Abstract
Few attempts have been made to incorporate multiple aspects of physical activity (PA) to classify patterns linked with health. Temporal PA patterns integrating time and activity counts were created to determine their association with health status. Accelerometry data from the National Health and Nutrition Examination Survey 2003–2006 was used to pattern PA counts and time of activity from 1,999 adults with one weekday of activity. Dynamic time warping and kernel k-means clustering partitioned 4 participant clusters representing temporal PA patterns. Multivariate regression models determined associations between clusters and health status indicators and obesity, type 2 diabetes, and metabolic syndrome. Cluster 1 with a temporal PA pattern of the lowest activity counts reaching 4.8e4 cph from 6:00–23:00 was associated with higher body mass index (BMI) (β=2.5±0.6 kg/m2, 95% CI:1.0, 4.1), higher waist circumference (WC) (β=6.4±1.3 cm, 95% CI:2.8, 10.0), and higher odds of obesity (OR: 2.4; 95% CI: 1.3, 4.4) compared with Cluster 3 with activity counts reaching 9.6e4–1.2e5cph between 16:00–21:00. Cluster 1 was also associated with higher BMI (β=1.5±0.5kg/m2, 95% CI:0.1, 2.8) and WC (β=3.6±1.3cm, 95% CI:0.1, 7.0) compared to Cluster 4 with activity counts reaching 9.6e4 cph between 8:00–11:00. A Temporal PA pattern with the lowest PA counts had significantly higher mean BMI and WC compared to temporal PA patterns of higher activity counts performed early (8:00–11:00) or late (16:00–21:00) throughout the day. Temporal PA patterns appear to meaningfully link to health status.
Keywords: temporal, timing, physical activity patterns, adults, health status, body mass index, waist circumference, obesity
Introduction
About 13% of the world’s adult population were considered obese in 2016 (World Health Organization, 2020a). Obesity is both an outcome and a contributor to disease development including type 2 diabetes (T2D) and metabolic syndrome (MetS) (Després and Lemieux, 2006; Nguyen et al., 2011). Low physical activity (PA) is a potentially modifiable risk factor for obesity (U.S. Department of Health and Human Services, 2018).
Engaging the population in PA is a public health priority given its well documented beneficial effects. Specifically, increased exercise has been shown to aid in weight loss (Swift et al., 2018), lower waist circumference (WC) (Waller et al., 2008) and blood pressure (Dimeo et al., 2012).
Moreover, most previous PA research has focused on the association between intensity or counts of PA and health (Dyck et al., 2015; Littman et al., 2005; Strath et al., 2008; Trombold et al., 2013). Beyond these two aspects, timing of activity may also be relevant to health. A few studies have shown a potential benefit to modulating time of activity in relationship with health outcomes (Alizadeh et al., 2017; Chomistek et al., 2016; Zhao et al., 2014, Zhao et al., 2016). A limitation of these studies is a focus on vague unspecified parts of the day i.e., morning vs. evening without considering the specific timing of activity throughout the day. Consideration of the pattern of activity throughout a day, or “temporal PA patterns”, may provide insight to behavioral patterns related to health, however studies on temporal PA patterns are scarce. One of the challenges is utilizing methods that will characterize PA patterns as an exposure by integrating timing and other characteristics of PA in relation to health.
Our previous work revealed an association between temporal dietary patterns and obesity using a novel distance measure based on dynamic time warping (DTW) (Aqeel et al., 2020). A similar methodology is used herein to identify similarities in the time and counts of activity over a 24-hour period and to perform dimensionality reduction. Groups exhibiting similar activity are expected to display similar health status indicator values and risk of disease that are distinct from other temporally defined groups. Thus, the hypothesis for this study is that differences in health status exist between U.S. adult (aged 20–65 y) participant clusters demonstrating similar 24-hour temporal PA patterns as generated from accelerometry data of the 2003–2006 National Health and Nutrition Examination Survey (NHANES).
Methods
Participants and Data Collection
NHANES 2003–2006 used a complex, stratified, multistage probability sampling design to provide a representative sample of the total civilian non-institutionalized U.S. population (Centers for Disease Control and Prevention CDC, 2020a). Sociodemographic characteristics were collected during the in-person household interview and participants subsequently completed a health examination in the mobile examination center that included anthropometric measurements, laboratory tests, and recruitment for the PA assessment component. Consent was obtained from participants and NHANES protocols and content were approved by the National Center for Health Statistics (NCHS) Research Ethics Review Board (Centers for Disease Control and Prevention CDC, 2020b).
Analytic Sample
NHANES 2003–2006 included PA accelerometry data combined for this analysis. Both short- and long- term health status indicators were included to investigate whether PA patterns would associate with them differently. Inclusion criteria specified non-pregnant U.S. adults aged 20–65 y with one random weekday of valid accelerometer data and complete sociodemographic, anthropometric and laboratory data (n=1,999) (see Appendix A). Pregnant women, children, adolescents, and adults older than retirement age were excluded because their daily activity patterns may include variation characteristic to the life stages they represent (U.S. Department of Health and Human Services, 2018).
Anthropometric Assessment and Laboratory Tests
Weight was measured using a digital scale to the nearest 0.1 kilogram (McDowell et al., 2008). Height and WC were measured with a stadiometer and tape measure respectively, to the nearest 0.1 centimeter (McDowell et al., 2008). BMI was calculated as weight in kilograms divided by height in meters squared (World Health Organization, 2020b).
Blood was drawn and processed according to standard procedures (NHANES contents in detail, 2003; NHANES contents in detail, 2005). Fasting plasma glucose and triglycerides were assessed after participants fasted ≥ 8–24 hours. Fasting plasma glucose was measured using a hexokinase method (NHANES data documentation, 2003a; NHANES data documentation, 2005a) and triglycerides were measured enzymatically (NHANES data documentation, 2003b; NHANES data documentation, 2005b). Hemoglobin A1c, total cholesterol, and high-density lipoprotein cholesterol (HDL-C) were based on samples taken regardless of fasting state. Hemoglobin A1c was measured with high performance liquid chromatography (NHANES data documentation, 2003c; NHANES data documentation, 2005c), total cholesterol was measured enzymatically, and HDL-C was analyzed using a direct HDL-C immunoassay method (NHANES data documentation, 2003d; NHANES data documentation, 2005d, e). Blood pressure was measured following standard procedures; the average value for up to three measurements was used (Mellen et al., 2008).
Disease Categories
Disease categories included obesity, T2D, and MetS. T2D classification was based on fasting plasma glucose (≥126 mg/dL), hemoglobin A1c (≥ 6.5%) or self-reported: “yes” in response to the question “have you ever been told by a doctor you have diabetes?” or to using glucose-lowering medications (American Diabetes Association, 2014). The National Cholesterol Education Program Adult Treatment Panel III definition of MetS was classified based on the presence of ≥3 of the following risk factors: 1) WC (>102 cm for men, >88 cm for women); 2) triglycerides (>150 mg/dL) or taking antihyperlipidemic medications; 3) HDL-C (<40 mg/dL in men, <50 mg/dL in women); 4) hypertension (>130/>85 mmHg) or taking antihypertensive medications; and 5) impaired fasting glucose (>110 mg/dL) or taking glucose-lowering medications (Alexander et al., 2003).
Accelerometer Data Collection and Analysis
The ActiGraph model 7164 accelerometer was used to collect objective information on participants’ PA. The Actigraph records vertical accelerations as “counts” representing the relative intensity of each movement (Metzger et al., 2010). Monitors recorded 7 days of activity from 12:01 a.m. the day after the health examination (NHANES data documentation, 2005f). Ten hours of wear time was considered a valid day which was calculated by subtracting non-wear time from the total daily observation time (Troiano et al., 2008). Given the exploratory nature of this analysis, one random weekday of accelerometer data was chosen from each person’s valid days so that each valid day had an equal chance of being selected. Inclusion of all activity types has the advantage of holistically evaluating PA links to health and aligning with the goals of the study. Total activity counts (TAC)/day, a proxy for total volume of PA performed and accounting for minutes spent in sedentary, light, moderate, and vigorous activity (Chomistek et al., 2017) was used to investigate PA patterns distributed over a 24-hour day.
Temporal Physical Activity Patterns
Temporal PA patterning was defined by partitioning of a PA dataset into mutually exclusive clusters using cluster analysis that incorporates timing, intensity and duration of activity. This study mainly focused on a distance-based method for the patterning research. Several distance measures for comparing time series were investigated including the constrained DTW with Sakoe-Chiba band (CDTW) and the modified DTW (MDTW) based on previous work to pattern dietary intake (Eicher-Miller et al., 2020). The original and the compact representation of PA time series are the required input format by CDTW and MDTW, respectively. The original PA time series is one-dimensional of length 1440, with each entry representing PA counts at the corresponding minute. Leveraging the sparsity of PA data, the original PA time series was converted into its “compact representation” by summing PA counts in each hour and extracting the counts and hourly time stamps of non-zero hours to form a new time series of two dimensions (PA counts and time stamp). CDTW and MDTW belong to the elastic distance family and find the optimal matching path among counts of activity in two time series (Eicher-Miller et al., 2020). The matching is “optimal” in the sense that the summed difference between matched counts is minimized. The Sakoe-Chiba bandwidth in CDTW and the weight parameter beta in MDTW are controlling parameters to avoid pathological matchings (e.g., matching morning to evening activities). While the Sakoe-Chiba band rigorously limits the maximum time difference between matched entries, the weight parameter beta controls the matching through a time difference penalty term: larger beta indicates more penalty on matching entries that are different in time. Bandwidths ranging between 60–720 min (60-min increments) and beta ranging from 0–10 (1 increment) were explored in CDTW and MDTW, respectively. Further, the distance measures were coupled with kernel k-means algorithm (Dhillon, Guan, and Kulis, 2004) to partition the time series into mutually exclusive clusters such that intra-cluster activity occasions are more similar and inter-cluster activities are more different. In this way, each cluster represents a specific temporal PA pattern. Cluster number k=4 was selected to maintain consistency with previous development of temporal patterning (Eicher-Miller et al., 2020; Eicher-Miller et al., 2016; Khanna et al., 2011). CDTW with bandwidth 240 min (representing a constraint of a maximum of 4 hours between two matched activity occasions) performed the best compared with CDTW over the values of bandwidth and compared with MDTW over the values of beta based on inferential analyses with health status indicators prioritized as: 1) most significant differences between six pairwise comparisons, 2) highest model R2, and 3) largest difference between highest and lowest mean of health status indicators.
Statistical Analysis
The Rao Scott F adjusted chi-square statistic was used to determine significant differences among clusters by selected characteristics: survey year (2003–2006), sex (male or female), race/ethnicity (Mexican American and other Hispanic, Non-Hispanic white, Non-Hispanic black, and other-race including multi-race), age groups (20–34, 35–49, and 50–65 y), employment status (employed or unemployed), marital status (married/living with a partner or single/divorced/separated/widowed), household size (1–3 people or >4 people), poverty to income ratio (PIR), and BMI categorized as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2) (World Health Organization, 2020b). PIR was calculated as reported household income divided by the federal poverty guideline for household income (0–0.99, 1–1.99, 2–2.99, 3–3.99, 4–4.99, and ≥5). Potential collinearity between confounders employment status and PIR as well as between marital status and household size were investigated and results indicated absence of collinearity as per low variance inflation <10 and high tolerance values >0.1.
Analysis of variance determined differences in means of health status indicators by temporal PA patterns. Multiple linear regression models determined associations between temporal PA patterns and health status indicators. For risk of obesity, T2D and MetS, multivariate logistic regression was used to estimate odds ratio comparing the four temporal PA patterns. Potential confounders included survey year, sex, age group, race/ethnicity, employment status, marital status, household size, PIR, TAC and BMI (except for models with BMI, WC, and obesity as the outcome). Power calculations were performed for outcomes BMI and WC a priori to examine whether effect size considered to be clinically meaningful (Bodegard et al., 2013; Cerhan et al., 2014; Mulligan et al., 2019) could be reliably detected using the study sample. Survey weights were constructed for the 2003–2006 survey years as directed by the NCHS (Johnson et al., 2013). Sampling weights were rescaled so that the sum of the weights matched the survey population at the midpoint of the 4 years. Adjustment for the complex survey design including clustering and stratification followed NCHS guidelines (Centers for Disease Control and Prevention CDC, 2020a). Comparisons between groups were considered statistically significant when p<0.05/6 (Tukey-Kramer type adjustment for multiple comparisons). Analyses used SAS survey procedures in version 9.4.
Visualization
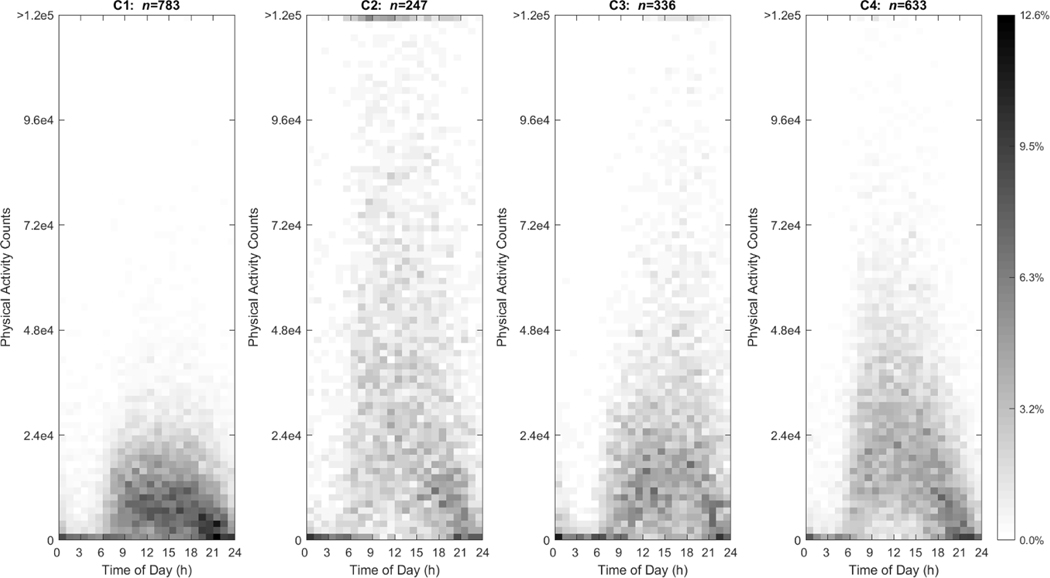
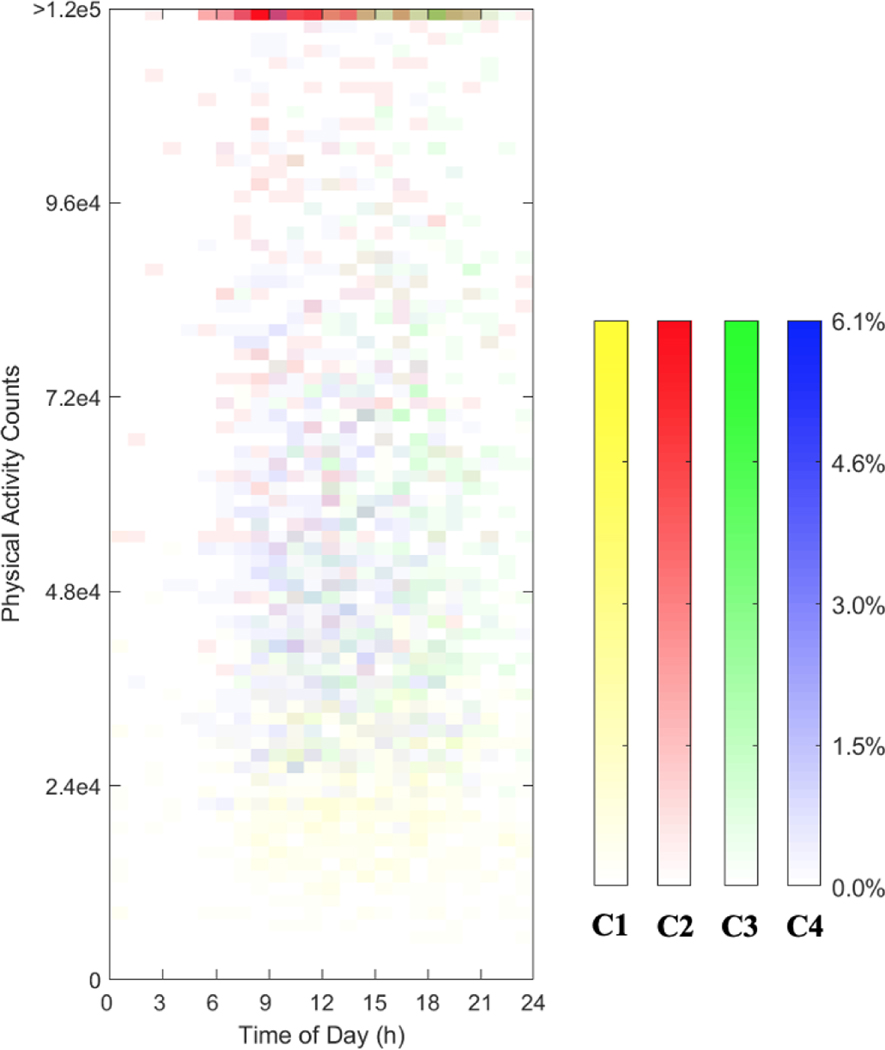
The visualization (Fig. 1) illustrates the distribution of non-zero PA counts in each cluster using heat maps. Each activity occasion in the heat map is marked by its time stamp and PA counts. Time axis ranged from 0=12:00 to 24:00 the next day with PA counts ranging from 0 to > 1.2e5 at a particular hour. The proportion of individuals that had the corresponding activity is indicated through shading and ranged from 0% to 12.6% of each cluster with darker shading signifying a greater proportion of the cluster engaged in the specified PA counts at that hour Fig. 1 exhibits four distinct temporal PA patterns. Fig. 2 adds color to differentiate the 4 clusters.
Fig. 1.
Heat maps for CDTW clusters (A-D) which depict activity counts ranging from 0 counts/hour (cph) to > 1.2e5 cph (y-axis) for U.S. adults ages 20–65 y as drawn from NHANES 2003–2006 over a 24-hour day from time 0=12:00 to 24:00 the next day (x-axis). The proportion of the sample is indicated by the inverse gray-scale legend with 0.0% of the cluster participants to 12.6% of the cluster participants.
Fig. 2.
Heat maps for CDTW clusters (C1-C4) which depict the distribution of the largest activity occasion within each cluster for U.S. adults ages 20–65 y as drawn from NHANES 2003–2006. The activity counts ranged from 0 cph to >1.2e5 cph(y-axis) over a 24-hour day from time 0=12:00 to 24:00 the next day (x-axis). The proportion of the sample is indicated by the inverse color-scale legend with 0.0% of the cluster participants to 6.1% of the cluster participants.
Results
Characteristics of participants are presented in Table 1. Clusters 2 and 3 included proportionately equivalent numbers of participants, 12.4% and 16.8%, respectively, whereas Cluster 1 had the largest proportion (39.2%) followed by Cluster 4 (31.6%). Significant differences were present among clusters by sex, age, employment status, marital status, household size, PIR, and BMI. Females were more heavily represented in Cluster 1 (64.1%), while males featured more prominently in Cluster 2 (78.9%). Additionally, Cluster 1 included a higher proportion of age group 50–65 y compared to other age groups (47.8%), whereas Clusters 2 and 3, included a higher proportion of the age group 20–34 y (44.9% and 45.5%, respectively). Compared to all the other clusters, Cluster 1 included the lowest proportion of employed individuals (58.0%). Moreover, all clusters included a larger proportion of individuals who are married/ living with a partner and a household comprising 1–3 individuals compared to four or more. Further, smaller proportions of individuals at the lowest household PIR (0 to 0.99) were included in Cluster 2 (14.6%), Cluster 3 (14.9%) and Cluster 4 (14.5%), whereas larger proportions were included in Cluster 1 (18.6%). The proportional representation of Clusters 2, 3 and 4 in the higher ratios of PIR of ≥ 5.00 compared with Cluster 1 was also observed. Regarding BMI, normal weight was more highly represented in Clusters 2 and 3 (42.5% and 37.8%, respectively); while obese category was more heavily represented in Clusters 1 and 4 (45.8% and 33.8%, respectively) compared to the other two clusters.
Table 1.
Characteristics of clusters representing temporal PA patterns of U.S. adults ages 20–65 y NHANES 2003–2006 (n=1,999).
| Characteristic | Total (n) | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | p-valuea |
|---|---|---|---|---|---|---|
|
| ||||||
| n (%) | ||||||
| Total | 1999 | 783 (39.2) | 247 (12.4) | 336 (16.8) | 633 (31.6) | |
| Survey year | 0.37 | |||||
| 2003–2004 | 975 | 384 (49.0) | 120 (48.6) | 178 (53.0) | 293 (46.3) | |
| 2005–2006 | 1024 | 399 (51.0) | 127 (51.4) | 158 (37.0) | 340 (53.7) | |
| Sex | <0.0001 | |||||
| Male | 1029 | 281 (35.9) | 195 (78.9) | 185 (55.1) | 368 (58.1) | |
| Female | 970 | 502 (64.1) | 52 (21.1) | 151 (44.9) | 265 (41.9) | |
| Race/Ethnicity | 0.08 | |||||
| Mexican American | 428 | 143 (18.3) | 53 (21.5) | 61 (18.2) | 171 (27.0) | |
| Other Hispanic | 58 | 17 (2.2) | 9 (3.6) | 10 (3.0) | 22 (3.5) | |
| Non-Hispanic white | 982 | 387 (49.4) | 124 (50.2) | 178 (53.0) | 293 (46.3) | |
| Non-Hispanic black | 427 | 187 (23.8) | 54 (21.9) | 66 (19.5) | 120 (19.0) | |
| Other | 104 | 49 (6.3) | 7 (2.8) | 21 (6.3) | 27 (4.2) | |
| Age group (year) | <0.0001 | |||||
| 20–34 | 616 | 177 (22.6) | 111 (44.9) | 153 (45.5) | 175 (27.6) | |
| 35–49 | 691 | 232 (29.6) | 93 (37.7) | 113 (33.6) | 253 (40.0) | |
| 50–65 | 692 | 374 (47.8) | 43 (17.4) | 70 (20.9) | 205 (32.4) | |
| Employment Status | <0.0001 | |||||
| Employed | 1448 | 454 (58.0) | 211 (85.4) | 260 (77.4) | 523 (82.6) | |
| Unemployed | 551 | 329 (42.0) | 36 (14.6) | 76 (22.6) | 110 (17.4) | |
| Marital status | 0.01 | |||||
| Married/living with a partner | 1311 | 497 (63.5) | 159 (64.4) | 200 (59.5) | 455 (71.9) | |
| Single, divorced, separated, widowed | 687 | 285 (36.4) | 88 (35.6) | 136 (40.5) | 178 (28.1) | |
| Household size | 0.0004 | |||||
| 1–3 people | 1255 | 549 (70.1) | 140 (56.7) | 209 (62.2) | 357 (56.4) | |
| 4 or more people | 744 | 234 (29.9) | 107 (43.3) | 127 (37.8) | 276 (43.6) | |
| Household PIR | 0.02 | |||||
| 0–0.99 | 324 | 146 (18.6) | 36 (14.6) | 50 (14.9) | 92 (14.5) | |
| 1.00–2.99 | 459 | 181 (23.1) | 59 (23.9) | 73 (21.7) | 146 (23.1) | |
| 2.00–2.99 | 308 | 138 (17.6) | 37 (15.0) | 47 (14.0) | 86 (13.6) | |
| 3.00–3.99 | 297 | 106 (13.6) | 41 (16.5) | 39 (11.6) | 111 (17.5) | |
| 4.00–4.99 | 189 | 72 (9.2) | 18 (7.3) | 36 (10.7) | 63 (10.0) | |
| ≥5.00 | 422 | 140 (17.9) | 56 (22.7) | 91 (27.1) | 135 (21.3) | |
| BMIb | <0.0001 | |||||
| Underweight | 26 | 14 (1.8) | 3 (1.2) | 5 (1.5) | 4 (0.6) | |
| Normal weight | 575 | 176 (22.5) | 105 (42.5) | 127 (37.8) | 167 (26.4) | |
| Overweight | 682 | 234 (29.9) | 87 (35.2) | 113 (33.6) | 248 (39.2) | |
| Obese | 716 | 359 (45.8) | 52 (21.1) | 91 (27.1) | 214 (33.8) | |
Note. BMI: body mass index, PIR: poverty to income ratio.
Rao Scott F adjusted χ2p-value is a goodness-of-fit, one-sided test; statistical significance is indicated when p<0.05. Analyses were adjusted for clustering and stratification. Sample weights were constructed and applied to the analysis as directed by NCHS. Weight were rescaled so that the sum of the weights matched the survey population at the midpoint of the 4 years covering 03–06.
BMI: categories were defined per the World Health Organization (World Health Organization, 2020b).
Characteristics of Temporal Physical Activity Patterns
Compared to all other clusters, Cluster 1 demonstrated the lowest activity counts reaching up to 4.8e4 cph for activity occasions from 6:00 to 23:00 (Fig. 1 and Table 2). A more prominent decrease in activity was observed towards the end of the day between 19:00 to 21:00 with activity reaching up to 1.2e4 cph. Contrarily, Cluster 2 revealed a pattern with the highest activity counts reaching >1.2e5 cph; the activity tended to taper off with a higher percentage of the cluster performing activity reaching up to 7.2e4 cph after 18:00. Cluster 3 demonstrated low activity counts reaching up to 4.8e4 cph between 6:00 to 12:00, whereas the level of activity tended to increase towards later hours reaching up to 9.6e4-1.2e5 cph between 16:00 to 21:00. The activity counts in Cluster 4 were lower compared to Clusters 2 and 3 reaching 9.6e4 cph between 8:00 to 11:00 and activity counts tended to be lower towards later hours of the day reaching up to 4.8e4 cph after 18:00. Generally, in all of the clusters, the percentage of participants engaging in high activity counts tended to be lower compared to the percentage of participants engaging in low activity counts. Fig. 2 confirms patterns revealed in Fig. 1, variation in the unique patterns inherent to each cluster are apparent regarding highest and lowest activity throughout the day.
Table 2.
Qualitative description of clusters representing temporal PA patterns of U.S. adults ages 20–65 y NHANES 2003–2006 (n=1,999).
| Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | |
|---|---|---|---|---|
|
| ||||
| Characteristics | ||||
| n (%) | 783 (39.2) | 247 (12.4) | 336 (16.8) | 633 (31.6) |
| Overall temporal pattern | Low PA counts throughout the day with a sharp decline between 19:00–21:00 | High PA counts throughout the day with a decline after 18:00 | Lower PA counts between 6:00–12:00 | Higher PA counts between 8:00–11:00 |
| Higher counts between 16:00–21:00 | Lower counts after 18:00 | |||
| Percentage of cluster engaging in high vs. low activity within cluster | Higher percentage ~6–12% engaged in low PA counts reaching up to 1.2e4 cph | Higher percentage ~3–8% engaged in PA counts reaching up to 7.2e4 cph | Higher percentage ~4–9% engaged in PA counts reaching up to 4.8e4 cph | Higher percentage ~4–10% engaged in PA counts reaching up to 4.8e4 cph |
| Lower percentage ~1–3% engaged in PA counts between 2.4e4–4.8e4 cph | Lower percentage ~1–4% engaged in PA counts between 7.2e4–>1.2e5 cph | Lower percentage 1–2% engaged in PA counts between 7.2e4–1.2e5 cph | Lower percentage ~1–4% engaged in PA counts between 4.8e4 – 9.6e4 cph | |
Note. cph: counts per hour, PA: physical activity
Association of Temporal Physical Activity Patterns with Adiposity and Chronic Disease
Significant differences in mean BMI and WC were present among all clusters except for Clusters 2 and 3 in the unadjusted model (see Appendix B). In the adjusted models, significant differences in mean BMI between all clusters remained except between Clusters 2 and 3 as well as 3 and 4 (Table 3). Significant differences in mean WC were present between all clusters except Clusters 2 and 3 as well as 2 and 4 in the adjusted models (Table 4). The significantly different mean BMI was greatest between Clusters 1 and 2 (β=2.7±0.6 kg/m2, 95% CI:1.1, 4.3), similar to the results of the unadjusted model (β=3.5±0.5 kg/m2, 95% CI: 2.1, 5.0; see Appendix B). The significantly different mean WC was greatest between Clusters 1 and 3 (β=6.4±1.3 cm, 95% CI: 2.8, 10.0), similar to the results of the unadjusted model (β=7.4±1.2 cm, 95% CI: 4.2, 10.6; see Appendix B).
Table 3.
Mean BMI (kg/m2)and covariate-adjusted regression model results for clusters representing temporal PA patterns of U.S. adults ages 20–65 y as drawn from the NHANES, 2003–2006a.
| Adjusted modelsb | n (%) | BMIc, (kg/m2) | βd ± SE compare to Cluster 2 | 95% CI | βd ± SE compare to Cluster 3 | 95% CI | βd ± SE Compare to Cluster 4 | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Cluster 1 | 783 (39.2) | 30.3 (0.3) | 2.7 ± 0.6 | 1.1, 4.3f | 2.5 ± 0.6 | 1.0, 4.1f | 1.5 ± 0.5 | 0.1, 2.8e |
| Cluster 2 | 247 (12.4) | 26.9 (0.4) | −0.2 ± 0.5 | −1.5, 1.1 | −1.3 ± 0.5 | −2.5, −0.0e | ||
| Cluster 3 | 336 (16.8) | 27.3 (0.3) | −1.1 ± 0.5 | −2.3, 0.1 | ||||
| Cluster 4 | 633 (31.6) | 28.6 (0.2) |
Note. BMI: body mass index, SE: standard error
Significant differences among clusters in mean BMI were present amongst all clusters except Clusters 2 and 3 in the unadjusted model at p<0.05 (see Appendix B).
Models were adjusted for survey year, sex, age, employment status, marital status, household size, race/ethnicity, poverty to income ratio, and total activity counts/day.
Values are Mean (SEM).
ß represents difference between mean BMI of cluster and reference cluster. Differences in mean BMI are different than those between raw means because they represent differences in least square means.
p<0.05
p<0.001
Table 4.
Mean WC (cm) and covariate-adjusted regression model results for clusters representing temporal PA patterns of U.S. adults ages 20–65 y as drawn from the NHANES, 2003–2006a.
| Adjusted modelsb | n (%) | WCc, (cm) | βd ± SE compare to Cluster 2 | 95% CI | βd± SE compare to Cluster 3 | 95% CI | βd ± SE Compare to Cluster 4 | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Cluster 1 | 783 (39.2) | 101.4 (0.6) | 5.9 ± 1.6 | 1.6, 10.2f | 6.4 ± 1.3 | 2.8, 10.0f | 3.6 ± 1.3 | 0.1, 7.0e |
| Cluster 2 | 247 (12.4) | 94.2 (0.9) | 0.5 ± 1.3 | −3.0, 3.9 | −2.3 ± 1.2 | −5.6, 0.9 | ||
| Cluster 3 | 336 (16.8) | 93.9 (0.8) | −2.8 ± 1.0 | −5.6, −0.1e | ||||
| Cluster 4 | 633 (31.6) | 97.6 (0.6) |
Note. WC: waist circumference, SE: standard error
Significant differences among clusters in mean WC were present amongst all clusters except Clusters 2 and 3 in the unadjusted model at p<0.05 (see Appendix B).
Models were adjusted for survey year, sex, age, employment status, marital status, household size, race/ethnicity, poverty to income ratio, and total activity counts/day.
Values are Mean (SEM).
ß represents difference between mean WC of cluster and reference cluster. Differences in mean WC are different than those between raw means because they represent differences in least square means.
p<0.05
p<0.01
Significant differences in the odds of obesity relative to normal weight status were present between all clusters except Clusters 1 and 4 as well as 2 and 3 in the unadjusted model (see Appendix B). In adjusted models, significant differences were present between all clusters except Clusters 1 and 4 as well as 2 and 3 (Table 5). The significantly different odds of obesity was greatest between Clusters 1 and 2 (OR: 2.9, 95% CI: 1.3, 6.7), similar to results in the unadjusted model (OR: 3.8, 95% CI: 2.0, 7.2; see Appendix B).
Table 5.
Odds of obesity relative to normal weight status and covariate-adjusted regression model results for clusters representing temporal PA patterns of U.S. adults ages 20–65 y as drawn from the NHANES, 2003–2006a.
| Adjusted modelsb | n (%) | ORc,d compare to Cluster 2 | 95% CI | ORc,d compare to Cluster 3 | 95% CI | ORc,d compare to Cluster 4 | 95% CI |
|---|---|---|---|---|---|---|---|
| Cluster 1 | 783 (39.2) | 2.9 | 1.3, 6.7f | 2.4 | 1.3, 4.4f | 1.3 | 0.7, 2.4 |
| Cluster 2 | 247 (12.4) | 0.8 | 0.4, 1.6 | 0.5 | 0.2, 0.9f | ||
| Cluster 3 | 336 (16.8) | 0.6 | 0.3, 0.9e | ||||
| Cluster 4 | 633 (31.6) |
Note.
Significant differences among clusters in odds ratio of obesity relative to normal weight status in the unadjusted model were similar to those in the adjusted model at p<0.01 (see Appendix B).
Models were adjusted for survey year, sex, age, employment status, marital status, household size, race/ethnicity, poverty to income ratio, and total activity counts/day.
OR represents odds ratio of obesity relative to normal of cluster and reference cluster.
Obesity was defined as BMI ≥ 30 kg/m2(World Health Organization, 2020b).
p<0.05
p<0.01
Unadjusted and adjusted model results for the other health status indicators, T2D and MetS are available in Appendix B. In the adjusted models, one significant difference was present in mean hemoglobin A1c between Clusters 1 and 3 (β=0.2, 95% CI: 0.0, 0.4; see Appendix B) and in odds of T2D between Clusters 2 and 4 (OR: 3.1, 95% CI: 1.2, 8.1; see Appendix B). There were no significant differences in the adjusted models of all other examined health status indicators and MetS (see Appendix B).
Discussion
Temporal PA patterns are associated with BMI, WC and obesity. Clinical relevance of differences in mean BMI and WC associated with temporal PA patterns may be contended (Bodegard et al., 2013; Cerhan et al., 2014; Mulligan et al., 2019). Therefore, observed mean differences in health status indicators imply that temporal PA patterns may be an important health exposure that holds promise for early detection of lifestyle factors promoting health and disease in the population. Reverse causation in the observed associations cannot be ruled out using the cross-sectional study design, nevertheless, the aim of this study was not to establish causation but to examine whether developed patterns using a novel methodology meaningfully link to health.
An abundance of research examines the relationship between PA and health. Most studies have focused on categorizing participants based on intensity and frequency of activity (Fishman et al., 2016; Luke et al., 2011; Tudor-Locke et al., 2017), while others examined daily PA patterns focused on distinct time periods such as type of day (weekday vs. weekend) (Treuth et al., 2007), activity phenotypes including “weekend warrior” (Metzger et al., 2008; Michael, 2014), and seasonality (Silva et al., 2011). A few studies investigated diurnal patterns of PA (data collected over 5–7 days) and health (Fukuoka et al., 2018; Niemelä et al., 2019; Xu et al., 2019; Zeitzer et al., 2018). Distinct temporal PA patterns observed in this study have been detected by two other studies that used k-means and x-means clustering approaches to derive clusters using time and overall activity measured by metabolic equivalent of tasks (METs) (Fukuoka et al., 2018; Niemelä et al., 2019). Similarities with the current study include presence of an overall inactive/low activity pattern (Cluster 1) and two patterns of higher activity that differed in timing of activity “afternoon engaged/morning engaged” (Fukuoka et al., 2018) or “moderately active/evening active” (Niemelä et al., 2019) (“early/late peaks” in activity in Clusters 4 and 3, respectively).
Cluster 1 was associated with significantly higher BMI, WC, and odds of obesity compared with Clusters 2 and 3, which demonstrates that a lower activity pattern is linked with the most adverse health outcomes as evidenced by prior research (Arsenault et al., 2010; Chastin et al., 2015; Fishman et al., 2016). This cluster included the highest number of participants (39.2%) which supports evidence of a high level of sedentary behavior among U.S. adults (U.S. Department of Health and Human Services, 2018; Diaz et al., 2016; Yang et al., 2019). Moreover, Cluster 1 predominantly includes ages 50–65 y, which is consistent with evidence that activity tends to decline with age (Basset et al., 2010).
Findings of significantly lower mean BMI and WC associated with Clusters 2, 3, and 4 compared with Cluster 1 with the lowest activity counts as well as significantly lower odds of obesity associated with Clusters 2 and 3 (higher activity counts throughout and later in a day, respectively) compared to Clusters 1 and 4 (low activity counts throughout or early in a day, respectively) support previous literature showing that higher activity counts are associated with improved health status (Dyck et al., 2015; Healy et al., 2011; Strath et al., 2008), but add new information regarding the timing of these patterns. Additionally, the significantly lower mean WC and odds of obesity in Cluster 3 (higher PA counts performed between 16:00–21:00) compared to Cluster 4 (higher PA counts performed between 8:00–11:00) is interesting as models controlled for TAC thus, these findings may indicate that observed differences could be explained by temporal differences in these patterns. Limited evidence exists regarding the relevance of time of activity through the day in terms of links to health (Fukuoka et al., 2018; Niemelä et al., 2019; Xu et al., 2019; Zeitzer et al., 2018), so further development of temporal PA patterns may allow additional exploration of time as a potentially important factor.
Certain sociodemographic characteristics such as those included in this study (Table 1) have been shown to be associated with PA-related differences in health. Temporal PA patterns with higher counts (Clusters 2, 3, and 4) were more heavily represented by males, which corroborates trends observed in two U.S. surveillance systems showing males were significantly more likely to be physically active compared to females (Carlson et al., 2009). Additionally, the low proportion of participants with PIR level of 0–0.99 included in the clusters with higher PA counts and a respectively high proportion of participants with PIR level of 0–0.99 included in the cluster with the lowest activity counts (Cluster 1) supports findings of an inverse relationship between prevalence of PA and household poverty level (Bassett et al., 2010).
Elements other than intensity and duration of activity such as time of activity can be an important aspect of PA patterns and may describe PA better within the context of lifestyle. Moreover, timing of activity occasions may also be tied to dietary intake and sleep-wake regimens. For instance, an individual with a “night owl” behavior pattern may have a greater evening preference and choose to exercise later compared to one with an “early bird” morning preference (Marinac et al., 2019). Insights to these behaviors within a day and as part of an overall routine over the long-term (months and years) may reveal stronger associations to health compared to their separate consideration and allow for more targeted interventions based on overall lifestyle. Further, the rapid accumulation of data on health behaviors through technology-assisted assessment tools including those targeting dietary and activity patterns will provide additional data for future investigation of whether and how the timing of these activities influences health. Integrating these data will add further knowledge of how daily behavioral patterns may contribute to metabolic dysfunction and chronic disease.
Strengths of this research include the use of a comprehensive approach to classifying PA exposure that considers the complexity of activity over a 24-hour period. Limitations of this study include the cross-sectional nature which provides a snapshot of the participants’ activity patterns and cannot demonstrate causation. Also, the sample size represented ~8% of the original sample of participants; therefore, study results should be interpreted with caution. Attrition was mostly attributable to the age range 20–65 y and the inclusion of health status indicators examined in a fasting subsample of participants (both criteria resulted in ~84% loss of the original sample). Additionally, one valid weekday was used to represent activity occasions of the participants; since information regarding the distribution of timing of activity patterns over multiple days is limited, exploration of the time, counts, and sequence of activity over multiple days represents a research gap for future study. Furthermore, though a valid day has been shown to be sufficient for producing reliable population-level estimates of accelerometer-measured activity (Wolff-Hughes et al., 2016), patterns of activity could differ based on type of day and may potentially vary more on the weekends compared with the weekdays. Finally, accelerometers do not capture all types of activity including static activities (NHANES data documentation, 2005f) and may not represent the true activity levels of the U.S. population (Metzger et al., 2008).
Conclusion
In this cross-sectional study, temporal PA patterns were found to be associated with BMI, WC, and obesity. Individuals with higher activity counts performed throughout the day, early (8:00 to 11:00) or late (16:00 to 21:00) in a day exhibited lower mean BMI and WC compared to those with lower activity counts. The incorporation of time of day with total counts and sequence of activity is possible to create temporal PA patterns that are related to health. Future analysis of prospective cohort studies is needed to examine whether these patterns are linked to chronic disease.
Supplementary Material
Appendix A. Flow chart representing sample size attrition and reason for exclusion.
Appendix B. Unadjusted and adjusted regression model results for all examined health status indicators and disease categories.
Temporal patterns created by a data-driven approach link meaningfully with health
Dynamic time warping and kernel-k means for time-based physical activity patterns
Joining time and physical activity for multidimensional patterns linked to health
Temporal patterns of higher physical activity counts related to health status
Temporal activity patterns are associated with BMI and waist circumference
Acknowledgments
Funding: This research was supported by the National Cancer Institute of the National Institutes of Health under award number R21CA224764 and Purdue University. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Prior to issuing a press release concerning the outcomes of this research, please notify the NIH awarding IC in advance to allow for coordination.
List of abbreviations:
- BMI
body mass index
- CDTW
constrained with Sakoe-Chiba band dynamic time warping
- cph
counts/hour
- DTW
dynamic time warping
- HDL-C
high-density lipoprotein cholesterol
- MDTW
modified dynamic time warping
- NCHS
National Center for Health Statistics
- NHANES
Nutrition and Health Examination Survey
- PA
physical activity
- PIR
poverty to income ratio
- TAC
total activity counts/day
- WC
waist circumference
Footnotes
HAE-M, ED, SD, AB, EAR, EH: Funding Acquisition. HAE-M, ED, SG, AB, EAR, EH, MA, JG, and LL: Conceptualization and Methodology. MA, JG, and LL: Formal Analysis. HAEM, ED, and SG: Supervision. MA: Writing- Original draft preparation. HAE-M, ED, SG, AB, EAR, EH, MA, JG and LL: Writing- Reviewing and Editing, All authors read and approved the final manuscript.
Declaration of interests
☒ The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Conflict of interest: none.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- Alexander CM, Landsman PB, Teutsch SM, Haffner SM, 2003. NCEP-Defined Metabolic Syndrome, Diabetes, and Prevalence of Coronary Heart Disease Among NHANES III Participants Age 50 Years and Older. Diabetes 52, 1210–1214. 10.2337/diabetes.52.5.1210 [DOI] [PubMed] [Google Scholar]
- Alizadeh Z, Younespour S, Rajabian Tabesh M, Haghravan S, 2017. Comparison between the effect of 6 weeks of morning or evening aerobic exercise on appetite and anthropometric indices: a randomized controlled trial. Clin. Obes. 7, 157–165. 10.1111/cob.12187 [DOI] [PubMed] [Google Scholar]
- American Diabetes Association, 2014. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 37, S81–S90. Available from: 10.2337/dc14-S081 (Accessed Mar 20, 2020). [DOI] [PubMed] [Google Scholar]
- Marah Aqeel, Jiaqi Guo, Luotao Lin, Saul Gelfand, Edward Delp, Anindya Bhadra, Elizabeth Richards, Erin Hennessy, Heather Eicher-Miller, 2020. Temporal Dietary Patterns are Associated with Obesity in U.S. Adults. J Nutr. 150 (12), 3259–3268. 10.1093/jn/nxaa287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arsenault BJ, Rana JS, Lemieux I, Després J-P, Kastelein JJP, Boekholdt SM, Wareham NJ, Khaw K-T, 2010. Physical inactivity, abdominal obesity and risk of coronary heart disease in apparently healthy men and women. Int. J. Obes. 34, 340–347. 10.1038/ijo.2009.229 [DOI] [PubMed] [Google Scholar]
- Bassett DR, Wyatt HR, Thompson H, Peters JC, Hill JO, 2010. Pedometer-Measured Physical Activity and Health Behaviors in U.S. Adults: Med. Sci. Sports Exerc. 42, 1819–1825. 10.1249/MSS.0b013e3181dc2e54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodegard J, Sundström J, Svennblad B, Östgren CJ, Nilsson PM, Johansson G, 2013. Changes in body mass index following newly diagnosed type 2 diabetes and risk of cardiovascular mortality: A cohort study of 8486 primary-care patients. Diabetes Metab. 39, 306–313. 10.1016/j.diabet.2013.05.004 [DOI] [PubMed] [Google Scholar]
- Carlson SA, Densmore D, Fulton JE, Yore MM, Kohl HW, 2009. Differences in Physical Activity Prevalence and Trends from 3 U.S. Surveillance Systems: NHIS, NHANES, and BRFSS. J. Phys. Act. Health 6, S18–S27. 10.1123/jpah.6.s1.s18 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2020a. National Center for Health Statistics (NCHS). About the National Health and Nutrition Examination Survey (NHANES) Available from: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm (Accessed Mar 27, 2020).
- Centers for Disease Control and Prevention (CDC), 2020b. National Center for Health Statistics (NCHS). NCHS Research Ethics Review Board (ERB) Approval Available from: http://www.cdc.gov/nchs/nhanes/irba98.htm (Accessed Dec 25, 2019).
- Cerhan JR, Moore SC, Jacobs EJ, Kitahara CM, Rosenberg PS, Adami H-O, Ebbert JO, English DR, Gapstur SM, Giles GG, Horn-Ross PL, Park Y, Patel AV, Robien K, Weiderpass E, Willett WC, Wolk A, Zeleniuch-Jacquotte A, Hartge P, Bernstein L, Berrington de Gonzalez A, 2014. A Pooled Analysis of Waist Circumference and Mortality in 650,000 Adults. Mayo Clin. Proc. 89, 335–345. 10.1016/j.mayocp.2013.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chastin SFM, Palarea-Albaladejo J, Dontje ML, Skelton DA, 2015. Combined Effects of Time Spent in Physical Activity, Sedentary Behaviors and Sleep on Obesity and Cardio-Metabolic Health Markers: A Novel Compositional Data Analysis Approach. PLOS ONE 10, e0139984. 10.1371/journal.pone.0139984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chomistek AK, Shiroma EJ, Lee I-M, 2016. The Relationship Between Time of Day of Physical Activity and Obesity in Older Women. J. Phys. Act. Health 13, 416–418. 10.1123/jpah.2015-0152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chomistek AK, Yuan C, Matthews CE, Troiano RP, Bowles HR, Rood J, Barnett JB, Willett WC, Rimm EB, Bassett DR, 2017. Physical Activity Assessment with the ActiGraph GT3X and Doubly Labeled Water: Med. Sci. Sports Exerc. 49, 1935–1944. 10.1249/MSS.0000000000001299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Després J-P, Lemieux I, 2006. Abdominal obesity and metabolic syndrome. Nature 444, 881–887. [DOI] [PubMed] [Google Scholar]
- Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JE, Blair SN, Hooker SP, 2016. Patterns of Sedentary Behavior in US Middle-Age and Older Adults: The REGARDS Study. Med. Sci. Sports Exerc. 48, 430–438. 10.1249/MSS.0000000000000792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeo F, Pagonas N, Seibert F, Arndt R, Zidek W, Westhoff TH, 2012. Aerobic Exercise Reduces Blood Pressure in Resistant Hypertension. Hypertension 60, 653–658. 10.1161/HYPERTENSIONAHA.112.197780 [DOI] [PubMed] [Google Scholar]
- Dyck DV, Cerin E, De Bourdeaudhuij I, Hinckson E, Reis RS, Davey R, Sarmiento OL, Mitas J, Troelsen J, MacFarlane D, Salvo D, Aguinaga-Ontoso I, Owen N, Cain KL, Sallis JF, 2015. International study of objectively measured physical activity and sedentary time with body mass index and obesity: IPEN adult study. Int. J. Obes. 39, 199–207. 10.1038/ijo.2014.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eicher-Miller HA, Gelfand S, Hwang Y, Delp E, Bhadra A, Guo J, 2020. Distance metrics optimized for clustering temporal dietary patterning among U.S. adults. Appetite 144, 104451. 10.1016/j.appet.2019.104451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eicher-Miller HA, Khanna N, Boushey CJ, Gelfand SB, Delp EJ, 2016. Temporal Dietary Patterns Derived among the Adult Participants of the National Health and Nutrition Examination Survey 1999–2004 Are Associated with Diet Quality. J. Acad. Nutr. Diet. 116, 283–291. 10.1016/j.jand.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishman EI, Steeves JA, Zipunnikov V, Koster A, Berrigan D, Harris TA, Murphy R, 2016. Association between Objectively Measured Physical Activity and Mortality in NHANES: Med. Sci. Sports Exerc. 48, 1303–1311. 10.1249/MSS.0000000000000885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuoka Y, Zhou M, Vittinghoff E, Haskell W, Goldberg K, Aswani A, 2018. Objectively Measured Baseline Physical Activity Patterns in Women in the mPED Trial: Cluster Analysis. JMIR Public Health Surveill. 4, e10. 10.2196/publichealth.9138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N, 2011. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur. Heart J. 32, 590–597. 10.1093/eurheartj/ehq451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhillon IS, Guan Y, and Kulis B., 2004. Kernel k-means, spectral clustering and normalized cuts. Presented at the Proceedings of the tenth ACM SIGKDD international conference on Knowledge discovery and data mining, Seattle, WA, USA., pp. 551–556. [Google Scholar]
- Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR, 2013. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vital Health Stat. Ser. 2, Data Eval. Methods Res. 161, 1–24 [PubMed] [Google Scholar]
- Khanna N, Eicher-Miller HA, Boushey CJ, Gelfand SB, Delp EJ, 2011. Temporal Dietary Patterns Using Kernel k-Means Clustering, in: 2011 IEEE International Symposium on Multimedia. Presented at the 2011 IEEE International Symposium on Multimedia (ISM), IEEE, Dana Point, CA, USA, pp. 375–380. 10.1109/ISM.2011.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littman AJ, Kristal AR, White E, 2005. Effects of physical activity intensity, frequency, and activity type on 10-y weight change in middle-aged men and women. Int. J. Obes. 29, 524–533. 10.1038/sj.ijo.0802886 [DOI] [PubMed] [Google Scholar]
- Luke A, Dugas LR, Durazo-Arvizu RA, Cao G, Cooper RS, 2011. Assessing Physical Activity and its Relationship to Cardiovascular Risk Factors: NHANES 2003–2006. BMC Public Health 11, 387. 10.1186/1471-2458-11-387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinac CR, Quante M, Mariani S, Weng J, Redline S, Cespedes Feliciano EM, Hipp JA, Wang D, Kaplan ER, James P, Mitchell JA, 2019. Associations Between Timing of Meals, Physical Activity, Light Exposure, and Sleep With Body Mass Index in Free-Living Adults. J. Phys. Act. Health 16, 214–221. 10.1123/jpah.20170389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell MA, Fryar CD, Ogden CL, Flegal KM, 2008. National Health Statistics Reports. Anthropometric Reference Data for Children and Adults: United States, 20032006. 10.1037/e623932009-001 [DOI] [PubMed] [Google Scholar]
- Mellen PB, Gao SK, Vitolins MZ, Goff DC, 2008. Deteriorating Dietary Habits Among Adults With Hypertension: DASH Dietary Accordance, NHANES 1988–1994 and 1999–2004. Arch. Intern. Med. 168, 308–314. 10.1001/archinternmed.2007.119 [DOI] [PubMed] [Google Scholar]
- Metzger JS, Catellier DJ, Evenson KR, Treuth MS, Rosamond WD, Siega-Riz AM, 2010. Associations between Patterns of Objectively Measured Physical Activity and Risk Factors for the Metabolic Syndrome. Am. J. Health Promot. 24, 161–169. 10.4278/ajhp.08051151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzger JS, Catellier DJ, Evenson KR, Treuth MS, Rosamond WD, Siega-Riz AM, 2008. Patterns of Objectively Measured Physical Activity in the United States: Med. Sci. Sports Exerc. 40, 630–638. 10.1249/MSS.0b013e3181620ebc [DOI] [PubMed] [Google Scholar]
- Michael M, 2014. Clustering physical activity phenotypes using the ATLAS index on accelerometric data from an epidemiologic cohort study. Stud. Health Technol. Inform. 763–767. 10.3233/978-1-61499-432-9-763 [DOI] [PubMed] [Google Scholar]
- Mulligan AA, Lentjes MAH, Luben RN, Wareham NJ, Khaw K-T, 2019. Changes in waist circumference and risk of all-cause and CVD mortality: results from the European Prospective Investigation into Cancer in Norfolk (EPIC-Norfolk) cohort study. BMC Cardiovasc. Disord. 19, 238. 10.1186/s12872-019-1223-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHANES contents in detail, 2003. NHANES 2003–2004. Available from: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/manuals.aspx?BeginYear=2003 (Accessed December 21, 2019).
- NHANES contents in detail, 2005. NHANES 2005–2006. Available from: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2005 (Accessed December 21, 2019).
- NHANES data documentation, 2003a. NHANES 2003–2004. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2003-2004/L10AM_C.htm (Accessed Dec 28, 2019).
- NHANES data documentation, 2003b. NHANES 2003–2004. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2003-2004/L13AM_C.htm (Accessed Dec 28, 2019).
- NHANES data documentation, 2003c. NHANES 2003–2004. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2003-2004/L10_C.htm (Accessed Dec 29, 2019).
- NHANES data documentation, 2003d. NHANES 2003–2004. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2003-2004/L13_C.htm (Accessed Dec 28, 2019).
- NHANES data documentation, 2005a. NHANES 2005–2006. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/GLU_D.htm (Accessed Dec 28, 2019).
- NHANES data documentation, 2005b. NHANES 2005–2006. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/TRIGLY_D.htm (Accessed Dec28, 2019).
- NHANES data documentation, 2005c. NHANES 2005–2006. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/GHB_D.htm (Accessed Dec 29, 2019).
- NHANES data documentation, 2005d. NHANES 2005–2006. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/TCHOL_D.htm (Accessed Dec 21, 2019).
- NHANES data documentation, 2005e. NHANES 2005–2006. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/HDL_D.htm (Accessed Dec 20, 2019).
- NHANES data documentation, 2005f. NHANES 2005–2006. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/PAXRAW_D.htm (Accessed Dec 20, 2019).
- Nguyen NT, Nguyen X-MT, Lane J, Wang P, 2011. Relationship Between Obesity and Diabetes in a US Adult Population: Findings from the National Health and Nutrition Examination Survey, 1999–2006. Obes. Surg 21, 351–355. 10.1007/s11695010-0335-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemelä M, Kangas M, Farrahi V, Kiviniemi A, Leinonen A-M, Ahola R, Puukka K, Auvinen J, Korpelainen R, Jämsä T, 2019. Intensity and temporal patterns of physical activity and cardiovascular disease risk in midlife. Prev. Med. 124, 33–41. 10.1016/j.ypmed.2019.04.023 [DOI] [PubMed] [Google Scholar]
- Silva P, Welk G, Mota J, 2011. Seasonal differences in physical activity and sedentary patterns: The relevance of the PA context. J Sports Sci Med 10, 66–72. [PMC free article] [PubMed] [Google Scholar]
- Strath SJ, Holleman RG, Ronis DL, Swartz AM, Richardson CR, 2008. Objective Physical Activity Accumulation in Bouts and Nonbouts and Relation to Markers of Obesity in US Adults. Prev Chronic Dis. 5, 11. [PMC free article] [PubMed] [Google Scholar]
- Swift DL, McGee JE, Earnest CP, Carlisle E, Nygard M, Johannsen NM, 2018. The Effects of Exercise and Physical Activity on Weight Loss and Maintenance. Prog. Cardiovasc. Dis. 61, 206–213. 10.1016/j.pcad.2018.07.014 [DOI] [PubMed] [Google Scholar]
- Treuth MS, Catellier DJ, Schmitz KH, Pate RR, Elder JP, McMurray RG, Blew RM, Yang S, Webber L, 2007. Weekend and Weekday Patterns of Physical Activity in Overweight and Normal-weight Adolescent Girls*. Obesity 15, 1782–1788. 10.1038/oby.2007.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, Mcdowell M, 2008. Physical Activity in the United States Measured by Accelerometer: Med. Sci. Sports Exerc. 40, 181–188. 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- Trombold JR, Christmas KM, Machin DR, Kim I-Y, Coyle EF, 2013. Acute high-intensity endurance exercise is more effective than moderate-intensity exercise for attenuation of postprandial triglyceride elevation. J. Appl. Physiol. 114, 792–800. 10.1152/japplphysiol.01028.2012 [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Schuna JM, Han H, Aguiar EJ, Green MA, Busa MA, Larrivee S, Johnson WD, 2017. Step-Based Physical Activity Metrics and Cardiometabolic Risk: NHANES 2005–2006. Med. Sci. Sports Exerc. 49, 283–291. 10.1249/MSS.0000000000001100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services; 2018. 2018 Physical Activity Guidelines for Americans. Washington, D.C., pp 1–118. Available from: https://health.gov/ourwork/physical-activity/current-guidelines (Accessed April 10, 2020). [Google Scholar]
- Waller K, Kaprio J, Kujala UM, 2008. Associations between long-term physical activity, waist circumference and weight gain: a 30-year longitudinal twin study. Int. J. Obes. 32, 353–361. 10.1038/sj.ijo.0803692 [DOI] [PubMed] [Google Scholar]
- Wolff-Hughes DL, McClain JJ, Dodd KW, Berrigan D, Troiano RP, 2016. Number of accelerometer monitoring days needed for stable group-level estimates of activity. Physiol. Meas. 37, 1447–1455. 10.1088/0967-3334/37/9/1447 [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2020a. Obesity and overweight. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed March 15, 2020).
- World Health Organization, 2020b: Body Mass Index-BMI. Available from: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (Accessed Feb 10, 2020).
- Xu SY, Nelson S, Kerr J, Godbole S, Johnson E, Patterson RE, Rock CL, Sears DD, Abramson I, Natarajan L, 2019. Modeling Temporal Variation in Physical Activity Using Functional Principal Components Analysis. Stat. Biosci. 11, 403–421. 10.1007/s12561-019-09237-3 [DOI] [Google Scholar]
- Yang L, Cao C, Kantor ED, Nguyen LH, Zheng X, Park Y, Giovannucci EL, Matthews CE, Colditz GA, Cao Y, 2019. Trends in Sedentary Behavior Among the US Population, 2001–2016. JAMA 321, 1587. 10.1001/jama.2019.3636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeitzer JM, Blackwell T, Hoffman AR, Cummings S, Ancoli-Israel S, Stone K, Osteoporotic Fractures in Men (MrOS) Study Research Group, 2018. Daily Patterns of Accelerometer Activity Predict Changes in Sleep, Cognition, and Mortality in Older Men. J. Gerontol. Ser. A 73, 682–687. 10.1093/gerona/glw250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H, Chu X-Q, Lian X-Q, Wang Z-M, Gao W, Wang L-S, 2014. Relationship Between Time of Day Physical Exercise and the Reduced Risk of Coronary Artery Disease in a Chinese Population. Int. J. Sport Nutr. Exerc. Metab. 24, 139–147. 10.1123/ijsnem.2012-0226 [DOI] [PubMed] [Google Scholar]
- Zhao S, Zhang Z, Long Q, Ma Y, Lian X, Yang Y, Gao W, Chen Z, Wang L, 2016. Association between Time of Day of Sports-Related Physical Activity and the Onset of Acute Myocardial Infarction in a Chinese Population. PLOS ONE 11, e0146472. 10.1371/journal.pone.0146472 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix A. Flow chart representing sample size attrition and reason for exclusion.
Appendix B. Unadjusted and adjusted regression model results for all examined health status indicators and disease categories.