Abstract
Background: The Coronavirus Disease 2019 (COVID-19) pandemic remains serious public issue. COVID-19 vaccine is a vital strategy to prevent this critical pandemic. However, unwillingness to take this vaccine are key barriers to manage the COVID-19 pandemic. The control of this pandemic will depend principally on the people acceptance of COVID-19 vaccine. Therefore, this systematic review and meta-analysis was intended to determine the acceptance rate toward COVID-19 vaccine in Africa. Methods: African Journals OnLine, PubMed, Cochrane Review, HINARI, EMBASE, Google Scholar, Web of Science, and Scopus were used to retrieve related articles. The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines were used for this study. Random-effect model, a funnel plot, Egger’s test, I2 statistic, subgroup analysis was done. The study was performed by using a STATA version 11 statistical software. Results: A total of 22 studies with 33,912 study participants were included in this systematic review and meta-analysis. From this finding, the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa was 48.93% (95% CI: [39.49, 58.37]). The subgroup analysis revealed that the pooled prevalence of COVID-19 vaccine acceptance among adults in Africa was highest (66.03%, 95% CI [62.84, 69.22]) in Southern Africa, and Lowest (24.28%, 95% CI [3.26, 45.30]) in Northern Africa. Conclusion: This study showed that the estimate of the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa was very low. All concerned bodies should be actively involved to improve the acceptance rate of COVID-19 vaccine.
Keywords: COVID-19, acceptance, vaccine, systematic review, meta-analysis, Africa
Introductions
The COVID-19 remains a worldwide challenge,1 since it has been declared by the WHO as a pandemic.2 It has been stated to be a global community health emergency.3 It has affected all individuals over all nations, and continents.4 It has led to substantial morbidity and mortality.5,6 There is also an extensive economic crisis in addition to considerable deaths and morbidity related to this pandemic.7 COVID 19 has spread quickly in Africa and worldwide. Different measures have been applied across countries and this caused a secondary social and economic effect on children and their households.8 The pandemic has deteriorated mental health in families with children <18.9 COVID-19 has also devastatingly influenced children’s development worldwide.10 It is also substantially interrupted child vaccination.11 It is a major mental health issue of the population,12 which has an enormous impact on youth mental health.13 It has a significant stress on healthcare systems, patients, and healthcare workers.14 Moreover, the COVID-19 pandemic’s influences tuberculosis (TB) or human immunodeficiency virus (HIV) treatment and prevention services significantly.15
The COVID-19 pandemic is a vast encounter and put a substantial problem on the African continent.16 This burden requires urgent measures to control globally.17 COVID-19 may put a considerable burden on the poor and vulnerable populations.7 Initially, due to the lack of a COVID-19 vaccine, different prevention strategies were employed worldwide.18 Several measures are being applied by African’s which include limits on large gatherings, travel bans, school closures, augmented testing, and country lockdown.7 However, the pandemic is continuing its burden worldwide. Thus, when a safe and effective vaccine is available, the government should be equipped to distribute a COVID-19 vaccine with opportunity for equitable access.19 The willingness for COVID-19 vaccination is found to be determined by information about vaccine efficacy, individual variety, and vaccine development.20 There is a debate concerning the safety and efficacy of COVID-19 vaccines and this may lead to low vaccination rates.21 Despite researchers working speedily and collaboratively for the development of vaccine, the need of the population for a COVID-19 vaccine might be delayed by vaccine hesitancy.22 The COVID-19 response and the community health benefits’ of an effective vaccine might be determined by the individuals unwillingness for this vaccine.23 Moreover, vaccine hesitancy may challenge the actual effectiveness of COVID-19 vaccine.24 Only a low percent of the parents had accepted to vaccine their children against COVID-19.25 Additionally, many parents are not willing to enroll their child in a clinical trial for a COVID-19 vaccine.26 Thirty-five percent of the caregivers were unwilling to vaccinate their children against COVID-19.27 This would impact the achievement of herd immunity for COVID-19 and extend the effects of the pandemic by far.28
Recognizing the adult acceptance rate regarding COVID-19 vaccine will support for the development and application of effective approaches to enhance vaccination for this pandemic.29 Minimizing the vaccine hesitancy for COVID-19 vaccine and using strategies to control the pathogen may be as remarkable as discovering a safe and effective vaccine.30 It is essential to initiate offering public health education about COVID-19 vaccines preceding the availability of this vaccine to improve their perception regarding COVID-19 vaccination.28 Besides, it is an ethical and a humanistic responsibility to confirm that this vaccine is safe for the community.31 It is crucial to warrant healthcare workers and population to have access to reliable and sufficient information concerning this vaccine to raise its acceptance rate.32 Since the attitude of the healthcare workers toward COVID-19 vaccine were found to influence their own use of the vaccine and their intention to suggest a vaccine to their patients, future education needs to be prioritized for them to be accepted by the population.33
Methods
Research Questions
What is the level of acceptance toward COVID-19 vaccine among adults in Africa?
Study Setting
This systematic review and meta-analysis included only studies conducted in Africa.
Search Strategies
African Journals OnLine, PubMed, Cochrane Review, HINARI, EMBASE, Google Scholar, Web of Science, and Scopus were used to retrieve related articles. During this, the search was done by using the keywords such as; “willingness,” “acceptance,” “hesitancy,” “Intention,” “COVID-19,” “SARS-CoV-2,” “vaccine,” and “Africa.” To integrate these keywords; Boolean operators “AND” and “OR” were used.
Eligibility Criteria
In this systematic review and meta-analysis; all cross-sectional studies done among adults in Africa and articles published in English language up to June 14, 2021 were used as an inclusion criteria. Whereas, articles in which the outcome variable was not clearly defined and measured, articles with poor quality were excluded from this systematic review and meta-analysis.
Outcome Measurement
In this systematic review and meta-analysis, primary outcome was the prevalence of acceptance toward COVID-19 vaccine among adults in Africa, which was reported within the included studies. The acceptance of COVID-19 vaccine was measured by using a dichotomized “Yes” and “No” questions. The participants were asked “Did you have the intention to accept COVID-19 vaccine if it is available in the future?”
Data Extraction
All studies obtained from all databases were exported to Endnote version 8 software and the duplicates were removed. Finally, all studies were exported to Microsoft Excel spreadsheet. The Titles and abstracts of studies retrieved using the search strategy and those from additional sources were screened to identify studies that satisfy the inclusion criteria. Then studies that satisfied the inclusion criteria by title or abstract screening went through a full text review for eligibility and data extraction.
Data Synthesis and Reporting
This systematic review and meta-analysis done on the acceptance rate of COVID-19 vaccine was conducted by using the PRISMA flowchart diagram,34,35 and PRISMA checklist.35
Quality Assessment
This systematic review and meta-analysis have included cross-sectional studies. The quality of all included articles were determined by the Newcastle–Ottawa Scale (NOS) quality assessment criteria for cross-sectional studies.36,37 At this time, the modified NOS for cross-sectional studies was used to include studies and articles with ≥5 out of 10 considered as a high quality score.38
Statistical Analysis
The acceptance toward COVID-19 vaccine among adults in Africa was pooled using a random-effect model. Heterogeneity was determined by using I2 statistics.39-41 Moreover, publication bias was checked by funnel plots and the Egger’s test. The Egger’s test P value <.05, it was considered as significant evidence of publication bias.42 Sensitivity analyses and subgroup analysis were performed to identify possible moderators of the heterogeneity.
Ethics Approval and Consent to Participate
Not applicable. This is because the study is a Systematic Review and Meta-analysis. There is no data collected from the people for the purpose of this study. The study was performed by reviewing the recently published articles.
Result
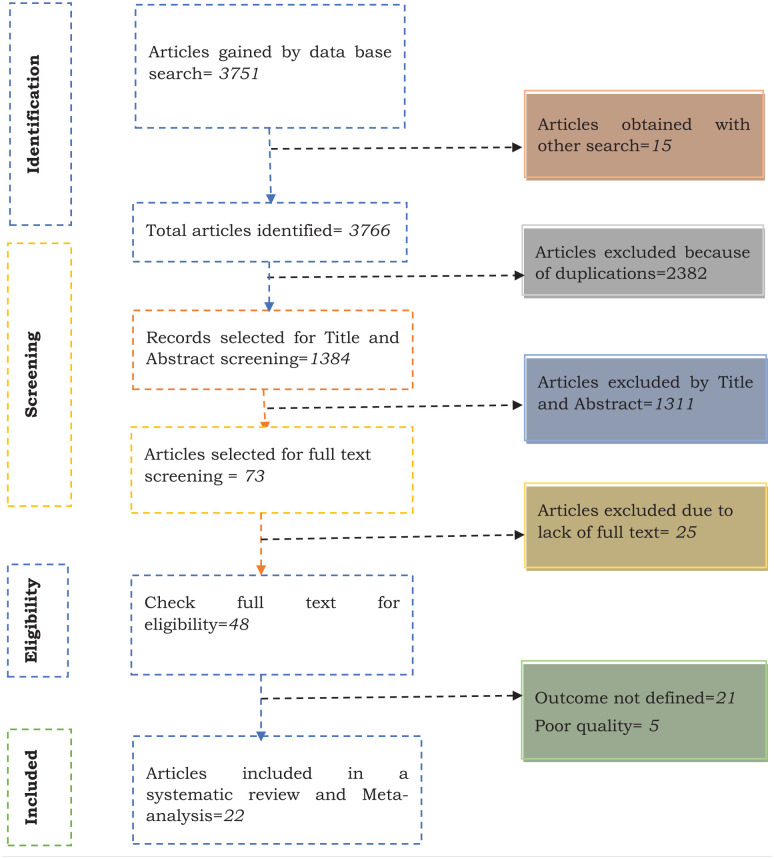
Different search strategies, African Journals OnLine, PubMed, Cochrane Review, HINARI, EMBASE, Google Scholar, Web of Science, and Scopus were used to retrieve the related articles. Using them, a total of 3766 articles were identified. From this, 2382 articles were excluded because of duplication. From 1384 articles left, 1311 articles were excluded by the titles and abstracts due they were unrelated. Out of 73 articles certain for full text screening, 25 were excluded due to lack of full text. Furthermore, 48 full-text articles were checked for eligibility and 26 articles were excluded with a reason (21 because of outcome variable was not defined and measured well and 5 because of poor quality). Lastly, 22 articles were met the eligibility criteria and included in to this systematic review and meta-analysis (Figure 1).
Figure 1.
PRISMA Flowchart diagram of the study selection for systematic review and meta-analysis on the acceptance toward COVID-19 vaccine in Africa.
Characteristics of the Included Studies
A total of 22 cross-sectional studies published up to June 14, 2021 were included in this systematic review and meta-analysis. The largest sample size was 10,618 from south Africa, southern Africa,43 while the smallest sample size was 234 from Ghana, western Africa.44 The largest and smallest acceptance rates of adults toward COVID-19 vaccine were 80.9% from Ethiopia, eastern Africa,45 and 13.52% from Egypt, Northern Africa,46 respectively. Furthermore, the estimated pooled prevalence for this acceptance rate of COVID-19 among adults in Africa has been included 33,912 study participants (Table 1).
Table 1.
Characteristics of the studies included in the Systematic Review and Meta-analysis on the level of acceptance toward COVID-19 vaccine among adults in Africa.
| S.N | Author | Year | Country | Subregion | Study design | Sample size | Prevalence |
|---|---|---|---|---|---|---|---|
| 1 | Abebe et al47 | 2021 | Ethiopia | Eastern Africa | Cross-sectional | 492 | 62.6% |
| 2 | Adebisi et al48 | 2021 | Nigeria | Western Africa | Cross-sectional | 517 | 74.47% |
| 3 | Agyekum et al44 | 2021 | Ghana | Western Africa | Cross-sectional | 234 | 39.32% |
| 4 | Ahmed et al49 | 2021 | Somalia | Eastern Africa | Cross-sectional | 4543 | 76.78% |
| 5 | Belsti et al50 | 2021 | Ethiopia | Eastern Africa | Cross-sectional | 1184 | 31.42% |
| 6 | Chiedozie et al51 | 2021 | Nigeria | Western Africa | Cross-sectional | 499 | 51.1% |
| 7 | Dereje et al45 | 2021 | Ethiopia | Eastern Africa | Cross-sectional | 409 | 80.9% |
| 8 | Ditekemena et al52 | 2021 | DR Congo | Middle Africa | Cross-sectional | 4131 | 55.92% |
| 9 | Echoru et al53 | 2021 | Uganda | Eastern Africa | Cross-sectional | 1067 | 53.61% |
| 10 | Eniade et al54 | 2021 | Nigeria | Western Africa | Cross-sectional | 368 | 40.5% |
| 11 | Hoque et al55 | 2020 | South Africa | Southern Africa | Cross-sectional | 346 | 63.3% |
| 12 | Mohamed Hussein et al46 | 2021 | Egypt | Northern Africa | Cross-sectional | 488 | 13.52% |
| 13 | Kabamba Nzaji et al56 | 2020 | DR Congo | Middle Africa | Cross-sectional | 613 | 27.7% |
| 14 | Kanyike et al57 | 2021 | Uganda | Eastern Africa | Cross-sectional | 600 | 37.33% |
| 15 | Mose and Yeshaneh58 | 2021 | Ethiopia | Eastern Africa | Cross-sectional | 396 | 70.7% |
| 16 | Ngoyi et al33 | 2020 | DR Congo | Middle Africa | Cross-sectional | 439 | 25.28% |
| 17 | Olomofe et al59 | 2021 | Nigeria | Western Africa | Cross-sectional | 776 | 58.25% |
| 18 | Saied et al60 | 2021 | Egypt | Northern Africa | Cross-sectional | 2133 | 34.97% |
| 19 | Alice Tobin et al61 | 2021 | Nigeria | Western Africa | Cross-sectional | 1228 | 50.24% |
| 20 | Zewude and Habtegiorgis62 | 2021 | Ethiopia | Eastern Africa | Cross-sectional | 319 | 46.08% |
| 21 | Dinga et al63 | 2021 | Cameroon | Middle Africa | Cross-sectional | 2512 | 15.45% |
| 22 | Runciman et al43 | 2021 | South Africa | Southern Africa | Cross-sectional | 10 618 | 67% |
Publication Bias
The publication bias was assessed by using Egger’s test and funnel plot. From Egger’s test, a P-value was .237. Since Egger’s test was statistically insignificant, this suggests that there was no publication bias. Concerning to the funnel plot, it shows the symmetrical distribution of the included articles, while this suggests there is no evidence for publication bias for this meta-analysis (Figure 2).
Figure 2.
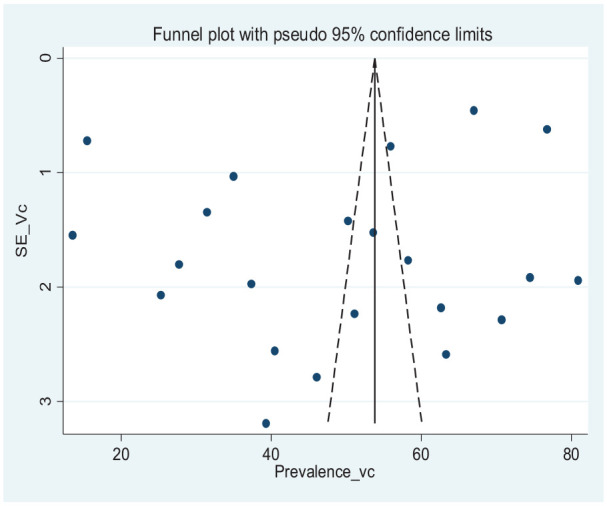
Funnel plot with 95% confidence limits of the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa.
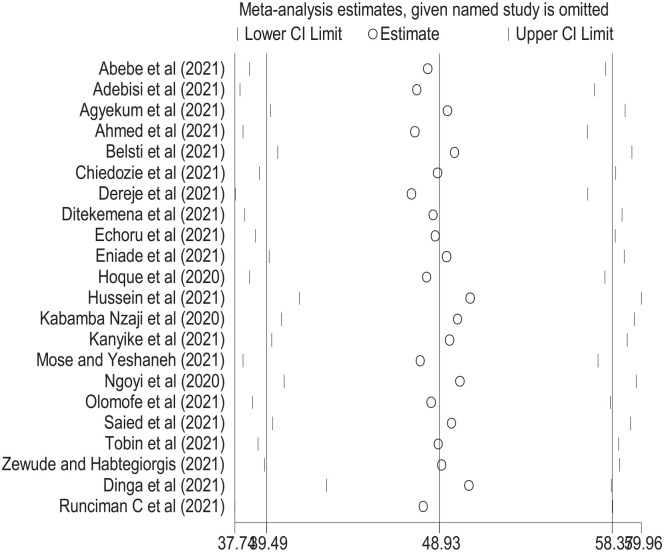
Sensitivity Analysis
The results of a sensitivity analysis revealed that no single study was influenced the overall acceptance toward COVID-19 vaccine among adults in Africa (Figure 3).
Figure 3.
The results of sensitivity analysis of 22 studies conducted on the acceptance toward COVID-19 vaccine among adults in Africa.
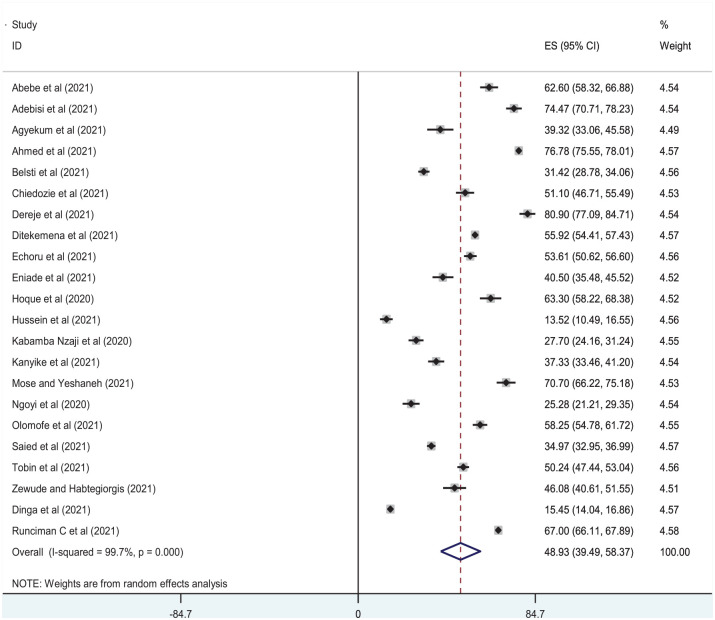
Acceptance Rate of COVID-19 Vaccine
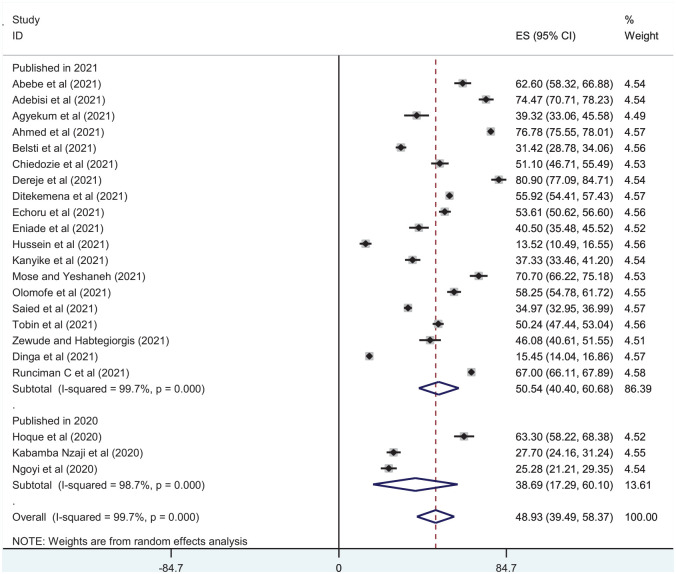
This meta-analysis was used the random effect model to estimate the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa, and it was 48.93% (95% CI [39.49, 58.37]). The level of heterogeneity was (I2 = 99.7%, P = .000) (Figure 4).
Figure 4.
Forest plot of pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa.
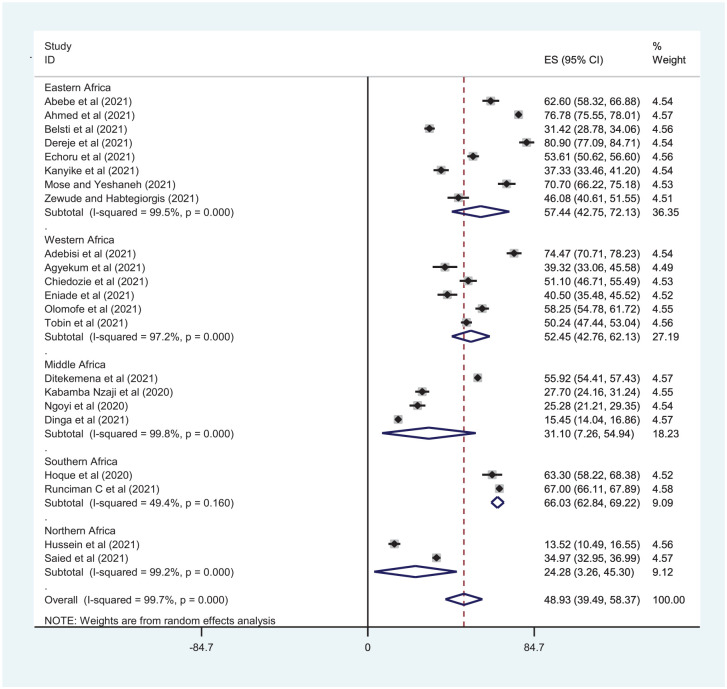
Subgroup Analysis
The subgroup analysis was desired to be performed due to the presence of a significant level of heterogeneity among the included studies. To check the sources of heterogeneity, subgroup analysis was done by using subregion and publication year to assess the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa.
Subgroup Analysis by Subregion
The pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa was (57.44%, 95% CI [42.75, 72.13], I2 = 99.5%, P = .000) in Eastern Africa, (52.45%, 95% CI [42.76, 62.13], I2 = 97.2%, P = .000) in Western Africa, (31.10%, 95% CI [7.26, 54.94], I2 = 99.8%, P = .000) in Middle Africa, (66.03%, 95% CI [62.84, 69.22], I2 = 49.4%, P = .160) in Southern Africa, and (24.28%, 95% CI [3.26, 45.30], I2 = 99.2%, P = .000) in Northern Africa (Figure 5).
Figure 5.
Subgroup analysis by subregion on the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa.
Subgroup Analysis by Publication Year
The pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa was (38.69%, 95% CI [17.29, 60.10], I2 = 98.7%, P = .000) for studies published in 2020, and (50.54%, 95% CI [40.40, 60.68], I2 = 99.7%, P = .000) for studies published in 2021 (Figure 6).
Figure 6.
Subgroup analysis by year of publication on the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa.
Discussion
COVID-19 pandemic remains a serious public problem and, to date, it has not been controlled effectively worldwide. Different strategies were implemented to manage and control it but have not been effective to halt the pandemic. Because of this, COVID-19 vaccine was developed and found better than other strategies implemented. COVID-19 vaccine is a vital strategy to slow this critical pandemic. However, hesitance toward this vaccine is a major barrier to manage the COVID-19 pandemic. Because of this, the control of this pandemic will depend principally on the people acceptance of COVID-19 vaccine. Therefore, this systematic review and meta-analysis was intended to determine the acceptance rate of COVID-19 vaccine in Africa.
This systematic review and meta-analysis were done by using comprehensive search strategies to include studies involving African adult individuals. It was done based on PRISMA guidelines and checklists. The quality of the included studies was determined by using the modified NOS assessment. Based on this assessment, all studies with high methodological quality were included. All included studies were observational studies (cross-sectional). Regarding publication bias, it was assessed by using Egger’s test and funnel plots.
This is the first systematic review and meta-analysis done on the level of acceptance of COVID-19 vaccine among adults in Africa. This information has significant implications for the government, researchers, health care policymakers and implementers, communities, and healthcare providers. This systematic review meta-analysis showed that the estimate of the pooled prevalence of acceptance rate of COVID-19 vaccine among adults in Africa was 48.93% (95% CI: [39.49, 58.37]).
This finding was lower when compared with the study conducted in Turkey (84.6%),64 South Carolina (60.6%),65 United States (66.0%),66 China (63%),67 Australia (80%),68 Saudi Arabia (64.72%),69 UK (86%),70 Japan (65.7%),71 Israel (85%),72 Bangladesh (74.6%),73 Iran (64.2%),74 Italy (86.1%),75 France (77.6%),76 China (60.4%),77 Vietnam (76.10%),78 Pakistan (70.25%),79 Latin America and the Caribbean (80.0%),80 and United States (63.7%).81 This might be due to the differences in the sociodemographic characteristics of the study population and the awareness level of the study participants toward the COVID-19 vaccine. Furthermore, government, healthcare providers, and the stakeholder’s commitment toward the prevention strategies of COVID-19 could have significant contributions for the acceptance of COVID-19 vaccine among the participants. This finding was consistent when compared with the study conducted in Kuwait (53.1%),82 Palestine (40%),83 Malaysia (48.2%),84 England (55.8%),25 Greece (57.7%),85 and Saudi Arabia (48%).86 However, this finding was higher when compared with the 2 studies conducted in Jordan (36.8%),87 and Jordan (37.4%).88 This could be due to the differences in the sociodemographic characteristics of the study population.
The subgroup analysis was desired to be performed due to the presence of a significant level of heterogeneity among the included studies. To check the sources of heterogeneity, subgroup analysis was done by using subregion and publication year to assess the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa. The pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa was (57.44%, 95% CI [42.75, 72.13]) in Eastern Africa, (52.45%, 95% CI [42.76, 62.13]) in Western Africa, (31.10%, 95% CI [7.26, 54.94]) in Middle Africa, (66.03%, 95% CI [62.84, 69.22]) in Southern Africa, and (24.28%, 95% CI [3.26, 45.30]) in Northern Africa. Whereas, the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa was (38.69%, 95% CI [17.29, 60.10]) for studies published in 2020, and (50.54%, 95% CI [40.40, 60.68]) for studies published in 2021.
Overall, according to the findings of this systematic review and meta-analysis, the estimate of the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa was less than 50%, which indicates there are critical issues to manage and control this pandemic in Africa. Primarily, long-term restriction of movement was employed as a strategy to stop the spread of COVID-19.89 However, there was a crucial necessity to develop effective vaccines as the most controlling method to halt COVID-19 since it was extensive globally.90 Because of this, scientists struggled to provide a proven treatment for COVID-19. Because of the lack of highly effective therapies against COVID-19, the development of vaccines against COVID-19 was a priority to stop the pandemic. Nevertheless, the achievement of this method relies on people’s willingness for immunization.91 Furthermore, vaccines were being developed by numerous countries for the aim of a permanent solution for this pandemic.71 It is believed that the availability of COVID-19 vaccine with wide uptake might contribute to the development of herd immunity and guard the most vulnerable individuals against COVID-1989 and the public may think that their personal protection behaviors can replace COVID-19 vaccination to avoid COVID-19. They may trust commitment to these precautions is satisfactory for the prevention of COVID-19.92
Since the pandemic is leading a considerable effect on all citizens, it requires a cooperative response.93 Nevertheless, vaccine hesitancy remains a blockade to population vaccination against this pandemic.94 It can be a barrier to the distribution of COVID-19 vaccines.95 This is a significant impending issue for this pandemic.96 Even, COVID-19 survivors were revealed to be refusing or uncertain toward this vaccine.93 Since COVID-19 vaccines were hastily developed worldwide, the population may be more concerned for the safety of the vaccine than the risk of COVID-19 infection which likely contribute to vaccine hesitancy.94
Conclusions
This systematic review and meta-analysis showed that the estimate of the pooled prevalence of acceptance toward COVID-19 vaccine among adults in Africa was very low. With this level of acceptance toward COVID-19 vaccine, it would be enormously problematic to manage and control this pandemic. Besides, this may extend the era of this pandemic.
Furthermore, this finding would have a significant contribution for governments, healthcare providers, stakeholders, health policy-makers and implementers, researchers, and for the entire population. All concerned bodies should be actively involved to improve the acceptance rate of COVID-19 vaccine, which could minimize the morbidity and mortality associated with this pandemic, and also to halt the era of this pandemic. It is substantial to initiate offering health education to the population regarding COVID-19 vaccination to enhance their acceptance rate toward this vaccine. The population needs to be conscious regarding the importance, safety, and efficacy of COVID-19 vaccine.
Footnotes
Author Contributions: Addisu Dabi Wake has contributed to the conception of the study, drafting or revising the article, writing the manuscript, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Addisu Dabi Wake  https://orcid.org/0000-0003-1219-0836
https://orcid.org/0000-0003-1219-0836
Data Sharing Statement: The data used to support the findings of this study are available from the corresponding author on reasonable request.
References
- 1.Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254-266. doi: 10.1016/j.cca.2020.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jin Y, Yang H, Ji W, et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12:372. doi: 10.3390/v12040372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang L, Wang Y, Ye D, Liu Q. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int J Antimicrob Agents. 2020;55:105948. doi: 10.1016/j.ijantimicag.2020.105948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133-2134. doi: 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- 5.Dariya B, Nagaraju GP. Understanding novel COVID-19: its impact on organ failure and risk assessment for diabetic and cancer patients. Cytokine Growth Factor Rev. 2020;53:43-52. doi: 10.1016/j.cytogfr.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu Q, Shi Y. Coronavirus disease (COVID-19) and neonate: what neonatologist need to know. J Med Virol. 2020;92:564-567. doi: 10.1002/jmv.25740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ataguba JE. COVID-19 pandemic, a War to be won: understanding its economic implications for Africa. Appl Health Econ Health Policy. 2020;18:325-328. doi: 10.1007/s40258-020-00580-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The impact of COVID-19 on children in West and Central Africa: learning from 2020; save the children. Resource Centre. Accessed June 18, 2021. https://resourcecentre.savethechildren.net/node/18647/pdf/rapport_covid_anglais.pdf.
- 9.Gadermann AC, Thomson KC, Richardson CG, et al. Examining the impacts of the COVID-19 pandemic on family mental health in Canada: findings from a national cross-sectional study. BMJ Open. 2021;11(1):e042871. doi: 10.1136/bmjopen-2020-042871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoshikawa H, Wuermli AJ, Britto PR, et al. Effects of the global Coronavirus disease-2019 pandemic on early childhood development: short- and long-term risks and mitigating program and policy actions. J Pediatr. 2020;223:188-193. doi: 10.1016/j.jpeds.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fahriani M, Anwar S, Yufika A, et al. Disruption of childhood vaccination during the COVID-19 pandemic in Indonesia. Narra J. 2021;1:1-11. doi: 10.52225/narraj.v1i1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kajdy A, Feduniw S, Ajdacka U, et al. Risk factors for anxiety and depression among pregnant women during the COVID-19 pandemic: a web-based cross-sectional survey. Medicine. 2020;99:e21279. doi: 10.1097/MD.0000000000021279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liang L, Ren H, Cao R, et al. The effect of COVID-19 on youth mental health. Psychiatr Q. 2020;91:841-852. doi: 10.1007/s11126-020-09744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deprest J, Choolani M, Chervenak F, et al. Fetal diagnosis and therapy during the COVID-19 pandemic: guidance on behalf of the International Fetal Medicine and Surgery Society. Fetal Diagn Ther. 2020;47:689-698. doi: 10.1159/000508254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nachega JB, Kapata N, Sam-Agudu NA, et al. Minimizing the impact of the triple burden of COVID-19, tuberculosis and HIV on health services in sub-Saharan Africa. Internet J Infect Dis. 2021. doi: 10.1016/j.ijid.2021.03.038https://www.ijidonline.com/article/S1201-9712(21)00256-3/abstract [DOI] [PMC free article] [PubMed]
- 16.Ogunbiyi O. The disproportionate burden of COVID-19 in Africa. COVID-19 pandemic. Elsevier Public Health Emergency Collection. 2022;179-187. doi: 10.1016/B978-0-323-82860-4.00021-5https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8175763/ [DOI]
- 17.Dashraath P, Wong JLJ, Lim MXK, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222:521-531. doi: 10.1016/j.ajog.2020.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borriello A, Master D, Pellegrini A, Rose JM. Preferences for a COVID-19 vaccine in Australia. Vaccine. 2021;39:473-479. doi: 10.1016/j.vaccine.2020.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lazarus JV, Ratzan SC, Palayew A, et al. Author correction: a global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):354-358. doi: 10.1038/s41591-020-01226-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hursh SR, Strickland JC, Schwartz LP, Reed DD. Quantifying the impact of public perceptions on vaccine acceptance using behavioral economics. Front Public Health. 2020;8:608852. doi: 10.3389/fpubh.2020.608852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alley SJ, Stanton R, Browne M, et al. As the pandemic progresses, how does willingness to vaccinate against COVID-19 evolve? Int J Environ Res Public Health. 2021;18: 1-14. doi: 10.3390/ijerph18020797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020;35:785-788. doi: 10.1007/s10654-020-00675-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daly M, Robinson E. Willingness to vaccinate against COVID-19 in the US: longitudinal evidence from a nationally representative sample of adults from April-October 2020. Preprint. Posted online November 30, 2020. medRxiv. doi: 10.1101/2020.11.27.20239970 [DOI] [Google Scholar]
- 24.Graffigna G, Palamenghi L, Boccia S, Barello S. Relationship between citizens’ health engagement and intention to take the COVID-19 vaccine in Italy: a mediation analysis. Vaccines. 2020;8:576. doi: 10.3390/vaccines8040576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020;38:7789-7798. doi: 10.1016/j.vaccine.2020.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldman RD, Staubli G, Cotanda CP, et al. Factors associated with parents’ willingness to enroll their children in trials for COVID-19 vaccination. Hum Vaccin Immunother. 2021;17:1607-1611. doi: 10.1080/21645515.2020.1834325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldman RD, Yan TD, Seiler M, et al. Caregiver willingness to vaccinate their children against COVID-19: cross sectional survey. Vaccine. 2020;38:7668-7673. doi: 10.1016/j.vaccine.2020.09.084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marcec R, Majta M, Likic R. Will vaccination refusal prolong the war on SARS-CoV-2? Postgrad Med J. 2021;97:143-149. doi: 10.1136/postgradmedj-2020-138903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qiao S, Tam CC, Li X. Risk exposures, risk perceptions, negative attitudes toward general vaccination, and COVID-19 vaccine acceptance among college students in South Carolina. Preprint. Posted online November 30 2020. medRxiv. doi: 10.1177/08901171211028407. [DOI] [PubMed] [Google Scholar]
- 30.Neumann-Böhme S, Varghese NE, Sabat I, et al. Once we have it, will we use it? A european survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21:977-982. doi: 10.1007/s10198-020-01208-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuppalli K, Brett-Major DM, Smith TC. COVID-19 vaccine acceptance: we need to start now. Open Forum Infect Dis. 2021;8:ofaa658. doi: 10.1093/ofid/ofaa658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kucukkarapinar M, Karadag F, Budakoglu I, et al. COVID-19 vaccine hesitancy and its relationship with illness risk perceptions, affect, worry, and public trust: an online serial cross-sectional survey from Turkey. Psychiatry Clin Psychopharmacol. 2021;31:98-109. doi: 10.5152/pcp.2021.21017 [DOI] [Google Scholar]
- 33.Ngoyi JM, Mbuyu LK, Kibwe DN, Kabamba LN, Umba EK, Tambwe PN, et al. Covid-19 vaccination acceptance among students of the Higher Institute of Medical Techniques of Lubumbashi, Democratic Republic of Congo. Rev L’Infirmier Congo. 2020;4:48-52. [Google Scholar]
- 34.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700-b2700. doi: 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006-1012. doi: 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 36.Modesti PA, Reboldi G, Cappuccio FP, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One. 2016;11:e0147601. doi: 10.1371/journal.pone.0147601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Ottawa Hospital Research Institute. [Google Scholar]
- 38.Yazew KG, Walle TA, Azagew AW. Prevalence of anti-diabetic medication adherence and determinant factors in Ethiopia: a systemic review and meta-analysis, 2019. Int J Afr Nurs Sci. 2019;11:100167. doi: 10.1016/j.ijans.2019.100167 [DOI] [Google Scholar]
- 39.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 40.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11:193-206. doi: 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- 41.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Runciman C, Roberts B, Alexander K, Bohler-Muller N, Bekker M. UJ-HSRC Covid-19 Democracy Survey. Willingness to Take a Covid-19 Vaccine: A Research Briefing. University of Johannesburg, Centre for Social Change, Human Sciences Research Council, and Developmental, Capable and Ethical State; 2021. [Google Scholar]
- 44.Agyekum MW, Afrifa-Anane GF, Kyei-Arthur F, Addo B. Acceptability of COVID-19 vaccination among health care workers in Ghana. Adv Public Health. 2021;2021:1-8. doi: 10.1155/2021/9998176 [DOI] [Google Scholar]
- 45.Dereje N, Tesfaye A, Tamene B, Alemeshet D, Abe H, Tesfa N, et al. COVID-19 vaccine hesitancy in Addis Ababa, Ethiopia: a mixed-methods study. Preprint. medRxiv. doi: 10.1101/2021.02.25.21252443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mohamed Hussein AAR, Galal I, Makhlouf NA, et al. A national survey of potential acceptance of COVID-19 vaccines in healthcare workers in Egypt. Preprint. medRxiv 2021.01.11.21249324. doi: 10.1016/j.ajg.2021.09.001. [DOI] [Google Scholar]
- 47.Abebe H, Shitu S, Mose A. Understanding of COVID-19 vaccine knowledge, attitude, acceptance, and determinates of COVID-19 vaccine acceptance among adult population in Ethiopia. Infect Drug Resist. 2021;14:2015-2025. doi: 10.2147/IDR.S312116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adebisi YA, Alaran AJ, Bolarinwa OA, Akande-Sholabi W, Lucero-Prisno DE. When it is available, will we take it? Social media users’ perception of hypothetical COVID-19 vaccine in nigeria. Pan Afr Med J. 2021;38:230. doi: 10.11604/pamj.2021.38.230.27325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ahmed MAM, Colebunders R, Gele AA, et al. COVID-19 vaccine acceptability and adherence to preventive measures in Somalia: results of an online survey. Vaccines. 2021;9: 1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Belsti Y, Gela YY, Akalu Y, et al. Willingness of Ethiopian population to receive COVID-19 vaccine. J Multidiscip Healthc. 2021;14:1233-1243. doi: 10.2147/JMDH.S312637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chiedozie AP, Chukwuebuka OJ, Chidimma CF, Onyinyechi OV, Chijioke AK, Chibuzor OS, et al. Willingness to accept a potential COVID-19 vaccine in Nigeria. Am J Med Sci Med. 2021;9:1-5. doi: 10.12691/ajmsm-9-1-1 [DOI] [Google Scholar]
- 52.Ditekemena JD, Nkamba DM, Mutwadi A, et al. COVID-19 vaccine acceptance in the Democratic Republic of Congo: a cross-sectional survey. Vaccines. 2021;9:1-11. doi: 10.3390/vaccines9020153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Echoru I, Ajambo PD, Keirania E, Bukenya EEM. Sociodemographic factors associated with acceptance of COVID-19 vaccine and clinical trials in Uganda: a cross-sectional study in western Uganda. BMC Public Health. 2021;21(1):1106. doi: 10.1186/s12889-021-11197-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eniade OD, Olarinmoye A, Otovwe A, Akintunde FE, Okedare OO, Aniyeloye AO. Willingness to accept COVID-19 vaccine and its determinants among Nigeria citizens: a web-based cross-sectional study. J Adv Med Med Res. 2021;33(8)13-22. doi: 10.9734/jammr/2021/v33i830881 [DOI] [Google Scholar]
- 55.Hoque AM, Buckus S, Hoque M, Hoque ME, Van Hal G. COVID-19 vaccine acceptability among pregnant women at a primary health care facility in Durban, South Africa. Eur J Med Health Sci. 2020;2(5):1-6. doi: 10.24018/ejmed.2020.2.5.493 [DOI] [Google Scholar]
- 56.Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmat Obs Res. 2020;11:103-109. doi: 10.2147/POR.S271096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kanyike AM, Olum R, Kajjimu J, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Trop Med Health. 2021;49:37. doi: 10.1186/s41182-021-00331-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mose A, Yeshaneh A. COVID-19 vaccine acceptance and its associated factors among pregnant women attending Antenatal care clinic in southwest Ethiopia: institutional-based cross-sectional study. Int J Gen Med. 2021;14:2385-2395. doi: 10.2147/IJGM.S314346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Olomofe CO, Soyemi VK, Udomah BF, Owolabi AO, Ajumuka EE, Igbokwe CM, et al. Predictors of uptake of a potential covid-19 vaccine among Nigerian adults. Preprint. medRxiv preprint: Infectious Diseases (except HIV/AIDS); 2021. doi: 10.1101/2020.12.28.20248965. [DOI] [Google Scholar]
- 60.Saied SM, Saied EM, Kabbash IA, Abdo SAE. Vaccine hesitancy: beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol. 2021;93:4280-4291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alice Tobin E, Okonofua M, Adeke A, Obi A. Willingness to accept a COVID-19 vaccine in Nigeria: a population-based cross-sectional study. Ann Med Health Sci Res. 2021;7:53. [Google Scholar]
- 62.Zewude B, Habtegiorgis T. Willingness to take COVID-19 vaccine among people most at risk of exposure in southern Ethiopia. Pragmat Obs Res. 2021;12:37-47. doi: 10.2147/POR.S313991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dinga JN, Sinda LK, Titanji VPK. Assessment of vaccine hesitancy to a COVID-19 vaccine in Cameroonian adults and its global implication. Vaccines. 2021;9:175. doi: 10.3390/vaccines9020175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kaplan AK, Sahin MK, Parildar H, Adadan Guvenc I. The willingness to accept the COVID-19 vaccine and affecting factors among healthcare professionals: a cross-sectional study in Turkey. Int J Clin Pract. 2021;75:e14226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tam CC, Qiao S, Li X. Factors associated with decision making on COVID-19 vaccine acceptance among college students in South Carolina. Preprint. medRxiv 2020;:2020.12.03.20243543. doi: 10.1101/2020.12.03.20243543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ehde DM, Roberts MK, Herring TE, Alschuler KN. Willingness to obtain COVID-19 vaccination in adults with multiple sclerosis in the United States. Multiple Scler Relat Disord. 2021;49:102788. doi: 10.1016/j.msard.2021.102788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kwok KO, Li KK, Wei WI, Tang A, Wong SYS, Lee SS. Editor’s choice: Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021;114:103854. doi: 10.1016/j.ijnurstu.2020.103854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Seale H, Heywood AE, Leask J, et al. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect Dis. 2021;21:120. doi: 10.1186/s12879-021-05833-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657-1663. doi: 10.2147/JMDH.S276771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Williams L, Gallant AJ, Rasmussen S, et al. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020;25:1039-1054. doi: 10.1111/bjhp.12468 [DOI] [PubMed] [Google Scholar]
- 71.Yoda T, Katsuyama H. Willingness to receive COVID-19 vaccination in Japan. Vaccines. 2021;9:1-8. doi: 10.3390/vaccines9010048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zigron A, Dror AA, Morozov NG, et al. COVID-19 vaccine acceptance among dental professionals based on employment status during the pandemic. Front Med. 2021;8:618403. doi: 10.3389/fmed.2021.618403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Abedin M, Islam MA, Rahman FN, et al. Willingness to vaccinate against COVID-19 among Bangladeshi adults: understanding the strategies to optimize vaccination coverage. PLoS One. 2021;16:e0250495. doi: 10.1371/journal.pone.0250495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Askarian M, Fu L, Taghrir MH, Borazjani R, Shayan Z, Taherifard E, et al. Factors Affecting Covid-19 Vaccination Intent Among Iranians: COVID-19 Vaccination Acceptance. SSRN Scholarly Paper. Social Science Research Network; 2020. [Google Scholar]
- 75.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35:781-783. doi: 10.1007/s10654-020-00670-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38:7002-7006. doi: 10.1016/j.vaccine.2020.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gan L, Chen Y, Hu P, et al. Willingness to receive SARS-CoV-2 vaccination and associated factors among Chinese adults: a cross sectional survey. Int J Environ Res Public Health. 2021;18:1993. doi: 10.3390/ijerph18041993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Huynh G, Tran T, Nguyen HN, Pham L. COVID-19 vaccination intention among healthcare workers in Vietnam. Asian Pac J Trop Med. 2021;14:159. doi: 10.4103/1995-7645.312513 [DOI] [Google Scholar]
- 79.Malik A, Malik J, Ishaq U. Acceptance of COVID-19 vaccine in Pakistan among health care workers. PLoS One. 2021;16:e0257237. doi: 10.1371/journal.pone.0257237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Urrunaga-Pastor D, Bendezu-Quispe G, Herrera-Añazco P, et al. Cross-sectional analysis of COVID-19 vaccine intention, perceptions and hesitancy across Latin America and the Caribbean. Travel Med Infect Dis. 2021;41:102059. doi: 10.1016/j.tmaid.2021.102059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kuter BJ, Browne S, Momplaisir FM, et al. Perspectives on the receipt of a COVID-19 vaccine: a survey of employees in two large hospitals in Philadelphia. Vaccine. 2021;39:1693-1700. doi: 10.1016/j.vaccine.2021.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Alqudeimat Y, Alenezi D, AlHajri B, et al. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. 2021;30:262-271. doi: 10.1159/000514636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rabi R, Maraqa B, Nazzal Z, Zink T. Factors affecting nurses’ intention to accept the COVID-19 vaccine: a cross-sectional study. Public Health Nurs. 2021;38:781-788. doi: 10.1111/phn.12907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wong LP, Alias H, Wong P-F, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16:2204-2214. doi: 10.1080/21645515.2020.1790279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kourlaba G, Kourkouni E, Maistreli S, et al. Willingness of Greek general population to get a COVID-19 vaccine. Glob Health Res Policy. 2021;6:3. doi: 10.1186/s41256-021-00188-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Alfageeh EI, Alshareef N, Angawi K, Alhazmi F, Chirwa GC. Acceptability of a COVID-19 vaccine among the Saudi population. Vaccines. 2021;9:226. doi: 10.3390/vaccines9030226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front Public Health. 2021;9:632914. doi: 10.3389/fpubh.2021.632914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS One. 2021;16:e0250555. doi: 10.1371/journal.pone.0250555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021;21(3):318-319. doi: 10.1016/S1473-3099(20)30559-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dong D, Xu RH, Wong EL, et al. Public preference for COVID-19 vaccines in China: a discrete choice experiment. Health Expect. 2020;23:1543-1578. doi: 10.1111/hex.13140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Peretti-Watel P, Seror V, Cortaredona S, Launay O, Raude J, Verger P, et al. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020;20:769-770. doi: 10.1016/S1473-3099(20)30426-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang K, Wong EL-Y, Ho KF, et al. Change of willingness to accept COVID-19 vaccine and reasons of vaccine hesitancy of working people at different waves of local epidemic in Hong Kong, China: repeated cross-sectional surveys. Vaccines. 2021;9:62. doi: 10.3390/vaccines9010062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gerussi V, Peghin M, Palese A, et al. Vaccine hesitancy among Italian patients recovered from COVID-19 infection towards Influenza and Sars-Cov-2 vaccination. Vaccines. 2021;9:172. doi: 10.3390/vaccines9020172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775-779. doi: 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Longchamps C, Ducarroz S, Crouzet L, et al. COVID-19 vaccine hesitancy among persons living in homeless shelters in France. Vaccine. 2021;39:3315-3318. doi: 10.1016/j.vaccine.2021.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Taylor S, Landry CA, Paluszek MM, Groenewoud R, Rachor GS, Asmundson GJG. A proactive approach for managing COVID-19: the importance of understanding the motivational roots of vaccination hesitancy for SARS-CoV2. Front Psychol. 2020;11:575950. doi: 10.3389/fpsyg.2020.575950 [DOI] [PMC free article] [PubMed] [Google Scholar]