Abstract
We present a case of Grade II, well-differentiated rectal neuroendocrine tumor in a 39-year-old patient. Following different sequential treatment modalities, the disease progressed both on metabolic (18F-fluorodeoxyglucose positron emission tomography-computed tomography [18F-FDG PET/CT]) and somatostatin receptor (SSTR)-imaging (68Ga-DOTA-Tyr3-octreotate [68Ga-DOTATATE] PET/CT), and the patient received three cycles of peptide receptor radiotherapy (PRRT). Two years later, upon new progression due to the appearance of metabolically active, 68Ga-DOTATATE PET/CT-negative liver lesions, targeted treatment with everolimus was introduced. Further morphologic and metabolic progression occurred 4 months after everolimus initiation, however, this time liver lesions demonstrated increased SSTR-expression on68Ga-DOTATATE PET/CT. Thus, the patient became eligible for a second PRRT course.
Keywords: Everolimus, peptide receptor radiotherapy, somatostatin receptor, up-regulation
INTRODUCTION
Neuroendocrine neoplasms (NENs) most commonly originate from the gastrointestinal tract and pancreas. Although they make up only about 2% of all gastroenteropancreatic (GEP) tumors, their incidence has increased over the past two decades.[1] Most GEP-NENs are well-differentiated neuroendocrine tumors (NETs). Peptide receptor radiotherapy (PRRT) is an established effective therapeutic option in progressive somatostatin receptor (SSTR)-positive NETs.[2] Since one of the main determinants for using PRRT is the presence of high SSTR-expression in tumors, a variety of drugs as well as radiation have been shown to upregulate SSTRs expression of NETs in an attempt to improve PRRT efficacy.[3] Through its inhibition of the mammalian target of rapamycin, everolimus not only regulates cell growth and proliferation in NETs but has also a direct radiosensitization and antiangiogenic effect.[3] However, a SSTR-upregulation following everolimus has not yet been well established in NENs. Here, we present a case of a Grade II, well-differentiated rectal NET, in which following everolimus, we observed reappearance of high uptake on 68Ga-DOTA-Tyr3-octreotate (68Ga-DOTATATE) positron emission tomography (PET)/computed tomography (CT) imaging of previously SSTR-negative liver metastases.
CASE REPORT
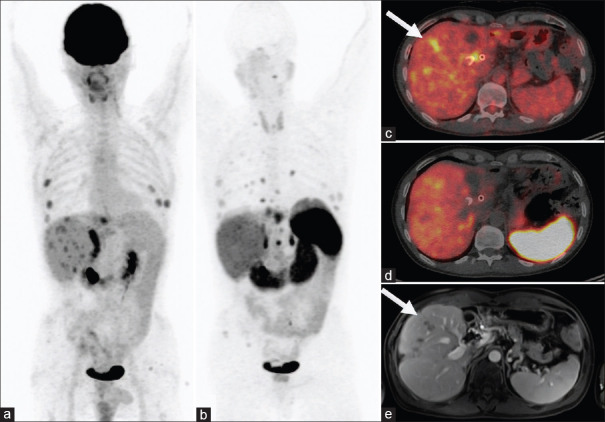
A 39-year-old male patient was diagnosed with well-differentiated rectal NET (Grade II, Ki67: 10%) and synchronous hepatic, bone, and pulmonary metastases. After unsuccessful treatment with three cycles of cisplatin/irinotecan, the patient underwent pelvic external beam radiotherapy with subsequent surgical resection of the primary tumor and whole liver selective internal radiotherapy (SIRT) with 90Y-microspheres. Post-SIRT 68Ga-DOTATATE PET/CT exhibited disease progression, thus 177Lu-DOTATATE PRRT was initiated (the total administered activity of 22.5GBq, divided into three cycles), achieving near-complete response. The disease progressed 2 years after the last PRRT with the appearance of new, metabolically active liver lesions, successfully treated by three cycles of capecitabine/temozolomide (CAPTEM) chemotherapy achieving a complete metabolic response with no signs of disease on abdominal magnetic resonance imaging (MRI). Complete response was sustained for 4 months when new liver lesions appeared on the 18F-fluorodeoxyglucose (18F-FDG) PET/CT [Figure 1a and c]. 68Ga-DOTATATE PET/CT confirmed the extrahepatic progression of the disease, however, no SSTR over-expression was observed in the metabolically active new liver lesions [Figure 1b and d]. Contrast-enhanced abdominal MRI confirmed the morphological progression in the liver [Figure 1e] and due to the absence of metabolic response after one cycle of reintroduced CAPTEM, targeted treatment with everolimus was initiated.
Figure 1.
Metabolically active liver metastases of a rectal neuroendocrine tumor (a, c, e), showing no 68Ga-DOTA-Tyr3-octreotate uptake (b and d)
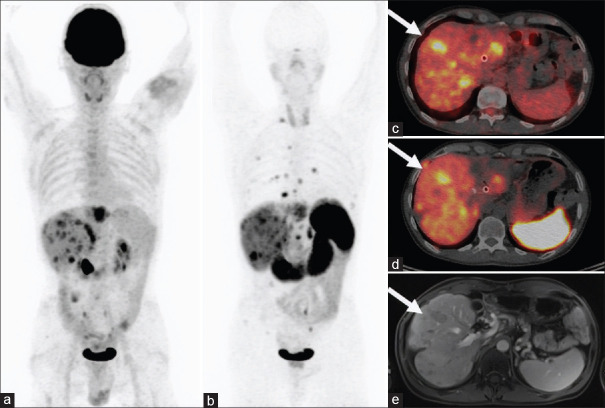
After 4 months under everolimus, further progression of the preexisting liver lesions was observed on 18F-FDG PET/CT [Figure 2a and c] as well on the abdominal MRI [Figure 2e], but interestingly, they presented with increased radiotracer uptake on the 68Ga-DOTATATE PET/CT [Figure 2b and d]. This phenomenon suggests that during treatment with everolimus an over-expression of SSTRs in the liver lesions has occurred, making the patient eligible for a second course of PRRT.
Figure 2.
Disease progression with increased number and size of metabolically active liver lesions after 4 months of treatment with everolimus (a, c, e); however, appearing of increased uptake on 68Ga-DOTA-Tyr3-octreotate positron emission tomography-computed tomography imaging (b and d)
DISCUSSION
Recently published in vitro data have demonstrated that certain drugs can up-regulate SSTRs in different NET cell lines through alterations in the epigenetic regulatory mechanisms.[4] Nölting et al., showed the upregulation of SSTR-subtype 2 expression in pancreatic and pulmonary NET cell lines under everolimus alone or synergistically combined with a selective PI3K inhibitor.[5] In a clinical setting, everolimus has been shown to significantly decrease Ki67 in NETs on repeated biopsies after treatment initiation[6](raising the hypothesis of a possible not only decrease of the rate of proliferation but also, promotion of the cellular differentiation). These results provide a plausible explanation for the disease evolution that we observed in our patient, which cannot solely be attributed to the morphological progression of the lesions. To the best of our knowledge, only two similar clinical cases have been published so far, where everolimus or CAPTEM chemotherapy resulted in markedly increased 68Ga-DOTATATE uptake in the tumor lesions.[7,8]
Several reports about targeted agents, immune checkpoint inhibitors, and combination of agents (e.g., RAF and MEK inhibitors) already show promises in re-differentiation of radioiodine-resistant thyroid cancers, where they could improve the efficacy of radioiodine therapy.[9] In NET patients, further in vivo research is necessary to investigate on SSTRs up-regulation under everolimus, with the purpose of improving and optimizing therapeutic management, especially PRRT.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3:1335–42. doi: 10.1001/jamaoncol.2017.0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hope TA, Bodei L, Chan JA, El-Haddad G, Fidelman N, Kunz PL, et al. NANETS/SNMMI consensus statement on patient selection and appropriate use of 177lu-DOTATATE peptide receptor radionuclide therapy. J Nucl Med. 2020;61:222–7. doi: 10.2967/jnumed.119.240911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adant S, Shah GM, Beauregard J-M. Combination treatments to enhance peptide receptor radionuclide therapy of neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2020;47:907–21. doi: 10.1007/s00259-019-04499-x. [DOI] [PubMed] [Google Scholar]
- 4.Veenstra MJ, van Koetsveld PM, Dogan F, Farrell WE, Feelders RA, Lamberts SWJ, et al. Epidrug-induced upregulation of functional somatostatin type 2 receptors in human pancreatic neuroendocrine tumor cells. Oncotarget. 2018;9:14791–802. doi: 10.18632/oncotarget.9462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nölting S, Rentsch J, Freitag H, Detjen K, Briest F, Möbs M, et al. The selective PI3Kα inhibitor BYL719 as a novel therapeutic option for neuroendocrine tumors: Results from multiple cell line models. PLoS One. 2017;12:e0182852. doi: 10.1371/journal.pone.0182852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yao JC, Phan AT, Chang DZ, Wolff RA, Hess K, Gupta S, et al. Efficacy of RAD001 (everolimus) and octreotide LAR in advanced low- to intermediate-grade neuroendocrine tumors: Results of a phase II study. J Clin Oncol. 2008;26:4311–8. doi: 10.1200/JCO.2008.16.7858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basu S, Ostwal V. Observation on enhanced avidity on somatostatin receptor targeted 68Ga-DOTATATE PET-CT following therapy with everolimus and capecitabine–temozolamide. Nucl Med Commun. 2016;37:669–71. doi: 10.1097/MNM.0000000000000507. [DOI] [PubMed] [Google Scholar]
- 8.Sharma P, Basu S. Occurrence of 'Redifferentiation akin' phenomenon on [68Ga] Ga-DOTATATE PET-CT following CAPTEM chemotherapy in Metastatic Neuroendocrine Tumours with intermediate MiB-1 index: What could be the molecular explanation? J Nucl Med Technol. 2020;48:290–1. doi: 10.2967/jnmt.120.241539. [DOI] [PubMed] [Google Scholar]
- 9.Aashiq M, Silverman DA, Na'ara S, Takahashi H, Amit M. Radioiodine-refractory thyroid cancer: molecular basis of redifferentiation therapies, management, and novel therapies. Cancers (Basel) 2019;11:1382. doi: 10.3390/cancers11091382. [DOI] [PMC free article] [PubMed] [Google Scholar]