Abstract
Objectives:
To examine patient characteristics and outcomes among opioid use disorder patients enrolled in low-threshold buprenorphine treatment during the COVID-19 pandemic.
Methods:
This paper describes the adaptation of the Project Connections (PC) program, a low-threshold buprenorphine program in Baltimore, in response to the COVID-19 pandemic. This paper examines patient characteristics and initial outcomes of patients served during a rapid protocol shift to telehealth that allowed buprenorphine initiation without an in-person encounter following a state-mandated stay-at-home order. Patient characteristics were compared to a subsample of patients enrolled in the program before the COVID-19 pandemic.
Results:
In March 2020, there was a sharp increase in new enrollments to the PC program. A total of 143 patients completed an intake assessment between March and May 2020 and 140 began treatment with buprenorphine/naloxone. Those who completed an intake assessment were primarily male (68.5%), Black (83.2%), had a mean age of 43.2 years (SD = 11.7), and reported a mean of 17.0 years of opioid use (SD = 12.9). The majority of patients were unemployed (72.7%) and reported previous criminal justice involvement (69.2%). Of those who completed an intake assessment, 96.5% returned for a second visit. Among those for whom 30-day retention data was available (n = 113), 63.7% were engaged for 30 days or longer.
Conclusions:
The PC program illustrates that offering on-demand, flexible treatment is an opportunity to increase opioid use disorder treatment access, even during a public health emergency that disrupted access to services. Relaxation of buprenorphine telehealth regulations allowed for flexibility in treatment and benefits vulnerable populations.
Keywords: buprenorphine. opioid agonist treatment, COVID-19, harm reduction, low-threshold treatment
Individuals with substance use disorders (SUDs) may be particularly vulnerable to the devastating impacts caused by the Coronavirus (COVID-19) pandemic given the acute effect of drug use on general respiratory and pulmonary health.1 For people of color and other marginalized communities, these risks are exacerbated by social determinants of health marked by poverty, housing instability, and greater likelihood of incarceration that contribute to decreased access to quality healthcare.2,3 Homelessness and incarceration may confine individuals to circumstances where they are in close proximity with others, placing them at high-risk of COVID-19 exposure.4–6 Rates of COVID-19 infection and resulting death have been substantially higher among communities of color,7 highlighting existing health inequalities that have been intensified by the pandemic.8,9 Additionally, the recommended protocol of social distancing and related public health measures have disrupted traditional access to care such as syringe exchange services, SUD treatment, primary care, mental health treatment, and psychosocial supports.1
Simultaneously, the opioid crisis continues unabated. Opioid use disorder (OUD) continues to be a leading cause of injury-related mortality across the United States.10 Thus, it remains essential to curtail COVID-19 related risks while maintaining and increasing access to treatment for particularly vulnerable populations to minimize harm related to both the virus and the ramifications of untreated opioid use. Fortunately, medications for OUD such as methadone and buprenorphine reduce mortality and improve health outcomes for individuals with OUD.11 However, treatment access is often stymied as a result of numerous logistical barriers.12,13
In Maryland, the first reported cases of COVID-19 began in early March with community transmission first noted by mid-March. In response to this, many SUD treatment programs reduced their operating hours and patient capacity and halted new admissions during the transition to telehealth. This led to decreased access to addiction treatment at a time when patients with OUD encountered increased COVID-19 related stressors such as social isolation, decreased access to public transportation, and closure of in-person support groups. With respect to recommended COVID-19 social distancing guidelines, modifications were announced by the Substance Abuse and Mental Health Administration in March 2020 to make treatment more accessible. Buprenorphine, which previously required a full in-person evaluation by a waivered provider, is now able to be prescribed via phone and requires less frequent monitoring. The loosening of federal guidelines for buprenorphine prescribing offers a viable opportunity to reach those who had been previously hindered by multiple barriers to initiating treatment.14
Amidst these public health crises, and with novel opportunities for lower-barrier treatment delivery, it is imperative to adapt addiction treatment models so that they are compliant with COVID-19 safety protocols and accessible to marginalized populations, who were already stigmatized and underserved by the traditional healthcare system. Low-barrier, flexible models for treatment are well-poised to bridge these gaps. Before COVID-19, low-threshold treatment programs demonstrated increased ability to reach vulnerable populations, such as those lacking stable housing or insurance, compared to traditional treatment programs.15,16 Qualitative studies have found that patients report positive experiences in low-threshold treatment settings and appreciated the flexible and harm reduction-oriented treatment model.17,18 Thus, low-threshold treatment models that operate within a harm reduction context may provide a viable opportunity to increase treatment access and engagement to vulnerable populations.
The Project Connections (PC) program, operated by Behavioral Health Leadership Institute (BHLI) – a nonprofit organization in Baltimore, has demonstrated initial success in maintaining a low-barrier, high-quality treatment approach.16 The BHLI model aims to meet vulnerable individuals “where they are,” both in location by creating pop-up clinics that are colocated in the community or through a mobile setting and in circumstance by reducing unnecessary program requirements. The program is committed to providing low-threshold, high-quality evidence-based treatment despite encountering challenges related to COVID-19. This paper describes the adaptation of the PC program in response to COVID-19 that focused on using its flexible approach to provide continuous, effective treatment while observing COVID-19 safety protocols and adapting to new buprenorphine regulations.
METHODS
Program Description
The PC Buprenorphine Program consists of a multisite project that has been in operation since 2001 by BHLI, a local nonprofit organization in Baltimore. The PC program has been described in depth previously.19
The program was expanded in 2017 with the addition of a van serving as a free-standing clinic located outside of the local jail every weekday. This site, the PC at Re-Entry (PCARE) van, is focused on increasing access and engagement with individuals who have been recently released from detention. The van location is also particularly accessible for individuals who are homeless due to its proximity to a large city shelter and homeless encampment site. The PCARE program aims to provide high-quality, individualized buprenorphine treatment that minimizes the usual barriers experienced by vulnerable populations. The program is predicated on an on-demand model of treatment, which allows interested individuals to speak with a clinician and receive an initial prescription for buprenorphine (if medically appropriate) when they come to the van. The PCARE model also attempts to resolve other commonly reported barriers, for example, by providing photo identification for patients who do not have state-issued identification cards so that they may fill their prescription. Additional details of the program's operations have been reported elsewhere16 and, recently, BHLI added an outreach component that works to optimize care coordination and address additional psychosocial needs. The ultimate goal is to achieve stability, and then, when the patient and treatment team agree, transition the patient to ongoing treatment either through a comprehensive primary care practice or a long-term OUD treatment program, as appropriate.
Protocol Changes Related to COVID-19
Pursuant to the advent of COVID-19 and subsequent needs for social isolation and quarantine, the BHLI organization shifted their operational protocol for all PC sites consistent with social distancing guidelines. As mentioned, community transmission of COVID-19 was noted in Maryland by mid-March and a statewide stay-at-home order was initiated by March 30th.
In mid-March, the PCARE team moved outdoors on the sidewalk with a collapsible canopy (for inclement weather) to meet with clients in a socially distanced manner. The clinical team met with patients outside to conduct intakes for new patients and follow-ups for continuing patients. The outreach team continued to engage patients and regularly communicated with the clinical team regarding any patients with outstanding needs. To minimize direct contact with bodily fluids, the PCARE team halted collection of oral fluid swabs used for confirmatory toxicology testing. Finally, to decrease the need to travel to the program and to decrease congestion at the site, prescribing practices were changed. Based on provider discretion and patient history (including housing status, access to pharmacy, and ability to safely store medication), patients were provided prescriptions for up to 4 weeks (previously 1–2 weeks). Naloxone was offered at each visit to reduce overdose risk. Several patients received multiple kits to distribute at their housing programs or shelters where kits were not readily available, but where overdose risk was high. Finally, BHLI used this interim period to prepare for the eventual transition to telehealth by updating patient contact information, delivering health education related to COVID-19, and reiterating program-related safety protocols.
On March 30th, concurrent with the statewide stay-at-home order and the loosening of regulations for buprenorphine by the Drug Enforcement Administration that allowed for buprenorphine initiation via telehealth, PC shifted to a fully telehealth protocol. Consistent with the mission of flexible adaptation while providing individualized and high-quality treatment, BHLI created a unique telehealth model that reflected the paucity of resource capacity of the program's target population, such as a lack of smartphone technology. BHLI organized a Zoom protocol that allowed the nurse and provider to conference with a patient on regular phone lines without the need for internet connection or other special technology. Additionally, the PCARE van remained parked at its usual location to serve as a physical representation of the program for those who could not be updated via phone. A large sign on the van door offered program contact information to anyone interested in treatment as an existing or new patient.
For telehealth visits, patients called in by phone to the Zoom conference call line that connected the provider, nurse, and patient to discuss clinical needs and determine appropriate medication for upcoming weeks. Prescriptions of clinically appropriate duration and dosages were called into partner pharmacies. Patients were given a scheduled time (eg, Wednesday morning) for follow-up telehealth appointments, but the telehealth schedule remained flexible to accommodate new patients or patients who missed their scheduled day.
In parallel to telehealth visits, a nurse monitored an additional phone line for new and established patients to contact the clinical team. Patients were able to leave voicemails or texts after hours for follow-up the next business day. Following each shift, the team sent out a team-wide email describing the daily clinical flow. The team also notified the outreach team regarding patient-identified issues. The outreach team followed up with patients to address potential barriers to care (eg, lack of insurance) or other COVID-19 related challenges, such as food and housing insecurity. The outreach team also made daily calls to remind patients of phone appointments and to conduct routine check-ins. Additionally, staff from one PC site offered a voluntary weekly telehealth support group. Before the COVID-19 pandemic, in-person visits were accompanied by toxicology; however, throughout the pandemic, the program chose to suspend toxicology in accordance with clinical guidance provided by the American Society of Addiction Medicine,20 and thus routine toxicology was not included as a component of the telehealth visits.
Finally, the van driver put out a large basket of naloxone kits each day on the sidewalk outside of the van. Approximately 200 kits were distributed between April and the end of May. This is significant because other access to naloxone was greatly limited due to program closures, whereas overdose deaths in Baltimore City have been rising throughout the year.21
Partnership With Commercial Pharmacy
During this time, PC leveraged its existing partnership with the national office of a commercial pharmacy to overcome patient-level barriers to obtaining medication (notably medication cost and lack of identification). This partnership allowed BHLI to seamlessly create more relaxed protocols with local pharmacies during the COVID-19 pandemic so buprenorphine could be supplied safely while reducing logistical barriers. This relationship was especially critical during the COVID-19 pandemic because, while pharmacies remained open, there were increased barriers resulting from patients transitioning from shelters to motels to promote social distancing and from limited services for obtaining IDs. Furthermore, patient report of medication theft increased and the partnership between BHLI and the pharmacy allowed for quick resolution (via medication refill).
Initial Outcome Reporting
We report demographic and clinical characteristics among patients who initiated buprenorphine treatment between March 1 and May 31, 2020, a critical period during the stay-at-home order in Maryland. We report the number of patients served during this time period, the proportion who returned for at least one visit after the initial buprenorphine prescription, and the proportion who were engaged in care for at least 30 days (measured in days between the first prescription and the last patient telehealth visit). We also report trends in the number of intakes over different stages of protocol changes. Lastly, we conducted chi-square tests of independence for categorical variables and one-way analyses of variance for continuous variables to evaluate any significant differences by sociodemographic and drug use characteristics among persons engaged during this time period compared to those who were established in the program before COVID-19 related protocol changes. Sociodemographic characteristics were defined as sex, race, age, housing status, employment status, and prior criminal justice involvement.
RESULTS
Patient Characteristics (March – May 2020)
Between March 1 and May 31, 2020, 143 new patients initiated buprenorphine treatment. The majority of these patients were male (68.5%) and Black (83.2%), with a mean age of 43.2 years (SD = 11.7). These patients were largely unemployed (72.7%), had a history of criminal justice involvement (69.2%), and reported a mean length of opioid use of 17.0 years (SD = 12.9). Roughly one third of patients reported a previous overdose event (33.5%). Compared to individuals who were previously engaged with the program before March 2020 (hereinafter referred to as the “established” subsample, n = 179), there were no statistically significant differences in patient characteristics (see Table 1), with the exception of total years of opioid use and past 30-day opioid use. Those who initiated care in March through May reported significantly more opioid use days compared to the established subsample (27.0 days versus 23.5 days, P = 0.002), but less total years of use (17.0 years [SD = 12.9] newly-enrolled patients versus 21.4 years [SD = 12.8] established patients, P = 0.007).
TABLE 1.
Patient Demographics of New and Established Patients in the Project Connections Program
| Established Patients n = 179 | New Patients n = 143 | Total n = 322 | P | |
| Sex | 0.41 | |||
| Male – n (%) | 127 (71.0) | 98 (68.5) | 225 (69.9) | |
| Female – n (%) | 52 (29.0) | 44 (30.8) | 96 (29.8) | |
| Transfemale – n (%) | 0 (0.0) | 1 (0.7) | 5 (0.3) | |
| Age (yrs) – mean (SD) | 45.0 (11.8) | 43.2 (11.7) | 44.2 (11.8) | 0.18 |
| Race/Ethnicity | 0.29 | |||
| Black – n (%) | 138 (77.1) | 119 (83.2) | 257 (79.8) | |
| White – n (%) | 31 (17.3) | 18 (12.6) | 49 (15.2) | |
| Other – n (%) | 6 (3.4) | 1 (0.7) | 7 (2.2) | |
| Missing – n (%) | 4 (2.2) | 5 (3.5) | 9 (2.8) | |
| Currently employed | 23 (12.8) | 17 (11.9) | 40 (12.4) | 0.78 |
| Currently insured | 163 (91.0) | 124 (86.7) | 287 (89.1) | 0.26 |
| Reported homelessness | 50 (27.9) | 30 (21.0) | 80 (24.8) | 0.22 |
| Criminal justice involvement | 139 (77.7) | 99 (69.2) | 238 (73.9) | 0.22 |
| Drug use behavior | ||||
| Years of opioid use∗ | 21.4 (12.8) | 17.0 (12.9) | 19.6 (13.0) | 0.007 |
| Days of opioid use (past 30 d)† | 23.5 (10.1) | 27.0 (7.1) | 24.7 (9.3) | 0.002 |
| Polysubstance use | 128 (71.5) | 97 (67.8) | 225 (69.9) | 0.48 |
| Injection drug use – n (%) | 55 (30.7) | 32 (22.4) | 87 (27.0) | 0.24 |
Percentages may not add up due to rounding.
Data available for 245 patients.
Data available for 259 patients.
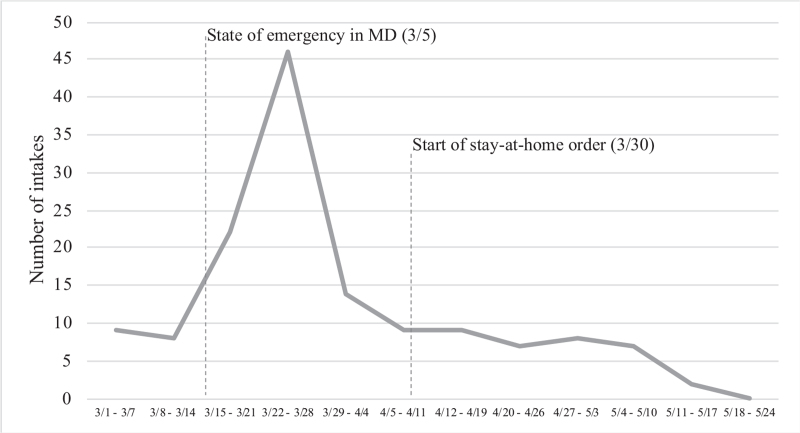
Trends in New Intakes and Clinical Encounters
As BHLI prepared for social distancing guidelines in the first 2 weeks of March, there were an average of 8.5 new intakes and 96.5 follow-up visits per week. By mid-March, many other treatment providers in Baltimore reduced their hours and halted new enrollments. During this time, PCARE experienced a sharp increase in intakes (see Fig. 1), with a total of 68 intakes over the last 2 weeks of March. Following the transition to telehealth, intakes decreased with approximately 9.4 new intakes completed per week in April.
FIGURE 1.
Number of completed intakes from March to May 2020, per week.
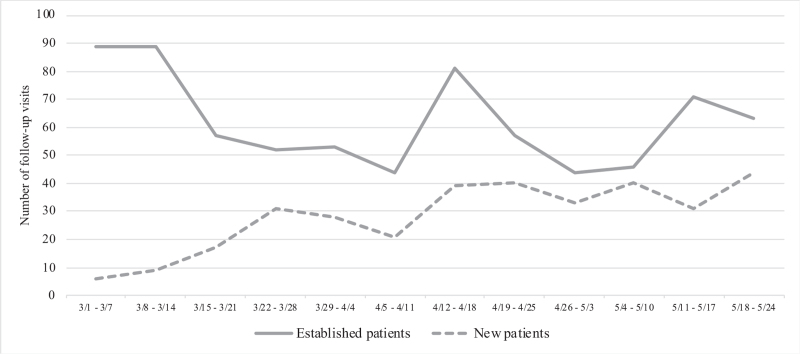
Retention and Follow-up Telehealth Visits
Among patients who initiated care in March – May 2020 (n = 143), 97.9% (n = 140) received their first buprenorphine prescription and 96.5% (n = 138) re-engaged with the clinical team for a second visit. Among a subsample of newly enrolled patients who completed an intake assessment in March through mid-April (n = 113), 63.7% of patients (n = 72) were engaged for 30 days or longer. There were no statistically significant differences in patients who remained engaged for 30 days compared to those who were lost to follow-up based on age, sex, race, housing status, employment status, or prior criminal justice involvement. Furthermore, the proportion of newly enrolled patients who were engaged for at least 30 days did not differ significantly compared to a cohort of PCARE patients who enrolled in treatment from March through May of 2019 (n = 23, 62.2% of 37 total patients enrolled in March–May 2019).
Figure 2 shows the flow of follow-up telehealth visits throughout March to May 2020 for both established patients and newly enrolled patients. The majority of follow-up visits in early to mid-March occurred among established patients as the clinical team was beginning to extend their prescribing protocol. Follow-up visits for newly enrolled patients continued to increase through the end of March through May.
FIGURE 2.
Number of follow-up telehealth visits from March to May 2020, per week.
DISCUSSION
The PC Buprenorphine Program illustrates the ability of low-threshold buprenorphine programs to reach traditionally underserved populations, even within the context and resulting instability of a public health crisis such as COVID-19. The majority of the patients reached during this time reported a long history of polysubstance use and had a number of other vulnerabilities such as unstable housing and unemployment. Despite the challenges faced by this patient population, many patients successfully engaged in treatment, as marked by the proportion of patients who were still engaged in treatment after 30 days (63%). The proportion of newly enrolled patients who were engaged in treatment after 30 days was similar to 30-day retention among a cohort who completed intakes during the same timeframe in 2019 (when only in-person visits were conducted). These findings are consistent with other studies of buprenorphine treatment among marginalized populations22–24 and further demonstrates the ability of low-threshold buprenorphine programs to successfully engage vulnerable populations.
Now more than ever, there is a critical need to continue to provide access to the life-saving medication buprenorphine, which remains highly controlled and is largely inaccessible for those in need of treatment.25–27 On-demand and low-threshold treatment like BHLI's PC are able to reach patients who are often missed in other settings by making treatment accessible and patient-centered. This is in contrast to many traditional addiction treatment programs whose strict program requirements (eg, need for photo identification, need to pay co-pay) prevent many people from seeking care. Although this sample reported numerous vulnerabilities, the PC program was successfully able to continue to provide high-quality and low-threshold care via telehealth.
The loosening of federal guidelines for buprenorphine prescribing (particularly via telehealth) is a viable opportunity to expand low-threshold and flexible care, consistent with the BHLI PC model, and to decrease the current treatment gap for those with OUD. Although the policy changes were implemented in response to the COVID-19 pandemic, the relaxation of these requirements has highlighted the potential to remove logistical barriers (such as transportation to frequent in-person appointments). The response to the COVID-19 pandemic as it relates to providing substance use treatment creates an opportunity to expand a more accessible and equitable treatment system that is grounded in harm reduction.14 This approach to treatment should be extended and promoted beyond the scope of the current COVID-19 pandemic. Although decreased regulation of buprenorphine may increase concerns related to medication diversion, strict provisions that prioritize these concerns are associated with stigma and limit their use.28 In balancing the need for increased access to treatment with the need to reduce diversion, it is important to adapt treatment models to minimize stigma and promote access to high-quality care, particularly for disenfranchised populations.
Although there is the opportunity to expand access to life-saving treatment options, it is critical to continue to reach highly vulnerable populations that have been historically devastated by the opioid epidemic. Though telehealth has minimized a number of barriers related to treatment delivery, challenges remain for those who cannot access these types of services, such as those experiencing homelessness or individuals who do not have reliable phone access. These challenges required the PC program to remain flexible in response to individual patient circumstance. BHLI's experience demonstrates the value of providing treatment that is accessible and that minimizes these barriers. However, even with a telehealth approach, difficulties exacerbated by poverty and stigma may reduce engagement. For example, telehealth is optimal with reliable phone access. Although BHLI created a model that could operate without smartphone technology, there were a number of patients who did not own any type of phone. Showing commitment to treatment engagement, many patients asked peers or the pharmacy to borrow a phone in order to do whatever they could to reach the program. To reach this population, even during health emergencies, policies are needed to increase free public phone access and to relax ID requirements.
There are limitations to note regarding this study. The reported patient characteristics and outcomes are from a single treatment program in Baltimore City and generalizability to other settings or geographic areas is limited. In addition, because information gathered through self-report, information could have been subject to social desirability effects.
CONCLUSIONS
In light of this population's myriad of vulnerabilities, it is incumbent to create public health solutions that facilitates easier access to treatment even when a crisis emerges. Medications such as buprenorphine are safe, effective, and must be readily accessible at the critical moment when an individual decides to seek treatment. Individuals with OUD face a plethora of barriers to healthcare that have been highlighted by the COVID-19 pandemic. The success of the BHLI PC low-threshold buprenorphine program illustrates that more accessibility and greater attention to minimizing barriers to care are both feasible and urgently needed.
Footnotes
Behavioral Health Leadership Institute Project Connections operations were supported by grants from the Abell Foundation, Open Society Institute – Baltimore, Carefirst Community Foundation, the Krieger Fund, Behavioral Health Systems Baltimore, Maryland Department of Health, and Purdue Pharma LP. Ms. Nordeck was also supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number T32DA007292.
The authors report no conflicts of interest.
REFERENCES
- 1.Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med 2020; 173(1):61–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. 2018 National Healthcare Quality and Disparities Report. Agency for Healthcare Research and Quality; 2019. [PubMed] [Google Scholar]
- 3.Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. Lancet 2017; 389(10077):1464–1474. [DOI] [PubMed] [Google Scholar]
- 4.Kinner SA, Young JT, Snow K, et al. Prisons and custodial settings are part of a comprehensive response to COVID-19. Lancet Public Health 2020; 5(4):e188–e189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health 2020; 5(4):e186–e187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saloner B, Parish K, Ward JA, DiLaura G, Dolovich S. COVID-19 cases and deaths in federal and state prisons. JAMA 2020; 324:602–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yancy CW. COVID-19 and African Americans. JAMA 2020; 323(19):1891–1892. [DOI] [PubMed] [Google Scholar]
- 8.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health 2011; 32(1):381–398. [DOI] [PubMed] [Google Scholar]
- 9.Dorn A van, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet Lond Engl 2020; 395(10232):1243–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson N. Drug and opioid-involved overdose deaths — United States, 2017-2018. MMWR Morb Mortal Wkly Rep 2020; 69:290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 2017; 357:j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J Subst Abuse Treat 2016; 61:47–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma A, Kelly SM, Mitchell SG, Gryczynski J, O’Grady KE, Schwartz RP. Update on barriers to pharmacotherapy for opioid use disorders. Curr Psychiatry Rep 2017; 19(6):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krawczyk N, Fingerhood MI, Agus D. Lessons from COVID 19. Are we finally ready to make opioid treatment accessible? J Subst Abuse Treat 2020; 117.doi:10.1016/j.jsat.2020.108074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall G, Neighbors CJ, Iheoma J, et al. Mobile opioid agonist treatment and public funding expands treatment for disenfranchised opioid-dependent individuals. J Subst Abuse Treat 2014; 46(4):511–515. [DOI] [PubMed] [Google Scholar]
- 16.Krawczyk N, Buresh M, Gordon MS, Blue TR, Fingerhood MI, Agus D. Expanding low-threshold buprenorphine to justice-involved individuals through mobile treatment: Addressing a critical care gap. J Subst Abuse Treat 2019; 103:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Snow RL, Simon RE, Jack HE, Oller D, Kehoe L, Wakeman SE. Patient experiences with a transitional, low-threshold clinic for the treatment of substance use disorder: a qualitative study of a bridge clinic. J Subst Abuse Treat 2019; 107:1–7. [DOI] [PubMed] [Google Scholar]
- 18.Truong C, Krawczyk N, Dejman M, et al. Challenges on the road to recovery: exploring attitudes and experiences of clients in a community-based buprenorphine program in Baltimore City. Addict Behav 2019; 93:14–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daniels AM, Salisbury-Afshar E, Hoffberg A, Agus D, Fingerhood MI. A novel community-based buprenorphine program: client description and initial Outcomes. J Addict Med 2014; 8(1):40–46. [DOI] [PubMed] [Google Scholar]
- 20. American Society of Addiction Medicine. COVID-19 - Adjusting Drug Testing Protocols. Published June 30, 2020. Available at: https://www.asam.org/Quality-Science/covid-19-coronavirus/adjusting-drug-testing-protocols. Accessed July 15, 2020. [Google Scholar]
- 21. Cohn M. Opioid-related deaths make a disappointing uptick in early 2020, possibly related to coronavirus. The Baltimore Sun. Available at: https://www.baltimoresun.com/health/bs-hs-overodose-deaths-first-quarter-20200611-r5pvlyzqrffo3ndvwc2oh3y7cy-story.html. Published June 11, 2020. Accessed July 13, 2020. [Google Scholar]
- 22.Lee CS, Rosales R, Stein MD, et al. Brief report: low-barrier buprenorphine initiation predicts treatment retention among Latinx and non-Latinx primary care patients. Am J Addict 2019; 28(5):409–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carter J, Zevin B, Lum PJ. Low barrier buprenorphine treatment for persons experiencing homelessness and injecting heroin in San Francisco. Addict Sci Clin Pract 2019; 14(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stancliff S, Joseph H, Fong C, Furst T, Comer SD, Roux P. Opioid maintenance treatment as a harm reduction tool for opioid-dependent individuals in New York City: the need to expand access to buprenorphine/naloxone in marginalized populations. J Addict Dis 2012; 31(3):278–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walley AY, Alperen JK, Cheng DM, et al. Office-based management of opioid dependence with buprenorphine: clinical practices and barriers. J Gen Intern Med 2008; 23(9):1393–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hutchinson E, Catlin M, Andrilla CHA, Baldwin L-M, Rosenblatt RA. Barriers to primary care physicians prescribing buprenorphine. Ann Fam Med 2014; 12(2):128–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haffajee RL, Bohnert ASB, Lagisetty PA. Policy pathways to address provider workforce barriers to buprenorphine treatment. Am J Prev Med 2018; 54: 6, Supplement 3: S230–S242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Doernberg M, Krawczyk N, Agus D, Fingerhood M. Demystifying buprenorphine misuse: has fear of diversion gotten in the way of addressing the opioid crisis? Subst Abuse 2019; 40(2):148–153. [DOI] [PMC free article] [PubMed] [Google Scholar]