) | Control group (N = 21) | P-value | |
|---|---|---|---|
| Age, y (±SD) (n) | 54,23 (±7,846) (n = 30) | 51,52 (±8,412) (n = 21) | .244 |
| Time since diagnosis, mo (±SD) (n) | 48,31 (±44,42) (n = 29) | 39,76 (±34,49) (n = 21) | .466 |
| Surgery (n) | 29/29 | 21/21 | NA |
| Chemotherapy (n) | 14/29 | 15/21 | .102 |
| Radiation (n) | 23/30 | 17/21 | .714 |
| Hormone treatment (n) | 21/29 | 15/21 | .939 |
| Antibodies (n) | 4/26 | 2/18 | .685 |
Abbreviations: n, number of patients; SD, standard deviation.
During the study, some patients from both the intervention and control group dropped out due to personal or medical reasons. There were 14 dropouts from the intervention group and 7 dropouts from the control group. No adverse events were observed. The average training participation of the intervention group was 67%.
The results of the between-group and within-group comparison from baseline (t0) to post-intervention (t2) assessment of self-efficacy, distress, fear, and depression are presented in Table 2. The results of the assessment after 12 weeks will not be presented within this publication because of an insufficient number of patients completing this assessment.
Table 2.
Group Comparison From Baseline to 6 Months Assessment.
| Group | Baseline | 6 mo | Delta | P-valuea | P-valueb |
|---|---|---|---|---|---|
| Mean ± SD (median) | Mean ± SD (median) | Mean ± SD (median) | |||
| Self-efficacy (SWE) | |||||
| Overall score | |||||
| Intervention | 27.7 ± 5.1 (28.0) | 31.0 ± 4.3 (32.0) | 2.9 ± 3.5 (3.0) | .107 | .014 |
| Control | 26.8 ± 4.6 (28.5) | 26.8 ± 4.7 (28.5) | 0.4 ± 5.6 (0.0) | .905 | |
| Perceived Stress Questionnaire (PSQ-20) | |||||
| Worries | |||||
| Intervention | 45.7 ± 15.2 (46.7) | 24.8 ± 11.2 (23.3) | −16.7 ± 12.9 (−20.0) | .168 | .006 |
| Control | 49.5 ± 27.0 (46.7) | 40.5 ± 20.7 (33.3) | −11.3 ± 17.5 (−6.7) | .019 | |
| Tension | |||||
| Intervention | 49.3 ± 11.8 (46.7) | 44.2 ± 11.1 (43.3) | −4.9 ± 13.0 (−6.7) | .316 | .151 |
| Control | 48.1 ± 6.0 (46.7) | 48.6 ± 11.2 (46.7) | 1.0 ± 10.8 (0.0) | .608 | |
| Joy | |||||
| Intervention | 42.2 ± 19.3 (40.0) | 65.2 ± 23.6 (60.0) | 18.5 ± 14.4 (13.3) | .018 | .003 |
| Control | 44.8 ± 23.7 (40.0) | 47.2 ± 20.4 (53.3) | 4.8 ± 19.8 (0.0) | .667 | |
| Demands | |||||
| Intervention | 50.5 ± 13.5 (46.7) | 45.3 ± 14.7 (46.7) | −5.6 ± 12.1 (−6.7) | .511 | .136 |
| Control | 57.1 ± 13.0 (53.3) | 47.1 ± 16.0 (40.0) | −9.7 ± 12.1 (−6.7) | .019 | |
| Overall score | |||||
| Intervention | 50.8 ± 15.3 (51.7) | 33.1 ± 16.8 (34.2) | −15.2 ± 9.8 (−13.3) | .152 | .005 |
| Control | 56.3 ± 19.5 (55.0) | 49.9 ± 20.4 (40.0) | −10.0 ± 12.1 (−5.0) | .005 | |
| Hospital Anxiety and Depression Scale (HADS) | |||||
| Overall score | |||||
| Intervention | 22.0 ± 1.9 (23.0) | 20.1 ± 2.4 (20.0) | −2.2 ± 3.2 (−2.5) | .430 | .043 |
| Control | 22.0 ± 2.9 (22.0) | 20.8 ± 2.0 (20.0) | −1.2 ± 3.7 (−1.0) | .135 | |
| Fear subscale | |||||
| Intervention | 11.8 ± 1.3 (12.0) | 10.1 ± 1.4 (10.0) | −1.8 ± 2.0 (−1.5) | .616 | .009 |
| Control | 11.2 ± 1.4 (11.5) | 10.1 ± 1.6 (10.0) | −1.0 ± 2.5 (−2.0) | .166 | |
| Depression subscale | |||||
| Intervention | 10.2 ± 1.6 (10.0) | 10.0 ± 1.2 (10.0) | −0.4 ± 2.2 (−1.0) | .650 | .396 |
| Control | 10.8 ± 1.9 (11.0) | 10.6 ± 0.7 (10.5) | −0.2 ± 2.0 (0.0) | .820 | |
Abbreviation: SD, standard deviation.
Between group comparison for delta (Mann-Whitney U-test).
Within group comparison from baseline to 6 months (Wilcoxon test).
P-values in bold indicate statistically significant differences between or within the groups (P < .05).
Self-efficacy
Self-efficacy (SWE) analysis of the original data showed no significant difference between both groups. There was a significant improvement in the overall self-efficacy score within the intervention group from baseline to 6 months (P = .014), while the score remained unchanged within the control group.
Distress
The inter-group comparison showed significant improvement regarding the subscale “joy” (P = .018), favoring the intervention group. There were no further significant differences between the groups.
Analysis of the intra-group comparison of the original data showed several significant changes from baseline to the 6 months. There was a significant reduction of the subscale “worries” in both the intervention (P = .006) and control (P = .019) group. Both groups showed no relevant change for the subscale “tension.” However, there was a significant decrease of “demands” in the control group (P = .019). Both groups showed a significant decrease in the overall score (P = .005).
Fear and Depression
From baseline to the 6 months assessment there were no significant differences between the groups regarding the subscales of fear and depression, nor the overall score. Analysis of the intra-group comparison showed significant improvements within the “fear” subscale (P = .009) and the overall score (P = .043), which decreased from baseline to 6 months. There were no significant changes within the control group.
Discussion
At the start of this randomized controlled 2-armed intervention pilot study it was hypothesized that a holistic orientated training schedule which was borrowed from the “Kyusho Jitsu” martial art for 24 weeks would have a positive effect on the psychological well-being when faced with a life-threatening disease such as breast cancer. Feasibility as the primary outcome, as well as secondary outcomes such as quality of life and the level of physical activity were published elsewhere.27 Our findings showed that a Kyusho Jitsu intervention with breast cancer survivors is feasible27 and improved several outcomes of the participants. In addition, we wanted to explore the influences on self-efficacy, distress, fear, and depression. The Kyusho Jitsu intervention showed a significant rise of the self-efficacy score of the intervention group from baseline to 6 months (P = .014), though the difference was not significant when compared to the control group. This result corroborates the findings of Yeh et al10 who found that Tai Chi improved not only self-efficacy and social support, but overall empowerment with additional gains such as internal locus of control, self-awareness and stress management.
Some studies have shown that exercise reduces stress, anxiety, and depression among adults,32,33 but to our knowledge there are no studies investigating the influence of Kyusho Jitsu on distress. Galantino et al34 reported increased relaxation, reduced stress, and enhanced sleep quality and duration of breast cancer survivors while doing Tai Chi. Our findings only showed a significant difference for the subscale “joy” (P = .018), favoring the intervention group. The other subscales between both groups were not significant, which is why we cannot conclude the intervention to be effective regarding overall distress. Anyway, both groups significantly reduced their scores for “worries” and the overall score. We assume that, the increasing time since diagnosis and therapy leaded to decreasing levels of distress.35
Wipfli et al17 report that exercise interventions support the alleviation of anxiety. Our findings support this by showing a significant reduction of the fear scale and overall scale from the baseline to 6 months in the Kyusho Jitsu intervention group. Furthermore, our findings support the findings of Galantino et al34 who tested Tai Chi for the well-being of breast cancer survivors and found a significant improvement from the baseline to follow-up for the HADS anxiety scale.34 In our study we did not find any significant differences between both groups regarding the HADS, though, we found a significant reduction of the anxiety subscale from baseline to 6 months (P = .009) within the intervention group. This might be due to the improved coping mechanisms learned in the Kyusho Jitsu training routine. Kyusho Jitsu could thus be an effective method to sustainably lower the level of anxiety in post-care breast cancer patients. Unfortunately, we found no significant improvements in the depressive subscale. Therefore, it could be posited that Kyusho Jitsu neither improves or impairs depressive symptomatology.
Regarding the execution of the study, it can be said that on the positive side, the first randomized controlled supervised martial arts study in this setting with breast cancer patient in the follow-up care. It was a homogeneous group (age, type of therapy). Furthermore, the group had a good group dynamic, which is why after completing the study, 11 participants actually joined a Kyusho Jitsu club. No adverse events or negative physical side effects were observed.
However, this study was initially planned as a cross-over design after 24 weeks, but due to a high number of dropouts in both groups on the 1 side, and the high interest of eleven participants of the intervention group who ultimately joined a Kyusho Jitsu Club, a cross-over design was not realized. Furthermore, we had a low number of cases (51) which led to a small amount of data being gathered; this resulted in high sources of errors, that is that small variations will have had an impact on the results. Also, because of the small sample size it was not possible to do further analyses regarding weight status, type of diagnosis or type of treatment in terms of depression symptoms, for example. Additionally, the exercise intervention was hard to systemize, due to the individualized nature of the program itself.
Conclusion
To summarize, our prospective, randomized-controlled 2-armed intervention study did not show relevant differences between both groups to be considered effective. Though, the comparison within the intervention group may suggest that specialized martial arts training can support the psychological rehabilitation and may be beneficial in preventing distress, improving self-efficacy and reducing fear. However, further studies are needed to confirm these findings and to investigate the long-term effects of this training method.
Footnotes
Author Contributions: As the principal investigator F.B. was responsible for the study concept and design. T.N., J.S. and F.B. recruited participants and collected data. J.L.S., M.S., C.-A.M. and F.B. did the statistical analysis and interpretation of the data. J.L.S., M.S., C.-A.M. and F.B. drafted the manuscript. All authors approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by an anonymous contributor.
Trial Registration: DRKS-ID: DRKS00011245, Date of Registration in DRKS: 2017/02/14
https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00011245
ORCID iDs: Timo Niels  https://orcid.org/0000-0002-7309-0161
https://orcid.org/0000-0002-7309-0161
Carrie-Ann Minto  https://orcid.org/0000-0001-5425-3095
https://orcid.org/0000-0001-5425-3095
Freerk T Baumann  https://orcid.org/0000-0002-4450-7351
https://orcid.org/0000-0002-4450-7351
References
- 1.Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends—an update. Cancer Epidemiol Biomarkers Prev. 2016;25:16-27. [DOI] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209-249 [DOI] [PubMed] [Google Scholar]
- 3.Krebs in Deutschland für 2015/2016. Gemeinsame Publikation des Zentrums für Krebsregisterdaten und der Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. Robert Koch Institut; 2019. [Google Scholar]
- 4.Stanton AL, Danoff-Burg S, Huggins ME. The first year after breast cancer diagnosis: hope and coping strategies as predictors of adjustment. Psychooncology. 2002;11:93-102. [DOI] [PubMed] [Google Scholar]
- 5.Fallowfield L, Ratcliffe D, Jenkins V, Saul J. Psychiatric morbidity and its recognition by doctors in patients with cancer. Br J Cancer. 2001;84:1011-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burstein HJ, Winer EP. Aromatase inhibitors and arthralgias: a new frontier in symptom management for breast cancer survivors. J Clin Oncol. 2007;25:3797-3799. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160-174. [DOI] [PubMed] [Google Scholar]
- 8.Bandura A. Self-Efficacy: The Exercise of Control. W H Freeman/Times Books/Henry Holt & Co; 1997. [Google Scholar]
- 9.Murley B, Haas B, Hermanns M, Wang YT, Stocks E. Influence of Tai Chi on self-efficacy, quality of life, and fatigue among patients with cancer receiving chemotherapy: a pilot study brief. J Holist Nurs. 2019;37:354-363. [DOI] [PubMed] [Google Scholar]
- 10.Yeh GY, Chan CW, Wayne PM, Conboy L. The impact of Tai Chi exercise on self-efficacy, social support, and empowerment in heart failure: insights from a qualitative sub-study from a randomized controlled trial. PLoS One. 2016;11:e0154678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mustian KM, Katula JA, Gill DL, Roscoe JA, Lang D, Murphy K. Tai Chi Chuan, health-related quality of life and self-esteem: a randomized trial with breast cancer survivors. Support Care Cancer. 2004;12:871-876. [DOI] [PubMed] [Google Scholar]
- 12.Ploos van Amstel FK, van den Berg SW, van Laarhoven HW, Gielissen MF, Prins JB, Ottevanger PB. Distress screening remains important during follow-up after primary breast cancer treatment. Support Care Cancer. 2013;21:2107-2115. [DOI] [PubMed] [Google Scholar]
- 13.Vahdaninia M, Omidvari S, Montazeri A. What do predict anxiety and depression in breast cancer patients? A follow-up study. Soc Psychiatry Psychiatr Epidemiol. 2010;45:355-361. [DOI] [PubMed] [Google Scholar]
- 14.Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44:81-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Irwin ML, Crumley D, McTiernan A, et al. Physical activity levels before and after a diagnosis of breast carcinoma: the Health, Eating, Activity, and Lifestyle (HEAL) study. Cancer. 2003;97:1746-1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rethorst CD, Wipfli BM, Landers DM. The antidepressive effects of exercise: a meta-analysis of randomized trials. Sports Med. 2009;39:491-511. [DOI] [PubMed] [Google Scholar]
- 17.Wipfli BM, Rethorst CD, Landers DM. The anxiolytic effects of exercise: a meta-analysis of randomized trials and dose-response analysis. J Sport Exerc Psychol. 2008;30:392-410. [DOI] [PubMed] [Google Scholar]
- 18.Resnick HE, Carter EA, Aloia M, Phillips B, HE. Cross-sectional relationship of reported fatigue to obesity, diet, and physical activity: results from the third national health and nutrition examination survey. J Clin Sleep Med. 2006;2:163-169. [PubMed] [Google Scholar]
- 19.Theorell-Haglöw J, Lindberg E, Janson C. What are the important risk factors for daytime sleepiness and fatigue in women? Sleep. 2006;29:751-757. [DOI] [PubMed] [Google Scholar]
- 20.Lautenschlager NT, Cox KL, Flicker L, et al. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. JAMA. 2008;300:1027-1037. [DOI] [PubMed] [Google Scholar]
- 21.Rovio S, Kåreholt I, Helkala EL, et al. Leisure-time physical activity at midlife and the risk of dementia and Alzheimer’s disease. Lancet Neurol. 2005;4:705-711. [DOI] [PubMed] [Google Scholar]
- 22.Brown JC, Winters-Stone K, Lee A, Schmitz KH. Cancer, physical activity, and exercise. Compr Physiol. 2012;2:2775-2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stagl JM, Antoni MH, Lechner SC, Carver CS, Lewis JE. Postsurgical physical activity and fatigue-related daily interference in women with non-metastatic breast cancer. Psychol Health. 2014;29:177-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vardar-Yagli N, Sener G, Saglam M, et al. Associations among physical activity, comorbidity, functional capacity, peripheral muscle strength and depression in breast cancer survivors. Asian Pac J Cancer Prev. 2015;16:585-589. [DOI] [PubMed] [Google Scholar]
- 25.Navarro-Sanz A, Espejo-Reina A, Cerezo-Guzman MV, et al. Synchronized pedaling with martial arts improves quality of life of women with breast cancer. Int J Sports Med. 2018;39:978-983. [DOI] [PubMed] [Google Scholar]
- 26.Liu L, Tan H, Yu S, Yin H, Baxter GD. The effectiveness of tai chi in breast cancer patients: a systematic review and meta-analysis. Complement Ther Clin Pract. 2020;38:101078. [DOI] [PubMed] [Google Scholar]
- 27.Strunk MA, Zopf EM, Steck J, Hamacher S, Hallek M, Baumann FT. Effects of Kyusho Jitsu on physical activity-levels and quality of life in breast cancer patients. In Vivo. 2018;32:819-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwarzer R, Jerusalem MH. Skalen zur Erfassung von Lehrer-und Schülermerkmalen. Dokumentation der psychometrischen Verfahren im Rahmen der Wissenschaftlichen Begleitung des Modellversuchs Selbstwirksame Schulen. Freie Universität Berlin; 1999. [Google Scholar]
- 29.Levenstein S, Prantera C, Varvo V, et al. Development of the Perceived Stress Questionnaire: a new tool for psychosomatic research. J Psychosom Res. 1993;37:19-32. [DOI] [PubMed] [Google Scholar]
- 30.Fliege H, Rose M, Arck P, Levenstein S, Klapp BF. PSQ – Perceived Stress Questionnaire – German Modified Version. ZPID (Leibniz Institute for Psychology Information) – Testarchiv; 2009. [Google Scholar]
- 31.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [DOI] [PubMed] [Google Scholar]
- 32.Dunn AL, Trivedi MH, O'Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33:S587-S597;discussion 609. [DOI] [PubMed] [Google Scholar]
- 33.Galper DI, Trivedi MH, Barlow CE, Dunn AL, Kampert JB. Inverse association between physical inactivity and mental health in men and women. Med Sci Sports Exerc. 2006;38:173-178. [DOI] [PubMed] [Google Scholar]
- 34.Galantino ML, Callens ML, Cardena GJ, Piela NL, Mao JJ. Tai chi for well-being of breast cancer survivors with aromatase inhibitor-associated arthralgias: a feasibility study. Altern Ther Health Med. 2013;19:38-44. [PubMed] [Google Scholar]
- 35.Helgeson VS, Snyder P, Seltman H. Psychological and physical adjustment to breast cancer over 4 years: identifying distinct trajectories of change. Health Psychol. 2004;23:3-15. [DOI] [PubMed] [Google Scholar]