Abstract
Introduction and importance
Intestinal webs which are categorized under type-1 intestinal atresia rarely occur in the jejunum. These webs are occasionally diagnosed late because their central fenestration allows the passage of food.
Case presentation
We report a toddler who presented with atypical symptoms of bowel obstruction and non-specific plain radiograph and ultrasound findings. The diagnosis of jejunal obstruction was made possible with contrast-enhanced computed tomography and obstruction was found to be the result of a jejunal web at the surgery.
Clinical discussion
Few cases of jejunal webs are reported in the literature. The jejunum is the site of only 8% of webs and 33% of jejunal webs are associated with other congenital anomalies and/or prematurity.
Conclusion
Jejunal web needs a high degree of suspicion to be diagnosed and should be kept in mind as a differential diagnosis in the setting of unexplained persistent non-bilious emesis in otherwise normal toddlers.
Keywords: Bowel obstruction, Pediatric imaging, Jejunal web, CT-scan, Case report, Pediatric surgery
Highlights
-
•
Jejunum is the site of 8% of webs and 33% of jejunal webs are associated with other congenital anomalies and/or prematurity.
-
•
Jejunal webs may become only intermittently symptomatic because their central fenestration allows passage of food.
-
•
Vascular, Re-canalization, disrupted endodermal development and hyper-proliferation theories are proposed as their etiology
-
•
Intra-operative endoscopy for localizing and resection of jejunal webs is a new approach in the treatment of this entity.
1. Introduction
Intestinal atresias are historically divided into four types based on Louw and Barnard classification [1]: Type-1: intestinal webs, type-2: fibrous cord, type-3a: V-shaped mesenteric defect, type-3b: apple peel atresia, and type-4: multiple atresias. Type 1 intestinal atresia is considered to be rare and the most common site of webs is known to be the second part of the duodenum. The jejunum is the site of only 8% of webs [2].Vascular theory and Re-canalization theory have been proposed as the underlying etiologies of intestinal webs. However, a recent case report suggested that mucosal hyper-proliferation in a jejunal web might be another mechanism for intestinal web formation [3]. Jejunal webs often present in the neonatal period but may become only intermittently symptomatic or may present later in their life because their central fenestration allows passage of food. We present a case of jejunal web in a toddler with atypical symptoms of bowel obstruction. This case report has been reported following the SCARE criteria [4].
2. Case presentation
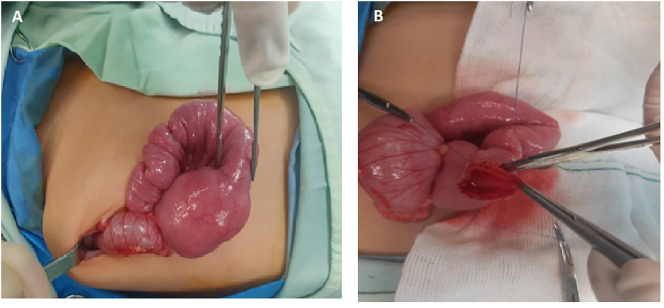
Our hospital exempts ethics approval for case reports. Written informed consent was obtained from the patient's parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request. A 2.5-year-old girl was admitted to our center with a history of intermittent non-bilious vomiting 2 months before admission. The patient's symptoms increased in frequency from two times a week to two times a day in a matter of a couple of months. She had normal defecation and a normal amount of gas passage. Her past medical, psychosocial, and drug history were unremarkable apart from the history of the cesarean section because of breech presentation. The patient came from an urban middle-class family without any history of genetic disorders. On clinical examination, abdominal distension was noted along with mild fullness in the epigastrium. No significant tenderness, signs of dehydration, or visible peristalsis was detected. Laboratory findings were unremarkable. On a plain abdominal radiograph, a fluid-filled distended stomach was present and the distal non-dilated bowel loops contained gas (Fig. 1-A). On ultrasound, dilation of the stomach and a few proximal small bowel loops was seen and the exam was otherwise normal (Fig. 1-B). On contrast-enhanced computed tomography the stomach and duodenum along with proximal jejunum were dilated up to 56 mm. Passage of oral contrast and existence of gas distal to the level of transition zone suggested high-grade partial obstruction of proximal jejunum. Mild thickening and hyper-enhancement of the jejunal mucosa were also identified at the level of obstruction (Fig. 2). Echocardiography which was performed to rule out concomitant congenital heart disease found to be unremarkable. The surgery was performed by an attending physician with 6 years of experience in pediatric surgery (M.G). During surgical exploration, duodenum and proximal jejunum appeared significantly dilated and a 4 mm thick web with a central perforation was identified at a 20 cm distance from the duodenojejunal flexure. The web was excised circumferentially and end-to-end anastomosis was performed without any immediate complications. The patient was discharged uneventfully. On pathologic examination, the excised segment consisted of a double layer of small intestinal mucosa separated by submucosa consistent with a jejunal web. The surgery was uneventful; the patient parents adhered to the post-surgery instructions and reported no adverse events. The child was nursed in lateral and low head position and was administered a single dose of an antiemetic. The patient was discharged two days later without any signs of post–intubation stridor. In the follow-up visit one week after the surgery, the patient's parents were fully satisfied with the result and reported no residual symptoms (Fig. 3).
Fig. 1.
A: Abdominal radiograph shows stomach (arrow) containing food material. No evidence of air-fluid level or intra-peritoneal gas is noted. B: Ultrasound image demonstrates a significantly distended stomach. (Arrow).
Fig. 2.
Coronal (A) and transverse (B) abdomen-pelvic CT images with oral and IV contrast show hugely distended stomach (arrow), duodenum (arrowhead) and proximal of jejunum (star) are present.
Fig. 3.
A: Transition zone and proximal dilated loop of jejunum B: Excision of the jejunal web.
3. Discussion
Jejunal web is an unusually encountered cause of bowel obstruction [5]. Vascular, Re-canalization, disrupted endodermal development such as mutations in Fgfr2IIIb, Fgf10, or Cdx2 genes and hyper-proliferation theories have been proposed as the etiology of intestinal webs in the literature [3]. The age at presentation and severity of symptoms depend on the location of the web as well as the presence or absence of a central fenestration and its size [1]. Presence of a central fenestration makes the diagnosis of the intestinal web delayed and challenging [6]. Presenting clinical features in delayed cases usually include failure to thrive and intermittent bilious vomiting [6]. A recent article has reported a case of the jejunal web becoming symptomatic only after foreign body entrapment at the age of 3 years [5]. Few cases of jejunal webs are reported in the literature. Lin et al. in their study on gastrointestinal webs demonstrated that the majority of intestinal webs were located in the second part of the duodenum. The jejunum was the site of only 8% of webs. No significant gender predilection existed. 33% of jejunal webs were associated with other congenital anomalies and/or prematurity. All the cases presented with bilious vomitus and all had abnormal ultrasound findings but only 67% had abnormal plain radiography [5]. Burjonrappa et al. on a study of 14 type-1 jejunoileal atresias found that 50% had associated anomalies, the majority of which were gastrointestinal and cardiac concomitant anomalies [7]. Table 1 summarizes the demographic data, associated conditions, clinical presentation, and outcome of patients that were reported as cases of jejunal web in the literature since 2000. Surgical excision is the treatment of choice in the case of the jejunal web and is performed with different approaches including intra-operative endoscopy for localizing and resection of the web [8].
Table 1.
Cases of jejunal web reported in the English literature since 2000.
| Author | Year | Gender | Age at presentation | History of prematurity/prenatal insults | Primary clinical presentation | Associated anomaly | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Yik Y.I (1) | 2019 | Male | 3y/o | None | Foreign body entrapment | None | Surgical excision | Complete recovery |
| Ssentongo P. (2) | 2018 | Female | 2y/o | None | Recurrent visible intestinal peristalsis/Failure to thrive | None | Surgical excision | Complete recovery |
| Afzal J. (3) | 2018 | Female | 8 m/o | None | Bilious vomit/Failure to thrive | Double jejunal webs/Midgut malrotation | Segmental resection/Ladd's procedure | Complete recovery |
| Sharma C (4) | 2017 | Male | 8 m/o | None | Intermittent bilious vomit | None | Surgical excision | Complete recovery |
| Male | 2y/o | None | Intermittent bilious vomit/Failure to thrive | None | Surgical excision | Complete recovery | ||
| Upadhaya V.D. (5) | 2016 | Male | 34w/o (gestational age) | Prematurity | Suspected intestinal atresia on antenatal scan/bilious aspirate | Bilateral hydroureteronephrosis | Surgical excision | Complete recovery |
| Tang Paula M.Y. (6) | 2015 | Male | 7d/o | None | Repeated undigested milk and bilious vomit | None | Surgical excision | Complete recovery |
| Hemant Janugade (7) | 2014 | Female | 2.5y/o | None | Abdominal distension/vomit/incomplete defecation/malnourishment | None | Surgical excision | Complete recovery |
| Rudolph B. (8) | 2012 | Female | 8d/o | None | Bilious vomit | None | Segmental resection | Complete recovery |
| Baba A.A (9) | 2010 | Male | 3d/o | None | Bilious vomit/No meconium passage since birth | Double jejunal web | Surgical excision | Delayed recovery |
| Seltz L.B. (10) | 2008 | Male | 13 m/o | None | Fever/Bilious vomit/Cough/Failure to thrive | None | Surgical excision | Complete recovery |
| Kothari P.R (11) | 2003 | Male | 4y/o | None | Intermittent bilious vomit/Failure to thrive/visible peristalsis | None | Surgical excision | Complete recovery |
Our patient presented atypically with a history of non-bilious emesis since 2 months ago. No history of prematurity, prenatal insults, or associated congenital anomalies existed. The only notable point of her history was a breech presentation. No typical sign of atresia including bilious emesis or failure to thrive was noted. Plain abdominal radiograph and ultrasound did not help make the diagnosis and the impression of jejunal obstruction was first suspected in contrast-enhanced CT scan and confirmed at surgery, where the web was excised.
4. Conclusion
Jejunal web which needs a high degree of suspicion to be diagnosed and in order to prevent complications should be kept in mind as a differential diagnosis in the setting of unexplained persistent non-bilious emesis in otherwise normal toddlers.
Ethical approval
Our hospital exempts ethics approval for case reports.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
S.K. designed the study. M.G. performed the surgery. A.B. and F.Z. performed the imaging studies. S.K., A.B. wrote the paper with input from all authors.
Guarantor
Fatemeh Zamani, MD
Research registration
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors declare that there is no conflict of interest.
References
- 1.Louw J., Barnard C. Congenital intestinal atresia observations on its origin. Lancet. 1955;266(6899):1065–1067. doi: 10.1016/s0140-6736(55)92852-x. [DOI] [PubMed] [Google Scholar]
- 2.Lin H.-H., Lee H.-C., Yeung C.-Y., Chan W.-T., Jiang C.-B., Sheu J.-C. Congenital webs of the gastrointestinal tract: 20 years of experience from a pediatric care teaching hospital in Taiwan. Pediatr. Neonatol. 2012;53(1):12–17. doi: 10.1016/j.pedneo.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Rudolph B., Ewart M., Levin T.L., Douglas L.C., Borenstein S.H., Thompson J.F. Mucosal hyperplasia in infant with jejunal web. J. Pediatr. Gastroenterol. Nutr. 2013;57(1):e2–e3. doi: 10.1097/MPG.0b013e3182638c1d. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Yik Y.I., How A.K. An unexpected encounter with jejunal web after foreign bodies entrapment in a toddler. Med J Malaysia. 2019;74(3):231–233. [PubMed] [Google Scholar]
- 6.Sharma C., Shah H., Waghmare M., Desale J., Dwivedi P. Delayed presentation of jejunal atresia. Dev. Period Med. 2017;21:95. doi: 10.34763/devperiodmed.20172102.9597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burjonrappa S.C., Crete E., Bouchard S. Prognostic factors in jejuno-ileal atresia. Pediatr. Surg. Int. 2009;25(9):795–798. doi: 10.1007/s00383-009-2422-y. [DOI] [PubMed] [Google Scholar]
- 8.De Backer T., Voet V., Vandenplas Y., Deconinck P. Simultaneous laparotomy and intraoperative endoscopy for the treatment of high jejunal membranous stenosis in a 1-year-old boy. Surg. Laparosc. Endosc. 1993;3(4):333–336. [PubMed] [Google Scholar]