Abstract
Background
Severe Mental Disorders (SMDs) affect multiple generations although this is poorly studied. The aim of this study was to investigate the intergenerational and multidimensional impacts of SMD in rural Ethiopia.
Methods
This comparative study was nested within an existing population-based cohort study. We collected data from a total 5762 family members of 532 households (266 households with at least one family member with SMD and 266 sex and age matched mentally well controls from the neighborhood) in 2019. The main outcomes were multidimensional poverty, mortality, food insecurity, and family satisfaction.
Findings
Multidimensional poverty Index was higher in the households of persons with SMD (74·44%) than the comparison households (38·35%). School attendance was lower in children of people with SMD (63·28%) than children of the comparisons (78·08%). The median years of schooling was also lower among children of people with SMD than the controls. This lower attendance was also true among siblings of people with SMD (35·52%) than the comparisons (49·33%). Over the course of 20 years, family members who have a person with SMD in their household had 23% increased risk of death compared to family members who did not have a person with SMD in their household. Severe food insecurity was also higher in the SMD households (20·68%) than the comparison (13·53%) while family satisfaction was lower.
Interpretation
Families of people with SMD experience pervasive multidimensional and intergenerational impacts. Interventions should consider the broader family social and healthcare needs of the broader family.
Keywords: Severe Mental Disorders, Multidimensional, Intergenerational impact, LMICs
Research in context.
Evidence before this study
We have published a systematic review searching from PubMed, PsycINFO, Embase and Global Index Medicus from the inception of each database up to 9 November 2019. We also did manual searches of gray literature. We combined terms for illness, terms for list of family members affected by the illness and terms for impact dimensions with the Boolean term AND.
We found that SMD had multidimensional impacts on the family, which included physical health problems, psychological difficulties, and socioeconomic drift. Impacts on children included higher mortality, poor school performance and nutritional problems.
The level of impact of the illness depends on patient related factors, family member-related factors and factors related to health service delivery. The other factors such as age of onset, duration of illness, number of hospitalizations and current functioning also predicted the level of impact. We have updated the search on 5th April 2021 and no new evidence were generated on the intergenerational impact of SMD.
Added value of this study
Though there was abundant evidence of the " subjective burden" associated with caring for a person with SMD, there were significant deficiencies on the multidimensional and intergenerational impacts of the illness. The available evidence is also concentrated in economically advanced countries. Moreover, most of the available studies lack comparison, and their quality is low. In this study, we demonstrate that the presence of SMD in the household is a risk factor for multidimensional poverty, higher mortality and low children's school enrollment and early dropout.
Implications of all the available evidence
Available family focused interventions mainly relate to psychoeducation. However, families of people with SMD suffer from pervasive multidimensional and intergenerational impacts. This indicates that inclusive and intergenerational interventions may be required for the achievement of the Sustainable Development Goals (SDGs).
Alt-text: Unlabelled box
1. Introduction
Severe Mental Disorders (SMDs; schizophrenia, bipolar disorder, and major depression) are disabling disorders with serious negative consequences extending to family members [1]. These consequences may be severe in resource-limited countries, where the treatment gap for mental disorders is very high [2] and family members take almost all the obligations of caring for the person with the illness [3].
The consequences are also long-lasting and multidimensional persisting even when the person with the illness is not living in the same household [4,5]. The extent of the burden is affected by patient related factors such as illness severity, premorbid personality, and premorbid economic status [6] and family-related factors such as family members' health, social support, economic status, and understanding of the illness and treatment options. The most commonly reported effects in the literature are psychological and financial burdens. Family members also report physical health problems, including increased risk for accident, arthritis, high blood pressure, gastric ulcers, and headaches [7,8].
The financial problems are related to disability, time spent for caregiving, difficulty keeping a job, and cost of treatment and treatment side effects [8,9]. The problems usually persist and result in decreased social class, chronic poverty, reduced living standards, and food insecurity [10,11].
The family members' social and marital relationships may also suffer. These are characterized by less social event participation, fewer marriages, higher divorce rate, poorer family cohesion, lower family satisfaction, and a strained family environment [12]. The illness of the family member will also affect their children and sibling's future [13]. The offspring may not get a chance to go to school, drop out early, or their performances may be poor, while the siblings cannot choose their own future such as time of marriage [14].
Though there is abundant evidence of the "burden" associated with caring for a person with SMD, the current care modality is highly centered on the person with the illness. Evidence is deficient on the multidimensional and intergenerational impacts of the illness. Moreover, most of the available studies lack comparison, and their quality is low [1]. In this study, we aimed to indicate whether the presence of SMD in the household is a risk factor for multidimensional poverty, higher mortality and children schooling. We also aimed to assess whether there is an association between food insecurity, family satisfaction, and the presence of SMD in a well-characterized sample from the Butajira community-based study on SMD [15,16].
2. Methods
This study adhered to STROBE (Strengthening the Reporting of OBservational Studies in Epidemiology) reporting guideline. We nested this comparative study within an existing population-based cohort on SMD in two predominantly rural districts of Meskan and Mareko, Southern Nations Nationalities and Peoples Region (SNNPR), Ethiopia. Participants (n = 919; 358 with schizophrenia, 346 with bipolar disorder, and 215 with major depression) were recruited between 1998 and 2001 through a population-based rigorous and structured double-stage screening of 68,368 respondents. First, screening was done with the Composite International Diagnostic Interview (CIDI) and community key-informants. Then confirmatory diagnostic assessment was done by trained clinicians using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) [15,16]. The data of the cohort can be accessed from AF with reasonable request.
2.1. Participants
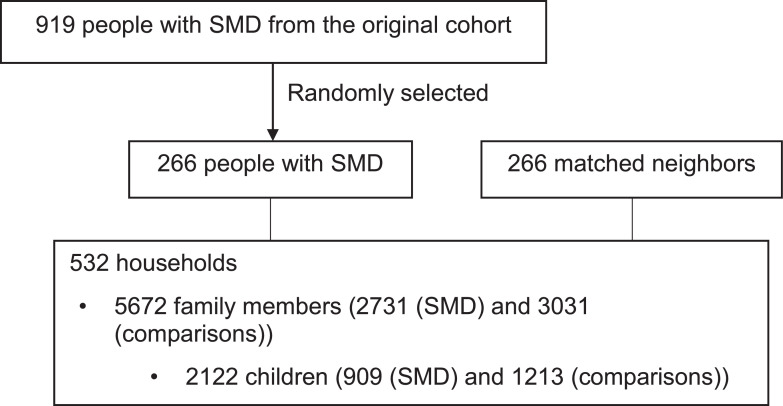
We selected 266 households randomly using computer generated numbers from the Butajira cohort and 266 sex and age (±5 years) matched neighboring households, which did not have a person with SMD. Since the comparisons were recruited for this particular study, we excluded households where a family has developed SMD after the establishment of the cohort (n = 2). We included households of people with SMD who died before the data collection (n = 37), but we have excluded households where more than one family member had SMD. We excluded these households to avoid the multiplicative effect of the problem. The comparison neighboring households were the closest match after turning anticlockwise from the index household (households with SMD) (Fig. 1). The clockwise turning was done after tossing a coin.
Fig. 1.
Participant selection procedure.
2.2. Outcomes
The primary outcomes were current multidimensional poverty (health, education and living standard; see below), and 20 years mortality while current food insecurity and family satisfaction were the secondary outcomes.
2.3. Measurements
Multidimensional Poverty Index (MPI): This is a measure of intensity and nature of poverty in three dimensions: health, education, and living standards with ten indicators. It was developed in 2010 by Oxford Poverty and Human Development Initiative (OPHI) and the United Nations Development Program (UNDP) Human Development Report. MPI is considered a better way of estimating poverty than other measures such as income and expenditure. It will be used as an indicator of the Sustainable Development Goals (SGDs) [17]. The measure has been modified in different settings. In Ethiopia, the assets include cattle and land, which is not the case in developed countries. Since this study was conducted through a family key informant, it was impossible to measure the nutritional status of each family member mainly due to their absence. The tool categorizes households into three groups: multidimensionally poor (deprivation in one-third of the indicators), severe poverty (deprived in half of the indicators), and vulnerable to poverty (deprivation in 20–33·3% of the indicators) [17]. We have reported both indicator specific and composite score reports. For the indicator specific report, we have calculated proportion of household level deprivation based on the recommendation of the UNDP. For the composite score analysis, we categorized households into two groups: multidimensionally poor (deprivation in one-third of the indicators or more) and not poor.
Mortality: We assessed mortality among family members and reasons for death with WHO verbal autopsy [18]. The tool helps to confirm death and cause death where physician confirmation of the cause of death is not possible. Earlier studies in the setting (Butajira district) showed a high ability of the tool to show probable causes of death where the sensetivity reaches up to 78% while the specificity reaches up to 98% [19].
Household food insecurity: We used the Household Food Insecurity Access Scale (HFIAS) to assess food insecurity. The tool has three domains: anxiety or uncertainty about food supply, insufficient quality of food (variety and preference), inadequate quantity of food supply, and the physical consequences of insufficiency [20]. It had been used and validated in different settings, including the current study setting [21]. We used an improved version of the tool with an added lead-in statement by Tirfessa et al. [10]. For the analysis, we categorized households into two groups: not severely food insecure (food secure, mildly food insecure, moderately food insecure) and severely food insecure.
The Family Satisfaction Scale (FSS) was used to assess key informants' satisfaction with household members' closeness, flexibility, and communication. The tool was developed based on the Circumplex Model, assuming that balanced levels of flexibility and cohesion are conducive to healthy family functioning [22]. It has ten items with five response levels (ranges from very dissatisfied to extremely satisfied) where a higher score shows better satisfaction. The tool has excellent psychometric properties in earlier studies [23]. Though it was not validated in Ethiopia, we have conducted transcultural adaptation which improved the understandability of the tool.
Life events: Presence or absence of threatening life events in the family was assessed with List of Threatening Experiences Questionnaire (LTE-Q). LTE-Q is a list of twelve stressful life events with yes/no responses such as: illness, bereavement, crime and legal events. Occurrence of one or more of these life events will be considered as a positive outcome [24].
Oslo Social Support Scale (OSSS-3) was used to measure actual and perceived social support. It had three items with 5-point scale in the first two items and 4-point scale for the last item. The sum score scale ranging from 3 to 14 where high score indicates better support [25].
2.4. Measurement adaptation and pre-test
Steps have included (1) systematic review [1], which helped identification of available measurement tools; (2) qualitative study for selection and modification of the measurement tools; (3) Expert meetings to finalize the selection of the measurements.
Then we supplied five days training for data collectors and coordinators. The training included detailed procedures for approaching each key informant and used role play to practice the interview. As part of the training, each data collector conducted two supervised interviews in the field. Lastly, we have also undertaken cognitive interviewing with 15 participants as part of the transcultural adaptation of FSS. In the cognitive interviewing, we asked the participant's understanding of the issue, how they mentally process it and respond to the concepts in the tool. We conducted transcultural adaptation of FSS because FSS was not adapted and some of the items were difficult to conceptualize in the study setting. We have changed the wording of item 8 and item 10 which improved the understandability of the tool. A pre-test was also done to assess the measures' overall understandability and familiarize the data collection team about the participant selection.
2.5. Method of data collection
One adult family key informant reported the household data. The informant was selected by the family members and considered as the one with better information about the family. In the pre-test phase, we involved more than one family member of the same household to check the consistency of the data across family key-informants. There were 100% agreement across the informants, and we continued the actual data collection with a single informant. With the participant's help, we drew up a detailed family tree and used this as a framework to inquire about each household and family member. The data collection procedure was similar in both groups.
2.6. Statistical analysis
We conducted either McNemar's test (MPI, mortality, food insecurity) or paired t-test (family satisfaction) to assess the association between SMD and the outcome of interest. We have checked normality of the data a priori with histogram and scatter plot. Negative binomial regression was used to determine the relationship between the number of deaths among family members and exposure to SMD after adjusting for crucial factors such as family size and major life events. Zero-inflated negative binomial regression was used to determine the relationship between schooling and exposure to a sibling or parental SMD after weighting for the number of school-aged children in the household. We used the Poisson working model to model prevalence ratio and to identify factors associated with multidimensional poverty. We also used Multivariable logistic regression to find factors associated with household food insecurity. Kaplan Meier curve were used to assess the differences in years of schooling among children and sibling of people with SMD and comparison.
2.7. Ethical consideration
We obtained ethical clearance from the Institutional Review Board of the College of Health Sciences, Addis Ababa University (Ref. No: AAUMF 03–008). The data collectors read the information sheet for all the participants before they signed or gave a fingerprint. We involved witness in the process when the participant was not able to read and write. In the information sheet, we have included statements about consent, confidentiality, and participants’ right to withdraw from the study at any time.
2.8. Role of funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
3. Results
3.1. Participant characteristics
We have collected data of 5762 family members from 532 households (out of 550 approached) through their key informants. Of the family members, 2122 were children of people with SMD and their comparisons, 2034 were siblings and the remaining were parents and spouses of people with SMD and their comparisons. There was no significant difference in the mean age of people with SMD (n = 266 (106 with Schizophrenia, 95 with bipolar disorder and 65 with Major depression)) and their comparison (n = 266) (44·81 (±9·57) vs 44·27 (±9·61)) (p-value=0.52). Only 51·13% of people with SMD were currently married while 81·95% of the comparisons were married (p-value<0·001) (Supporting information 1).
3.2. Key-informant characteristics
Two hundred eleven (39·66%) key informants were spouses of the person with SMD, 176 (33·08) were siblings, while the remaining were either parents or offspring. The household size ranged from 3 to 26 with a median (IQR) of 11 (8,16). The informants' age ranged from 25 to 77 years, with a median (IQR) of 40 (32, 50). More than half (53·57%) of the informants have attended formal education. There were no significant differences between the informants of the two groups in terms of educational status (p-value=0.35), age (p-value=0.21), and relationship (p-value=0.33).
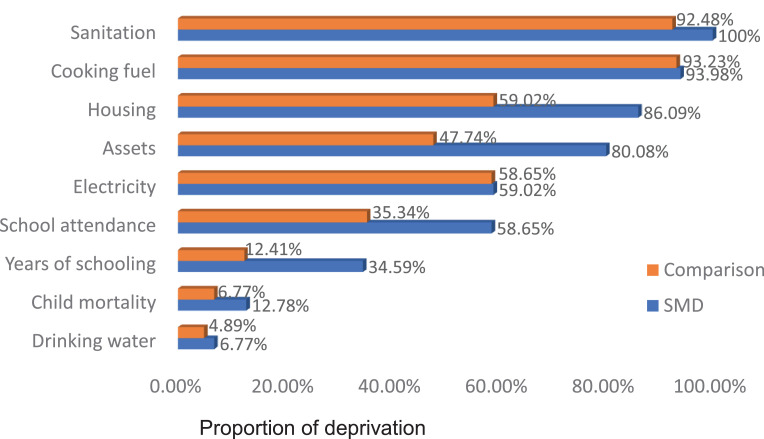
3.3. Multidimensional poverty (Household level)
Multidimensional poverty was significantly higher in the households of a person with SMD (74·44%) than the comparison group (38·35%) (p-value<0.001). This difference was statistically different in the five indicators of MPI (child mortality, years of schooling, school attendance, housing, and assets) (Fig. 2). Severe poverty was also higher in the exposed households (27·07%) than the non-exposed arm (5·64%) (p-value<0.001).
Fig. 2.
Proportion of households fulfilling specific poverty indicator of Multidimensional Poverty (SMD vs. comparison (n = 266 for each group).
The figure shows higher deprivation among households with SMD compared with the comparisons in five out of nine indicators of MPI. These included child mortality, years of schooling, school attendance, assets, and housing.
After adjusting for household head's (the head of the household where the person with SMD and the comparison lives) age, marital status, years of education, residence, family size, social support, and known medical problem among family members, households which contain a person with SMD had two times higher risk of experiencing multidimensional poverty compared to the comparison households (Table 1).
Table 1.
Associations of selected household characteristics with Multidimensional Poverty.
| Characteristics | CPR (95% CI) | APR (95% CI) |
|---|---|---|
| SMD (yes) | 1·94 (1·64, 2·30)⁎⁎ | 2·01 (1·69, 2·39)⁎⁎⁎ |
| Age (head of the household) | 1·00 (0·98, 1·01) | ·99 (0·99, 1·00) |
| Head of the household marital status (currently married) | 1·02 (0·88, 1·20) | 0·87 (0·74,1·03) |
| Years of education (household head) | ·96 (0·94, 0·98)⁎⁎⁎ | ·98 (0·96, 1·00) |
| Residence (urban) | ·71 (0·58, 0·86)⁎⁎ | ·81 (0·66, 0·98)* |
| Household size | 1·02 (1·01, 1·04)* | 1·02 (1·01, 1·04)* |
| Social support | ·96 (0·91, 0·99)* | ·97 (0·94, 0·99)* |
| Known medical problem (yes) | 1·16 (0·99, 1·35) | 1·01 (0·85,1·19) |
CPR: Crude Prevalence Ratio; APR: Adjusted Prevalence Ratio.
P-value<0·001.
P-value<0·01.
P-value<0·05.
4. Schooling
4.1. Children school attendance
Of 2122 children, 1660 were aged eight years and above during the data collection period. School attendance was lower in children of people with SMD (63·27%) than children of the comparisons (79·78%) (p-value<0.001). After weighting for school-aged children in the household and adjusting for important confounders, being in the SMD group, rural residence, smaller household size and lower social support were significantly associated with lower school attendance (Table 2).
Table 2.
Associations of selected variables with children not being enrolled to school.
| Characteristics | CPR (95% CI) | APR (95%CI) |
|---|---|---|
| SMD (yes) | 1·94 (1·64, 2·30)⁎⁎ | 2·01 (1·69, 2·39)⁎⁎⁎ |
| Age (head of the household) | 1·00 (0·98, 1·01) | ·99 (0·99, 1·00) |
| Head of the household marital status (currently not married) | 1·02 (0·88, 1·20) | ·87 (0·74,1·03) |
| Years of education (household head) | ·96 (0·94, 0·98)⁎⁎⁎ | ·98 (0·96, 1·00) |
| Residence (urban) | ·71 (0·58, 0·86)⁎⁎ | ·81 (0·66, 0·98)* |
| Household size | 1·02 (1·01, 1·04)* | 1·02 (1·01, 1·04)* |
| Social support | ·96 (0·91, 0·99)* | ·97 (0·94, 0·99)* |
| Known medical problem (yes) | 1·16 (0·99, 1·35) | 1·01 (0·85,1·19) |
| Threatening life events (yes) | 1·00 (0·81, 1·24) | ·92 (0·73, 1·16) |
CPR: Crude Prevalence Ratio; APR: Adjusted Prevalence Ratio.
P-value<0·001.
P-value<0·01.
P-value<0·05.
4.2. Children of years of schooling
Median grade at the time of dropout from school was also lower among children of people with SMD than the controls (6 (4, 8) vs. 7 (4, 10)) (p-value<0.01). Eighty-three percent of children of people with SMD dropped out before grade nine while it was 67% in children of the comparison. Only two percent children of people with SMD pass to the second tier of secondary school (11th,12th) compared with 11% in children of the comparisons (Supporting information 2). The grade of dropout is not associated with the children's sex (p-value=0.08) and age (p-value=0.12).
4.3. Sibling schooling
School attendance was lower among siblings of people with SMD (35·52%) than siblings of the comparisons (49·33%) (p-value<0.01). Sixty-five percent of the sibling of people with SMD dropped out before grade nine, while it was 52% in the comparison's sibling (p-value<0.01). Twelve percent siblings of people with SMD learn beyond grade 12 while 22% siblings of the comparison learn beyond grade 12 (Supporting information 3).
4.4. Mortality
This section of the study involved 5762 people (2731 in the SMD households and 3031 in the control households) involving parents, sibling, spouse, and children. Five hundred seventy-eight deaths reported since the establishment of the cohort (309 in the SMD group and 269 in the control group). Accident and acute illnesses were the most frequently mentioned causes of death. Suicide was reported as the cause of death in 6 SMD households and 3 comparison households. The mean age at death was 44·27 (±27·76) years in the SMD families and 45·17 (±27·16) years in the control families, which were not statistically different (p-value=0.21).
In multivariable analysis, mortality was significantly related to having a family member with SMD and higher number of family members (p-value=0.02). Family members who have a person with SMD in the household had a 23% increased risk of death than family members who did not have a person with SMD (Table 3).
Table 3.
Associations of selected household characteristics and mortality among family members in rural Ethiopia.
| Characteristics | CIRR (95% CI) | AIRR(95% CI) |
|---|---|---|
| SMD (yes) | 1·15(0·94, 1·40) | 1·23 (1·01, 1·49)* |
| Years of education (household head) | ·99 (0·96, 1·01) | ·99 (0·97, 1·02) |
| Residence (urban) | 1·01 (0·98, 1·01) | 1·05 (0·82, 1·34) |
| Household size | 1·08 (1·05, 1·10)⁎⁎⁎ | 1·08 (1·05, 1·10)⁎⁎⁎ |
| Food insecurity (yes) | 1·31 (1·01, 1·70)* | 1·16 (0·90, 1·49) |
| Social support | 1·00 (0·99, 1·01) | 1·00 (0·88, 1·01) |
CIRR: Crude Incidence Risk Ratio; AIRR: Adjusted Incidence Risk Ratio.
P-value<0·001.
P-value<0·05.
4.5. Food insecurity and family satisfaction
Ninety-one (17·1%) households fulfilled the criteria for severe food insecurity based on HFIAS. Food insecurity was significantly higher in the SMD households (20·68%) than in the controls (13·53%) (p-value=0.01). These unfavorable reports were true in all the nine items of HFIAS (Supporting information 4). In multivariable analysis (adjusting for household head's age, years of education, marital status, residence, family size, and social support), the odds to be severely food insecure in SMD households was 1·7 times higher than the controls (Table 4). The mean family satisfaction scale score was lower in households who have a person with SMD compared to the controls (P-value=0·01) (Supporting information 5).
Table 4.
Associations of selected household characteristics and food insecurity in rural Ethiopia.
| Characteristics | COR (95% CI) | AOR (95% CI) |
|---|---|---|
| SMD (yes) | 1·53 (1·04, 2·24)* | 1·67 (1·03, 2·75)* |
| Household head marital status (currently married) | ·99 (0·67, 1·48) | 1·20 (0·62, 1·91) |
| Age (household head) | ·97 (0·97, 1·01) | ·99 (0·98, 1·01) |
| Years of education (household head) | ·96 (0·92, 1·01) | ·95 (0·90, 1·02) |
| Household size | 1·04 (0·99, 1·09) | 1·07 (1·01, 1·14)* |
| Residence (urban) | 1·17 (0·78, 1·74) | ·67 (0·39, 1·14) |
| Social support | ·98 (0·95, 1·02) | 1·02 (0·89, 1·18) |
COR: Crude Odds Ratio; AOR: Adjusted Odds Ratio.
P-value<0·05.
5. Discussion
This study aimed to understand whether the presence of SMD in a household is a risk factor for multidimensional poverty and higher morality and to assess whether there is an association between food insecurity, family satisfaction, and the presence of SMD. Our results show that family members of people with SMD were more exposed to higher multidimensional poverty, greater mortality risk, more heightened food insecurity, and lower family satisfaction.
Our study is unique in many ways. Prior studies focused on exploring and describing the subjective (emotional) burden of the illness on the primary caregivers. In the current study, we report the impact of the illness on the household, all family members and across three generations to demonstrate the multidimensional and intergenerational impacts over many years. This was done in a well characterized cohort of people with SMD identified through a population-based study. Though we randomly selected 266 from 919 in the cohort, there were no significant differences in important variables (sex, age, living place and diagnosis). We have used matched control groups for comparison, which was done rarely in previous studies. Earlier studies mainly focused on schizophrenia and bipolar disorder, while our study also included severe depression. These are essential inputs to develop family-inclusive and potentially inter-generational interventions. The study also highlights the need for preventive inter-generational interventions.
The well-established social causation (poverty may result in mental illness) and social drift (mental illness pushes people into poverty) theories explain the relationship between mental illness and poverty [11]. Households with SMD report higher poverty levels, more exposure to food insecurity, and lower living standards [10,26]. The current study explains the dimensions of poverty using the Multidimensional Poverty Index (MPI) [17]. We find that MPI was two times higher in SMD households indicating that unless we critically consider strategies to mitigate the intergenerational and multidimensional impacts of SMD, we may fail to achieve the SDGs.
The finding about food insecurity is consistent with earlier studies where households with SMD experience more severe food insecurity [10,27]. This can be explained by disability, stigma, time spent on caregiving, and coping mechanisms [10,28]. This is a critical area for designing short and long-term interventions.
Our finding of a 23% increased risk of death among family members of all ages has not been reported. Weissman et al. [6] was the first to report higher mortality among children of people with severe depression than the controls over 30 years [3]. Mortality should be considered as an important target for future studies and intervention development.
Our results of lesser family satisfaction were also reported in high-income countries. We have not explored the cause for this but the general concern about the illness, each family member's role in the care process, and the cost of treatment may contribute [29,30].
Though we believe this study is an important input, the study had some limitations: (1) we did not measure one of the ten MPI dimensions (nutritional status) because our study was done through key informants. But it is important to note that the overall trend in this regard is very clear from our study; (2) Since we did not find a death certificate record, we may not get the precise cause of death, but we have used a locally validated verbal autopsy questionnaire. (3) As the study is based on 20 years of retrospective data, recall bias is likely in some variables. We have tried to make sure we obtained consistent information by involving multiple informants initially.
Our study shows that families of people with SMD suffer from pervasive multidimensional (mortality, multidimensional poverty, education, food insecurity and family satisfaction) and intergenerational (parents, sibling, spouse, and children) impacts. In low-income setting where there is no formal social welfare system, the impact is substantial. Interventions should consider the broader need of the family including education. Multidimensional poverty indicators are also prevalent among the control group. A broader poverty reduction intervention at the population level are needed.
Contributors
WF and AF conceived the study, and they were part of the whole process of the Study. WF and AF have access to raw data, and they are responsible for it. TKJC, DK and GM participated in the design of the study, reviewed all versions and made corrections. All the authors read and approved the final version.
Data sharing statement
The full dataset can be accessed from the corresponding author with reasonable request.
Declaration of Competing Interest
All authors have nothing to disclose
Funding
This work was supported through the DELTAS Africa Initiative (DEL-15–01). The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS) Alliance for Accelerating Excellence in Science in Africa and supported by the New Partnership for Africa's Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust (DEL-15–01) and the UK government. The views expressed in this publication are those of the author(s) and not necessarily those of AAS, NEPAD Agency, WellcomeTrust or the UK government. Original study funded by the Stanley Medical Research Institute. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2021.101151.
Appendix. Supplementary materials
References
- 1.Fekadu W., Mihiretu A., Craig T.K.J., Fekadu A. Multidimensional impact of severe mental illness on family members: systematic review. BMJ Open. 2019;9(12) doi: 10.1136/bmjopen-2019-032391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fekadu A., Medhin G., Lund C. The psychosis treatment gap and its consequences in rural Ethiopia. BMC Psychiatry. 2019;19(1):325. doi: 10.1186/s12888-019-2281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thornicroft G., Tansella M., Becker T. The personal impact of schizophrenia in Europe. Schizophr Res. 2004;69(2–3):125–132. doi: 10.1016/s0920-9964(03)00191-9. [DOI] [PubMed] [Google Scholar]
- 4.Van Wijngaarden B., Schene A.H., Koeter M.W. Family caregiving in depression: impact on caregivers’ daily life, distress, and help seeking. J Affect Disord. 2004;81(3):211–222. doi: 10.1016/S0165-0327(03)00168-X. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher S.K., Mechanic D. Living with the mentally ill: effects on the health and functioning of other household members. Soc Sci Med. 1996;42(12):1691–1701. doi: 10.1016/0277-9536(95)00296-0. 1982. [DOI] [PubMed] [Google Scholar]
- 6.Weissman M.M., Wickramaratne P., Nomura Y. Families at high and low risk for depression: a 3-generation study. Arch Gen Psychiatry. 2005;62(1):29–36. doi: 10.1001/archpsyc.62.1.29. [DOI] [PubMed] [Google Scholar]
- 7.Igberase O.O., Morakinyo O., Lawani A.O., James B.O., Omoaregba J.O. Burden of care among relatives of patients with schizophrenia in midwestern Nigeria. Int J Soc Psychiatry. 2012;58(2):131–137. doi: 10.1177/0020764010387544. [DOI] [PubMed] [Google Scholar]
- 8.Shibre T., Medhin G., Teferra S. Predictors of carer-burden in schizophrenia: a five-year follow-up study in Butajira, Ethiopia. Ethiop Med J. 2012;50(2):125–133. [PubMed] [Google Scholar]
- 9.Hailemichael Y., Hanlon C., Tirfessa K. Catastrophic health expenditure and impoverishment in households of persons with depression: a cross-sectional, comparative study in rural Ethiopia. BMC Public Health. 2019;19(1):930. doi: 10.1186/s12889-019-7239-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tirfessa K., Lund C., Medhin G., Hailemichael Y., Fekadu A., Hanlon C. Food insecurity among people with severe mental disorder in a rural Ethiopian setting: a comparative, population-based study. Epidemiol Psychiatr Sci. 2019;28(4):397–407. doi: 10.1017/S2045796017000701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ritsher J.E., Warner V., Johnson J.G., Dohrenwend B.P. Inter-generational longitudinal study of social class and depression: a test of social causation and social selection models. Br J Psychiatry. 2001;40:s84–s90. doi: 10.1192/bjp.178.40.s84. Supplement. [DOI] [PubMed] [Google Scholar]
- 12.Terzian A.C., Andreoli S.B., de Oliveira L.M., de Jesus Mari J., McGrath J. A cross-sectional study to investigate current social adjustment of offspring of patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2007;257(4):230–236. doi: 10.1007/s00406-007-0714-6. [DOI] [PubMed] [Google Scholar]
- 13.Hatfield A.B., Lefley H.P. Future involvement of siblings in the lives of persons with mental illness. Community Ment Health J. 2005;41(3):327–338. doi: 10.1007/s10597-005-5005-y. [DOI] [PubMed] [Google Scholar]
- 14.Ranning A., Laursen T., Agerbo E. School performance from primary education in the adolescent offspring of parents with schizophrenia and bipolar disorder- a national, register-based study. Psychol Med. 2018;48(12):1993–2000. doi: 10.1017/S0033291717003518. [DOI] [PubMed] [Google Scholar]
- 15.Alem A., Kebede D., Fekadu A. Clinical course and outcome of schizophrenia in a predominantly treatment-naive cohort in rural Ethiopia. Schizophr Bull. 2009;35(3):646–654. doi: 10.1093/schbul/sbn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shibre T., Kebede D., Alem A. Schizophrenia: illness impact on family members in a traditional society–rural Ethiopia. Soc Psychiatry Psychiatr Epidemiol. 2003;38(1):27–34. doi: 10.1007/s00127-003-0594-7. [DOI] [PubMed] [Google Scholar]
- 17.Alkire S, Jindra C, Robles G, Vaz A. Multidimensional Poverty Index 2016: brief methodological note and results. OPHI briefing 2016;42:2.
- 18.Organization W.H. World Health Organization; 2007. Verbal autopsy standards: Ascertaining and attributing cause of death. [Google Scholar]
- 19.Misganaw A., Mariam D.H., Araya T., Aneneh A. Validity of verbal autopsy method to determine causes of death among adults in the urban setting of Ethiopia. BMC Med Res Methodol. 2012;12(1):1–9. doi: 10.1186/1471-2288-12-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coates J, Swindale A, Bilinsky P. Household food insecurity access scale (HFIAS) for measurement of household food access: Indicator guide (v. 3). Washington, DC: food and nutrition technical assistance project, academy for educational Development. 2007:1--36.
- 21.Marques E.S., Reichenheim M.E., de Moraes C.L., Antunes M.M., Salles-Costa R. Household food insecurity: a systematic review of the measuring instruments used in epidemiological studies. Public Health Nutr. 2015;18(5):877–892. doi: 10.1017/S1368980014001050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olson D.H., Wilson M. Family satisfaction scale. Fam Invent. 1982:89–103. [Google Scholar]
- 23.Hu X., Summers J.A., Turnbull A., Zuna N. The quantitative measurement of family quality of life: a review of available instruments. J Intellect Disabil Res JIDR. 2011;55(12):1098–1114. doi: 10.1111/j.1365-2788.2011.01463.x. [DOI] [PubMed] [Google Scholar]
- 24.Brugha T.S., Cragg D. The list of threatening experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand. 1990;82(1):77–81. doi: 10.1111/j.1600-0447.1990.tb01360.x. [DOI] [PubMed] [Google Scholar]
- 25.Abiola T., Udofia O., Zakari M. Psychometric properties of the 3-item Oslo Social Support scale among clinical students of Bayero University Kano, Nigeria. Malays J Psychiatry. 2013;22(2):32–41. [Google Scholar]
- 26.Yu Y.H., Peng M.M., Bai X. Schizophrenia, social support, caregiving burden and household poverty in rural China. Soc Psychiatry Psychiatr Epidemiol. 2020;55:1–10. doi: 10.1007/s00127-020-01864-2. [DOI] [PubMed] [Google Scholar]
- 27.Trani J.F., Bakhshi P., Kuhlberg J. Mental illness, poverty and stigma in India: a case-control study. BMJ Open. 2015;5(2) doi: 10.1136/bmjopen-2014-006355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan S.C., Yeoh A.L., Choo I.B. Burden and coping strategies experienced by caregivers of persons with schizophrenia in the community. J Clin Nurs. 2012;21(17–18):2410–2418. doi: 10.1111/j.1365-2702.2012.04174.x. [DOI] [PubMed] [Google Scholar]
- 29.Romero S., Delbello M.P., Soutullo C.A., Stanford K., Strakowski S.M. Family environment in families with versus families without parental bipolar disorder: a preliminary comparison study. Bipolar Disord. 2005;7(6):617–622. doi: 10.1111/j.1399-5618.2005.00270.x. [DOI] [PubMed] [Google Scholar]
- 30.van Wijngaarden B., Koeter M., Knapp M. Caring for people with depression or with schizophrenia: are the consequences different? Psychiatry Res. 2009;169(1):62–69. doi: 10.1016/j.psychres.2008.06.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.