To the Editor:
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) coronavirus disease (COVID-19) pandemic impacted healthcare delivery in the United States and around the world. Constraints surrounding personal protective equipment and the need for social distancing (1) to minimize disease spread led to the rapid adoption of telehealth to continue patient care. Telehealth has been implemented across many specialties (1–9) and championed as a measure to increase access in medically underserved or rural locations (10). Although telehealth may be as effective as in-person care (11, 12), it is already associated with high patient satisfaction (2, 13), convenience (3), cost-effectiveness (3, 11), and reduction in healthcare costs (14). Technological challenges, start-up cost, and reimbursement concerns have prevented larger-scale adoption (15). Within cystic fibrosis (CF), smaller pilot studies have described the feasibility of telehealth implementation in individual CF centers (16–18); however, the CF clinician experience has not been described. Our study aimed to characterize telehealth usage patterns, attitudes, and preferences among clinicians for future telehealth care.
This work was accepted for virtual abstract presentation at the North American Cystic Fibrosis Conference 2020 and published in the Pediatric Pulmonology Conference Abstract Supplement (19).
Methods
Cross-sectional web-based surveys were distributed to clinicians at seven U.S. CF programs. The CF programs included were the University of Alabama-Birmingham (Adult), Boston Children’s Hospital/Brigham and Women’s Combined (Adult), Virginia Commonwealth University (Adult), Doernbecher Children’s Hospital (Pediatrics), Cincinnati Children’s Hospital (Pediatrics), University of Virginia (Pediatrics), and Boston Children’s Hospital (Pediatrics). Clinicians were defined as physicians, nurse practitioners, physician’s assistants, registered nurses, registered dietitians, social workers, mental health providers, pharmacists, respiratory therapists, and physical therapists. Clinicians were eligible to participate if they completed one CF telehealth visit. The survey was produced by a multidisciplinary clinician working group from participating centers. The survey included 35 questions (18 multiple choice, 9 yes/no, 7 Likert scale, and 1 open ended). The questions explored 1) the construct of current telehealth visits, 2) perceptions surrounding telehealth experiences, and 3) preferences for future telehealth care (Table 1). An initial survey to establish perceptions of telehealth experience was distributed from May to June 2020. A follow-up survey including identical questions and themes was redistributed from August to September 2020. The follow-up survey sought to investigate the durability and consistency of clinician perceptions following 6 months of telehealth experience. The survey was administered using Google Forms (Google), descriptive statistics and nonparametric test of hypotheses were performed using STATA 15 (StataCorp.), and figures were created using GraphPad Prism 8.4 (GraphPad Software).
Table 1.
Key questions from the CF clinician telemedicine survey
| What were barriers to using telehealth before March 2020? | What platforms do you use to conduct your visits? |
| How do you access your telehealth platform? | Are your visits conducted mostly with audio only or audio plus video? |
| Which of the following scenarios best describes your commonly used visit structure? | What is your preferred visit structure? |
| Have you experienced technical difficulties logging onto or during telemedicine visits? | How satisfied are you with your overall experience using telemedicine services in the care of patients with CF? |
| How do you think the lack of pulmonary function testing impacts the care provided through telemedicine? | How do you think the lack of vital signs impacts the care provided through telemedicine? |
| How do you think the lack of weight impacts the care provided through telemedicine? | How do you think the lack of physical exam impacts the care provided through telemedicine? |
| How do you think the lack of throat or sputum cultures impacts the care provided through telemedicine? | How do you feel telemedicine affects the clinician–patient relationship? |
| Of telemedicine visits performed so far, what proportion do you feel should have been conducted in person? | Compared with in-person office visits, telemedicine visits are? |
| If telemedicine visits were to be offered in the future for routine patient care, about how many visits per year would you prefer to be completed by telemedicine? | If telemedicine visits were to be offered in the future, what type of visits do you think would be appropriate to perform over telehealth? |
Definition of abbreviation: CF = cystic fibrosis.
Results
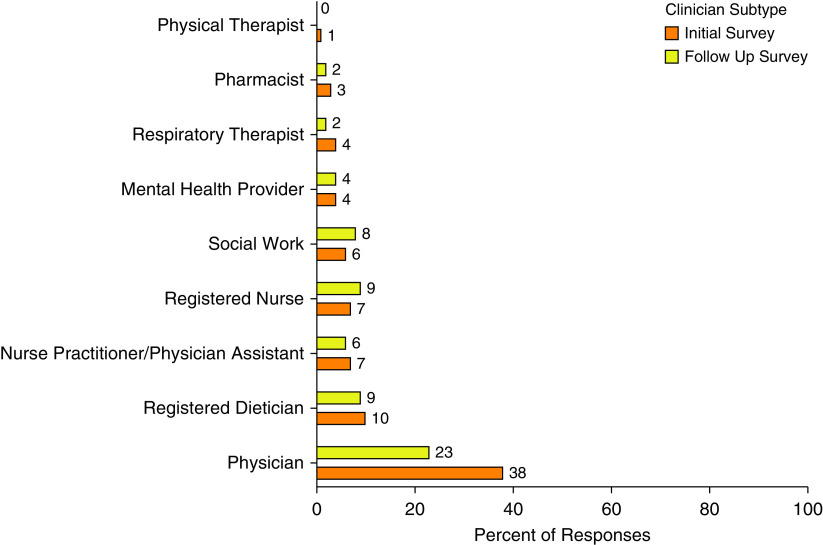
A total of 80 clinicians from medium and large CF programs in the Northeast, Midwest, South, and Pacific Northwest completed the initial survey and 63 the follow-up survey (Figure 1). Most (90%) had never previously used telehealth, 83% felt they received adequate training before beginning telehealth, and 65% reported completing more than 10 visits at the time of the survey. Zoom was the most commonly available (56% initial, 57% follow-up) platform for visits. On initial assessment, a variety of interdisciplinary structures and single-discipline visits were used; however, on follow-up assessment, an interdisciplinary asynchronous format (multiple clinicians evaluated the patient sequentially during the same visit) was predominantly used (48%). The majority of visits (89% initial, 95% follow-up) incorporated audio plus video connectivity, were predominantly accessed by computer (75% initial, 89% follow-up), and were conducted from the clinician’s home (74% initial, 57% follow-up). At 6 months, 83% endorsed experiencing a technical complication at least once following implementation, although 88% experiencing difficulty were able to complete the encounter.
Figure 1.
Clinician subtype of respondents to initial and follow-up survey assessment.
Barriers to previous telehealth implementation and concerns about missing assessments are presented for the cohort and for pediatric and adult clinicians in Figure 2. Despite concern about missing assessments, 78% initially felt that none or few of the patients evaluated by telehealth should have been evaluated in person. This decreased to 68% on follow-up assessment (P = 0.4). Satisfaction (86% initial, 89% follow-up; P = 0.7), positive impact on clinician–patient relationship (58% initial, 57% follow-up; P = 1), and improved efficiency (56% more efficient than in-person visits on both assessments; P = 0.9) remained consistent across both assessments.
Figure 2.

(A) Perceived barriers to telehealth use among all clinician respondents. (B) Concern regarding missing components from in-person clinical evaluations among all clinician respondents. (C) Perceived barriers to telehealth use by adult/pediatric clinicians. (D) Concern regarding missing components from in-person clinical evaluations by adult/pediatric clinicians.
If future telehealth visits were offered, clinicians preferred that some/most visits (96% initial, 99% follow-up; P = 0.1) be performed using telehealth. Quarterly (95% both assessments; P = 1) and hospital follow-up (69% initial, 61% follow-up; P = 0.4) were identified as the most appropriate future visit types. Interdisciplinary synchronous structure (44%) was initially preferred for future visits, but interdisciplinary asynchronous structure (58%) became preferred on repeat assessment (P = 0.03). Nearly all respondents (92% initial, 89% follow-up; P = 0.6) were interested in technology to remotely assess oximetry or lung function.
Discussion
The COVID-19 pandemic led to healthcare delivery reorganization and rapid telehealth implementation for routine CF care. Our cross-sectional survey of clinicians indicates that although most had no prior experience using telehealth, clinicians found it to be highly satisfying and efficient and to have improved the clinician–patient relationship. Currently, no standardized format for telehealth delivery exists for CF or other pulmonary diseases. Our findings indicate that clinicians prefer the interdisciplinary care model and desire to continue to use telehealth for future routine ambulatory care and suggest durability of perceptions and preferences over the initial 6 months of use. Of the interdisciplinary care models, the asynchronous model became preferred over time by clinicians. This is likely related to improved clinician comfort with telehealth, adaptation of the telehealth care delivery model to improve visit efficiency, and its similarity to care delivery during in-person visits.
Our study also revealed an increase in perceived barriers to telehealth use over time (Figures 2A and 2B). In particular, it was anticipated that clinicians would have concerns surrounding missing components of routine assessment. When evaluating concern for these missing components by subtype (Figures 2C and 2D), pediatric and adult clinicians exhibited similar levels of concern over time. Interestingly, when asked about the perceived barrier these missing components imparted to telehealth use, adult clinicians perceived the barrier to decline whereas pediatric clinicians perceived an increase over the 6-month period. This may be related to pediatric clinicians’ concerns about technological limitations, concern surrounding missing the acquisition of new pathogens, or the potential for delayed diagnosis of a subacute exacerbation. Regarding the growing concern for technological limitations, it is unclear if these concerns are related to lack of institutional support, limitations among patients/families to technology to access visits, deficiencies in software interface, or a combination of the above. Interestingly, technological limitations appeared to be an area of growing concern among pediatric clinicians but not among adult clinicians. Future investigations should seek to further characterize these barriers, including the role of social determinants to help ensure the equitable provision of care. Furthermore, growing concerns surrounding regulation and reimbursement highlight the need for future policy and advocacy investigations.
Telehealth also allows for opportunities for technology innovation. For example, the majority of clinicians expressed that lack of pulmonary function testing testing imparted a moderate or greater difficulty to patient care. Clinicians also endorsed interest in technology to assess lung function remotely, and the provision of home spirometers via a current Cystic Fibrosis Foundation initiative could further enhance telehealth services. However, questions still remain about the accuracy of home spirometry (20, 21). The impact of telehealth on clinical and patient-reported outcomes remains unknown. Future studies should continue to explore the integration of innovative technologies into the care delivery model and focus on other areas of clinician concern such as microbiological culture acquisition and potential implications of Pseudomonas eradication in children.
Future investigations should address these gaps and continue to explore avenues to optimize the CF care delivery model (i.e., the optimal number of visits to perform by telehealth and alternative models of telehealth care delivery such as hybrid visits). Hybrid models may alleviate perceived barriers to care noted in our study by allowing a clinician to assess a patient in person, while also minimizing exposures.
Our study has several limitations. First, our study includes a small sample size of clinicians and may be subject to ascertainment bias. Furthermore, the second survey had reduced response at one of the survey sites, which is likely secondary to survey fatigue. The multicenter design of our study did, however, allow for sampling of clinicians from different regions and care center sizes across the country. Second, our study lacks long-term perception data, and it is feasible that clinician perception will change over time. We will collect long-term data to further assess the impact of continued exposure on the durability of perceptions. Finally, owing to the design of our study, we do not know the response rate of clinicians and cannot be sure how representative the responses are of the total experience of telehealth at the centers we surveyed.
Conclusions
In conclusion, we characterized telehealth usage patterns and preferences among a cohort of CF clinicians. Telehealth was well accepted, and our findings highlight the utility of telehealth for enhancing interdisciplinary CF healthcare delivery. Future studies are needed to understand its impact on clinical and patient-reported outcomes.
Acknowledgments
Acknowledgment
The authors thank all members of the multicenter collaboration that facilitated survey development and broad data collection, their clinician colleagues who participated in telehealth, and the Cystic Fibrosis Learning Network. Boston Children’s Hospital: Rachel Gordon, M.P.H., Katherine Barnico, R.N., Tregony Simoneau, M.D., Jenny Chan Yuen, M.S.P.H., and Suzanne Dahlberg for statistical analysis. Boston Children’s Hospital and Brigham and Women’s Hospital: Simona Rits and Lindsey McMahon, B.A., M.P.H. University of Virginia: Deborah Froh, M.D., and Rhonda List. Cincinnati Children’s: Lisa Mullen, M.H.S.A. Oregon Health & Science University: Ben McCullar, R.N.
Footnotes
Supported by U.S. National Institutes of Health grants 1K08HL138153-01A1 and 2P30DK072482-12 and by the Cystic Fibrosis Foundation (20Y0 [G.M.S.], AC004 [G.S.S.], and CC235 [A.U.]).
Author Contributions: R.C.P., J.D., A.N., J.B., M.R.P., N.C., C.S., A.U., G.M.S., and G.S.S. conceived of the study. R.C.P., G.M.S., and G.S.S. analyzed the data. R.C.P. wrote the original draft. All authors reviewed the final research letter before submission.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Gadzinski AJ, Ellimoottil C. Telehealth in urology after the COVID-19 pandemic. Nat Rev Urol. 2020;17:363–364. doi: 10.1038/s41585-020-0336-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kavousi Y, Al-Adas Z, Crutchfield JM, Karamanos E, Swanson C, Lin JC. Early clinical experience using telemedicine for the management of patients with varicose vein disease. J Telemed Telecare. 2019;25:54–58. doi: 10.1177/1357633X17734580. [DOI] [PubMed] [Google Scholar]
- 3. Qubty W, Patniyot I, Gelfand A. Telemedicine in a pediatric headache clinic: a prospective survey. Neurology. 2018;90:e1702–e1705. doi: 10.1212/WNL.0000000000005482. [DOI] [PubMed] [Google Scholar]
- 4. Lonergan PE, Washington Iii SL, Branagan L, Gleason N, Pruthi RS, Carroll PR, et al. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19: cross-sectional analysis. J Med Internet Res. 2020;22:e19322. doi: 10.2196/19322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berg EA, Picoraro JA, Miller SD, Srinath A, Franciosi JP, Hayes CE, et al. COVID-19-a guide to rapid implementation of telehealth services: a playbook for the pediatric gastroenterologist. J Pediatr Gastroenterol Nutr. 2020;70:734–740. doi: 10.1097/MPG.0000000000002749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lesher AP, Shah SR. Telemedicine in the perioperative experience. Semin Pediatr Surg. 2018;27:102–106. doi: 10.1053/j.sempedsurg.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 7. Fang JL, Collura CA, Johnson RV, Asay GF, Carey WA, Derleth DP, et al. Emergency video telemedicine consultation for newborn resuscitations: the Mayo Clinic experience. Mayo Clin Proc. 2016;91:1735–1743. doi: 10.1016/j.mayocp.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 8. Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, III, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28:e469–e476. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gadzinski AJ, Gore JL, Ellimoottil C, Odisho AY, Watts KL. Implementing telemedicine in response to the COVID-19 pandemic. J Urol. 2020;204:14–16. doi: 10.1097/JU.0000000000001033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016;79:169–176. doi: 10.1038/pr.2015.192. [DOI] [PubMed] [Google Scholar]
- 11. Eze ND, Mateus C, Cravo Oliveira Hashiguchi T. Telemedicine in the OECD: an umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS One. 2020;15:e0237585. doi: 10.1371/journal.pone.0237585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Donelan K, Barreto EA, Sossong S, Michael C, Estrada JJ, Cohen AB, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25:40–44. [PubMed] [Google Scholar]
- 13. Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31:269–275. doi: 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Xu CQ, Smith AC, Scuffham PA, Wootton R. A cost minimisation analysis of a telepaediatric otolaryngology service. BMC Health Serv Res. 2008;8:30. doi: 10.1186/1472-6963-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24:4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gur M, Nir V, Teleshov A, Bar-Yoseph R, Manor E, Diab G, et al. The use of telehealth (text messaging and video communications) in patients with cystic fibrosis: a pilot study. J Telemed Telecare. 2017;23:489–493. doi: 10.1177/1357633X16649532. [DOI] [PubMed] [Google Scholar]
- 17. Wood J, Mulrennan S, Hill K, Cecins N, Morey S, Jenkins S. Telehealth clinics increase access to care for adults with cystic fibrosis living in rural and remote Western Australia. J Telemed Telecare. 2017;23:673–679. doi: 10.1177/1357633X16660646. [DOI] [PubMed] [Google Scholar]
- 18. Compton M, Soper M, Reilly B, Gettle L, List R, Bailey M, et al. A feasibility study of urgent implementation of cystic fibrosis multidisciplinary telemedicine clinic in the face of COVID-19 pandemic: single-center experience. Telemed J E Health. 2020;26:978–984. doi: 10.1089/tmj.2020.0091. [DOI] [PubMed] [Google Scholar]
- 19. Perkins R, Davis J, Bailey J, NeSmith A, Solomon GM, Sawicki GS, et al. Telehealth implementation in cystic fibrosis care during COVID-19: the clinician experience. Poster session abstracts. Pediatr Pulmonol. 2020;55:S359. [Google Scholar]
- 20. Gerzon R, Jöbsis Q, Bannier M, Winkens B, Dompeling E. FEV1 measurement at home versus measurement in the hospital in children with asthma and cystic fibrosis. Eur Respir Soc. 2019;54:PA2679. [Google Scholar]
- 21.Berlinski A.Implementation of pediatric home spirometry: potential height bias J Cyst Fibros[online ahead of print] 29 Aug 2020 10.1016/j.jcf.2020.08.016 [DOI] [PubMed] [Google Scholar]