Abstract
This study examined the mediation role of perceived social support in the association between hope and health-related quality of life with coronavirus anxiety in the elderly. The research was conducted by descriptive method with a structural equations design. The population included all the over-60 elderly individuals residing in Sanandaj city, Iran, in 2021. Among them, 220 individuals were selected through available sampling method. To gather the data, the questionnaires of coronavirus anxiety, perceived social support, hope and health-related quality of life were used. Data analysis was conducted by using structural equations modeling and via SPSSv23 and AMOSv26 software. Data analysis indicated that there is a significant and negative relationship between hope, health-related quality of life, and perceived coronavirus anxiety among the elderly. Moreover, perceived social support plays a mediating role in the relationship of both hope and health-related quality of life with coronavirus anxiety. The present study provided an important insight regarding the mediating role of perceived social support in the relationship of hope and health-related quality of life with coronavirus anxiety the elderly. Through creating programs to hold suitable interventions for improving perceived social support, the COVID-19–related anxiety can be reduced during its prevalence.
Keywords: coronavirus anxiety, COVID-19, elderly, health-related quality of life, perceived social support
Introduction
On January 30, 2020, the World Health Organization (WHO) spread a news on the spread of a new coronavirus, after which an emergency status for public health was announced, and on the 11th of February in the same year, the new virus was called Coronavirus 2019 disease (COVID-19) by WHO (World Health Organization, 2020). Up to now (June 7, 2021), the COVID-19 pandemic has led to death of over 3,800,000 people all around the globe among whom around 82,000 deaths have been reported in Iran (Johns Hopkins University, 2021). According to the reports of the Iranian Health Ministry in April 2021, the pandemic status of COVID-19 is still concerning in Iran, and the mortality rate is still high compared to the past and Iran is on the verge of experiencing the fourth wave of COVID-19 (Ministry of Health & Medical Education of Islamic Republic of Iran, 2021). This disease creates fear and concern among public particularly amongst special groups such as the elderly, patients’ caregivers and health service providers, and individuals with underlying diseases (Schoch-Spana, 2020). Accordingly, the existing data shows that coronavirus results in higher mortality in the elderly compared to other groups and its rate varies from 3.6 to 14.8. This can be due to low efficiency of the body’s immune system and having underlying diseases in the elderly (Mehra et al., 2020). The elderly being at risk is bold in the media, and the elderly are continuously recommended to take more precautions. Moreover, compared to other groups, the elderly are more dependent on others in doing their daily activities and social distancing related to COVID-19 has led to more isolation among them. All these factors have increased fear and anxiety from COVID-19 among the elderly (Mehra et al., 2020; Rosenblum, 2021; Siew et al., 2021).
Anxiety-related disorders and symptoms are among the most extensive mental disorders in the elderly even when there is no crisis period (Rosenblum, 2021). In the literature, some studies have focused on the mental health of the elderly during the COVID-19 pandemic crisis (Rosenblum, 2021; Siew et al., 2021). In general, these studies indicate the increase in depression and anxiety symptoms in the elderly. For instance, in a survey conducted in May–January 2020 in England on 7127 older populations, about 12% of the elderly reported worse levels of depression and anxiety during the quarantine period. This rate in both genders together (with the superiority of women) equaled 34.8% (Robb et al., 2020). However, among the majority of the conducted study in the coronavirus period, especially in the discussions on problems such as anxiety, very little attention has been given to the elderly individuals (Robb et al., 2020). Based on our knowledge, some studies have pointed to variables such as social isolation (Siew et al., 2021), daily functional self-actualization and functional cognition (Rosenblum, 2021), and subjective loneliness (Robb et al., 2020) as the predictive factors in the elderly. According to cognitive models (Lazarus and Folkman, 1984), when people are faced with stressful and anxiety-provoking resources such as diseases similar to COVID-19 in their lives, a collection of factors including personal resources (e.g., perceived social support and hope - both have cognitive dimensions (Levkovich et al., 2021; Snyder, 2002)) and physio-psychological health status (e.g., quality of life) will be effective in how people deal or cope with these stresses. The present study is focused on all the above-mentioned factors.
One of the important sources of adaptation and coping with stressful events is the support and attention that the elderly receive from close ones. Perceived social support is defined as the perceived access to the caregiver in case of need (Levkovich et al., 2021). Curfew and quarantine regulations, besides their positive consequences regarding preventing and coping with COVID-19, can result in negative psychological effects such as reduced social relations (Amirfakhraei et al., 2020). Perceived social support includes cognitive and mental dimensions of individuals regarding supportive relations and behaviors, and studies have reported that this concept is an effective resource for coping with problems and challenges that can work as the main resource of personal care and subjective well-being, especially in the elderly (Levkovich et al., 2021; Şahin et al., 2019). However, studies suggest that perceived social support can play a mediating role in the relationship between variables such as social isolation and mental health improvement (Gong et al., 2020; Xu et al., 2020).
Hope is another resource of adaptation and resiliency that can lead to improved mental health during a universal health-related crisis (Gallagher et al., 2021). Research has suggested that individuals with high levels of hope are more likely to better adapt to life challenges and use more effective coping strategies in face of problems (Karababa, 2020; Wang et al., 2017). Although studies conducted on COVID-19 are quite new, but at least in two studies (Mirhosseini et al., 2020), it has been shown that hope might be related to flexibility in face of chronic stressful factors related to the COVID-19 pandemic and it can potentially play a role in overcoming the anxiety caused by this crisis. In a prospective cohort study (Long et al., 2020) investigating the impact of hope on health and psychological well-being of the elderly, the authors concluded that hope is strongly associated with indices of physical health, health behaviors, and numerous psychological and social dimensions.
In recent years, health-related quality of life has received worldwide attention (Ping et al., 2020). According to its definition, this concept refers to the perceived effects of physical and mental health on every individual’s ability for having a productive life (Bowling, 1995); Therefore, this is a multi-dimensional concept and, as a result, an important outcome criterion in the old age (Helvik et al., 2016). As findings show, one reason for high mortality rates of COVID-19 among the elderly is rooted in their weak immune system and underlying diseases (Mehra et al., 2020); so, it seems that this concept can affect the level of concern and anxiety among the elderly. According to the findings of a study (Suzuki et al., 2020), low health-related quality of life was accompanied by reduced physical activities and, as a result, reduced psychological well-being in the elderly during COVID-19 limitations.
According to the COVID-19 pandemic and the concerning mortality rate of the elderly that can be a stressful factor for other elderlies, it is necessary that the mental health of this age group would receive more attention. The increasing evidence on negative psychological factors shows that they may lead to increased distress during pandemic (like social distancing and feeling of loneliness), but the investigations on resources of adaptation and psychological resilience of the elderly (such as hope and health-related quality of life) showing that these resources might lead to greater well-being or even their growth in stressful events like COVID-19 are still new. Identifying resilience and other protective factors during the COVID-19 pandemic disease can contribute to the efforts aimed at facilitating mental health among the elders during the worldwide pandemic. Accordingly, by the aim of enriching the existing limited knowledge, the present research aims to develop a causal model of coronavirus anxiety for elders based on hope and health-related quality of life with the mediating role of perceived social support.
Methods
Participants
This is a descriptive study with a structural equations design conducted in Sanandaj, Iran, in 2021. The sample included 220 older adults who were selected using available sampling method. The frequency distribution of male individuals was 61.8, and it was 38.2% for female individuals. Among these, one participant (0.5%) was single, 188 were married (85.5%), and 31 (14.1%) were divorced or widowed. The employment status for all 220 participants was as follows: 75 (34.1%) housewives, 107 individuals (48.6%) self-employed, 37 individuals (16.8%) employee, and one individual (0.5%) trooper. Mean and SD of age was 67.08 ± 7.34 for men, and it was 66.14 ± 9.69 for women. Regarding education level, 98 individuals (44.5%) were illiterate, 75 (34.1%) had middle school degree, 27 individuals (12.3%) diploma, 15 individuals (6.8%) associate degree, and five individuals (2.3%) bachelor’s degree or higher.
Procedure
The sampling process was as follows: First, four trained researchers, by referring to daily nursing homes, cultural centers, parks and retirement centers, after introducing themselves and explaining the objectives and nature of the research, invited the elderly to participate in the research. In the next step, the researchers followed the social distancing and health protocols and administered the questionnaires in the form of individual interviews to the elderly who met the inclusion criteria. In this way, the researchers read the items of each questionnaire to the elderly. The reason for conducting the interview was to ensure that the elderly fully understood the questionnaires items and to address any questions they might have. It is noteworthy that before the interviews began, the informed consent forms were filled, the research confidentiality was explained, and the elders were prepared mentally for the process. The study inclusion criteria were as follows: Age 60 years or higher, having no cognitive problems (using Abbreviated Mental Test (AMT)), and having no severe and delimiting physical disease. The exclusion criteria were having no tendency to participate in the study and incomplete delivery of the questionnaires.
Measures
Corona Disease Anxiety Scale (CDAS): This tool has been developed and validated for evaluating the anxiety created by the coronavirus pandemic in Iran in 2019 (Alipour et al., 2020). The final version of this tool includes 18 items and two dimensions. Items 1–9 assess psychological symptoms and items 10–18 assess physical symptoms. This tool is scored with a 4-score Likert (0 = never to 3 = always). The highest and lowest scores are respectively 0–4. Higher scores indicate a higher level of anxiety in the individual. The reliability of this tool shows a higher level of anxiety in the individual. The reliability of Corona Disease Anxiety Scale (CDAS) by Cronbach’s alpha was 0.87 for the first factor and 0.86 for the second factor, and it was 0.91 for the whole scale (Alipour et al., 2020). The reliability of this scale in the present study was 0.96 by Cronbach’s alpha.
Multidimensional Scale of Perceived Social Support (MSPSS): This scale includes 12 items that assess the level of perceived social support in the elders in three domains of family members, friends, and other significant people in life based on a 7-score Likert scale (from completely disagree to completely agree). The validity and reliability of this scale have been reported to be desirable by the original developers in 1988 (Zimet et al., 1988). In the present research, the total reliability of multidimensional scale of perceived social support (MSPSS) equaled 0.95 by Cronbach’s alpha method.
The Adult Hope Scale (AHS): This scale includes 12 items among which 8 items are the main assessment items and the other 4 items are lie-detectors (fillers) and are not counted in the scoring (Snyder et al., 1991). From these 8 items, 4 items are related to agency thinking (goal-directed energy: Items 2, 9, 10, and 12) and four items are related to pathways thinking (planning to meet goals: Items 1, 4, 6, and 8). The scoring system is based on a 5-point Likert scale from 0 to 4 but this scoring system has been reversed for questions 3, 7, and 11 (Snyder et al., 1991). Extensive research has been conducted the convergent and divergent validity of this scale and a meta-analysis showed a total internal consistency equaling 0.82 for Adult Hope Scale (AHS) (Hellman et al., 2013). In the present research, the reliability of AHS equaled 0.94 for the total score by Cronbach’s alpha method.
The Health Survey-Short Form (SF-12): (SF-12) (with 12 items) which is used extensively in different studies includes eight dimensions divided into physical and mental health subscales. The answers are given based on yes/no questions and Likert-type multi-option statements. Questions 1, 8, 10, and 11 are scored reversely (Ware et al., 1996). The validity and reliability of SF-12 are confirmed in different studies (Ware et al., 1996). In the present research, SF-12 obtained a total score of 0.91 by Cronbach’s alpha method.
Data Analyses Procedures
Data was analyzed using the Statistical Package for Social Science (SPSS v23) and Analysis of Moment Structures (AMOS v26) software. Initial analyses (e.g., exploring missing data, outliers, and normality) were conducted using SPSS software. Analysis of Moment Structures was used to analyze the four steps of SEM: 1. To develop a measurement model for each scale, 2. to develop a measurement model for all scales, 3. to perform a structural regression model, and 4. to examine the mediation effect of perceived social support.
Results
Table 1 shows mean, SD, coronavirus anxiety, perceived social support, health-related quality of life and hope, and the correlation matrix between the research variables. Results of Table 1 show that the relationship between perceived social support (r = −.61, p < .01), hope (r = −.62, p < .01) and health-related quality of life (r = −.65, p < .01) with coronavirus anxiety is significant and negative. The highest correlation coefficient is related to the relationship between perceived social support and hope (r =.722 p < .01).
Table 1.
Correlation Between Study Variables, and the Mean, and SD.
| Variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. CDAS | 1 | −0.613** | −0.617** | −0.654** |
| 2. MSPSS | 1 | 0.660** | 0.722** | |
| 3. SF-12 | 1 | 0.476** | ||
| 4. AHS | 1 | |||
| M | 16.18 | 62.41 | 23.38 | 31.58 |
| SD | 12.64 | 16.42 | 7.14 | 8.46 |
Note. CDAS: corona disease anxiety scale, MSPSS: multidimensional scale of perceived social support, SF-12: the health survey-short form, AHS: the adult hope scale, M: mean, SD: standard deviation, **p < .01.
Measurement Model for Each Scale
Confirmatory factor analysis was performed on each scale. The results indicated that all items had factor loading values greater than .5 and were remained in the scales. In addition, results of measurement model fit are shown in Table 2 and reveal an acceptable model fit for each scale.
Table 2.
Measurement Model for Each Scale.
| Measurement model | No. of items | CMIN/df | RMSEA | CFI | GFI | TLI |
|---|---|---|---|---|---|---|
| CDAS | 18 | 2.16 | .07 | .97 | .91 | .96 |
| MSPSS | 12 | 2.14 | .07 | .98 | .93 | .97 |
| SF-12 | 12 | 1.85 | .06 | .99 | .97 | .98 |
| AHS | 12 | 1.65 | .05 | .98 | .95 | .97 |
Note. CMIN, chi-square; RMSEA, root mean square error of approximation; CFI, comparative fit index; GFI, goodness of fit index; TLI, Tucker–Lewis index.
Structural Model
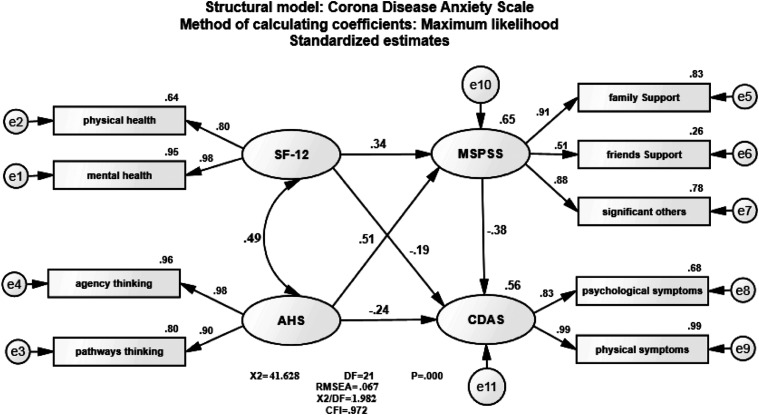
The structural regression model showed a good model (CMIN/df = 1.98, p < .01, CFI = .97, GFI = .98, TLI = .94, and RMSEA =.067). The findings showed that personal standards between health-related quality of life with coronavirus anxiety are negative. The path coefficient between hope with coronavirus anxiety is negative, the path coefficient between perceived social support and coronavirus anxiety is negative, and the path coefficient between hope and health-related quality of life is significant and positive. The studied variables explained 56% of the variance in coronavirus anxiety in the elderly (see Figure 1).
Figure 1.
Structural model for the corona disease anxiety. Note. CDAS: corona disease anxiety scale, MSPSS: multidimensional scale of perceived social support, SF-12: the health survey-short form, AHS: the adult hope scale, for all estimates p < .01.
Mediation Test of Perceived Social Support
The results showed perceived social support mediates the relationship hope and health-related quality of life with coronavirus anxiety. According to the findings of Table 3, in the direct model the relationship between hope and health-related quality of life with coronavirus anxiety was significant (β = −.46, β = −.31). In addition, the results based on the mediation model show significant relationship between hope and perceived social support (β = −.51) and health-related quality of life and perceived social support (β = −.34) and perceived social support with coronavirus anxiety (β = −.38). However, although the size of the standard regression weight for the direct relationship between hope and health-related quality of life with coronavirus anxiety reduced when perceived social support was added as a mediator variable in the mediation model, it was still significant. Therefore, the partial mediation of perceived social support on the relationship between hope and health-related quality of life with coronavirus anxiety was supported.
Table 3.
Standard Regression Weight in the Mediation, Direct, and Indirect Model.
| Relationship | Direct without Mediator | Direct with Mediator | Indirect effect | Result |
|---|---|---|---|---|
| SF-12 ---> CDAS | −.31** | −19* | −.129* | Partial mediation |
| AHS ---> CDAS | −.46** | −.24** | −.196* | Partial mediation |
** = p < .001; ** = p < .01
Discussion
The findings of the present study show the significant and negative association between hope, health-related quality of life, and perceived social support with coronavirus anxiety among older adults. However, the present study has provided important evidence on the mediating role of perceived social support on the relationship between each variable of hope and health-related quality of life with coronavirus anxiety.
The role of perceived social support as the mediating variable in the relationship between different variables in elders has been introduced and confirmed in various studies. For example, consistent with the findings of the present study, other researchers have indicated that perceived social support plays moderating and mediating roles in the relationships between some variables such as loneliness and corona anxiety (Xu et al., 2020), perceived emotional intelligence and psychological well-being (Rey et al., 2019), depression and suicide ideation (Oon-Arom et al., 2021), visual impairment and depression (Gong et al., 2020), and socio-economic status and quality of life (Henriques et al., 2020). These findings clearly indicate the protective and resiliency role of perceived social support in coping with stressful events (such as COVID-19) among the elders. The obtained findings can be explained in at least three perspectives. First, the findings of the present research showed that perceived social support has a significant and negative relationship with corona anxiety in elders. Based on the Terror Management Theory (Greenberg et al., 1994), every time the prevalence of mortality increases due to the occurrence of a crisis, people’s anxiety will also increase. Hence, to resist against anxiety and manage it, individuals may get involved with interactions and obtain social support from closed ones in this path (Xu et al., 2020). It appears that according to the mortality rate of COVID-19 particularly in elders, as the findings of the present study suggested, increase in perceived social support can reduce corona anxiety among the elders. Second, the findings of the current study regarding the mediating role of perceived social support in the relationship between hope, health-related quality of life and corona anxiety are consistent with the Stress-Buffering Model (Cohen, 2004). This model indicates that social support has a protective role against the negative effects of stress (e.g., anxiety) caused by negative events of life on mental and physical health. In fact, social support or the resources available for the individual or the resources that the individual imagines are available (perceived) might help them feel more control over the stressful condition and, therefore, cope with the current situation with more feelings of self-efficacy and hope, or it might lead to more emotional disclosure and processing of negative events that eventually brings about positive consequences for quality of life (physically and psychologically; e.g., lower levels of depression or anxiety, better access to health care, etc.) (Szkody et al., 2020; Xu et al., 2020). The mediating role of perceived social support in other crises has been confirmed (Arnberg et al., 2012). Third, perceived social support is especially notable in Asian populations (including Iran) that have collective cultures, where feelings of togetherness and family support are of more value compared to European countries and the social support of family and friends is associated with more reduction in psychological stresses (Oon-Arom et al., 2021; Singh et al., 2015).
The findings of the present study also suggested that hope exerts a direct (negative) and significant effect on corona anxiety. In other words, with the increase in hope, corona anxiety will be reduced. Despite the newness of research on the relationship between hope and COVID-19’s psychological effects, the findings of the present research are consistent with a number of similar studies (Gallagher et al., 2021; Mirhosseini et al., 2020). Generally, it has been suggested that hope predicts higher levels of positive mental health and lower levels of mental problems such as depression and anxiety (Alarcon et al., 2013; Gallagher et al., 2021). Furthermore, the findings of the present study suggested that health-related quality of life has a negative and significant association with corona anxiety in elders. The findings are consistent with studies showing that elders, who experience more anxiety in the COVID-19 period, obtain lower scores in health-related quality of life (Daneshfar et al., 2021; Levkovich et al., 2021; Suzuki et al., 2020). The relationship between negative psychological aspects such as corona anxiety and health-related quality of life in elders can be explained such that while elders are anxious about their family and themselves being infected with COVID-19, they might, on the one hand, choose to help in controlling and restraining this disease by isolating themselves, or, on the other hand, this isolation might bring about negative impacts such as lower quality of life for them (Levkovich et al., 2021).
One of the limitations of the present study is related to the use of self-report scales for participants that may lead to bias in the results, although the researchers did their best to complete the questionnaires orally and in the frame of interviews. The next limitation is related to the dynamic nature of COVID-19 and the experience of different waves of this disease, and this fact might lead to the fact that the obtained statistics and values may change over time and this necessitates performing longitudinal studies. Another limitation is that there is no control group and the data studied is only questionnaires answered by the population selected (self-reported).
Conclusion
The findings of the present study provide important insights for improving the current understanding of the relationship between hope and health related quality of life with coronavirus anxiety in elders. Perceived social support shows significant implications as a mediating mechanism for interventions aiming at reducing coronavirus anxiety in elders. Moreover, the findings of the present study showed that the COVID-19 pandemic exerts negative effects on mental health of the elders and this population group possesses protective resources (internal and external resources) that can be used to help them show better coping with the stressful conditions.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Mohammad Rostami https://orcid.org/0000-0002-5696-543X
References
- Alarcon G. M., Bowling N. A., Khazon S. (2013). Great expectations: A meta-analytic examination of optimism and hope. Personality and Individual Differences, 54(7), 821-827. 10.1016/j.paid.2012.12.004. [DOI] [Google Scholar]
- Alipour A., Ghadami A., Alipour Z., Abdollahzadeh H. (2020). Preliminary validation of the corona disease anxiety scale (CDAS) in the Iranian sample. Quarterly Journal of Health Psychology, 8(32), 163-175. 10.30473/hpj.2020.52023.4756. [DOI] [Google Scholar]
- Amirfakhraei A., Masoumifard M., Esmaeilishad B., DashtBozorgi Z., Baseri L. D. (2020). Prediction of corona virus anxiety based on health concern, psychological hardiness, and positive meta-emotion in diabetic patients. Journal of Diabetes Nursing, 8(2), 1072-1083. [Google Scholar]
- Arnberg F. K., Hultman C. M., Michel P.-O., Lundin T. (2012). Social support moderates posttraumatic stress and general distress after disaster. Journal of Traumatic Stress, 25(6), 721-727. 10.1002/jts.21758 [DOI] [PubMed] [Google Scholar]
- Bowling A. (1995). The concept of quality of life in relation to health. Medicina Nei Secoli, 7(3), 633-645. [PubMed] [Google Scholar]
- Cohen S. (2004). Social relationships and health. American Psychologist, 59(8), 676-684. 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Daneshfar Z., Jahanian Sadatmahalleh S., Youseflu S., Bahri Khomami M., Kazemnejad A. (2021). Influential factors on quality of life in married Iranian women during the COVID-19 pandemic in 2020: A path analysis. BMC Women’s Health, 21(1), 102-108. 10.1186/s12905-020-01114-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher M. W., Smith L. J., Richardson A. L., D’Souza J. M., Long L. J. (2021). Examining the longitudinal effects and potential mechanisms of hope on COVID-19 stress, anxiety, and well-being. Cognitive Behaviour Therapy, 50, 234-245. 10.1080/16506073.2021.1877341. [DOI] [PubMed] [Google Scholar]
- Gong X., Ni Z., Wu B. (2020). The mediating roles of functional limitations and social support on the relationship between vision impairment and depressive symptoms in older adults. Ageing and Society, 40(3), 465-479. 10.1017/S0144686X18001010. [DOI] [Google Scholar]
- Greenberg J., Pyszczynski T., Solomon S., Simon L., Breus M. (1994). Role of consciousness and accessibility of death-related thoughts in mortality salience effects. Journal of Personality and Social Psychology, 67(4), 627-637. 10.1037//0022-3514.67.4.627. [DOI] [PubMed] [Google Scholar]
- Hellman C. M., Pittman M. K., Munoz R. T. (2013). The first twenty years of the will and the ways: An examination of score reliability distribution on snyder’s dispositional hope scale. Journal of Happiness Studies, 14(3), 723-729. [Google Scholar]
- Helvik A. S., Corazzini K., Selbæk G., Bjørkløf G. H., Laks J., Šaltytė Benth J., Østbye T., Engedal K. (2016). Health-related quality of life in older depressed psychogeriatric patients: One year follow-up. BMC Geriatrics, 16(1), 131-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henriques A., Silva S., Severo M., Fraga S., Barros H. (2020). Socioeconomic position and quality of life among older people: The mediating role of social support. Preventive Medicine, 135, 106073. 10.1016/j.ypmed.2020.106073. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins University . (2021). Coronavirus resource center. https://coronavirus.jhu.edu/map.html.
- Karababa A. (2020). The moderating role of hope in the relationship between maladaptive perfectionism and anxiety among early adolescents. The Journal of Genetic Psychology, 181(2-3), 159-170. 10.1080/00221325.2020. [DOI] [PubMed] [Google Scholar]
- Lazarus R. S., Folkman S. (1984). Stress, appraisal, and coping. New York, NY: Springer Publishing Company. [Google Scholar]
- Levkovich I., Shinan-Altman S., Essar Schvartz N., Alperin M. (2021). Depression and health-related quality of life among elderly patients during the covid-19 pandemic in Israel: A cross-sectional study. Journal of Primary Care & Community Health, 12, 2150132721995448. 10.1177/2150132721995448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long K. N. G., Kim E. S., Chen Y., Wilson M. F., Worthington Jr E. L., Jr, VanderWeele T. J. (2020). The role of hope in subsequent health and well-being for older adults: An outcome-wide longitudinal approach. Global Epidemiology, 2, 100018. [Google Scholar]
- Mehra A., Rani S., Sahoo S., Parveen S., Singh A. P., Chakrabarti S., Grover S. (2020). A crisis for elderly with mental disorders: Relapse of symptoms due to heightened anxiety due to COVID-19. Asian Journal of Psychiatry, 51, 102114. 10.1016/j.ajp.2020.102114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health & Medical Education of Islamic Republic of Iran . (2021). Infection and death rates due to Covid 19. https://behdasht.gov.ir/.
- Mirhosseini S., Dadgari A., Basirinezhad M. H., Mohammadpourhodki R., Ebrahimi H. (2020). The role of hope to alleviate anxiety in covid-19 outbreak among community dwellers: An online cross-sectional survey. Annals of the Academy of Medicine, Singapore, 49(10), 723-730. 10.47102/annals-acadmedsg.2020341 [DOI] [PubMed] [Google Scholar]
- Oon-Arom A., Wongpakaran T., Kuntawong P., Wongpakaran N. (2021). Attachment anxiety, depression, and perceived social support: A moderated mediation model of suicide ideation among the elderly. International Psychogeriatrics, 33(2), 169-178. 10.1017/S104161022000054X. [DOI] [PubMed] [Google Scholar]
- Ping W., Zheng J., Niu X., Guo C., Zhang J., Yang H., Shi Y. (2020). Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS One, 15(6), e0234850. 10.1371/journal.pone.0234850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey L., Extremera N., Sánchez-Álvarez N. (2019). Clarifying the links between perceived emotional intelligence and well-being in older people: Pathways through perceived social support from family and friends. Applied Research in Quality of Life, 14(1), 221-235. 10.1007/s11482-017-9588-6. [DOI] [Google Scholar]
- Robb C. E., de Jager C. A., Ahmadi-Abhari S., Giannakopoulou P., Udeh-Momoh C., McKeand J., Middleton L., Car J., Majeed A., Ward H., Middleton L. (2020). Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: A survey of older adults in London, UK. Frontiers in Psychiatry, 11, 591120. 10.3389/fpsyt.2020.591120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum S. (2021). State anxiety related to daily function among older adults during the covid-19 pandemic: Are there gender differences? JMIR Aging, 4(2), e25876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin D. S., Özer Ö., Yanardağ M. Z. (2019). Perceived social support, quality of life and satisfaction with life in elderly people. Educational Gerontology, 45(1), 69-77. 10.1080/03601277.2019.1585065. [DOI] [Google Scholar]
- Schoch-Spana M. (2020). COVID-19’s Psychosocial Impacts the pandemic is putting enormous stress on all of us but especially on health care workers and other specific groups. Scientific American Blog Network, 20. https://blogs.scientificamerican.com/observations/covid-19s-psychosocial-impacts. [Google Scholar]
- Siew S. K. H., Mahendran R., Yu J. (2021). Directional effects of social isolation and quality of life on anxiety levels among community-dwelling older adults during a COVID-19 lockdown. The American Journal of Geriatric Psychiatry, S1064-7481(21), 00287. 10.1016/j.jagp.2021.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., McBride K., Kak V. (2015). Role of social support in examining acculturative stress and psychological distress among Asian American immigrants and three sub-groups: Results from NLAAS. Journal of Immigrant and Minority Health, 17(6), 1597-1606. 10.1007/s10903-015-0213-1. [DOI] [PubMed] [Google Scholar]
- Snyder C. R. (2002). Hope theory: Rainbows in the mind. Psychological Inquiry, 13(4), 249-275. 10.1207/S15327965PLI1304_01. [DOI] [Google Scholar]
- Snyder C. R., Harris C., Anderson J. R., Holleran S. A., Irving L. M., Sigmon S. T., Yoshinobu L., Gibb J., Langelle C., Harney P. (1991). The will and the ways: Development and validation of an individual-differences measure of hope. Journal of Personality and Social Psychology, 60(4), 570-585. 10.1037//0022-3514.60.4.570. [DOI] [PubMed] [Google Scholar]
- Suzuki Y., Maeda N., Hirado D., Shirakawa T., Urabe Y. (2020). Physical activity changes and its risk factors among community-dwelling japanese older adults during the COVID-19 epidemic: Associations with subjective well-being and health-related quality of life. International Journal of Environmental Research and Public Health, 17(18), 6591. 10.3390/ijerph17186591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkody E., Stearns M., Stanhope L., McKinney C. (2020). Stress‐buffering role of social support during COVID‐19. Family Process, 47(2), 424-439. 10.1111/famp.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Xu X., Zhou M., Chen T., Yang X., Chen G., Gong Q. (2017). Hope and the brain: Trait hope mediates the protective role of medial orbitofrontal cortex spontaneous activity against anxiety. Neuroimage, 157, 439-447. 10.1016/j.neuroimage.2017.05.056. [DOI] [PubMed] [Google Scholar]
- Ware J., Jr., Kosinski M., Keller S. D. (1996). A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220-233. 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2020). Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Xu J., Ou J., Luo S., Wang Z., Chang E., Novak C., Wang Y., Zheng S., Wang Y. (2020). Perceived social support protects lonely people against COVID-19 anxiety: A Three-wave longitudinal study in China. Frontiers in Psychology, 11, 566965. 10.3389/fpsyg.2020.566965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G. D., Dahlem N. W., Zimet S. G., Farley G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30-41. 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]