Abstract
Objectives. To empirically evaluate the relationship between presence of a state or federal prison and COVID-19 case and death counts.
Methods. We merged data on locations of federal and state prisons and of local and county jails with daily case and death counts in the United States. We used a selection-on-observables design to estimate the correlation between prisons and COVID-19 spread, controlling for known correlates of COVID-19.
Results. We found empirical evidence that the presence and capacities of prisons are strong correlates of county-level COVID-19 case counts. The presence of a state or federal prison in a county corresponded with a 9% increase in the COVID-19 case count during the first wave of the pandemic, ending July 1, 2020.
Conclusions. Our results suggest that the public health implications of these facilities extend beyond the health of employees and incarcerated individuals, and policymakers should explicitly consider the public health concerns posed by these facilities when developing pandemic-response policy.
Prisons, meat-packing plants, nursing homes, and rural health systems have all been identified as structural vulnerabilities to US public health,1 but our understanding of the role of prisons in COVID-19 spread is limited. As of November 30, 2020, at least 252 000 incarcerated individuals (incarcerated persons and detainees) and employees in US prisons and jails tested positive for the coronavirus, and 1450 died.2 Incarcerated individuals are a highly vulnerable population whose barriers to timely health care include requiring incarcerated individuals to pay copays for health care, a practice that is legal in 35 states.3–5 People of color are both disproportionately represented in prisons and disproportionately affected by COVID-19.6–8 Finally, prisons are vital to the economy of many small and midsized towns in America.9 Despite these issues and calls for increased public health interventions in prisons,10 the statistical relationship between prisons and COVID-19 cases and deaths has not been adequately quantified.
Recent work has highlighted the structural vulnerabilities of prisons and the public health risk to the surrounding communities.1 , 11 Incarcerated individuals and employees at prisons are at risk from “crowded dormitories, shared lavatories, limited medical and isolation resources, daily entry and exit of staff members and visitors, continual introduction of newly incarcerated or detained persons, and transport of incarcerated or detained persons in multi-person vehicles.”12(p587) There have been numerous case outbreaks in prisons,5 , 13 particularly during the first wave of the pandemic.14
Prisons are worthy of special public health scrutiny because closing prisons is politically and practically challenging compared with other institutional settings (such as meat-packing plants and schools) that have also been shown to foster COVID-19 outbreaks. Even when prisons are “shut down,” incarcerated individuals and correctional employees remain on-site, and employees typically return to their homes after their shifts. In contrast, meat-packing plant closures have been somewhat successful in slowing outbreak growth, in part because meat-packing plant employees are not on-site.15 The inability to close a prison suggests that containing and slowing an outbreak from a prison may pose a greater challenge. In this light, our finding that outbreak magnitude is increasing in proportion to prison population and capacity has important implications for local public health officials as well as prison facility planning and management.
The evidence we show that prisons are correlated with COVID-19 spread could be of particular use to researchers and policymakers working in rural and suburban contexts. Over 2.1 million people are incarcerated in the United States at any given time; following a surge of prison construction in the 1990s, a disproportionate number of prisons are located in nonmetropolitan areas.9 , 16 , 17 There is a broad literature of community economic development on the impacts of prisons on the communities in which they are located.18 , 19 The existing literature on the public health implications of prisons on the surrounding communities, however, focuses more on public health within the prison populations as opposed to potential spillovers from prisons to the health of the surrounding population. In light of the current pandemic and the salience of these facilities, our work provides vital insight on the intersection between prisons and short- and long-term public health outcomes.
METHODS
We analyzed the presence of state and federal prisons as a correlate of COVID-19 spread by matching data on prison locations and capacities, reported cases and deaths, and county-level demographic and weather controls. Our data extended from January 20, 2020 (the date of the first reported US case) through July 1, 2020; this roughly corresponds to the “first wave” of the outbreak. Our identification came from a selection-on-observables design, using counties without prisons as our control group. This assumes that pre–COVID-19 prison location decisions are orthogonal to outbreak severity after controlling for county-level covariates. We controlled for county-level characteristics that have already been identified in the literature as correlates of COVID-19 spread.15 , 20 This helped to strengthen the quality of our control group and ruled out alternative explanations of a statistical relationship between case load and location of prisons other than the presence and size of the facilities themselves.
We modeled our econometric methods and choices of control variables on existing literature15 , 20; the former provided the core methodology for estimating community-level correlations of COVID-19 cases, and the latter demonstrated the importance of meat-processing plants in community transmission. We estimated the following using ordinary least squares regression:
| (1) |
where Outcomec is the inverse hyperbolic sine transformation of either cases or deaths in county c or is the outbreak delay, defined as the difference between the first reported US case and when cases within the county exceeded 1 per 100 000. (We used the inverse hyperbolic sine transformation to account for zeros. Using data through July 1, 2020, there were 24 counties with 0 cases and 1106 with 0 deaths.) The variable Prisoncis either a binary measure of state or federal prison presence, or a continuous measure of prison capacity (measured in 1000-person increments). Our parameter of interest, β, measures the effects of prisons on the outcome of interest. Each χj is a county-level regressor drawn from the existing COVID-19 literature, including presence of a meat-packing facility, log population, population density, indicators for degree of county urbanness or rurality, population share commuting by public transit and outside the county, population share older than 75 years, population share residing in a nursing home, average daily temperature in February to April 2020, log household median income, the social capital index, and Republican vote share during the 2018 congressional election. We also controlled for the days since first case—that is, the days (measured from July 1) since cases in that county exceeded 1 per 100 000 population. All else being equal, counties with earlier outbreaks will likely have more total cases. We included state fixed effects (γ s) and used robust standard errors in all specifications. Following best practices in the literature, we should not have—and did not—cluster at the state level.21 As we only had 1 observation for each county, we were thus unable to cluster standard errors at the level of treatment (the county), as would otherwise be recommended
We first estimated this relationship between prisons and cases using a pooled approach, analyzing the total number of cases and deaths in each county. In this approach, we truncated data at July 1, 2020, to best predict the effect of prison presence on the first wave of COVID-19. There is reason to believe that after the first wave, the policy landscape became increasingly complicated, making it difficult to disentangle the effect of these facilities from endogenous school shutdowns, university openings, etc. Limiting analysis to the first wave also avoids issues of differential susceptibility as more of the community has full or partial immunity from previous waves. Additionally, the first wave of the pandemic is important to study in and of itself given that a first wave is guaranteed in future pandemics, although subsequent waves are not.
Even after limiting analysis to the first wave of the pandemic, we may have contaminated controls if counties responded to early outbreaks by building testing centers, sourcing ventilators, or adjusting work and school policies, which might bias the results of our pooled sample. To account for this, we estimated Equation 1 using a duration-equalized sample, where we subsampled the data starting 30 days after the initial onset in each county and resampled every 30 days. We defined initial onset as the day that cases first exceeded 1 per 100 000 population. This created a “snapshot” of prison and control counties at the same relative point in the outbreak.
Our identification strategy relied on exogeneity between prison presence and COVID-19 spread and death rate after controlling for other county characteristics. Although the placement of prisons clearly predates COVID-19 and therefore cannot be subject to reverse causality, there are legitimate concerns related to both unobserved heterogeneity and measurement error. However, Taylor and coauthors found that ordinary least squares results are robust to alternative modeling strategies aimed at addressing endogeneity of facility location, including instrumental variables and matching on observables.15 We took this as supportive evidence that prison location is largely exogenous to COVID-19 spread. Our identification rested on the stable unit treatment value assumption, requiring that there were no spatial spillovers between counties with prisons and those without. To control for spatial spillovers, we included measures of the share of the population commuting out of the state and county for work. To the extent that we may not have fully captured spatial spillovers, we expected them to inflate cases and deaths in nontreated counties, biasing our results toward zero. As in all studies with observational data, the identification was imperfect, but, in the most plausible cases, it biased our results toward zero. Our findings are best interpreted as a lower bound for the correlation between prison presence and scale on COVID-19 transmission.
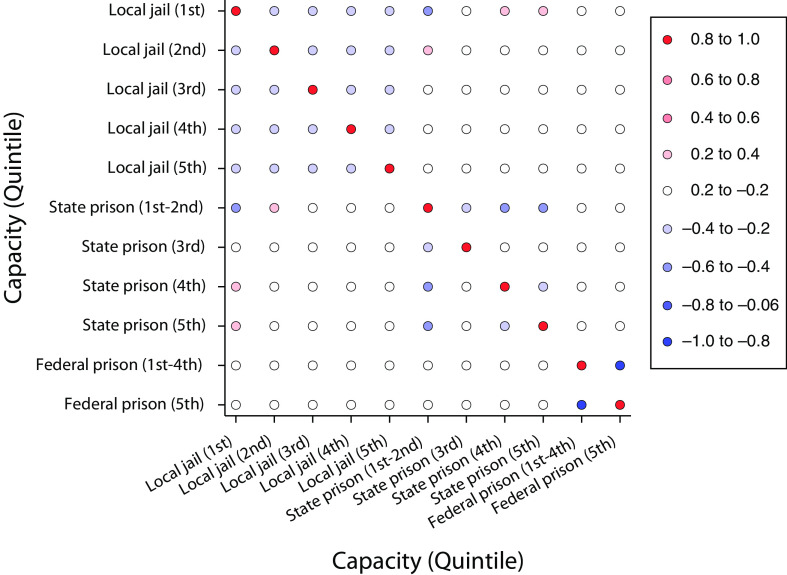
COVID-19 case data came from 2 public data sources. First, we used county-level data on case counts and deaths collected by Johns Hopkins University.22 Second, we used a daily tracker of case counts available through the New York Times.2 We used this second source of case counts in the duration-equalized analysis, following existing work.20 Prison capacities and locations came from the US Department of Homeland Security.23 There are 5808 incarceration facilities in the data, 2100 of which are state or federal facilities. We considered a facility as being present in the county if it had a capacity greater than 0. The data do not include private prisons, which account for roughly 8% of the US prison population.24 Of 3142 counties and county equivalents, 922 had a prison (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Figure 1 presents a correlation matrix of the number of jails and state and federal prisons in a county, which we divided into quintiles by capacity. The presence of a prison of any size was negatively correlated with the presence of a second prison in the same county, which reflects the fact that counties must bid for prison contracts, and being awarded 1 contract decreases the chance of being awarded another. We took this as evidence that prisons were not strongly colocated.
FIGURE 1—
Correlation Scatterplot of Number of Jails and State and Federal Prisons in a County, by Quintiles and Capacity: United States, 2020
Note. The color gradient represents the correlation coefficient. Presence of a state or federal prison is broken up by the total capacity of state or federal prisons within the county. For state prisons, we combine the first and second quintiles, which contain all counties with no prison capacity (54% of counties). For federal prisons, the first through fourth quintiles contain the counties with no prison capacity (93% of counties).
County-level demographic data (population, household median income, share of the population aged 75 years and older, and share of the population commuting by public transit, out of the county, and out of the state) came from the 2018 and 2019 American Community Survey 5-year estimates.25 County land area came from the US Census Bureau. Urban–rural classifications came from the National Center for Health Statistics Urban–Rural Classification Scheme for Counties.26 Population share residing in a nursing home came from the Nursing Home Compare Datasets: Provider Info.27 We used the Social Capital Index, which is a county-level index with mean 0 and standard deviation 1.28 Average daily temperature from February to April came from the National Oceanic and Atmospheric Administration.29 Slaughterhouse and meat processor presence came from the Meat, Poultry and Egg Product Inspection Directory, available through the US Department of Agriculture.30 Republican vote share in the 2018 midterm congressional election came from Stephen Pettigrew.31 Geographic matching used SimpleMaps.32 We report covariate means and standard deviations by whether the county contained a prison (Tables A and B, available as supplements to the online version of this article at https://www.ajph.org). Our final sample consisted of 2979 counties with matched prison presence data and control variables and 1880 counties with matched prison capacity data and control variables. We tested for robustness to this smaller sample in online Table G (available as a supplement to the online version of this article at https://www.ajph.org).
RESULTS
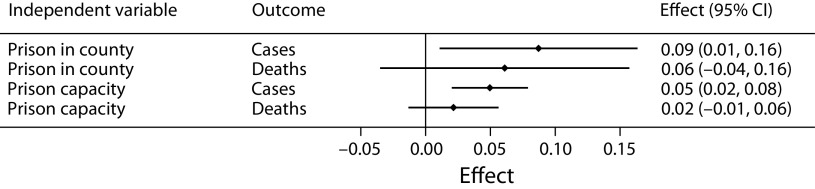
After controlling for covariates, we found that COVID-19 cases were 9% higher in counties with a prison (Figure 2) and that they were increasing in proportion to incarcerated population and total capacity (measured in 1000-person increments). An additional 1000-person capacity is correlated with a 4.96% increase in cases.
FIGURE 2—
Relationship Between State or Federal Prison Presence and Inverse Hyperbolic Sine (IHS)-Transformed Cases or Deaths by Prison Presence and Capacity: United States, 2020
Note. CI = confidence interval. We use ordinary least squares regression to estimate the relationship between state or federal prison presence (a binary indicator equal to 1 if the county does have a state or federal prison) and the number of IHS-transformed COVID-19 cases or deaths.22 Column 1 describes the treatment variable of interest (prison presence or county-level prison capacity in 1000-person increments). Column 2 describes the outcome variable of interest. The points and spikes represent the estimated effect size and 95% confidence interval, whereas the last column states these effect sizes and confidence intervals in numbers. We include state-level fixed effects to account for state policy and economic factors that may be associated with COVID-19 spread. We control for presence of a meat processor within the county, days since cases exceeded 1 per 100 000 population, logged population, population density, urban–rural classification dummies, population share commuting by public transit, population share older than 75 years, population share living in a nursing home, average temperature February to April, logged median household income, the social capital index value, and 2018 midterm Republican vote share.
We found no evidence that prisons were correlated with COVID-19 deaths. Medical researchers and epidemiologists have shown that the causal chain from cases to deaths is complex and can be affected by individual access to health care, preexisting conditions, and hospital capacity, including ventilator access.33 , 34 Health care access may be higher in the vicinity of prisons, as prison employees are typically state or federal employees with health care benefits for themselves and their families. (We are unaware of prison employees being required to report for duty despite being sick, unlike in the meatpacking industry.) Our results highlight the need for a nuanced investigation of the link between prisons and fatal or nonfatal COVID-19 cases.
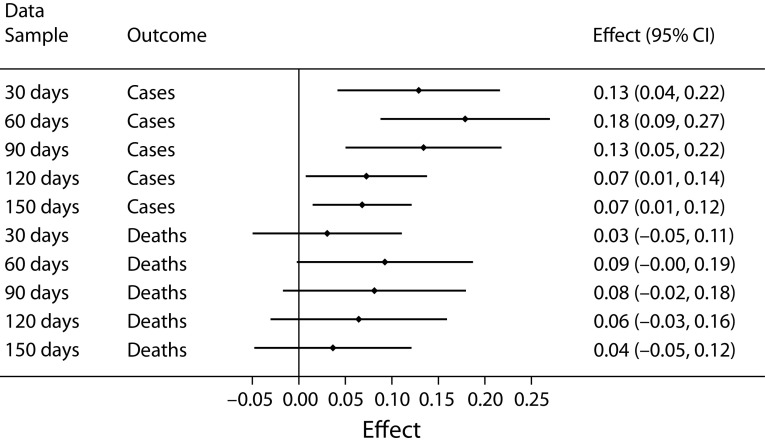
Figure 3 shows that the relationship between prison presence and COVID-19 cases was robust to different outbreak duration choices. Prison presence corresponded to an 11% increase in cases after 30 days and a 16% increase after 60 days, both of which were larger effects than in the pooled sample. The result plateaued after 120 days, supporting our choice of the July 1 cutoff.
FIGURE 3—
Relationship Between State or Federal Prison Presence and Inverse Hyperbolic Sine (IHS)-Transformed Cases or Deaths by Days Since Outbreak: United States, 2020
Note. CI = confidence interval. We use ordinary least squares regression to estimate the relationship between state or federal prison presence (using binary indicator equal to 1 if the county does have a state or federal prison) and IHS-transformed cases or deaths using a duration-equalized sample of counties a certain number of days since outbreak onset.35 Column 1 indicates the number of days since outbreak onset in that county. Column 2 indicates the outcome variable of interest. The points and spikes represent the estimated effect size and 95% confidence interval, whereas the last column states these effect sizes and confidence intervals in numbers. We include state-level fixed effects to account for state policy and economic factors that may be associated with COVID-19 spread. We control for presence of a meat processor within the county, logged population, population density, urban–rural classification dummies, population share commuting by public transit, population share older than 75 years, population share living in a nursing home, average temperature February to April, logged median household income, the social capital index value, and 2018 midterm Republican vote share.
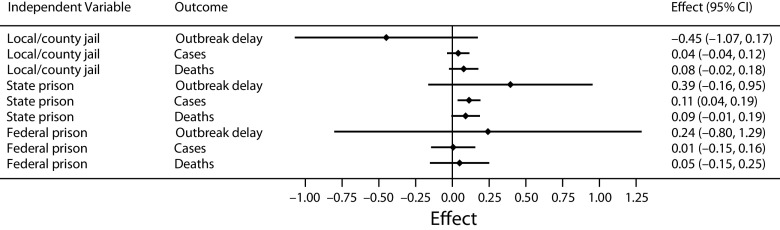
We investigated the relationship of federal prisons, state prisons, and jails with COVID-19 outcomes in Figure 4 and Table G (available as a supplement to the online version of this article at https://www.ajph.org). When we included jails, we found no evidence that counties with a prison or jail had larger outbreaks than counties with neither. Considering each type of facility separately, we found that cases were 11% higher in counties with a state prison, whereas cases were no higher in counties with a federal prison or a jail. The weak relationship between jails and cases was likely due to attenuation bias, since 61.2% of all counties had at least 1 jail or prison, whereas only 31% of counties had a state or federal prison. The null result for federal prisons suggests that the federal prison lockdown, which went into effect on April 1, 2020, may have been successful in slowing COVID-19 spread in and around prisons.36 , 37
FIGURE 4—
Relationship Between Prisons or Jail Presence by Governance Type and Either COVID-19 Outbreak Delay, Inverse Hyperbolic Sine (IHS)-Transformed Cases, or IHS-Transformed Deaths: United States, 2020
Note. CI = confidence interval. We use ordinary least squares regression to estimate the relationship between prisons or jail presence by governance type (a binary indicator equal to 1 if the county has a jail, state prison, or federal prison) and either COVID-19 outbreak delay (days since cases exceeded 1 per 100 000 population in the county), IHS-transformed cases, or IHS-transformed deaths.22 Column 1 describes the treatment variable of interest (a binary indicator for whether the county has a jail, a state prison, or a federal prison). Column 2 describes the outcome variable of interest. The points and spikes represent the estimated effect size and 95% confidence interval, whereas the last column states these effect sizes and confidence intervals in numbers. We include state-level fixed effects to account for state policy and economic factors that may be associated with COVID-19 spread. We control for presence of a meat processor within the county, days since cases exceeded 1 per 100 000 population, logged population, population density, urban–rural classification dummies, population share commuting by public transit, population share older than 75 years, population share living in a nursing home, average temperature February to April, logged median household income, the social capital index value, and 2018 midterm Republican vote share.
DISCUSSION
We found that the presence of a prison corresponded with a 9% increase in cases within the county. Cases increased with the capacity of the prison, and federal and state prisons were stronger correlates of case counts than local and county jails (hereafter, “jails”). We conclude that both the presence and scale of incarceration facilities matter for disease spread.
We calculated a back-of-the-envelope estimate of US COVID-19 cases associated with presence of prisons. In our data, there were 2 653 050 confirmed COVID-19 cases as of July 1, 2020. As we expected the effects of prisons to be particularly important for rural and suburban communities, we calculated these associated cases for each of the rural–urban classification groups. Using the coefficients from Figure 2, we found that 132 582 cases (4.9% of all cases as of July 1) were associated with prisons, with the greatest number of associated cases found in larger, more metropolitan areas. These numbers are smaller than those found in studies looking at the Sturgis Motorcycle Rally superspreader event (in August 202038) and at meat processors15 but are still sizable and important. This is particularly true when we consider the opt-in nature of these large superspreader events, in contrast to the absence of choice that incarcerated individuals have in where they are incarcerated and how correctional facilities respond to transmission risk.
Next, we accounted for heterogeneity in the effect by urban–rural classification. Table K (available as a supplement to the online version of this article at https://www.ajph.org) uses the coefficients from 3 separate regressions of prisons on case counts, split by urban–rural classification (regression results are reported in Table J, available as a supplement to the online version of this article at https://www.ajph.org). Increases in prison capacity are correlated with increases in cases in all classifications. However, smaller counties have smaller capacity prisons, on average, and the dummy for prison presence is only significant in large, urban counties. Less than 1% of micropolitan or noncore cases are associated with prison presence, whereas the population share in large central or fringe counties is over 16%, or 300 903 cases.
Finally, we used the coefficient estimates from our main specification to conduct a back-of-the-envelope calculation of the number of spillover cases beyond those in prison outbreaks themselves. We collected state-level cumulative totals of the number of cases and deaths among incarcerated individuals and corrections officers and staff around July 1, 2020 (data collected by the Marshall Project16). (Some states did not report on exactly July 1, 2020, so data comes from June 28 to July 3.) We then compared the number of cases and deaths in prisons to the estimated cases associated with prisons to estimate the spillover of cases beyond 6 prison environments. We estimated a total spillover of 95 055 cases and 3336 deaths across all 50 states (excluding the District of Columbia, for which prison-specific case and death data were not available). We take this as suggestive evidence that the effects of prisons on COVID-19 transmission extends beyond cases and deaths among incarcerated individuals and corrections officers and staff.
Limitations
Despite the significant results presented here, there are limitations when using data on COVID-19 case counts and deaths. Testing is inconsistent throughout the United States, and shortages of tests have made it difficult for individuals exhibiting symptoms to get tested.39 This is exacerbated by the fact that asymptomatic carriers are often unlikely to be tested at all, making reported case counts a noisy proxy for the true level of cases.
Pertinent to our work, testing protocol in prisons varied significantly across states and facilities. In late April, some facilities began testing all incarcerated individuals, whereas others had stopped testing altogether.40 We cannot rule out that the spike in cases we detected was influenced by large-scale testing in the prisons. However, we detected a significant increase in cases 30 days after outbreak onset, which is before the earliest reported mass testing in prison for the median county. Moreover, we found a difference up to 150 days after the outbreak onset, suggesting continued cases beyond an initial testing spike. Finally, our estimate of prison-related cases exceeds the actual number of cases in prisons, suggesting spread from prisons to the surrounding community.
Finally, we interpret our results as correlational evidence of the relationship between these facility types and COVID-19 spread, rather than causal evidence. Although the location decision for prisons should be exogenous to county-level spread, future work is needed to strengthen this causal link. As data become available, especially at an individual level, researchers may distinguish between the risk of prison presence and the risk of proximity to a prison.
CONCLUSION
We present the first empirical evidence that prisons are strongly correlated with COVID-19 case counts. The relationship is robust to multiple specifications and is increasing in prison capacity. Our results highlight public health concerns in suburban and rural America with respect to the presence and scale of prison facilities. Although economies of scale exist in general for prisons in terms of profitability and cost-effectiveness and for local policymakers in terms of job creation, we found evidence that public health risk is higher around larger facilities. These counties may also need proportional public health infrastructure to cope with potential adverse outcomes.
Our results suggest that coordinated responses, particularly closures, may be effective in slowing the spread of outbreaks in and around prisons. Prisons, in conjunction with small or underfunded local hospitals, may make rural outbreaks worse or unmanageable. Community leaders will want to consider the role of prisons when developing response plans for outbreaks of communicable disease. Such response plans should include the spatial distribution of personal protective equipment, equipment such as ventilators, and general prevention funds, making specific considerations for the safety of incarcerated individuals, prison employees, and their families. Coordination between prison and public health officials on mitigation strategies is vital to keeping these essential institutions functional.
Finally, this work speaks to structural vulnerabilities of the US health care system that are deserving of the focus of policymakers. The impact of COVID-19 in these facilities—and the impact of these facilities on their wider communities—underscores how unprepared US health care and carceral systems are for global health crises.
ACKNOWLEDGMENTS
We thank Sakina Shibuya for creating the maps used in the article and Matthew Kures for assistance with finding data on commuting patterns. We thank attendees of the University of Wisconsin-Madison Applied Economics seminar and Midwest Economics Association annual conference for their feedback.
CONFLICTS OF INTEREST
The authors do not report any conflicts of interest.
HUMAN PARTICIPANT PROTECTION
No human participants were involved in this study. All data were publicly accessible county-level aggregates.
Footnotes
REFERENCES
- 1.Solis J, Franco-Paredes C, Henao-Martínez AF, Krsak M, Zimmer SM. Structural vulnerability in the US revealed in three waves of COVID-19. Am J Trop Med Hyg. 2020;103(1):25–27. doi: 10.4269/ajtmh.20-0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.New York Times. 2020. https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html#clusters
- 3.Eisen LB. Charging Inmates Perpetuates Mass Incarceration. New York, NY: Brennan Center for Justice; 2015. [Google Scholar]
- 4.Coll S. The jail health-care crisis. New Yorker. February 25, 2019. https://www.newyorker.com/magazine/2019/03/04/the-jail-health-care-crisis
- 5.Carissimo J. CDC report details extent of coronavirus outbreaks in US jails and prisons. CBS News. May 6, 2020. https://www.cbsnews.com/news/coronavirus-outbreaks-jails-prisons-cdc-report-covid-19
- 6.Moore JT, Ricaldi JN, Rose CE, et al. Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020—22 states, February–June 2020. Morb Mortal Wkly Rep. 2020;69(33):1122–1126. doi: 10.15585/mmwr.mm6933e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oppel RA, Jr, Gebeloff R, Lai KKR, Wright W, Smith M. The fullest look yet at the racial inequity of coronavirus. New York Times. July 5, 2020. https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html
- 8.The Sentencing Project. 2018. https://www.sentencingproject.org/ publications/un-report-on-racial-disparities
- 9.King R, Mauer M, Huling T. 2003. http://prison.ppjr.org/files/tracy%20huling%20 prisons%20economy%20study.pdf
- 10.Auerbach J, Miller BF. COVID-19 exposes the cracks in our already fragile mental health system. Am J Public Health. 2020;110(7):969–970. doi: 10.2105/AJPH.2020.305699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen PN. The COVID-19 epidemic in rural US counties. Eur J Environ Public Health. 2020;4(2):em0050. [Google Scholar]
- 12.Wallace M, Hagan L, Curran KG, et al. COVID-19 in Correctional and Detention Facilities. Atlanta, GA: US Dept of Health and Human Services, Center for Disease Control and Prevention; 2020. p. 19. [Google Scholar]
- 13.Blakinger K. 2020. https://www.themarshallproject.org/2020/04/15/what-happens-when-more-than-300-000-prisoners-are-locked-down
- 14.The Marshall Project. 2020. https://www.themarshallproject.org/2020/05/01/a-state-by-state-look-at-coronavirus-in-prisons#prisoner-cases
- 15.Taylor CA, Boulos C, Almond D. Livestock plants and COVID-19 transmission. Proc Natl Acad Sci USA. 2020;117(50):31706–31715. doi: 10.1073/pnas.2010115117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beale CL. Rural prisons: an update. Rural Development Perspectives. 1996;11(2):1992–1994. [Google Scholar]
- 17.Bureau of Justice Statistics. 2018. https://www.bjs.gov/index.cfm?ty=kfdetail&iid=487
- 18.Eason J. Mapping prison proliferation: region, rurality, race and disadvantage in prison placement. Soc Sci Res. 2010;39(6):1015–1028. doi: 10.1016/j.ssresearch.2010.03.001. [DOI] [Google Scholar]
- 19.Genter S, Hooks G, Mosher C. Prisons, jobs and privatization: the impact of prisons on employment growth in rural US counties, 1997–2004. Soc Sci Res. 2013;42(3):596–610. doi: 10.1016/j.ssresearch.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Desmet K, Wacziarg R. 2020. http://www.nber.org/papers/w27329
- 21.Abadie A, Athey S, Imbens G, Wooldridge J. 2017. http://arxiv.org/abs/1710.02926
- 22.Johns Hopkins University. 2020. https://github.com/CSSEGISandData/COVID-19/tree/master/csse_covid_19_data/csse_covid_19_daily_reports_us
- 23.US Dept of Homeland Security. 2020. https://hifld-geoplatform.opendata.arcgis.com/datasets/prison-boundaries/explore
- 24.The Sentencing Project. 2019. https://www.sentencingproject.org/publications/private-prisons-united-states
- 25.US Census Bureau. 2018. https://www.census.gov/programs-surveys/acs
- 26.National Center for Health Statistics. 2020. https://www.cdc.gov/nchs/data_access/urban_rural.htm
- 27.Centers for Medicare & Medicaid Services. 2020. https://data.medicare.gov/data/nursing-home-compare [PubMed]
- 28.Rupasingha A, Goetz SJ, Freshwater D. The production of social capital in US counties. J Socio-Econ. 2006;35(1):83–101. doi: 10.1016/j.socec.2005.11.001. [DOI] [Google Scholar]
- 29.National Centers for Environmental Information. 2020. https://www.ncdc.noaa.gov/cag/county/mapping
- 30.Food Safety and Inspection Service. 2020. https://www.fsis.usda.gov/inspection/establishments/meat-poultry-and-egg-product-inspection-directory
- 31.Pettigrew S. 2018. [DOI]
- 32.SimpleMaps. 2020. https://simplemaps.com/data/us-cities
- 33.Imam Z, Odish F, Gill I, et al. Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States. J Intern Med. 2020;288(4):469–476. doi: 10.1111/joim.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Imam Z, Odish F, Armstrong J, et al. Independent correlates of hospitalization in 2040 patients with COVID-19 at a large hospital system in Michigan, United States. J Gen Intern Med. 2020;35(8):2516–2517. doi: 10.1007/s11606-020-05937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.New York Times. 2020. https://github.com/nytimes/covid-19-data
- 36.Gerstein J. 2020. https://www.politico.com/news/2020/04/01/federal-prisons-start-14-day-lockdown-to-fight-virus-158937
- 37.Hummer D. United States Bureau of Prisons’ response to the COVID-19 pandemic. Victims & Offenders. 2020;15(7-8):1262–1276. doi: 10.1080/15564886.2020.1829765. [DOI] [Google Scholar]
- 38.Dave D, Friedson AI, Sabia JJ, Dave D, Friedson AI. 2020.
- 39.Abbott BB, Lovett I. Covid-19 test shortages prompt health authorities to narrow access. Wall Street Journal. 2020. https://www.wsj.com/articles/covid-19-test-shortages-prompt-health-authorities-to-narrow-access-11595515592
- 40.Aspinwall C, Neff J. 2020. https://www.themarshallproject.org/2020/04/24/these-prisons-are-doing-mass-testing-for-covid-19-and-finding-mass-infections