Glifozins are a relatively new class of drugs targeting and inhibiting sodium-glucose co-transporters (SGLTs). SGLT2 is the major cotransporter involved in glucose reabsorption in the kidney, and its inhibitors prevent the reabsorption of glucose in the kidney, increasing glycosuria and lowering blood glucose levels.1,2 Of the numerous SGLT2 inhibitors available, empagliflozin, canagliflozin, and dapagliflozin have been approved and licenced by both the EMA and the FDA.
Recent evidence has shown that these drugs can have beneficial effects in patients with cardiovascular disorders.
Evidence from clinical trials
Two landmark clinical trials involvingtype 2 diabetes mellitus (T2DM) patients with an elevated risk of cardiovascular disease have shown that subjects treated with canagliflozin had a lower risk of cardiovascular events than those who received placebo.3 Moreover, among HF patients with a reduced ejection fraction, the risk of worsening HF or death from cardiovascular causes was lower among those who received dapagliflozin than among those who received placebo, regardless of the presence or absence of diabetes.4 Another trial demonstrated that among patients receiving recommended therapy for HF, those treated with empagliflozin had a lower risk of cardiovascular death or HF hospitalization than those in the placebo group, independent from the presence of diabetes.2 In addition, the effects of sotagliflozin, which also acts on intestinal SGLT1, have been recently tested in T2DM patients who had a recent episode of decompensated HF, revealing a protective effect of this less specific SGLT2 inhibitor on deaths from cardiovascular causes and hospitalizations and urgent visits for HF, without unanticipated increases in adverse events.5
Mechanisms underlying the beneficial effects of SGLT2 inhibition in cardiovascular outcomes
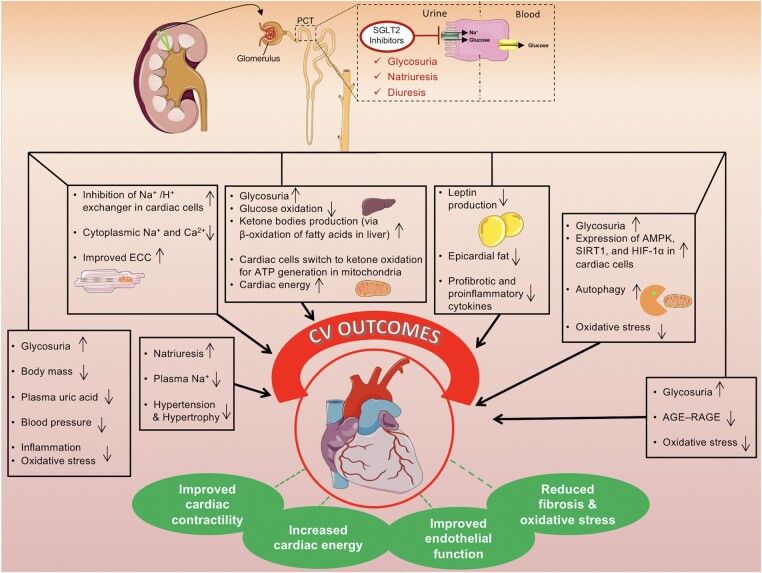
Numerous pathophysiological pathways contribute to the cardiovascular effects of SGLT-2 inhibition. Although SGLT2 inhibitors lower glucose levels, the effects on cardiovascular and renal outcomes are not (only) dependent on glucose lowering (Figure 1).
Figure 1.
Cartoon depicting the mechanism of action of SGLT2 inhibitors and their beneficial effects of on the cardiovascular system. AGE-RAGE, advanced glycation end products/receptor; ECC, excitation–contraction coupling; PCT, proximal convoluted tubule.
The main mechanisms proposed to explain the beneficial effects on cardiovascular outcomes include improved cardiomyocyte calcium handling, reduction of blood pressure (most likely attributable to an ameliorated endothelial function), enhanced myocardial energetics, decreased inflammation, induction of autophagy and lysosomal degradation, and reduced epicardial fat.
Conflict of interest: none declared.
References
- 1.Kalyani RR.Glucose-lowering drugs to reduce cardiovascular risk in type 2 diabetes. NEJM 2021;384:1248–1260. [DOI] [PubMed] [Google Scholar]
- 2.Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, Januzzi J, Verma S, Tsutsui H, Brueckmann M, Jamal W, Kimura K, Schnee J, Zeller C, Cotton D, Bocchi E, Böhm M, Choi D-J, Chopra V, Chuquiure E, Giannetti N, Janssens S, Zhang J, Gonzalez Juanatey JR, Kaul S, Brunner-La Rocca H-P, Merkely B, Nicholls SJ, Perrone S, Pina I, Ponikowski P, Sattar N, Senni M, Seronde M-F, Spinar J, Squire I, Taddei S, Wanner C, Zannad F.. Cardiovascular and renal outcomes with empagliflozin in heart failure. NEJM 2020;383:1413–1424. [DOI] [PubMed] [Google Scholar]
- 3.Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR.. Canagliflozin and cardiovascular and renal events in type 2 diabetes. NEJM 2017;377:644–657. [DOI] [PubMed] [Google Scholar]
- 4.McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Bělohlávek J, Böhm M, Chiang C-E, Chopra VK, de Boer RA, Desai AS, Diez M, Drozdz J, Dukát A, Ge J, Howlett JG, Katova T, Kitakaze M, Ljungman CEA, Merkely B, Nicolau JC, O’Meara E, Petrie MC, Vinh PN, Schou M, Tereshchenko S, Verma S, Held C, DeMets DL, Docherty KF, Jhund PS, Bengtsson O, Sjöstrand M, Langkilde A-M.. Dapagliflozin in patients with heart failure and reduced ejection fraction. NEJM 2019;381:1995–2008. [DOI] [PubMed] [Google Scholar]
- 5.Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, Lewis JB, Riddle MC, Voors AA, Metra M, Lund LH, Komajda M, Testani JM, Wilcox CS, Ponikowski P, Lopes RD, Verma S, Lapuerta P, Pitt B.. Sotagliflozin in patients with diabetes and recent worsening heart failure. NEJM 2021;384:117–128. [DOI] [PubMed] [Google Scholar]