Abstract
Up to 50% of the people who have died from COVID-19 had metabolic and vascular disorders. Notably, there are many direct links between COVID-19 and the metabolic and endocrine systems. Thus, not only are patients with metabolic dysfunction (eg, obesity, hypertension, non-alcoholic fatty liver disease, and diabetes) at an increased risk of developing severe COVID-19 but also infection with SARS-CoV-2 might lead to new-onset diabetes or aggravation of pre-existing metabolic disorders. In this Review, we provide an update on the mechanisms of how metabolic and endocrine disorders might predispose patients to develop severe COVID-19. Additionally, we update the practical recommendations and management of patients with COVID-19 and post-pandemic. Furthermore, we summarise new treatment options for patients with both COVID-19 and diabetes, and highlight current challenges in clinical management.
Introduction
Although many people with SARS-CoV-2 infection show no or mild symptoms, the resulting systemic disease, COVID-19, has various presentations, including severe illness and fatal outcomes.
Around a fifth of the global population is affected by one or more chronic conditions, putting them at increased risk of severe COVID-19 (defined as fever and at least one sign or symptom of respiratory disease and requirement for hospitalisation), if infected with SARS-CoV-2.1 Underlying conditions were reported in more than 50% of patients with COVID-19 and around a third of patients had multiple comorbidities.2 Age and comorbidities that are common in older people (eg, ≥65 years), such as obesity, diabetes, hypertension, and pulmonary, cardiovascular, kidney, and non-alcoholic fatty liver disease, influence the progression and prognosis of COVID-19.3, 4, 5, 6, 7, 8 Additionally, COVID-19 in conjunction with type 2 diabetes and obesity, which are both characterised by severe insulin resistance,9 has numerous consequences. BMI is strongly correlated with immune signatures that predict severe COVID-19.10 Distinct immunological signatures discriminate severe COVID-19 from critical pneumonia that is not driven by SARS-CoV-2,10 and the presence of obesity might shift severe manifestations of COVID-19 to younger age groups (aged <50 years), as reported by researchers at Johns Hopkins.11 Additionally, underlying diseases might be aggravated, increasing the susceptibility of patients to serious long-term consequences.12, 13 The severity and mortality of COVID-19 associated with these medical conditions showed considerable geographical differences.2 Deprived populations with scarce access to health services in normal circumstances are most vulnerable during times of crisis.14 Furthermore, in some low-income and middle-income countries, a high socioeconomic status is sometimes associated with obesity; whereas, in high-income countries, the inverse is often the case.15 In countries with a low prevalence of obesity, the fatality rates from COVID-19 have been lower than in countries with a high prevalence of obesity, although potential confounders should be taken into account.15
Now, more than 1·5 years after the initial outbreak of SARS-CoV-2, there is strong evidence that people with metabolic diseases are not only more susceptible to severe COVID-19, but also have an increased risk of post-acute sequelae of COVID-19 and vaccine breakthrough.16, 17, 18
Metabolic and endocrine pathways linked to SARS-CoV-2
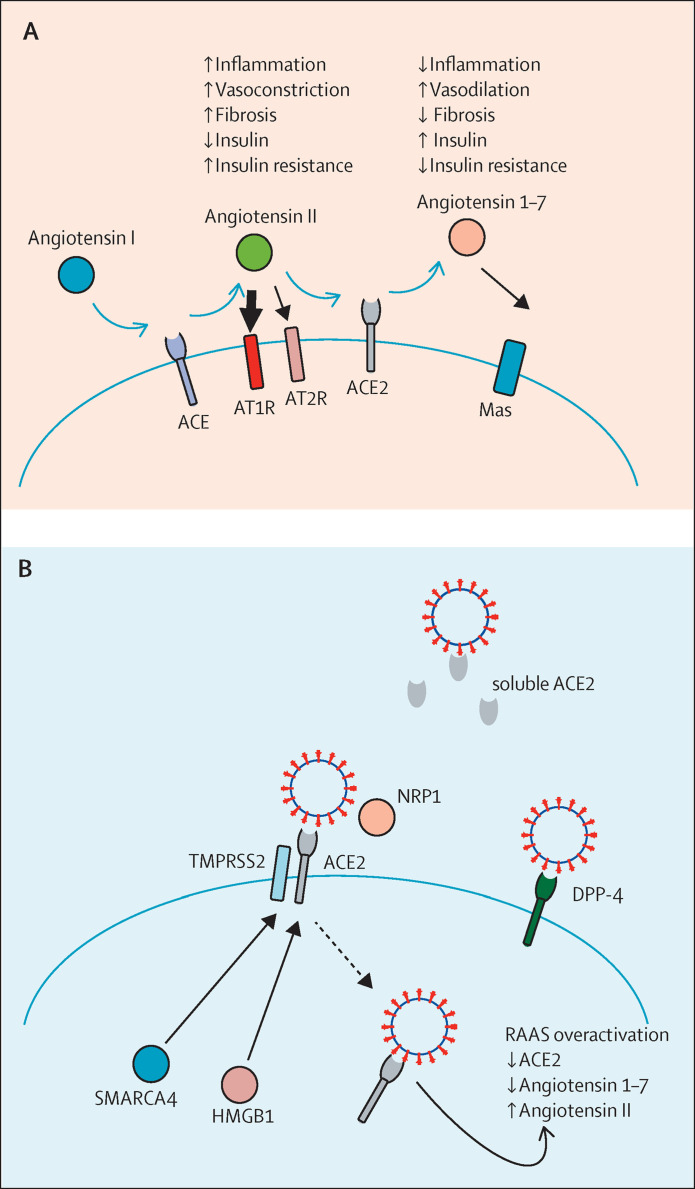
Entry of SARS-CoV-2 into cells is mediated via binding of viral spike glycoproteins to cellular angiotensin-converting enzyme (ACE) 2. In the renin–angiotensin–aldosterone system (RAAS), ACE2 acts as key regulator, controlling the generation of the vasodilating angiotensin 1–7 from angiotensin II. Furthermore, ACE2 is able to cleave angiotensin I to angiotensin 1–9, which can be further converted to angiotensin 1–7 by ACE. ACE2, angiotensin 1–7, and its Mas receptor constitute the vasoprotective arm of the RAAS, leading to anti-inflammatory and antifibrotic responses (figure 1 A).19 However, when ACE activity is high and ACE2 is inhibited, angiotensin II acts via the angiotensin II receptors, AT1R and AT2R, to exert proinflammatory responses and to stimulate aldosterone production. Therefore, deregulation of the ACE or ACE2 balance can lead to arterial hypertension accompanied by an exaggerated inflammatory response, which, in the absence of adequate intervention, might culminate in end-organ damage.20
Figure 1.
The RAAS in COVID-19
(A) When the RAAS is activated, angiotensinogen produced in the liver is cleaved to angiotensin I in the kidney. Angiotensin I is further converted to angiotensin II by ACE. Angiotensin II binds to its receptors, AT1R and AT2R, causing the release of aldosterone from the zona glomerulosa in the adrenal cortex. In the second part of the RAAS, angiotensin II is converted by ACE2 to the vasodilatory angiotensin 1–7, which binds to its Mas receptor, thereby possessing opposing actions of angiotensin II and ACE. (B) ACE2 consists of two forms, a membrane-spanning protein and a circulating soluble form, both capable of binding to the spike protein on the surface of SARS-CoV-2. Expression of ACE2 is regulated by HMGB1 and SMARCA4. Following infection with SARS-CoV-2, the viral spike protein is cleaved by TMPRSS2 and the membrane form of ACE2 is internalised with the virus, leading to a decrease in ACE2. This stage might result in overactivation of the ACE or angiotensin II part of the RAAS, thereby augmenting signalling through AT1R and AT2R. Virus entry is facilitated by NRP1, which promotes the interaction between SARS-CoV-2 and ACE2. A suggested alternative receptor for virus entry is DPP-4. RAAS=renin–angiotensin–aldosterone system. ACE=angiotensin-converting enzyme.
Cellular concentrations of ACE2 depend on several factors, such as other RAAS components, gene polymorphisms, and clinical conditions (eg, hypertension and vascular diseases).21 ACE2 is expressed in many tissues and cell types; therefore, at the onset of the pandemic, high ACE2 expression was speculated to be partly responsible for infection with SARS-CoV-2.22 In the endocrine system, ACE2 is expressed in all organs of the hypothalamus–pituitary–adrenal cortex (HPA) axis;23 however, contradicting results have been presented in pancreatic islets. Some reports show no expression of ACE2 in the islets of Langerhans but in pancreatic epithelial cells only,24, 25, 26 whereas other studies in patients without COVID-19 have shown expression of ACE2 in β cells.27, 28, 29 A sub-group of authors of this Review previously investigated expression of ACE2 and SARS-CoV-2 infection of β cells in 11 patients who died due to COVID-19.30 Compared with other study cohorts of just one to three patients, we observed that only around 30% of the patients expressed ACE2 in β cells, indicating that other factors were also involved in the infection. Whether the expression of ACE2 observed in some patients with COVID-19 was due to the infection itself or, conversely, that these patients were infected due to the high expression of ACE2, remains uncertain. Expression of ACE2 is increased following inflammatory stress, which suggests enhanced β-cell sensitivity to SARS-CoV-2 during inflammatory conditions.27
Following binding of SARS-CoV-2 to ACE2, the receptor is internalised by the infected cell, leading to a distinct downregulation of ACE2. This downregulation of ACE2 in the intestinal epithelium has been suggested to lead to upregulation of SGLT1, thereby precipitating hyperglycaemia.31 Furthermore, the protective arm of the RAAS is potentially removed, which might lead to a multiorgan hyperinflammatory response (ie, cytokine storm). Thus, the RAAS and, in particular, ACE2 seem to offer attractive therapeutic targets against COVID-19.32 Although medications, such as ACE inhibitors and angiotensin II receptor blockers, could increase ACE2 expression and potentiate SARS-CoV-2 cell entry,33 increased ACE2 production would result in a higher circulating concentration of soluble ACE2, which would potentially neutralise SARS-CoV-2 (table 1 ).36 Use of ACE inhibitors or angiotensin II receptor blockers has been reported to be higher in patients with COVID-19 than in patients without, which is caused by the higher prevalence of COVID-19 among people with hypertension, cardiovascular, and renal diseases.48, 49, 50 Nevertheless, to the best of our knowledge, none of the observational studies performed to date has shown an association between the use of ACE inhibitors or angiotensin II receptor blockers and disease outcome, severity, or death.37 Significant and independent associations between plasmatic aldosterone and C-reactive protein concentrations and the severity of COVID-19 have been reported.51
Table 1.
Glucose-lowering medications with potential interfering effects on COVID-19
| Potential positive effects | Potential negative effects | |
|---|---|---|
| Glucocorticoids34, 35 | Anti-inflammatory effects | Risk of hyperglycaemia |
| ACE inhibitors and angiotensin II receptor blockers33, 36, 37 | Increases expression of soluble ACE2; neutralises virus | Increased expression of membrane-bound ACE2 might increase virus entry (no clinical evidence) |
| Metformin38, 39 | Stabilises ACE2; modulates ACE2–angiotensin II–AT1R axis; inhibits host–virus binding; inhibits mitochondrial complex I; protects endothelium and vasculature; decreases virus maturation | Risk of dehydration, lactic acidosis, chronic kidney disease, and acute kidney injury |
| SGLT2 inhibitors22, 40 | Reduces viral load; positive effects on cardiovascular and renal functions | Risk of dehydration, diabetic ketoacidosis, and acute kidney injury |
| GLP-1 receptor agonists22, 41, 42 | Anti-inflammatory effects; improves endothelial dysfunction; improves cardiovascular and renal functions | Reduces appetite and increases satiety; gastrointestinal symptoms |
| DPP-4 inhibitors40, 43, 44 | Blocks virus uptake; reduces inflammatory response; well tolerated | Increases mortality in older patients (likely due to confounding by indication) |
| Insulin22, 45, 46, 47 | Anti-inflammatory effects | Hypoglycaemia; high doses increase COVID-19 mortality |
Of note, many of these results are retrospective and confounded by indications, patients' risk profiles, or severity of diseases. ACE=angiotensin-converting enzyme.
SARS-CoV-2 spike proteins require two proteolytic processing steps before cell entry. These steps are mediated by host-cell proteases, such as furin, TMPRSS2, and cathepsin L, leading to fusion of the viral envelope and the plasma or endosome membrane of the host cell (figure 1B).52, 53
At the time of writing, a number of new variants of the original SARS-CoV-2 strain have emerged, which are up to 90% more contagious.54, 55, 56 The alpha (B.1.1.7), beta (B.1.351), and gamma (P.1) variants are mutated in the receptor binding domain of the spike protein, whereby the binding affinity to ACE2 is increased.57 Another lineage, the delta (B.1.617.2) variant, has an even higher affinity for ACE2 than do other variants, and shows increased transmissibility.58 Thus, blocking the interaction between ACE2 and the receptor binding domain could be a potential approach to inhibit transmission of and infection with SARS-CoV-2,53 and the SARS-CoV-2 receptor binding domain could serve as a central target for conceiving therapeutic strategies against COVID-19.59
Additional factors expressed in pancreatic β cells have been identified as crucial for infection with SARS-CoV-2 (figure 1B).29, 30 NRP1, known to bind furin-cleaved substrates, facilitates SARS-CoV-2 entry and infectivity,60 suggesting that virus entry is increased in cells with a low expression of ACE2 due to promotion of the interaction between SARS-CoV-2 and ACE2 via NRP1. In addition, HMGB1, a DNA-binding protein that regulates chromatin and is known to be proviral, was shown to regulate the expression of ACE2 and be essential for viral entry.61 Furthermore, HMGB1 is released from necroptotic cells, and systemic concentrations of TNFα and IFNγ were shown to cause necroptosis in individuals with SARS-CoV-2 infection.62 Along similar lines, the key kinase mediator of necroptosis, RIPK3, is strongly upregulated in patients with severe COVID-19,63 indicating a feed-forward loop of cell death and inflammation.64 Alongside HMGB1, members of the switching defective–sucrose nonfermenting chromatin-remodelling complex, such as SMARCA4, regulate the expression of ACE2 (figure 1B).61 These alternative factors are potential new therapeutic targets for inhibiting SARS-CoV-2 infection.
The MERS-CoV receptor, DPP-4, has also been suggested as an alternative receptor for SARS-CoV-2.65 DPP-4 has been shown to be expressed by cells of the immune system, on epithelial and endothelial cells in the pancreas, lung, and kidney,66 and in both the exocrine and endocrine pancreas.30 DPP-4 is an aminopeptidase with an important role in glucose metabolism, and DPP-4 inhibitors are widely used for the treatment of type 2 diabetes.67 First reports did not show any clinical evidence to suggest that drugs targeting pathways related to DPP-4 exhibit any benefits or harm in relation to human coronavirus infections.68 However, a study with 2·8 million people showed worse COVID-19 outcomes in patients with diabetes receiving DPP-4 inhibitors than in those who had not received such treatment, although this finding was probably due to confounding by indication.40 Reports have since suggested improved clinical outcomes and a reduced risk of mortality in patients with COVID-19 and diabetes receiving DPP-4 inhibitor therapy (table 1).43, 44 These contradictory results from observatory studies emphasise the importance of well designed randomised, double-blind, placebo-controlled clinical trials to ascertain a potential benefit.
Predisposition to severe COVID-19 outcomes in patients with metabolic and endocrine diseases
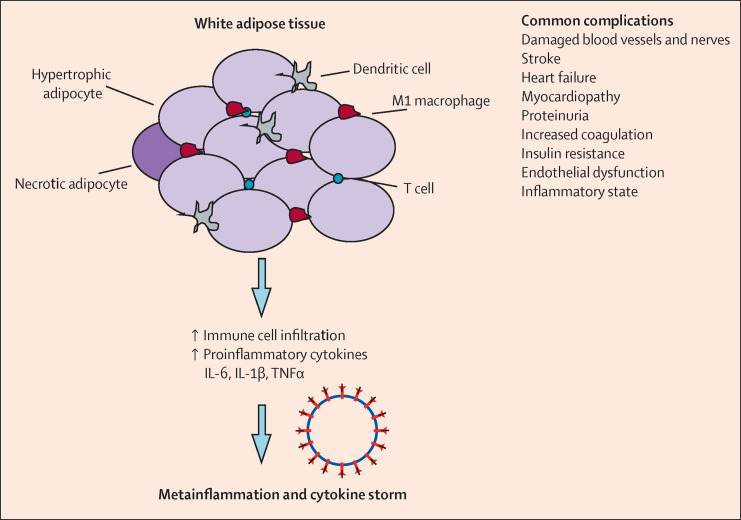
Excess adiposity is a risk factor for severe COVID-19 and mortality though a number of mechanisms, including increased inflammation, hypercoagulation, and mechanical obstruction.69 One explanation for the predisposition to poor outcomes in patients with severe COVID-19 and obesity might be the physical stress on ventilation through obstruction of diaphragm excursion. Furthermore, diabetes and obesity are associated with an increased risk of pulmonary fibrosis, chronic obstructive pulmonary disorder, and reduced respiratory function.70 Obesity, diabetes, and hypertension increase the risk of stroke and cardiovascular complications,71 risk factors that are also observed in patients with severe COVID-19 (figure 2 ). These patients exhibit an exacerbated coagulation response due to overexpression of prothrombotic factors, such as coagulation factors (II, VII, VIII, IX, XI, and XII), PAI-1, and von Willebrand factor, which, in combination with pre-existing conditions, could increase the probability of stroke or pulmonary embolism.3, 72, 73
Figure 2.
Clinical manifestations and complications of diabetes or obesity and COVID-19
In the white adipose tissue of individuals with obesity, adipocytes are hypertrophic and the tissue is infiltrated with proinflammatory immune cells that secrete cytokines, chemokines, and adipokines, leading to a permanent inflammatory phenotype. In diabetes, insulin resistance also leads to an increased infiltration of M1 macrophages into adipose tissue. Following infection with SARS-CoV-2, this chronic inflammation might aggravate COVID-19 symptoms in a synergy effect, resulting in metaflammation and a cytokine storm, which contribute to severe COVID-19.
Metabolic dysfunction might lead to a baseline state of chronic inflammation, given that proinflammatory cytokines, such as TNFα, IL-6, and IL-1β, are upregulated in the adipose tissue of patients with metabolic syndrome. These cytokines inhibit insulin signalling.74 In turn, cytokine upregulation results in paracrine and endocrine effects, which lead to an increase in leptin and PAI-1, and a reduced release of adiponectin.75 Thus, metabolic organs, such as white adipose tissue, skeletal muscle, the liver, and the pancreas, are infiltrated with macrophages and other immune cells (figure 2).76 In diabetes, insulin resistance leads to an increased infiltration of macrophages into adipose tissue, especially M1 macrophages.77 Obesity is also associated with a high baseline expression of the IL-6 receptor. Compared with individuals without overweight, the expression of the IL-6 receptor in individuals with obesity is not downregulated by an increased cytokine concentration, therefore leading to a constant low-grade inflammatory state, termed metaflammation.78 Dysfunction in insulin signalling further contributes to chronic inflammation via activation of AP-1 and NFkB, leading to a decrease in anti-inflammatory cytokines and an increase in TNFα, IL-6, and IL-1β. This shift from a predominantly anti-inflammatory profile to a proinflammatory profile enhances insulin resistance.79
Type 2 diabetes is a progressive disease due to insulin resistance, together with chronic inflammation and endothelial and β-cell dysfunction.80 In severe COVID-19, the inflammatory response to SARS-CoV-2 infection can worsen insulin resistance and endothelial dysfunction (figure 2). Synergy between COVID-19 and type 2 diabetes and obesity might further amplify the inflammatory response and downregulate interferon responses, contributing to increased disease severity in patients with diabetes and obesity.12 Dysregulation of the RAAS and downregulation of ACE2 expression, in conjunction with stress signalling, can increase insulin resistance.77 Thus, insulin resistance, by triggering airway hyper-reactivity, increases the risk of respiratory failure and cardiopulmonary collapse in patients with diabetes and COVID-19.77
Besides their role in the immune response against viral infections, cytokines activate the HPA axis, resulting in the release of adrenal glucocorticoids.81 In turn, glucocorticoids produce negative feedback on immune cells to suppress further synthesis and release of cytokines. Thereby, the host receive a partially protective signal against the destructive consequences of an overactive immune response, such as tissue damage, autoimmunity, or septic shock.34, 82 Such effects have been clinically reported during dexamethasone administration, which, at the time of writing, is the most effective treatment for patients with severe COVID-19 with pulmonary involvement.34 Furthermore, inhaled glucocorticoids (eg, budesonide) have been shown to reduce the time to partial recovery after early COVID-19.83 These findings have led to the widespread use of glucocorticoids to treat patients with not only moderate-to-severe but also, frequently, mild forms of COVID-19 (table 1).
Diseases of the HPA axis are per se not expected to increase the risk of severe COVID-19. However, hormonal replacement therapies or immunosuppression might increase the possibility of an undesirable outcome. Thus, patients with primary or secondary adrenal insufficiency are at increased risk of poor prognosis if the glucocorticoid replacement therapy is not adequately controlled.84
A prospective study in patients with renal disease showed that full vaccination with the mRNA-1273 vaccine (Moderna) induced a seroconversion rate of 95% in patients on dialysis, whereas this rate was markedly impaired in recipients of kidney transplants (42%).45 Seroconversion rates were lower in both of these patient subgroups vaccinated with the BNT162b2 mRNA vaccine (Pfizer–BioNTech).45 Furthermore, immunosuppressive drug number and type were major determinants of seroconversion failure in patients on dialysis and in transplant recipients, suggesting immune monitoring and adaption of vaccination protocols for these patients.
Effects of SARS-CoV-2 on the metabolic and endocrine systems
Following infection with SARS-CoV-2, toll-like receptors 2, 3, and 4 are activated, and IL-1β and IL-6 are released.85 The metaflammation observed in patients with metabolic disorders allows for a hyperimmune response, which reaches pathogenic levels. This cytokine release provokes fever, systemic inflammation, and subsequent sepsis.85
In terms of the pathophysiology, endocrine and metabolic organs (including the brain, pancreas, liver, skeletal muscle, and adipose tissue) might be damaged either directly or indirectly by viral infection and contribute to the development of new-onset hyperglycaemia or insulin resistance in survivors of COVID-19. Based on experiments in islets isolated from human donors and infected with SARS-CoV-2, and on data from post-mortem tissue from patients who died due to COVID-19, SARS-CoV-2 can infect and replicate in cells of the endocrine and exocrine pancreas.28 Furthermore, infiltration with immune cells and signs of necroptosis in the exocrine and endocrine pancreata have been observed in patients with COVID-19.30 These findings could imply that β-cell infection with SARS-CoV-2 might lead to either direct or indirect impairment of β-cell function, causing variable degrees of metabolic dysregulation.
New-onset hyperglycaemia, ketoacidosis, diabetes, and severe metabolic complications of pre-existing diabetes have been frequently observed in patients with COVID-19.86, 87, 88, 89, 90, 91, 92 Data from the German Diabetes Prospective Follow-up Registry, a nationwide registry with a coverage of more than 90% of paediatric patients with type 1 diabetes, have shown a significant increase in diabetic ketoacidosis and severe ketoacidosis at diabetes diagnosis during the COVID-19 pandemic, especially in children younger than 6 years.93 Of note, indirect effects, such as changes in parental behaviour and health-care accessibility, might have also had an influence on the increase in prevalence of new-onset type 1 diabetes in children.94 Nevertheless, evidence is accumulating suggesting COVID-19 as a cause or trigger of new-onset diabetes.17 Observations of pancreatitis following COVID-19 have also been reported.95 Nonetheless, whether COVID-19 can directly or indirectly lead to new-onset diabetes or accelerate pre-existing unrecognised diabetes or prediabetes remains a subject of discussion.96 As such, this notion is currently being examined in a global registry, CoviDiab.92 Furthermore, a group of international software developers, data scientists, and health professionals have built a non-for-profit graph database, CovidGraph, to make all information related to COVID-19 searchable and accessible in one database.
Implications for medications and therapy
Diabetes and obesity are among the main risk factors associated with morbidity in patients with COVID-19. Reducing the risk factors associated with COVID-19 morbidity could be a reasonable goal for public health (panel ). Apart from medical considerations, patients with chronic conditions have been especially vulnerable throughout the pandemic due to reduced access to medical care and personal insecurity due to quarantine measures. In many places around the world, access to diabetes care has been reduced, and patients have been reluctant to access on-site medical care because of fear of exposure to SARS-CoV-2 infection on medical premises. A global survey of health-care professionals reported that management of diabetes and hypertension was often disrupted during the pandemic.105 Additional complications have also resulted from considerable reductions in physical activity, changes in eating habits, and associated-weight gain. Overall, physical activity was lower in adults with type 2 diabetes during lockdown restrictions, particularly in women, older people, individuals with obesity, and minority ethnic populations.106 Despite the expected negative impact of lockdown, retrospective analyses have not reported a worsening of glucose control due to lifestyle changes.107
Panel. Current recommendations of metabolic disease management in a pandemic situation.
-
•
Encourage patients to restrict social contact to reduce risk of infection97
- •
-
•
Encourage patients to incorporate a healthy lifestyle during lockdown and quarantine22
-
•
Individual management: help patients to establish an individual set of self-management goals (eg, measurement rate, bodyweight, steps per day, waist circumference, blood pressure) and to adhere to these goals consistently100
-
•
Digital support: help patients to make use of online education, virtual consultation, and digital health (eg, measurements of temperature, physical activity, bodyweight, waist circumference, and blood pressure, which will be digitally transferred to the physician)101
-
•
Behavioural support: help patients to use digital stress management tools to increase resilience and stress resistance102
-
•
Intensify foot care103
-
•
Check for new diabetes90
-
•
Manage cardiac risk9
- •
-
•
Monitor urinary excretion and oedema in patients with chronic kidney disease12
-
•
Optimise metabolic and blood pressure control101
-
•
Perform intensified glucose monitoring (eg, self-monitoring of blood glucose five times per day, flash and continuous glucose monitoring) to identify early deterioration of glycaemic condition and monitor blood pressure if hypertensive101
-
•
Avoid grade 2 hypoglycaemia (2·2–3·0 mmol/L [40·0–55·0 mg/dL]) and grade 3 hypoglycaemia (1·7–2·2 mmol/L [30·0–40·0 mg/dL])104
-
•
Target ranges:22
-
•
Fasting plasma glucose concentration: 4·0–8·0 mmol/L (72·0–144·0 mg/dL)
-
•
Fasting plasma glucose concentration of patients in intensive care: 6·7–11·1 mmol/L (120·0–200·0 mg/dL)
-
•
HbA1c: <53·0 mmol/mol (7%)
By contrast, it is evident that an endemic increase in excess weight and obesity in the global population, suggested to have caused more than a doubling of the number of people with type 2 diabetes over the past two decades, has now contributed to an excess of deaths due to COVID-19.108 Therefore, there is an urgent need for expert advocacy in societal changes for the prevention of type 2 diabetes and obesity, directed at improving the diet and lifestyle of populations. Individually targeted, evidence-based health promotion, weight management, behavioural change, and psychosocial support services need vigorous support from diabetologists and other health professionals on the front-line.109
An increase in perceived stress has been shown to be associated with reduced glycaemic control and increased risk of COVID-19.110, 111 Strategies to avoid physical inactivity and reduce stress levels can promote cardiovascular protection, and have to be considered during the pandemic. Promotion of physical activity is prioritised by public health agencies and has been incorporated into routine medical care (panel). A home-based training protocol could be an important and effective strategy for individuals who need to remain safe and physically active at home.112 The interlinked pathological mechanisms between metabolic diseases and COVID-19 create the pathophysiological basis for how to treat diabetes and control dysglycaemia. Managing patients with type 2 diabetes should always include a component of reducing or eliminating insulin resistance in these patients, as well as reducing hyperglycaemia (panel).
In the past 18 months, we have gained substantial insights into the association of glucose-lowering therapies and drug classes, and their association with mortality related to COVID-19 (table 2 ).77, 113 These findings indicated that there is no reason to cease antidiabetic or hypertensive medication during the pandemic. However, as most studies were observational, performed retrospectively, and might have been affected by confounding by indication, well designed clinical studies are urgently needed. Until now, DARE-19 is the only published, randomised, double-blind, placebo-controlled trial of a glucose-lowering agent in patients hospitalised with COVID-19 with at least one cardiometabolic risk factor.114 This trial, which excluded critically ill patients, suggested that the SGLT2 inhibitor, dapagliflozin, was safe and well tolerated, but did not result in a significant risk reduction in organ dysfunction or death, nor in an improvement in clinical recovery.114 Another observational study investigating SGLT2 inhibitors in patients with type 2 diabetes and COVID-19 was associated with an 18% reduction in mortality.77 However, this finding was probably due to confounding by indication, given the reduced use of this drug class in older people, particularly those with renal insufficiency and frailty. Caution should be taken when using these drugs because they require hydration and appropriateness of insulin doses to prevent euglycaemic or hyperglycaemic ketoacidosis (table 1).
Table 2.
| No COVID-19 | Mild COVID-19 (primary care) | Moderate COVID-19 (hospital) | Severe COVID-19 (intensive care) | |
|---|---|---|---|---|
| Recommendations according to guidelines | Metformin; DDP-4 inhibitors; SGLT2 inhibitors; GLP-1 receptor agonists; sulfonylurea; α-glucosidase inhibitors; thiazolidinedione; insulins | Metformin; DPP-4 inhibitors; SGLT2 inhibitors; GLP-1 receptor agonists; insulins; sulfonylurea; α-glucosidase inhibitors | DPP-4 inhibitors; SGLT2 inhibitors; GLP-1 receptor agonists; insulins | DPP-4 inhibitors; insulins |
| Use with caution | NA | Thiazolidinedione | Metformin; α-glucosidase inhibitors; SGLT2 inhibitors | NA |
| Contraindications | NA | NA | Thiazolidinedione; sulfonylurea | Metformin; α-glucosidase inhibitors; SGLT2 inhibitors; thiazolidinedione |
NA=not applicable.
In addition to the findings that dapagliflozin had no negative effect on predisposition to SARS-CoV-2 infection or aggravation of the disease course, there have been suggestions that DPP-4 inhibitors and metformin might even exert protective effects against SARS-CoV-2 infection (table 1).38, 39 Various multicentre observational studies have reported either no or reduced association with the use of DPP-4 inhibitors and mortality related to COVID-19.40, 43, 44, 115, 116, 117 DPP-4 inhibitors belong to a group of drugs associated with many advantages (ie, they are well tolerated by patients with diabetes), even in severe cases of COVID-19 (table 2). This drug class is well tolerated; can be used adapted by dose, even in end-stage renal disease (except for saxagliptin); and has a low risk of hypoglycaemia. As mentioned earlier in this Review, in a UK analysis, people older than 70 years receiving DPP-4 inhibitor therapy had a slightly increased risk of mortality.40 However, this result was probably due to confounding by indication since DPP-4 inhibitors are more likely to be used in older people and in patients with kidney disease and frailty. This study, which was a large, nationally representative, population-based observational study of 2·85 million people with type 2 diabetes also presented statistical evidence that patients who were prescribed metformin, SGLT2 inhibitors, and sulfonylureas had a lower mortality risk than did patients who did not use these medications.40 In this cohort, α-glucosidase inhibitors were associated with a 26% increase in COVID-19 mortality; however, the number of deaths related to COVID-19 was too small to evaluate. Use of α-glucosidase inhibitors should be carefully considered.40
Metformin seems to be an effective therapy with pleiotropic effects for patients in acute, chronic, and even recovery phases of COVID-19.118, 119 However, some observational studies have shown a marked increase of lactic acidosis in hospitalised patients with diabetes and COVID-19 on metformin, albeit without an effect on mortality.120
The continued use of sulfonylurea might be justified in stable patients with COVID-19 who are not at risk of hypoglycaemia and have regular meals in an ambulatory setting.77 GLP-1 receptor agonists appear to be neutral to COVID-19 mortality and should be carefully evaluated in severely ill patients with COVID-19, considering their anorexic effects. However, their potential benefits should also be balanced, given that these drugs have anti-inflammatory actions and protective effects on the lung, and could be effective against COVID-19.41, 42
To reduce cytokine release in patients with moderate-to-severe COVID-19, IL-6 receptor blockade with tocilizumab is used.121 This treatment has been reported to have a positive effect on insulin resistance and insulin sensitivity.122 However, hyperglycaemia has been shown to impair the effectiveness of this medication,123 which further emphasises the importance of glycaemic control in patients with COVID-19.
It is important to differentiate between ongoing diabetes treatment and treatment of hyperglycaemia arising during acute SARS-CoV-2 infection. Currently, there is a strong rationale to maintain recommendations to avoid treatment with metformin or SGLT2 inhibitors in patients with severe COVID-19 to reduce the risk of lactic acidosis or ketoacidosis associated with use of these drugs in the presence of severe infection. In patients with severe COVID-19, intravenous insulin treatment is essential to maintain adequate glycaemic control and to avoid the development of acidosis. In many cases, insulin requirements are extremely high, reflecting the impact of the hyperinflammatory state on insulin resistance.77 Insulin also has anti-inflammatory effects through the suppression of oxidative and inflammatory stress.46 Many patients previously on oral hypoglycaemic agents will require conversion to insulin during the acute stages of COVID-19, and will require ongoing treatment with subcutaneous insulin following hospital discharge. Managing decreasing insulin requirements during the recovery stage and reducing insulin appropriately to avoid hypoglycaemia are important considerations in patients with diabetes recovering from COVID-19.
Importance of risk stratifications
In addition to a potential risk of developing type 1 diabetes,17 impairment of islet function in people with metabolic disorders should be considered after infection with SARS-CoV-2.5, 22, 124 Even without extensive destruction of islets, many patients are likely to need enhanced treatment with insulin to avoid ketoacidosis and hyperglycaemia, both of which need to be closely monitored. Patients with obesity also have an increased insulin requirement due to impaired insulin secretion and increasing insulin resistance, which might contribute to their increased risk of mortality. Furthermore, based on findings from the Recovery Trial,34 nearly all patients with severe COVID-19 are now receiving dexamethasone, a powerful anti-inflammatory glucocorticoid. Although dexamethasone inhibits inflammation,125 it is still a matter of debate whether steroid-induced hyperglycaemia, which increases the need for insulin therapy shortly after application (ie, within 4–6 h), is due to impaired insulin secretion, worsening of insulin action, or both.126 By contrast, patients with type 2 diabetes and COVID-19 receiving insulin treatment had a worse prognosis, with increased mortality associated with insulin therapy, compared with their counterparts who had not received insulin treatment.47 This finding is probably explained by confounding with severity of disease, given that insulin treatment is a marker for advanced diabetes.77 Although insulin treatment in the intensive care unit (ICU) is not debatable, hyperglycaemia in people with diabetes admitted to ICU should be handled by intravenous insulin using exact dosing with a perfusion device. Frequent glucose monitoring is mandatory with use of glucocorticoid and anti-inflammatory drug therapy, and prophylactic anticoagulant therapy should be provided in patients with diabetes and COVID-19.113 Importantly, the US Food and Drug Administration has issued guidance on an emergent basis to expand the availability and capability of non-invasive, remote monitoring devices for patients with diabetes during the COVID-19 pandemic.127 This change was made in an effort to improve the ability of health-care providers to monitor patients while reducing their exposure to SARS-CoV-2. Both hyperglycaemia and hypoglycaemia are associated with poor survival in patients with COVID-19. Fasting blood glucose concentration in patients with COVID-19 with or without diabetes at admission was a strong predictor of death among patients directly admitted to ICU,128 and severe hyperglycaemia after admission was a strong predictor of death among patients not in ICU.129 Almost 50% of hospitalised patients with COVID-19 were hyperglycaemic and even normoglycaemic patients showed alterations in their glycaemic control, with insulin resistance and an abnormal cytokine profile.90 It was also found that less variability in glucose excursions measured as time in range was associated with a lower risk of all-cause mortality and cardiovascular mortality among patients with type 2 diabetes.130 These findings indicate that acute hyperglycaemia and long-term glycaemic control are essential in patients with COVID-19 and that short-term glycaemic control might improve the prognosis; however, it is still not established whether acute hyperglycaemia is an aetiological factor driving poor prognosis or whether it simply reflects the severity of the disease.113
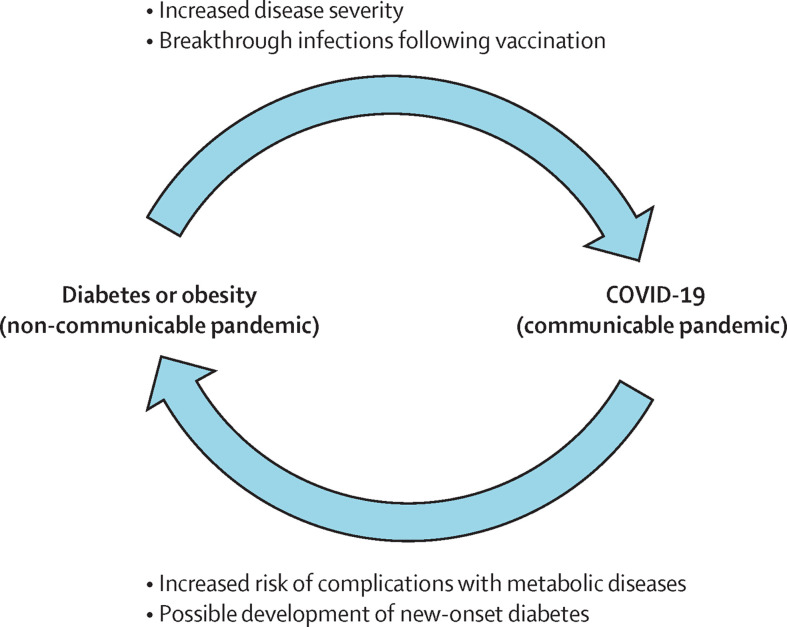
Breakthrough infections and metabolic disease
Accumulating evidence, including data from Israel, show that, even with a complete vaccination, patients can be infected with particular SARS-CoV-2 mutants, such as the delta variant.16 Most importantly, despite being fully vaccinated, patients who developed severe symptoms of COVID-19 frequently had comorbidities, such as hypertension (71%), diabetes (48%), congestive heart failure (27%), and chronic kidney disease (24%).16 Given how patients with diabetes and metabolic disease seem to be the most susceptible to developing severe symptoms of COVID-19, regardless of vaccination status, the necessity for adequate control of glycaemia and blood pressure in older populations, even after a successful vaccination programme, has to be maintained with high priority (figure 3 ).
Figure 3.
Interplay between metabolic diseases and COVID-19
On one hand, metabolic diseases increase the risk of severe COVID-19. On the other hand, COVID-19 might lead to new-onset metabolic diseases or worsening of already existing metabolic disorders.
Long-term consequences and monitoring after COVID-19
Evidence from the outbreak of the closely related SARS-CoV in 2002–03 suggests that there is a likelihood of long-term metabolic sequelae from COVID-19. Long-term metabolic abnormalities have been observed for up to 12 years in survivors of severe acute respiratory syndrome. These abnormalities included dyslipidaemia and cardiovascular disease, as well as signs of abnormal glucose metabolism with insulin resistance, hyperglycaemia, and diabetes.131, 132 Furthermore, a chronic post-viral syndrome characterised by chronic fatigue, variable non-specific myalgia, depression, and sleep disorders was observed.133 Similar long-term consequences of COVID-19, termed post-COVID and long COVID syndromes,134 or post-acute sequelae of COVID-19, have been reported.18 It was shown that, beyond the first 30 days of illness, survivors of COVID-19 exhibited a significantly higher risk of death and health resource use.135 In relation to metabolic diseases, a study from Spain, which investigated the long-term outcomes of 766 patients with COVID-19 1 year after hospital discharge, showed that seven (1%) of the 543 patients who were alive after 1 year and provided data had developed new-onset diabetes and that 11 (10%) of the 109 patients who had diabetes had worsening of glycaemic control.17 A study from Italy showed that glycaemic abnormalities could be detected at least 2 months after recovery from COVID-19.90
COVID-19 survivors frequently develop physical, psychosocial, and cognitive impairments that require rehabilitation programmes.136 Prolonged exposure to stressors, such as those experienced through isolation, increases the risk of developing major depression, anxiety, and post-traumatic stress disorders.137 Furthermore, following treatment in ICU, persistent impairment in mental health is commonly described and a high prevalence of depression has been observed.138 It should also be considered that particular therapies affecting expression of ACE2 (eg, ACE inhibitors or angiotensin II receptor blockers) might also influence the RAAS and neuroendocrine stress axis.36 Other unexpected complications can occur after COVID-19, such as invasive fungal sinusitis (mucormycosis), which usually affects people with poor immunity or uncontrolled diabetes.139 Steroid treatment is another risk factor for mucormycosis, meaning that the high doses of steroids administered to patients with severe COVID-19 might induce this side-effect, as shown in India.140
Patients admitted to hospital with COVID-19 will need close monitoring for risk factor control following discharge, with potential use of novel therapies to reduce the risk of medium-term complications.141 A follow-up study of people discharged from hospital following admission with COVID-19 showed that, at a mean follow-up of 140 days, nearly a third of patients were readmitted and 12% had died.142 Follow-up of patients with post-COVID-19 will include assessment and monitoring of cardiovascular and renal complications, and risk factor control. Patients with hyperglycaemia at admission will need follow-up to establish if these patients have new-onset diabetes.
The disproportionate excess risk of mortality from COVID-19 in people with both types of diabetes warrants vaccination prioritisation (panel), a guideline that is included in most national vaccination strategies.98, 99 After vaccination, disease management should follow evidence-based guidelines for patients with COVID-19 and type 2 diabetes.113 The rampant spread of COVID-19 in countries with a high prevalence of diabetes, such as India, Turkey and Brazil are undoubtedly of serious concern.143, 144, 145 The implications might be far reaching, particularly regarding the care of patients with diabetes or other metabolic diseases, and their outcomes (including mortality). In Africa, the situation is, at the time of writing, seemingly different, despite how the emergence of new SARS-CoV-2 variants is raising concern. Reasons for the lower severity of morbidity and mortality in Africa compared with other world regions might include the young age demographic, quick action, public support, favourable climate, and good community health systems.146 As a region with limited health-care resources, it will be important for Africa, particularly sub-Saharan Africa, to put emphasis on prevention strategies.
Smart disease management during and following the pandemic has been proposed. An integrated model of digital disease management might considerably relieve the burden to ambulatory health care, if it is implemented as an interoperable digital solution following evidence-based medical knowledge, operated by addressing the personal needs of patients, and hosted by an approved medical body.147, 148 This model requires the following considerations: the patient must have access to evidence-based health information in a language adjusted for health literacy, there must be medical indicators representing the therapeutic goal or corridor for patients, such an indicator must be technically measurable, and the patient must have a therapy that can be adjusted by patient self-management. Applying smart digital disease management might have the potential to substantially reduce the throughput in the ambulatory health-care system.149 This approach could be an option in regions with a fast growing prevalence of patients with chronic diseases or in regions with a reduced density of medical services. Ultimately, this approach to disease management might be the optional virtual solution for ambulatory care in patients with chronic and metabolic diseases during a pandemic.
Conclusions
The COVID-19 pandemic has presented unique challenges for people with metabolic diseases, a patient group with a high risk of severe SARS-CoV-2 infection. Pending definitive evidence regarding the long-term effects of COVID-19 on risk of incident diabetes, the susceptibility of β cells to inflammation and oxidative stress is well supported by clinical and experimental studies. This finding is especially relevant given that β cells are scarce in number yet make up one of the most metabolically active cell types in the human body.150
There has been increased emphasis on the importance of self-care activities for people with diabetes to optimise their diabetes management; however, this has proven difficult because of restrictions due to lockdown and reduced face-to-face education on diabetes.151 During the pandemic, we have learned how to optimise pharmacological management, including ICU treatment, for patients with diabetes with or without COVID-19.12, 113 The pandemic has also presented people with diabetes and their health-care teams with an opportunity to innovate and transition towards increasingly digitalised care, to continue supporting patients from their own homes.102 Preventative measures, including increased physical activity and enhanced health nutrition, are important in reversing insulin resistance and could be effective in reducing mortality related to COVID-19.
The COVID-19 pandemic has revealed the inherent inertia and limitations of our global health-care systems. It would be a progressive failure not to respond to this alarm signal and change our strategies to help to prevent diabetes and obesity with societal measures, diagnose metabolic syndromes as early as possible, focus on diabetes remission rather than progressive and expensive treatment, and individualise diabetes management to meet sustainable prevention of complications by use of all available evidence and technology. The vulnerability of resource-limited systems, notably in low-income countries and disadvantaged communities with knock-on effects on the global community, calls for urgent action to close these care gaps by reforming the health-care system, which was highlighted in the Lancet Commission on diabetes.152
The effects of COVID-19 and its follow-up diseases will probably be seen for many years to come. As such, we might have to learn to live with the virus and be aware of possible complications for people at higher risk of severe disease including people with diabetes and other metabolic diseases. The non-communicable pandemic of metabolic disease due to diabetes and obesity, affecting 0·5 billion people worldwide, could be considered as the foundation for the communicable COVID-19 pandemic, which has disproportionately affected this patient group (figure 3).
In high-income countries, there is a high prevalence of metabolic diseases and a high incidence of COVID-19. However, in low-income and middle-income countries, where the prevalence of metabolic diseases is lower, the incidence of COVID-19 is unclear due to underreporting and fewer testing services for SARS-CoV-2. Therefore, a question that still remains to be fully answered is whether the risk of SARS-CoV-2 infection is the same for everybody or whether, based on specific receptor pathways, there is an increased risk of infection for patients with metabolic disease.
Search strategy and selection criteria
We searched PubMed and Google Scholar, with no language restrictions, for articles published from date of inception to Sept 28, 2021. Search items included “COVID-19”, “post-COVID”, “long COVID”, “SARS-CoV-2”, “ACE2”, “DPP4”, diabetes”, “metabolic syndrome”, “obesity”, “hyperglycaemia”, “hyperglycemia”, “hypoglycaemia”, “hypoglycemia”, “insulin”, “steroids”, “glucocorticoid”, “dexamethasone”, “complications”, “risk”, “long-term consequences”, and “endocrine system”. The reference lists of original articles, narrative reviews, clinical guidelines, position statements, systematic reviews, and meta-analyses were screened for relevant publications. The final reference list was selected based on relevance to the topic of this Review, with preference given to the most recent relevant publications.
Declaration of interests
KK reports acting as a consultant or speaker, or receiving grants for investigator-initiated studies for AstraZeneca, Novartis, Novo Nordisk, Sanofi-Aventis, Lilly and Merck Sharp & Dohme, Boehringer Ingelheim, Bayer, Berlin-Chemie AG–Menarini Group, Janssen, and Napp. JSS reports personal fees as a consultant or advisor for Abvance, Adocia, Astra-Zeneca, Avotres, Bayer, Biozeus, Boehringer-Ingelheim, Dalcor, Dance Biopharm–Aerami Therapeutics, Diavacs, Duologics, Elcelyx, Eli Lilly, Enthera, Esperion, Geneuro, Ideal Life, Imcyse, Immunomolecular Therapeutics, Intarcia, Kamada, Kriya, Moerae Matrix, Novo-Nordisk, Oramed, Orgenesis, Pila Pharma, Precigen ActoBiotics, Preziba/Signos, Provention Bio, Sanofi, Tolerion, Valeritas, Viacyte, Viela Bio, vTv Therapeutics, and Zafgen. JHDV reports personal fees as consultant or advisor for Adocia, Novo Nordisk, and Zealand. ER reports personal fees as consultant or advisor for Abbott, Air Liquide, AstraZeneca, Boehringer-Ingelheim, Cellnovo, Dexcom, Eli Lilly, Insulet, Johnson & Johnson (Animas, LifeScan), Medirio, Medtronic, Novo Nordisk, Roche Diagnostics, Sanofi-Aventis, and Tandem; and research grant or material support from Abbott, Dexcom, Insulet, Roche Diagnostics, and Tandem. BG reports personal fees as consultant or advisor for Novo Nordisk, Pfizer, Merck Sharp & Dohme, Astra Zeneca, and Takeda. FR reports personal fees as a consultant or advisor for Ethicon, Medtronic, and Novo Nordisk. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
The work of CS, AL, BL, and SRB is partly supported by grants from the Deutsche Forschungsgemeinschaft, a German Research foundation (project number 314061271 and 288034826). AL is supported by an additional grant from DFG (project number 324141047).
Acknowledgments
Contributors
CS, PEHS, AL, RL, and SRB wrote several sections of the Review. Remaining authors wrote smaller sections of the review. CS and RL prepared the figures. CS, PEHS, and RL prepared the tables. All authors reviewed successive drafts of the Review. All authors approved the final submitted version and had final responsibility for the decision to submit for publication.
References
- 1.Clark A, Jit M, Warren-Gash C, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020;8:e1003–e1017. doi: 10.1016/S2214-109X(20)30264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thakur B, Dubey P, Benitez J, et al. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci Rep. 2021;11 doi: 10.1038/s41598-021-88130-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8:782–792. doi: 10.1016/S2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Batabyal R, Freishtat N, Hill E, Rehman M, Freishtat R, Koutroulis I. Metabolic dysfunction and immunometabolism in COVID-19 pathophysiology and therapeutics. Int J Obes. 2021;45:1163–1169. doi: 10.1038/s41366-021-00804-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costa FF, Rosário WR, Ribeiro Farias AC, de Souza RG, Duarte Gondim RS, Barroso WA. Metabolic syndrome and COVID-19: An update on the associated comorbidities and proposed therapies. Diabetes Metab Syndr. 2020;14:809–814. doi: 10.1016/j.dsx.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369 doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh A, Hussain S, Antony B. Non-alcoholic fatty liver disease and clinical outcomes in patients with COVID-19: a comprehensive systematic review and meta-analysis. Diabetes Metab Syndr. 2021;15:813–822. doi: 10.1016/j.dsx.2021.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh AK, Gillies CL, Singh R, et al. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes Metab. 2020;22:1915–1924. doi: 10.1111/dom.14124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stefan N, Birkenfeld AL, Schulze MB. Global pandemics interconnected – obesity, impaired metabolic health and COVID-19. Nat Rev Endocrinol. 2021;17:135–149. doi: 10.1038/s41574-020-00462-1. [DOI] [PubMed] [Google Scholar]
- 10.Kreutmair S, Unger S, Núñez NG, et al. Distinct immunological signatures discriminate severe COVID-19 from non-SARS-CoV-2-driven critical pneumonia. Immunity. 2021;54:1578–1593. doi: 10.1016/j.immuni.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kass DA, Duggal P, Cingolani O. Obesity could shift severe COVID-19 disease to younger ages. Lancet. 2020;395:1544–1545. doi: 10.1016/S0140-6736(20)31024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bornstein SR, Rubino F, Ludwig B, et al. Consequences of the COVID-19 pandemic for patients with metabolic diseases. Nat Metab. 2021;3:289–292. doi: 10.1038/s42255-021-00358-y. [DOI] [PubMed] [Google Scholar]
- 13.Gregory JM, Slaughter JC, Duffus SH, et al. COVID-19 severity is tripled in the diabetes community: a prospective analysis of the pandemic's impact in type 1 and type 2 diabetes. Diabetes Care. 2021;44:526–532. doi: 10.2337/dc20-2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5:e240. doi: 10.1016/S2468-2667(20)30085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simpson AHR, Simpson CJ, Frost H, Welburn SC. COVID-19: Obesity, deprivation and death. J Glob Health. 2020;10 doi: 10.7189/jogh.10.020389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brosh-Nissimov T, Orenbuch-Harroch E, Chowers M, et al. BNT162b2 vaccine breakthrough: clinical characteristics of 152 fully vaccinated hospitalized COVID-19 patients in Israel. Clin Microbiol Infect. 2021 doi: 10.1016/j.cmi.2021.06.036. published online July 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maestre-Muñiz MM, Arias Á, Mata-Vázquez E, et al. Long-term outcomes of patients with coronavirus disease 2019 at one year after hospital discharge. J Clin Med. 2021;10 doi: 10.3390/jcm10132945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramakrishnan RK, Kashour T, Hamid Q, Halwani R, Tleyjeh IM. Unraveling the mystery surrounding post-acute sequelae of COVID-19. Front Immunol. 2021;12 doi: 10.3389/fimmu.2021.686029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simões e Silva AC, Silveira KD, Ferreira AJ, Teixeira MM. ACE2, angiotensin-(1-7) and Mas receptor axis in inflammation and fibrosis. Br J Pharmacol. 2013;169:477–492. doi: 10.1111/bph.12159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li XC, Zhang J, Zhuo JL. The vasoprotective axes of the renin-angiotensin system: Physiological relevance and therapeutic implications in cardiovascular, hypertensive and kidney diseases. Pharmacol Res. 2017;125:21–38. doi: 10.1016/j.phrs.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coto E, Avanzas P, Gómez J. The renin-angiotensin-aldosterone system and coronavirus disease 2019. Eur Cardiol. 2021;16:e07. doi: 10.15420/ecr.2020.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bornstein SR, Rubino F, Khunti K, et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8:546–550. doi: 10.1016/S2213-8587(20)30152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lv Q, Yang Q, Cui Y, et al. Effects of taurine on ACE, ACE2 and HSP70 expression of hypothalamic-pituitary-adrenal axis in stress-induced hypertensive rats. Adv Exp Med Biol. 2017;975:871–886. doi: 10.1007/978-94-024-1079-2_69. [DOI] [PubMed] [Google Scholar]
- 24.Coate KC, Cha J, Shrestha S, et al. SARS-CoV-2 cell entry factors ACE2 and TMPRSS2 are expressed in the microvasculature and ducts of human pancreas but are not enriched in β cells. Cell Metab. 2020;32:1028–1040.e4. doi: 10.1016/j.cmet.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kusmartseva I, Wu W, Syed F, et al. Expression of SARS-CoV-2 entry factors in the pancreas of normal organ donors and individuals with COVID-19. Cell Metab. 2020;32:1041–1051.e6. doi: 10.1016/j.cmet.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu F, Long X, Zhang B, Zhang W, Chen X, Zhang Z. ACE2 expression in pancreas may cause pancreatic damage after SARS-CoV-2 infection. Clin Gastroenterol Hepatol. 2020;18:2128–2130.e2. doi: 10.1016/j.cgh.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fignani D, Licata G, Brusco N, et al. SARS-CoV-2 receptor angiotensin I-converting enzyme type 2 (ACE2) is expressed in human pancreatic β-cells and in the human pancreas microvasculature. Front Endocrinol (Lausanne) 2020;11 doi: 10.3389/fendo.2020.596898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Müller JA, Groß R, Conzelmann C, et al. SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas. Nat Metab. 2021;3:149–165. doi: 10.1038/s42255-021-00347-1. [DOI] [PubMed] [Google Scholar]
- 29.Wu CT, Lidsky PV, Xiao Y, et al. SARS-CoV-2 infects human pancreatic β cells and elicits β cell impairment. Cell Metab. 2021;33:1565–1576.e5. doi: 10.1016/j.cmet.2021.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steenblock C, Richter S, Berger I, et al. Viral infiltration of pancreatic islets in patients with COVID-19. Nat Commun. 2021;12 doi: 10.1038/s41467-021-23886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumar A, Faiq MA, Pareek V, et al. Relevance of SARS-CoV-2 related factors ACE2 and TMPRSS2 expressions in gastrointestinal tissue with pathogenesis of digestive symptoms, diabetes-associated mortality, and disease recurrence in COVID-19 patients. Med Hypotheses. 2020;144 doi: 10.1016/j.mehy.2020.110271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young MJ, Clyne CD, Chapman KE. Endocrine aspects of ACE2 regulation: RAAS, steroid hormones and SARS-CoV-2. J Endocrinol. 2020;247:R45–R62. doi: 10.1530/JOE-20-0260. [DOI] [PubMed] [Google Scholar]
- 33.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8:e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Esguerra JLS, Ofori JK, Nagao M, et al. Glucocorticoid induces human beta cell dysfunction by involving riborepressor GAS5 LincRNA. Mol Metab. 2020;32:160–167. doi: 10.1016/j.molmet.2019.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grover A, Oberoi M. A systematic review and meta-analysis to evaluate the clinical outcomes in COVID-19 patients on angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Eur Heart J Cardiovasc Pharmacother. 2021;7:148–157. doi: 10.1093/ehjcvp/pvaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lei C, Qian K, Li T, et al. Neutralization of SARS-CoV-2 spike pseudotyped virus by recombinant ACE2-Ig. Nat Commun. 2020;11 doi: 10.1038/s41467-020-16048-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bouhanick B, Cracowski JL, Faillie JL. DPP-4 inhibitors and severe course of illness in patients with COVID-19. Therapie. 2021;76:359–360. doi: 10.1016/j.therap.2021.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Samuel SM, Varghese E, Büsselberg D. Therapeutic potential of metformin in COVID-19: reasoning for its protective role. Trends Microbiol. 2021 doi: 10.1016/S0966-842X(21)00063-9. published online March 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khunti K, Knighton P, Zaccardi F, et al. Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England. Lancet Diabetes Endocrinol. 2021;9:293–303. doi: 10.1016/S2213-8587(21)00050-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Katsiki N, Ferrannini E. Anti-inflammatory properties of antidiabetic drugs: a “promised land” in the COVID-19 era? J Diabetes Complications. 2020;34 doi: 10.1016/j.jdiacomp.2020.107723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nohara H, Nakashima R, Kamei S, et al. Intratracheal GLP-1 receptor agonist treatment up-regulates mucin via p38 and exacerbates emphysematous phenotype in mucus hypersecretory obstructive lung diseases. Biochem Biophys Res Commun. 2020;524:332–339. doi: 10.1016/j.bbrc.2020.01.081. [DOI] [PubMed] [Google Scholar]
- 43.Pal R, Banerjee M, Mukherjee S, Bhogal RS, Kaur A, Bhadada SK. Dipeptidyl peptidase-4 inhibitor use and mortality in COVID-19 patients with diabetes mellitus: an updated systematic review and meta-analysis. Ther Adv Endocrinol Metab. 2021;12 doi: 10.1177/2042018821996482. 2042018821996482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rhee SY, Lee J, Nam H, Kyoung DS, Shin DW, Kim DJ. Effects of a DPP-4 inhibitor and RAS blockade on clinical outcomes of patients with diabetes and COVID-19. Diabetes Metab J. 2021;45:251–259. doi: 10.4093/dmj.2020.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stumpf J, Siepmann T, Lindner T, et al. Humoral and cellular immunity to SARS-CoV-2 vaccination in renal transplant versus dialysis patients: a prospective, multicenter observational study using mRNA-1273 or BNT162b2 mRNA vaccine. Lancet Reg Health Eur. 2021 doi: 10.1016/j.lanepe.2021.100178. published online July 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dandona P, Ghanim H. Diabetes, obesity, COVID-19, Insulin, and other antidiabetes drugs. Diabetes Care. 2021;44:1929–1933. doi: 10.2337/dci21-0003. [DOI] [PubMed] [Google Scholar]
- 47.Yu B, Li C, Sun Y, Wang DW. Insulin treatment is associated with increased mortality in patients with COVID-19 and type 2 diabetes. Cell Metab. 2021;33:65–77. doi: 10.1016/j.cmet.2020.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin-angiotensin-aldosterone system blockers and the risk of COVID-19. N Engl J Med. 2020;382:2431–2440. doi: 10.1056/NEJMoa2006923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mehta N, Kalra A, Nowacki AS, et al. Association of use of angiotensin-converting enzyme inhibitors and angiotensin ii receptor blockers with testing positive for coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1020–1026. doi: 10.1001/jamacardio.2020.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang P, Zhu L, Cai J, et al. Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020;126:1671–1681. doi: 10.1161/CIRCRESAHA.120.317134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Villard O, Morquin D, Molinari N, et al. The plasmatic aldosterone and c-reactive protein levels, and the severity of COVID-19: the Dyhor-19 study. J Clin Med. 2020;9 doi: 10.3390/jcm9072315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science. 2021;372 doi: 10.1126/science.abg3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Faria NR, Mellan TA, Whittaker C, et al. Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil. Science. 2021;372:815–821. doi: 10.1126/science.abh2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leung K, Shum MH, Leung GM, Lam TT, Wu JT. Early transmissibility assessment of the N501Y mutant strains of SARS-CoV-2 in the United Kingdom, October to November 2020. Euro Surveill. 2021;26 doi: 10.2807/1560-7917.ES.2020.26.1.2002106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khan A, Zia T, Suleman M, et al. Higher infectivity of the SARS-CoV-2 new variants is associated with K417N/T, E484K, and N501Y mutants: an insight from structural data. J Cell Physiol. 2021;236:7045–7057. doi: 10.1002/jcp.30367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alai S, Gujar N, Joshi M, Gautam M, Gairola S. Pan-India novel coronavirus SARS-CoV-2 genomics and global diversity analysis in spike protein. Heliyon. 2021;7 doi: 10.1016/j.heliyon.2021.e06564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lan J, Ge J, Yu J, et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 60.Cantuti-Castelvetri L, Ojha R, Pedro LD, et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020;370:856–860. doi: 10.1126/science.abd2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wei J, Alfajaro MM, DeWeirdt PC, et al. Genome-wide CRISPR screens reveal host factors critical for SARS-CoV-2 infection. Cell. 2021;184:76–91. doi: 10.1016/j.cell.2020.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Karki R, Sharma BR, Tuladhar S, et al. Synergism of TNF-α and IFN-γ triggers inflammatory cell death, tissue damage, and mortality in SARS-CoV-2 infection and cytokine shock syndromes. Cell. 2021;184:149–168. doi: 10.1016/j.cell.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nakamura H, Kinjo T, Arakaki W, Miyagi K, Tateyama M, Fujita J. Serum levels of receptor-interacting protein kinase-3 in patients with COVID-19. Crit Care. 2020;24:484. doi: 10.1186/s13054-020-03209-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Linkermann A, Stockwell BR, Krautwald S, Anders HJ. Regulated cell death and inflammation: an auto-amplification loop causes organ failure. Nat Rev Immunol. 2014;14:759–767. doi: 10.1038/nri3743. [DOI] [PubMed] [Google Scholar]
- 65.Li Y, Zhang Z, Yang L, et al. The MERS-CoV Receptor DPP4 as a candidate binding target of the SARS-CoV-2 spike. iScience. 2020;23 doi: 10.1016/j.isci.2020.101400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lambeir AM, Durinx C, Scharpé S, De Meester I. Dipeptidyl-peptidase IV from bench to bedside: an update on structural properties, functions, and clinical aspects of the enzyme DPP IV. Crit Rev Clin Lab Sci. 2003;40:209–294. doi: 10.1080/713609354. [DOI] [PubMed] [Google Scholar]
- 67.Mulvihill EE, Drucker DJ. Pharmacology, physiology, and mechanisms of action of dipeptidyl peptidase-4 inhibitors. Endocr Rev. 2014;35:992–1019. doi: 10.1210/er.2014-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Drucker DJ. Coronavirus Infections and type 2 diabetes-shared pathways with therapeutic implications. Endocr Rev. 2020;41 doi: 10.1210/endrev/bnaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Seidu S, Gillies C, Zaccardi F, et al. The impact of obesity on severe disease and mortality in people with SARS-CoV-2: a systematic review and meta-analysis. Endocrinol Diabetes Metab. 2020;4 doi: 10.1002/edm2.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ayres JS. A metabolic handbook for the COVID-19 pandemic. Nat Metab. 2020;2:572–585. doi: 10.1038/s42255-020-0237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 2020;8:616–627. doi: 10.1016/S2213-8587(20)30110-8. [DOI] [PubMed] [Google Scholar]
- 72.Akhmerov A, Marbán E. COVID-19 and the heart. Circ Res. 2020;126:1443–1455. doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Avula A, Nalleballe K, Narula N, et al. COVID-19 presenting as stroke. Brain Behav Immun. 2020;87:115–119. doi: 10.1016/j.bbi.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Boucher J, Kleinridders A, Kahn CR. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb Perspect Biol. 2014;6 doi: 10.1101/cshperspect.a009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Amin MN, Hussain MS, Sarwar MS, et al. How the association between obesity and inflammation may lead to insulin resistance and cancer. Diabetes Metab Syndr. 2019;13:1213–1224. doi: 10.1016/j.dsx.2019.01.041. [DOI] [PubMed] [Google Scholar]
- 76.Lauterbach MA, Wunderlich FT. Macrophage function in obesity-induced inflammation and insulin resistance. Pflugers Arch. 2017;469:385–396. doi: 10.1007/s00424-017-1955-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Santos A, Magro DO, Evangelista-Poderoso R, Saad MJA. Diabetes, obesity, and insulin resistance in COVID-19: molecular interrelationship and therapeutic implications. Diabetol Metab Syndr. 2021;13:23. doi: 10.1186/s13098-021-00639-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sindhu S, Thomas R, Shihab P, Sriraman D, Behbehani K, Ahmad R. Obesity is a positive modulator of IL-6R and IL-6 expression in the subcutaneous adipose tissue: significance for metabolic inflammation. PLoS One. 2015;10 doi: 10.1371/journal.pone.0133494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract. 2014;105:141–150. doi: 10.1016/j.diabres.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 80.Schwarz PEH, Timpel P, Harst L, et al. Blood sugar regulation for cardiovascular health promotion and disease prevention: JACC health promotion series. J Am Coll Cardiol. 2018;72:1829–1844. doi: 10.1016/j.jacc.2018.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marx C, Ehrhart-Bornstein M, Scherbaum WA, Bornstein SR. Regulation of adrenocortical function by cytokines–relevance for immune-endocrine interaction. Horm Metab Res. 1998;30:416–420. doi: 10.1055/s-2007-978907. [DOI] [PubMed] [Google Scholar]
- 82.Steenblock C, Todorov V, Kanczkowski W, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the neuroendocrine stress axis. Mol Psychiatry. 2020;25:1611–1617. doi: 10.1038/s41380-020-0758-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ramakrishnan S, Nicolau DV, Jr, Langford B, et al. Inhaled budesonide in the treatment of early COVID-19 (STOIC): a phase 2, open-label, randomised controlled trial. Lancet Respir Med. 2021;9:763–772. doi: 10.1016/S2213-2600(21)00160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Isidori AM, Pofi R, Hasenmajer V, Lenzi A, Pivonello R. Use of glucocorticoids in patients with adrenal insufficiency and COVID-19 infection. Lancet Diabetes Endocrinol. 2020;8:472–473. doi: 10.1016/S2213-8587(20)30149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Conti P, Ronconi G, Caraffa A, et al. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents. 2020;34:327–331. doi: 10.23812/CONTI-E. [DOI] [PubMed] [Google Scholar]
- 86.Alsadhan I, Alruwashid S, Alhamad M, et al. Diabetic ketoacidosis precipitated by Coronavirus disease 2019 infection: case series. Curr Ther Res Clin Exp. 2020;93 doi: 10.1016/j.curtheres.2020.100609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Heaney AI, Griffin GD, Simon EL. Newly diagnosed diabetes and diabetic ketoacidosis precipitated by COVID-19 infection. Am J Emerg Med. 2020;38:2491e3–2491e4. doi: 10.1016/j.ajem.2020.05.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hollstein T, Schulte DM, Schulz J, et al. Autoantibody-negative insulin-dependent diabetes mellitus after SARS-CoV-2 infection: a case report. Nat Metab. 2020;2:1021–1024. doi: 10.1038/s42255-020-00281-8. [DOI] [PubMed] [Google Scholar]
- 89.Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab. 2020;22:1935–1941. doi: 10.1111/dom.14057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Montefusco L, Ben Nasr M, D'Addio F, et al. Acute and long-term disruption of glycometabolic control after SARS-CoV-2 infection. Nat Metab. 2021;3:774–785. doi: 10.1038/s42255-021-00407-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Naguib MN, Raymond JK, Vidmar AP. New onset diabetes with diabetic ketoacidosis in a child with multisystem inflammatory syndrome due to COVID-19. J Pediatr Endocrinol Metab. 2020;34:147–150. doi: 10.1515/jpem-2020-0426. [DOI] [PubMed] [Google Scholar]
- 92.Rubino F, Amiel SA, Zimmet P, et al. New-onset diabetes in COVID-19. N Engl J Med. 2020;383:789–790. doi: 10.1056/NEJMc2018688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kamrath C, Mönkemöller K, Biester T, et al. Ketoacidosis in children and adolescents with newly diagnosed type 1 diabetes during the COVID-19 pandemic in Germany. JAMA. 2020;324:801–804. doi: 10.1001/jama.2020.13445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Salmi H, Heinonen S, Hästbacka J, et al. New-onset type 1 diabetes in Finnish children during the COVID-19 pandemic. Arch Dis Child. 2021 doi: 10.1136/archdischild-2020-321220. published online May 27. [DOI] [PubMed] [Google Scholar]
- 95.Kumaran NK, Karmakar BK, Taylor OM. Coronavirus disease-19 (COVID-19) associated with acute necrotising pancreatitis (ANP) BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2020-237903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Accili D. Can COVID-19 cause diabetes? Nat Metab. 2021;3:123–125. doi: 10.1038/s42255-020-00339-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bailey B, Whelen ML, Strunk DR. Adhering to COVID-19 health guidelines: examining demographic and psychological predictors of adherence. Appl Psychol Health Well-Being. 2021 doi: 10.1111/aphw.12284. published online May 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pal R, Bhadada SK, Misra A. COVID-19 vaccination in patients with diabetes mellitus: current concepts, uncertainties and challenges. Diabetes Metab Syndr. 2021;15:505–508. doi: 10.1016/j.dsx.2021.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.McGovern AP, Thomas NJ, Vollmer SJ, Hattersley AT, Mateen BA, Dennis JM. The disproportionate excess mortality risk of COVID-19 in younger people with diabetes warrants vaccination prioritisation. Diabetologia. 2021;64:1184–1186. doi: 10.1007/s00125-021-05404-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Müller G, Weser G, Schwarz PE. The European perspective of diabetes prevention: the need for individualization of diabetes prevention. J Endocrinol Invest. 2013;36:352–357. doi: 10.1007/BF03347104. [DOI] [PubMed] [Google Scholar]
- 101.Royal Australian College of General Practitioners Diabetes management during coronavirus. https://www.racgp.org.au/clinical-resources/covid-19-resources/other-health-issues/diabetes-management-during-coronavirus
- 102.Quinn LM, Davies MJ, Northern A, et al. Use of MyDesmond digital education programme to support self-management in people with type 2 diabetes during the COVID-19 pandemic. Diabet Med. 2021;38 doi: 10.1111/dme.14469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rogers LC, Snyder RJ, Joseph WS. Diabetes-related amputations: a pandemic within a pandemic. J Am Podiatr Med Assoc. 2020 doi: 10.7547/20-248. published online Nov 3. [DOI] [PubMed] [Google Scholar]
- 104.MedGen Serum hypoglycemia. https://www.ncbi.nlm.nih.gov/medgen/?term=282198&report=FullReport
- 105.Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14:965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rowlands AV, Henson JJ, Coull NA, et al. The impact of COVID-19 restrictions on accelerometer-assessed physical activity and sleep in individuals with type 2 diabetes. Diabet Med. 2021 doi: 10.1111/dme.14549. published online March 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gregg EW, Sophiea MK, Weldegiorgis M. Diabetes and COVID-19: population impact 18 months into the pandemic. Diabetes Care. 2021;44:1916–1923. doi: 10.2337/dci21-0001. [DOI] [PubMed] [Google Scholar]
- 108.McGurnaghan SJ, Weir A, Bishop J, et al. Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland. Lancet Diabetes Endocrinol. 2021;9:82–93. doi: 10.1016/S2213-8587(20)30405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Petrie JR, Boyle JG, Ali K, Smith C, Morrison D, Kar P. A post COVID-19 ‘Marshall Plan’ for type 2 diabetes. Diabet Med. 2021;38 doi: 10.1111/dme.14439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cyranka K, Dudek D, Małecki MT, Matejko B, Klupa T. Psychological crisis intervention for COVID-19 lockdown stress in patients with type 1 diabetes mellitus: survey study and qualitative analysis. JMIR Ment Health. 2021;8 doi: 10.2196/28097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ruissen MM, Regeer H, Landstra CP, et al. Increased stress, weight gain and less exercise in relation to glycemic control in people with type 1 and type 2 diabetes during the COVID-19 pandemic. BMJ Open Diabetes Res Care. 2021;9 doi: 10.1136/bmjdrc-2020-002035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ruberti OM, Telles GD, Rodrigues B. Stress and physical inactivity: two explosive ingredients for the heart in COVID-19 pandemic times. Curr Cardiol Rev. 2021 doi: 10.2174/1573403X17666210126103204. published online Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ceriello A, Prattichizzo F. Pharmacological management of COVID-19 in type 2 diabetes. J Diabetes Complications. 2021;35 doi: 10.1016/j.jdiacomp.2021.107927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kosiborod MN, Esterline R, Furtado RHM, et al. Dapagliflozin in patients with cardiometabolic risk factors hospitalised with COVID-19 (DARE-19): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol. 2021;9:586–594. doi: 10.1016/S2213-8587(21)00180-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Cariou B, Pichelin M, Goronflot T, et al. Phenotypic characteristics and prognosis of newly diagnosed diabetes in hospitalized patients with COVID-19: results from the CORONADO study. Diabetes Res Clin Pract. 2021;175 doi: 10.1016/j.diabres.2021.108695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Noh Y, Oh IS, Jeong HE, Filion KB, Yu OHY, Shin JY. Association between DPP-4 inhibitors and COVID-19-related outcomes among patients with type 2 diabetes. Diabetes Care. 2021;44:e64–e66. doi: 10.2337/dc20-1824. [DOI] [PubMed] [Google Scholar]
- 117.Solerte SB, D'Addio F, Trevisan R, et al. Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and covid-19: a multicenter, case-control, retrospective, observational study. Diabetes Care. 2020;43:2999–3006. doi: 10.2337/dc20-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kow CS, Hasan SS. Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: a meta-analysis. J Med Virol. 2021;93:695–697. doi: 10.1002/jmv.26498. [DOI] [PubMed] [Google Scholar]
- 119.Scheen AJ. Metformin and COVID-19: from cellular mechanisms to reduced mortality. Diabetes Metab. 2020;46:423–426. doi: 10.1016/j.diabet.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cheng X, Liu YM, Li H, et al. Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;32:537–547. doi: 10.1016/j.cmet.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Group RC. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397:1637–1645. doi: 10.1016/S0140-6736(21)00676-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Castañeda S, Remuzgo-Martínez S, López-Mejías R, et al. Rapid beneficial effect of the IL-6 receptor blockade on insulin resistance and insulin sensitivity in non-diabetic patients with rheumatoid arthritis. Clin Exp Rheumatol. 2019;37:465–473. [PubMed] [Google Scholar]
- 123.Marfella R, Paolisso P, Sardu C, et al. Negative impact of hyperglycaemia on tocilizumab therapy in COVID-19 patients. Diabetes Metab. 2020;46:403–405. doi: 10.1016/j.diabet.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Katulanda P, Dissanayake HA, Ranathunga I, et al. Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature. Diabetologia. 2020;63:1440–1452. doi: 10.1007/s00125-020-05164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Group WHOREAfC-TW. Sterne JAC, Murthy S, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: meta-analysis A. JAMA. 2020;324:1330–1341. doi: 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Perez A, Jansen-Chaparro S, Saigi I, Bernal-Lopez MR, Miñambres I, Gomez-Huelgas R. Glucocorticoid-induced hyperglycemia. J Diabetes. 2014;6:9–20. doi: 10.1111/1753-0407.12090. [DOI] [PubMed] [Google Scholar]
- 127.American Diabetes Association FDA expands remote patient monitoring in hospitals for people with diabetes during COVID-19; manufacturers donate CGM supplies. April 21, 2020. https://www.diabetes.org/newsroom/press-releases/2020/fda-remote-patient-monitoring-cgm
- 128.Zhu L, She ZG, Cheng X, et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31:1068–1077. doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Klonoff DC, Messler JC, Umpierrez GE, et al. Association between achieving inpatient glycemic control and clinical outcomes in hospitalized patients with COVID-19: a multicenter, retrospective hospital-based analysis. Diabetes Care. 2021;44:578–585. doi: 10.2337/dc20-1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lu J, Wang C, Shen Y, et al. Time in range in relation to all-cause and cardiovascular mortality in patients with type 2 diabetes: a prospective cohort study. Diabetes Care. 2021;44:549–555. doi: 10.2337/dc20-1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wu Q, Zhou L, Sun X, et al. Altered lipid metabolism in recovered SARS patients twelve years after infection. Sci Rep. 2017;7 doi: 10.1038/s41598-017-09536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010;47:193–199. doi: 10.1007/s00592-009-0109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wostyn P. COVID-19 and chronic fatigue syndrome: is the worst yet to come? Med Hypotheses. 2021;146 doi: 10.1016/j.mehy.2020.110469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594:259–264. doi: 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]
- 136.Barker-Davies RM, O'Sullivan O, Senaratne KPP, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54:949–959. doi: 10.1136/bjsports-2020-102596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Berger I, Werdermann M, Bornstein SR, Steenblock C. The adrenal gland in stress – adaptation on a cellular level. J Steroid Biochem Mol Biol. 2019;190:198–206. doi: 10.1016/j.jsbmb.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 138.Rohr M, Weiß A, Bein T, et al. Experiences, opinions and expectations of health care providers towards an intensive care unit follow-up clinic: Qualitative study and online survey. Intensive Crit Care Nurs. 2021 doi: 10.1016/j.iccn.2021.103084. published online July 23. [DOI] [PubMed] [Google Scholar]
- 139.Steinbrink JM, Miceli MH. Mucormycosis. Infect Dis Clin North Am. 2021;35:435–452. doi: 10.1016/j.idc.2021.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol. 2021;135:442–447. doi: 10.1017/S0022215121000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Khunti K, Davies MJ, Kosiborod MN, Nauck MA. Long COVID – metabolic risk factors and novel therapeutic management. Nat Rev Endocrinol. 2021;17:379–380. doi: 10.1038/s41574-021-00495-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ayoubkhani D, Khunti K, Nafilyan V, et al. Post-COVID syndrome in individuals admitted to hospital with COVID-19: retrospective cohort study. BMJ. 2021;372:n693. doi: 10.1136/bmj.n693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Correr CJ, Coura-Vital W, Frade JCQP, et al. Prevalence of people at risk of developing type 2 diabetes mellitus and the involvement of community pharmacies in a national screening campaign: a pioneer action in Brazil. Diabetol Metab Syndr. 2020;12:89. doi: 10.1186/s13098-020-00593-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mehta SR, Kashyap AS, Das S. Diabetes mellitus in India: the modern scourge. Med J Armed Forces India. 2009;65:50–54. doi: 10.1016/S0377-1237(09)80056-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Satman I, Omer B, Tutuncu Y, et al. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28:169–180. doi: 10.1007/s10654-013-9771-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Soy A. Coronavirus in Africa: five reasons why COVID-19 has been less deadly than elsewhere. Oct 20, 2020. https://www.bbc.com/news/world-africa-54418613
- 147.Timpel P, Harst L, Reifegerste D, Weihrauch-Blüher S, Schwarz PEH. What should governments be doing to prevent diabetes throughout the life course? Diabetologia. 2019;62:1842–1853. doi: 10.1007/s00125-019-4941-y. [DOI] [PubMed] [Google Scholar]
- 148.Jose T, Warner DO, O'Horo JC, et al. Digital health surveillance strategies for management of coronavirus disease 2019. Mayo Clin Proc Innov Qual Outcomes. 2021;5:109–117. doi: 10.1016/j.mayocpiqo.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Deckert A, Anders S, de Allegri M, et al. Effectiveness and cost-effectiveness of four different strategies for SARS-CoV-2 surveillance in the general population (CoV-Surv Study): a structured summary of a study protocol for a cluster-randomised, two-factorial controlled trial. Trials. 2021;22:39. doi: 10.1186/s13063-020-04982-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ogilvie RF. A quantitative estimation of the pancreatic islet tissue1. QJM. 1937;6:287–300. doi: 10.2337/diab.4.5.367. [DOI] [PubMed] [Google Scholar]
- 151.Jacob L, Rickwood S, Rathmann W, Kostev K. Change in glucose-lowering medication regimens in individuals with type 2 diabetes mellitus during the COVID-19 pandemic in Germany. Diabetes Obes Metab. 2021;23:910–915. doi: 10.1111/dom.14293. [DOI] [PubMed] [Google Scholar]
- 152.Chan JCN, Lim LL, Wareham NJ, et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2021;396:2019–2082. doi: 10.1016/S0140-6736(20)32374-6. [DOI] [PubMed] [Google Scholar]