Abstract
Objective
The phenotypic plasticity of vascular smooth muscle cells (VSMCs) is central to vessel growth and remodeling, but also contributes to cardiovascular pathologies. New technologies including fate mapping, single cell transcriptomics, and genetic and pharmacologic inhibitors have provided fundamental new insights into the biology of VSMC. The goal of this review is to summarize the mechanisms underlying VSMC phenotypic modulation and how these might be targeted for therapeutic benefit.
Methods
We summarize findings from extensive literature searches to highlight recent discoveries in the mechanisms underlying VSMC phenotypic switching with particular relevance to intimal hyperplasia. PubMed was searched for publications between January 2001 and December 2020. Search terms included VSMCs, restenosis, intimal hyperplasia, phenotypic switching or modulation, and drug-eluting stents. We sought to highlight druggable pathways as well as recent landmark studies in phenotypic modulation.
Results
Lineage tracing methods have determined that a small number of mature VSMCs dedifferentiate to give rise to oligoclonal lesions in intimal hyperplasia and atherosclerosis. In atherosclerosis and aneurysm, single cell transcriptomics reveal a striking diversity of phenotypes that can arise from these VSMCs. Mechanistic studies continue to identify new pathways that influence VSMC phenotypic plasticity. We review the mechanisms by which the current drug-eluting stent agents prevent restenosis and note remaining challenges in peripheral and diabetic revascularization for which new approaches would be beneficial. We summarize findings on new epigenetic (DNA methylation/TET methylcytosine dioxygenase 2, histone deacetylation, bromodomain proteins), transcriptional (Hippo/Yes-associated protein, peroxisome proliferator-activity receptor-gamma, Notch), and β3-integrin-mediated mechanisms that influence VSMC phenotypic modulation. Pharmacologic and genetic targeting of these pathways with agents including ascorbic acid, histone deacetylase or bromodomain inhibitors, thiazolidinediones, and integrin inhibitors suggests potential therapeutic value in the setting of intimal hyperplasia.
Conclusions
Understanding the molecular mechanisms that underlie the remarkable plasticity of VSMCs may lead to novel approaches to treat and prevent cardiovascular disease and restenosis.
Keywords: Smooth muscle, Intimal hyperplasia, Restenosis, Atherosclerosis, Differentiation, Phenotypic modulation
Methods
We summarize findings from extensive literature searches to highlight recent discoveries in the mechanisms underlying vascular smooth muscle cell (VSMC) phenotypic switching with particular relevance to intimal hyperplasia. PubMed was searched from January 2001 to December 2020. Search terms included vascular smooth muscle cells, restenosis, intimal hyperplasia, phenotypic switching or modulation, and drug-eluting stents. Case reports and retrospective studies were excluded. We highlight pathways with therapeutic potential and recent landmark studies, preferentially selecting studies incorporating both in vitro and in vivo evidence. We do not focus on microRNAs (miRNAs), which are reviewed thoroughly elsewhere.1 We regret that space constraints preclude a truly comprehensive review given the scope of this field.
VSMC phenotypic switching
VSMCs comprise the muscular tunica media where their contractile function regulates vascular tone and diameter, blood pressure, and blood flow distribution to tissues. Although these cells contribute to cardiovascular pathologies such as intimal hyperplasia and restenosis, it is now increasingly appreciated that VSMCs, through their unique phenotypic plasticity, represent a reservoir of distinct potential fates that influence vascular physiology in many ways. Pathologies of phenotypically modulated VSMCs include atherosclerosis, vascular calcification, intimal hyperplasia and restenosis, transplant vasculopathy, aneurysm, hypertension, and abnormal tumor vasculature. In this review, we focus on the contribution of VSMCs to intimal hyperplasia and on the pathways that target VSMC phenotypic modulation by current drug-eluting stent agents as well as evolving research on pathways that suggest novel therapeutic approaches.
VSMCs are distinct from skeletal and cardiac myocytes in that they do not terminally differentiate, but retain a high degree of cellular plasticity allowing these cells to dramatically alter their phenotype in response to environmental cues and extracellular signals.2 This property allows for VSMC to contribute to the growth, remodeling, and repair of the vasculature, but can also drive cardiovascular pathologies. In a mature healthy vessel, VSMC exhibit a differentiated quiescent contractile state and rarely proliferate.3 This differentiated phenotype is characterized by expression of a repertoire of smooth muscle (SM)-specific contractile and contractile-associated proteins including SM-myosin heavy chain (MYH11), SM-α-actin (ACTA2), SM22α (TAGLN), calponin (CNN1), h-caldesmon (CALD1), smoothelin (SMTN),2 leiomodin 1 (LMOD1),4 channel proteins K(VCA)Beta-1 (KCNMB1)5 and Kv1.5 (KCNA5),6 and the intermediate filament protein synemin (SYNM)7 (Fig 1). Differentiated VSMC also exhibit a typical elongated myocyte morphology. Depending on environmental stimuli or cell culture conditions, VSMC can dedifferentiate to a variety of distinct phenotypes.8,9 VSMC phenotypic modulation can be monitored by multiple characteristics, including the downregulation of the contractile marker genes and loss of contractility. Modulated VSMC also acquire new phenotype-specific genes, morphologies, and functions, including proliferation, migration, and altered extracellular matrix (ECM) synthesis.
Fig 1.
Characteristics of the differentiated contractile and dedifferentiated “synthetic” vascular smooth muscle cell (VSMC) phenotypes. VSMCs exist in a quiescent, contractile differentiated phenotype characterized by an elongated myocyte morphology (white arrow) and the indicated marker genes. In response to stimuli such as platelet-derived growth factor (PDGF)-BB, VSMCs switch to a dedifferentiated synthetic phenotype with rhomboid morphology characterized by increased protein synthesis, proliferation, migration, and upregulation of the indicated genes.
Many signals influence VSMC phenotype. These include contractility, mechanical forces, integrins, ECM, cytokines, and growth factors. Through multiple distinct signaling pathways (reviewed in10), extracellular inputs converge on core transcription factors that govern VSMC differentiation. These include SRF and myocardin, which act at the CArG [CC(A/T)6GG DNA binding motif] regulatory elements in the proximal promoters or introns of most contractile genes, and KLF4, a factor induced by platelet-derived growth factor (PDGF) that binds to GC elements near CArGs and promotes dedifferentiation. Notably, Kruppel-like factor 4 (KLF4) and octamer-binding transcription factor 4 (OCT4) are both stem cell genes involved in reprogramming and have been shown to play key roles in VSMC phenotype in mouse atherosclerotic lesions.11,12 This expression of these Yamanaka factors13 may help to explain the dramatic phenotypic plasticity of VSMCs. Epigenetic mechanisms also contribute to VMSC plasticity,14 with TET methylcytosine dioxygenase 2 (TET2)15 and DNA methyltransferases (DNMT)16 playing key roles. Histone acetylation also influences VSMC phenotype14 (see the Histone deacetylase section). Importantly, the histone modification H3K4me2 at contractile gene proximal promoter CArG elements serves a permanent marker of the VSMC lineage that persists despite phenotypic modulation14,17 and may represent a key mechanism that defines VSMC lineage identity and plasticity. miRNAs are also important regulators of VSMC phenotype and have therapeutic potential. These include miR-145, which regulates KLF4.18 Although miRNAs have therapeutic potential, we refer the reader to extensive reviews on miRNAs in VSMCs.1,19
VSMC phenotypic switching in disease states
Intimal hyperplasia and restenosis
VSMC undergo dedifferentiation in response to mechanical vascular injury as occurs in arterial balloon angioplasty or stenting. Although VSMCs in mature atherosclerotic plaques have already undergone dedifferentiation to a spectrum of phenotypes (see the Atherosclerosis and calcification section), inflation of the balloon distends the vessel, causing mechanical injury to the vessel wall. This injury-induced phenotypic modulation of VSMCs promotes repair of the lesion, but failure to appropriately resolve the healing response can lead to intimal hyperplasia and restenosis.20 Intimal hyperplasia is not limited to catheter-based interventions, but also occurs at anastomoses in bypass procedures, grafts, and fistula creation. In these injury-induced cases, local inflammatory stimuli promote VSMC phenotypic switching to a “synthetic” phenotype, characterized by a loss of contractile markers, a transition to a rhomboid morphology, and a marked increase in proliferation, migration, and protein synthesis. In the context of injury, dedifferentiated VSMC re-enter the cell cycle and migrate from the medial layer to the vessel intima. These intimal VSMC synthesize and secrete copious ECM components and proteins that contribute to remodeling such as matrix metalloproteinases (MMPs). This dedifferentiation is stimulated, in part, by growth factors secreted by platelets and other proinflammatory cells, including PDGF-BB.21 Transforming growth factor (TGF-β) is also highly upregulated post-injury and contributes to the ECM synthesis and intimal hyperplasia.22 In some cases, the remodeling resolves with the restoration of the vascular structural integrity and redifferentiation of the intimal VSMC to a quiescent, contractile state. In others cases, the inward remodeling does not resolve and progresses to intimal hyperplasia, often requiring repeat revascularization.23 Recent studies using multicolor lineage tracing have shown that a small number of VSMCs expand after injury to form clonal patches of neointimal cells.24 Identifying the mechanistic basis for the clonal expansion of these cells could provide new preventive strategies. The use of drug-eluting stents (DES; discussed elsewhere in this article) has improved outcomes in coronary artery revascularization, but challenges remain, most notably in treatment of peripheral vascular disease.
Atherosclerosis and calcification
Atherosclerosis is a chronic inflammatory condition characterized by intimal plaque formation in arteries. Endothelial cell (EC) activation and monocyte infiltration to the intima in a proinflammatory, hypercholesterolemic environment are key initiating factors, promoting phenotypic modulation of VSMCs.25 VSMCs form the outer fibrous cap, but recent discoveries reveal that VSMCs comprise a much larger percentage of the plaque than previously appreciated.11 Groundbreaking studies using SM lineage tracing approaches are refining our understanding of the many diverse roles of VSMCs in the formation and morphology of atherosclerotic lesions. Notably, 80% of VSMCs in lesions are not identifiable using classical contractile markers owing to their modulated phenotype, but are revealed as VSMC derived by genetic fate mapping.11 As in intimal hyperplasia after injury, atherosclerotic plaques are formed by the clonal expansion of a small number of dedifferentiated VSMC.24,26 A recent fate mapping analysis in mouse aortic root lesions made the key observation that VSMC do not directly invade to the plaque interior from the tunica media. Rather, modulated VSMC begin to migrate from the media at the edge of the plaque at 6 weeks after the initiation of a high-fat diet, first forming a fibrous cap to fully surround the growing lipid- and macrophage-rich core, and then subsequently diving from the fibrous cap layer into the lesion interior, where they contribute to the growth of the plaque and lumen narrowing.26
Modulated VSMCs can influence the overall plaque morphology and stability in multiple ways, contributing to the stabilizing fibrous cap, but also to the plaque interior, where their inflammatory activation and apoptosis can augment the necrotic core.25 Subsets of modulated VSMCs contribute to inflammation, apoptosis, and ECM remodeling that ultimately influence lesion vulnerability. VSMCs can assume multiple distinct phenotypes in the plaque.11,12 This includes a state expressing some markers of macrophages but poor phagocytic function. Data from single cell transcriptomics in plaques identified a subset of VSMC-derived cells termed fibromyocytes, which depend on the transcription factor Tcf21 and confer a more stable morphology.8 A single cell analysis of advanced mouse brachiocephalic and human coronary artery atherosclerotic lesions revealed a striking diversity of VSMC-derived cell phenotypes.9 Importantly, this work found that Galectin-3 (Lgals3), a cell surface lectin,27 is a marker of VSMCs undergoing phenotypic transitions in lesions.9 Notably, Lgals3 was found to mark pioneer VSMCs that initially invest the lesion and are the source of at least three other types of cells, including cells that contribute to calcification and destabilization in advanced lesions.9 It is not yet known whether Lgals3 represents a universal marker of phenotypically modulating VSMC in all physiologic contexts, but studies suggest that it marks modulated VSMC in pulmonary hypertension (PH) and actively contributes to the proliferative, migratory, fibrotic phenotype.27 Understanding which atherosclerotic lesions require intervention vs those that are likely to be stable remains a clinical challenge. New insights into how VSMC influence molecular determinants of plaque stability may lead to new methods for evaluation and treatment of lesions.
Vascular calcification is an active and complex process, regulated by multiple factors including cytokine signaling pathways. It is frequently seen in atherosclerosis, chronic kidney disease, hypertension, and diabetes.28 Vascular calcification occurs primarily in the arterial media and intima, and numerous vascular cells, including SMCs, myofibroblasts, vascular mesenchymal progenitors, and ECs are involved.28 SMCs contribute significantly to vascular calcification and undergo an osteogenic phenotype transition characterized by the loss of contractile markers and the acquisition of osteogenic markers, including Runx1/Cbfa1, osteopontin, alkaline phosphatase, and osteocalcin.29,30 VSMC Runx2 plays critical roles in both osteoblastic differentiation and maturation of chondrocytes during atherosclerosis-induced vascular calcification.31 Osteoblast-like cells promote collagen calcification in the ECM that ultimately leads to increased rigidity and decreased arterial pliability.32
Aneurysm
Aortic aneurysm (AA) is a distention and weakening of the vessel wall that can lead to a life-threatening dissection or rupture. AA can be associated with genetic mutations (thoracic AA and dissection [TAAD]) or traditional cardiovascular risk factors (abdominal AA). AA is characterized by VSMC apoptosis, inflammation and MMP expression, formation of reactive oxygen species,33,34 leading to the degradation of the ECM, elastin, and the media layer, decreasing wall tension and vascular integrity.35 VSMC phenotypic switching is observed in AA36,37 and loss of function mutations in many genes associated with the differentiated contractile phenotype (MYH11, ACTA2, MYLK, PRKG1, and TGF-β signaling) have been implicated in human TAA.38 Mechanical forces and contraction reinforce the differentiated contractile phenotype in healthy vessels, and loss of function of mechanotransduction genes can contribute to aneurysm.39 Deletion of Tagln in mice exacerbates abdominal AA by promoting reactive oxygen species.34 Human mutations in contractile genes ACTA2 and MYH11 associated with TAAD were linked with medial VSMC hyperplasia.40,41 TSC2 mutations leading to mechanistic target of rapamycin (mTOR) hyperactivation similarly promote hyperplasia in human TAAD42 and mouse models.43,44 Although proliferation had been assumed to be protective in degenerative aortic disease, elegant work revealed that mTOR hyperactivation leads to proliferation of phenotypically modulated Lgals3-expressing VSMC that have a degradative lysosome-rich phenotype and weaken the vessel wall. The ability of rapamycin to rescue this phenotype suggests a potential avenue for TAAD therapy.43 Clonal expansion was also noted in VSMC in AA with phenotypic switching toward phagocytic-like phenotypes, with upregulation of autophagy and endoplasmic reticulum stress responses identified as protective responses in mice and humans.37 SM-specific knockout of the TGF-β receptor in a hyperlipidemic mouse results in severe AA, in which VSMC assume a mesenchymal stem cell-like intermediate state before transdifferentiating to a diverse repertoire of phenotypes, including osteoblasts, chondrocytes, adipocytes, and macrophage-like cells.45 Noncoding RNA regulation of aneurysm is extensively reviewed elsewhere in AA,46 with many of these RNAs targeting the VSMC phenotype. Understanding how VSMC phenotypic switching is initiated and perturbed during AA progression leading to vascular compromise may lead to new preventative and therapeutic strategies for AA.
Pulmonary arterial hypertension
PH is a devastating disease, defined by a pulmonary arterial pressure of greater than 20 mm Hg.47 A key pathologic feature is muscularization of normally nonmuscular distal pulmonary arterioles, which contributes to elevated pulmonary arterial resistance and eventually right heart failure.48 Although several genetic variants associate with PH,49 there are limited effective therapies because of inadequate understanding of the underlying mechanisms. Studies with mouse models of hypoxia-induced PH have shed light on this pathogenesis. During the early onset of PH, pathologic VSMCs dedifferentiate by downregulating MYH11 and upregulating PDGFR-β. These cells clonally expand, migrate distally, and then redifferentiate.50 PDGFR-β+ progenitor VSMCs also upregulate KLF4 in a PDGF-dependent manner, and depleting Klf4 in VSMCs or Pdgfb in ECs or macrophages mitigates hypoxia-induced PH.51, 52, 53 Elucidating the gene expression profiles of specialized progenitor VSMCs may provide valuable insights into pathways that can be targeted to attenuate PH and likely other vasculoproliferative diseases.
Current agents targeting VSMC in intimal hyperplasia
Catheter-based interventions such as balloon angioplasty revolutionized the revascularization of atherosclerotic vessels, but were complicated by high rates of restenosis. Stents, or metallic mesh scaffolds, improved outcomes, but were still subject to in-stent restenosis.54 Coating these stents with biopolymers to elute antiproliferative drugs represented a significant advance and remains the state of the art. In this section, we review the mechanisms by which current DES agents target VSMC and intimal hyperplasia, current limitations in the field, and pathways for new VSMC-focused drug development.
Rapamycin-eluting stents
Rapamycin, also known as sirolimus, is a naturally occurring macrolide that inhibits VSMC proliferation and migration and prevents intimal hyperplasia.55 Sirolimus and its analogs (“Rapalogs”; eg, everolimus and zotarolimus) on DES are effective in preventing in-stent restenosis in coronary artery revascularization.56 Rapamycin analogs are the preferred choice compared with paclitaxel DES (see Paclitaxel-eluting stents) for the treatment of coronary restenosis, in nondiabetic and diabetic patients.56,57
Rapamycin inhibits mTOR complex 1 (mTORC1), the central cellular growth regulator that senses nutrient sufficiency and coordinately controls the balance between anabolic and catabolic processes. Nutrient deficiency inhibits mTORC1 kinase activity to suppress growth and promote autophagy.58 The mTORC1 pathway regulates protein synthesis and controls growth by regulating biosynthesis of nucleotides, lipids, and ribosomes,58 as well as proliferation and migration. Rapamycin inhibits intimal hyperplasia by inhibiting migration and proliferation of VSMCs (Fig 2), inducing p27kip and p21cip (cyclin-dependent kinase inhibitors)59 and G1-S cell cycle arrest.60
Fig 2.
Mechanisms of action of paclitaxel and rapamycin in vascular smooth muscle cells (VSMC). A, Paclitaxel stabilizes microtubules, inducing cytostatic G1 cell cycle arrest and inhibiting VSMC and migration. B, Rapamycin binds to FKBP12 and inhibits mechanistic target of rapamycin complex 1 (mTORC1), inhibiting phosphorylation of S6 kinase and 4E-BP1, regulating protein, and extracellular matrix (ECM) synthesis. The inhibition of mTORC1 relieves negative feedback inhibition of IRS1, resulting in an activation of the PI3K/AKT2 pathway and AKT2-mediated prosurvival and transcriptional signaling (GATA6, FOXOs), which influences contractile and cell cycle gene expression. Rapamycin also induces TET methylcytosine dioxygenase 2 (TET2), promoting DNA and histone modifications, opening chromatin at key contractile gene promoters, but repressing chromatin at synthetic genes.
Initial DES agents focused solely on antiproliferative mechanisms. Rapamycin is an attractive DES agent because it also combats excessive ECM synthesis and promotes VSMC differentiation.59 This differentiation requires Akt2 signaling61 to the transcription factors GATA-662 and FoxO4, a repressor of myocardin.63 This Akt activation is also antiapoptotic (cytostatic rather than a cytotoxic),64 and improves insulin sensitivity.64 Akt2 is required for the rapamycin antihyperplastic response63 (Fig 2). mTORC1 inhibition by other agents, including lovastatin,65 adiponectin,66 and resveratrol,67 also promotes VSMC differentiation. TET2 is a master epigenetic regulator of VSMC differentiation and is induced by rapamycin.15 The pleiotropic effects on VSMC phenotype likely underlie the efficacy of rapalogs in DES.
Paclitaxel-eluting stents
Paclitaxel (Taxol) is a plant-derived potent chemotherapeutic that stabilizes microtubule assembly by binding β-tubulin dimers, preventing their depolymerization,68 which interferes with cell division, motility, and morphology. The low doses of paclitaxel in DES induce a cytostatic G1 cell cycle arrest, inhibiting proliferation and migration without inducing apoptosis69 (Fig 2). As with rapamycin analogs, local stent-mediated paclitaxel delivery helps to limit systemic toxicity. Clinical trials support the efficacy of paclitaxel DES in preventing in-stent restenosis.70
Limitations of current therapies and need for better therapeutics
Although the rapamycin- and paclitaxel-eluting stents have improved outcomes compared with bare metal stents or angioplasty alone, challenges remain, including efficacy in diabetic patients and in peripheral vascular lesions. The decreased efficacy of rapamycin DES in patients with diabetes is likely explained by diminished rapamycin-induced Akt2 signaling61, 62, 63 owing to insulin resistance: Akt2 is the key insulin-stimulated isoform that regulates glucose homeostasis, and insulin signaling to Akt2 is attenuated in type 2 diabetes.71 Although everolimus-eluting stents demonstrated advantages over paclitaxel-eluting stents in patients with diabetes in coronary artery revascularization,57 better therapies for this large cohort of patients are needed.
DES have revolutionized coronary artery revascularization, but endovascular treatment of peripheral vascular disease has proven more vexing. Despite improved patency with stenting vs balloon alone, concerns regarding stent fracture72 and restenosis in the superficial femoral artery have limited the broad application of stents to the femoropopliteal segment.73 There has been controversy regarding safety of paclitaxel-eluting stents and balloons in peripheral vascular disease, but recent analyses suggest that these devices are safe and effective in femoropopliteal lesions.74 Bioabsorbable stents, despite higher thrombosis rates compared with DES in the coronary arteries,75 are gaining favor in the periphery76 and may represent a new platform for anti-restenotic drug delivery.
Potential new avenues for therapeutic modulation of SMC phenotype in intimal hyperplasia
In addition to unmet needs in percutaneous coronary intervention (PCI), agents that are ideal for local delivery are generally not suitable systemic therapies for more diffuse vascular diseases involving VSMC phenotypic switching, such as atherosclerosis and transplant vasculopathy, owing to the potential for adverse effects. In the remainder of this review, we highlight recent and ongoing studies of the basic mechanisms that govern VSMC injury response and phenotype modulation. These findings may suggest novel avenues to be explored for potential therapeutic intervention.
Epigenetic regulators
Gene expression is heavily influenced by epigenetic regulation, which refers to heritable changes that do not alter the DNA sequence but alter its expression. Modifications in DNA or histones alter the chromatin structure and accessibility. These include DNA methylation and post-translational modifications of histones (acetylation, methylation, phosphorylation, etc). These “chromatin marks” can be made in response to environmental exposures or signals. Epigenetic marks are made by “writer” proteins, removed by “erasers,” and interpreted by “reader” proteins. We discuss recent advances in each of these areas relevant to VSMC phenotype and intimal hyperplasia (Fig 3).
Fig 3.
Agents targeting epigenetic pathways in intimal hyperplasia. A, DNA methyltransferases (DNMTs) methylated cyotsines, generating 5mC that contributes to gene silencing and compacted chromatin. TET enzymes convert 5mC to 5hmC, an activating mark. Histone deacetylases (HDACs) remove acetyl groups from histones, promoting inactive chromatin and gene repression. Transcription factors associated with active (SRF, myocardin) and repressed (KLF4) contractile genes are shown. Drugs that regulate protein function are indicated italic text. B, Bromodomain proteins bind acetylated histones and coordinate with transcription factors to promote gene expression. Bromodomain inhibitors attenuate neointimal hyperplasia by inhibiting BRD4 effects on proliferation genes. Mithramycin A blocks vascular smooth muscle cell (VSMC) proliferation by inhibiting Yes-associated protein (YAP) transcriptional regulation of proproliferative genes. TET2, TET methylcytosine dioxygenase 2.
Modulation of DNA methylation
DNA methylation can repress gene expression. Hypermethylation-mediated repression of tumor suppressor genes is common in cancers and can be clinically targeted by DNMT inhibitors.16 The DNMT inhibitor 5-aza-2'-deoxycytidine attenuates atherosclerosis and neointima formation in mouse models.16 This study also determined that TET2 is a key gene repressed by DNMT-1 in VSMCs, implicating opposing programs of DNA methylation as central in regulating phenotypic switching.16 TET enzymes promote DNA cytosine hydroxymethylation and subsequent demethylation (direct writer and indirect eraser functions), which can activate genes that were previously repressed.77 TET2 is a master epigenetic regulator of VSMC differentiation that is induced by rapamycin and repressed by PDGF-BB and in vascular injury and atherosclerosis.15 Local TET2 knockdown exacerbates intimal hyperplasia, whereas TET2 overexpression rescues this effect. TET2 promotes chromatin remodeling, including histone modifications, to influence the coordinated programs of gene expression. TET2 exerts potent effects by regulating master VSMC transcription factors, including SRF, myocardin, and KLF4.15
Antioxidants have many beneficial functions by limiting oxidative stress, but ascorbic acid (vitamin C) notably also enhances the activity of TET enzymes78, 79, 80 and was reported to induce SM contractile proteins.81 In the setting of cancer, where dysregulated TET2 can contribute to oncogenesis, promoting TET activity with vitamin C induces cancer cell cytotoxicity and slows tumor growth.82 Several clinical studies have assessed whether antioxidant therapy can limit restenosis,83, 84, 85 reporting that oral vitamin C decreased the incidence of restenosis after angioplasty83 and vitamin C, in combination with vitamin E, decreased coronary allograft vasculopathy.86 Intravenous vitamin C also decreased restenosis after angioplasty for dialysis access.84 Another trial found no benefit of vitamin C after PCI, but this discrepancy could be due to the confounding effects of coadministered compounds.85 Improved delivery, such as intravenously or via a stent, could potentially improve outcomes; cancer trials have revealed the importance of pharmacokinetics, with far greater plasma vitamin C concentrations achievable with intravenous vs oral administration.82 A direct comparison in vitro showed that DES drugs inhibit both EC and VSMC proliferation, whereas vitamin C inhibited only SMC,87 which could help to limit thrombosis in the PCI setting. The pleiotropic beneficial effects of vitamin C on VSMC phenotype, low-density lipoprotein oxidation, and immune cell activity77 make this inexpensive molecule of great interest as a preventative therapy.
Histone deacetylase inhibitors
Histone modification influences chromatin structure, with histone acetylation opening chromatin to allow transcription factor access to DNA, facilitating gene expression.88 Histone deacetylases (HDACs) remove acetyl groups from lysine residues (eraser function) and typically repress gene expression, while HDAC inhibitors (HDACIs) promote gene activation.88 Enhanced HDAC activity is common in cancer and promotes proliferation, with several HDACIs approved for cancer treatment.89 In VSMCs, HDACs1-3 are transcriptionally induced by mitogens and HDACIs attenuate proliferation and migration, inducing G1 arrest, regulating cell cycle genes including Rb, cyclin D1, p21, and p27.90 Intraperitoneal administration of the pan HDACI Scriptaid decreased neointimal hyperplasia after injury in mice.90
HDACs can also regulate nonhistone proteins, including myocardin/MRTF, SRF, and KLF4. HDAC4 and HDAC5 can bind to myocardin and suppress VSMC contractile gene expression, which is rescued by the pan HDACI, trichostatin A.91 The selective HDAC6 inhibitor tubastatin A revealed that HDAC6 is required for PDGF-BB repression of contractile genes. HDAC6 associates with and inhibits MRTF-A nuclear translocation and cooperative function with SRF.92 Notably, perivascular delivery of tubastatin A decreased intimal hyperplasia in rats.93 Histone deacetylation contributes to the repressive effects of KLF4 on contractile gene transcription in vitro and after injury; PDGF-BB stimulation increases KLF4 binding to HDACs, and KLF4 recruits HDAC activity to contractile gene promoters, inhibiting SRF binding.94,95 PDGF-BB also increased HDAC4 expression and activity in VSMCs, with HDAC4 knockdown inhibiting proliferation and migration.96 Targeting HDAC4 with the class IIa HDACI MC1568 decreased neointimal hyperplasia after murine carotid ligation.96
HDAC inhibition prevents SMC de-differentiation and decreases restenosis by 50% in rodent models.90,93,96 Although this response is less dramatic than that of rapamycin or paclitaxel, further optimization of delivery may enhance efficacy. HDAC inhibition may be an attractive strategy; preclinical studies also suggest benefits in atherosclerosis97 and ischemia/reperfusion injury.98 HDACIs have not yet been tested in human cardiovascular disease, but further elucidation of their mechanisms of action and isoform specificity may facilitate this use.
Bromodomain inhibitors
The Bromodomain and extra terminal containing protein (BET proteins), which include BRD2, BRD3, and BRD4, are epigenetic reader proteins that bind to specific acetylated lysines and act as scaffolding proteins for transcription factors and cofactors to promote transcription.99 BRD2, BRD3, and BRD4 localize at enhancer regions, facilitating transcription factor recruitment.99 Additionally, BET family proteins may also exhibit histone acetyltransferase activity and can regulate transcription by acetylating H3K122.100
BRD4 is induced in neointima in human artery and vein grafts, and after angioplasty in rodents, whereas the BET bromodomain inhibitor JQ1 abrogates VSMC proliferation and migration.101 Local BRD4 knockdown or JQ1-releasing perivascular hydrogel mitigated intimal hyperplasia in rats after angioplasty.101 The intravenous administration of JQ1 significantly decreased intimal hyperplasia without adversely affecting re-endothelization, suggesting that BET inhibition may be advantageous in avoiding DES-associated prothrombotic events.102 Systemic JQ1 treatment also attenuated the effects of AngII on hypertension, medial thickening, and inflammation and identified BRD4 binding to VSMC super-enhancers that mediate AngII-induced gene expression.103 Small molecule BET inhibitors are in early preclinical development or phase II clinical trials for cancer and cardiovascular disease.99 JQ1 inhibits BET protein binding to acetylated histones104 and disrupts BET-mediated transcription of key oncogenes.105 Two other synthetic inhibitors, I-BET762 and I-BET151, have enhanced pharmacokinetics in vivo.106 RVX-208 (apabetalone), a BD2-selective quinazoline, initially identified during screening for ApoA1 expression inducers,107 increased high-density lipoprotein cholesterol levels and cholesterol efflux in primates108 and inhibited atherosclerosis in mice.109 This compound showed promising results in phase II trials, with decreased atheroma volume and inflammatory markers in patients with coronary artery disease.110,111 A multicenter phase III trial (BETonMACE) found no significant difference in apabetalone vs placebo on major adverse cardiovascular events in high-risk patients with coronary artery disease, but noted trends toward decreases in cardiovascular death and myocardial infarction.112 The US Food and Drug Administration recently granted apabetalone a Breakthrough Therapy Designation, a status for expediting drugs with preliminary clinical evidence indicating potential substantial improvement over available therapy.113
Transcriptional regulators
Hippo pathway
Organ size is controlled by both cell size, regulated by the mTOR pathway, and cell number, regulated by the Hippo pathway. The Hippo pathway, composed of multiple kinases and their downstream transcription factors, integrates inputs from upstream stimuli including cell density, mechanical forces, cellular stress, and G-protein coupled receptors (GPCR) signaling to control cell survival/apoptosis and proliferation.114 The activation of the Hippo pathway promotes phosphorylation of the transcriptional coregulator Yes-associated protein (YAP) (and its paralog, TAZ), leading to their degradation (Fig 4). YAP binds and cooperates with TEAD (transcription enhancer activation domain) family transcription factors and is an oncoprotein that regulates cell cycle genes.114 YAP is required for normal arterial development,115 but is repressed in adult contractile VSMC by miR15B/16.116 VSMC YAP is upregulated after angioplasty in rats117 and SM-specific YAP deletion attenuates injury-induced SMC proliferation and migration.117,118 Deletion of miR15B/16 significantly increases YAP expression and intimal hyperplasia after angioplasty.116 TEAD1 is also induced after vascular injury, and SMC-specific TEAD1 deletion inhibits intimal hyperplasia in mice, consistent with prior studies where YAP promotes the synthetic phenotype.118 TEAD1 promotes the activation of the transporter SLC1A5 and subsequent glutamine-dependent mTORC1 activation.118 This finding provided a new link between the Hippo and mTORC1 pathways that amplify each other to coordinately control cell growth and proliferation (reviewed in119). In addition to direct regulation of proliferation genes, Hippo signaling likely influences VSMC phenotype through this coordinate regulation of mTORC1.
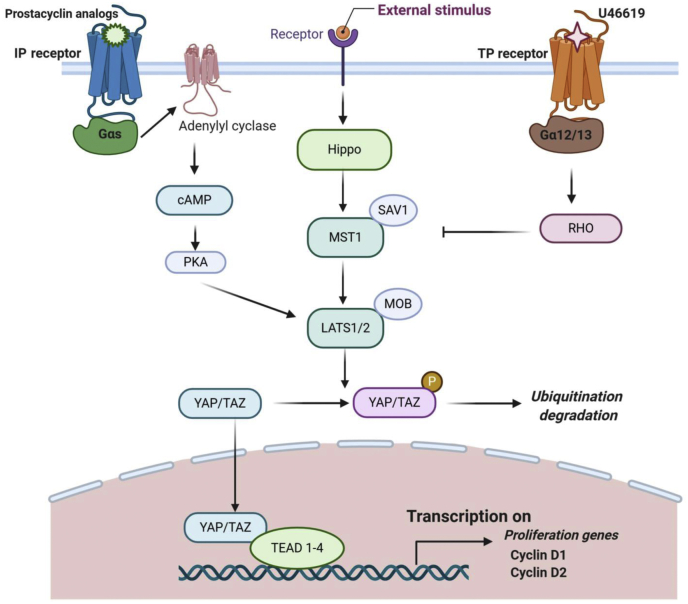
Fig 4.
The Hippo pathway. Activation of Hippo signaling by as yet unindentified receptors initiates a kinase cascade with sequential phosphorylation of MST1/2 and LATS1/2, culminating in phosphorylation of the Yes-associated protein (YAP) (or homologous TAZ) protein, which inducing its degradation. When the Hippo pathway is inactive, YAP or TAZ translocates into the nucleus, forms a complex with transcription enhancer activation domains (TEADs) and drives expression of proliferative genes. IP receptor activation by prostacyclin analogs and subsequent cyclic adenosine monophosphate (cAMP) signalling activates protein kinase A (PKA) phosphorylation and inhibition of YAP/TAZ. In contrast, TP receptor activation by U46619 activates Rho which inhibits MST1/2 and LATS1/2 kinases, preventing YAP/TAZ phosphorylation.
GPCR signaling that influences VSMC phenotype and intimal hyperplasia has also been linked to the Hippo pathway. Prostacyclin and thromboxane signal through GPCR (IP and TP) to mediate vasorelaxation and vasoconstriction, respectively.120 Prostacyclin promotes VSMC differentiation via cyclic adenosine monophosphate/protein kinase A.121 Notably, prostacyclin analogs or cyclic adenosine monophosphate also increase YAP/TAZ phosphorylation and degradation and inhibit TEAD-dependent proliferation and migration.122 Conversely, TP signaling is upregulated in vascular injury and promotes proliferation and migration.123 TP receptor blockade with sulotroban protected against late myocardial infarction after angioplasty, but did not significantly decrease restenosis in a clinical trial.123 In VSMCs, the TP agonist U46619 activated YAP/TAZ, whereas the inhibition of TP signaling attenuated YAP/TAZ activation and VSMC proliferation and migration after injury.124 It is likely that other GPCRs may also influence Hippo/YAP signaling in VSMC.
The Sp-1 transcription factor is induced by PDGF and in rat arterial injury and correlates with VSMC dedifferentiation.125 Sp-1 enhanced intimal hyperplasia by promoting YAP transcription. Furthermore, a stent eluting the Sp-1 inhibitor mithramycin A inhibited YAP and attenuated in-stent restenosis in rabbit angioplasty.125 The Sp1-and GPCR-based effects are examples of indirect regulation of YAP/TAZ, whose structure has been challenging to target with small molecules. More than 50 agents that indirectly target YAP/TAZ, through upstream regulators or effectors, have been identified and are of interest as potential cancer therapies.126 The increasing body of literature implicating the Hippo/YAP pathway in VSMC phenotype and intimal hyperplasia suggests that these agents may also be attractive candidates for novel therapeutic approaches.
The adiponectin/peroxisome proliferator-activity receptor-gamma axis
The transcription factor peroxisome proliferator-activity receptor-gamma (PPAR-γ) is a master regulator of fatty acid storage and glucose metabolism and adipose tissue development. Thiazolidinedione (TZD) drugs are agonists for PPAR-γ used to promote insulin sensitization in diabetic patients that also have beneficial effects on VSMC phenotype. Understanding these mechanisms is critical because diabetic patients face more virulent atherosclerosis and increased restenosis, with exogenous insulin increasing the risk of restenosis after endovascular intervention.127, 128, 129 TZDs modulate atherosclerosis development130,131 and may protect against in-stent restenosis in diabetic patients.130,132 TZDs exert antiproliferative, antiplatelet, and anti-inflammatory effects and promote VSMC differentiation (Fig 5). PPAR-γ agonists decrease intimal hyperplasia after PCI,133,134 and vascular PPAR-γ expression was strongly repressed after arterial stenting in minipigs. Systemic rosiglitazone treatment rescued both PPAR-γ and contractile protein expression after stenting and decreased inflammation.135 Rosiglitazone prevented VSMC dedifferentiation by reversing the PDGF-induced repression of PKG.136 Impaired PPAR-γ expression also contributes to VSMC phenotypic modulation in hypertension.137 PPAR-γ overexpression rescued dedifferentiation in VSMCs derived from spontaneously hypertensive rats, and rosiglitazone treatment prevented pathologic vascular remodeling in spontaneously hypertensive rats.137
Fig 5.
The adiponectin/peroxisome proliferator-activity receptor (PPAR)-γ pathway in vascular smooth muscle cells (VSMCs), thiazolidinediones (TZDs), synthetic ligands of PPAR-γ including roziglitazone, induce adiponectin expression. Secreated adiponectin binds AdipoR1 on the cell surface and inhibits mechanistic target of rapamycin complex 1 (mTORC1) through AMPKα2. This results in AKT2 activation and increased contractile gene expression. AMPKα2-mediated mTORC1 inhibition can increase insulin sensitivity. PPAR-γ also opposes VSMC phenotypic modulation by promoting PKG transcription and opposing prohypertensive actions of angiotensin II (AngII).
Although it is well-known that the metabolic syndrome contributes to cardiovascular risk, the molecular mechanisms that link diabetes, obesity, and vascular disease are incompletely understood. The status of energy stores in adipose depots is conveyed throughout the body by adipokines, adipose-derived circulating hormones. Adiponectin is an insulin-sensitizing adipokine secreted in inverse proportion to fat mass that protects against diabetes and atherosclerosis.138 Notably, TZDs induce adiponectin.139,140 In addition to direct transcriptional targets of PPAR-γ in VSMCs, this induction of adiponectin may also contribute to its beneficial effects in vivo. Adiponectin induces VSMC differentiation via AMPKα2-mediated mTORC1 inhibition66 (Fig 5). Similar to rapamycin, this promoted feedback activation of AKT2.66 Although adiponectin is primarily adipocyte derived, VSMCs can also secrete adiponectin, which may play a paracrine role in maintaining VSMC differentiation.141 Adiponectin also inhibits growth factor- and oxidized low-density lipoprotein-stimulated VSMC proliferation and migration.142,143 Notably, an orally administered adiponectin receptor agonist decreased intimal hyperplasia in mice and inhibited PDGF-induced VSMC proliferation.144 In models of restenosis and atherosclerosis, recombinant adiponectin decreased inflammation, oxidative stress, and apoptosis.145,146 Interestingly, statin therapy correlates with increased adiponectin, which could potentially explain statin cardiovascular benefits besides lipid lowering.147 Although adiponectin itself, which functions as a large protein multimer, is not a practical therapeutic target, synthetic adiponectin receptor agonists, downstream effectors, or agents that induce adiponectin expression may be a desirable target for DES and other cardiovascular therapies.
Notch pathway
The highly conserved Notch signaling pathway regulates many physiological processes, including cardiovascular development, through cell-cell interactions. Transmembrane ligands (including Jagged 1 and 2, and Delta-like ligand 1, 3, and 4) bind to a Notch family receptor (NOTCH1-4) on a neighboring cell, promoting transcriptional regulation by the Notch intracellular domain.148 The role of the Notch pathway in VSMC phenotypic modulation remains unclear; conflicting data have been reported. These discrepancies likely reflect divergent and context-dependent roles for Notch family members, but the data in aggregate point to a prodifferentiation function (see extensive review in148). Recent studies indicate opposing roles for Notch 2 and Notch 3 on PDGF-B-dependent VSMC proliferation. Notch 3, but not Notch 2, promotes VSMC survival and proliferation.149 Consistent with these roles, Notch3-null mice display reduced VSMCs in small-caliber vessels and are protected from hypoxia-induced pulmonary arterial hypertension, whereas elevated Notch3 levels in human pulmonary arterial hypertension predict disease severity.150,151 Notch family members are regulated after vascular injury, and the viral delivery of soluble Jagged 1 inhibits intimal hyperplasia after balloon angioplasty in rats,152 suggesting a potential therapeutic strategy.
Integrins
Integrin β3 and SMC expansion
Integrins are heterodimeric transmembrane glycoproteins formed by α and β subunits that regulate cell-cell and cell-matrix interactions.153 In VSMCs, integrin β3 associates with αv subunits and influences migration, survival, proliferation, and adhesion during vascular remodeling.154,155 Integrin β3 is highly upregulated in response to stimuli, such as mechanical injury, neointimal hyperplasia, disruption of elastic lamina, hyperglycemia, and hypercholesteremia,156, 157, 158 events that are associated with VSMC phenotypic switching and matrix remodeling.159 Integrin β3 binds to several ligands via an RGD (Arg-Gly-Asp) binding motif.160 The local administration of a synthetic RGD peptide, which effectively blocks β3 function, significantly attenuates lesion area and neointimal hyperplasia during restenosis following angioplasty or stent injury,161, 162, 163, 164 and Itgb3(–/–) mice are protected against neointimal lesion formation after carotid ligation with decreased SMC migration into the neointima.165 Bone marrow transplant experiments suggested that β3 from vascular cells was critical in neointimal formation. Itgb3(–/–) mice were also protected from hyperglycemia-induced restenosis, suggesting an advantage from β3 antagonism during vascular injury and diabetes.158 The inhibition of β3 also provided beneficial effects in supravalvular aortic stenosis,157 a pediatric arterial obstructive disorder of VSMC hyperproliferation owing to heterozygous loss-of-function mutations in the elastin gene.166 Excessive pathologic dedifferentiated VSMCs in elastin mutant arteries display enhanced β3 levels.157 Genetic deletion of β3 mitigated VSMC proliferation and stenosis and extended survival in a murine supravalvular aortic stenosis model. Importantly, treatment with a β3 inhibitor attenuated hypermuscularization and stenosis during elastin deficiency.
In contrast, Itgb3(–/–) mice display enhanced atherosclerosis in atheroprone backgrounds, likely owing to higher recruitment of SMCs into the plaque.26,167 Recent studies demonstrate that VSMC clonality in atherosclerotic plaques is mediated by β3.32 During early onset of plaque formation, medial VSMCs first migrate outward to form a highly proliferative and β3-rich cap and then dive into and populate the plaque core where they downregulate β3 levels and contractile markers. Deletion of β3 in bone marrow-derived cells enhances VSMC recruitment into the plaques with polyclonal expansion and increased transdifferentiation. These studies reveal a previously unknown role of β3 in regulating VSMC clonal expansion in atherosclerosis. Cell-specific Itgb3 knockout models will help to further dissect the role of β3 in VSMCs in regulating VSMC fate and expansion.
Taken together, genetic and pharmacologic studies highlight a critical role for β3 in regulating aberrant and excessive accumulation of VSMCs (Fig 6). Interestingly, abciximab (ReoPro), a β3-directed monoclonal Fab fragment, decreased intimal hyperplasia in restenosis models.168 Abciximab became the first US Food and Drug Administration-approved glycoprotein inhibitor for patients with acute coronary syndrome. Four human clinical trials noted contrasting effects of β3 antagonism on restenosis.168 This finding is likely from the dual targeting of β3 on both vascular and bone marrow-derived cells, each of which can impact the pathologic outcome differently (as seen with genetic models of bone marrow transplant). Thus, abciximab is an option for treating pathologies characterized by VSMC hyperproliferation with minimal bone marrow contribution such as arteriovenous fistula.168,169 Therapeutic strategies that could target β3 specifically in VSMCs may improve clinical restenosis outcomes.
Fig 6.
Integrin inhibition attenuates intimal hyperplasia. Schematic depiction of intimal hyperplasia after vascular injury, and strategies for β3-integrin inhibition that attenuate intimal hyperplasia. SMC, Smooth muscle cell; VSMC, vascular smooth muscle cell.
Conclusions and future perspectives
The therapeutic targeting of VSMC phenotypic modulation is critical to combat the massive burden of cardiovascular diseases on human health. Although several approaches have been used to prevent or attenuate VSMC phenotypic switching, they have limitations. DES are widely used for local drug delivery to prevent coronary artery restenosis after PCI, minimizing systemic side effects, but this approach has not translated as effectively in the peripheral vasculature. Furthermore, other approaches are required to target diffuse vascular pathologies such as atherosclerosis, calcification, stiffening, hypertension, and transplant vasculopathy. Plasmid or adenoviral-mediated gene therapy170 has demonstrated efficacy targeting MCP-1,171 MMP inhibitors,172 or endothelial nitric oxide synthase173 in models ranging from rodents to primates, but has not advanced to the clinic owing to practical limitations and concerns over viral safety.
Small molecule inhibitors efficiently target the minor segment of the proteome with well-defined binding pockets (eg, ion channels, GPCRs, nuclear receptors, and enzymes). However, targeting proteins that lack discrete binding pockets such as transcription factors, epigenetic regulators, and scaffolding proteins remains technically challenging.174 Proteolysis targeting chimera (PROTAC) technology is an emerging method to target undruggable proteins by exploiting the ubiquitin-mediated proteasome degradation pathway to selectively degrade target proteins in preclinical cancer research.175 Notably, epigenetic proteins have been successfully targeted by PROTAC.176 It will be of interest to determine whether PROTAC could be used to target VSMC epigenetic and transcriptional regulators in cardiovascular disease.
The phenotypic plasticity of VSMCs makes allows for extensive regenerative capacity. Recent advances in genetic and -omic approaches have provided valuable tools to carry out detailed and precise analyses of VSMC dynamics in health and disease. Understanding the regional and spatiotemporal regulation of VSMC fate, clonality, differentiation, and phenotypic modulation will help to uncover fundamental mechanistic insights essential to discovering novel therapeutic candidates. New technologies such as PROTAC, CRISPR-Cas9-mediated genome editing, and miRNA targeting may help to overcome current therapeutic limitations and test promising targets in VSMCs. Continued rigorous efforts on multiple fronts will help to translate these targets into viable cardiovascular therapies.
Author contributions
Conception and design: RC, PC, JD, AO, DG, ER, KM
Analysis and interpretation: Not applicable
Data collection: Not applicable
Writing the article: RC, PC, JD, AO, DG, ER, KM
Critical revision of the article: RC, PC, JD, AO, DG, ER, KM
Final approval of the article: RC, PC, JD, AO, DG, ER, KM
Statistical analysis: Not applicable
Obtained funding: DG, KM
Overall responsibility: KM
Footnotes
Supported by grants from the NIH (R35HL150766, R01HL133016, R01HL142674and R21NS088854 to D.M.G.), and AHA (Established Investigator Award, 19EIA34660321 to D.M.G.), and from the NIH (R0HL151222, R01HL142090, and R01 H146101) to K.A.M.
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS-Vascular Science policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Maguire E.M., Xiao Q. Noncoding RNAs in vascular smooth muscle cell function and neointimal hyperplasia. FEBS J. 2020;287:5260–5283. doi: 10.1111/febs.15357. [DOI] [PubMed] [Google Scholar]
- 2.Owens G.K., Kumar M.S., Wamhoff B.R. Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol Rev. 2004;84:767–801. doi: 10.1152/physrev.00041.2003. [DOI] [PubMed] [Google Scholar]
- 3.Gordon D., Reidy M.A., Benditt E.P., Schwartz S.M. Cell proliferation in human coronary arteries. Proc Natl Acad Sci U S A. 1990;87:4600–4604. doi: 10.1073/pnas.87.12.4600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nanda V., Miano J.M. Leiomodin 1, a new serum response factor-dependent target gene expressed preferentially in differentiated smooth muscle cells. J Biol Chem. 2012;287:2459–2467. doi: 10.1074/jbc.M111.302224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Long X., Tharp D.L., Georger M.A., Slivano O.J., Lee M.Y., Wamhoff B.R. The smooth muscle cell-restricted KCNMB1 ion channel subunit is a direct transcriptional target of serum response factor and myocardin. J Biol Chem. 2009;284:33671–33682. doi: 10.1074/jbc.M109.050419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arevalo-Martinez M., Cidad P., Garcia-Mateo N., Moreno-Estar S., Serna J., Fernandez M. Myocardin-dependent Kv1.5 channel expression prevents phenotypic modulation of human vessels in organ culture. Arterioscler Thromb Vasc Biol. 2019;39:e273–e286. doi: 10.1161/ATVBAHA.119.313492. [DOI] [PubMed] [Google Scholar]
- 7.Sward K., Krawczyk K.K., Moren B., Zhu B., Matic L., Holmberg J. Identification of the intermediate filament protein synemin/SYNM as a target of myocardin family coactivators. Am J Physiol Cell Physiol. 2019;317:C1128–C1142. doi: 10.1152/ajpcell.00047.2019. [DOI] [PubMed] [Google Scholar]
- 8.Wirka R.C., Wagh D., Paik D.T., Pjanic M., Nguyen T., Miller C.L. Atheroprotective roles of smooth muscle cell phenotypic modulation and the TCF21 disease gene as revealed by single-cell analysis. Nat Med. 2019;25:1280–1289. doi: 10.1038/s41591-019-0512-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alencar G.F., Owsiany K.M., Karnewar S., Sukhavasi K., Mocci G., Nguyen A. Stem cell pluripotency genes Klf4 and Oct4 regulate complex SMC phenotypic changes critical in late-stage atherosclerotic lesion pathogenesis. Circulation. 2020;142:2045–2059. doi: 10.1161/CIRCULATIONAHA.120.046672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi N., Chen S.Y. Smooth muscle cell differentiation: model systems, regulatory mechanisms, and vascular diseases. J Cell Physiol. 2016;231:777–787. doi: 10.1002/jcp.25208. [DOI] [PubMed] [Google Scholar]
- 11.Shankman L.S., Gomez D., Cherepanova O.A., Salmon M., Alencar G.F., Haskins R.M. KLF4-dependent phenotypic modulation of smooth muscle cells has a key role in atherosclerotic plaque pathogenesis. Nat Med. 2015;21:628–637. doi: 10.1038/nm.3866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cherepanova O.A., Gomez D., Shankman L.S., Swiatlowska P., Williams J., Sarmento O.F. Activation of the pluripotency factor OCT4 in smooth muscle cells is atheroprotective. Nat Med. 2016;22:657–665. doi: 10.1038/nm.4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takahashi K., Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 14.Gomez D., Swiatlowska P., Owens G.K. Epigenetic control of smooth muscle cell identity and lineage memory. Arterioscler Thromb Vasc Biol. 2015;35:2508–2516. doi: 10.1161/ATVBAHA.115.305044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu R., Jin Y., Tang W.H., Qin L., Zhang X., Tellides G. Ten-eleven translocation-2 (TET2) is a master regulator of smooth muscle cell plasticity. Circulation. 2013;128:2047–2057. doi: 10.1161/CIRCULATIONAHA.113.002887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhuang J., Luan P., Li H., Wang K., Zhang P., Xu Y. The yin-yang dynamics of DNA methylation ss the key regulator for smooth muscle cell phenotype switch and vascular remodeling. Arterioscler Thromb Vasc Biol. 2017;37:84–97. doi: 10.1161/ATVBAHA.116.307923. [DOI] [PubMed] [Google Scholar]
- 17.Gomez D., Shankman L.S., Nguyen A.T., Owens G.K. Detection of histone modifications at specific gene loci in single cells in histological sections. Nat Methods. 2013;10:171–177. doi: 10.1038/nmeth.2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cordes K.R., Sheehy N.T., White M.P., Berry E.C., Morton S.U., Muth A.N. miR-145 and miR-143 regulate smooth muscle cell fate and plasticity. Nature. 2009;460:705–710. doi: 10.1038/nature08195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leeper N.J., Maegdefessel L. Non-coding RNAs: key regulators of smooth muscle cell fate in vascular disease. Cardiovasc Res. 2018;114:611–621. doi: 10.1093/cvr/cvx249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marx S.O., Totary-Jain H., Marks A.R. Vascular smooth muscle cell proliferation in restenosis. Circ Cardiovasc Interv. 2011;4:104–111. doi: 10.1161/CIRCINTERVENTIONS.110.957332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jawien A., Bowen-Pope D.F., Lindner V., Schwartz S.M., Clowes A.W. Platelet-derived growth factor promotes smooth muscle migration and intimal thickening in a rat model of balloon angioplasty. J Clin Invest. 1992;89:507–511. doi: 10.1172/JCI115613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Majesky M.W., Lindner V., Twardzik D.R., Schwartz S.M., Reidy M.A. Production of transforming growth factor beta 1 during repair of arterial injury. J Clin Invest. 1991;88:904–910. doi: 10.1172/JCI115393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Libby P., Ridker P.M., Hansson G.K. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317–325. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 24.Chappell J., Harman J.L., Narasimhan V.M., Yu H., Foote K., Simons B.D. Extensive proliferation of a subset of differentiated, yet plastic, medial vascular smooth muscle cells contributes to neointimal formation in mouse injury and atherosclerosis models. Circ Res. 2016;119:1313–1323. doi: 10.1161/CIRCRESAHA.116.309799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tabas I., Garcia-Cardena G., Owens G.K. Recent insights into the cellular biology of atherosclerosis. J Cell Biol. 2015;209:13–22. doi: 10.1083/jcb.201412052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Misra A., Feng Z., Chandran R.R., Kabir I., Rotllan N., Aryal B. Integrin beta3 regulates clonality and fate of smooth muscle-derived atherosclerotic plaque cells. Nat Commun. 2018;9:2073. doi: 10.1038/s41467-018-04447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barman S.A., Li X., Haigh S., Kondrikov D., Mahboubi K., Bordan Z. Galectin-3 is expressed in vascular smooth muscle cells and promotes pulmonary hypertension through changes in proliferation, apoptosis, and fibrosis. Am J Physiol Lung Cell Mol Physiol. 2019;316:L784–L797. doi: 10.1152/ajplung.00186.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bostrom K.I. Where do we stand on vascular calcification? Vascul Pharmacol. 2016;84:8–14. doi: 10.1016/j.vph.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steitz S.A., Speer M.Y., Curinga G., Yang H.Y., Haynes P., Aebersold R. Smooth muscle cell phenotypic transition associated with calcification: upregulation of Cbfa1 and downregulation of smooth muscle lineage markers. Circ Res. 2001;89:1147–1154. doi: 10.1161/hh2401.101070. [DOI] [PubMed] [Google Scholar]
- 30.Speer M.Y., Yang H.Y., Brabb T., Leaf E., Look A., Lin W.L. Smooth muscle cells give rise to osteochondrogenic precursors and chondrocytes in calcifying arteries. Circ Res. 2009;104:733–741. doi: 10.1161/CIRCRESAHA.108.183053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin M.E., Chen T.M., Wallingford M.C., Nguyen N.B., Yamada S., Sawangmake C. Runx2 deletion in smooth muscle cells inhibits vascular osteochondrogenesis and calcification but not atherosclerotic lesion formation. Cardiovasc Res. 2016;112:606–616. doi: 10.1093/cvr/cvw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shanahan C.M., Crouthamel M.H., Kapustin A., Giachelli C.M. Arterial calcification in chronic kidney disease: key roles for calcium and phosphate. Circ Res. 2011;109:697–711. doi: 10.1161/CIRCRESAHA.110.234914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peng H., Zhang K., Liu Z., Xu Q., You B., Li C. VPO1 modulates vascular smooth muscle cell phenotypic switch by activating extracellular signal-regulated kinase 1/2 (ERK 1/2) in abdominal aortic aneurysms. J Am Heart Assoc. 2018;7:e010069. doi: 10.1161/JAHA.118.010069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhong L., He X., Si X., Wang H., Li B., Hu Y. SM22alpha (Smooth Muscle 22alpha) prevents aortic aneurysm formation by inhibiting smooth muscle cell phenotypic switching through suppressing reactive oxygen species/NF-kappaB (Nuclear Factor-kappaB) Arterioscler Thromb Vasc Biol. 2019;39:e10–e25. doi: 10.1161/ATVBAHA.118.311917. [DOI] [PubMed] [Google Scholar]
- 35.Michel J.B., Jondeau G., Milewicz D.M. From genetics to response to injury: vascular smooth muscle cells in aneurysms and dissections of the ascending aorta. Cardiovasc Res. 2018;114:578–589. doi: 10.1093/cvr/cvy006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mao N., Gu T., Shi E., Zhang G., Yu L., Wang C. Phenotypic switching of vascular smooth muscle cells in animal model of rat thoracic aortic aneurysm. Interact Cardiovasc Thorac Surg. 2015;21:62–70. doi: 10.1093/icvts/ivv074. [DOI] [PubMed] [Google Scholar]
- 37.Clement M., Chappell J., Raffort J., Lareyre F., Vandestienne M., Taylor A.L. Vascular smooth muscle cell plasticity and autophagy in dissecting aortic aneurysms. Arterioscler Thromb Vasc Biol. 2019;39:1149–1159. doi: 10.1161/ATVBAHA.118.311727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Milewicz D.M., Ramirez F. Therapies for thoracic aortic aneurysms and acute aortic dissections. Arterioscler Thromb Vasc Biol. 2019;39:126–136. doi: 10.1161/ATVBAHA.118.310956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Humphrey J.D., Schwartz M.A., Tellides G., Milewicz D.M. Role of mechanotransduction in vascular biology: focus on thoracic aortic aneurysms and dissections. Circ Res. 2015;116:1448–1461. doi: 10.1161/CIRCRESAHA.114.304936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guo D.C., Pannu H., Tran-Fadulu V., Papke C.L., Yu R.K., Avidan N. Mutations in smooth muscle alpha-actin (ACTA2) lead to thoracic aortic aneurysms and dissections. Nat Genet. 2007;39:1488–1493. doi: 10.1038/ng.2007.6. [DOI] [PubMed] [Google Scholar]
- 41.Pannu H., Tran-Fadulu V., Papke C.L., Scherer S., Liu Y., Presley C. MYH11 mutations result in a distinct vascular pathology driven by insulin-like growth factor 1 and angiotensin II. Hum Mol Genet. 2007;16:2453–2462. doi: 10.1093/hmg/ddm201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cao J., Gong L., Guo D.C., Mietzsch U., Kuang S.Q., Kwartler C.S. Thoracic aortic disease in tuberous sclerosis complex: molecular pathogenesis and potential therapies in Tsc2+/- mice. Hum Mol Genet. 2010;19:1908–1920. doi: 10.1093/hmg/ddq066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li G., Wang M., Caulk A.W., Cilfone N.A., Gujja S., Qin L. Chronic mTOR activation induces a degradative smooth muscle cell phenotype. J Clin Invest. 2020;130:1233–1251. doi: 10.1172/JCI131048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shi X., Ma W., Pan Y., Li Y., Wang H., Pan S. MiR-126-5p promotes contractile switching of aortic smooth muscle cells by targeting VEPH1 and alleviates Ang II-induced abdominal aortic aneurysm in mice. Lab Invest. 2020;100:1564–1574. doi: 10.1038/s41374-020-0454-z. [DOI] [PubMed] [Google Scholar]
- 45.Chen P.Y., Qin L., Li G., Malagon-Lopez J., Wang Z., Bergaya S. Smooth muscle cell reprogramming in aortic aneurysms. Cell Stem Cell. 2020;26:542–557.e11. doi: 10.1016/j.stem.2020.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Spin J.M., Li D.Y., Maegdefessel L., Tsao P.S. Non-coding RNAs in aneurysmal aortopathy. Vascul Pharmacol. 2019;114:110–121. doi: 10.1016/j.vph.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 47.Simonneau G., Montani D., Celermajer D.S., Denton C.P., Gatzoulis M.A., Krowka M. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53:1801913. doi: 10.1183/13993003.01913-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Frid M.G., Brunetti J.A., Burke D.L., Carpenter T.C., Davie N.J., Reeves J.T. Hypoxia-induced pulmonary vascular remodeling requires recruitment of circulating mesenchymal precursors of a monocyte/macrophage lineage. Am J Pathol. 2006;168:659–669. doi: 10.2353/ajpath.2006.050599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Southgate L., Machado R.D., Graf S., Morrell N.W. Molecular genetic framework underlying pulmonary arterial hypertension. Nat Rev Cardiol. 2020;17:85–95. doi: 10.1038/s41569-019-0242-x. [DOI] [PubMed] [Google Scholar]
- 50.Sheikh A.Q., Lighthouse J.K., Greif D.M. Recapitulation of developing artery muscularization in pulmonary hypertension. Cell Rep. 2014;6:809–817. doi: 10.1016/j.celrep.2014.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sheikh A.Q., Misra A., Rosas I.O., Adams R.H., Greif D.M. Smooth muscle cell progenitors are primed to muscularize in pulmonary hypertension. Sci Transl Med. 2015;7:308ra159. doi: 10.1126/scitranslmed.aaa9712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sheikh A.Q., Saddouk F.Z., Ntokou A., Mazurek R., Greif D.M. Cell autonomous and non-cell autonomous regulation of SMC progenitors in pulmonary hypertension. Cell Rep. 2018;23:1152–1165. doi: 10.1016/j.celrep.2018.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ntokou A., Dave J.M., Kauffman A.C., Sauler M., Ryu C., Hwa J. Macrophage-derived PDGF-B induces muscularization in murine and human pulmonary hypertension. JCI Insight. 2021;6:e139067. doi: 10.1172/jci.insight.139067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Garg S., Bourantas C., Serruys P.W. New concepts in the design of drug-eluting coronary stents. Nat Rev Cardiol. 2013;10:248–260. doi: 10.1038/nrcardio.2013.13. [DOI] [PubMed] [Google Scholar]
- 55.Gallo R., Padurean A., Jayaraman T., Marx S., Roque M., Adelman S. Inhibition of intimal thickening after balloon angioplasty in porcine coronary arteries by targeting regulators of the cell cycle. Circulation. 1999;99:2164–2170. doi: 10.1161/01.cir.99.16.2164. [DOI] [PubMed] [Google Scholar]
- 56.Kalra A., Rehman H., Khera S., Thyagarajan B., Bhatt D.L., Kleiman N.S. New-generation coronary stents: current data and future directions. Curr Atheroscler Rep. 2017;19:14. doi: 10.1007/s11883-017-0654-1. [DOI] [PubMed] [Google Scholar]
- 57.Kaul U., Bangalore S., Seth A., Arambam P., Abhaichand R.K., Patel T.M. Paclitaxel-eluting versus everolimus-eluting coronary stents in diabetes. N Engl J Med. 2015;373:1709–1719. doi: 10.1056/NEJMoa1510188. [DOI] [PubMed] [Google Scholar]
- 58.Sabatini D.M. Twenty-five years of mTOR: uncovering the link from nutrients to growth. Proc Natl Acad Sci U S A. 2017;114:11818–11825. doi: 10.1073/pnas.1716173114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martin K.A., Rzucidlo E.M., Merenick B.L., Fingar D.C., Brown D.J., Wagner R.J. The mTOR/p70 S6K1 pathway regulates vascular smooth muscle cell differentiation. Am J Physiol Cell Physiol. 2004;286:C507–C517. doi: 10.1152/ajpcell.00201.2003. [DOI] [PubMed] [Google Scholar]
- 60.Marx S.O., Jayaraman T., Go L.O., Marks A.R. Rapamycin-FKBP inhibits cell cycle regulators of proliferation in vascular smooth muscle cells. Circ Res. 1995;76:412–417. doi: 10.1161/01.res.76.3.412. [DOI] [PubMed] [Google Scholar]
- 61.Martin K.A., Merenick B.L., Ding M., Fetalvero K.M., Rzucidlo E.M., Kozul C.D. Rapamycin promotes vascular smooth muscle cell differentiation through insulin receptor substrate-1/phosphatidylinositol 3-kinase/Akt2 feedback signaling. J Biol Chem. 2007;282:36112–36120. doi: 10.1074/jbc.M703914200. [DOI] [PubMed] [Google Scholar]
- 62.Xie Y., Jin Y., Merenick B.L., Ding M., Fetalvero K.M., Wagner R.J. Phosphorylation of GATA-6 is required for vascular smooth muscle cell differentiation after mTORC1 inhibition. Sci Signal. 2015;8:ra44. doi: 10.1126/scisignal.2005482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jin Y., Xie Y., Ostriker A.C., Zhang X., Liu R., Lee M.Y. Opposing actions of AKT (protein kinase B) isoforms in vascular smooth muscle injury and therapeutic response. Arterioscler Thromb Vasc Biol. 2017;37:2311–2321. doi: 10.1161/ATVBAHA.117.310053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Patterson C., Mapera S., Li H.H., Madamanchi N., Hilliard E., Lineberger R. Comparative effects of paclitaxel and rapamycin on smooth muscle migration and survival: role of AKT-dependent signaling. Arterioscler Thromb Vasc Biol. 2006;26:1473–1480. doi: 10.1161/01.ATV.0000223866.42883.3b. [DOI] [PubMed] [Google Scholar]
- 65.Wagner R.J., Martin K.A., Powell R.J., Rzucidlo E.M. Lovastatin induces VSMC differentiation through inhibition of Rheb and mTOR. Am J Physiol Cell Physiol. 2010;299:C119–C127. doi: 10.1152/ajpcell.00429.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ding M., Xie Y., Wagner R.J., Jin Y., Carrao A.C., Liu L.S. Adiponectin induces vascular smooth muscle cell differentiation via repression of mammalian target of rapamycin complex 1 and FoxO4. Arterioscler Thromb Vasc Biol. 2011;31:1403–1410. doi: 10.1161/ATVBAHA.110.216804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Thompson A.M., Martin K.A., Rzucidlo E.M. Resveratrol induces vascular smooth muscle cell differentiation through stimulation of SirT1 and AMPK. PLoS One. 2014;9:e85495. doi: 10.1371/journal.pone.0085495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Derry W.B., Wilson L., Jordan M.A. Substoichiometric binding of Taxol suppresses microtubule dynamics. Biochemistry. 1995;34:2203–2211. doi: 10.1021/bi00007a014. [DOI] [PubMed] [Google Scholar]
- 69.Axel D.I., Kunert W., Goggelmann C., Oberhoff M., Herdeg C., Kuttner A. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997;96:636–645. doi: 10.1161/01.cir.96.2.636. [DOI] [PubMed] [Google Scholar]
- 70.Stone G.W., Ellis S.G., Cox D.A., Hermiller J., O'Shaughnessy C., Mann J.T. One-year clinical results with the slow-release, polymer-based, paclitaxel-eluting TAXUS stent: the TAXUS-IV trial. Circulation. 2004;109:1942–1947. doi: 10.1161/01.CIR.0000127110.49192.72. [DOI] [PubMed] [Google Scholar]
- 71.Cho H., Mu J., Kim J.K., Thorvaldsen J.L., Chu Q., Crenshaw E.B., 3rd Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKB beta) Science. 2001;292:1728–1731. doi: 10.1126/science.292.5522.1728. [DOI] [PubMed] [Google Scholar]
- 72.Schlager O., Dick P., Sabeti S., Amighi J., Mlekusch W., Minar E. Long-segment SFA stenting--the dark sides: in-stent restenosis, clinical deterioration, and stent fractures. J Endovasc Ther. 2005;12:676–684. doi: 10.1583/05-1672.1. [DOI] [PubMed] [Google Scholar]
- 73.Garcia L.A., Rosenfield K.R., Metzger C.D., Zidar F., Pershad A., Popma J.J. SUPERB final 3-year outcomes using interwoven nitinol biomimetic supera stent. Catheter Cardiovasc Interv. 2017;89:1259–1267. doi: 10.1002/ccd.27058. [DOI] [PubMed] [Google Scholar]
- 74.Drachman D.E., Garasic J.M. Paclitaxel-coated devices: safety and efficacy are in the PVI of the beholder. J Am Heart Assoc. 2021;10:e020289. doi: 10.1161/JAHA.120.020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ali Z.A., Gao R., Kimura T., Onuma Y., Kereiakes D.J., Ellis S.G. Three-year outcomes with the absorb bioresorbable scaffold: individual-patient-data meta-analysis from the ABSORB randomized trials. Circulation. 2018;137:464–479. doi: 10.1161/CIRCULATIONAHA.117.031843. [DOI] [PubMed] [Google Scholar]
- 76.Gray W.A., Cardenas J.A., Brodmann M., Werner M., Bernardo N.I., George J.C. Treating post-angioplasty dissection in the femoropopliteal arteries using the tack endovascular system: 12-month results from the TOBA II Study. JACC Cardiovasc Interv. 2019;12:2375–2384. doi: 10.1016/j.jcin.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 77.Lio C.J., Yuita H., Rao A. Dysregulation of the TET family of epigenetic regulators in lymphoid and myeloid malignancies. Blood. 2019;134:1487–1497. doi: 10.1182/blood.2019791475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yue X., Rao A. TET family dioxygenases and the TET activator vitamin C in immune responses and cancer. Blood. 2020;136:1394–1401. doi: 10.1182/blood.2019004158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yin R., Mao S.Q., Zhao B., Chong Z., Yang Y., Zhao C. Ascorbic acid enhances Tet-mediated 5-methylcytosine oxidation and promotes DNA demethylation in mammals. J Am Chem Soc. 2013;135:10396–10403. doi: 10.1021/ja4028346. [DOI] [PubMed] [Google Scholar]
- 80.Young J.I., Zuchner S., Wang G. Regulation of the epigenome by vitamin C. Annu Rev Nutr. 2015;35:545–564. doi: 10.1146/annurev-nutr-071714-034228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Arakawa E., Hasegawa K., Irie J., Ide S., Ushiki J., Yamaguchi K. L-ascorbic acid stimulates expression of smooth muscle-specific markers in smooth muscle cells both in vitro and in vivo. J Cardiovasc Pharmacol. 2003;42:745–751. doi: 10.1097/00005344-200312000-00008. [DOI] [PubMed] [Google Scholar]
- 82.Vissers M.C.M., Das A.B. Potential mechanisms of action for vitamin C in cancer: reviewing the evidence. Front Physiol. 2018;9:809. doi: 10.3389/fphys.2018.00809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tomoda H., Yoshitake M., Morimoto K., Aoki N. Possible prevention of postangioplasty restenosis by ascorbic acid. Am J Cardiol. 1996;78:1284–1286. doi: 10.1016/s0002-9149(96)00613-3. [DOI] [PubMed] [Google Scholar]
- 84.Yang C.W., Wu C.C., Luo C.M., Chuang S.Y., Chen C.H., Shen Y.F. A randomized feasibility study of the effect of ascorbic acid on post-angioplasty restenosis of hemodialysis vascular access ( NCT03524846) Sci Rep. 2019;9:11095. doi: 10.1038/s41598-019-47583-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cote G., Tardif J.C., Lesperance J., Lambert J., Bourassa M., Bonan R. Effects of probucol on vascular remodeling after coronary angioplasty. Multivitamins and Protocol Study Group. Circulation. 1999;99:30–35. doi: 10.1161/01.cir.99.1.30. [DOI] [PubMed] [Google Scholar]
- 86.Fang J.C., Kinlay S., Beltrame J., Hikiti H., Wainstein M., Behrendt D. Effect of vitamins C and E on progression of transplant-associated arteriosclerosis: a randomised trial. Lancet. 2002;359:1108–1113. doi: 10.1016/S0140-6736(02)08154-0. [DOI] [PubMed] [Google Scholar]
- 87.Kakade S., Mani G. A comparative study of the effects of vitamin C, sirolimus, and paclitaxel on the growth of endothelial and smooth muscle cells for cardiovascular medical device applications. Drug Des Devel Ther. 2013;7:529–544. doi: 10.2147/DDDT.S45162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dokmanovic M., Clarke C., Marks P.A. Histone deacetylase inhibitors: overview and perspectives. Mol Cancer Res. 2007;5:981–989. doi: 10.1158/1541-7786.MCR-07-0324. [DOI] [PubMed] [Google Scholar]
- 89.Hontecillas-Prieto L., Flores-Campos R., Silver A., de Alava E., Hajji N., Garcia-Dominguez D.J. Synergistic enhancement of cancer therapy using HDAC inhibitors: opportunity for clinical trials. Front Genet. 2020;11:578011. doi: 10.3389/fgene.2020.578011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Findeisen H.M., Gizard F., Zhao Y., Qing H., Heywood E.B., Jones K.L. Epigenetic regulation of vascular smooth muscle cell proliferation and neointima formation by histone deacetylase inhibition. Arterioscler Thromb Vasc Biol. 2011;31:851–860. doi: 10.1161/ATVBAHA.110.221952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cao D., Wang Z., Zhang C.L., Oh J., Xing W., Li S. Modulation of smooth muscle gene expression by association of histone acetyltransferases and deacetylases with myocardin. Mol Cell Biol. 2005;25:364–376. doi: 10.1128/MCB.25.1.364-376.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yoshida T., Gan Q., Shang Y., Owens G.K. Platelet-derived growth factor-BB represses smooth muscle cell marker genes via changes in binding of MKL factors and histone deacetylases to their promoters. Am J Physiol Cell Physiol. 2007;292:C886–C895. doi: 10.1152/ajpcell.00449.2006. [DOI] [PubMed] [Google Scholar]
- 93.Zhang M., Urabe G., Little C., Wang B., Kent A.M., Huang Y. HDAC6 regulates the MRTF-A/SRF axis and vascular smooth muscle cell plasticity. JACC Basic Transl Sci. 2018;3:782–795. doi: 10.1016/j.jacbts.2018.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McDonald O.G., Wamhoff B.R., Hoofnagle M.H., Owens G.K. Control of SRF binding to CArG box chromatin regulates smooth muscle gene expression in vivo. J Clin Invest. 2006;116:36–48. doi: 10.1172/JCI26505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yoshida T., Kaestner K.H., Owens G.K. Conditional deletion of Kruppel-like factor 4 delays downregulation of smooth muscle cell differentiation markers but accelerates neointimal formation following vascular injury. Circ Res. 2008;102:1548–1557. doi: 10.1161/CIRCRESAHA.108.176974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Usui T., Morita T., Okada M., Yamawaki H. Histone deacetylase 4 controls neointimal hyperplasia via stimulating proliferation and migration of vascular smooth muscle cells. Hypertension. 2014;63:397–403. doi: 10.1161/HYPERTENSIONAHA.113.01843. [DOI] [PubMed] [Google Scholar]
- 97.Manea S.A., Vlad M.L., Fenyo I.M., Lazar A.G., Raicu M., Muresian H. Pharmacological inhibition of histone deacetylase reduces NADPH oxidase expression, oxidative stress and the progression of atherosclerotic lesions in hypercholesterolemic apolipoprotein E-deficient mice; potential implications for human atherosclerosis. Redox Biol. 2020;28:101338. doi: 10.1016/j.redox.2019.101338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pickell Z., Williams A.M., Alam H.B., Hsu C.H. Histone deacetylase inhibitors: a novel strategy for neuroprotection and cardioprotection following ischemia/reperfusion injury. J Am Heart Assoc. 2020;9:e016349. doi: 10.1161/JAHA.120.016349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Borck P.C., Guo L.W., Plutzky J. BET epigenetic reader proteins in cardiovascular transcriptional programs. Circ Res. 2020;126:1190–1208. doi: 10.1161/CIRCRESAHA.120.315929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Devaiah B.N., Case-Borden C., Gegonne A., Hsu C.H., Chen Q., Meerzaman D. BRD4 is a histone acetyltransferase that evicts nucleosomes from chromatin. Nat Struct Mol Biol. 2016;23:540–548. doi: 10.1038/nsmb.3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang B., Zhang M., Takayama T., Shi X., Roenneburg D.A., Kent K.C. BET bromodomain blockade mitigates intimal hyperplasia in rat carotid arteries. EBioMedicine. 2015;2:1650–1661. doi: 10.1016/j.ebiom.2015.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang B., Chen G., Urabe G., Xie R., Wang Y., Shi X. A paradigm of endothelium-protective and stent-free anti-restenotic therapy using biomimetic nanoclusters. Biomaterials. 2018;178:293–301. doi: 10.1016/j.biomaterials.2018.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Das S., Senapati P., Chen Z., Reddy M.A., Ganguly R., Lanting L. Regulation of angiotensin II actions by enhancers and super-enhancers in vascular smooth muscle cells. Nat Commun. 2017;8:1467. doi: 10.1038/s41467-017-01629-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Filippakopoulos P., Qi J., Picaud S., Shen Y., Smith W.B., Fedorov O. Selective inhibition of BET bromodomains. Nature. 2010;468:1067–1073. doi: 10.1038/nature09504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jiang G., Deng W., Liu Y., Wang C. General mechanism of JQ1 in inhibiting various types of cancer. Mol Med Rep. 2020;21:1021–1034. doi: 10.3892/mmr.2020.10927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dawson M.A., Prinjha R.K., Dittmann A., Giotopoulos G., Bantscheff M., Chan W.I. Inhibition of BET recruitment to chromatin as an effective treatment for MLL-fusion leukaemia. Nature. 2011;478:529–533. doi: 10.1038/nature10509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.McLure K.G., Gesner E.M., Tsujikawa L., Kharenko O.A., Attwell S., Campeau E. RVX-208, an inducer of ApoA-I in humans, is a BET bromodomain antagonist. PLoS One. 2013;8:e83190. doi: 10.1371/journal.pone.0083190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bailey D., Jahagirdar R., Gordon A., Hafiane A., Campbell S., Chatur S. RVX-208: a small molecule that increases apolipoprotein A-I and high-density lipoprotein cholesterol in vitro and in vivo. J Am Coll Cardiol. 2010;55:2580–2589. doi: 10.1016/j.jacc.2010.02.035. [DOI] [PubMed] [Google Scholar]
- 109.Jahagirdar R., Zhang H., Azhar S., Tobin J., Attwell S., Yu R. A novel BET bromodomain inhibitor, RVX-208, shows reduction of atherosclerosis in hyperlipidemic ApoE deficient mice. Atherosclerosis. 2014;236:91–100. doi: 10.1016/j.atherosclerosis.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 110.Nicholls S.J., Gordon A., Johansson J., Wolski K., Ballantyne C.M., Kastelein J.J. Efficacy and safety of a novel oral inducer of apolipoprotein a-I synthesis in statin-treated patients with stable coronary artery disease a randomized controlled trial. J Am Coll Cardiol. 2011;57:1111–1119. doi: 10.1016/j.jacc.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 111.Nicholls S.J., Puri R., Wolski K., Ballantyne C.M., Barter P.J., Brewer H.B. Effect of the BET protein inhibitor, RVX-208, on progression of coronary atherosclerosis: results of the phase 2b, randomized, double-blind, multicenter, ASSURE trial. Am J Cardiovasc Drugs. 2016;16:55–65. doi: 10.1007/s40256-015-0146-z. [DOI] [PubMed] [Google Scholar]
- 112.Ray K.K., Nicholls S.J., Buhr K.A., Ginsberg H.N., Johansson J.O., Kalantar-Zadeh K. Effect of apabetalone added to standard therapy on major adverse cardiovascular events in patients with recent acute coronary syndrome and type 2 diabetes: a randomized clinical trial. JAMA. 2020;323:1565–1573. doi: 10.1001/jama.2020.3308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ray K.K., Nicholls S.J., Ginsberg H.D., Johansson J.O., Kalantar-Zadeh K., Kulikowski E. Effect of selective BET protein inhibitor apabetalone on cardiovascular outcomes in patients with acute coronary syndrome and diabetes: rationale, design, and baseline characteristics of the BETonMACE trial. Am Heart J. 2019;217:72–83. doi: 10.1016/j.ahj.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 114.Dey A., Varelas X., Guan K.L. Targeting the Hippo pathway in cancer, fibrosis, wound healing and regenerative medicine. Nat Rev Drug Discov. 2020;19:480–494. doi: 10.1038/s41573-020-0070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wang Y., Hu G., Liu F., Wang X., Wu M., Schwarz J.J. Deletion of yes-associated protein (YAP) specifically in cardiac and vascular smooth muscle cells reveals a crucial role for YAP in mouse cardiovascular development. Circ Res. 2014;114:957–965. doi: 10.1161/CIRCRESAHA.114.303411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Xu F., Ahmed A.S., Kang X., Hu G., Liu F., Zhang W. MicroRNA-15b/16 attenuates vascular neointima formation by promoting the contractile phenotype of vascular smooth muscle through targeting YAP. Arterioscler Thromb Vasc Biol. 2015;35:2145–2152. doi: 10.1161/ATVBAHA.115.305748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wang X., Hu G., Gao X., Wang Y., Zhang W., Harmon E.Y. The induction of yes-associated protein expression after arterial injury is crucial for smooth muscle phenotypic modulation and neointima formation. Arterioscler Thromb Vasc Biol. 2012;32:2662–2669. doi: 10.1161/ATVBAHA.112.254730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Osman I., He X., Liu J., Dong K., Wen T., Zhang F. TEAD1 (TEA Domain Transcription Factor 1) promotes smooth muscle cell proliferation through upregulating SLC1A5 (Solute Carrier Family 1 Member 5)-mediated glutamine uptake. Circ Res. 2019;124:1309–1322. doi: 10.1161/CIRCRESAHA.118.314187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ostriker A.C., Martin K.A. Hippo and hyperplasia. Circ Res. 2019;124:1282–1284. doi: 10.1161/CIRCRESAHA.119.314968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Arehart E., Stitham J., Asselbergs F.W., Douville K., MacKenzie T., Fetalvero K.M. Acceleration of cardiovascular disease by a dysfunctional prostacyclin receptor mutation: potential implications for cyclooxygenase-2 inhibition. Circ Res. 2008;102:986–993. doi: 10.1161/CIRCRESAHA.107.165936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fetalvero K.M., Shyu M., Nomikos A.P., Chiu Y.F., Wagner R.J., Powell R.J. The prostacyclin receptor induces human vascular smooth muscle cell differentiation via the protein kinase A pathway. Am J Physiol Heart Circ Physiol. 2006;290:H1337–H1346. doi: 10.1152/ajpheart.00936.2005. [DOI] [PubMed] [Google Scholar]
- 122.Kimura T.E., Duggirala A., Smith M.C., White S., Sala-Newby G.B., Newby A.C. The Hippo pathway mediates inhibition of vascular smooth muscle cell proliferation by cAMP. J Mol Cell Cardiol. 2016;90:1–10. doi: 10.1016/j.yjmcc.2015.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Savage M.P., Goldberg S., Bove A.A., Deutsch E., Vetrovec G., Macdonald R.G. Effect of thromboxane A2 blockade on clinical outcome and restenosis after successful coronary angioplasty. Multi-Hospital Eastern Atlantic Restenosis Trial (M-HEART II) Circulation. 1995;92:3194–3200. doi: 10.1161/01.cir.92.11.3194. [DOI] [PubMed] [Google Scholar]
- 124.Feng X., Liu P., Zhou X., Li M.T., Li F.L., Wang Z. Thromboxane A2 activates YAP/TAZ protein to induce vascular smooth muscle cell proliferation and migration. J Biol Chem. 2016;291:18947–18958. doi: 10.1074/jbc.M116.739722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Huang C., Zhao J., Zhu Y. Drug-eluting stent targeting Sp-1-attenuated restenosis by engaging YAP-mediated vascular smooth muscle cell phenotypic modulation. J Am Heart Assoc. 2020;9:e014103. doi: 10.1161/JAHA.119.014103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Pobbati A.V., Hong W. A combat with the YAP/TAZ-TEAD oncoproteins for cancer therapy. Theranostics. 2020;10:3622–3635. doi: 10.7150/thno.40889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bakken A.M., Palchik E., Hart J.P., Rhodes J.M., Saad W.E., Davies M.G. Impact of diabetes mellitus on outcomes of superficial femoral artery endoluminal interventions. J Vasc Surg. 2007;46:946–958. doi: 10.1016/j.jvs.2007.06.047. discussion: 58. [DOI] [PubMed] [Google Scholar]
- 128.Moussa I., Leon M.B., Baim D.S., O'Neill W.W., Popma J.J., Buchbinder M. Impact of sirolimus-eluting stents on outcome in diabetic patients: a SIRIUS (SIRolImUS-coated Bx Velocity balloon-expandable stent in the treatment of patients with de novo coronary artery lesions) substudy. Circulation. 2004;109:2273–2278. doi: 10.1161/01.CIR.0000129767.45513.71. [DOI] [PubMed] [Google Scholar]
- 129.Woudstra P., Damman P., Beijk M.A., Grundeken M.J., Harskamp R.E., Koch K.T. Clinical outcomes after bare-metal stenting in diabetic patients with lesions carrying a low risk of restenosis. Catheter Cardiovasc Interv. 2013;81:26–33. doi: 10.1002/ccd.24444. [DOI] [PubMed] [Google Scholar]
- 130.Walker K.L., Walsh D.B., Goodney P.P., Connell S.A., Stone D.H., Powell R.J. Retrospective review of superficial femoral artery stenting in diabetic patients: thiazolidinedione use may decrease reinterventions. BMC Cardiovasc Disord. 2014;14:184. doi: 10.1186/1471-2261-14-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nakayama T., Komiyama N., Yokoyama M., Namikawa S., Kuroda N., Kobayashi Y. Pioglitazone induces regression of coronary atherosclerotic plaques in patients with type 2 diabetes mellitus or impaired glucose tolerance: a randomized prospective study using intravascular ultrasound. Int J Cardiol. 2010;138:157–165. doi: 10.1016/j.ijcard.2008.08.031. [DOI] [PubMed] [Google Scholar]
- 132.Nishio K., Sakurai M., Kusuyama T., Shigemitsu M., Fukui T., Kawamura K. A randomized comparison of pioglitazone to inhibit restenosis after coronary stenting in patients with type 2 diabetes. Diabetes Care. 2006;29:101–106. doi: 10.2337/diacare.29.01.06.dc05-1170. [DOI] [PubMed] [Google Scholar]
- 133.Kubota T., Kubota N., Sato H., Inoue M., Kumagai H., Iwamura T. Pioglitazone ameliorates smooth muscle cell proliferation in cuff-induced neointimal formation by both adiponectin-dependent and -independent pathways. Sci Rep. 2016;6:34707. doi: 10.1038/srep34707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhou X., Chen S., Zhu M., Hua J., Dai J., Xu X. Different effects of thiazolidinediones on in-stent restenosis and target lesion revascularization after PCI: a meta-analysis of randomized controlled trials. Sci Rep. 2017;7:14464. doi: 10.1038/s41598-017-14873-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wu H., Yang Y., Zheng B., Chen K. Decreased PPAR-gamma expression after internal carotid artery stenting is associated with vascular lesions induced by smooth muscle cell proliferation and systemic inflammation in a minipig model. Int J Clin Exp Pathol. 2017;10:7375–7383. [PMC free article] [PubMed] [Google Scholar]
- 136.Yang H.M., Kim B.K., Kim J.Y., Kwon Y.W., Jin S., Lee J.E. PPARgamma modulates vascular smooth muscle cell phenotype via a protein kinase G-dependent pathway and reduces neointimal hyperplasia after vascular injury. Exp Mol Med. 2013;45:e65. doi: 10.1038/emm.2013.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zhang L., Xie P., Wang J., Yang Q., Fang C., Zhou S. Impaired peroxisome proliferator-activated receptor-gamma contributes to phenotypic modulation of vascular smooth muscle cells during hypertension. J Biol Chem. 2010;285:13666–13677. doi: 10.1074/jbc.M109.087718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Parker-Duffen J.L., Walsh K. Cardiometabolic effects of adiponectin. Best Pract Res Clin Endocrinol Metab. 2014;28:81–91. doi: 10.1016/j.beem.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yu J.G., Javorschi S., Hevener A.L., Kruszynska Y.T., Norman R.A., Sinha M. The effect of thiazolidinediones on plasma adiponectin levels in normal, obese, and type 2 diabetic subjects. Diabetes. 2002;51:2968–2974. doi: 10.2337/diabetes.51.10.2968. [DOI] [PubMed] [Google Scholar]
- 140.Liu M., Liu F. Up- and down-regulation of adiponectin expression and multimerization: mechanisms and therapeutic implication. Biochimie. 2012;94:2126–2130. doi: 10.1016/j.biochi.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ding M., Carrao A.C., Wagner R.J., Xie Y., Jin Y., Rzucidlo E.M. Vascular smooth muscle cell-derived adiponectin: a paracrine regulator of contractile phenotype. J Mol Cell Cardiol. 2012;52:474–484. doi: 10.1016/j.yjmcc.2011.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhang W., Shu C., Li Q., Li M., Li X. Adiponectin affects vascular smooth muscle cell proliferation and apoptosis through modulation of the mitofusin-2-mediated Ras-Raf-Erk1/2 signaling pathway. Mol Med Rep. 2015;12:4703–4707. doi: 10.3892/mmr.2015.3899. [DOI] [PubMed] [Google Scholar]
- 143.Chen X., Yuan Y., Wang Q., Xie F., Xia D., Wang X. Post-translational modification of adiponectin affects lipid accumulation, proliferation and migration of vascular smooth muscle cells. Cell Physiol Biochem. 2017;43:172–181. doi: 10.1159/000480336. [DOI] [PubMed] [Google Scholar]
- 144.Fairaq A., Shawky N.M., Osman I., Pichavaram P., Segar L. AdipoRon, an adiponectin receptor agonist, attenuates PDGF-induced VSMC proliferation through inhibition of mTOR signaling independent of AMPK: implications toward suppression of neointimal hyperplasia. Pharmacol Res. 2017;119:289–302. doi: 10.1016/j.phrs.2017.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Wang X., Pu H., Ma C., Jiang T., Wei Q., Zhang C. Adiponectin abates atherosclerosis by reducing oxidative stress. Med Sci Monit. 2014;20:1792–1800. doi: 10.12659/MSM.892299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Li Q.X., Ao X., Wen L., Zhong H.J., Zeng X.Y., Li Y. Effect of increased levels of adiponectin by administration of the adeno vector rAAV2/1-Acrp30 on glucose, lipid metabolism and ultrastructure of the aorta in Goto-Kakizaki rats with arteriosclerosis. Natl Med J India. 2012;25:5–9. [PubMed] [Google Scholar]
- 147.Chrusciel P., Sahebkar A., Rembek-Wieliczko M., Serban M.C., Ursoniu S., Mikhailidis D.P. Impact of statin therapy on plasma adiponectin concentrations: a systematic review and meta-analysis of 43 randomized controlled trial arms. Atherosclerosis. 2016;253:194–208. doi: 10.1016/j.atherosclerosis.2016.07.897. [DOI] [PubMed] [Google Scholar]
- 148.Baeten J.T., Lilly B. Notch signaling in vascular smooth muscle cells. Adv Pharmacol. 2017;78:351–382. doi: 10.1016/bs.apha.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Baeten J.T., Lilly B. Differential regulation of NOTCH2 and NOTCH3 contribute to their unique functions in vascular smooth muscle cells. J Biol Chem. 2015;290:16226–16237. doi: 10.1074/jbc.M115.655548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Li X., Zhang X., Leathers R., Makino A., Huang C., Parsa P. Notch3 signaling promotes the development of pulmonary arterial hypertension. Nat Med. 2009;15:1289–1297. doi: 10.1038/nm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Domenga V., Fardoux P., Lacombe P., Monet M., Maciazek J., Krebs L.T. Notch3 is required for arterial identity and maturation of vascular smooth muscle cells. Genes Dev. 2004;18:2730–2735. doi: 10.1101/gad.308904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Caolo V., Schulten H.M., Zhuang Z.W., Murakami M., Wagenaar A., Verbruggen S. Soluble Jagged-1 inhibits neointima formation by attenuating Notch-Herp2 signaling. Arterioscler Thromb Vasc Biol. 2011;31:1059–1065. doi: 10.1161/ATVBAHA.110.217935. [DOI] [PubMed] [Google Scholar]
- 153.Humphries J.D., Byron A., Humphries M.J. Integrin ligands at a glance. J Cell Sci. 2006;119:3901–3903. doi: 10.1242/jcs.03098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Clyman R.I., McDonald K.A., Kramer R.H. Integrin receptors on aortic smooth muscle cells mediate adhesion to fibronectin, laminin, and collagen. Circ Res. 1990;67:175–186. doi: 10.1161/01.res.67.1.175. [DOI] [PubMed] [Google Scholar]
- 155.Ishigaki T., Imanaka-Yoshida K., Shimojo N., Matsushima S., Taki W., Yoshida T. Tenascin-C enhances crosstalk signaling of integrin alphavbeta3/PDGFR-beta complex by SRC recruitment promoting PDGF-induced proliferation and migration in smooth muscle cells. J Cell Physiol. 2011;226:2617–2624. doi: 10.1002/jcp.22614. [DOI] [PubMed] [Google Scholar]
- 156.Hoshiga M., Alpers C.E., Smith L.L., Giachelli C.M., Schwartz S.M. Alpha-v beta-3 integrin expression in normal and atherosclerotic artery. Circ Res. 1995;77:1129–1135. doi: 10.1161/01.res.77.6.1129. [DOI] [PubMed] [Google Scholar]
- 157.Misra A., Sheikh A.Q., Kumar A., Luo J., Zhang J., Hinton R.B. Integrin beta3 inhibition is a therapeutic strategy for supravalvular aortic stenosis. J Exp Med. 2016;213:451–463. doi: 10.1084/jem.20150688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Panchatcharam M., Miriyala S., Yang F., Leitges M., Chrzanowska-Wodnicka M., Quilliam L.A. Enhanced proliferation and migration of vascular smooth muscle cells in response to vascular injury under hyperglycemic conditions is controlled by beta3 integrin signaling. Int J Biochem Cell Biol. 2010;42:965–974. doi: 10.1016/j.biocel.2010.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Blindt R., Krott N., Hanrath P., vom Dahl J., van Eys G., Bosserhoff A.K. Expression patterns of integrins on quiescent and invasive smooth muscle cells and impact on cell locomotion. J Mol Cell Cardiol. 2002;34:1633–1644. doi: 10.1006/jmcc.2002.2113. [DOI] [PubMed] [Google Scholar]
- 160.Ruoslahti E., Pierschbacher M.D. Arg-Gly-Asp: a versatile cell recognition signal. Cell. 1986;44:517–518. doi: 10.1016/0092-8674(86)90259-x. [DOI] [PubMed] [Google Scholar]
- 161.Matsuno H., Stassen J.M., Vermylen J., Deckmyn H. Inhibition of integrin function by a cyclic RGD-containing peptide prevents neointima formation. Circulation. 1994;90:2203–2206. doi: 10.1161/01.cir.90.5.2203. [DOI] [PubMed] [Google Scholar]
- 162.Bishop G.G., McPherson J.A., Sanders J.M., Hesselbacher S.E., Feldman M.J., McNamara C.A. Selective alpha(v)beta(3)-receptor blockade reduces macrophage infiltration and restenosis after balloon angioplasty in the atherosclerotic rabbit. Circulation. 2001;103:1906–1911. doi: 10.1161/01.cir.103.14.1906. [DOI] [PubMed] [Google Scholar]
- 163.Choi E.T., Engel L., Callow A.D., Sun S., Trachtenberg J., Santoro S. Inhibition of neointimal hyperplasia by blocking alpha V beta 3 integrin with a small peptide antagonist GpenGRGDSPCA. J Vasc Surg. 1994;19:125–134. doi: 10.1016/s0741-5214(94)70127-x. [DOI] [PubMed] [Google Scholar]
- 164.Srivatsa S.S., Fitzpatrick L.A., Tsao P.W., Reilly T.M., Holmes D.R., Jr., Schwartz R.S. Selective alpha v beta 3 integrin blockade potently limits neointimal hyperplasia and lumen stenosis following deep coronary arterial stent injury: evidence for the functional importance of integrin alpha v beta 3 and osteopontin expression during neointima formation. Cardiovasc Res. 1997;36:408–428. doi: 10.1016/s0008-6363(97)00184-3. [DOI] [PubMed] [Google Scholar]
- 165.Choi E.T., Khan M.F., Leidenfrost J.E., Collins E.T., Boc K.P., Villa B.R. Beta3-integrin mediates smooth muscle cell accumulation in neointima after carotid ligation in mice. Circulation. 2004;109:1564–1569. doi: 10.1161/01.CIR.0000121733.68724.FF. [DOI] [PubMed] [Google Scholar]
- 166.Ewart A.K., Jin W., Atkinson D., Morris C.A., Keating M.T. Supravalvular aortic stenosis associated with a deletion disrupting the elastin gene. J Clin Invest. 1994;93:1071–1077. doi: 10.1172/JCI117057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Weng S., Zemany L., Standley K.N., Novack D.V., La Regina M., Bernal-Mizrachi C. Beta3 integrin deficiency promotes atherosclerosis and pulmonary inflammation in high-fat-fed, hyperlipidemic mice. Proc Natl Acad Sci U S A. 2003;100:6730–6735. doi: 10.1073/pnas.1137612100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kokubo T., Uchida H., Choi E.T. Integrin alpha(v)beta(3) as a target in the prevention of neointimal hyperplasia. J Vasc Surg. 2007;45(Suppl A):A33–A38. doi: 10.1016/j.jvs.2007.02.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Castier Y., Lehoux S., Hu Y., Foteinos G., Tedgui A., Xu Q. Characterization of neointima lesions associated with arteriovenous fistulas in a mouse model. Kidney Int. 2006;70:315–320. doi: 10.1038/sj.ki.5001569. [DOI] [PubMed] [Google Scholar]
- 170.Lekshmi K.M., Che H.L., Cho C.S., Park I.K. Drug- and gene-eluting stents for preventing coronary restenosis. Chonnam Med J. 2017;53:14–27. doi: 10.4068/cmj.2017.53.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Egashira K., Zhao Q., Kataoka C., Ohtani K., Usui M., Charo I.F. Importance of monocyte chemoattractant protein-1 pathway in neointimal hyperplasia after periarterial injury in mice and monkeys. Circ Res. 2002;90:1167–1172. doi: 10.1161/01.res.0000020561.03244.7e. [DOI] [PubMed] [Google Scholar]
- 172.Johnson T.W., Wu Y.X., Herdeg C., Baumbach A., Newby A.C., Karsch K.R. Stent-based delivery of tissue inhibitor of metalloproteinase-3 adenovirus inhibits neointimal formation in porcine coronary arteries. Arterioscler Thromb Vasc Biol. 2005;25:754–759. doi: 10.1161/01.ATV.0000157582.33180.a9. [DOI] [PubMed] [Google Scholar]
- 173.Sharif F., Hynes S.O., Cooney R., Howard L., McMahon J., Daly K. Gene-eluting stents: adenovirus-mediated delivery of eNOS to the blood vessel wall accelerates re-endothelialization and inhibits restenosis. Mol Ther. 2008;16:1674–1680. doi: 10.1038/mt.2008.165. [DOI] [PubMed] [Google Scholar]
- 174.Crews C.M. Targeting the undruggable proteome: the small molecules of my dreams. Chem Biol. 2010;17:551–555. doi: 10.1016/j.chembiol.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kostic M., Jones L.H. Critical assessment of targeted protein degradation as a research tool and pharmacological modality. Trends Pharmacol Sci. 2020;41:305–317. doi: 10.1016/j.tips.2020.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Hsu J.H., Rasmusson T., Robinson J., Pachl F., Read J., Kawatkar S. EED-targeted PROTACs degrade EED, EZH2, and SUZ12 in the PRC2 complex. Cell Chem Biol. 2020;27:41–46.e17. doi: 10.1016/j.chembiol.2019.11.004. [DOI] [PubMed] [Google Scholar]