Significance
Research has documented the heavy cost COVID-19 mortality has placed on minorities. There is, however, less discussion of the inordinate burden that non–COVID-19 excess mortality (i.e., pandemic-era non–COVID-19 deaths in excess of the historical average) has exacted on this same group. Our analysis shows that minorities, particularly Black, non-Hispanic men, represent a disproportionate share of excess mortality and life years lost from non–COVID-19 causes. Early evidence suggests a combination of factors, including deaths of despair, murders, uninfected Alzheimer’s patients, reduced health care use, and economic dislocation. Moving forward, the challenge for the public health community is to understand the etiology of non–COVID-19 excess mortality and attack it with the same zeal as it attacks the virus.
Keywords: excess mortality, COVID-19, racial disparities
Abstract
The 2020 US mortality totaled 2.8 million after early March, which is 17.3% higher than age-population–weighted mortality over the same time interval in 2017 to 2019, for a total excess death count of 413,592. We use data on weekly death counts by cause, as well as life tables, to quantify excess mortality and life years lost from both COVID-19 and non–COVID-19 causes by race/ethnicity, age, and gender/sex. Excess mortality from non–COVID-19 causes is substantial and much more heavily concentrated among males and minorities, especially Black, non-Hispanic males, than COVID-19 deaths. Thirty-four percent of the excess life years lost for males is from non–COVID-19 causes. While minorities represent 36% of COVID-19 deaths, they represent 70% of non–COVID-19 related excess deaths and 58% of non–COVID-19 excess life years lost. Black, non-Hispanic males represent only 6.9% of the population, but they are responsible for 8.9% of COVID-19 deaths and 28% of 2020 excess deaths from non–COVID-19 causes. For this group, nearly half of the excess life years lost in 2020 are due to non–COVID-19 causes.
Three distinct literatures about the COVID-19 pandemic provide the backdrop for this paper. The first documents that COVID-19 mortality is more heavily concentrated in male and minority populations (1–4). The second shows that the US death count in 2020 has exceeded expected deaths based on the recent historical average (henceforth, “excess” deaths) and that the COVID-19 death count does not entirely explain the gap, meaning deaths from non–COVID-19 causes contribute to above-average mortality in 2020 (5–7). The third literature translates 2020 excess mortality in the US to the life years lost from COVID-19 and non–COVID-19 causes (8–11). In this paper, we merge these three literatures by using data on vital statistics to examine the burden of excess mortality by race/ethnicity, age, and gender/sex. We then use life tables to translate deaths at particular ages into life years lost. As non–COVID-19 excess death rates are high among the young, the fraction of excess deaths that are from COVID-19 is larger than the fraction of life years lost from the virus alone. As non–COVID-19 excess mortality is much more common among males, minorities, and the young, we document that the life years lost from non–COVID-19 excess death is heavily concentrated in minority men.
Results
The Demographics of COVID-19 Mortality and Non–COVID-19 Excess Mortality.
The ongoing COVID-19 pandemic has generated mortality counts for 2020 that exceed historical averages. In the first block of results in Table 1, we report 2,802,948 US deaths after week 9 (the week beginning March 8, which is when the US hit 500 cases) and through week 52 in 2020. Among all-cause deaths, 74% are for those 65 and over, with the corresponding number being 81% for COVID-19 deaths. Using average deaths from 2017 to 2019 as a baseline, we estimate 507,189 excess deaths in 2020. This number is close to the Centers for Disease Control and Prevention (CDC) estimate of 506,412 we get by summing estimated deaths across all states and weeks from their data (12). The average 2017 to 2019 population count on which this estimate is based is very close to the 2020 population for those under 65, but it understates the 2020 population for those 65 and over by 3.4 million. As pointed out by others (13), this demographic shift makes average deaths from 2017 to 2019 a poor measure of expected 2020 deaths; in particular, it is too small.
Table 1.
All-cause, COVID-19, and excess mortality through week 52 of 2020 using different methodologies
| Category | Aged 0–64 | Ages 65+ | Total |
| Data for 2020 | |||
| Population | 274,066,262 | 55,068,822 | 329,135,084 |
| All deaths after week 9, 2020 | 727,885 | 2,075,063 | 2,802,948 |
| COVID-19 deaths, 2020 | 69,681 | 293,198 | 362,879 |
| Data for 2017/2019 | |||
| Average population | 274,182,057 | 51,665,742 | 325,847,799 |
| Excess death calculations using averages of 2017–2019 as baseline | |||
| Predicted deaths after week 9 | 607,493 | 1,688,265 | 2,295,758 |
| Excess deaths after week 9 | 120,391 | 386,798 | 507,189 |
| % excess deaths from COVID-19 | 57.9% | 75.8% | 71.6% |
| Excess death calculations using reweighting averages of 2017–19 deaths with 2020 population | |||
| Predicted deaths after week 9 | 609,370 | 1,779,986 | 2,389,356 |
| Excess deaths after week 9 | 118,515 | 295,077 | 413,592 |
| % excess deaths from COVID-19 | 58.8% | 99.4% | 87.7% |
In the last three rows of Table 1, we predict 2020 deaths after week 9 by calculating the 2017 to 2019 average weekly death rate (i.e., weekly deaths/population at the start of the year) for 16 age groups (namely, 0 to 14, 85+, and every 5-y bin in between), then multiplying this rate by the age-specific population at the start of 2020. We predict 2,389,356 age-adjusted 2020 deaths, meaning there were 413,592 excess deaths after week 9 in 2020. As expected, age-adjusting 2017 to 2019 deaths reduces the number of excess deaths in the 65+ population by nearly 24% but has almost no impact on the under-65 population. Failing to age-adjust overstates the excess deaths by 91,721 in the 65+ age group. This magnitude makes sense. By failing to age-adjust, one understates the 65+ population by 3.4 million, and in the pooled period, there were roughly 32,700 deaths per million in this age group.
The last row of Table 1 shows that total excess deaths in 2020 are driven primarily by the severe acute respiratory virus coronavirus 2, but this is only part of the story. COVID-19 deaths in 2020 totaled 69,681 in the under-65 population and 293,198 in the 65+ population. For the latter group, this figure matches the age-population–weighted excess death prediction almost exactly. However, for the under-65 population, COVID-19 deaths represent less than 60% of predicted excess deaths, meaning these non–COVID-19 deaths represent an 8% increase in total mortality over the 2017 to 19 weighted average.
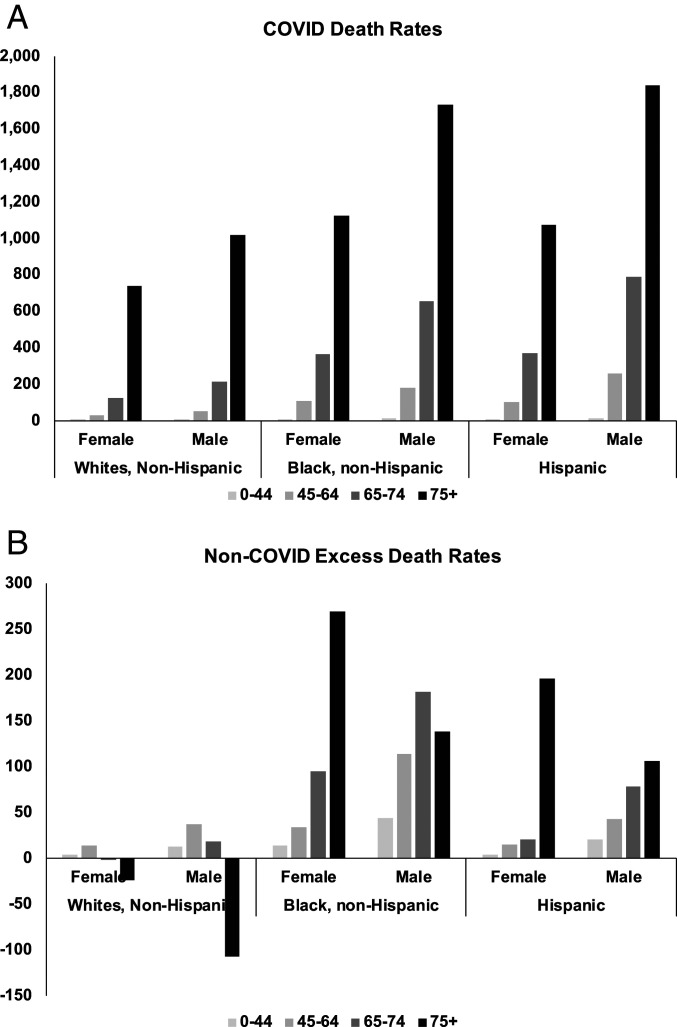
COVID-19 mortality rates are strongly correlated with age, race/ethnicity, and gender/sex. In Fig. 1A, we report COVID-19 mortality rates per 100,000 individuals after week 9 of 2020 for combinations of gender/sex, four age groups (0 to 44, 45 to 64, 65 to 74, and 75+), and three race/ethnicity groups (White, non-Hispanic; Black, non-Hispanic; and Hispanic). Although more age-group breakdowns are possible, these groups are sufficient for this purpose. We only report these three race/ethnic groups, which represent 93% of the population and 94% of COVID-19 deaths to date, because we will eventually merge in life-table data, and these three groups are the ones for which data are reported by the National Center for Health Statistics (NCHS).
Fig. 1.
Death rates (deaths/100,000) from COVID-19 (A) and excess deaths from non–COVID-19 causes (B) by age, gender/sex, and race/ethnicity through week 46 of 2020. Rates are age standardized within each age, gender/sex, and race/ethnicity group, that is, we weight the NCHS death rate for each 5-y age bin within the larger age interval by the size of the relevant population.
A full accounting of the non–COVID-19 excess mortality is currently not possible, but a variety of data sources suggest that the causes are varied. Although overall crime rates have fallen during the pandemic (14), murder rates have increased dramatically in many areas (15), reaching historical levels in some cities (16). There is evidence that deaths of despair (17, 18) (e.g., drug deaths, alcohol-related mortality, and suicides) have increased (19–22), but the latest evidence suggests suicides fell in 2020 (23). Early in the pandemic, health care use for non–COVID-19 reasons plummeted, possibly delaying necessary medical care and raising mortality (24, 25). Outpatient visits remained below historic levels in aggregate through late June and for some demographic groups (e.g., kids) and specialties (e.g., pulmonology and otolaryngology) through at least October (26, 27). Deaths among Alzheimer’s patients without a COVID-19 diagnosis have increased dramatically (28–30). Relatedly, although COVID-19 mortality among nursing home residents has been particularly high, there is also evidence of substantial non–COVID-19 excess mortality in nursing homes (31). Researchers have attributed these non–COVID-19 deaths to both difficulty in obtaining needed medical care due to extreme staff shortages as well as social isolation generated by efforts to stave off the spread of the virus within congregate settings (32–34). Finally, worse than usual hospital conditions (e.g., lacking supplies and staff, crowded emergency and intensive care units, etc.) have been reported in high-infection areas and likely contribute to excess mortality (35, 36). In the rest of the paper, we will refer to excess mortality as coming from COVID-19 and non–COVID-19 causes.
Three clear patterns, which others have documented, can be observed in Fig. 1A. Within each dyad, the COVID-19 mortality rate is always highest for males, highest for minorities, and sharply increasing in age. All else being equal, the age gradient is the most pronounced; the oldest group has a mortality rate that is nearly 200 times the youngest group. Holding age constant, minority males are particularly vulnerable, with a death rate 22% higher than White males. Across all races/ethnicities and ages, the male death rate exceeds that of females; the ratio ranges from a low of 1.25 for White, non-Hispanics aged 75+ to a high of 2.48 for Hispanics 0 to 44.
In Fig. 1B, we report the death rate for non–COVID-19 excess mortality across combinations of the same demographics. The expected mortality is calculated using 2017 to 2019 deaths by age/race/ethnicity/gender cell and age-adjusting to the 2020 population. A number of interesting patterns emerge. First, unlike COVID-19 death rates, there is not a consistent age gradient in non–COVID-19 excess mortality; rates are increasing in age for minority women and Hispanic men, but no other groups. Second, non–COVID-19 excess death rates are relatively low among non-Hispanic White individuals and Hispanic women, with a few exceptions. Hispanic females over the age of 75, who comprise just 0.4% of the US population, have the second highest non–COVID-19 excess death rate. Non-Hispanic White males under the age of 65, who comprise a more substantial 26% of the US population, have a non–COVID-19 excess death rate that is similar to the COVID-19 death rate for this group (14.7 versus 18.2). Third, among individuals 45 to 75, the Black, non-Hispanic non–COVID-19 excess death rate greatly exceeds that of other races/ethnicities. For this age group, the Black/White ratio of non–COVID-19 excess death rates is 4.7 for males and 8.5 for females; the Black/Hispanic ratio is 2.8 for males and 3.4 for females. Finally, non-Hispanic, White males and females over the age of 75 have substantial negative excess mortality from non–COVID-19 causes (i.e., 2017 to 2019 mortality exceeds 2020 non–COVID-19 mortality).
The age groups in Fig. 1 A and B vary considerably in size. Moving from the youngest to oldest group, the populations of the four age groups are 176.6, 77.7, 30.4, and 21.8 million. The disparities in the mortality rates by age and population mean two things. First, COVID-19 death counts are somewhat more even across age groups, as the younger groups are both larger in size and have lower rates. Second, compared to COVID-19 mortality rates, which are highest in older and less populous age groups, non–COVID-19 excess mortality rates are relatively high in younger, more populous age groups. This difference in COVID-19 and non–COVID-19 excess mortality rates across the age distribution means that although COVID-19 represents almost 90% of excess deaths, the virus accounts for a much smaller fraction of excess life years lost.
The Life Years Lost from COVID-19 and Non–COVID-19 Excess Mortality.
Using lifetables defined by race/ethnicity, age, and gender/sex, we calculate the life years lost from COVID-19 deaths and non–COVID-19 excess mortality. We first aggregate counts across age groups in each distinct gender/sex and race/ethnicity dyad. We then aggregate counts across race/ethnicity for males and females, across gender/sex for non-Hispanic White individuals and minorities, and finally for everyone—i.e., aggregate counts only include the three race/ethnicity groups we consider. We present these results in Table 2.
Table 2.
Excess death and life year lost by gender/sex and race/ethnicity through week 52 of 2020
| Excess deaths | Life years lost from excess mortality (in millions) | |||||||||
| Group | Percentage of population | All | Excess deaths | From COVID-19 | Not COVID-19–related | Percentage excess deaths from COVID-19 | All | From COVID-19 | Not COVID-19–related | Percentage life years lost from COVID-19 |
| All | 100.0% | 3,194,767 | 395,005 | 342,656 | 52,349 | 86.7% | 6.03 | 4.32 | 1.71 | 71.6% |
| Females | 50.7% | 1,525,906 | 174,368 | 157,450 | 16,918 | 90.3% | 2.31 | 1.87 | 0.44 | 81.0% |
| Males | 49.3% | 1,668,861 | 220,637 | 185,206 | 35,431 | 83.9% | 3.71 | 2.44 | 1.27 | 65.8% |
| White | 65.9% | 2,451,950 | 234,111 | 218,558 | 15,553 | 93.4% | 2.93 | 2.22 | 0.71 | 75.8% |
| Black/Hispanic | 34.1% | 742,817 | 160,894 | 124,098 | 36,796 | 77.1% | 3.09 | 2.09 | 1.00 | 67.7% |
| Non-Hispanic White females | 33.4% | 1,189,712 | 108,807 | 105,064 | 3,743 | 96.6% | 1.19 | 1.02 | 0.17 | 85.9% |
| Non-Hispanic White males | 32.5% | 1,262,238 | 125,304 | 113,494 | 11,810 | 90.6% | 1.75 | 1.20 | 0.54 | 68.9% |
| Non-Hispanic Black females | 7.5% | 207,476 | 36,658 | 27,602 | 9,056 | 75.3% | 0.61 | 0.41 | 0.19 | 68.1% |
| Non-Hispanic Black males | 6.9% | 233,008 | 45,449 | 30,583 | 14,866 | 67.3% | 0.87 | 0.45 | 0.42 | 51.2% |
| Hispanic females | 9.8% | 128,718 | 28,903 | 24,784 | 4,119 | 85.7% | 0.52 | 0.44 | 0.08 | 84.7% |
| Hispanic males | 10.0% | 173,615 | 49,884 | 41,129 | 8,755 | 82.4% | 1.10 | 0.79 | 0.30 | 72.4% |
The left-hand portion of Table 2 focuses on death counts by cause. The final six rows report statistics for each unique gender/sex and race/ethnicity dyad. For White women, COVID-19 deaths represent 96.6% of excess mortality. At the other end of the spectrum, the COVID-19 virus is only responsible for 67.3% of excess mortality for Black males. Once we aggregate across gender/sex, we see a stark difference in outcomes for non-Hispanic White individuals and minorities. Ninety-three percent of excess deaths are due to COVID-19 for White individuals but just 77% for minorities.
In the right-hand portion of Table 2, we report life years lost in millions of years by subgroup. The more than 395,000 excess deaths in 2020 generate just over 6 million life years lost, but only 71.6% of this loss is directly attributable to the virus. These numbers vary considerable by gender/sex and race/ethnicity. COVID-19 is directly responsible for roughly 86% of the life years lost among White females, 72% among Hispanic males, and just 51% among Black males. Compared to females, the relative burden of non–COVID-19 excess mortality on males is greater when measured in life years lost (65.8 versus 81%) than when measured using excess death counts (83.9 versus 90.3%), indicating that non–COVID-19 excess mortality for males occurs at younger ages than for females. A similar pattern can be observed for non-Hispanic White individuals compared to the other races/ethnicities—that is, non–COVID-19 excess mortality strikes White individuals at younger ages, leading to a greater number of life years lost per death.
The numbers in Table 2 indicate the high burden of both COVID-19 and non–COVID-19 excess mortality on minorities and especially Black, non-Hispanic males. For the population we consider, minorities comprise 34% of the sample but represent 36% of COVID-19 deaths, 70% of non–COVID-19 excess mortality, 50% of life years lost due to excess mortality, and 58% of life years lost from non–COVID-19 excess deaths. These disparities are even greater for non-Hispanic, Black males; they comprise just under 7% of the population but represent 11.5% of all excess deaths, 28% of non–COVID-19 excess deaths, and 24.5% of life years lost due to non–COVID-19 excess deaths. For this group, nearly half of the excess life years lost in 2020 was due to non–COVID-19 causes.
Discussion
Roughly 13% of the excess mortality observed in 2020 is due to non–COVID-19 causes. Although the current data do not allow a complete accounting of what is causing these deaths, circumstantial evidence suggests that many non–COVID-19 deaths are driven by the shutdown of the economy and efforts to increase social distancing to combat the virus. The high rates of deaths of despair, murders, and uninfected Alzheimer’s patients, plus the massive decline in health care use throughout the pandemic, indicate that the economic dislocation associated with efforts to quell the spread of the disease may have had some negative health costs.
Non–COVID-19 excess deaths are particularly common among middle-aged minority men, for whom economic dislocation has been common in 2020. Using data from the Current Population Survey, we calculate that in the 12 mo preceding March 2020, the unemployment gap between Black, non-Hispanic men and White, non-Hispanic men was 3.8 percentage points (SI Appendix, Fig. S2). By July of 2020, this gap had increased to 7.5 percentage points, and this gap was still 5.4 percentage points by November 2020. The numbers are similar for Hispanic men in that they had a 1 percentage point higher unemployment rate than White, non-Hispanic men in the 12 mo from March 2019 through February 2020. This gap balloons to 6.3 percentage points in May of 2020 and stands at 3 percentage points in November of 2020. These figures in no way prove that economic dislocation is in fact the cause of non–COVID-19 excess mortality. They do, however, suggest that although the virus itself has been particularly devastating for minorities, the concentration of excess death from non–COVID-19 causes is placing an even greater burden on minorities, especially Black, non-Hispanic males. For this latter group, a nearly equivalent number of life years have been lost from non–COVID-19 excess deaths as COVID-19 deaths. Health policy makers need a much better understanding of what is driving excess mortality from non–COVID-19 causes, as the effects are widening already cavernous differences.
Limitations.
Our key finding is that minorities in the US have shouldered a disproportionate share of the 2020 non–COVID-19 excess deaths. An important concern is the source of these deaths and, in particular, whether this finding can be explained by the fact that some COVID-19 deaths are not measured. While uncounted COVID-19 deaths certainly contribute to the non–COVID-19 total, we find mismeasurement to be an unlikely explanation for the racial/ethnic disparity. There are several reasons for this.
First, COVID-19 deaths that occur outside of a medical facility are much more likely to be miscoded; however, in 2019, non-Hispanic Black individuals over the age of 65 were no more likely to die at home than non-Hispanic White individuals (30.2 versus 30.7%), while Hispanics were only slightly more likely to die at home (35.2%) (37) (SI Appendix, Fig. S3).
Second, there are several reasons to believe that COVID-19 deaths were more likely to be undercounted at the start of the pandemic; for example, it was roughly mid-April before the US consistently exceeded 150,000 daily tests (38), and it became widely known that COVID-19 could cause deadly blood clotting in some instances (39). A total of 71% of non–COVID-19 excess deaths occur after week 18 (the week ending May 2). For minorities, this number is 70%. Moreover, minorities account for 69% of all non–COVID-19 excess deaths after week 18. Were minorities disproportionately affected by mismeasurement, we would expect their deaths to account for a smaller share of the late-year non–COVID-19 excess death total.
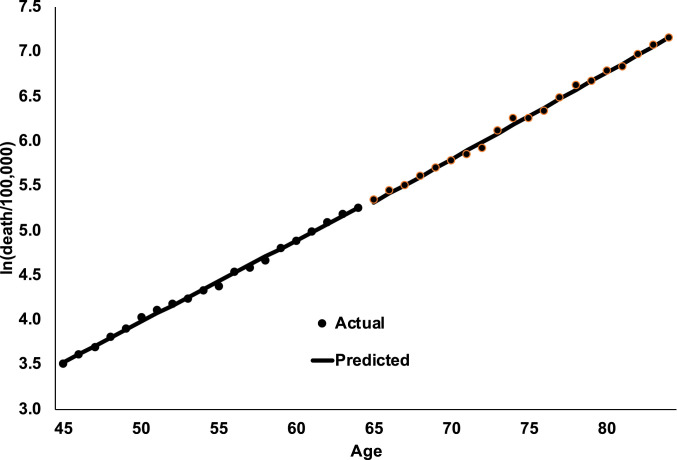
Third, there could be systematic/strategic reasons COVID-19 is mismeasured, which could differentially impact those of different races, ethnicities, or ages. For example, there is a financial incentive to identify whether a Medicare patient is COVID-19 positive, as the Centers for Medicare and Medicaid increased inpatient reimbursement rates by 20% for this group (40). If this differential incentive affects COVID-19 testing and/or coding, we would expect to see a spike in deaths from COVID-19 at age 65, when most people become eligible for Medicare. This can easily be tested with a regression discontinuity model (RDD) model. In Fig. 2, we report the natural log of COVID-19 death rates (deaths per 100,000) for all single years of age from 45 to 84 (black dots). We estimate a standard RDD model with linear trends in age and test whether there is a spike in death rates at age 65. These lines essentially show a Gompertz equation in ln(death rates) that is linear in age, with no discernable spike in deaths at age 65. This suggests that in this case, in which there is serious financial incentive to identify COVID-19 deaths, it is not occurring. Ideally, we would like to estimate similar models for different race/ethnic groups, but those data are currently not available.
Fig. 2.
Regression discontinuity design estimates of Ln(COVID-19 deaths/100,000) by age, through the end of 2020.
In addition to the above evidence, Fig. 1 makes it clear that while COVID-19 has been incredibly deadly for the elderly, the non–COVID-19 excess death burden has fallen on younger individuals. Were mismeasurement the primary cause of non–COVID-19 excess death, we might expect these age distributions to look more similar. Moreover, excess deaths among the young and among minorities fit the current narrative regarding an increase in mortality related to unintentional injuries (including drug poisonings) (41) and homicides (15). There is little doubt that some of the excess death we label “non–COVID-19” are truly mismeasured COVID-19 deaths; however, the evidence above suggests that measurement error represents a small share of these excess deaths and, more importantly, does not explain the large racial/ethnic disparity in non–COVID-19 excess death rates.
Methods
We use data from the NCHS that report weekly counts of COVID-19 and total deaths by week, gender/sex, age, race and ethnicity for the years 2015 to 2020 (42). We pulled data from the NCHS web page on April 1, 2021, which includes data reported by all states through week 52, which ended December 26, 2020. The final 5 d of 2020 are reported in week 1 of 2021. In these data, the NCHS reports death counts in age bins of 0 to 14, 5-y groups from 15 to 19 through 80 to 84, then 85 and above. We used population by gender/sex, age, race, and ethnicity as of January for 2017 to 2020 from the Census (43).
To calculate excess mortality in Table 2, we compare 2020 weekly deaths to the average weekly deaths from 2017 to 2019, age-adjusted by cell to the 2020 population. Although deaths by week are available back to 2015, we use data from the final three years as the baseline because the weekly death average in these years generated the highest correlation coefficient with weekly data from the first eight weeks of 2020 (the week ending February 22), when there were few COVID-19 deaths. In SI Appendix, Table S1, we recalculate excess death counts for the over and under 65 population using several alternative sets of prepandemic years. The difference between the highest and lowest excess death predictions across these different methods is only 6%.
Both COVID-19 and non–COVID-19 death rates in Fig. 1 are age-standardized within each age, gender/sex, and race/ethnicity group. In other words, we weight the NCHS death rate for each 5-y age bin within the larger age interval by the size of the relevant population. This addresses any concern that differences in death rates are explained by certain cohorts being younger or older on average than cohorts falling in the same age interval that are of a different gender/sex or race/ethnicity. Fig. 1 looks virtually identical without this adjustment.
We merge our main data file to NCHS life tables (44) to estimate the life years lost for different deaths. In SI Appendix, Fig. S1, we show that the distribution of COVID-19 deaths across different ages looks similar to the distribution of total deaths across different ages in 2019. Thus, for each age bin, we calculate the weighted average of life years lost across all ages within the bin, using age-specific 2019 death rates as the weights. Death counts for 2019 are taken from the CDC Wonder web page for the underlying cause of death (45). Basic results in Table 2 are virtually unchanged whether we use this method, the life years lost estimate for the middle age (e.g., we use life tables for 17 y olds for those aged 15 to 19, 7 y olds in the 0 to 14 age group, and for 91 y olds in the 85+ group), or the unweighted average life years left across the ages in in bin (for a comparison, SI Appendix, Table S2). The life tables report age-specific estimates for the entire population, for males and females, and by gender/sex for White non-Hispanics, Black non-Hispanics, and Hispanics. Because these life-table estimates are not available for other racial groups, when we disaggregate results by race/ethnicity, we only use these three groups.
Supplementary Material
Acknowledgments
We gratefully acknowledge the support of Notre Dame Research. We have not presented the findings at any conferences. We thank Elaine Griffin and Graham Ryan for excellent research assistance. No one else has contributed to this work.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission. N.G. is a guest editor invited by the Editorial Board.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2101386118/-/DCSupplemental.
Data Availability
The .csv data have been deposited in GitHub (https://github.com/christophercronin/PNAS2021) (46). All other data are included in the manuscript and/or supporting information.
References
- 1.Tai D. B. G., Shah A., Doubeni C. A., Sia I. G., Wieland M. L., The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin. Infect. Dis. 72, 703–706 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bassett M. T., Chen J. T., Krieger N., Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: A cross-sectional study. PLoS Med. 17, e1003402 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossen L. M., Branum A. M., Ahmad F. B., Sutton P., Anderson R. N., Excess deaths associated with COVID-19, by age and race and ethnicity – United States, January 26-October 3, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 1522–1527 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andrasfay T., Goldman N., Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proc. Natl. Acad. Sci. U.S.A. 118, e2014746118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Woolf S. H., Chapman D. A., Sabo R. T., Weinberger D. M., Hill L., Excess deaths from COVID-19 and other causes, March-April 2020. JAMA 324, 510–513 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woolf S. H., et al., Excess deaths from COVID-19 and other causes, March-July 2020. JAMA 324, 1562–1564 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weinberger D. M., et al.; Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern. Med. 180, 1336–1344 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldstein J. R., Lee R. D., Demographic perspectives on the mortality of COVID-19 and other epidemics. Proc. Natl. Acad. Sci. U.S.A. 117, 22035–22041 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quast T., Andel R., Gregory S., Storch E. A., Years of life lost associated with COVID-19 deaths in the United States. J. Public Health (Oxf.) 42, 717–722 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitra A. K., et al., Potential years of life lost due to COVID-19 in the United States, Italy, and Germany: An old formula with newer ideas. Int. J. Environ. Res. Public Health 17, 4392 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christakis D. A., Van Cleve W., Zimmerman F. J., Estimation of US children’s educational attainment and years of life lost associated with primary school closures during the coronavirus disease 2019 pandemic. JAMA Netw. Open 3, e2028786 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention , Weekly counts of deaths by jurisdiction and age. https://data.cdc.gov/NCHS/Weekly-counts-of-deaths-by-jurisdiction-and-age-gr/y5bj-9g5w/. Accessed 11 April 2021.
- 13.Shiels M. S., et al., Impact of population growth and aging on estimates of excess US deaths during the COVID-19 pandemic, March to August 2020. Ann. Intern. Med. 174, 437–443 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abrams D. S., COVID and crime: An early empirical look. J. Public Econ. 194, 104344 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenfeld R., Abt T., Lopez E., Pandemic, social unrest, and crime in U.S. cities, 2020 year-end update. https://covid19.counciloncj.org/2021/01/31/impact-report-covid-19-and-crime-3/. Accessed 31 August 2021.
- 16.Barrett D., 2020 saw an unprecedented spike in homicides from big cities to small towns. Washington Post, December 30, 2020. https://www.washingtonpost.com/national-security/reoord-spike-murders-2020/2020/12/30/1dcb057c-4ae5-11eb-839a-cf4ba7b7c48c_story.html. Accessed 31 August 2021.
- 17.Case A., Deaton A., Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. U.S.A. 112, 15078–15083 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Case A., Deaton A., Mortality and morbidity in the 21st century. Brookings Pap. Econ. Act. 2017, 397–476 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mulligan C. B., Deaths of Despair and the Incidence of Excess Mortality in 2020. National Bureau of Economic Research [Preprint] (2020). https://www.nber.org/papers/w28303 (Accessed 31 August 2021).
- 20.Glober N., et al., Impact of COVID-19 pandemic on drug overdoses in Indianapolis. J. Urban Health 97, 802–807 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slavova S., Rock P., Bush H. M., Quesinberry D., Walsh S. L., Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 214, 108176 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention , Overdose deaths accelerating during COVID-19. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html. Accessed 17 December 2020.
- 23.Ahmad F. B., Anderson R. N., The leading causes of death in the US for 2020. JAMA 325, 1829–1830 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ziedan E., Simon K. I., Wing C., Effects of state COVID-19 closure policy on non-COVID-19 health care utilization. National Bureau of Economic Research [Preprint] (2020). https://www.nber.org/papers/w27621 (Accessed 31 August 2021).
- 25.Patel S. Y., et al., Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern. Med. 181, 388–391 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chatterji P., Li Y., Effects of the COVID-19 pandemic on outpatient providers in the United States. Med. Care 59, 58–61 (2021). [DOI] [PubMed] [Google Scholar]
- 27.Mehrotra A., Chernew M., Linetsky D., Hatch H., Cutler D., Schneider E., The impact of the COVID-19 pandemic on outpatient care: Visits return to prepandemic levels, but not for all providers and patients. Commonwealth Fund, 15 October 2020. https://www.commonwealthfund.org/publications/2020/oct/impact-covid-19-pandemic-outpatient-care-visits-return-prepandemic-levels. Accessed 5 April 2021.
- 28.de Havenon A., Ney J. P., Callaghan B., Yaghi S., Majersik J. J., Excess neurological death in New York City after the emergence of COVID-19. J. Neurol. 268, 2026–2028 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wan W., Panic isolation has killed thousands of Alzheimer’s patients while families watch from afar. Washington Post, 1 September 2020. https://www.washingtonpost.com/health/2020/09/16/coronavirus-dementia-alzheimers-deaths/?arc404=true. Accessed 3 March 2021.
- 30.Centers for Disease Control and Prevention , Excess deaths associated with COVID-19. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm. Accessed 3 March 2021.
- 31.Cronin C. J., Evans W. N., Nursing home quality, COVID-19 deaths, and excess mortality. National of Bureau of Economics [Preprint] (2020). https://www.nber.org/papers/w28012 (Accessed 31 August 2021). [DOI] [PMC free article] [PubMed]
- 32.McGarry B. E., Grabowski D. C., Barnett L., Severe staffing and personal protective equipment shortages faced by nursing homes during the COVID-19 pandemic: Study examines staffing and personal protective equipment shortages faced by nursing homes during the COVID-19 pandemic. Health Aff. 39, 1812–1821 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu H., Intrator O., Bowblis J. R., Shortages of staff in nursing homes during the COVID-19 pandemic: What are the driving factors? J. Am. Med. Dir. Assoc. 21, 1371–1377 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Levere M., Rowan P., Wysocki A., The adverse effects of the COVID-19 pandemic on nursing home resident well-being. J. Am. Med. Dir. Assoc. 22, 948–954.e2 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Courage K. H., COVID-overwhelmed hospitals strain staff and hope to avoid rationing care. Scientific American, 27 January 2021. https://www.scientificamerican.com/article/covid-overwhelmed-hospitals-strain-staff-and-hope-to-avoid-rationing-care1/. Accessed 3 March 2021. [Google Scholar]
- 36.Wilde H., et al., The association between mechanical ventilator availability and mortality risk in intensive care patients with COVID-19: A national retrospective cohort study. medRxiv [Preprint] (2021). 10.1101/2021.01.11.21249461 (Accessed 31 August 2021). [DOI] [PMC free article] [PubMed]
- 37.Wonder CDC, Current multiple cause of death data. https://wonder.cdc.gov/mcd.html. Accessed 1 April 2021.
- 38.COVID Tracking Project , US daily testing. https://covidtracking.com/data/charts/us-daily-tests. Accessed 4 March 2021.
- 39.Cha A. E., A mysterious blood-clotting complication is killing coronavirus patients. Washington Post, 22 April 2020. https://www.washingtonpost.com/health/2020/04/22/coronavirus-blood-clots/. Accessed 29 March 2021.
- 40.Morse S., CMS adds 20% to inpatient Medicare COVID-19 patients. Healthcare Finance, 18 August 2020. https://www.healthcarefinancenews.com/news/cms-adds-20-inpatient-medicare-payment-covid-19-patients. Accessed 31 August 2021.
- 41.Ahmad F. B., Anderson R. N., The leading causes of death in the US for 2020. JAMA 325, 1829–1830 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Center for Health Statistics , Excess deaths associated with COVID-19. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm. Accessed 1 April 2021.
- 43.US Census Bureau , Census 2020 population figures. https://www.census.gov/data/tables/time-series/demo/popest/2010s-national-detail.html. Accessed 29 March 2021.
- 44.Centers for Disease Control and Prevention , Life tables. https://www.cdc.gov/nchs/products/life_tables.htm. Accessed 14 December 2020.
- 45.Centers for Disease Control and Prevention , Mortality data on CDC Wonder. https://wonder.cdc.gov/Deaths-by-Underlying-Cause.html. Accessed 1 April 2021.
- 46.Cronin C. J., Evans W. N., Excess mortality from COVID and non-COVID causes in minority populations. GitHub. https://github.com/christophercronin/PNAS2021. Deposited 21 July 2021. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The .csv data have been deposited in GitHub (https://github.com/christophercronin/PNAS2021) (46). All other data are included in the manuscript and/or supporting information.