Abstract
Background
Long-standing health disparities experienced by American Indians (AIs) are associated with increased all-cause mortality rates and shortened life expectancies when compared to other races and ethnicities. Nationally, these disparities have persisted with the COVID-19 pandemic as AIs are more likely than all other races to be infected, hospitalized, or die from SARS-CoV-2. The Mississippi Band of Choctaw Indians, the only federally recognized American Indian tribe in the state, has been one of the hardest hit in the nation.
Methods
Using de-identified data from the University of Mississippi Medical Center’s COVID-19 Research Registry, a retrospective cohort study was conducted to assess COVID-19 inpatient mortality outcomes among adults (≥ age 18) admitted at the state’s safety net hospital in 2020.
Results
Exactly 41% (n = 25) of American Indian adults admitted with a deemed diagnosis of COVID-19 died while in hospital, in comparison to 19% (n = 153) of blacks and 23% (n = 65) of whites. Racial disparities persisted even when controlling for those risk factors the CDC reported put adults at greatest risk of severe outcomes from the disease. The adjusted probability of inpatient mortality among American Indians was 46% (p < 0.00) in comparison to 19% among blacks and 20% among whites.
Conclusion
Although comorbidities were commonly observed among COVID-19 + American Indian inpatients, only one was associated with inpatient mortality. This challenges commonly cited theories attributing disparate COVID-19 mortality experiences among indigenous populations to disparate comorbidity experiences. Expanded studies are needed to further investigate these associations.
Keywords: American Indian, COVID-19, Mississippi, Inpatient mortality, Comorbidity, Health disparities
Introduction
American Indians (AIs) have experienced disproportionate disease burden and all-cause mortality rates since colonists settled in the Americas more than 5 centuries ago [1]. Today, the estimated 5.2 million AIs in the USA have a life expectancy 5.5 years less than all other races and ethnicities [2]. Compared with the general US population, AIs die at higher rates from accidents, cancer, diabetes, heart disease, homicide, influenza, kidney disease, pneumonia, stroke, and suicide [2]. The underlying reasons for these disparities have been heavily debated throughout the course of history, with contemporary suppositions often centered on such social determinants of health as discrimination, historical traumas, high rates of poverty, and inadequate education, nutrition, housing, and access to health care [1, 2].
As the SARS-CoV-2 pandemic (COVID-19) continues to rapidly spread across the globe, AIs are found to be one of the racial and ethnic minority groups at greatest risk of infection [3], hospitalization [4], and death [5] from the virus in the US. Studies conducted from January to June 2020 by the Centers for Diseases Control and Prevention (CDC) found AIs and Alaska Natives (ANs) 3.5 times as likely to be infected and almost twice as likely to die from the SARS-CoV-2 virus as non-Hispanic Whites [3, 5]. Across the nation, hospitalization rates for AIs/ANs were 3.7 times those of non-Hispanic Whites from March 2020 to March 2021 [4]. These rates outpace even those of other racial and ethnic minority groups of color such as Blacks, Hispanics and Latinos, and Pacific Islanders, also found to experience disparate infection, severe illness, and mortality rates from the virus causing COVID-19. Comparatively, rates of infection among Blacks are 1.1 times that of non-Hispanic Whites, hospitalization 2.8 times, and rates of death 1.9 times as of May 10, 2021 [6].
The more than 10,000 members of the Mississippi Band of Choctaw Indians (MBCI), the state’s only federally recognized tribe, have been one of the hardest hit AI tribes in the country from COVID-19 [7]. In just 1 year since the novel coronavirus reached the state in March 2020, more than 1 in 10—1831—members of the MBCI tribe contracted the virus and more than 1 in 100—114—died as a result [8]. As of March 8, 2021 AIs/ANs accounted for just 0.6% of cases in the state, but 1.6% of deaths [9].
Compelled by these disparities, this study was conducted with the primary objective of determining if inpatient mortality disparities persist among AI adults compared to all other races/ethnicities when controlling for those risk factors and comorbidities the CDC defined at the time as having the greatest evidence of putting adults at an increased risk of severe illness from the virus that causes COVID-19. Secondarily, this study aimed to identify those risk factors and comorbidities statistically significantly associated with inpatient mortality among AI adults.
Methods
Study Design and Setting
This retrospective cohort study was conducted at the University of Mississippi Medical Center (UMMC), the state’s only academic medical center and safety net hospital, using data from the UMMC COVID-19 Research Registry. The registry includes de-identified data from the Medical Center’s electronic health record system for all patients seen at a UMMC facility with a positive primary or secondary COVID-19 diagnosis. Institutional review board approval was not needed given the de-identified nature of the data and lack of intervention.
Cohort Identification
All adults, defined as those age 18 and up, admitted at UMMC in 2020 with a primary diagnosis of COVID-19 were included. To account for instances when patients were not confirmed COVID-positive until after admission, primary diagnoses were also extracted for all individuals with a secondary diagnosis of COVID-19 and independently screened by 2 authors. The authors, which included an emergency medicine physician and a population health science graduate student, screened primary diagnoses for known COVID-related symptoms (e.g., cough, respiratory distress, shortness of breath) and outcomes (e.g., acute respiratory failure with hypoxia, altered mental status, pulmonary embolism). Those with unrelated diagnoses (e.g., skull fracture, drug poisoning, burn) in conjunction with COVID-19 were excluded to prevent skewing of findings. Screeners reached a consensus on those patients to include with a secondary diagnosis of COVID-19 and a related primary diagnosis.
Data Abstraction and Variables of Interest
For all patients meeting inclusion criteria, age, sex, race(s), ethnicity, smoking status, diagnosis(es) name and associated ICD-10 diagnosis(es) code, insurance type, admission/discharge dates, discharge disposition, and patient status were abstracted on March 8, 2021. Patient status (alive/deceased) at the point of hospital discharge served as the inpatient mortality outcome of interest.
At the time of data abstraction and analysis in early March 2021, the CDC defined 10 risk factor and comorbidity categories with the strongest and most consistent evidence of putting adults of any age at increased risk of hospitalization and/or death as a result of COVID-19 infection [10]. These conditions include cancer; chronic kidney disease; COPD (chronic obstructive pulmonary disease); Down syndrome; heart failure, coronary artery disease, or cardiomyopathies; obesity (defined as a BMI > 30 kg/m2) and severe obesity (defined as a BMI ≥ 40 kg/m2); pregnancy; sickle cell disease; smoking; and type 2 diabetes mellitus [10]. All inpatient diagnoses data for included participants were screened for the reporting of any of these risk factors or conditions; diagnoses outside of these categories were excluded from analysis. These 10 condition categories in addition to race/ethnicity, age, and male sex served as the independent variables of interest in the multivariate regression model, given the believed association of each at the time with increased risk of severe illness or death from COVID-19.
Patients indicating AI/AN or Mississippi Band Choctaw Indian as their sole race or in any combination as their first and second race were evaluated as AIs. Those patients without a second race reported, either unknown or due to patient refusal, were categorized according to their primary race. Individuals with an unknown primary and secondary race as well as those with a single race of Asian, Hispanic, Multiracial, or Native Hawaiian/Pacific Islander were condensed into one “Unknown/Other” category for regression purposes given the small sample size they represented.
Age was evaluated as both a continuous and categorical independent variable. A binary smoking variable was created by defining smokers as those self-reporting “current every day smoker”, “current some day smoker”, “former smoker”, or “light tobacco smoker”. Binary codes were also created for each of the CDC’s 10 risk factor/condition categories, with heart failure, coronary artery disease, and cardiomyopathy diagnoses collapsed into 1 binary “heart conditions” variable.
Data Analyses
All statistical analyses were conducted using Stata/SE, version 16.0. Cohort characteristics were derived using descriptive statistics. Univariate and multivariate logistic regression models were utilized to investigate relationships between predictor variables (race/ethnicity, age, sex, and the defined CDC risk factors/comorbidities) and the primary inpatient mortality outcome of interest. Chi-square likelihood ratios were obtained to evaluate univariate regression models, while Wald chi-squares served as tests of individual predictors. To test for multicollinearity among independent regression variables, variance inflation factors (VIFs) were obtained.
Results
Study Population Demographics
A total of 1230 adults (aged 18–89) were admitted to UMMC between March 19 and December 31, 2020, either with a primary diagnosis of COVID-19 (n = 949), or with a secondary diagnosis of COVID-19 in combination with a related primary diagnosis (n = 281). Demographic information for included individuals is presented in Table 1. Self-identified females comprised 53.3% (n = 656) of the cohort. Self-reported racial composition included 65.9% African American/black (n = 811), 23.4% Caucasian/white (n = 288), 5% American Indian/Mississippi Band Choctaw Indian (n = 61), 4% Other (n = 49), 1.4% Unknown (n = 17), and < 1% Asian or Native Hawaiian/Pacific Islander (n = 4). Ethnic origins included 96.5% Not Hispanic or Latino (n = 1187), 3% Hispanic or Latino (n = 38), and < 1% Unknown (n = 5). The mean age of all participants was 58.3 years (± 16.6).
Table 1.
Demographic characteristics of patients with a deemed diagnosis of COVID-19 admitted at the University of Mississippi Medical Center, March–December 2020
| Race | Overall | ||||
|---|---|---|---|---|---|
| American Indian | Black | White | Other/Unknown | ||
| n = 61 (5.0%) | n = 811 (65.9%) | n = 288 (23.4%) | n = 70 (5.7%) | N = 1230 | |
| Sex, n (%) | |||||
| Female | 36 (59) | 438 (54) | 144 (50) | 38 (54) | 656 (53) |
| Male | 25 (41) | 373 (46) | 144 (50) | 32 (46) | 574 (47) |
| Age in years, n (%) | |||||
| Mean (SD) | 53.6 (15.7) | 57.6 (16.2) | 63.5 (16.3) | 48.3 (17.3) | 58.3 (16.6) |
| Median (IQR) | 54 (41–64) | 59 (48–69) | 66 (55–75) | 48 (35–61) | 60 (48–70) |
| 18–29 | 3 (4.9) | 57 (7.0) | 11 (3.8) | 13 (18.6) | 84 (6.8) |
| 30–39 | 11 (18.0) | 62 (7.6) | 21 (7.3) | 13 (18.6) | 107 (8.7) |
| 40–49 | 10 (16.4) | 107 (13.2) | 24 (8.3) | 11 (15.7) | 152 (12.4) |
| 50–59 | 13 (21.3) | 187 (23.1) | 40 (13.9) | 14 (20.0) | 254 (20.7) |
| 60–69 | 13 (21.3) | 209 (25.8) | 78 (27.1) | 10(14.3) | 310 (25.2) |
| 70–79 | 8 (13.1) | 131 (16.2) | 67 (23.3) | 7 (10.0) | 213 (17.3) |
| 80–89 | 3 (4.9) | 58 (7.2) | 47 (16.3) | 2 (2.9) | 110 (8.9) |
| Comorbidities/risk factors, n (%) | |||||
| Cancer | 4 (6.6) | 76 (9.4) | 61 (21.2) | 2 (2.9) | 143 (11.6) |
| Chronic kidney disease | 15 (24.6) | 236 (29.1) | 55 (19.1) | 4 (5.7) | 310 (25.2) |
| COPD | 0 (0.0) | 58 (7.2) | 48 (16.7) | 4 (5.7) | 110 (8.9) |
| Down syndrome | 0 (0.0) | 2 (0.3) | 2 (0.7) | 0 (0.0) | 4 (0.3) |
| Heart condition(s)* | 9 (14.8) | 206 (25.4) | 85 (29.5) | 12 (17.1) | 312 (25.4) |
| Obesity | 25 (41.0) | 292 (36) | 84 (29.2) | 23 (32.9) | 424 (34.5) |
| Pregnancy | 3 (4.9) | 21 (2.6) | 3 (1.0) | 20 (28.6) | 47 (3.8) |
| Sickle cell disease | 0 (0.0) | 20 (2.5) | 0 (0.0) | 0 (0.0) | 20 (1.6) |
| Smoking** | 15 (24.6) | 209 (25.8) | 77 (26.7) | 6 (8.6) | 307 (25.0) |
| Type 2 diabetes mellitus | 41 (67.2) | 436 (53.8) | 128 (44.4) | 23 (32.9) | 628 (51.1) |
| Patient status, n (%) | |||||
| Alive | 36 (59.0) | 658 (81.1) | 223 (77.4) | 57 (81.4) | 974 (79.2) |
| Deceased | 25 (41.0) | 153 (18.9) | 65 (22.6) | 13 (18.6) | 256 (20.8) |
COPD, chronic obstructive pulmonary disease; IQR, interquartile range; SD, standard deviation
*Heart condition(s) = heart failure, coronary artery disease, and/or cardiomyopathy diagnosis(es)
**Smoking = self-reported “current every day smoker”, “current some day smoker”, “former smoker”, or “light tobacco smoker”
Cohort Inpatient Mortality
Statistically significant associations between inpatient mortality and age, sex, smoking status, chronic kidney disease, COPD, Down syndrome, heart conditions, pregnancy, and type 2 diabetes were found in unadjusted logistic models (Tables 2 and 3). Given statistically insignificant numbers of patients who were pregnant, had Down syndrome, or sickle cell disease, these conditions were excluded from multivariate regression analyses. Multivariate logistic models including all other risk factors and conditions revealed age, race, sex, and heart conditions the only statistically significant predictors of inpatient mortality in the total inpatient population (Table 3).
Table 2.
Logistic regression results of possible predictors on inpatient mortality outcomes among American Indian adults with a deemed diagnosis of COVID-19 admitted at the University of Mississippi Medical Center in 2020
| Predictors | Unadjusted model, OR (95% CI) | Unadjusted mortality probability | Adjusted model, OR (95% CI) | Adjusted mortality probability |
|---|---|---|---|---|
| Age | 1.03 (1.00, 1.07) | * | 1.04 (0.99, 1.09) | * |
| Male sex | 1.23 (0.44, 3.48) | 0.44 | 1.01 (0.29, 3.55) | 0.23 |
| Female sex | 0.39 | 0.18 | ||
| Cancer | 1.48 (0.19, 11.26) | 0.50 | 0.67 (0.04, 10.49) | NE |
| Chronic kidney disease | 1.36 (0.42, 4.41) | 0.47 | 1.26 (0.28, 5.75) | NE |
| COPD | 5.00 (0.63, 39.39) | NE | 0.38 (0.01, 13.99) | NE |
| Heart condition(s)** | 3.47 (0.78, 15.51) | 0.67 | 8.97 (1.20, 66.87) | 0.27 |
| Obesity | 0.39 (0.13, 1.16) | 0.28 | 0.40 (0.09, 1.86) | 0.21 |
| Pregnancy | 0.21 (0.03, 1.58) | NE | - | - |
| Sickle cell disease | 0.47 (0.11, 2.05) | NE | - | - |
| Smoking*** | 0.43 (0.12, 1.56) | 0.27 | 0.23 (0.05, 1.08) | 0.24 |
| Type II diabetes | 1.45 (0.48, 4.40) | 0.44 | 1.22 (0.29, 5.06) | 0.22 |
Bolded items indicate P < 0.05
CI, confidence interval; COPD, chronic obstructive pulmonary disease; NE, not estimable; OR, odds ratio
*Age left as a continuous variable so therefore no specific probability
**Heart condition(s) = heart failure, coronary artery disease, and/or cardiomyopathy diagnosis(es)
***Smoking = self-reported “current every day smoker”, “current some day smoker”, “former smoker”, or “light tobacco smoker”
Adjusted model: race, age, sex, smoking status, cancer, chronic kidney disease, COPD, heart conditions, obesity, type II diabetes
Table 3.
Logistic regression results of possible predictors on inpatient mortality outcomes among adults of all races with a deemed diagnosis of COVID-19 admitted at the University of Mississippi Medical Center in 2020
| Predictors | Unadjusted model, OR (95% CI) | Unadjusted mortality probability | Adjusted model, OR (95% CI) | Adjusted mortality probability |
|---|---|---|---|---|
| Age | 1.04 (1.03, 1.05) | * | 1.04 (1.03, 1.05) | * |
| Male sex | 1.47 (1.12, 1.94) | 0.24 | 1.38 (1.02, 1.86) | 0.23 |
| Female sex | 0.18 | 0.19 | ||
| Cancer | 1.44 (0.97, 2.15) | 0.27 | 1.00 (0.65, 1.55) | 0.21 |
| Chronic kidney disease | 2.04 (1.51, 2.74) | 0.30 | 1.27 (0.91, 1.77) | 0.23 |
| COPD | 1.56 (1.00, 2.42) | 0.28 | 0.99 (0.61, 1.59) | 0.21 |
| Heart condition(s)** | 2.52 (1.88, 3.38) | 0.33 | 1.82 (1.32, 2.53) | 0.28 |
| Obesity | 0.81 (0.61, 1.09) | 0.19 | 1.14 (0.81, 1.59) | 0.22 |
| Pregnancy | 0.79 (0.01, 0.58) | 0.02 | - | - |
| Sickle cell disease | 0.42 (0.10, 1.81) | 0.10 | - | - |
| Smoking*** | 1.61 (1.19, 2.17) | 0.27 | 1.28 (0.92, 1.78) | 0.23 |
| Type II diabetes | 1.73 (1.30, 2.29) | 0.25 | 1.24 (0.91, 1.69) | 0.22 |
Bolded items indicate P < 0.05
CI, confidence interval; COPD, chronic obstructive pulmonary disease; OR, odds ratio
*Age left as a continuous variable so therefore no specific probability
**Heart condition(s) = heart failure, coronary artery disease, and/or cardiomyopathy diagnosis(es)
***Smoking = self-reported “current every day smoker”, “current some day smoker”, “former smoker”, or “light tobacco smoker”
Adjusted model: race, age, sex, smoking status, cancer, chronic kidney disease, COPD, heart conditions, obesity, type II diabetes
Low variance inflation factors (mean VIF = 1.83; all VIFs < 5.0) indicated an absence of multicollinearity among independent variables and more parsimonious models did not alter those predictors found statistically significant or non-significant. Given the evidence of clinical significance of the included risk factors and conditions and the absence of multicollinearity among them, the full multivariate regression model is reported here. The adjusted inpatient mortality probability among all patients was 28% for heart conditions (p < 0.00) and 23% for the male sex, chronic kidney disease, and self-reported smokers (p < 0.00), assuming all other multivariate regression predictors held constant.
Inpatient Mortality Among AIs
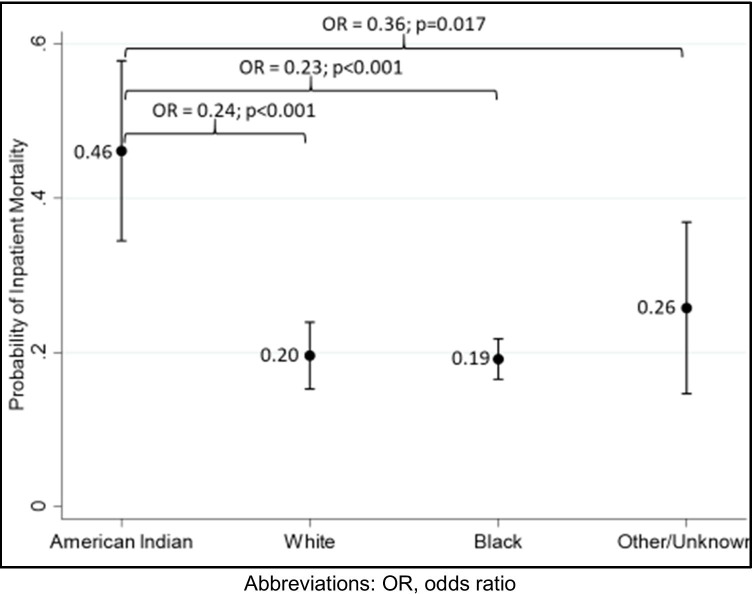
AIs represented approximately 5% (n = 61) of those admitted in 2020 due to COVID-19, yet they accounted for nearly 10% of all observed inpatient deaths in the study population. While the mortality prevalence for all included adults admitted with a primary diagnosis of COVID-19 was 20.8% (n = 256) in unadjusted statistics, the mortality prevalence among American Indians was more than double at 41% (n = 25). This compared with 22.6% of Caucasians/whites (n = 65), 18.9% of African Americans/blacks (n = 153), and 18.6% of inpatients with an Other/Unknown race (n = 13) who died while in the hospital. The adjusted probability of inpatient mortality among AIs was 46% (p < 0.00) in comparison to 19% for an otherwise identical black, 20% for white, and 26% for those of an other/unknown race, corresponding to reductions in the odds of death of 77% (OR = 0.23; p < 0.001), 76% (OR = 0.24; p < 0.001), and 64% (OR = 0.36; p = 0.017), respectively (Fig. 1). Holding all other adjusted model predictors constant, the probability of COVID-19 inpatient mortality among AIs with a heart condition was 27% (p < 0.00), 24% for smoking (p < 0.00), and 23% (p < 0.00) for the male sex. At all ages, the adjusted probability of inpatient mortality among American Indians was greater than that of all other races.
Fig. 1.
Adjusted probability of COVID-19 adult inpatient mortality at the University of Mississippi Medical Center in 2020 by race
Risk Factors and Comorbidities Among AIs
Risk factors and comorbidities most frequently observed among AIs admitted with COVID-19 were type 2 diabetes (67%, n = 41), obesity (41%, n = 25), chronic kidney disease (25%, n = 15), and smoking (25%, n = 15). Type 2 diabetes was the condition most commonly observed among AIs who died while in-hospital with 72% (n = 18) of the 25 AIs who died having the condition. Chronic kidney disease (28%, n = 7), obesity (28%, n = 7), and heart conditions (24%, n = 6) were also commonly observed among those who died prior to discharge.
Notably, heart conditions (OR, 8.97 [95% CI 1.20–66.87]; P = 0.032) were the only predictor significantly associated with inpatient mortality among AIs in adjusted analyses, however (Table 2). There was no significant difference in AI mortality outcomes for other predictors after adjustment. None of the 12 predictors assessed were significantly associated with AI inpatient mortality in unadjusted models.
Discussion
Limitations
This study is not without limitations. First, its cross-sectional and retrospective design do not allow for causal inferences. Also, comorbidities could only be evaluated on the binary basis of reported or not. Patients with both mild and severe disease are therefore classified uniformly and without distinction. Third, given insufficient sample sizes of pregnant patients or those with Down’s syndrome or sickle cell disease, their effect on inpatient mortality could not be determined. Also, a relatively small portion of the population (5%) was AI. This is remarkable, however, given AIs account for less than 1% of the state’s population. And finally, UMMC is the safety net hospital and the only level-1 trauma center in the state. Coupled with the shortage of beds in the state, it is plausible that inpatients could have been remarkably sicker than those admitted at other hospitals in the state at the same time. The likelihood of this may be greater in AI patients admitted as the official MBCI communities are located 55–105 mi from the main UMMC campus. Studies including other facilities across the state are needed to ensure a more generalizable and complete picture of the experiences of AIs with COVID-19 in Mississippi.
Conclusion
Consistent with empirical findings among AI populations [2], a high prevalence of comorbidities such as type 2 diabetes, obesity, and chronic kidney disease was observed among the AI study population. These conditions were not, however, found associated with inpatient mortality among AIs admitted at UMMC with COVID-19. In fact, of the 10 risk factors and underlying medical conditions, the CDC reported at the time with the greatest evidence of putting adults at increased risk of severe illness or death from the SARS-CoV-2 virus, only one—cardiovascular conditions—was found to have a statistically significant association of in-hospital death in the study population, regardless of race/ethnicity. This challenges theories routinely put forward attributing disparate mortality outcomes among AIs largely, if not solely, to disparate comorbidity experiences in the population.
Both proximal biological and distal social factors shape a population’s health. Systemic inequities experienced by AI populations may offer one possible downstream explanation for persistently disparate mortality rates in both the current pandemic and those historically. High rates of poverty and unemployment, education and medical care discrimination, and underfunding of health services have long been documented among AIs and associated with the lower health status they experience compared to other US populations [2]. Accurate and consistent reporting of race/ethnicity and AI population health data have been offered as critical initial steps to correct long-standing misclassifications and often resultantly, misappropriations of resources, to eliminate such disparities in the future [11].
In Mississippi, the poorest state in the country, these disparities may be exacerbated. Nearly 20% of Mississippians live in poverty, the highest rate of poverty in the nation, and more than 15% of adults aged 25 and older have not graduated from high school [12]. Moreover, all 8 of the official communities of the Mississippi Band of Choctaw Indians meet federal rural and medically underserved definitions [13, 14]. Notably the Health Resources & Services Administration (HRSA) has also designated all 8 communities as health professional shortage areas (HPSAs) in all 3 areas of consideration—primary care, dental care, and mental health [15].
COVID-19 prevention and treatment efforts among AIs in the state should seek to address these underlying factors contributing to the disparate infection, hospitalization, and mortality experiences. Initiatives in other regions may serve as a model to this end. The Navajo Safe Water project funded by the Indian Health Service, for instance, will provide clean water sources for more than 9,500 homes without piped water [16]. Mobile vaccination vehicles to reach AIs in rural areas, outreach efforts utilizing trusted local representatives, and culturally appropriate communications have resulted in similar successes [17]. Such initiatives provide a path forward to improved AI health in the current pandemic and beyond.
Funding
Dr. Seth Lirette is partially supported by the Mississippi Center for Clinical and Translational Research and Mississippi Center of Excellence in Perinatal Research COBRE funded by the National Institute of General Medical Sciences of the National Institutes of Health under Award Numbers 5U54GM115428 and P20GM121334. No other authors received support from any organization for the submitted work.
Data Availability
All data used to conduct this study are available.
Code Availability
All codes used to conduct this study are available.
Declarations
Ethics Approval
Ethics/Institutional Review Board approval was not needed given the de-identified nature of the data and lack of intervention.
Consent to Participate/Consent for Publication
Consent was not needed given the de-identified nature of the data and lack of intervention.
Conflicts of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jones DS. The persistence of American Indian health disparities. Am J Public Health. 2006;96(12):2122–2134. doi: 10.2105/AJPH.2004.054262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Indian Health Service. Indian health disparities. Rockville, MD. 2019.
- 3.Hatcher SM, Agnew-Brune C, Anderson M, et al. COVID-19 among American Indian and Alaska Native persons - 23 States, January 31-July 3, 2020. MMWR Surveill Summ. 2020;69(34):1166–1169. doi: 10.15585/mmwr.mm6934e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). cdc.gov. https://gis.cdc.gov/grasp/covidnet/covid19_3.html. Accessed 3 Apr 2021.
- 5.Arrazola J, Masiello MM, Joshi S, et al. COVID-19 mortality among American Indian and Alaska Native Persons - 14 States, January-June 2020. MMWR Surveill Summ. 2020;69(49):1853–1856. doi: 10.15585/mmwr.mm6949a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. cdc.gov. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html#footnote02. Accessed 23 Apr 2021.
- 7.Mitchell J, Finn J, Boudreau S. More Choctaws died of COVID than those in Hawaii. Or Alaska. Or Wyoming. Mississippi Center for Investigative Reporting. September 9, 2020. https://www.mississippicir.org/news/more-choctaws-have-died-of-covid-than-those-who-died-of-the-disease-in-hawaii-or-alaska-or-wyoming. Accessed 15 Mar 2021.
- 8.Important information on COVID-19. Choctaw Health Center. Updated March 8, 2021. https://www.choctaw.org/COVID19_MBCI.html. Accessed 11 Mar 2021.
- 9.COVID-19 in Mississippi. Mississippi State Department of Health. https://msdh.ms.gov/msdhsite/_static/14,0,420.html. Accessed 8 Mar 2021.
- 10.Underlying medical conditions associated with high risk for severe COVID-19: information for healthcare providers. cdc.gov. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html. Accessed 1 Mar 2021.
- 11.Bauer UE, Plescia M. Addressing disparities in the health of the American Indian and Alaska Native people: the importance of improved health data. Am J Public Health. 2014;104(Suppl 3):S255–S257. doi: 10.2105/AJPH.2013.301602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.QuickFacts: Mississippi. US Census Bureau. https://www.census.gov/quickfacts/MS. Accessed 3 Apr 2021.
- 13.Defining rural populations. Health Resources & Services Administration. https://www.hrsa.gov/rural-health/about-us/definition/index.html. Accessed 3 Apr 2021.
- 14.Medically underserved area (MUA) find. Health Resources & Services Administration. https://data.hrsa.gov/tools/shortage-area/mua-find. Accessed 3 Apr 2021.
- 15.What is shortage designation? Health Resources & Services Administration. https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation. Accessed 3 Apr 2021.
- 16.Navajo safe water: protecting you and your family's health. Navajo Nation COVID-19 Water Access Coordination Group . https://storymaps.arcgis.com/stories/1b4dc0d978c74d97a559e615730d4cd4. Accessed 1 Sept 2021.
- 17.Fact Sheet: Biden administration invests $4 billion in American Rescue Plan funding to combat COVID-19 in Indian country. The White House. https://www.whitehouse.gov/briefing-room/statements-releases/2021/04/16/fact-sheet-biden-administration-invests-4-billion-in-american-rescue-plan-funding-to-combat-covid-19-in-indian-country/. Published April 15, 2021. Accessed 1 Sept 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used to conduct this study are available.
All codes used to conduct this study are available.