Abstract
Background
Body mass index (BMI) increases while cardiometabolic risk factors decrease in individuals in high‐income countries. This paradoxical observation raises the question of whether current measures of overweight and obesity properly identify cardiometabolic risk.
Methods
A total of 3675 participants (59% women) aged 40–84 years with whole‐body dual‐energy x‐ray absorptiometry scans from the seventh survey of the Tromsø Study were included to examine the association between visceral adipose tissue (VAT) in grams and BMI, waist circumference (WC), waist‐to‐hip ratio (WHR), and waist‐to‐height ratio (WHtR). Further, their association with single cardiometabolic risk factors (blood pressure, triglycerides, total cholesterol, high‐density lipoprotein [HDL] cholesterol, glycated hemoglobin, high‐sensitivity C‐reactive protein), modified single components from the ATP Ⅲ criteria for metabolic syndrome (hypertension, diabetes, high triglycerides, and low HDL cholesterol), and metabolic syndrome were examined.
Results
VAT mass was strongly correlated with BMI (r ≥ 0.77), WC (r ≥ 0.80), WHR (r ≥ 0.58), and WHtR (r ≥ 0.78). WC was the strongest predictor for VAT (area under the curve: 0.90). Compared to anthropometric measures, the associations between VAT and metabolic syndrome as well as single components of metabolic syndrome were statistically significantly stronger, but the clinical differences were likely minor.
Conclusion
Although VAT mass showed statistically stronger associations with cardiometabolic risk compared to traditional anthropometrics, the clinical importance was likely small. Simple, clinically available tools seem to satisfactory substitute for VAT to identify cardiometabolic risk.
Keywords: cardiometabolic health, dual energy x‐ray absorptiometry, obesity, overweight, population studies, visceral adipose tissue
1. INTRODUCTION
The global obesity prevalence has tripled in the last 4 decades, and more than 2.8 million deaths per year can be attributed to overweight and obesity.1 Simultaneously, in high‐income countries, there has been a decline in other cardiometabolic risk factors including total cholesterol2 and blood pressure,3 and in the overall burden of cardiovascular disease.4, 5, 6 This paradox questions whether the current definition of overweight and obesity properly identifies cardiometabolic risk.
Traditionally, overweight and obesity are categorized by simple clinically available anthropometric measures including body mass index (BMI) or waist circumference (WC). The relevance of BMI has been questioned,7, 8 and WC has its limitations related to measurement error, that is, correct placement of measurement tape. Other measures, hypothesized to be more accurate in defining obesity compared to BMI and WC, are waist‐to‐hip ratio (WHR) and waist‐to‐height ratio (WHtR).9, 10 However, none of these measures distinguish fat mass from fat‐free mass, thus do not directly address the definition of overweight and obesity as “abnormal or excessive fat accumulation that may impair health.”1
Magnetic resonance imaging (MRI) and computed tomography (CT) are considered the most accurate assessment tools of body composition; however, they are resource demanding.11 Visceral adipose tissue (VAT) from dual‐energy x‐ray absorptiometry (DXA) is highly correlated with the corresponding measures from MRI and CT.12, 13 VAT, located intra‐abdominally and around the organs, is more metabolically active than subcutaneous fat and is linked to insulin resistance, metabolic syndrome, cardiovascular disease, and several types of cancer.14 Therefore, the current study hypothesized that DXA‐derived VAT might be a clinically more important marker than anthropometric measures when investigating the association between body composition and cardiometabolic disease risk. How DXA‐derived VAT performs against anthropometric measures in the association with cardiometabolic risk factors is currently unknown, as the most previous studies investigating such differences used other measurement methods to derive VAT.15, 16, 17, 18, 19, 20
The aim of this study was to investigate whether DXA‐derived VAT is more strongly associated with cardiometabolic risk than traditional anthropometric measures, using a large population‐based sample of middle‐aged and older adults.
2. MATERIAL AND METHODS
2.1. Sample
The Tromsø Study21 is an ongoing population‐based study consisting of seven surveys (Tromsø 1–7) conducted from 1974 to 2016, inviting large representative samples of the population in the Tromsø municipality in Norway. In the seventh survey (2015–2016), all inhabitants, 40 years and older, were invited (n = 32,591). A selected sub‐sample (n = 13,028) was invited to extended examinations about 2 weeks after attending the basic examination. This sub‐sample included a randomized sample (n = 9925) in addition to participants previously attending DXA, echocardiogram, and eye examinations in Tromsø 6 (2007–2008) (n = 3103). A total of 21,083 (65%) participants aged 40–99 years attended the basic examination, and 8346 attended the extended examinations (of those attending extended examinations, this equaled 64% of the initially selected sub‐sample). Among those attending basic examinations, 5232 participants were invited to DXA scans and 3683 (70%) attended whole‐body DXA scans. Eight participants were excluded because of incorrect placement in the DXA machine, resulting in the CoreScan application being unable to calculate VAT in the abdominal area. Therefore, 3675 participants with VAT measures were included in the analysis (Figure 1).
FIGURE 1.
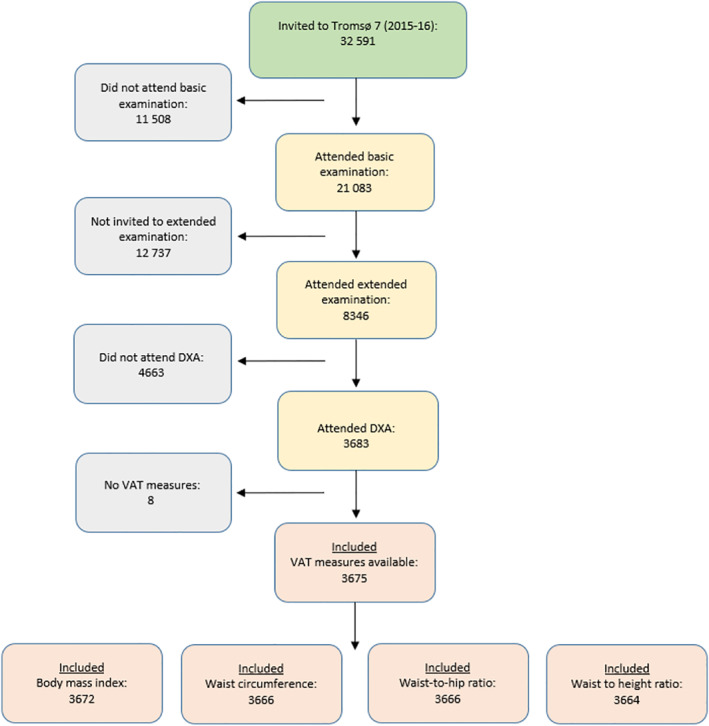
Inclusion of study participants: The Tromsø Study 2015–2016. DXA, dual‐energy x‐ray absorptiometry; VAT, visceral adipose tissue
This project was approved by the Regional Committee for Medical Research Ethics (REC North ref. 2017/1967), and all participants gave written informed consent.
2.2. Cardiometabolic risk factors and metabolic syndrome components
Information about self‐reported diabetes, use of antidiabetics (insulin or tablets), lipid‐lowering drugs, and antihypertensives from self‐administered questionnaires was included. Trained technicians performed all examinations using standard protocols. Non‐fasting blood samples were analyzed at the Department of Laboratory Medicine at the University Hospital of North Norway (ISO certification NS‐EN ISO 15189:2012) for total cholesterol (mmol/L), high‐density lipoprotein (HDL) cholesterol (mmol/L), triglycerides (mmol/L), high‐sensitivity C‐reactive protein (hs‐CRP, mg/L), and glycated hemoglobin (HbA1c, %). Systolic and diastolic blood pressures were measured three times with 2‐min intervals with a Dinamap ProCare 300 monitor (GE Healthcare), and the mean of the two last readings was used in the analyses. Single cardiometabolic risk factors (WC and fasting glucose excluded) were defined based on the National Cholesterol Education Program Adult Treatment Panel Ⅲ (NCEP ATP III) diagnostic components for the metabolic syndrome (2005 revision)22: hypertension (systolic blood pressure >130 mmHg and/or diastolic blood pressure >85 mmHg and/or use of antihypertensives) (n: 2498 [57% women]), high non‐fasting triglycerides (triglycerides ≥1.7 mmol/L and/or use of lipid‐lowering drugs) (n: 1659 [52% women]), low HDL cholesterol (HDL cholesterol <1.3 [women] or <1.0 [men] mmol/L and/or use of lipid‐lowering drugs) (n: 1164 [57% women]), and diabetes (self‐reported diabetes and/or HbA1c ≥ 6.5% and/or use of antidiabetics) (n: 311 [54% women]). Metabolic syndrome (MetS) was defined as the presence of three or more of the metabolic syndrome components presented above, as defined by NCEP ATP III (n: 493 [24%] women and 406 [28%] men). Waist circumference was excluded from the definition of MetS because it was included in the study for comparison to VAT.
2.3. Measures of adiposity
Body weight and height were measured with light clothing and no shoes to the nearest 0.1 kg and nearest 0.1 cm, respectively, using a Jenix DS‐102 height and weight scale (DongSahn Jenix). BMI was calculated as weight divided by height squared (kg/m2). WC and hip circumference were measured to the nearest 0.1 cm with a Seca measurement tape at the level of the umbilicus and the greater trochanters, respectively. BMI, WC, WHR (WC divided by hip circumference, cm/cm), and WHtR (WC divided by height, cm/cm) were included as continuous variables for association with VAT.
Whole‐body DXA scans were performed with a Lunar Prodigy Advance (GE Healthcare) according to guidelines from the manufacturer, and trained technicians inspected the post‐scan images. The DXA device was calibrated each morning with a phantom before starting measurements. The CoreScan application (EnCore version 17.0) was used to compute VAT from DXA scans, and VAT in grams (g) and volume (cm3) were included. Both VAT volume and VATindex (VAT [g] divided by height squared [g/m2]) were highly correlated (r: 1.00 and 0.99, respectively) with VAT mass (g). Therefore, only VAT mass was included for further analyses in the present study.
2.4. Statistical analyses
The software of the DXA machine is not sensitive enough to detect extremely low VAT values. Thus, we chose to transform VAT mass with values of 0 (n = 10) into the lowest value (2 g) measured in the overall sample. Descriptive analyses, Student's t‐test for comparison of means, and Wilcoxon rank‐sum test for comparison of median were used to present the study population characteristics (Table 1). To display the correlation between VAT and anthropometric measures, Pearson's correlation coefficients (r) in 10‐year age groups were presented (Table 2). Age‐adjusted partial correlations were used to investigate correlations between VAT, anthropometric measures, and cardiometabolic risk factors (Table 3). Although the cross‐sectional design of this study makes it difficult to establish causal pathways, receiver operating characteristics (ROC) analyses were performed to investigate the ability of VAT and anthropometric measures to predict MetS and single metabolic syndrome components (Figure 2). Area under the curves (AUCs) with confidence intervals (CIs) are presented. In addition, c‐statistics was applied to compare the age‐adjusted AUCs between VAT mass and the anthropometric variables in predicting MetS and single metabolic syndrome components (Table 4). Finally, to investigate which of the anthropometric measures that best predict VAT, VAT was dichotomized in two groups (at median), and the results from ROC analysis of VAT in relation to BMI, WC, WHR, and WHtR are presented (Figure 3). All analyses were performed separately in women and men. STATA 14 (STATA Corp LP) was used for all analyses.
TABLE 1.
Descriptive of study population attending part 2: The Tromsø Study 2015–2016
| Women (n = 2152) | Men (n = 1523) | p‐value | |
|---|---|---|---|
| Age (years) | 66.2 (8.92) | 65.9 (9.13) | 0.35 |
| 40–49 | 5.95 (128) | 6.70 (102) | 0.54 |
| 50–59 | 13.2 (284) | 12.3 (187) | 0.55 |
| 60–69 | 43.3 (932) | 47.4 (722) | 0.46 |
| 70–79 | 32.1 (691) | 27.5 (418) | 0.21 |
| 80+ | 5.44 (117) | 6.17 (94) | 0.36 |
| Weight (kg) | 71.3 (13.0) | 86.0 (13.2) | <0.001 |
| Height (cm) | 163.0 (6.25) | 176.4 (6.70) | <0.001 |
| BMI (kg/m2) | 26.8 (4.70) | 27.6 (3.72) | <0.001 |
| Waist (cm) | 91.2 (12.4) | 100.5 (10.5) | <0.001 |
| WHR (cm/cm) | 0.88 (0.08) | 0.97 (0.07) | <0.001 |
| WHtR (cm/cm) | 0.56 (0.08) | 0.57 (0.06) | <0.001 |
| VAT (g)—mean (SD) | 936.7 (632.5) | 1660.9 (876.6) | <0.001 |
| VAT (g)—median (25p–75p) | 832 (444–1302.5) | 1578 (1004–2222) | <0.001 |
| Hypertension (%[N]) | 66.2 (1415) | 71.7 (1083) | <0.001 |
| Diabetes (%[N]) | 8.05 (168) | 9.67 (143) | 0.09 |
| High triglycerides (%[N]) | 41.1 (864) | 53.1 (795) | <0.001 |
| Low HDL cholesterol (%[N]) | 31.7 (666) | 33.5 (498) | 0.97 |
| Metabolic syndrome (%[N]) | 24.0 (493) | 27.8 (406) | 0.01 |
Notes: Presented as proportion (n) or mean (SD). VAT mass is also presented as median with 25‐75% percentile. Student's t‐test was used to compare means and Wilcoxon rank‐sum was used to compare medians. Chi‐square test was used to compare proportions.
Among participants categorized as having low HDL (666 women and 498 men), 395 (59%) women and 351 (71%) was due to use of lipid‐lowering medication, not low HDL levels <1.3 (women) or <1.0 (men).
There are minor differences in number of participants according to different variables included.
Abbreviations: BMI, body mass index; VAT, visceral adipose tissue; SD, standard deviation; p, percentile; WHR, waist‐to‐hip ratio; WHtR, waist‐to‐height ratio.
TABLE 2.
Pearson's correlation coefficients of VAT with anthropometrics in 10‐year age groups: The Tromsø Study 2015‐2016
| BMI (kg/m2) | WC (cm) | WHR (cm/cm) | WHtR (cm/cm) | |
|---|---|---|---|---|
| Women | 0.77 | 0.80 | 0.58 | 0.78 |
| 40–49 | 0.75 | 0.80 | 0.61 | 0.77 |
| 50–59 | 0.83 | 0.84 | 0.64 | 0.83 |
| 60–69 | 0.76 | 0.80 | 0.58 | 0.78 |
| 70–79 | 0.77 | 0.79 | 0.53 | 0.76 |
| 80+ | 0.70 | 0.69 | 0.43 | 0.60 |
| Men | 0.78 | 0.82 | 0.69 | 0.79 |
| 40–49 | 0.87 | 0.88 | 0.64 | 0.85 |
| 50–59 | 0.74 | 0.79 | 0.70 | 0.77 |
| 60–69 | 0.81 | 0.84 | 0.72 | 0.79 |
| 70–79 | 0.78 | 0.79 | 0.64 | 0.76 |
| 80+ | 0.73 | 0.81 | 0.63 | 0.76 |
Note: All associations were significant with p‐value <0.001.
Abbreviations: BMI, body mass index; VAT, visceral adipose tissue; WC, waist circumference; WHR, waist‐to‐hip ratio; WHtR, waist‐to‐height ratio.
TABLE 3.
Partial* correlations between VAT, BMI, WC, WHR, WHtR, and cardiometabolic risk factors. The Tromsø Study 2015–2016
| Women | VAT (g) | BMI (kg/m2) | WC (cm) | WHR (cm/cm) | WHtR (cm/cm) |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 0.12 | 0.15 | 0.15 | 0.12 | 0.16 |
| Diastolic blood pressure (mmHg) | 0.08 | 0.07 | 0.09 | 0.08 | 0.08 |
| Triglycerides (mmol/L) | 0.44 | 0.33 | 0.37 | 0.33 | 0.29 |
| Total cholesterol (mmol/L) | −0.006 | −0.01 | −0.02 | 0.006 | −0.02 |
| HDL cholesterol (mmol/L) | −0.43 | −0.36 | −0.37 | −0.29 | −0.39 |
| HbA1c (%) | 0.24 | 0.16 | 0.19 | 0.17 | 0.20 |
| hs‐CRP (mg/L) | 0.14 | 0.16 | 0.14 | 0.09 | 0.16 |
| Men | VAT (g) | BMI (kg/m2) | WC (cm) | WHR (cm/cm) | WHtR (cm/cm) |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 0.11 | 0.09 | 0.10 | 0.08 | 0.10 |
| Diastolic blood pressure (mmHg) | 0.13 | 0.10 | 0.12 | 0.10 | 0.09 |
| Triglycerides (mmol/L) | 0.38 | 0.30 | 0.31 | 0.31 | 0.27 |
| Total cholesterol (mmol/L) | −0.02 | −0.009 | −0.009 | −0.02 | −0.004 |
| HDL cholesterol (mmol/L) | −0.38 | −0.34 | −0.36 | −0.31 | −0.34 |
| HbA1c (%) | 0.27 | 0.23 | 0.23 | 0.24 | 0.26 |
| hs‐CRP (mg/L) | 0.08 | 0.08 | 0.10 | 0.12 | 0.10 |
Note: All correlations, were significant <0.001, except for total cholesterol (p‐value: 0.41–0.80 and 0.33–0.88 in women and men, respectively).
Abbreviations: BMI, body mass index (kg/m2); HDL, high‐density lipoprotein; hs‐CRP, high‐sensitivity C‐reactive protein; mmol, millimole; mmHg, millimeters of mercury; VAT, visceral adipose tissue; WC, waist circumference; WHR, waist‐to‐hip ratio; WHtR, waist‐to‐height ratio.
*Age‐adjusted.
FIGURE 2.
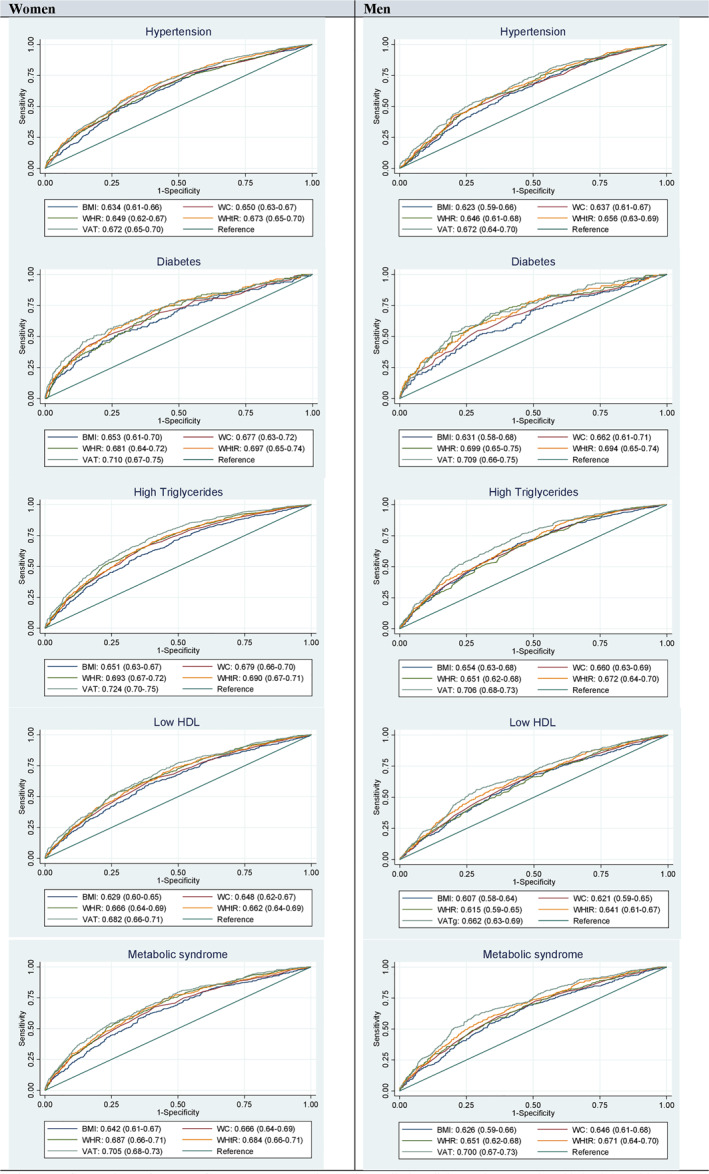
Comparison of BMI, WC, WHR, WHtR, and VAT in predicting diabetes, hypertension, high triglycerides, and low HDL cholesterol: The Tromsø Study 2015–2016. BMI, body mass index; HDL, high‐density lipoprotein; VAT, visceral adipose tissue; WC, waist circumference; WHR, waist‐to‐hip ratio; WHtR, waist‐to‐height ratio
TABLE 4.
AUC in women and men in different age adjusted models and c‐statistics comparison between models with VAT and models with anthropometric measures. The Tromsø Study 2015–2016
| Model 1 VAT (g) | Model 2 BMI (kg/m2) | P | Model 3 WC (cm) | P | Model 4 WHR (cm/cm) | P | Model 5 WHtR (cm/cm) | P | |
|---|---|---|---|---|---|---|---|---|---|
| Women | |||||||||
| Hypertension | 0.774 (0.75–0.79) | 0.775 (0.75–0.80) | 0.72 | 0.778 (0.76–0.80) | 0.29 | 0.777 (0.75–0.79) | 0.57 | 0.782 (0.76–0.80) | 0.07 |
| Diabetes | 0.722 (0.68–0.76) | 0.681 (0.64–0.72) | 0.001 | 0.700 (0.66–0.74) | 0.04 | 0.703 (0.66–0.74) | 0.20 | 0.711 (0.68–0.76) | 0.37 |
| High triglycerides | 0.729 (0.71–0.75) | 0.673 (0.65–0.70) | <0.001 | 0.695 (0.67–0.72) | <0.001 | 0.706 (0.68–0.73) | 0.006 | 0.700 (0.68–0.72) | <0.001 |
| Low HDL | 0.691 (0.67–0.71) | 0.655 (0.63–0.68) | <0.001 | 0.667 (0.64–0.69) | <0.001 | 0.679 (0.65–0.70) | 0.17 | 0.674 (0.65–0.70) | 0.02 |
| Metabolic syndrome | 0.728 (0.70–0.75) | 0.693 (0.67–0.72) | <0.001 | 0.706 (0.68–0.73) | <0.001 | 0.721 (0.70–0.75) | 0.37 | 0.715 (0.69–0.74) | 0.05 |
| Men | |||||||||
| Hypertension | 0.732 (0.70–0.76) | 0.718 (0.69–0.75) | 0.04 | 0.714 (0.68–0.74) | 0.005 | 0.713 (0.68–0.74) | 0.01 | 0.719 (0.69–0.75) | 0.05 |
| Diabetes | 0.752 (0.71–0.79) | 0.717 (0.67–0.76) | 0.002 | 0.726 (0.68–0.77) | 0.01 | 0.750 (0.71–0.79) | 0.90 | 0.741 (0.70–0.78) | 0.32 |
| High triglycerides | 0.707 (0.68–0.73) | 0.663 (0.64–0.69) | <0.001 | 0.663 (0.64–0.69) | <0.001 | 0.653 (0.63–0.68) | <0.001 | 0.673 (0.65–0.70) | <0.001 |
| Low HDL | 0.699 (0.67–0.73) | 0.681 (0.65–0.71) | 0.01 | 0.675 (0.65–0.70) | <0.001 | 0.676 (0.65–0.70) | 0.006 | 0.683 (0.65–0.71) | 0.03 |
| Metabolic syndrome | 0.753 (0.73–0.78) | 0.725 (0.70–0.75) | 0.001 | 0.723 (0.69–0.75) | <0.001 | 0.727 (0.70–0.76) | 0.002 | 0.731 (0.70–0.76) | 0.003 |
Notes: Model 1: age and grams of visceral adipose tissue, Model 2: age and body mass index, Model 3: age and waist circumference, Model 4: age and waist‐to‐hip ratio, Model 5: age and waist‐to‐height ratio. Numbers indicating AUC for the model.
P: p‐Value from C‐statistics by comparing to the model with VAT and age (Model 1).
CI for VAT changed slightly between comparisons of different anthropometrics due to small variations in N.
Abbreviations: BMI, body mass index (kg/m2); HDL, high‐density lipoprotein; VAT, visceral adipose tissue; WC, waist circumference; WHR, waist‐to‐hip ratio; WHtR, waist‐to‐height ratio.
FIGURE 3.
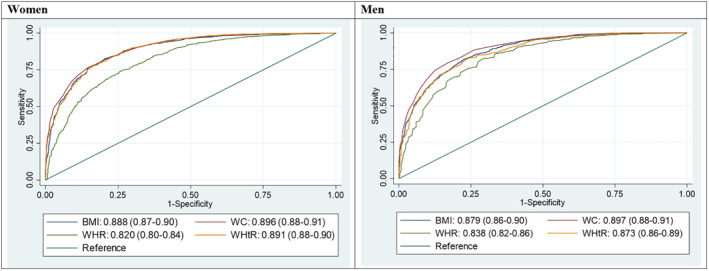
Comparison of VAT with anthropometric variables: The Tromsø Study 2015–2016. *VAT mas cut at median: women ≤832 or >832, men ≤1578 or >1578. BMI, body mass index; VAT, visceral adipose tissue; WC, waist circumference; WHR, waist‐to‐hip ratio; WHtR, waist‐to‐height ratio
3. RESULTS
Of the 3675 participants with whole‐body DXA scans, 3672, 3666, and 3664 also had valid BMI, WC/WHR, and WHtR measures, respectively (Figure 1). Mean age was similar in women and men (66.2 and 65.9 years, respectively). Men had higher mean values of VAT and anthropometric measures than women (Table 1). Mean values of BMI were in the overweight bracket for both women and men, and according to mean values of WC, women were at very high risk and men at high risk for cardiometabolic disease (Table 1). In women. 66% had hypertension, 8% diabetes, 41% high triglycerides, 32% low HDL cholesterol, and 24% had MetS. In men, 72% had hypertension, 10% diabetes, 53% high triglycerides, 34% low HDL cholesterol, and 28% had MetS (Table 1).
3.1. Correlations between VAT mass and anthropometric variables
Table 2 shows that the age‐specific correlations between VAT and the anthropometrics were all relatively high, although somewhat lower in women than in men, and lower in older adults. The strongest age‐specific correlations in both women and men were observed between VAT and WC (r: 0.69–0.84 and 0.79–0.88 in women and men, respectively) and the weakest correlation between VAT and WHR (r: 0.43–0.64 and r: 0.63–0.72 in women and men, respectively) (Table 2).
3.2. Associations with cardiometabolic risk, single metabolic syndrome components, and MetS
VAT and anthropometrics were consistently associated with all cardiometabolic risk factors (Table 3), except for total cholesterol. However, the correlations were low (r < 0.3) for most associations except for HDL cholesterol and triglycerides that were moderately correlated (both r: ≥0.3) to VAT and the anthropometric measures.
Based on the ROC analyses (Figure 2), VAT was not superior to the anthropometric variables in predicting hypertension or diabetes in women nor men, nor low HDL cholesterol in men. VAT was a stronger predictor for high triglycerides than BMI (AUC 95% CI: 0.72 [0.70–0.75] vs. 0.65 [0.63–0.67] in women, and 0.71 [0.68–0.73] vs. 0.65 [0.63–0.68]) in men). Also, VAT was a stronger predictor than BMI for low HDL cholesterol in women (AUC 95% CI: 0.68 [0.66–0.71] vs. 0.63 [0.60–0.65]). For prediction of MetS, VAT was stronger than BMI in both women and men (AUC 95% CI: 0.71 [0.68–0.73] vs. 0.64 [0.61–0.67] in women, and 0.70 [0.67–0.73] vs. 0.63 [0.59–‐0.66]) in men).
Comparison of AUCs between age‐adjusted models with VAT and age‐adjusted models with anthropometrics showed that VAT was a stronger predictor than all anthropometric measures (although only borderline significantly better than WHtR) to predict hypertension in men (Table 4). To predict diabetes, VAT was significantly stronger than BMI and WC in both men and women. VAT was significantly stronger than all anthropometrics to predict high triglycerides in both women and men (Table 4). In the prediction of low HDL cholesterol, VAT was stronger than BMI, WC, and WHtR in women and stronger than all anthropometrics in men. Finally, to predict MetS, VAT was in women stronger than BMI and WC, and borderline significantly stronger than WHtR. In men, VAT was stronger than all anthropometrics in the prediction of MetS (Table 4).
3.3. Associations between the different anthropometric parameters with VAT mass
The ROC curves in Figure 3 show that all anthropometrics were strong predictors of VAT (AUC > 0.80). WC was the strongest predictor (AUC: 0.90), while the AUCs for WHR were the weakest (0.82 and 0.84, in women and men, respectively).
4. DISCUSSION
In this analysis of 3675 middle‐aged and older adults, we found that VAT was moderately to strongly correlated with all included anthropometric measures. The correlation between DXA‐derived VAT measures and anthropometric measures is well established,23, 24, 25 but previous studies include narrower age ranges (29–55 years)20, 23, 25 or smaller samples (81–939 participants).12, 20, 23, 24 Thus, together with the additional ROC analysis and comparison with MetS and single metabolic syndrome components, the current study is an important contribution for establishing if DXA‐derived VAT has clinical importance over and above traditional anthropometric risk factors to predict cardiometabolic risk. The association between anthropometric measures and VAT derived from CT or MRI,16, 19, 26, 27 ultrasound,15 and bioelectrical impedance17, 18 has previously been investigated. Although CT and MRI are considered the most accurate techniques to quantify body composition, neither are suitable for population studies,11 and because DXA‐derived VAT is highly correlated with VAT measured by CT and MRI, it is considered a preferable substitute for the more resource‐demanding measures.12, 13
The presented ROC curves showed that among the anthropometric measures, WC had the strongest association with VAT; however, no other studies confirming this result were found. A previous study using DXA found that WHtR was the best anthropometric predictor for VAT, although closely followed by WC.20 However, this study was based on a small sample (n = 81) with younger participants (mean age = 38.4) than the present study, which makes comparison challenging.20 The high correlation between VAT and WC is considered as reasonable, as they are both measures from approximately the same area in the abdominal region. However, all anthropometric measures were considered strong predictors of VAT with high AUCs (≥0.82), and it is reasonable to assume that they all serve as satisfactory substitutes for VAT.
Although the correlations between VAT and all anthropometrics were overall moderate to strong, they were weakest in the oldest age group. This might be explained by changes in body composition with increasing age, where VAT mass increases relative to the abdominal subcutaneous fat mass.28, 29 It has been observed that subcutaneous fat decreases rapidly after the age of 70 years, while VAT does not have the same steep decline.30 Additionally, WC has been reported to be a satisfactory surrogate for VAT in adults, but not in older adults.19 The age difference in body composition could potentially be explained by the change in sex hormones and in physical activity levels among the elderly.19 Thus, conventional anthropometric measurements might not properly capture the changes in body composition that occurs with increasing age. This emphasizes the need for more accurate adiposity measurements in the older age groups.
VAT mass and anthropometric measures had similar associations and correlations to the cardiometabolic risk factors. The correlations were higher for triglycerides and HDL cholesterol compared to the other cardiometabolic risk factors. Although VAT was statistically significantly better than anthropometrics in the prediction of single metabolic risk factor components and MetS, the clinical differences were likely minor given the similar AUCs. Thus, the anthropometric measures are considered as satisfactory substitutes for VAT.
VAT was more strongly associated with high triglycerides compared to the anthropometric measures, which corresponds to the findings from a previous study.23 Although VAT AUCs were significantly higher for several of the single metabolic syndrome components and MetS (Table 4), the clinical differences are likely small given the proximity between AUCs for VAT and anthropometric variables (e.g., the lowest AUC for MetS was 0.642 for BMI compared to 0.705 for VAT in women). Although VAT is statistically more accurate, the more accessible and less resource‐demanding clinical measurements show similar predictive abilities of cardiometabolic risk factors and metabolic syndrome components. Longitudinal study designs and intervention studies are needed to investigate the potential differences between VAT and anthropometric measures and their association with incidence of metabolic syndrome and cardiometabolic disease.
4.1. Strength and limitations
There are several strengths of this study. First, a large population‐based sample with a wide age range of adults and older women and men was included. Second, all examinations and all definitions in the current analysis are performed and created by standard criteria, thus enabling comparison with future studies. Further, when performing DXA scans, the technicians were given standardized training and used protocols according to the manufacturer's recommendation. Also, all scans were inspected post‐measurement, and regions of interest were adjusted to ensure standardization between participants. However, measurement error in DXA scans is a potential limitation.31 The accuracy of VAT measured by DXA decreases with increasing BMI.31 As about 46% and 22% of our study sample were overweight and obese, respectively, a measurement error may occur and is difficult to detect. Another limitation is that the cross‐sectional design limits our possibility to study whether anthropometric measures are equally good as VAT to predict future health.
5. CONCLUSION
VAT mass showed moderate to high correlations with all included anthropometric measures. The strongest association was observed between VAT and WC. Although VAT was a statistically more accurate predictor of single metabolic syndrome components and MetS, the clinical difference compared to the anthropometric variables was small given the similar AUCs. The conclusion from this study is that anthropometric measures are satisfactory substitutes to VAT in identifying cardiometabolic risk.
CONFLICT OF INTEREST
The authors have no competing interests.
AUTHOR CONTRIBUTIONS
Marie W. Lundblad analyzed the data. Marie W. Lundblad, Bjarne K. Jacobsen, Jonas Johansson, and Laila A. Hopstock interpreted the results. Bjarne K. Jacobsen, Jonas Johansson, Lene F. Andersen, and Laila A. Hopstock were responsible for supervision. Sameline Grimsgaard and Laila A. Hopstock were responsible for the conceptualization, funding acquisition, and resources. Laila A. Hopstock administered the project. All authors were involved in writing and reviewing the paper and had final approval of the submitted version.
ACKNOWLEDGEMENTS
We are grateful to all study participants and the staff responsible for data collection.
Lundblad MW, Jacobsen BK, Johansson J, Grimsgaard S, Andersen LF, Hopstock LA. Anthropometric measures are satisfactory substitutes for the DXA‐derived visceral adipose tissue in the association with cardiometabolic risk—The Tromsø Study 2015–2016. Obes Sci Pract. 2021;7(5):525‐534. doi: 10.1002/osp4.517
REFERENCES
- 1.World Health Organization. Obesity and Overweight 2020. https://www.who.int/news‐room/fact‐sheets/detail/obesity‐and‐overweight. Accessed April 18, 2020. [Google Scholar]
- 2.Farzadfar F, Finucane MM, Danaei G, et al. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country‐years and 3·0 million participants. Lancet. 2011;377(9765):578‐586. [DOI] [PubMed] [Google Scholar]
- 3.NCD Risk Factor Collaboration . Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population‐based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joseph P, Leong D, McKee M, et al. Reducing the global burden of cardiovascular disease, Part 1. Circ Res. 2017;121(6):677‐694. [DOI] [PubMed] [Google Scholar]
- 5.Mensah GA, Wei GS, Sorlie PD, et al. Decline in cardiovascular mortality. Circ Res. 2017;120(2):366‐380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nuttall FQ. Body mass index. Nutr Today. 2015;50(3):117‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001;2(3):141‐147. [DOI] [PubMed] [Google Scholar]
- 9.Ashwell M, Gibson S. Waist‐to‐height ratio as an indicator of ‘early health risk’: simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open. 2016;6(3):e010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashwell M, Gunn P, Gibson S. Waist‐to‐height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta‐analysis. Obes Rev. 2012;13(3):275‐286. [DOI] [PubMed] [Google Scholar]
- 11.Lohman TML. ACSM's Body Composition Assessment. Human Kinetics; 2019. [Google Scholar]
- 12.Kaul S, Rothney MP, Peters DM, et al. Dual‐energy X‐ray absorptiometry for quantification of visceral fat. Obesity. 2012;20(6):1313‐1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheung AS, De Rooy C, Hoermann R, et al. Correlation of visceral adipose tissue measured by Lunar Prodigy dual X‐ray absorptiometry with MRI and CT in older men. Int J Obes. 2016;40(8):1325‐1328. [DOI] [PubMed] [Google Scholar]
- 14.Shuster A, Patlas M, Pinthus JH, Mourtzakis M. The clinical importance of visceral adiposity: a critical review of methods for visceral adipose tissue analysis. Br J Radiol. 2012;85(1009):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borruel S, Molto JF, Alpanes M, et al. Surrogate markers of visceral adiposity in young adults: waist circumference and body mass index are more accurate than waist hip ratio, model of adipose distribution and visceral adiposity index. PloS One. 2014;9(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Camhi SM, Bray GA, Bouchard C, et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity. 2011;19(2):402‐408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gadekar T, Dudeja P, Basu I, Vashisht S, Mukherji S. Correlation of visceral body fat with waist–hip ratio, waist circumference and body mass index in healthy adults: a cross sectional study. Med J Armed Forces India. 2018;76(1):41‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jabłonowska‐Lietz B, Wrzosek M, Włodarczyk M, Nowicka G. New indexes of body fat distribution, visceral adiposity index, body adiposity index, waist‐to‐height ratio, and metabolic disturbances in the obese. Kardiol Pol. 2017;75(11):1185‐1191. [DOI] [PubMed] [Google Scholar]
- 19.Ping Z, Pei X, Xia P, et al. Anthropometric indices as surrogates for estimating abdominal visceral and subcutaneous adipose tissue: a meta‐analysis with 16,129 participants. Diabetes Res Clin Pract. 2018;143:310‐319. [DOI] [PubMed] [Google Scholar]
- 20.Swainson MG, Batterham AM, Tsakirides C, Rutherford ZH, Hind K. Prediction of whole‐body fat percentage and visceral adipose tissue mass from five anthropometric variables. PloS One. 2017;12(5):e0177175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njølstad I. Cohort profile: the Tromso study. Int J Epidemiol. 2012;41(4):961‐967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2(5‐6):231‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miazgowski T, Kucharski R, Sołtysiak M, et al. Visceral fat reference values derived from healthy European men and women aged 20‐30 years using GE Healthcare dual‐energy x‐ray absorptiometry. PloS One. 2017;12(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rothney MP, Catapano AL, Xia J, et al. Abdominal visceral fat measurement using dual‐energy X‐ray: association with cardiometabolic risk factors. Obesity. 2013;21(9):1798‐1802. [DOI] [PubMed] [Google Scholar]
- 25.Vasan SK, Osmond C, Canoy D, et al. Comparison of regional fat measurements by dual‐energy X‐ray absorptiometry and conventional anthropometry and their association with markers of diabetes and cardiovascular disease risk. Int J Obes. 2018;42(4):850‐857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katzmarzyk PT, Heymsfield SB, Bouchard C. Clinical utility of visceral adipose tissue for the identification of cardiometabolic risk in white and African American adults. Am J Clin Nutr. 2013;97(3):480‐486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neamat‐Allah J, Wald D, Hüsing A, et al. Validation of anthropometric indices of adiposity against whole‐body magnetic resonance imaging–a study within the German European Prospective Investigation into Cancer and Nutrition (EPIC) cohorts. PloS One. 2014;9(3):e91586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marzetti E, Calvani R, Calvani R, et al. Sarcopenia: an overview. Aging Clin Exp Res. 2017;29(1):11‐17. [DOI] [PubMed] [Google Scholar]
- 29.Ponti F, Santoro A, Mercatelli D, et al. Aging and imaging assessment of body composition: from fat to facts. Front Endocrinol. 2019;10:861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Swainson MG, Batterham AM, Hind K. Age‐ and sex‐specific reference intervals for visceral fat mass in adults. Int J Obes. 2019;44(2):289‐296. [DOI] [PubMed] [Google Scholar]
- 31.Meredith‐Jones K, Haszard J, Stanger N, Taylor R. Precision of DXA‐derived visceral fat measurements in a large sample of adults of varying body size. Obesity. 2018;26(3):505‐512. [DOI] [PubMed] [Google Scholar]


