Abstract
Objectives. To examine changes in abortions in Louisiana before and after the COVID-19 pandemic onset and assess whether variations in abortion service availability during this time might explain observed changes.
Methods. We collected monthly service data from abortion clinics in Louisiana and neighboring states among Louisiana residents (January 2018‒May 2020) and assessed changes in abortions following pandemic onset. We conducted mystery client calls to 30 abortion clinics in Louisiana and neighboring states (April‒July 2020) and examined the percentage of open and scheduling clinics and median waits.
Results. The number of abortions per month among Louisiana residents in Louisiana clinics decreased 31% (incidence rate ratio = 0.69; 95% confidence interval [CI] = 0.59, 0.79) from before to after pandemic onset, while the odds of having a second-trimester abortion increased (adjusted odds ratio [AOR] = 1.91; 95% CI = 1.10, 3.33). The decrease was not offset by an increase in out-of-state abortions. In Louisiana, only 1 or 2 (of 3) clinics were open (with a median wait > 2 weeks) through early May.
Conclusions. The COVID-19 pandemic onset was associated with a significant decrease in the number of abortions and increase in the proportion of abortions provided in the second trimester among Louisiana residents. These changes followed service disruptions.
The COVID-19 pandemic has had clear direct effects on people’s health.1 Yet, pandemics can also have an impact on the health of populations indirectly.2 For example, pandemics can disrupt health care delivery systems and use of health services, thereby indirectly affecting health.3–6 Research to date on indirect effects of the COVID-19 pandemic has focused on changes in primary care utilization7 and care disruptions for infectious diseases such as HIV and tuberculosis and for childhood vaccination.8–11 Research also indicates that people were experiencing scheduling and financial barriers to reproductive health services because of the COVID-19 pandemic, including delays to care or canceled appointments in addition to concerns about ability to afford contraceptive methods.12
The COVID-19 pandemic may have influenced availability and use of abortion care, in particular. Commentaries have focused on state designations of abortion as a nonessential service in Texas and several other US states in March and April 2020.13–15 Less research has focused empirically on changes in number, type, and timing of abortions during the pandemic. One study explored experiences of 103 independent abortion clinics in the early months of the pandemic.16 This study showed that, while clinics in all regions were affected by the pandemic and by general public health responses to the pandemic, more facilities in the South and Midwest temporarily closed, canceled, or postponed abortion services.16 Another study found a 27% increase in the rate of medication abortion requests to an online provider, with statistically significant increases in Louisiana, among other states.17 This suggests a decrease in availability of clinic-based abortions or other barriers to obtaining facility-based abortion care. A study in Texas examined changes in number and timing of abortions during the period Texas designated abortion a nonessential service. This study showed that the number of abortions in Texas decreased and the number of Texas residents obtaining abortions in neighboring states increased.18
It is not yet known, though, whether other states experienced changes in number and timing of abortions following pandemic onset. This information is important, as previous research suggests that multiple factors—including pandemic-related abortion bans, pre-existing restrictive abortion policies, the pandemic itself (i.e., clinicians and staff getting sick), and general public health responses to the pandemic—have contributed to disruptions in the abortion care delivery system.16 Examining whether other states have experienced changes in abortions is especially relevant in light of a January 2021 US Supreme Court ruling that reinstated a prohibition on mailing medication abortion pills. In this case, the federal government cited data from 2 states that indicated that the number of total abortions had increased during the pandemic and thus argued that access to abortion had not been limited.19
Examining changes in abortions in Louisiana during the COVID-19 pandemic can help answer outstanding questions regarding whether and where the number and timing of abortions changed during the early months of the pandemic. Focusing on Louisiana is relevant, as Louisiana was an early COVID-19 hotspot.20 Also, while Louisiana did not officially designate abortion a nonessential service,21 Louisiana’s official statement about which health facilities were deemed essential (in effect from March 21‒May 1, 2020)14 was ambiguously worded22 and, thus, may have resulted in service disruptions as abortion clinics navigated their legal rights to remain open.
Documenting changes in the number, type, and timing of abortions is vital to better understand the pandemic’s indirect health impacts. Such measures are important, as being unable to obtain a wanted abortion has significant adverse consequences on the health and well-being of women, children, and families,23–26 and, although second-trimester abortion is very safe, delays in abortion care can increase risk of complications.27 , 28 Risks associated with continuing an unwanted pregnancy may also be especially relevant during the pandemic.29–34 As a way to reduce risks from in-person contact during the pandemic, many professional health associations have endorsed innovations in medication abortion delivery that eliminate clinic visits.35 , 36 Thus, the relative proportion of each abortion method may shift during the pandemic.
We examined changes in abortions among Louisiana residents in the early months of the COVID-19 pandemic compared with previous years, as well as changes in abortion service availability. Specifically, we aimed to (1) examine changes in number, type, and timing of abortions among Louisiana residents from before to during the early months of the pandemic and (2) describe availability of abortion services in Louisiana and 3 neighboring states during the early months of the pandemic to explore whether variations in abortion service availability in these states might explain any observed changes in abortions.
METHODS
We obtained data on all abortions provided in Louisiana’s 3 abortion clinics between January 1, 2018, and May 31, 2020, as part of data collection for a separate study. University of California, San Francisco, research assistants abstracted data from the Induced Termination of Pregnancy (ITOP) forms that the state of Louisiana requires for all abortions provided in Louisiana. We also obtained monthly data on abortions provided to Louisiana residents at all clinics in Arkansas and Mississippi and at 17 of 24 open facilities in Texas, which provided 93% of all abortions in Texas.37 Arkansas, Mississippi, and Texas facilities provided the study team with information on Louisiana residents obtaining care at their location between September 2018 and May 2020, based on their administrative records.
We obtained data on whether abortion clinics were open and scheduling abortion appointments through mystery calls to all publicly advertised clinics38 between April 2, 2020, and July 8, 2020, in Louisiana and 3 neighboring states (Arkansas, Mississippi, and Texas) where we anticipated Louisiana residents might obtain abortions. The University of California, San Francisco, study team made calls weekly in April and biweekly in May and early June, and placed final calls the first week of July. For each week of calls, research assistants called each clinic up to 3 times over 3 consecutive days or until successful contact was made (whichever occurred first) between 9 am and 5 pm in that clinic’s time zone. A similar protocol was used for Texas clinics, although precise timing of calls differed; another study team was already conducting a mystery call study in Texas, and we did not want to burden Texas clinics with duplicate efforts.
Measures
Abortion data from Louisiana and neighboring states included 3 outcomes: (1) Total abortions was the number of abortions provided per month, (2) medication abortion was the number of medication abortions (vs other types of abortion) per month, and (3) trimester was the number of abortions provided in the second versus first trimester (≥ 12 weeks vs < 12 weeks) per month.
We created additional variables for analyses. COVID-19 pandemic was a dichotomous variable identifying whether the abortion was provided before versus after pandemic onset. We used March 2020 as pandemic onset for total abortions and medication abortion analyses, as March was when the first shelter-in-place orders were imposed.39 We used April 2020 for trimester analyses to allow time for the delay to appear. Time was continuous of months beginning in January 2018. Postpandemic onset time was 0 for months January 2018 through February 2020 and continuous (1, 2, 3) beginning March 2020, delayed by 1 month for trimester analyses. Season was a categorical variable of which quarter (January‒March, April‒June, July‒September, October‒December) the abortion occurred to account for seasonal trends in abortion.40
Mystery client data included the following variables: Open and scheduling was a dichotomous variable of whether a clinic was open and scheduling appointments versus whether a clinic was either closed or open but not scheduling appointments. If a clinic did not answer after 3 call attempts, a clinic was considered closed or not scheduling. Wait time was a continuous variable of number of days to the clinic’s next available preabortion consultation visit required by the state. Abortion type was a categorical variable of types of first-trimester abortions the clinic was providing (medication abortion only, aspiration abortion only, or both).
Analysis
We first examined abortion data descriptively to compare numbers of abortions and percentages of second-trimester and of medication abortions across years and across comparative months of March to May in 2018, 2019, and 2020. We then analyzed abortion data by using segmented regression, a method for interrupted time-series analyses,41 using generalized linear models with Poisson link functions for count data (i.e., total abortions) and logit link for binary data of medication and second-trimester abortions. The goal of the modeling was to assess whether there was a change in abortions at pandemic onset and then whether the trend in abortions changed after pandemic onset. In each case, we first estimated a regression model with only the main predictor of COVID-19 pandemic and the relevant outcome (e.g., number of abortions per month) over the 29-month study period. We then included variables for time and for postpandemic onset time and, in a separate model, then added the variable for season. Final segmented regression models included COVID-19 pandemic, time, postpandemic time, and season. We also assessed whether findings varied if we removed the season variable and allowed for a 1-month autocorrelation. Findings were substantively similar when we used this alternative modeling approach.
Primary analyses focused on abortions among Louisiana residents in Louisiana clinics. Secondary analyses focused on abortions among Louisiana residents in Louisiana clinics and in clinics in neighboring states of Arkansas, Mississippi, and Texas. We used the postestimation margins commands in Stata version 15 (StataCorp LP, College Station, TX) to obtain predictions of changes in outcomes, and used the predict command to graph relevant output by month, adjusting for seasonality. Then, using the mystery call data, we computed the proportion of clinics that were open and scheduling and the proportion offering different types of first-trimester abortion (medication or aspiration), as well as median and range of wait times. S. C. M. R. and N. F. B. conducted analyses.
RESULTS
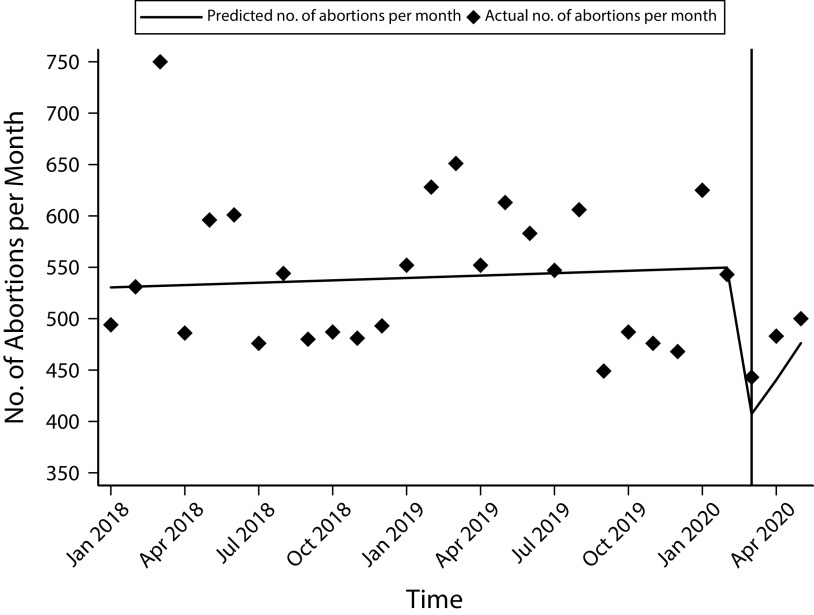
There were 6419 abortions among Louisiana residents at Louisiana clinics in 2018 and 6612 in 2019. Comparing the 3-month period March through May across years, there were 1832 abortions in 2018, 1816 in 2019, and 1426 in 2020. Segmented regression indicated a 31% decrease in total abortions at pandemic onset (COVID-19 pandemic incidence rate ratio [IRR] = 0.69; 95% confidence interval [CI] = 0.59, 0.79; P < .001). The model adjusted mean number of abortions was 558 abortions per month before pandemic onset and 382 abortions per month in the 3 months following. Total abortions increased from March through May 2020 (postpandemic onset time IRR = 1.08; 95% CI = 1.01, 1.15; P = .03; Figure 1 and Table 1).
FIGURE 1—
Actual and Predicted Number of Abortions Among Louisiana Residents in Louisiana Clinics per Month: January 2018‒May 2020
Note. Vertical line indicates March 2020. The black trend line reflects the predicted values at the average season.
TABLE 1—
Segmented Regressions Predicting Changes in the Total Number, Timing, and Type of Abortions Related to the COVID-19 Pandemic Among Louisiana Residents Obtaining Care in Louisiana: January 2018–May 2020
| Total Abortions, IRRa (95% CI) | Medication Abortions, AOR (95% CI) | Second-Trimester Abortions,b AOR (95% CI) | |
| COVID-19 pandemicc | 0.69 (0.59, 0.79) | 0.61 (0.44, 0.84) | 1.91 (1.10, 3.33) |
| Time | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.01) | 1.00 (0.99, 1.01) |
| Postpandemic onset time | 1.08 (1.01, 1.15) | 0.96 (0.83, 1.11) | 0.95 (0.68, 1.32) |
| Season | |||
| Jan‒Mar (Ref) | 1 | 1 | 1 |
| Apr‒Jun | 0.96 (0.92, 1.01) | 1.49 (1.36, 1.63) | 0.71 (0.62, 0.81) |
| Jul‒Sep | 0.87 (0.83, 0.91) | 1.36 (1.24, 1.49) | 0.87 (0.76, 1.00) |
| Oct‒Dec | 0.80 (0.77, 0.84) | 1.30 (1.18, 1.43) | 0.81 (0.71, 0.94) |
Note. AOR = adjusted odds ratio; CI = confidence interval; IRR = incidence rate ratio.
The analysis of total abortions was assessed using Poisson models, generating IRRs. The analyses of second-trimester and medication abortions were assessed with logistic regression models, generating AORs.
Analyses for change in second-trimester abortions used before versus after April 2020 for the designation of COVID-19 pandemic and postpandemic time, whereas analyses for change in total abortions and medication abortions used before versus after March 2020.
COVID-19 pandemic designates whether the abortion was provided before or after the onset of the COVID-19 pandemic; time refers to months since January 2018; postpandemic time refers to months after the onset of the pandemic.
In 2018 and 2019, 42% of abortions among Louisiana residents in Louisiana clinics were medication abortions. Comparing the March-through-May period across years, 43% of abortions were medication abortions in 2018 and 2019, and 31% in 2020. Using segmented regression, this difference was statistically significant (COVID-19 pandemic adjusted odds ratio [AOR] = 0.61; 95% CI = 0.44, 0.84; P = .003).
In 2018 and 2019, 11% to 12% of abortions among Louisiana residents in Louisiana clinics were in the second trimester. When we compared the April-through-May period across years, 10% of abortions were in the second trimester in 2018 and 2019 and 17% in 2020. In April through May 2018, there were 974 first-trimester and 107 second-trimester abortions; in April through May 2019, there were 1039 first-trimester and 119 second-trimester abortions; and in April through May 2020, there were 818 first-trimester and 163 second-trimester abortions. When we used segmented regression, there were higher odds of an abortion occurring in the second trimester after (vs before) April 2020 (COVID-19 pandemic AOR = 1.91; 95% CI = 1.10, 3.33; P = .02).
Analyses of the number, timing, and type of abortions among Louisiana residents at Arkansas, Louisiana, Mississippi, and Texas clinics September 2018 through May 2020 showed similar results (Table A, available as a supplement to the online version of this article at http://www.ajph.org). That the findings for Louisiana residents in Louisiana plus neighboring states were consistent with the main analyses reflects the lack of underlying change in the number of Louisiana residents obtaining abortions in Arkansas, Mississippi, and Texas (209 in March‒May 2019 and 193 in March‒May 2020).
Abortion Service Availability
In early April 2020, 33% of the 30 abortion clinics were open and scheduling abortion appointments, with a median wait of 7 days (range = 0‒27). By the end of April, this increased to 67%, with a median wait of 10.5 days (range = 3‒19). These measures remained relatively steady through July (Table 2). During the first 3 weeks of April, most open and scheduling clinics (range = 70%‒80%) offered only medication abortion, while remaining clinics offered both medication and aspiration abortions. By the last week of April, the proportion of open and scheduling clinics offering only medication abortion had decreased to 50% and, by early May, had decreased to 27%; this remained relatively steady through July. Only 1 clinic in June and 1 in July offered aspiration abortion only (not shown).
TABLE 2—
Open Clinics and Waiting Time for an Abortion Appointment by State and by Week: Arkansas, Louisiana, Mississippi, and Texas, April‒July 2020
| No. of Clinics in State | % (No.), Median (Range), or % | ||||||||
| Apr 2 | Apr 9 | Apr 16 | Apr 23 | May 7 | May 21 | Jun 4 | Jul 2 | ||
| % open and scheduling (no. of open clinics) | |||||||||
| AR | 2 | 50 (1) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) |
| LA | 3 | 33 (1) | 33 (1) | 67 (2) | 33 (1) | 67 (2) | 33 (1) | 100 (3) | 33 (1) |
| MS | 1 | 100 (1) | 100 (1) | 100 (1) | 100 (1) | 100 (1) | 100 (1) | 100 (1) | 100 (1) |
| TXa | 24 | 29 (7) | 25 (6) | 38 (9) | . . . | 88 (21) | . . . | 75 (18) | 71 (17) |
| Total | 30 | 33 (10) | 33 (10) | 47 (14) | 67a (4) | 87 (26) | 67a (4) | 80 (24) | 70 (21) |
| Median wait time in days at open and scheduling clinics | |||||||||
| AR | 7 (7‒7) | 12 (10‒14) | 10 (7‒13) | 10 (3‒17) | 14 (7‒21) | 13 (5‒20) | 3 (1‒5) | 8 (6‒9) | |
| LA | 19 (19‒19) | 21 (21‒21) | 22 (19‒24) | 19 (19‒19) | 16 (12‒20) | 8 (8‒8) | 12 (9‒12) | 8 (8‒8) | |
| MS | 4 (4‒4) | 12 (12‒12) | 7 (7‒7) | 4 (4‒4) | 9 (9‒9) | 13 (13‒13) | 13 (13‒13) | 17 (17‒17) | |
| TXa | 7 (0‒27) | 8 (0‒23) | 3 (1‒25) | . . . | 8 (0‒21) | . . . | 6 (1‒13) | 6 (0‒20) | |
| Total | 7 (0‒27) | 12 (0‒23) | 6 (1‒25) | 10.5a (3‒19) | 8 (0‒21) | 10.5a (5‒20) | 6 (1‒13) | 6 (0‒20) | |
| % of open and scheduling clinics providing only medication abortion | |||||||||
| AR | 0 | 100 | 50 | 100 | 50 | 50 | 50 | 50 | |
| LA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| MS | 0 | 0 | 100 | 0 | 0 | 0 | 0 | 0 | |
| TXa | 100 | 100 | 100 | . . . | 29 | . . . | 28 | 18 | |
| Total | 70 | 80 | 79 | 50a | 27 | 25a | 25 | 19 | |
Calls in Texas were not made during the weeks of Apr 23 and May 21, so the denominator is 6 in those weeks.
Service availability varied across states. In Arkansas and Mississippi, all clinics were open and scheduling for nearly the entire study period. In Louisiana and Texas, fewer than half of clinics were open and scheduling at multiple time points. In Louisiana, typically 1 or 2 of the state’s 3 clinics were open and scheduling in March, April, May, and July. In Texas, while fewer than half of clinics were open and scheduling in April, most were open by May. Similarly, median wait times varied by state. The median wait in Louisiana was greater than 2 weeks through the beginning of May; median waits in Arkansas and Mississippi were typically greater than 1 week; median waits in Texas were approximately 1 week. By contrast with clinics in other states, Louisiana clinics provided both medication and aspiration abortion when they were open and scheduling throughout the study time period.
Posthoc Analysis of Medication Abortion
That the proportion of medication abortions decreased after pandemic onset appeared counterintuitive given that mystery calls indicated that the majority of clinics were providing medication abortion only in the first months following pandemic onset. A posthoc exploration of changes in total abortions and medication abortions at Louisiana clinics found the decrease in abortions was concentrated among 2 clinics, where there was a 42% decrease in abortions. By contrast, the third clinic (which was the only one open and scheduling at all mystery call time points) had a 17% increase in abortions. Unlike most other clinics in the sample, this clinic provided both aspiration and medication abortions throughout the mystery call period. In the 2 clinics where the reduction in total abortions was concentrated, more than half of abortions in 2018 and 2019 were medication abortions, whereas in the clinic that remained open and scheduling and saw the increase in abortions, only 12% of abortions in 2018 and 2019 were medication abortions. Rather than indicating a decrease in medication abortions within clinics, the data indicate a shift in where Louisiana residents obtained care in the early months of the pandemic (i.e., more obtained care at the single clinic that typically provided more aspiration than medication abortions).
DISCUSSION
This study showed that onset of the COVID-19 pandemic was associated with a 31% reduction in the number of abortions in Louisiana and an increase in the proportion of abortions provided in the second trimester. This pattern of findings is similar to changes observed in Texas.18 These findings indicate that changes in the number and timing of abortions during the pandemic occurred not only because of an explicit executive order ban in Texas but also in the context of an ambiguously worded executive order in an early pandemic hotspot. By contrast with the Texas study,18 however, we did not observe a corresponding increase in clinic-based abortions among Louisiana residents in neighboring states, nor did we observe a rapid increase in the number of abortions in May after Louisiana’s executive order was no longer in effect. Future research should examine whether other states in different abortion-policy and COVID-19 contexts experienced similar changes in abortion in the early months of the pandemic.
Previous research has shown that most abortion clinics continued to provide abortion care in the early months of the pandemic, with more service disruptions occurring in the Midwest and South.16 This study echoes those findings, as it highlights significant service disruptions in Louisiana and neighboring states. Mystery call data indicate that Louisiana and Texas abortion clinics experienced more notable disruptions than clinics in Arkansas and Mississippi. While the service delivery system in Texas rebounded by May when the state’s executive order ban ended,42 disruptions persisted in Louisiana until July. As the changes in number and timing of abortions in Louisiana followed these service disruptions in March through May 2020, changes in number and timing of abortions in Louisiana may also have persisted beyond May 2020; this should be examined in future research.
In April, most clinics we called reported offering only medication abortion, consistent with other research,16 although this was not the case in Louisiana where open clinics consistently offered both medication and aspiration abortion. That most of the clinics in Arkansas, Mississippi, and Texas offered only medication abortion in April underscores the ongoing importance of medication abortion in the abortion care delivery system, particularly when limiting in-person contact is key. During the pandemic, a federal judicial ruling temporarily allowed clinicians to provide medication abortion by telemedicine and mail medications directly to patients.43 This was not possible, however, in states with laws that ban telemedicine for abortion care, such as the states in this study.44 Our posthoc analyses indicate that decreases in medication abortion among Louisiana residents may be attributable to a shift in the clinics where people obtained care during the pandemic; more Louisiana residents obtained care at a clinic that had historically provided fewer medication abortions.
There are health implications of the decreased number of abortions associated with pandemic onset. People unable to obtain clinic-based abortions postpone seeking abortion; attempt to self-manage their abortions, which may put them at legal risk17 , 45; or continue their pregnancies, which increases risks of adverse health outcomes.23–26 Other research indicates that the number Louisiana residents making online self-managed abortion requests to 1 online provider increased in the early weeks of the pandemic, although not by the same amount facility-based abortions decreased.17 While research is needed to assess precise increases in births attributable to people being unable to obtain abortions in Louisiana, findings suggest we might see such an increase. Thus, the COVID-19 pandemic may have indirect effects on maternal and child health in Louisiana.
There are 2 larger implications. First, our findings indicate that, as with other forms of health care,6 the pandemic was associated with reductions in availability and use of abortion services. One explanation is that the Louisiana health department released an order that was ambiguous regarding whether abortion was considered an essential service.14 , 46 This order may have contributed to declines in availability as clinics explored whether they could remain open, suggesting that abortion services can be disrupted without outright bans. Another explanation is that Louisiana was an early hotspot in terms of number of COVID-19 cases.16 This context could have influenced availability and use of abortion services directly through providers and patients becoming sick or through general public health responses that affected transportation and caregiving infrastructure, as has been documented elsewhere.16 That this disruption persisted in Louisiana through July suggests that the ambiguously worded order may have had a lasting impact on availability of abortion services in Louisiana and also that the pandemic and general public health responses may have continued to influence the ability of Louisiana clinics to provide abortion care. The latter explanation would indicate an ongoing need for policies that make delivery of medication abortion without an in-person visit easier and for including abortion providers in emergency response planning. Future research should seek to understand whether and which pandemic-specific versus pre-existing policies have been the biggest barriers to abortion care during the pandemic.
Second, as mystery call data indicate, clinics can be “in between”46 open and closed47; they may remain open yet have long waits or may not offer all types of abortion. It is important for research to use more complex measures of abortion service availability than traditional metrics such as the number of counties with an abortion clinic.48
Limitations
There are limitations. First, we only had data on the number of abortions in the 3 months after pandemic onset and thus cannot assess whether or when the number of abortions returned to prepandemic levels. However, focusing on March through May 2020 means most people having abortions likely became pregnant either before or soon after pandemic onset, when it was not yet clear how long the pandemic would last. Thus, abortion numbers from March through May 2020 are less likely to be influenced by pandemic-related influences on contraception access and childbearing intentions and may be more easily attributable to variations in abortion service availability during this time. In addition, the recent Texas study used this same time period.18 Second, we do not have mystery call data before April 2020, and mystery call data from Texas were obtained on a different timeline. Third, Louisiana residents could have traveled to other states; if so, we overestimated the decrease in abortions among Louisiana residents. However, this would mean that Louisiana residents would have had to dramatically increase their distance traveled, as nearly three fourths of Louisiana residents of reproductive age live more than 150 miles from the nearest out-of-state abortion clinic.49
Conclusions
While most abortion clinics remained open and continued to provide care during the first months of the COVID-19 pandemic, most Louisiana clinics did not. In Louisiana, a 31% decrease in the number of abortions and an increase in the proportion of abortions provided in the second trimester followed this service disruption. Thus, the COVID-19 pandemic has had indirect effects on abortion care, which may result in adverse maternal and child health outcomes moving forward.
ACKNOWLEDGMENTS
This work was supported by grants from an anonymous private foundation and the Packard Foundation.
The authors thank Nicole Bloom, Sara Daniel, Alexandra McBrayer, Jessica Navarro, Miriam Parra, and Elsa Vizcarra for research assistance and project support; John Boscardin for statistical support; and Ushma Upadhyay for creating the database of abortion facilities.
CONFLICTS OF INTEREST
There are no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
The institutional review boards of the University of California, San Francisco, and University of Texas, Austin, granted ethical approval for this research.
Footnotes
REFERENCES
- 1.Centers for Disease Control and Prevention. 2020. https://covid.cdc.gov/covid-data-tracker
- 2.Madhav N, Oppenheim B, Gallivan M, Mulembakani P, Rubin E, Wolfe N. Pandemics: risks, impacts, and mitigation. In: Jamison DT, Gelband H, Horton S, et al., editors. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd ed. Washington, DC: The World Bank; 2017. [DOI] [Google Scholar]
- 3.Masroor S. Collateral damage of COVID-19 pandemic: delayed medical care. J Card Surg. 2020;35(6):1345–1347. doi: 10.1111/jocs.14638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI. A war on two fronts: cancer care in the time of COVID-19. Ann Intern Med. 2020;172(11):756–758. doi: 10.7326/M20-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lange SJ, Ritchey MD, Goodman AB, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795–800. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges. The Commonwealth Fund; 2020. [DOI] [Google Scholar]
- 7.Lewis C, Seervai S, Shah T, Abrams MK, Zephyrin L. Primary care and the COVID-19 pandemic. The Commonwealth Fund; 2020. [DOI] [Google Scholar]
- 8.Jiang H, Zhou Y, Tang W. Maintaining HIV care during the COVID-19 pandemic. Lancet HIV. 2020;7(5):e308–e309. doi: 10.1016/S2352-3018(20)30105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saunders MJ, Evans CA. COVID-19, tuberculosis and poverty: preventing a perfect storm. Eur Respir J. 2020;56(1):2001348. doi: 10.1183/13993003.01348-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amimo F, Lambert B, Magit A. What does the COVID-19 pandemic mean for HIV, tuberculosis, and malaria control? Trop Med Health. 2020;48(1):32. doi: 10.1186/s41182-020-00219-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. 2020. https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19
- 12.Lindberg LD, VandeVusse A, Mueller J, Kirstein M. Early impacts of the COVID-19 pandemic: findings from the 2020 Guttmacher survey of reproductive health experiences. New York, NY: Guttmacher Institute; 2020. [DOI] [Google Scholar]
- 13.Bayefsky MJ, Bartz D, Watson KL. Abortion during the COVID-19 pandemic—ensuring access to an essential health service. N Engl J Med. 2020;382(19):e47. doi: 10.1056/NEJMp2008006. [DOI] [PubMed] [Google Scholar]
- 14.Sobel S, Ramaswamy A, Frederiksen B, Salganicoff A. State action to limit abortion access during the COVID-19 pandemic. Kaiser Family Foundation; 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/state-action-to-limit-abortion-access-during-the-covid-19-pandemic [Google Scholar]
- 15.Keating D, Tierney L, Meko T.In these states, pandemic crisis response includes attempts to stop abortion Washington PostApril 23, 2020. https://www.washingtonpost.com/nation/2020/04/21/these-states-pandemic-crisis-response-includes-attempts-stop-abortion/?arc404=true
- 16.Roberts SCM, Schroeder R, Joffe C. COVID-19 and independent abortion providers: findings from a rapid response survey. Perspect Sex Reprod Health. 2020;52(4):217–225. doi: 10.1363/psrh.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aiken ARA, Starling JE, Gomperts R, Tec M, Scott JG, Aiken CE. Demand for self-managed online telemedicine abortion in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Obstet Gynecol. 2020;136(4):835–837. doi: 10.1097/AOG.0000000000004081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White K, Kumar B, Goyal V, Wallace R, Roberts SCM, Grossman D. Changes in abortion in Texas following an Executive Order ban during the coronavirus pandemic. JAMA. 2021;325(7):691–693. doi: 10.1001/jama.2020.24096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Food and Drug Administration et al. v American College of Obstetricians and Gynecologists et al., 592 US ___ (2021. https://www.supremecourt.gov/opinions/20pdf/20a34_3f14.pdf
- 20.Louisiana coronavirus map and case count. New York Times. October 7, 2020. https://www.nytimes.com/interactive/2021/us/louisiana-covid-cases.html
- 21.Donley G, Chen BA, Borrero S. The legal and medical necessity of abortion care amid the COVID-19 pandemic. J Law Biosci. 2020;7(1):lsaa013. doi: 10.1093/jlb/lsaa013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cappello O. Surveying state executive orders impacting reproductive health during the COVID-19 pandemic. New York, NY: Guttmacher Institute; 2020. [Google Scholar]
- 23.Roberts SCM, Biggs MA, Chibber KS, Gould H, Rocca CH, Foster DG. Risk of violence from the man involved in the pregnancy after receiving or being denied an abortion. BMC Med. 2014;12(1):144. doi: 10.1186/s12916-014-0144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Foster DG, Biggs MA, Ralph L, Gerdts C, Roberts SCM, Glymour MM. Socioeconomic outcomes of women who receive and women who are denied wanted abortions in the United States. Am J Public Health. 2018;108(3):407–413. doi: 10.2105/AJPH.2017.304247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foster DG, Biggs MA, Raifman S, Gipson J, Kimport K, Rocca CH. Comparison of health, development, maternal bonding, and poverty among children born after denial of abortion vs after pregnancies subsequent to an abortion. JAMA Pediatr. 2018;172(11):1053–1060. doi: 10.1001/jamapediatrics.2018.1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ralph LJ, Schwarz EB, Grossman D, Foster DG. Self-reported physical health of women who did and did not terminate pregnancy after seeking abortion services: a cohort study. Ann Intern Med. 2019;171(4):238–247. doi: 10.7326/M18-1666. [DOI] [PubMed] [Google Scholar]
- 27.Upadhyay UD, Desai S, Zlidar V, et al. Incidence of emergency department visits and complications after abortion. Obstet Gynecol. 2015;125(1):175–183. doi: 10.1097/AOG.0000000000000603. [DOI] [PubMed] [Google Scholar]
- 28.Zane S, Creanga AA, Berg CJ, et al. Abortion-related mortality in the United States: 1998‒2010. Obstet Gynecol. 2015;126(2):258–265. doi: 10.1097/AOG.0000000000000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flaherman VJ, Afshar Y, Boscardin J, et al. Infant outcomes following maternal infection with SARS-CoV-2: first report from the PRIORITY study. Clin Infect Dis. 2020:ciaa1411. doi: 10.1093/cid/ciaa1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Allotey J, Stallings E, Bonet M, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Diriba K, Awulachew E, Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal‒fetal transmission: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):39. doi: 10.1186/s40001-020-00439-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pirjani R, Hosseini R, Soori T, et al. Maternal and neonatal outcomes in COVID-19 infected pregnancies: a prospective cohort study. J Travel Med. 2020;27(7):taaa158. doi: 10.1093/jtm/taaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Di Mascio D. Maternal and perinatal outcomes of pregnant women with SARS-COV-2 infection. Ultrasound Obstet Gynecol. 2021;57(2):232–241. doi: 10.1002/uog.23107. [DOI] [PubMed] [Google Scholar]
- 34.Preis H, Mahaffey B, Heiselman C, Lobel M. Vulnerability and resilience to pandemic-related stress among U. Soc Sci Med. 2020;266:113348. doi: 10.1016/j.socscimed.2020.113348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Abortion Federation. 2020. https://prochoice.org/abortion-covid-19
- 36.Raymond EG, Grossman D, Mark A, et al. Commentary: no-test medication abortion: a sample protocol for increasing access during a pandemic and beyond. Contraception. 2020;101(6):361–366. doi: 10.1016/j.contraception.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baum SE, White K, Hopkins K, Potter JE, Grossman D. Rebound of medication abortion in Texas following updated mifepristone label. Contraception. 2019;99(5):278–280. doi: 10.1016/j.contraception.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cartwright AF, Karunaratne M, Barr-Walker J, Johns NE, Upadhyay UD. Identifying national availability of abortion care and distance from major US cities: systematic online search. J Med Internet Res. 2018;20(5):e186. doi: 10.2196/jmir.9717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kates J, Michaud J, Tolbert J. Stay-at-home orders to fight COVID-19 in the United States: the risks of a scattershot approach. Kaiser Family Foundation; 2020. https://www.kff.org/policy-watch/stay-at-home-orders-to-fight-covid19 [Google Scholar]
- 40.Franklin TE, Theisen G, Salyer CV, Pinkston C, Gunaratnam B. The seasonality of abortion in Kentucky. Contraception. 2017;95(2):181–185. doi: 10.1016/j.contraception.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 41.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 42.Donley G, Chen BA, Borrero S. The legal and medical necessity of abortion care amid the COVID-19 pandemic. J Law Biosci. 2020;7(1):lsaa013. doi: 10.1093/jlb/lsaa013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kunzelman M. Judge: women can get abortion pill without doctor visits. US News. July 13, 2020. https://www.usnews.com/news/us/articles/2020-07-13/judge-women-can-get-abortion-pill-without-doctor-visits
- 44.Guttmacher Institute. 2020. https://www.guttmacher.org/state-policy/explore/medication-abortion
- 45.Aiken ARA, Starling JE, van der Wal A, et al. Demand for self-managed medication abortion through an online telemedicine service in the United States. Am J Public Health. 2020;110(1):90–97. doi: 10.2105/AJPH.2019.305369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Louisiana Department of Health. 2020. https://ldh.la.gov/assets/oph/Coronavirus/resources/providers/LDH-MEMO-UPDATE-RESTORE-MED-SURG-Procedures.pdf
- 47.McGowan ML, Norris AH, Bessett D. Care churn—why keeping clinic doors open isn’t enough to ensure access to abortion. N Engl J Med. 2020;383(6):508–510. doi: 10.1056/NEJMp2013466. [DOI] [PubMed] [Google Scholar]
- 48.Jones R, Witwer E, Jerman J. Abortion incidence and service availability in the United States, 2017. New York, NY: Guttmacher Institute; 2019. [DOI] [Google Scholar]
- 49.Roberts SCM, Fuentes L, Kriz R, Williams V, Upadhyay UD. Implications for women of Louisiana’s law requiring abortion providers to have hospital admitting privileges. Contraception. 2015;91(5):368–372. doi: 10.1016/j.contraception.2015.02.001. [DOI] [PubMed] [Google Scholar]