Significance
On May 25, 2020, George Floyd, an unarmed Black American male, was murdered by a White police officer in Minneapolis. Footage of his death was widely shared and caused widespread protests. Using data from Gallup before and after his death, we found an unprecedented level of anger and sadness in the population, particularly among Black Americans. Using US Census data, we found that, compared to White Americans, Black Americans reported significantly larger increases in depression and anxiety symptoms after Floyd’s death. Police brutality against Black Americans places Black Americans at disproportionate risk for reduced mental health, both reflecting and reinforcing US racial inequality.
Keywords: police killings, racism, mental health, public health, social inequality
Abstract
On May 25, 2020, George Floyd, an unarmed Black American male, was killed by a White police officer. Footage of the murder was widely shared. We examined the psychological impact of Floyd’s death using two population surveys that collected data before and after his death; one from Gallup (117,568 responses from n = 47,355) and one from the US Census (409,652 responses from n = 319,471). According to the Gallup data, in the week following Floyd’s death, anger and sadness increased to unprecedented levels in the US population. During this period, more than a third of the US population reported these emotions. These increases were more pronounced for Black Americans, nearly half of whom reported these emotions. According to the US Census Household Pulse data, in the week following Floyd’s death, depression and anxiety severity increased among Black Americans at significantly higher rates than that of White Americans. Our estimates suggest that this increase corresponds to an additional 900,000 Black Americans who would have screened positive for depression, associated with a burden of roughly 2.7 million to 6.3 million mentally unhealthy days.
On May 25, 2020, George Floyd was killed in police custody in Minneapolis, Minnesota. Protests in many US cities and around the world followed his death to express disapproval of police brutality against unarmed Black citizens and support for the Black Lives Matter movement (1). His murder has been described as a “collective moral injury” (2), the impact of which we investigate in this study.
Psychological and Health Impacts of Police Killings
Floyd’s death is among a number of high-profile cases from the past decade that have increased public attention toward police killings of unarmed Black Americans (3). In the United States, Black men are 2.5 to 3 times more likely than White men to be killed by police (4, 5). In 2019 and 2020, at least 30 unarmed Black Americans were killed by police (6).*
The video of Floyd’s death and the subsequent protests were widely shared by media outlets and on social media (1, 7). Previous work has found widespread, easily accessible social media coverage of killings to produce cumulative trauma (8, 9) and result in negative psychological effects on the larger Black community (8–12), especially when viewed in the historical context of structural and cultural racism and discrimination in the United States (12). Indeed, experiences with racism and discrimination are a cornerstone of Black identity in the United States (13), and experiences with police brutality toward Black Americans can vicariously traumatize other Black Americans (3).
That is, police brutality can affect both the physical and psychological health of individuals, including increased risk of cardiovascular disease (14), high blood pressure (14, 15), diabetes, and obesity (15); increased fear of victimization and experiences with racial biases; and decreased self-regard (3). More broadly, experiences with racial discrimination are linked to lower physical and psychological health among Black Americans (4, 14, 15), including increased rates of post-traumatic stress disorder (8, 9), depression (9, 12, 16), and anxiety (11, 16), even after adjusting for sociodemographic factors (17).
Although there are a variety of factors that protect Black Americans from the mental health effects of such racial discrimination (e.g., ingroup identification, resilience, and religious identity), which might allow them to have a level of psychological well-being that is comparable to that of White Americans (see ref. 18 for a discussion of the Black–White Mental Health Paradox), it is well documented that racism continues to maintain and reinforce health disparities between Black and White Americans.
The Present Study
We must deepen our understanding of how racial killings permeate the minds and bodies of those exposed to them. To investigate the impact of Floyd’s murder, we draw on the Gallup COVID-19 Panel survey (117,568 responses from n = 47,355) to compare rates of anger (a response to threat and violation) and sadness (emotional pain associated with loss, despair, and grief) for Black and White Americans before and after his death. Previous work has found that footage of Black Americans experiencing police brutality elicits both emotions in Americans of color (8, 9). Anger and sadness are risk factors for cardiovascular mortality (19) and a symptom of depression (20), respectively. To estimate the mental health impact, we use the US Census Household Pulse data (409,652 responses from n = 319,471) to compare depression and anxiety rates for Black and White Americans before and after Floyd’s death.†
Results
Anger and Sadness.
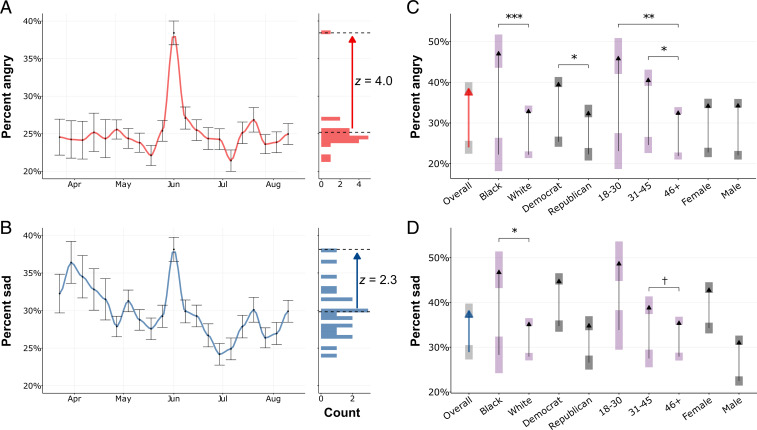
In the Gallup data for the week following Floyd’s death (June 1 to 7), anger increased to 38.4% and sadness to 38.1% of the US population (Fig. 1 A and B). When compared to the four weeks preceding Floyd’s death (April 27 to May 24), this represents a roughly 1.56-fold increase in population anger and a 1.32-fold increase in population sadness (both P values < 0.001), despite elevated levels of both anger and sadness in 2020, as compared to historical mean levels, due to COVID-19.‡
Fig. 1.
(A and B) Weekly percentage of the respondents reporting having experienced anger (A) and sadness (B) in the representative 2020 Gallup Panel COVID-19 survey. Percentages and error bars (indicating SEs) are weighted estimates derived through poststratification on gender, age, race, Hispanic ethnicity, education, and region. Histograms on the right show associated distributions of weeks; the arrows point to the week after Floyd’s death and are labeled with SDs across all 2020 weeks (z scores). (C and D) Increases of anger (C) and sadness (D) experienced by different racial, gender, age, and political groups in the week after Floyd’s death (June 1 to 7) compared to the four baseline weeks (April 27 to May 24); shaded boxes indicate SEs; colors have been added to aid readability. Gallup did not provide weights suitable for the subgroup analysis in C and D; they are unweighted means and SEs. The Overall arrow is based on Gallup weights (same as A and B). Between-bar significances are calculated as the proportion of bootstrapped samples with a greater difference than the observed. *P < 0.05; **P < 0.01; ***P < 0.001; †P < 0.1.
Put differently, compared to all weeks in 2020 for which the data were available, in the week following Floyd’s death, rates of anger increased by z = 4.0 and sadness by z = 2.3 SDs.
This is the largest spike—by far—ever observed in US Gallup phone-survey data.§ For comparison, the week after the mass shooting at Sandy Hook Elementary School resulted in the highest anger and sadness levels reported in historical Gallup data following a violent event—16.1% of the population reported feeling angry and 22.2% sad. Increases in anger and sadness following Floyd’s death were highly significant across demographic and socioeconomic groups (Black, White, Asian, and Hispanic Americans; men and women; Democrats and Republicans; age and income brackets; and Americans with and without college education) (Fig. 1 C and D; all P values 0.002).
Anger and Sadness Among Black Americans.
Previous research suggests that identification as a member of an affected group plays a key role in the experience of collective emotion (21). During the week following Floyd’s death, 47.7% of Black Americans reported feelings of anger, a more than 2.1-fold increase compared to the baseline period (22.3%); and 47.3% reported feelings of sadness (compared to a 28.3% baseline), a 1.67-fold increase (Fig. 1 C and D). On the other hand, White Americans reported a significantly lower increase in anger and sadness (anger, P < 0.001; sadness, P = 0.011); anger increased from 22.2 to 33.5% and sadness from 27.9 to 35.7%.
Depression and Anxiety.
Beyond the experience of acute negative emotions, the mental health of Black Americans is disproportionately impacted by reports of the killing of unarmed Black Americans (11).
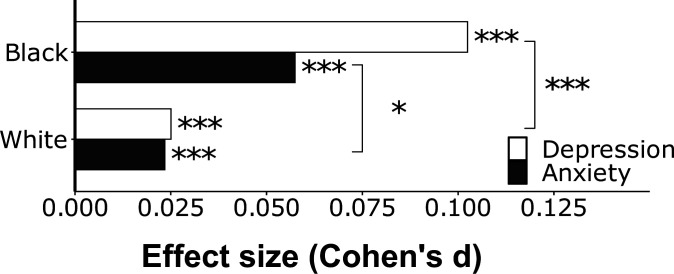
We used data from the US Census Household Pulse Survey to investigate the depression and anxiety impact of Floyd’s death. We compared the responses in the week following Floyd’s death (May 28 to June 2) to the five preceding weeks (April 23 to May 26). To examine the mental health impact, we computed the overall symptom severity for the Patient Health Questionnaire (PHQ-2) depression and Generalized Anxiety Disorder (GAD-2) surveys (as the sum of item scores). We found that depression and anxiety severity increased significantly (P < 0.001) for both White and Black Americans in the week after Floyd’s death.
This increase was significantly larger for Black than for White Americans (depression: Cohen’s d = 0.102 vs. d = 0.025, P < 0.001; anxiety: Cohen’s d = 0.057 vs. d = 0.022, P = 0.019) (Fig. 2). The percentage of Black Americans meeting the customary threshold on the PHQ-2 screener to screen for depression [three points or higher (22)] increased by 3.2% (from 26.7 to 29.9%) in the week after Floyd’s death compared to the preceding five weeks. White Americans experienced an increase of 1.2%.
Fig. 2.
Increases in anxiety and depression as standardized effect sizes (Cohen’s values) comparing the five weeks before Floyd’s death (April 23 to May 26) to the week following Floyd’s death (May 28 to June 2) using data from the US Census Household Pulse survey. Depression was measured by using the PHQ-2 and anxiety using the GAD-2 screener. We used the sum of the person-level item scores to estimate total symptom severity. Estimates incorporate Census-provided weights for age, gender, education, race, and nonresponse. Significance tests of bars are based on a weighted test; significance between bars is based on a test comparing the two values. See SI Appendix for full methods. *P < 0.05; ***P < 0.001.
The Role of Physical Proximity.
Previous work has shown that traumatic collective events related to race and police brutality correlate with mental ill-health and depressive symptoms in the local and regional communities where they occur (3, 9).
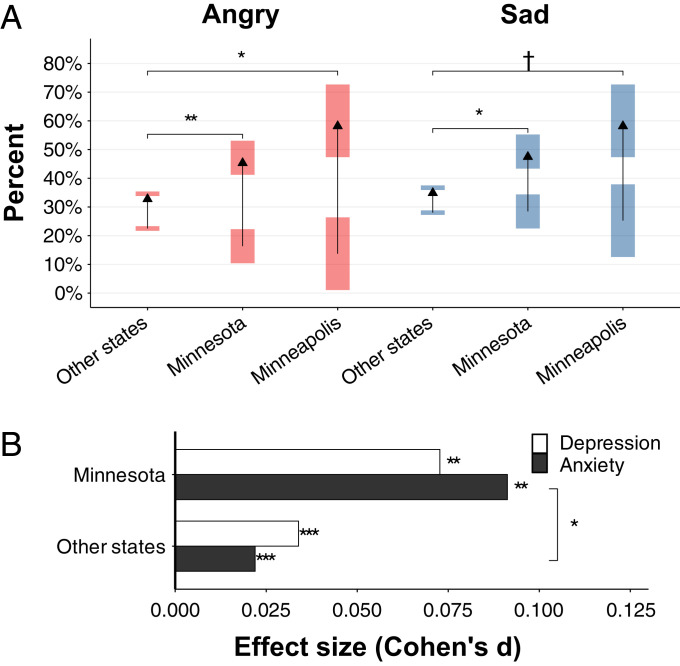
Accordingly, we hypothesized that anger and sadness and depression and anxiety would increase more significantly within Minnesota than in other states in the week following Floyd’s death. We found increases in Minnesota to be significantly larger than in other states for Gallup-measured emotions (anger, P = 0.005; and sadness, P = 0.013), as well as for Census-measured anxiety severity (P = 0.011) (Fig. 3).
Fig. 3.
(A) Increases in sadness and anger reported in the week following Floyd’s death compared to the four baseline weeks (analogous to Fig. 1 C and D). Increases in anger and sadness were significantly larger in Minnesota than in other states during the same period. (B) Increases in anxiety and depression as standardized effect sizes (Cohen’s d values) during the week of Floyd’s death, as compared to the previous five-week baseline period using data from the US Census Household Pulse survey (analogous to Fig. 2). While anxiety and depression symptom severity increased significantly (P < 0.001) nationwide in response to Floyd’s death, these increases were more pronounced in Minnesota. *P < 0.05; **P < 0.01; ***P < 0.001; †P < 0.1.
The increase in effect size with geographic proximity to Floyd’s death offers a further robustness check that the wider population response of increased negative emotion and decreased mental health was due to Floyd’s death.
Discussion
The killing of George Floyd—an unarmed Black man—by a White police officer was filmed in its entirety and shared nationally. Data from a representative Gallup survey of Americans suggest that anger and sadness in the US population increased to unprecedented levels after his death. For anger, in particular, the magnitude of the effect is without comparison in the 2020 and historical Gallup data. The effect was most pronounced for Black Americans; following Floyd’s death, nearly half of Black respondents indicated having felt angry and sad, a response significantly greater than that of White Americans.
Floyd’s death was traumatizing for the Black community. The US Census data suggest that Black Americans had significantly larger increases in depression- and anxiety-symptom severity following Floyd’s death than White Americans did. The depression rate among Black Americans (as measured by the PHQ-2) increased by 3.2% in the week after Floyd’s death, which was 2.05% more than the increase in rate for White Americans.
At a PHQ-2 threshold of three or greater, the PHQ-2 has a sensitivity of 72% and a specificity of 85% for major depressive disorder when compared to semistructured interviews (22). Considering only the 2.05% increase in Black Americans relative to White Americans, this suggests that of 44 million Black Americans, 903,389 would have additionally screened positive for depression as a result of the vicarious trauma experienced by the Black community. Assuming that each of these additional positive screens is associated with three to seven days of mental unhealth, this would translate to between 2.7 million and 6.3 million additional mentally unhealthy days. This estimate is congruent with previous work by Bor et al. (3), who conservatively estimate an additional burden of 55 million mentally unhealthy days for Black Americans due to police killings of unarmed Black Americans.
This burden of poor mental health extends beyond psychological distress. The downstream effects of a depressive episode, for instance, result in negative outcomes for an individual’s physical health, social and professional life, family, and personal wealth (23). Depressed individuals have an increased risk of all-cause mortality and are twice as likely to die prematurely when compared to the general population (24).
Depression leads to decreased productivity and performance in the workplace (23). Over time, such declines can result in demotions, layoffs, or unemployment (25), which further subject Black Americans and their families to economic hardship and precarity.
Our findings offer an important caveat to the literature on the Black–White Mental Health Paradox (i.e., Black Americans exhibit similar or better mental health relative to White Americans): We have identified evidence that collective trauma due to police killings significantly reduces mental health for Black Americans in the period following the killing, while White Americans experience a significantly lower impact. Thus, beyond static conceptions of mental health and lifetime mental health risk measures, racial police killings represent a dynamic shock to the psychological well-being of Black Americans not experienced by White Americans. Additionally, this impact may not be fixed across space. The data suggest that the mental health impact is more pronounced when one lives in close proximity to the killing.
The strong in-group closeness and identification in the face of discrimination and inequality among Black Americans has been suggested as one of the reasons for the relative robustness of Black mental health (18). In the case of highly visible victimization of an in-group member, strong racial identity may engender perceptions of collective threat and vulnerability and the larger sense of “linked fate,” or that one’s fate is inextricably shaped by the fate of the group (16). Monk (16) has found that the perception of linked fate is not protective, but instead associated with higher incidence of unipolar and bipolar depression and anxiety disorders. Monk’s findings suggest that 60% of Black Americans feel a sense of linked fate with one another (16)—it could be the case that the highly visible and emotional murder of George Floyd has increased the percentage of Black Americans experiencing the feeling that “that could have been me or a member of my family” and, thus, foregrounded collective threat and vulnerability in a way that negatively impacts Black mental health. Indeed, in the aftermath of Floyd’s death, Black parents became more worried that their children would experience racial bias and became more likely to prepare their children to experience racial bias (26). The ubiquity of smartphones has increased the likelihood that police killings are captured on video and widely shared, thus increasing the potential number of traumatic exposures for Black Americans. However, we do not wish to imply that the recording and sharing of police killings is the fundamental problem or the right point for intervention; the exposed police brutality against Black Americans is the root problem.
Given research suggesting that those who identify with the affected group are most affected by traumatic group events (21) and our own findings that Black Americans were more impacted by Floyd’s death than White Americans, as were those who lived in close proximity to the killing, it seems reasonable to assume that Black men in Minnesota were particularly impacted by Floyd’s death. One limitation of our study was that the sample sizes in our datasets did not allow us to test this hypothesis directly; future research is needed to test this.
These data highlight the persistent reality of systemic racism in the United States (27, 28). Black Americans are killed by the police at disproportionate rates, which places Black Americans at disproportionate risk for reduced mental health, along with its negative physical health and economic consequences. Among Black Americans, mental health episodes are often more acute, longer-lasting, and more debilitating than for any other race or ethnic group (11).
In order to have a more equitable society in which Black Lives Matter, we must acknowledge that the mental lives of Black Americans matter as well. We must move toward a society where no group is disproportionately burdened by seeing their in-group killed and disproportionately burdened by anger, sadness, depression, and anxiety because of it.
Acknowledgments
We thank Lauris Olson (University of Pennsylvania libraries) for facilitating access to the Gallup data used in this study; and H. Andrew Schwartz for his feedback on this work.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
*These numbers are likely underestimated due to underreporting and difficulty in collecting data (4).
†Both the Gallup and US Census survey designs provide weights to reduce bias. Please see SI Appendix for full methods.
‡Historical mean levels were 14% (SD 0.9%) for anger (measured by Gallup from 2009 to 2013 and 2016) and 17.8% (SD 1.0%) for sadness (2009 to 2016).
§Gallup measured anger in the US 2009–2013, 2016, and 2020; sadness 2009–2016 and 2020.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2109139118/-/DCSupplemental.
Data Availability
Aggregated weekly Census data (for depression and anxiety), analysis code, and Gallup data descriptives (for sadness and anger) are shared in the publicly accessible Open Science Framework repository associated with this article (https://osf.io/ytsae) (29). We are not at liberty to share the Gallup Panel COVID-19 data, which is available from the Gallup organization. The US Census Household Pulse Survey data has been previously published (US Census Bureau, Household Pulse Survey Data Tables. Retrieved from https://www.census.gov/programs-surveys/household-pulse-survey/data.html).
Change History
November 17, 2021: Figure 3 has been updated; please see accompanying Correction for details.
References
- 1.Gallagher R. J., Reagan A. J., Danforth C. M., Dodds P. S., Divergent discourse between protests and counter-protests: #BlackLivesMatter and #AllLivesMatter. PLoS One 13, e0195644 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbot O., George Floyd and our collective moral injury. Am. J. Public Health 9, 1253 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bor J., Venkataramani A. S., Williams D. R., Tsai A. C., Police killings and their spillover effects on the mental health of black Americans: A population-based, quasi-experimental study. Lancet 392, 302–310 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Edwards F., Lee H., Esposito M., Risk of being killed by police use of force in the United States by age, race-ethnicity, and sex. Proc. Natl. Acad. Sci. U.S.A. 116, 16793–16798 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinyangwe S., McKesson D., Elzie J., Mapping police violence. https://mappingpoliceviolence.org/ (Accessed 20 May 2021).
- 6.Washington Post, Police shootings database: 2015-2021 (2021). https://www.washingtonpost.com/graphics/investigations/police-shootings-database/ (Accessed 1 May 2021).
- 7.Giorgi S., et al., Twitter corpus of the #BlackLivesMatter movement and counter protests: 2013 to 2020. arXiv [Preprint] (2020). https://arxiv.org/abs/2009.00596 (Accessed 1 May 2021).
- 8.Williams M. T., Metzger I. W., Leins C., DeLapp C., Assessing racial trauma within a DSM-5 framework: The UConn Racial/Ethnic Stress & Trauma Survey. Pract. Innov. (Wash. D. C.) 3, 242–260 (2018). [Google Scholar]
- 9.Galovski T. E., et al., Exposure to violence during Ferguson protests: Mental health effects for law enforcement and community members. J. Trauma. Stress 29, 283–292 (2016). [DOI] [PubMed] [Google Scholar]
- 10.Ross C. T., A multi-level Bayesian analysis of racial bias in police shootings at the county-level in the United States, 2011–2014. PLoS One 10, e0141854 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams D. R., Stress and the mental health of populations of color: Advancing our understanding of race-related stressors. J. Health Soc. Behav. 59, 466–485 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams D. R., Lawrence J. A., Davis B. A., Racism and health: Evidence and needed research. Annu. Rev. Public Health 40, 105–125 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts S. O., Bareket-Shavit C., Wang M., The souls of Black folks and the weight of Black ancestry in U.S. Black Americans’ racial categorization. J. Pers. Soc. Psychol. (2021, in press). [DOI] [PubMed] [Google Scholar]
- 14.Hicken M. T., Lee H., Morenoff J., House J. S., Williams D. R., Racial/ethnic disparities in hypertension prevalence: Reconsidering the role of chronic stress. Am. J. Public Health 104, 117–123 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sewell A. A., et al., Illness spillovers of lethal police violence: The significance of gendered marginalization. Ethn. Racial Stud. 44, 1089–1114 (2020). [Google Scholar]
- 16.Monk E. P. Jr, Linked fate and mental health among African Americans. Soc. Sci. Med. 266, 113340 (2020). [DOI] [PubMed] [Google Scholar]
- 17.Borrell L. N., Kiefe C. I., Williams D. R., Diez-Roux A. V., Gordon-Larsen P., Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Soc. Sci. Med. 63, 1415–1427 (2006). [DOI] [PubMed] [Google Scholar]
- 18.Keyes C. L., The Black-White paradox in health: Flourishing in the face of social inequality and discrimination. J. Pers. 77, 1677–1706 (2009). [DOI] [PubMed] [Google Scholar]
- 19.Gallo L. C., Matthews K. A., Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychol. Bull. 129, 10–51 (2003). [DOI] [PubMed] [Google Scholar]
- 20.Fried E. I., Epskamp S., Nesse R. M., Tuerlinckx F., Borsboom D., What are ‘good’ depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J. Affect. Disord. 189, 314–320 (2016). [DOI] [PubMed] [Google Scholar]
- 21.Goldenberg A., Garcia D., Halperin E., Gross J. J., Collective emotions. Curr. Dir. Psychol. Sci. 29, 154–160 (2020). [Google Scholar]
- 22.Levis B.et al.; Depression Screening Data (DEPRESSD) PHQ Collaboration , Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression: Systematic review and meta-analysis. JAMA 323, 2290–2300 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lépine J. P., Briley M., The increasing burden of depression. Neuropsychiatr. Dis. Treat. 7 (Suppl. 1), 3–7 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ösby U., Brandt L., Correia N., Ekbom A., Sparén P., Excess mortality in bipolar and unipolar disorder in Sweden. Arch. Gen. Psychiatry 58, 844–850 (2001). [DOI] [PubMed] [Google Scholar]
- 25.Lerner D., Henke R. M., What does research tell us about depression, job performance, and work productivity? J. Occup. Environ. Med. 50, 401–410 (2008). [DOI] [PubMed] [Google Scholar]
- 26.Sullivan J. N., Eberhardt J. L., Roberts S. O., Conversations about race in Black and White US families: Before and after George Floyd’s death. Proc. Nat. Acad. Sci. U.S.A., in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roberts S. O., Rizzo M. T., The psychology of American racism. Am. Psychol. 76, 475–487 (2021). [DOI] [PubMed] [Google Scholar]
- 28.Richeson J. A., Sommers S. R., Toward a social psychology of race and race relations for the twenty-first century. Annu. Rev. Psychol. 67, 439–463 (2016). [DOI] [PubMed] [Google Scholar]
- 29.Eichstaedt J. C., Giorgi S., Sherman G., Guntuku S., The impact of the murder of George Floyd: Data and code. Open Science Framework. https://osf.io/ytsae/. Deposited 20 May 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Aggregated weekly Census data (for depression and anxiety), analysis code, and Gallup data descriptives (for sadness and anger) are shared in the publicly accessible Open Science Framework repository associated with this article (https://osf.io/ytsae) (29). We are not at liberty to share the Gallup Panel COVID-19 data, which is available from the Gallup organization. The US Census Household Pulse Survey data has been previously published (US Census Bureau, Household Pulse Survey Data Tables. Retrieved from https://www.census.gov/programs-surveys/household-pulse-survey/data.html).