Abstract
Among the challenges facing research translation—the effort to move evidence into policy and practice—is that key questions chosen by investigators and funders may not always align with the information priorities of decision makers, nor are the findings always presented in a form that is useful for or relevant to the decisions at hand. This disconnect is a problem particularly for population health, where the change agents who can make the biggest difference in improving health behaviors and social and environmental conditions are generally nonscientists outside of the health professions. To persuade an audience that does not read scientific journals, strong science may not be enough to elicit change. Achieving influence in population health often requires four ingredients for success: research that is responsive to user needs, an understanding of the decision-making environment, effective stakeholder engagement, and strategic communication. This article reviews the principles and provides examples from a national and local initiative.
Keywords: dissemination and implementation, public health policy, community engagement, research translation, health-in-all policies
INTRODUCTION
Recent years have witnessed growing interest in translational research in the biomedical and clinical sciences. Translational research is one of several related terms that connote putting research into practice, but these terms mean different things to different people (83). For scientists, the health care services industry, and many clinical investigators, translational research refers to T1, the bench-to-bedside enterprise of bringing drugs to market and converting basic science discoveries into new diagnostic and therapeutic tools (26). Many health services researchers speak of implementation science (T2–T4) (58), which studies ways to close the gap between optimal and actual care (36, 51). The National Institutes of Health (NIH) funds D&I (dissemination and implementation) research aimed at getting trial findings into practice (29).
These terms share two interesting features: They characterize the work as research (e.g., translational research1), and they view translation as the end of a process. For many investigators, a trial reaches its final step when its results are disseminated. Viewing translational research as an end point differs from viewing research translation as an input to the work of improving population health. Those working to better the health of communities—be they public health officers, clinicians, legislators, or parents—find greater value in research information that relates to their needs and priorities (4). Getting answers to their key questions may do more to improve public health than would the information available in most journal articles.
Translational research has a long history in public health. Decades ago, the research that identified evidence-based health behaviors (e.g., smoking cessation, physical activity), screening tests (e.g., mammography), and immunizations spawned its own form of implementation science: behavioral science research on how to help people adopt healthier behaviors; health services research on how health systems can improve uptake of clinical preventive services; and policy research on how to help communities adopt evidence-based policies. But in public health as in medicine, uptake of research evidence has often been disappointingly slow and incomplete (55, 60, 77). For example, rates of physical inactivity and obesity remain high (2), an6d many Americans are not acting on the evidence of life-saving forms of cancer screening (56). Research does not leap from the pages of journals into daily behavior.
One reason for this slow uptake may be misaligned agendas. Research that conforms to the academy’s interests may be less impactful than research shaped by the needs of decision makers or end users. This difference in agendas is seen in the very questions that scientific studies address, which often reflect the intellectual interests of scientists or funders (e.g., NIH) and the priorities stipulated in calls for proposals. Although they are fundamentally important, these questions may not always be framed to address the priorities of decision makers or to be usable on the front line (67, 80).2 Research may be more translatable if researchers learned more about the user’s agenda before doing the research. The problem may not be—as the academy sees it—how to get the community engaged in research, but how researchers can become engaged in the community and make their studies more relevant to the stakeholders working to improve public health.3 To use a business analogy, the consumer may not be buying the product (research) because developers are ignoring the needs of the market (end users). In such circumstances, lack of uptake is to be expected.
A greater research focus on the needs of stakeholders could enhance the relevance of the academy, but it serves a more urgent purpose: to rectify the failure of the United States to keep pace with the advancing health status of other high-income countries. Americans have lower life expectancy and poorer health status than do their peers in 16 other countries, a pattern that has been worsening since the 1980s (85). A 2013 report documented the alarming scale of the problem and predicted further deterioration without a transformative change in social policy and health system design, including a shift in research priorities (85). The public health community has called on the academy to supply the data urgently needed to inform policy and practice decisions (37, 85).
This article argues that effective research translation to support meaningful change in population health requires better research aimed at user needs, but it also requires three other ingredients for success: an understanding of the decision-making environment, stakeholder engagement, and strategic communication. After describing each of these components, we illustrate their synthesis in two examples at the national and local levels.
SCIENTIFIC RESEARCH
A society committed to population health should invest a portion of its research in supplying the information needed by those who can influence change (see sidebar, Stakeholders Who Benefit from Research Translation). This proposition is not to diminish the imperative for other forms of research. Independent scientific inquiry for its own sake remains vital. Research that proves useful to public health—from basic science to applied research—is frequently undertaken without a clear idea of how it will affect policy and may not require the help of policy makers or change agents to be implemented. Nor do we ignore how often policy makers misinterpret or ignore science in their decisions. Presenting the evidence does not always result in evidence-based policy or practice, especially in today’s polarized political environment.
We focus here, however, on the circumstances in which decision makers turn to the research community for factual evidence to inform decisions, and in this setting, the research community should be prepared to deliver a straight answer. Scholarship is important in all forms of research but includes unique characteristics to make translational research useful for these decision makers. Some examples follow.
Key Questions
Specific aims cannot be formulated around user needs without first learning the information priorities of decision makers and the environment in which they operate (6). Meeting them where they are—learning their agenda, the opportunities and threats they perceive, and how they believe scientific evidence could help—is a change in orientation for many researchers, but it is a prerequisite if scientists (or funders) are to define a user-oriented research agenda.
Data
Objective methods of data collection and analysis are always important to scholarship; however, especially in policy circles, data must be documented with sufficient transparency to establish trustworthiness and to minimize concerns about bias and partisan distortion.
Sampling
Large samples enhance statistical power, but decision makers often want evidence that pertains to themselves, their demographic group, or their local geographic area—where sample sizes may be inadequate or data may be censored. Although external validity is important, an evaluation of every intervention in every locale is untenable. This limitation creates an inherent tension between the community’s desire for evidence-based solutions that are contextualized and culturally appropriate and robust evidence that can be extrapolated at the population level. Investigators must often tolerate an uncomfortable degree of statistical uncertainty to deliver the kind of contextualized data that decision makers seek.
Presentation
Gathering the data is only one step in research translation; researchers must package the findings in a format and venue that are appropriate for the audience. The standard deliverables of academia—peer-reviewed articles or scientific presentations framed around the 4-part template of introduction, methods, results, and discussion—are rarely in the format, length, or language the policy maker needs. As epitomized by the request for an “elevator speech,” busy decision makers often need findings distilled into talking points that are brief and sharply focused (see Strategic Communication, below).
Research translation benefits from an iterative process in which the investigator invites feedback from the decision maker on how to improve the content or presentation of the material; relevant feedback, in turn, can be incorporated into new drafts to enhance their utility and relevance. This input—combined with principles from graphic design, communication science, marketing, and the psychology of information processing—can enhance the presentation of research. Through repetition and deeper interactions with diverse end users, researchers can build their skills in framing the evidence for nonscientific audiences.
UNDERSTANDING THE DECISION-MAKING ENVIRONMENT
Of great importance to population health research is the perspective of decision makers who can act on the evidence and create change. Although some decision makers can use evidence and data from original sources that were not necessarily gathered or packaged for policy purposes, much of today’s science suffers from a disconnect with real-world decisions, often because the needs of users were not considered. For research intended for implementation, the relationship with the decision maker should be bidirectional if translational research is to be truly translational, that is, if both parties are to arrive at a common understanding of each other’s language and priorities.4 Because the decision maker’s priorities may differ starkly from what seems important to investigators, a useful prelude to translational research—well before a grant is finalized—is to make a genuine effort to understand the decision-making environment.5 Investigators who embrace this approach recognize the need to “leave the campus” and their professional comfort zone to experience frontline conditions. They engage in networking, connect with colleagues and organizations with a deeper understanding of the decision maker’s world, and learn the language,6 pace, practices, and chief concerns of the people who will be using their research—all vital intelligence7 that can enhance the framing, timing, and dissemination of their research.
The first step is to clarify the user audience(s) with whom to engage, which can later help in planning dissemination activities. One way to clarify this audience is to consider the change agents whose decisions offer the greatest prospect of effecting meaningful change in health outcomes.
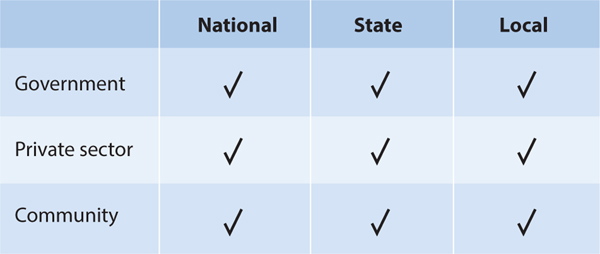
This audience depends on the topic: Certain health outcomes are driven by the decisions of patients, parents, practitioners, businesses, public health officials, community organizers, funders, or lawmakers. A matrix of potential audiences can be constructed (see example in Figure 1). Certain questions may help narrow the list to arrive at a strategic focus:
Figure 1.
Example of matrix for clarifying relevant decision makers. In this example, the project has identified nine audiences in government, the private sector, and the community at the national, state, and local levels. From Center on Society and Health, Virginia Commonwealth University.
Is meaningful change more likely at the national, state, or local level—or some combination thereof?
What is the role of government, the private sector, or the community?
If the government (federal, state, or local) plays an important role, are prospects best in the executive or legislative branch, or both? Which executive branch agencies deal with this issue? Which legislative committees have jurisdiction? Which legislators are passionate about the topic?
Which elements of the private sector play a role? Is this issue the purview of employers, health plans, health care delivery systems, restaurants, supermarket chains, developers, media, advertisers, or other industries?
Which stakeholders should be engaged (see sidebar)? Are communities of practice or impacted populations most important to engage? Which relevant community organizations should be involved?
Understanding the decision-making environment also helps researchers to expose information and data needs that matter most to decisions affecting population health, which can then be translated into research questions for future research (or informed by dissemination of existing data). If approached correctly, one-on-one meetings with key decision makers or other change agents—e.g., legislators or their staff, agency heads, business executives, civic officials—can yield important insights about the obstacles to funding or implementation of the actions favored by relevant change agents. Crucial to eliciting this information is to eschew an advocacy or critical posture and to convince the decision maker that the discussion is free of agendas and aimed solely at learning and eliciting advice. A sense of safety allows both parties to abandon defensive stances and speak freely about challenges and opportunities.
With this tone established, the researcher and decision maker can work together to consider which types of information (data or otherwise) could be most useful in addressing their top concerns about a population health problem and which align best with their priorities. Decision makers who request scientific evidence may misunderstand the data they need, the scientific method, or the kinds of information that research can realistically supply. Open dialogue helps decision makers clarify (or even change) their approach once they know more about the evidence. The informed decision maker may be able to identify critical questions that data collection and analysis could inform.8
STAKEHOLDER AND COMMUNITY ENGAGEMENT
The Role of Stakeholders
The translation of research into action often depends on the engagement of stakeholders—those who have an interest in an outcome (see sidebar). Foremost among these is the impacted community, which we discuss next. The engagement of other stakeholders can also be vital, not only because successful implementation depends on their buy-in, leadership, or material support, but also because their insights help enhance the researcher’s understanding of the issues. The medical profession has come to recognize the importance of the environment outside the clinic—in the community—where patients and caregivers can find support for managing diabetes and other chronic diseases (1, 76) and, more recently, for addressing obesity and lifestyle issues. Interest in closer collaboration between primary care and public health (2, 38) has been resurging, along with increasing enthusiasm for broader partnerships (beyond public health and medicine) to achieve transformational change in health outcomes.
Because the most important opportunities for advancing the public’s health are often the most complex, multisector engagement is necessary to develop real-world, sustainable solutions (19). The Health in All Policies movement (70) calls for engaging nonhealth sectors—e.g., transportation, housing, employers, schools, retailers—to change living conditions in ways that can meaningfully improve health, but engaging decision makers in sectors that lack a public health mission often requires advocates to demonstrate the value of the proposition. Making that case begins by explaining how decisions potentially impact health—a connection many have not considered— and by demonstrating how the interests of stakeholders in nonhealth sectors might benefit from improved health outcomes.
Engaging stakeholders often succeeds when incentives are aligned to create a win-win situation in which all parties have something to gain by collaborating (7, 24). In numerous US cities, diverse sectors—from real estate to finance—have joined hands to achieve “collective impact” (44) that improves the bottom line for all concerned, such as lowering health care costs while also creating jobs, preventing crime, and yielding other societal benefits (24). Research and evaluation are important in these initiatives, as actors from multiple sectors look to a common set of metrics and data dashboards to track whether their programs and policies are improving outcomes. Although these multisector collective impact initiatives often operate at the local level, national and state initiatives can also be important to population health and require their own kind of stakeholder engagement to elicit the buy-in of interest groups.
Community Engagement
A cornerstone of research translation is giving voice to those who are most directly affected, such as local residents, parents, patients, and caregivers, especially those who are most vulnerable. Determining what matters most to these groups is essential knowledge before research begins. Community engagement is also valuable in the subsequent tasks of data collection and analysis and the translation of results into meaningful action. Incorporating the perspective of those with lived experience can enhance the quality, validity, relevance, cultural competence, and accountability of health research and can help focus dissemination efforts on ways to benefit affected populations (15, 78). Communities benefit not only from using research to support progress but also from the opportunity for the “expression of self-determination” (57, p. 4). Their input can help researchers, as well as community organizations and private-sector partners, by generating data to inform program activities (72). Academic institutions can benefit from new partnerships between stakeholders and the popularity of community-centered programs and services (33).
Meaningful engagement treats the community as true partners and therefore requires more than token efforts, such as appointing a patient to a committee or advisory board.9 It embraces a broad agenda, from identifying a problem to formulating research priorities, refining causal models, improving study designs, conducting research, disseminating findings to target populations, and connecting research to an action/policy agenda (53). Although community engagement for research translation sometimes involves long-term arrangements (e.g., advisory boards, consortiums), shorter-term arrangements, limited to specific steps in the process (e.g., community forums, focus groups, educational outreach teams), are common (32). Principles of community-based participatory research (CBPR) are important to research translation, including mutual respect and trust, colearning, shared decision making, equitable involvement, respect for indigenous knowledge, cultural humility, capacity building, empowerment, valuing diversity, prioritization of research that benefits the community, co-ownership of data and research products, and dissemination of findings to the community (41, 40, 57, 17, 74, 79, 78).10 This work takes time and often requires flexibility, humility, and commitment. Researchers must be prepared to defend the value of research to their respective stakeholders and to reevaluate and realign research goals to their partners’ interests (47).
Particularly for disenfranchised populations (e.g., low-income communities, communities of color), the historic relationship with academic institutions, a legacy of mistrust, or past exploitation by researchers can pose challenges in developing coequal partnerships (40). If handled with delicacy, engagement efforts that emphasize respect can build trust between these parties (23, 74). The importance of taking the time to show respect and to develop this trust cannot be overstated. Timing is crucial: Relationship building should occur well before a research project begins. Although researchers may have conceptual and methodological expertise, no level of training can replace the value of lived experience in creating culturally appropriate solutions (22). Cementing trust and a stable partnership for ongoing collaboration requires that researchers commit resources to meet regularly with stakeholders and continue dialogue. This stable investment in relationships is how the community is assured that commitments are genuine.11 Researchers must also be prepared to commit time or expertise for projects important to the community that are not directly linked to (or funded by) their research.
STRATEGIC COMMUNICATION
Interactions with decision makers, stakeholders, and the public benefit from strategic use of effective communication science, a discipline that is not the traditional expertise of many public health and other academic researchers. The academy’s primary channels of communication—professional journals and scientific conferences—often reach small audiences and deliver specialized content with poor uptake outside of their professions (28). Whereas traditional public health campaigns generally achieve modest impact on public behavior or policy (45), other industries achieve dramatic shifts in behaviors—among consumers, voters, politicians, and other targets—by strategically using the tools of communication, advertising, marketing, and journalism. Researchers can exploit these tools to better convey important messages affecting population health.
Successful campaigns should begin early in a project to engage audiences throughout the ideation, planning, production, and distribution processes and to help ensure an end product that is of value to intended users (28, 50, 71). Strategic communication, which leverages available resources and targets audiences to maximize impact, requires explicit specification of communication goals and deliverables as early as possible so that research and communication efforts remain aligned throughout a project. Such initiatives also benefit when objectives of the campaign have measurable outcomes by which to gauge success.
Target Audience
Specifying the target audience(s) is a prerequisite to tailoring outreach efforts (46), but it is often overlooked. Businesses often use a market segmentation strategy, which entails creating materials for particular audiences (e.g., Congressional staff, employers). Generally, a more defined target audience requires simpler, less costly, and more effective outreach that is customized to the geographic, psychographic, and demographic characteristics of the audience (20, 31, 48, 50, 66).
Strategically selected news media can help disseminate research findings and talking points. At a minimum, researchers should undergo media training to learn how to handle interviews and avoid mistakes that generate unfavorable coverage. A hesitant or reactive approach to media outreach can limit or derail dissemination efforts. Putting out research findings and hoping for media uptake is a typical practice in academic research settings but often yields predictably poor results. Researchers can disseminate their message by proactively contacting the media as part of a planned communication strategy, targeting media outlets that align with the geographic location, demographic profile, and characteristics of the intended audience. Investing in ongoing relationships with media organizations and individual reporters in ways that resonate with their typical coverage interests helps establish researchers as reliable sources of information and increases the likelihood that research findings and key talking points will be reported.
The Message
Effective talking points are crucial to the communication strategy and should focus on a succinct message and key takeaways (the elevator speech) as well as provide cues on the desired response to the information (the ask). These bulleted messages may not always mirror the points an investigator might list in the results or conclusions section of a scientific paper. When project goals and target audiences are clearly defined, talking points can be crafted to speak the language of the intended audience. For example, the messaging for business leaders might refer to return on investment, strengthening their brand, and workforce productivity, whereas members of Congress will recognize references to entitlement spending and scoring by CBO (Congressional Budget Office).
Pithy language is difficult to craft when scientists attempt to convey the complexity, nuance, and interconnectedness of factors that impact public health. The tentative language that belongs in scientific papers can lose the attention of busy lay audiences. To successfully connect with lay audiences and the media, language needs to be approachable, free of jargon, and relevant to their interests. It should also avoid words that stir ideological or political sensitivities. For example, research showing that “social determinants of health” raised concerns about socialism and overbearing government among some audiences (68) led the Robert Wood Johnson Foundation to adopt new language about the importance of “conditions where people live, work, and play.”
The Medium
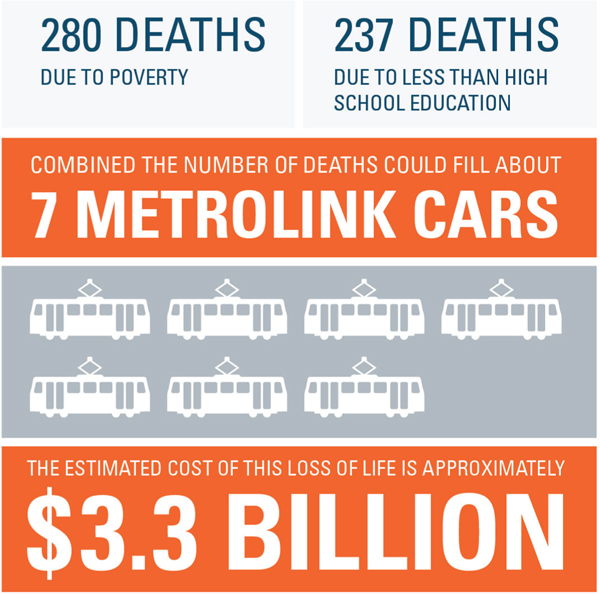
Decisions about goals and target audiences help determine the deliverable, such as the best dissemination medium to use. The most effective communication efforts are not a distraction from, but instead are seamlessly integrated into, the lives of their target audiences, reaching them where they are, considering the people, places, and media they interact with daily, and understanding the information sources and formats they trust. Gaining more in-depth knowledge of where and how target audiences receive information can help determine the best products and forums for outreach, which may include media releases, one-on-one meetings, policy briefings, nontraditional products such as videos and infographics (Figure 2), single-page fact sheets (42), social media campaigns (81), town hall meetings, or public forums. Selecting the right tools and outlets should be a deliberate process that sets realistic goals based on available time and resources and follows a proactive timetable.
Figure 2.
Graphic from the first For the Sake of All policy brief (64) illustrating the estimated number of deaths attributable to low levels of education and poverty among African American adults 25 years and older in the City of St. Louis and St. Louis County in 2011.
Researchers who want their work to make an impact or change policy find it helpful to package their findings in ways that are succinct, engaging, and aesthetically suited to the audience. Although detailed papers are useful reference materials, a bulleted summary that fits onto one page, includes policy implications or action items, and is artfully presented can be far more effective (20, 21, 42). Complex data, graphs, p-values, and methodological details may resonate with the academy, but simpler, dramatic findings coupled with human narratives (for which the investigator may enlist the help of journalists) tend to be more impactful for a non-academic audience. A single, compelling infographic (Figure 2) or statistic can say more to a general audience than pages of data tables. Talent in graphic art design—attending to layout, colors, and other design features—can present the evidence with far greater power than can traditional academic materials (61, 69).
No modern discussion of communication strategies can ignore the role of information technology. The websites, list serves, and email blasts that were transformative a decade ago are now being eclipsed by social media tools, blogs, and mobile device applications (3, 65). Web 2.0 media permit customization of content and allow communicators to reach (and interact with) larger, more targeted audiences at little cost and with breathtaking speed. Whereas research papers wait for months to be printed by publishers, researchers can now communicate findings, talking points, and powerful graphics to targeted audiences with the speed of a keystroke. Research findings can be disseminated in real-time conversations and briefings that engage their audiences on social media and through live webinars, Google hangouts, and other digital platforms. The audiences can vastly exceed journal circulations or the readership of traditional print media.12
Using electronic platforms for research translation is not without costs or risks. Premature release of data can compromise peer-reviewed publication. Time must be invested to maintain an effective presence, reach targeted audiences, and keep pace with rapid technological advances. Frequent updates to websites and social media accounts are necessary to establish a following and a reputation as a consistent and reliable source and to drive traffic to websites via search engines (5, 25, 82, 81). Social media often convey misinformation and are cluttered with banal content. Nonetheless, these tools, when used strategically, can play a key role in movement building and the sharing of ideas (34).
A NATIONAL EXAMPLE: THE EDUCATION AND HEALTH INITIATIVE
The Education and Health Initiative was a recently completed effort to raise awareness about the health implications of educational attainment and the return on investment of conditions that foster academic achievement and economic opportunity. The project was led by the Center on Society and Health at Virginia Commonwealth University with funding from the Robert Wood Johnson Foundation, which also contracted with two communication firms13 to assist in stakeholder engagement and strategic outreach.
The Initiative’s goal, adopted early in the project, was to raise awareness by helping policy makers in two policy silos—health policy and education reform—connect the dots and recognize the interconnections. The message for leaders in health policy was that better education could reduce disease rates and help control the rising costs of health care. The message for education leaders was that the potential health benefits of improved education could bolster their arguments for policies and funding. The target audiences were defined around a six-cell matrix that included governmental and private-sector policy makers at the national, state, and local levels. The team planned outreach strategies to Congress, executive branch agencies, and national organizations in Washington, DC, as well as to health care systems, businesses and employers, foundations, media, academia, state and local governments, and communities. Planned deliverables included four waves of products with visual design tools to package scientific evidence in compelling messages about the relationship between education and health, focusing on the following themes:
Education: It matters more to health than ever before (January 2014),
Why education matters to health: exploring the causes (April 2014),
Health care: necessary but not sufficient (September 2014), and
The return on investment (pending).
A set of products was planned for each wave, with segmented (social) marketing to audiences with different levels of interest: an engaging visual product with a brief message that invites readers to the website for more details, a print issue brief covering the topic in limited depth, and an online version of the issue brief that allows the user to click “Read more” hyperlinks to open more detailed content, data, and charts. An online landing page was designed as a communication hub for these resources (12).
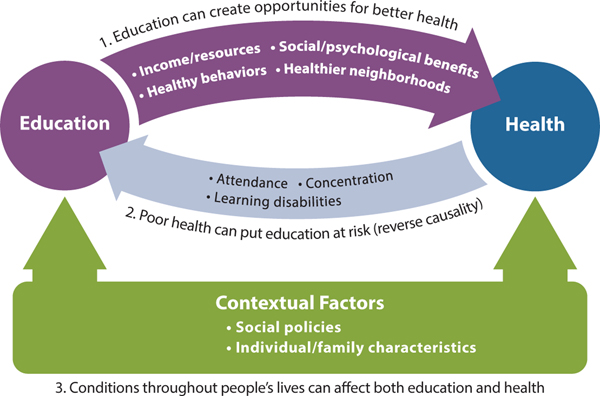
While the research team assembled published literature and analyzed data for the scientific content, it also met regularly with the two communication firms to coordinate the selection, design, and development of the final products. In preparing for the first release on the growing importance of education, the team abandoned plans for an infographic and chose to develop a three-minute “white board” video (9) to deliver the content in a more dynamic medium. Producing this video, along with the companion print (8) and online issue briefs, required a tempered balance between scientific accuracy and clear messaging; graphic artists to transform scientific data into attractive graphics (Figure 3); and style decisions about visual layout, color palettes, and voiceovers.
Figure 3.
Schematic designed by the research team and graphic artist to simplify complex causal relationships linking educational attainment and health outcomes. Reprinted from Why Education Matters to Health: Exploring the Causes (10).
Ahead of the January 2014 release of the first materials, the research team worked to build relationships with stakeholders in both the education and health policy worlds to provide advance notice of the releases and to solicit their advice on products and dissemination. One-on-one meetings and briefings were held in Washington, DC, with the leadership of national education organizations,14 members of Congress and their staff,15 the National Governors Association, and the National Conference of State Legislatures. Two meetings were held with the Committee for Education Funding, which represents 114 education organizations (16). Outreach also included the major medical and public health organizations and state-level audiences in business and local government, focusing on the change agents at the nexus of education and health.
The communication firms prepared email blasts to more than 400 contacts with potential interest in the topic, including print, broadcast, and new media. The relationships cultivated with the above organizations and members of Congress greatly expanded dissemination. Many organizations volunteered to disseminate the materials to their members and contacts or featured the project on their blogs (84). For example, the Committee for Education Funding distributed the materials to contacts on Capitol Hill, the Obama administration, and the Committee’s own mailing list of 350 contacts at 113 education organizations and tweeted to its 6,000 followers.16The Robert Wood Johnson Foundation used its considerable communication resources to further publicize the materials. Within a week of the January 7 release, the white board video (9) had been viewed more than 10,000 times.
The second phase of the project, released in April 2014, discussed potential explanations for the association between education and health. The science included a review of published research on the topic, but the team also engaged residents of a low-income urban neighborhood to elicit their perspectives about causal factors. In a May 2013 meeting and several follow-up discussions with a team of residents who participate in an ongoing CBPR partnership with the Center on Society and Health (13), the residents developed a causal model from their own perspective, which introduced many themes not fully described in the literature. To give voice to this population and put a human face on the science, the April 2014 issue brief (10) included direct quotes from these residents, who were also featured onscreen in an accompanying five-minute video (11). The underlying science was published in an Institute of Medicine background paper (86); the community engagement exercise is also the subject of a pending book chapter commissioned by the National Institutes of Health. The September 2014 issue brief (on the role of health care) was released in a September 23, 2014, Twitter chat that was conducted in collaboration with Kaiser Permanente of Northern California, which shared data for the report and tweeted live during the event.
A LOCAL EXAMPLE: FOR THE SAKE OF ALL
For the Sake of All is a multidisciplinary project funded by the Missouri Foundation for Health to report on the health and well-being of African Americans in the City of St. Louis and St. Louis County. The project’s first phase had four goals:
To inform the public about the social determinants of health as they impact African Americans in St. Louis, one of the minority populations in the city most impacted by health disparities;
To present the regional economic and health consequences of intervening (or failing to intervene) on social determinants of health;
To provide evidence of the impact of persistent disparities on all members of the region, regardless of race or socioeconomic status; and
To influence the policy agenda on health disparities by broadening the conversation beyond personal responsibility and the delivery of medical care alone.
The research team, from Washington University in St. Louis and Saint Louis University, received guidance on the project from a cross-sectoral community partner group (CPG) that included key representatives in the St. Louis region from public health and health care, business, education, media, community/economic development, and civic engagement. The community was engaged throughout this project, from the cross-sectoral CPG to community stakeholders. For example, the research team shared drafts of each brief with CPG members and community stakeholders with expertise on the topic to gather input on framing of issues and recommendations. This iterative drafting process not only provided researchers with valuable input, but also increased the buy-in of important stakeholders once the briefs and report were released—which then created a key constituency for dissemination of project publications within stakeholders’ networks. Project leadership and staff also met with more than 50 organizations and individuals representing key constituencies in the region, including community organizations, advocacy groups, health care organizations, and educational institutions.
Key deliverables were a series of five policy briefs aligned with researchers’ areas of expertise and CPG perceptions of priority issues:
How can we save lives—and save money—in St. Louis? (August 2013) (64),
How does health influence school dropout? (September 2013) (73),
How can we improve mental health in St. Louis? (October 2013) (35),
Segregation: Divided cities lead to differences in health (November 2013) (30), and
Chronic disease in St. Louis: progress for better health (December 2013) (22).
The deliverables also included a final report (27) released at a May 2014 community conference. Both the policy briefs and the final report included recommendations for targeted policies and programmatic interventions to address health disparities and community health:
Invest in high-quality early childhood development for all children.
Help low-to-moderate-income families create economic opportunities.
Invest in coordinated school health for all students.
Invest in mental health awareness, screening, treatment, and surveillance.
Invest in quality neighborhoods for all residents of St. Louis.
Coordinate and expand chronic and infectious disease prevention and management.
An important partner was the Policy Forum at the Brown School, which facilitates engagement between the academy and public sector through education, discussion, and research. Policy Forum staff with experience in the state legislature, assisted by CPG members and community stakeholders with policy outreach experience, helped to shape the project’s presentation to policy makers. The strategy had to account for the highly fragmented political structure of metropolitan St. Louis: St. Louis County and the City of St. Louis are separate counties, and St. Louis County includes more than 90 municipalities. Briefings were held for the Mayor of the City of St. Louis, the City Treasurer, and the President and Health and Human Services Committee of the Board of Aldermen (legislative body). At the state level, members of the Missouri Legislative Black Caucus and the governor’s staff were briefed.
In keeping with the principle of meeting policy makers where they are, project recommendations were presented within the framework of publicly available priorities of the policy makers. For example, the mayoral briefing included a matrix to link project recommendations to the City of St. Louis Sustainability Plan (14). Even when priorities were unknown in advance, meetings with policy makers encouraged a win-win discussion of how enacting the project’s evidence-based and community-informed recommendations could advance the agendas of policy makers and their constituencies. This ongoing policy engagement has elicited positive responses; several policy makers and local officials have signaled an interest in future collaboration.
A Community Feedback Forum was held to elicit feedback on draft elements, which were incorporated into the final report. This engagement work culminated in the representation of a very diverse group of individuals and organizations at the Community Conference where the final report was released. Representatives from local and state governments, major funders, community and economic developers, K-12 and higher education, community organizations, and local residents all attended, and many expressed interest in collaborating to advance the recommendations.
The project’s broad public and policy maker audience required materials to present clear and compelling content. Primarily descriptive in nature, the briefs (22, 30, 35, 64, 73) and final report (27) relied on secondary analyses of publicly available data and, where possible, findings localized to the zip code or census tract level. Geospatial analysis and mapping were used liberally to help readers visualize the geography of the region’s inequality (18, 49). A health literacy consultancy helped ensure that the policy briefs were accessible, and a graphic design firm developed professional-grade layout and images. The study followed recommendations from the Robert Wood Johnson Foundation’s research on effective communication about social determinants of health (68).
Proactive media partnerships with the nationally recognized African American weekly newspaper, the St. Louis American, and an online journal focused on local issues, the St. Louis Beacon, were crucial to successful dissemination. These media partners published news articles on each of the briefs and the final report. Editorials, commentaries, and other supplemental content helped provide context for news stories. In addition, news stories gave a human face and voice to the data being presented. For example, the article accompanying the brief on residential segregation described how a local resident’s neighborhood left her isolated from needed resources (43). As journalists know, such narratives can be effective in communicating health information and persuading audiences (59). Steady coverage by the media partners also spurred reporting by other local news outlets such as St. Louis Public Radio and the daily St. Louis Post-Dispatch newspaper. By the time the final report was released, many of the region’s major media outlets were reporting on the project.
Reporting on health disparities resonates in a region that has struggled with persistent segregation and stark social, economic, and health inequities. It helped to give this information a local context, and therefore maps on educational attainment, poverty, segregation, and health outcomes (e.g., life expectancy, chronic disease mortality) featured highways, school districts, local landmarks (e.g., MetroLink public transit system, the St. Louis Rams football stadium), and neighborhoods familiar to readers. Professionally designed, attractive, and compelling images and graphics were not only effective in communicating content (52, 75), but also easy to transfer to print, television, and online news media. A website (http://forthesakeofall.org/) that provided project content and additional resources on the social determinants of health also supported communication efforts, allowing For the Sake of All to be shared nationally and internationally. The look and feel of the briefs and final report cannot be underestimated as a factor in their effective reception by both the community and policy maker audiences (61, 69).
The next step of this project is a second phase, in which For the Sake of All will focus on moving from research to implementation of the reports’ recommendations. This phase will emphasize targeted engagement of policy makers, business leaders, and community groups with vested interests in advancing recommendations and priorities outlined in the reports, particularly those affecting children and youth. Several emerging trends, including regional exploration of a cradle-to-career collective impact framework, make issues related to children and youth especially attractive as initial targets. The second phase will also focus on evaluating and packaging For the Sake of All for potential replication in other communities.
CONCLUSIONS
The principles outlined in this article do not eliminate the challenges of behavior change that have always impeded research translation. However striking the evidence is of health benefits, patients face difficulties in adopting and maintaining healthy lifestyles, physicians are slow to adopt new practice norms (54), and organizations and government bureaucracies resist culture change (60). The tenets emphasized in this article—strong science, understanding the decision-making environment, stakeholder engagement, and strategic communication—do not remove these behavioral roadblocks, but they may create a healthier environment for understanding and dialogue that can ultimately facilitate research translation. The two examples featured in this article involve the translation of research on social determinants of health, but the principles apply to the implementation of many forms of research and practice guidelines as well as other efforts to translate evidence into improved policy and practice.
STAKEHOLDERS WHO BENEFIT FROM RESEARCH TRANSLATION.
The actors who influence population health and who can benefit from research are diverse. Important decisions are made by the following:
People caring for their own health (or their caretakers), who can use research to make choices about healthy lifestyles, disease management, and injury prevention.
Clinicians, social workers, teachers, and other service providers, who can use research to determine how best to care for patients/clients.
Employers, who can implement policies to improve the health and safety of workers.
Manufacturers, who can make products and services safer and more healthful for consumers.
Urban planners and developers, who can modify the built environment to improve health and reduce harmful exposures.
Community members and organizations, who can form coalitions for collective impact (44) on health outcomes, including advocacy organizations, interest groups, coalitions, voluntary associations, and nonprofit organizations that represent the involved parties.
Investors, community foundations, and health plans, who can make investments to promote health and the social determinants of health (24).
Elected officials and voters, who can enact legislation and invest in policies and programs that can improve public health.
This article describes change agents as decision makers rather than policy makers, a term that too often connotes politicians and government officials rather than the diverse spectrum of actors who together shape population health.
ACKNOWLEDGMENTS
This article discusses work funded by the Robert Wood Johnson Foundation (grant 70227), the Missouri Foundation for Health (grant 13-0085-HPC-13), The Institute for Integrative Health, and the National Institutes of Health (CTSA ULTR00058, National Center for Advancing Translational Sciences). The authors thank the Virginia Commonwealth University Center for Clinical and Translational Research, the community researchers participating in Engaging Richmond, the George Warren Brown School of Social Work at Washington University in St. Louis, the College for Public Health and Social Justice at Saint Louis University, and the For the Sake of All community partner group and community stakeholders for supporting this work.
Footnotes
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
The term translational research assigns researchers and studies as the actors in the implementation challenge. A slight rearrangement of the term, research translation, is used here because it allows for a broader class of actors, such as community health workers, health plans, social workers, or other noninvestigators who work outside the bounds of a scientific study but are well positioned to put research into practice.
This may help explain the frustrations experienced by each party: the academic community in understanding why their studies are not taken up readily by practitioners, and the public’s frustration with research that is “out of touch with the real world.” Academics often lament the difficulty of persuading local physicians to help refer patients for trials or enticing eligible patients to enroll. At higher levels of the research community, setbacks in stimulating community-engaged research have challenged NIH and the Clinical and Translational Science Awards program (39). The academy might encounter a different response if they ask decision makers for input about priorities and understand the burning questions for which science could help.
In this article we use “stakeholders” to refer to those with an interest, or stake, in the outcome and “community” as the stakeholder group most impacted by the condition of interest. Community members, a subgroup of stakeholders (see sidebar), may be residents of a geographic area, members of a community of identity, or any group with common characteristics, needs, or goals. The issue of who represents a community is important in organizing engagement strategies (41). Stakeholders include those most able to use research information to impact health through programs and policies. Successful implementation often depends on their buy-in, leadership, or material support. Participants may be individuals who bring their personal experiences and perspectives to the discussion or those who serve as representatives of a particular community or organization or its clients. Other influencers include the change agents in local government and the private sector with the power and finances to address problems (see sidebar). The private sector (e.g., employers and business groups) is an increasingly influential stakeholder in health-related research.
This bidirectional approach is a departure from the unidirectional teacher–student relationship the academic knows best (or the educator role adopted by many physicians and scientists when they share their expertise with laypeople). It is a different power relationship, built on a coequal partnership in which all parties are respected for having wisdom to impart.
Not all circumstances require these steps.Often, a coherent and convincing case for action is not dependent on more research but instead depends on connecting the dots and being prepared for a propitious moment to act on existing data, and these conditions are difficult to predict in advance.
A nomenclature that differs from the jargon of academics can become essential shorthand in communicating with decision makers. Use of these buzz words and acronyms can quickly establish bona fides and demonstrate to decision makers that the researcher understands the decision maker’s world and can gather information that speaks to their concerns.
For example, the researcher might learn about pending legislation/regulations, the policy calendar, and influential leaders, organizations, and their contact details as well as key influencers of elected officials’ behaviors, such as political donations, relevant advocacy groups, constituent demographics, and the phase of the election cycle.
Issues articulated in the decision maker’s language (e.g., “What is the bang for the buck?”) can be rephrased as research questions (e.g., “What is the cost per quality-adjusted life year?”) or testable hypotheses
Genuine stakeholder engagement is a departure from the instrumental view of community engagement as a tool for more effective subject recruitment, enhanced community/gatekeeper access and trust, or dissemination of findings.
Scholarship around other forms of stakeholder engagement in research remains underdeveloped. The lack of evidence-based strategies has led large funding agencies (e.g., PCORI) to promote the development of stakeholder engagementmethodologies (63).
Continuity with the community remains important even after studies terminate or lack support from sponsored programs. Stipends to reimburse community members for their time, and the time of academic faculty and staff, are difficult to finance through infrastructure dollars. The leadership of a university or research agency must often be convinced that investments in relationship building are as meaningful for translational research as are investments in laboratories for bench science.
As of 2014, Facebook reported 1.3 billion active users (∼18% of the global population). Twitter reported a 119% revenue increase in 2014.
The two firms include Burness Communications, which works regularly with the Robert Wood Johnson Foundation on issues related to public health and social determinants of health, andVox Communications, which brings expertise in education policy.
The organizations included, among others, the Alliance for a Healthier Generation, the American Federation of Teachers, the Association for Supervision and Curriculum Development, the Committee for Education Funding, the College Board, the Council of Chief State School Officers, Generations United, the National Association of State Boards of Education, and the National Education Association.
Senators BarbaraMikulski, Bernard Sanders, ElizabethWarner, and the staff of Senator Tim Kaine and Congressman Eric Cantor were briefed either in one-on-one meetings or in appearances at US Senate hearings.
In other examples, SenateHELPCommittee staff circulatedmaterials to all Senate Democratic legislative aides, theNational Conference of State Legislatures circulated materials to its listserv of education-focused legislators and staff, the American Public Health Association used its Public Health Newswire, the National Network of Public Health Institutes shared the issue brief and video on a number of its wires, and PolicyLink used social media and distributed materials through its Promise Neighborhoods Institute, a network of almost 60 sites.
LITERATURE CITED
- 1.Ackermann RT, Holmes AM, Saha C. 2013. Designing a natural experiment to evaluate a national healthcare-community partnership to prevent type 2 diabetes. Prev. Chronic Dis 10:E12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ASTHO (Assoc. State Territorial Health Officials). Primary care. ASTHO, Arlington, VA. http://www.astho.org/programs/access/primary-care/ [Google Scholar]
- 3.Bernhardt JM, Mays D, Kreuter MW. 2011. Dissemination 2.0: closing the gap between knowledge and practice with new media and marketing. J. Health Commun 16(Suppl. 1):32–44 [DOI] [PubMed] [Google Scholar]
- 4.Best A, Stokols D, Green LW, Leischow S, Holmes B, Buchholz K. 2003. An integrative framework for community partnering to translate theory into effective health promotion strategy. Am. J. Health Promot 18:168–76 [DOI] [PubMed] [Google Scholar]
- 5.Briones RL, Kuch B, Fisher Liu B, Jin Y. 2011. Keeping up with the digital age: how the American Red Cross uses social media to build relationships. Public Relat. Rev 37:37–43 [Google Scholar]
- 6.Brownson RC, Chriqui JF, Stamatakis KA. 2009. Understanding evidence-based public health policy. Am. J. Public Health 99:1576–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Camden Coalit. Healthc. Provid. 2014. About the coalition. Camden Coalit. Healthc. Provid., Camden, NJ.http://www.camdenhealth.org/about/about-the-coalition/history/ [Google Scholar]
- 8.Cent. Soc. Health. 2014. Education: It matters more to health than ever before. Issue Brief, Jan. Cent. Soc Health, Va. Commonw. Univ., Richmond. http://societyhealth.vcu.edu/DownFile.ashx?fileid=1739 [Google Scholar]
- 9.Cent. Soc. Health. 2014. Education: It Matters More to Health Than Ever Before. YouTube video, 3:23, posted by Robert Wood Johnson Found. on Jan. 8.http://www.youtube.com/watch?v=C8N4wka3wak
- 10.Cent. Soc. Health. 2014. Why education matters to health: exploring the causes. Issue Brief, April. Cent. Soc Health, Va. Commonw. Univ., Richmond. http://www.societyhealth.vcu.edu/DownFile.ashx?fileid=1795 [Google Scholar]
- 11.Cent. Soc. Health. 2014. Why Education Matters to Health: Exploring the Causes. YouTube video, 4:33, posted by Robert Wood Johnson Found. on April 29.http://www.youtube.com/watch?v=V3rsdBBFAN8 [Google Scholar]
- 12.Cent. Soc. Health. 2014. Education: Your lifespan is closely tied to the amount of education you received or completed. Cent. Soc Health, Va. Commonw. Univ., Richmond. http://www.societyhealth.vcu.edu/Landing.aspx?nav=310 [Google Scholar]
- 13.Cent. Soc. Health. 2014. Engaging Richmond. Cent. Soc Health, Va. Commonw. Univ., Richmond. http://www.societyhealth.vcu.edu/Page.aspx?nav=283 [Google Scholar]
- 14.City St. Louis Plan. Comm. 2013. City of St. Louis Sustainability Plan St. Louis, MO: City St. Louis. https://www.stlouis-mo.gov/government/departments/planning/documents/upload/130219%20STL%20Sustainability%20Plan.pdf [Google Scholar]
- 15.Cochran PAL, Marshall CA, Garcia-Downing C, Kendall E, Cook D, et al. 2008. Indigenous ways of knowing: implications for participatory research and community. Am. J. Public Health 1:22–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Comm. Educ. Fund. Member organizations. Comm. Educ. Fund., Washington, DC.http://cef.org/who-we-are/member-organizations/ [Google Scholar]
- 17.CTSA (Clin. Transl. Sci. Awards) Consort. Community Engagem. Key Funct. Comm. Task Force, Natl. Inst. Health. 2011. Principles of Community Engagement. Atlanta: Cent. Dis. Control Prev., Agency for Toxic Subst. Dis. Registr. 2nd Ed.http://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf [Google Scholar]
- 18.Dent B, Torguson J, Hodler T. 2008. Cartography: Thematic Map Design. New York: McGraw-Hill. 6th ed. [Google Scholar]
- 19.Diez Roux AV. 2011. Complex systems thinking and current impasses in health disparities research. Am. J. Public Health 101:1627–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dobbins M, DeCorby K, Twiddy T. 2004. A knowledge transfer strategy for public health decision makers. Worldviews Evid. Based Nurs 1:120–28 [DOI] [PubMed] [Google Scholar]
- 21.Dobbins M, Rosenbaum P, Plews N, Law M, Fysh A. 2007. Information transfer: What do decision makers want and need from researchers? Implement. Sci 2:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Drake BF, Elder K. 2013. Chronic disease in St. Louis: progress for better health Policy Brief, Dec. For the Sake of All, Wash. Univ., St. Louis Univ., St. Louis, MO. http://forthesakeofall.files.wordpress.com/2013/12/policy-brief-51.pdf [Google Scholar]
- 23.Entwistle VA, Renfrew MJ, Yearley S, Forrester J, Lamont T. 1998. Lay perspectives: advantages for health research. BMJ 316:463–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fed. Reserve Bank. 2012. Investing in What Works for America’s Communities: Essays on People Place and Purpose. San Francisco: Fed. Reserve Bank San Franc., Low Income Invest. Fund [Google Scholar]
- 25.Flanagan W. 2010. Social media marketing. Proc. Conf. Corpor. Commun., p. 9. New York: Corp. Commun. Int. Baruch Coll./CUNY [Google Scholar]
- 26.Fontanarosa PB, DeAngelis CD. 2002. Basic science and translational research in JAMA. JAMA 287:1728. [DOI] [PubMed] [Google Scholar]
- 27.For the Sake of All.2014. A Report on the Health and Well-Being of African Americans in St. Louis—and Why It Matters for Everyone St. Louis, MO: Wash. Univ. St. Louis, Saint Louis Univ. [Google Scholar]
- 28.Gagnon ML. 2011. Moving knowledge to action through dissemination and exchange. J. Clin. Epidemiol 64:25–31 [DOI] [PubMed] [Google Scholar]
- 29.Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. 2012. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am. J. Public Health 102:1274–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goodman MS, Gilbert KL. 2013. Segregation: divided cities lead to differences in health. Policy Brief, Nov. For the Sake of All, Wash. Univ., St. Louis Univ., St. Louis, MO. http://forthesakeofall.files.wordpress.com/2013/11/policy-brief-4.pdf [Google Scholar]
- 31.Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, et al. 2006. Lost in knowledge translation: time for a map? J. Contin. Educ. Health Prof 26:13–24 [DOI] [PubMed] [Google Scholar]
- 32.Hood NE, Brewer T, Jackson R, Wewers ME. 2010. Survey of community engagement in NIH-funded research. Clin. Transl. Sci 3:19–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Horowitz CR, Robinson M, Seifer S. 2009. Community-based participatory research from the margin to the mainstream: Are researchers prepared? Circulation 19:2633–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Howard PN, Duffy A, Freelon D, Hussain M, Mari W, Mazaid M. 2011. Opening closed regimes: What was the role of social media during the Arab spring?Work. Pap. 2011.1. Proj. Inf. Technol. Polit. Islam, Univ. Wash., Seattle. http://pitpi.org/wp-content/uploads/2013/02/2011_Howard-Duffy-Freelon-Hussain-Mari-Mazaid_pITPI.pdf [Google Scholar]
- 35.Hudson DL. 2013. How can we improve mental health in St. Louis? Invest in our community and raise awareness. Policy Brief, Oct. For the Sake of All, Wash. Univ., St. Louis Univ., St. Louis, MO. http://forthesakeofall.files.wordpress.com/2013/10/policy-brief-3.pdf [Google Scholar]
- 36.Inst. Med. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: Natl. Acad. Press; [PubMed] [Google Scholar]
- 37.Inst. Med. 2011. For the Public’s Health: The Role of Measurement in Action and Accountability. Washington, DC: Natl. Acad. Press [Google Scholar]
- 38.Inst. Med. 2012. Primary Care and Public Health: Exploring Integration to Improve Population Health. Washington, DC: Natl. Acad. Press; [PubMed] [Google Scholar]
- 39.Inst. Med. 2013. The CTSA Program at NIH: Opportunities for Advancing Clinical and Translational Research. Washington, DC: Natl. Acad. Press; [PubMed] [Google Scholar]
- 40.Israel BA, Eng E, Schulz AJ, Parker EA. 2005. Methods in Community-Based Participatory Research for Health. San Francisco: Jossey-Bass [Google Scholar]
- 41.Israel BA, Schulz AJ, Parker EA, Becker AB. 1998. Review of community-based research: assessing partnership approaches to improve public health. Annu. Rev. Public Health 19:173–202 [DOI] [PubMed] [Google Scholar]
- 42.Izumi BT, Schulz AJ, Israel BA, Reyes AG. 2010. The one-pager: a practical policy advocacy tool for translating community-based participatory research into action. Prog. Community Health Partnersh.: Res. Educ. Action 4(2):141–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Joiner R. 2013.Can segregation make you sick? Researchers study effectsof health. St. Louis Beacon November. 6. https://www.stlbeacon.org/#!/content/33545/segregation_and_health_110513?coverpage=4266 [Google Scholar]
- 44.Kania J, Kramer M. 2011. Collective impact. Stanford Soc. Innov. Rev Winter:36–41 [Google Scholar]
- 45.Kreuter MW, Bernhardt JM. 2009. Reframing the dissemination challenge: a marketing and distribution perspective. Am. J. Public Health 99:2123–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kreuter MW, Wray RJ. 2003. Tailored and targeted health communication: strategies for enhancing information relevance. Am. J. Health Behav 2(Suppl. 3):S227–32 [DOI] [PubMed] [Google Scholar]
- 47.Leischow SJ, Best A, Trochim WM, Clark PI, Gallagher RS, et al. 2008. Systems thinking to improve the public’s health. Am. J. Prev. Med 35:S196–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Loiselle CG, Semenic S, Côté B. 2005. Sharing empirical knowledge to improve breastfeeding promotion and support: description of a research dissemination project. Worldviews Evid.-Based Nurs 2:25–32 [DOI] [PubMed] [Google Scholar]
- 49.MacEachren AM. 1995. How Maps Work: Representation, Visualization, and Design. New York: Guilford Press [Google Scholar]
- 50.McBride T, Coburn A, MacKinney C, Mueller K, Slifkin R, Wakefield M. 2008. Bridging health research and policy: effective dissemination strategies. J. Public Health Manag. Pract 14:150–54 [DOI] [PubMed] [Google Scholar]
- 51.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, et al. 2003. The quality of health care delivered to adults in the United States. N. Engl. J. Med 348:2635–45 [DOI] [PubMed] [Google Scholar]
- 52.McGuire WJ. 1991. Theoretical foundations of campaigns. In Public Communication Campaigns, ed. Rice RE, Atkin CK, pp. 43–65. Newbury Park, CA: Sage. 2nd ed. [Google Scholar]
- 53.Minkler M. 2010. Linking science and policy through community-based participatory research to study and address health disparities. Am. J. Public Health 100(Suppl. 1):S81–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mittman BS, Tonesk X, Jacobson PD. 1992. Implementing clinical practice guidelines: social influence strategies and practitioner behavior change. QRB Qual. Rev. Bull 18:413–22 [DOI] [PubMed] [Google Scholar]
- 55.Morris ZS, Wooding S, Grant J. 2011. The answer is 17 years, what is the question: understanding time lags in translational research. J. R. Soc. Med 104:510–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Natl. Cent. Health Stat. 2011. Health, United States, 2010: With Special Feature on Death and Dying. Hyattsville, MD: Natl. Cent. Health Stat. [PubMed] [Google Scholar]
- 57.NCAI (Natl. Congr. Am.Indians) Policy Res. Cent./MSU Cent. Native Health Partners. 2102Walk Softly and Listen Carefully: Building Research Relationships with Tribal Communities. Washington, DC/Bozeman, MT: NCAI Policy Res. Cent. Montana State Univ. Cent. Native Health Partn. [Google Scholar]
- 58.NIH (Natl. Inst. Health). 2014. Implementation science information and resources. Fogarty Int. Cent, NIH, Bethesda, Md. http://www.fic.nih.gov/researchtopics/pages/implementationscience.aspx [Google Scholar]
- 59.Niederdeppe J, Bu QL, Borah P, Kindig DA, Robert SA. 2008. Message design strategies to raise public awareness of social determinants of health and population health disparities. Milbank Q. 86:481–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Noonan RK, Wilson KM, Mercer SL. 2012. Navigating the road ahead: public health challenges and the interactive systems framework for dissemination and implementation. Am. J. Community Psychol 50:572–80 [DOI] [PubMed] [Google Scholar]
- 61.Norman DA. 2004. Emotional Design: Why We Love (Or Hate) Everyday Things. New York: Basic Books [Google Scholar]
- 62.Ogden CL, Carroll MD, Kit BK, Flegal KM. 2013. Prevalence of obesity among adults: United States, 2011–2012. NCHS Data Brief 131:1–8 [PubMed] [Google Scholar]
- 63.PCORI (Patient-Cent. Outcomes Res. Inst.), Method. Comm. 2013. The PCORI Methodology Report. Washington, DC: PCORI.http://www.pcori.org/research-we-support/research-methodology-standards [Google Scholar]
- 64.Purnell J. 2013. How can we save lives—and save money—in St. Louis? Invest in economic and educational opportunity Policy Brief, Aug. For the Sake of All, Wash. Univ., St. Louis Univ., St. Louis, MO. http://forthesakeofall.files.wordpress.com/2013/08/policy-brief-1.pdf [Google Scholar]
- 65.Ratzan SC. 2011. Our new “social” communication age in health. J. Health Commun 16:803–4 [DOI] [PubMed] [Google Scholar]
- 66.Reardon R, Lavis J, Gibson J. 2006. From Research to Practice: A Knowledge Transfer Planning Guide. Toronto: Inst. Work Health [Google Scholar]
- 67.Revere D, Turner AM, Madhavan A, Rambo N, Bugni PF, et al. 2007. Understanding the information needs of public health practitioners: a literature review to inform design of an interactive digital knowledge management system. J. Biomed. Inform 40:410–21 [DOI] [PubMed] [Google Scholar]
- 68.Robert Wood Johnson Found. 2010. A New Way to Talk About the Social Determinants of Health. Princeton, NJ: Robert Wood Johnson Found. http://www.rwjf.org/content/dam/farm/reports/reports/2010/rwjf63023 [Google Scholar]
- 69.Robins D, Holmes J. 2008. Aesthetics and credibility in web site design. Inf. Process. Manag 44:386–99 [Google Scholar]
- 70.Rudolph L, Caplan J, Ben-Moshe K, Dillon L. 2013. Health in All Policies: A Guide for State and Local Governments. Washington, DC/Oakland, CA: Am. Public Health Assoc./Public Health Inst. [Google Scholar]
- 71.Scullion PA. 2002. Issues in research: effective dissemination strategies. Nurse Res. 10:65–77 [DOI] [PubMed] [Google Scholar]
- 72.Shore N, Brazauskas R, Drew E, Wong KA, Moy L, et al. 2011. Understanding community-based processes for research ethics review: a national study. Am. J. Public Health 101(Suppl.1):S359–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tate WF. 2013. How does health influence school dropout? Policy Brief, Sept. For the Sake of All, Wash. Univ., St. Louis Univ., St. Louis, MO. http://forthesakeofall.files.wordpress.com/2013/09/policy-brief-2.pdf [Google Scholar]
- 74.Viswanathan M, Ammerman A, Eng E, Gartlehner G, Lohr KN, et al. 2004. Community-Based Participatory Research: Assessing the Evidence. Evid. Rep./Technol. Assess. No. 99. RTI—Univ. NC Evid.-Based Pract. Cent. AHRQ Publ. 04-E022–2 Rockville, MD: Agency Healthc. Res. Qual. [PMC free article] [PubMed] [Google Scholar]
- 75.Waddill P, McDaniel M. 1992. Pictorial enhancement of text memory: limitations imposed by picture type and comprehension skill. Mem. Cognit 20:472–82 [DOI] [PubMed] [Google Scholar]
- 76.Wagner EH, Glasgow RE, Davis C, Bonomi AE, Provost L, et al. 2001. Quality improvement in chronic illness care: a collaborative approach. Jt. Comm. J. Qual. Improv 27:63–80 [DOI] [PubMed] [Google Scholar]
- 77.Wallace J, Nwosu B, Clarke M. 2012. Barriers to the uptake of evidence from systematic reviews and meta-analyses: a systematic review of decision makers’ perceptions. BMJ Open 2(5):pii:e001220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wallerstein N, Duran B. 2010. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am. J. Public Health 100(Suppl. 1):S40–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wallerstein NB, Duran B. 2006. Using community-based participatory research to address health disparities. Health Promot. Pract 7:312–23 [DOI] [PubMed] [Google Scholar]
- 80.Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, et al. 2008. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am. J. Community Psychol 41:171–81 [DOI] [PubMed] [Google Scholar]
- 81.Waters RD, Burnett E, Lamm A, Lucas J. 2009. Engaging stakeholders through social networking: how nonprofit organizations are using Facebook. Public Relat. Rev 35:102–6 [Google Scholar]
- 82.Westcott S. 2007. Face time: Charities flock to social-networking Web sites to reach out to new people, spark discussion, and help raise money. Chron. Philanthr 19:39. http://philanthropy.com/article/Face-Time/54580/ [Google Scholar]
- 83.Woolf SH. 2008. The meaning of translational research and why it matters. JAMA 299:211–13 [DOI] [PubMed] [Google Scholar]
- 84.Woolf SH. 2014. Connecting the dots between education, health and opportunity. Ideas Blog, June27. Investing in What Works for America’s Communities, San Francisco. http://www.whatworksforamerica.org/connecting-the-dots-between-education-health-and-opportunity/#.U7mslk1OWpo [Google Scholar]
- 85.Woolf SH, Aron L, eds., Panel on Understanding Cross-National Health Differences Among High-Income Countries, Natl. Res. Counc., Comm. Popul., Div. Behav. Soc. Sci. Educ., Board on Popul. Health Public Health Pract., Inst. Med. 2013. U.S. Health in International Perspective: Shorter Lives, Poorer Health Washington, DC: Natl. Acad. Press; [PubMed] [Google Scholar]
- 86.Zimmerman E, Woolf SH. 2014. Understanding the Relationship Between Education and Health. Discuss. Pap. Roundtable Popul. Health, Inst. Med Washington, DC: Natl. Acad. Sci.http://www.iom.edu/Global/Perspectives/2014/UnderstandingTheRelationship.aspx [Google Scholar]