Abstract
Introduction
An increase of suicidal thinking within the COVID-19 pandemic has been postulated. Yet, direct comparisons with pre-COVID-19 rates are missing.
Methods
The present study investigated whether levels and rates of suicidal ideation have changed between 2016 and 2020. Data of N = 664 university students (five cohorts: 2016: n = 105, 2017: n = 117, 2018: n = 108, 2019: n = 154, 2020: n = 180) were collected by online surveys.
Results
The rate of students suffering from suicidal ideation was twice as high in 2020 than in previous years. Furthermore, levels of suicidal thinking and of depression were higher in 2020 than in 2019 and 2016.
Limitations
The sample size of the current study was rather modest and suicide ideation was assessed with a single item only.
Conclusions
The rate of students suffering from suicidal ideation was twice as high in 2020 than in previous years. Help-lines and online counselling should be promoted to the public and the possibilities of telepsychotherapy for suicidal people should be used and expanded.
Keywords: Covid-19, Suicide ideation, Suicide attempts, Depression
1. Introduction
The COVID-19 pandemic of 2020 is a major global health challenge. Concerns have been raised about a possible increase in suicide rates due to the pandemics effects on factors such as social isolation, loneliness, depression as well as domestic violence, unemployment and financial problems (Reger et al., 2020). Though, preliminary studies found no increase in suicide rates in the first half of 2020 (e.g., Deisenhammer and Kemmler, 2020; Qin and Mehlum, 2020), an increase in suicide rates has recently been reported for the second half of 2020 in Japan (Tanaka and Okamoto, 2021). With regard to suicidal ideation, both a British and an American longitudinal study found an increase in suicidal thinking already within the first weeks of the pandemic: In a sample of 3,120 America residents, Killgore et al. (2020) showed that for those under lockdown the percentage of suicidal ideation increased significantly from April 2020 (17.6%) to June 2020 (30.7%). Similarly, O'Connor et al. (2020) found increased rates of suicidal thinking between March and May 2020 (8.2% to 9.8%) in a sample of 3,077 adults in the UK; with this increase being especially pronounced in younger adults (18–29 years). The increased burden on young adults was also found in a ten-country cross-sectional study by Cheung et al. (2020): The overall prevalence of suicidal ideation ranged from 7.6% in the UK to 24.9% in the Philippines, with males exhibiting higher levels of suicidal ideation than females and the youngest age group having the highest prevalence of suicidal ideation. Though, there is a reason to believe that suicidal ideation has increased during the pandemic, none of the aforementioned studies made direct comparisons with pre-COVID-19 rates. Therefore, it is unclear, if there is really an increase in suicidal thinking in young people that is attributable to the pandemic.
In Germany, significant restrictions were imposed to contain the COVID-19 pandemic with the strongest restrictions coming into force between March and June 2020 and again from December 2020 onwards. Within these time periods public and social life was shut down and due to suspension of face-to-face teaching, students had to shift to online modes of learning for the whole year.
On this background, the aim of the current study was to compare level and percentage of suicidal thinking in cohorts of German university students in the years 2016 to 2020. Furthermore, changes in depression within the same frame of time were investigated (cf., Bueno-Notivol et al., 2020).
2. Methods
2.1. Procedure and participants
Data for the present study was drawn from the ongoing “Bochum Optimism and Mental Health (BOOM)”-project, a longitudinal investigation of risk and protective factors in mental health. In the frame of the BOOM-project, all freshmen who enroll at a large university in the Ruhr region can contribute their e-mail address to the BOOM participation pool and agree to be contacted for different investigations of the university. Data collection for the current analysis took place from October to December in the years 2016, 2017, 2018, 2019, and 2020. Each year, respectively 200 second-year students were randomly collected from the BOOM participation pole and received an e-mail that included an invitation to the online survey. The responsible Ethics Committee approved the study implementation. There were no specific requirements for participation that was voluntary and compensated by course credits. Overall 664 students participated in the five surveys (2016: N = 105, 81.9% women, Mage(SDage) = 22.51(5.96), range: 18–59; 2017: N = 117, 78.6% women, Mage(SDage) = 22.53(4.71), range: 18–43; 2018: N = 108, 73.1% women, Mage(SDage) =20.59(4.45), range: 18–49; 2019: N = 154, 84.4% women, Mage(SDage) = 21.98(4.86), range: 18–47; 2020: N = 180, 73.3% women, Mage(SDage) = 21.33(5.74), range: 18–54). All data sets were complete, and there were no missing data. All participants were provided instruction and gave informed consent to participant via an online form. Furthermore, all participants were provided with information where to receive help in case of psychological distress.
2.2. Measures
Suicidal Ideation and Behavior. Twelve-month suicide ideation (“How often have you thought about killing yourself in the past year?”) was assessed using the respective item of the Suicidal Behaviors Questionnaire-Revised (SBQ-R; Osman et al., 2001). This item is rated on a 5-point Likert-type scale (1 = never, 5 = very often (five or more times)). Previous research reported an acceptable test-retest reliability of the twelve-month suicide ideation item (e.g., r = 0.60, p < .05; Taylor et al., 2011). In addition, lifetime suicide attempts were assessed using the respective item-response from the SBQ-R: “Have you ever attempted suicide, and really hoped to die?” If participants affirmed this question, they were asked how often they attempted suicide in their lifetime. The SBQ-R has been recommended for screening purposes and has repeatedly been used in clinical and non-clinical samples (Osman et al., 2001). In the present study, the point-biserial correlation between the twelve-month suicide ideation item and the lifetime suicide attempts item was high in all investigated cohorts: 2016 sample: r = 0.629, 2017 sample: r = 0.568, 2018 sample: r = 0.638, 2019 sample: r = 0.643, 2020 sample: r = 0.688; all: p < .01.
Depression. Depression was measured by a subscale of the Depression-Anxiety-Stress Scales 21 (DASS-21; Lovibond and Lovibond, 1995) that is a well-established instrument in clinical and non-clinical samples. The seven depression items (e.g., “I felt that life was meaningless”) are presented with a 4-point Likert-type scale (0 = did not apply to me at all, 3 = applied to me very much or most of the time). The sum score of the items can range between 0 and 21. The higher the sum score, the higher the level of the depression symptoms. In the current samples, the DASS-21 depression subscale had good psychometric properties in all investigated cohorts: Internal consistency was Cronbach's α 2016 = 0.878, α 2017 = 0.917, α 2018 = 0.877, α 2019 = 0.909, α 2020 = 0.872; mean interitem correlation: r mi2016 = 0.520, r mi2017 = 0.619, r mi2018 = 0.513, r mi2019 = 0.600, r mi2020 = 0.492. Moroever, an exploratory factor analysis (EFA) using a principal component analysis (PCA; rotation method: varimax) revealed the previously reported unidimensional factor structure of the subscale in all cohorts (e.g., Henry and Crawford, 2005): eigenvalue of the factor: 2016 sample: 4.237, 2017 sample: 4.788, 2018 sample: 4.104, 2019 sample: 4.617, 2020 sample: 3.985; explained variance by the factor: 2016 sample: 60.5%, 2017 sample: 67.5%, 2018 sample: 58.6%, 2019 sample: 66%, 2020 sample: 56.9%; factor loadings ranged between: 2016 sample: 0.421 (Item 2) to 0.889 (Item 3); 2017 sample: 0.722 (Item 2) to 0.886 (Item 3); 2018 sample: 0.633 (Item 2) to 0.833 (Item 1); 2019 sample: 0.680 (Item 2) to 0.854 (Item 3, Item 5); 2020 sample: 0.591 (Item 2) to 0.796 (Item 5).
2.3. Statistical analyses
Statistical analyses were conducted with SPSS 26. After descriptive analyses, a multivariate analysis of variance (MANOVA) was calculated to compare the means of the investigated variables (i.e., suicide ideation and depression) between the five samples; age and gender were included as covariates to control for them. Since the Box's test was significant (p = .001), the Hotelling's trace statistics were used. Partial eta-squared (η2 p) served as the effect-size measure of main effects, Hedge's g was included as effect-size measure of post-hoc comparisons between groups due to the different sizes of the five samples. Post-hoc comparisons were all Bonferroni-corrected (level of significance: p < .05, two-tailed). Next, the relationship between suicide ideation and depression symptoms was assessed by the calculation of zero-order bivariate correlations in each year-specific sample.
3. Results
Twelve-month suicide ideation (SBQ-R Suicide Ideation > 1) was found in 21% (n = 22) of the 2016 sample, 23.4% (n = 28) of the 2017 sample, 35.2% (n = 38) of the 2018 sample, 26.6% (n = 41) of the 2019 sample, and 60% (n = 108) of the 2020 sample. Lifetime suicide attempts were reported by 1% (n = 1) of the 2016 sample, 1.7% (n = 2) of the 2017 sample, 2.8% (n = 3) of the 2018 sample, 4.5% (n = 7) of the 2019 sample, and 5% (n = 9) of the 2020 sample.
Descriptive data of all study variables and results of the MANOVA are presented in Table 1 . Hotelling's trace was significant, T = 0.030, F(8,1310) = 2.418, p = .014, η2 p = 0.015 (small effect), indicating that the levels of the investigated variables differ between the five samples. Main effects for suicide ideation and depression symptoms were significant (see Table 1).
Table 1.
Mean comparisons (multiple analysis of variance, MANOVA) of twelve-month suicide ideation and depression symptoms, and correlation between both variables (separately for the samples from 2016 to 2020).
| Descriptive statistics and multiple analysis of variance | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2016, N = 105 | 2017, N = 117 | 2018, N = 108 | 2019, N = 154 | 2020, N = 180 | ||||
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | F | p | η2p | |
| Suicide Ideation | 1.40 (0.89) | 1.62 (1.25) | 1.76 (1.24) | 1.52 (0.99) | 1.89 (1.00) | 3.756 | .005 | .022 |
| Depression Symptoms | 4.75 (4.54) | 5.84 (5.60) | 5.94 (5.03) | 4.95 (5.11) | 6.82 (5.23) | 3.315 | .011 | .020 |
| Correlation analyses | ||||||||
| Suicide Ideation | Suicide Ideation | Suicide Ideation | Suicide Ideation | Suicide Ideation | ||||
| Depression Symptoms | .576⁎⁎ | .633⁎⁎ | .505⁎⁎ | .536⁎⁎ | .429⁎⁎ | |||
Notes. M=Mean; SD=Standard Deviation; p=significance; η2p=partial eta-squared, effect-size measure;.
⁎⁎p<.01.
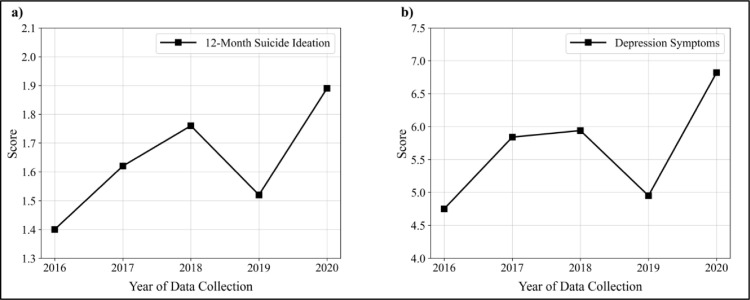
As shown in Fig. 1 , the levels of both variables increased between the years 2016 and 2018, decreased in 2019, and remarkably increased again in 2020. Pairwise comparisons indicated a significant higher twelve-month suicide ideation level in 2020 than in 2016 (2016 < 2020: mean difference, md = 0.457, p = .006, 95% Confidence Interval, CI [.085, 0.828], effect size: g = 0.51), and in 2019 (2019 < 2020: md = 0.336, p = .046, 95%CI [.004, 0.668], g = 0.37). For depression symptoms, pairwise comparisons indicated a significant higher depression level in 2020 than in 2016 (2016 < 2020: mean difference, md = 1.917, p = .025, 95%CI [.135, 3.699], g = 0.41), and in 2019 (2019 < 2020: md = 1.732, p = .023, 95%CI [.138, 3.326], g = 0.36).
Fig. 1.
Means of the investigated variables in the years 2016 to 2020: a) Twelve-month suicide ideation; b) Depression symptoms (2016: N = 105, 2017: N = 117, 2018: N = 108, 2019: N = 154, 2020: N = 180).
The twelve-month suicide ideation and depression symptoms were significantly positively correlated. The correlations ranged between r = 0.429 and r = 0.633 (all: p < .01; see Table 1).
4. Discussion
The aim of the present study was to compare rates of suicidal thinking in cohorts of German university students in the years 2016 to 2020. There were two main findings: (1) Suicidal thinking was more common in German students in 2020 than in the years before; (2) Depression levels were higher in 2020 than in 2016.
The present results complement previous findings showing an increase in suicidal thinking (Killgore et al., 2020; O'Connor et al., 2020) and depression (Bueno-Notivol et al., 2020) during the pandemic. However, different from previous studies, the current study entailed comparisons of the level and percentage of suicidal thinking during the pandemic with pre-pandemic levels: It was shown that the rate of students suffering from suicidal ideation within the past year was twice as high in 2020 than in previous years. Furthermore, the level of suicidal thinking was higher in 2020 than in 2019 and 2016. The results point to the significant burden of the pandemic on young people.
Depression symptoms belong to significant risk factors of suicide ideation (Brailovskaia et al., 2019; Teismann et al., 2018). In line with available research (Smith et al., 2006; Taylor et al., 2011), depression symptoms were positively associated with suicide ideation in each investigated cohort. Moreover, the level of depression was higher in 2020 than in 2016. Notably, individuals with enhanced levels of depression symptoms often lack functional strategies to cope with uncertain and stressful situations. They tend to rumination and experience intensive feelings of hopelessness and helplessness that can contribute to suicide ideation (Liu and Alloy, 2010). The outbreak of the pandemic and the further course of the COVID-19 situation are uncertain and stressful in many ways (Charles et al., 2021). Therefore, the present results allow the hypothetical assumption that the current increase of suicide ideation might at least partly be explained by the found enhancement of depression symptoms.
At the same time, it should be emphasized that the level of suicidal ideation is still comparatively low in 2020; very few students report long-lasting suicidal thoughts. In addition, rates of suicidal ideation in the present study cannot be compared with that in other COVID-19 studies (Cheung et al., 2020; Killgore et al., 2020; O'Connor et al., 2020), as all of these studies assessed suicidal ideation during the past one to two weeks, whereas the present study asked about suicidal ideation within the past twelve months. Nevertheless, the increase in suicidal thinking and depression among German students must be taken very seriously. Help-lines and online counselling for depressed and suicidal thinking should be promoted to the public and the possibilities of telepsychotherapy for suicidal people should be used and expanded (Jobes et al., 2020).
In addition, future studies should focus on further risk factors of suicide ideation as well as on protective factors that might reduce it specifically during the pandemic in young people. This knowledge could contribute to the identification of individuals at risk for suicide ideation and it could support the professional services in the extraordinary COVID-19 situation. Following recent research (Fava et al., 2019), a potential risk factor might be mental pain. Mental pain describes a subjective perception of negative changes or an impending destruction of the self that can be associated with loneliness, helplessness and anxiety (Cassel, 1982; Orbach et al., 2003; Shneidman, 1993). Enhanced levels of mental pain were previously found to be accompanied by suicide-related outcomes (Ducasse et al., 2017). A potential protective factor might be euthymia. Euthymia is conceptualized by the absence of mental disorders and the simultaneous presence of emotional well-being and psychological flexibility (Carrozzino et al., 2019). Individuals with high levels of euthymia are characterized by enhanced stress resistance and functional coping-strategies in unknown situations (Guidi and Fava, 2020). Therefore, they could be at less risk for suicide ideation especially during the pandemic outbreak.
There are several limitations to the present study. First, suicide ideation – as in all other aforementioned studies – was assessed with a single item only. Second, the present study does not allow generalization to other non-student samples. Third, it remains unclear to what extent the increase in suicidal ideation is accompanied by an increase in suicidal behavior and suicides. Evaluations of national suicide rates must be seen in this regard. Fourth, the sample size of the current study was rather modest. Future studies using larger samples are warranted. Fifth, even though, the SBQ-R is a well-established instrument for the assessment of suicide-related outcome (Osman et al., 2001), a recall bias considering the twelve-month suicide ideation cannot be excluded that might affect all investigated cohorts (Schmier and Halpern, 2004).
Taken together, the current study underscores the far-reaching effect and burden of the COVID-19 pandemic on young people. Universities need to be aware of this and implement, expand and promote support services.
Declaration of Competing Interest
none.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Competing interests: none.
References
- Brailovskaia J., Teismann T., Zhang X.C., Margraf J. Grandiose narcissism, depression and suicide ideation in Chinese and German students. Current Psychology. 2019:1–9. [Google Scholar]
- Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2020;21 doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrozzino D., Svicher A., Patierno C., Berrocal C., Cosci F. The euthymia scale: a clinimetric analysis. Psychother. Psychosom. 2019;88:119–122. doi: 10.1159/000496230. [DOI] [PubMed] [Google Scholar]
- Cassel E.J. The nature of suffering and the goals of medicine. N. Engl. J. Med. 1982;306:639–645. doi: 10.1056/NEJM198203183061104. [DOI] [PubMed] [Google Scholar]
- Charles N.E., Strong S.J., Burns L.C., Bullerjahn M.R., Serafine K.M. Increased mood disorder symptoms, perceived stress, and alcohol use among college students during the COVID-19 pandemic. Psychiatry Res. 2021;296 doi: 10.1016/j.psychres.2021.113706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung T.C.C., Lam S.C., Lee P.H., Xiang Y.T., Yip P.S.F. Global Imperative of Suicidal Ideation in TEN countries amid the COVID-19 Pandemic. Front Psychiatry. 2020;11:1558. doi: 10.3389/fpsyt.2020.588781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deisenhammer E.A., Kemmler G. Decreased suicide numbers during the first 6 months of the COVID-19 pandemic. Psychiatry Res. 2020;295 doi: 10.1016/j.psychres.2020.113623. -e113623. [DOI] [PubMed] [Google Scholar]
- Ducasse D., Holden R.R., Boyer L., Artero S., Calati R., Guillaume S., Courtet P., Olié E. Psychological pain in suicidality: a meta-analysis. J. Clin. Psychiatry. 2017;79:16r10732. doi: 10.4088/JCP.16r10732. [DOI] [PubMed] [Google Scholar]
- Fava G.A., Tomba E., Brakemeier E.-.L., Carrozzino D., Cosci F., Eöry A., Leonardi T., Schamong I., Guidi J. Mental pain as a transdiagnostic patient-reported outcome measure. Psychother. Psychosom. 2019;88:341–349. doi: 10.1159/000504024. [DOI] [PubMed] [Google Scholar]
- Guidi J., Fava G.A. The emerging role of euthymia in psychotherapy research and practice. Clin. Psychol. Rev. 2020;82 doi: 10.1016/j.cpr.2020.101941. [DOI] [PubMed] [Google Scholar]
- Henry J.D., Crawford J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005;44:227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- Jobes D.A., Crumlish J.A., Evans A.D. The COVID-19 pandemic and treating suicidal risk: the telepsychotherapy use of CAMS. J. Psychother. Integr. 2020;30:226. [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Allbright M.C., Dailey N.S. Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R.T., Alloy L.B. Stress generation in depression: a systematic review of the empirical literature and recommendations for future study. Clin. Psychol. Rev. 2010;30:582–593. doi: 10.1016/j.cpr.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- O'Connor R.C., Wetherall K., Cleare S., McClelland H., Melson A.J., Niedzwiedz C.L., O'Carroll R.E., O'Connor D.B., Platt S., Scowcroft E. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry. 2020:1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orbach I., Mikulincer M., Gilboa-Schechtman E., Sirota P. Mental pain and its relationship to suicidality and life meaning. Suicide Life Threat. Behav. 2003;33:231–241. doi: 10.1521/suli.33.3.231.23213. [DOI] [PubMed] [Google Scholar]
- Osman A., Bagge C.L., Gutierrez P.M., Konick L.C., Kopper B.A., Barrios F.X. The Suicidal Behaviors Questionnaire-Revised (SBQ-R) AssessmentAssessment. 2001;8:443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Qin P., Mehlum L. National observation of death by suicide in the first 3 months under COVID-19 pandemic. Acta Psychiatr. Scand. 2020 doi: 10.1111/acps.13246. [DOI] [PubMed] [Google Scholar]
- Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and coronavirus disease 2019—A perfect storm? JAMA Psychiatry. 2020;77:1093–1094. doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Schmier J.K., Halpern M.T. Patient recall and recall bias of health state and health status. Expert. Rev. Pharmacoecon. Outcomes Res. 2004;4:159–163. doi: 10.1586/14737167.4.2.159. [DOI] [PubMed] [Google Scholar]
- Shneidman E. Suicide as psychache. J. Nerv. Ment. Dis. 1993;181:147–149. doi: 10.1097/00005053-199303000-00001. [DOI] [PubMed] [Google Scholar]
- Smith J.M., Alloy L.B., Abramson L.Y. Cognitive vulnerability to depression, rumination, hopelessness, and suicidal ideation: multiple pathways to self-injurious thinking. Suicide Life Threat. Behav. 2006;36:443–454. doi: 10.1521/suli.2006.36.4.443. [DOI] [PubMed] [Google Scholar]
- Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nature Human Behav. 2021;5:229–238. doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- Taylor P.J., Gooding P.A., Wood A.M., Johnson J., Tarrier N. Prospective predictors of suicidality: defeat and entrapment lead to changes in suicidal ideation over time. Suicide Life Threat. Behav. 2011;41:297–306. doi: 10.1111/j.1943-278X.2011.00029.x. [DOI] [PubMed] [Google Scholar]
- Teismann T., Forkmann T., Brailovskaia J., Siegmann P., Glaesmer H., Margraf J. Positive mental health moderates the association between depression and suicide ideation: a longitudinal study. Int. J. Clin. Health Psychol. 2018;18:1–7. doi: 10.1016/j.ijchp.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]