Abstract
Purpose:
Pediatric readiness scores may be a useful measure of a hospital’s preparedness to care for children. However, there is limited evidence linking these scores with patient outcomes or other metrics, including the need for interfacility transfer. This study aims to determine the association of pediatric readiness scores with the odds of interfacility transfer among a cohort of non-injured children (< 18 years old) presenting to emergency departments (ED) in small rural hospitals in the state of California.
Methods:
Data from the National Pediatric Readiness Project assessment were linked with the California Office of Statewide Health Planning and Development’s ED and inpatient databases to conduct a cross-sectional study of pediatric interfacility transfers. Hospitals were manually matched between these data sets. Logistic regression was performed with random intercepts for hospital and adjustment for patient-level confounders.
Findings:
A total of 54 hospitals and 135,388 encounters met the inclusion criteria. EDs with a high pediatric readiness score (>70) had lower adjusted odds of transfer (aOR: 0.55, 95% CI: 0.33-0.93) than EDs with a low pediatric readiness score (≤ 70). The pediatric readiness section with strongest association with transfer was the “Policies, Procedures, and Protocols” section; EDs in the highest quartile had lower odds of transfer than EDs in the lowest quartile (aOR: 0.54, 95% CI: 0.31-0.91).
Conclusions:
Pediatric patients presenting to EDs at small rural hospitals with high pediatric readiness scores may be less likely to be transferred. Additional studies are recommended to investigate other pediatric outcomes in relation to hospital ED pediatric readiness.
Keywords: access to care, emergency medical care, pediatric readiness, quality, utilization of health services
While children represent more than 20% of overall emergency department (ED) visits, many EDs are not fully prepared to provide comprehensive pediatric services.1 In fact, 75% of pediatric ED encounters occur in EDs that see fewer than 20 pediatric patients per day, and many of these EDs are critical in serving their rural communities.1,2 Small EDs with low pediatric volume may be less likely to provide definitive care for children due to insufficient equipment, lack of pediatric staffing, and limited expertise in sub-specialty care.3 Pediatric patients cared for in rural EDs are up to 3 times more likely than urban counterparts to be transferred.3,4 In addition, pediatric transfer rates for common conditions have increased over time, placing a strain on pediatric hospital care at large referral centers.5 While necessary in some cases for optimal patient health, the transfer process may put the patient at risk for adverse events. Patients often undergo repeated, unnecessary laboratory and radiologic tests at the destination hospital,6–9 which sometimes place significant emotional and financial burdens on the patient’s family. These considerations are particularly relevant for rural families given the additional travel and lodging needs.4
Several professional organizations recognized the pediatric-specific challenges of emergency care and formed the National Pediatric Readiness Project (NPRP), a multi-phase quality improvement collaborative aimed at improving pediatric emergency care. The NPRP established a survey-based quantitative measure of pediatric readiness that evaluates ED compliance with the 2009 “Guidelines of Care of Children in the Emergency Department.”10 Recent studies have found that EDs with increased pediatric readiness were associated with decreased hospital length of stay and decreased mortality.7,11
In light of the risks of transfer and the policy-driven efforts to improve pediatric readiness,12 this study aims to determine the association between pediatric readiness and the odds of interfacility transfer among EDs in small rural hospitals. We hypothesized that among these EDs, non-injured patients that presented to an ED with a higher pediatric readiness score would have lower odds of transfer. The secondary aim of this study was to identify which components of pediatric readiness were most strongly associated with transfer.
Methods
Data Sources
This is a statewide cross-sectional study of children treated in non-military California hospitals in 2012. Hospital-level pediatric readiness data were obtained from the NPRP pediatric readiness assessment.10 This assessment was piloted in California in 2011-2012 and had a 90% response rate.13 Individual encounter data were obtained from 2 administrative data sets from the California Office of Statewide Health Planning and Development (OSHPD): Emergency Department Data and Patient Discharge Data. Patient Discharge Data consists of encounters that resulted in an inpatient encounter, including admissions that began as emergency department encounters.14
Study Population
As shown in Figure 1, this study used the most recent overlapping data between the NPRP pediatric readiness assessment results and OSHPD databases. We included ED encounters in 2012 for pediatric patients ages 0 to 17 years that resulted in a discharge home, admission to the index hospital, or transfer to another non-psychiatric, acute care hospital. This was obtained from the discharge location directly from the database rather than from inference of same-day visits to 2 emergency departments. Outcomes at a post-transfer hospital were not studied. Encounters with any diagnosis classified as an “injury and poisoning”15 were excluded given their unique transfer patterns.16,17 Encounters that resulted in death were also excluded. Consistent with prior pediatric transfer research, encounters with Medicare as a primary payer were excluded since Medicare primarily insures adult populations and children that need sub-specialized care.17
Figure 1.
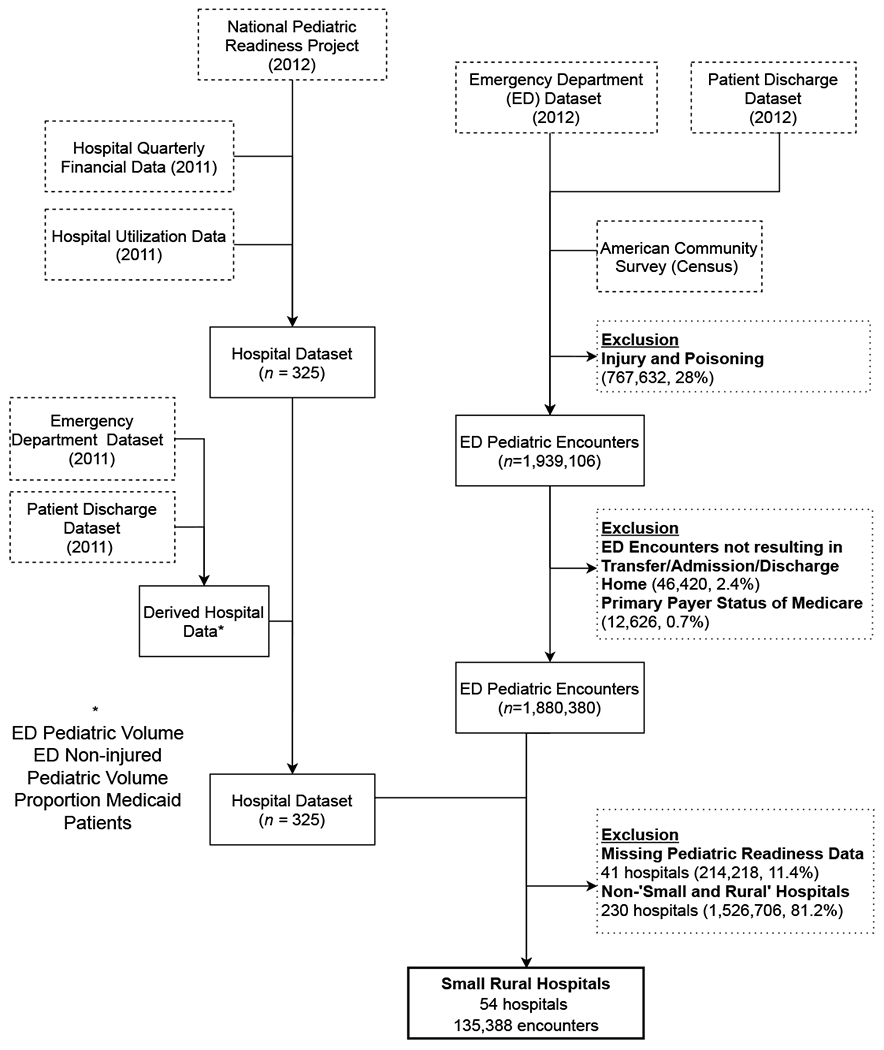
Study Population and Data Flow Diagram
We were interested in studying the pediatric readiness at EDs in small rural hospitals. Therefore, we included Critical Access Hospitals (CAH), designated by the Centers for Medicare and Medicaid Services, and “small and rural” hospitals, as designated by OSHPD. To be designated a CAH, the hospital must maintain 25 or fewer beds, have an average length of stay less than 96 hours, and be at least 35 miles from another hospital.2 The “small and rural” designation was defined in law as an acute care hospital with “no more than 76 acute care beds and is located in an incorporated place or census designated place of 15,000 or less according to the 1980 Federal Census.”18,19 There were 25 hospitals that were both designated CAH and “small and rural,” and there were 29 hospitals that were only “small and rural”.
Primary Outcome Measure
The primary outcome measure was whether a patient encounter resulted in an interfacility transfer. A transfer was defined as an ED encounter with a discharge to an acute care hospital. Non-transfers were patient encounters at the index hospital that resulted in a discharge home or admission to the same hospital.
Exposure Measures
The main exposure of interest was the weighted pediatric readiness score (0-100) from the NPRP assessment. A score of 100 indicated that the ED had all of the 2009 “Guidelines of Care of Children in the Emergency Department,” excluding the guidelines for ED support services which were not measured. The assessment contained 6 sections: Administration/Coordination; Personnel; Quality Improvement; Pediatric Patient Safety; Policies, Procedures, and Protocols; and Equipment and Supplies.10,13 During the evaluation of independent variables for the multivariable analysis, it was noted that the distribution of pediatric readiness scores supported the transformation from a continuous to a dichotomous variable. Specifically, EDs with scores below 70 were noted to have similarly high transfer rates and EDs with scores greater than or equal to 70 have similarly lower transfer rates; therefore we dichotomized pediatric readiness scores at 70.20 (Appendix 1).
Patient Characteristics
Demographic variables included patient age, gender, race/ethnicity, insurance, and primary spoken language. Median household income level and attainment of a bachelor’s degree were obtained from the American Community Survey 2012 5-year estimates and matched by ZIP Code tabulation area.21 Previous studies have shown these to be associated with decreased transfer.3,17 A patient was considered to have a complex chronic condition if they had one or more ICD-9 diagnoses that met one of the definitions in the pediatric complex chronic conditions classification system.22 Severity of illness was determined by applying an ICD-9 code classification system that determines the amount of resources needed to diagnose and treat a child at an ED with a specific diagnosis. This is an ordinal scale from 1 to 5, with 1 representing the lowest severity of illness and 5 being the greatest severity of illness.23
Hospital Characteristics
Hospital characteristics included teaching hospital status, emergency department level, trauma center designation, pediatric trauma designation, and financial control (“Investor/For-Profit,” “Non-Profit,” or “Unknown”).19,24 Additional characteristics were derived from OSHPD encounter-level data, including ED pediatric volume, ED non-injured pediatric volume, and proportion Medicaid-insured encounters.14 For these characteristics, we utilized 2011, rather than 2012, encounter data in case the act of completing the pediatric readiness assessment changed practices at that institution. The dichotomous variable pediatric inpatient capabilities was obtained from the NPRP assessment.10 Driving distance was calculated to the closest “highly pediatric resourced” hospital—a hospital with a pediatric emergency department, pediatric inpatient capabilities and pediatric intensive care unit.25 Distance is an important factor in transfer decisions and initial triage by emergency medical services.26,27 Distances were calculated using the R package (R Foundation, Vienna, Austria) “gmapsdistance,” which relies on Geographic Information Systems and Google Maps Distance Matrix Applications Programming Interface.28,29
Data and Statistical Analyses
NPRP hospital data were matched to the OSHPD data sets manually using hospital name and address. In bivariate analyses, categorical variables were compared using Pearson chi-square tests and continuous variables were compared using Wilcoxon rank-sum tests. For variables with cell counts less than 5, Fisher Exact Tests were used instead. Confounders were selected from the literature and using directed acyclic graph (DAG) theory. A comprehensive DAG was created that incorporated the exposure of interest and potential confounders, and the software DAGitty was utilized to identify a minimal set of confounders to include in regression models.30,31 Patient-level confounders included age, gender, race/ethnicity, insurance, severity of illness, and having a complex chronic condition. Insurance was included as a patient-level and index hospital-level confounder since there is evidence that insurance may affect transfer and ED choice at each level.3,32 Derived index hospital variables (eg, pediatric volume and percent Medicaid) were standardized by subtracting the sample mean and dividing the result by the sample standard deviation to put the variables on a similar scale and to stabilize model estimates. The variable pediatric inpatient capabilities was also included in the model.
Clustering by hospital was quantified by calculating the intraclass correlation. To account for clustering by hospital, multivariable mixed-effects logistic regression models included random intercepts for each hospital. Collinearity was assessed in these models using a conservative variance inflation factor threshold of 5. The need for interaction terms was assessed by placing an interaction term, between the exposure of interest and a covariate, and then checking for a statistically significant P value for the coefficient for that term. As a sensitivity analysis, we limited the population to encounters at CAHs, a commonly studied hospital population.2 In another sensitivity analysis, the non-transfer, comparison group was partitioned into admissions and discharges home. As an exploratory analysis, we analyzed each of the components of pediatric readiness with transfer using the same covariates in the core model in the primary analysis.
For this study, a P value less than .05 was considered significant. Sample size calculations were not conducted for the planned analyses. Statistical analyses were conducted using R version 3.5.2 and Stata 15 (StataCorp LLC, College Station, Texas). This study was approved by the University of California, Davis Institutional Review Board and by the California Committee for the Protection of Human Subjects. This manuscript was prepared using the REporting of studies Conducted using Observational Routinely collected health Data (RECORD) extension of the STROBE (STrengthening the Reporting of Observational Epidemiology) Statement.33
Results
Characteristics of Study Sample
In 2012, there were 135,388 pediatric encounters in 54 hospitals across California that met inclusion criteria (Figure 1). All of these hospitals had standby or basic emergency departments (Table 1). None of the hospitals were teaching institutions nor had pediatric trauma centers. Twenty-five of the hospitals were CAHs representing 20,824 encounters. Of the ED encounters, 1.44% resulted in a transfer and 1.49% resulted in an admission at the index hospital. Transferred patients tended to be younger compared to non-transferred patients (median years (IQR): 4.7 (0.9-12.0) vs 5.0 (1.7-11.3), P < .01). Male patients had higher proportions of transfers than female patients (1.6% vs 1.2%, P < .01) and White patients had higher proportions of transfer than other races/ethnicities. Patients with higher severity of illness or a complex chronic condition had higher transfer proportions (Table 2). For a comparison of hospital responders and non-responders to the NPRP assessment see Appendix 2. The pediatric readiness score ranged from 33.76 to 95.21 (Appendix 1). For the presence of certain components and weighted scores see Appendix 3.
Table 1.
Characteristics of Index Hospitals
| Pediatric Readiness Score | Low (≤70) n = 44 | High (>70) n = 10 | P a |
|---|---|---|---|
| Variable, n (%) | |||
| Pediatric Inpatient Capabilities | 26 (59%) | 7 (70%) | .72 |
| Emergency Department License Level | .48 | ||
| Standby | 21 (48%) | 3 (30%) | |
| Basic | 23 (52%) | 7 (70%) | |
| Comprehensive | 0 (0%) | 0 (0%) | |
| Trauma Center Designation | .01 | ||
| Level I or Level II | 0 (0%) | 0 (0%) | |
| Level III or Level IV | 5 (11%) | 5 (50%) | |
| None | 39 (89%) | 5 (50%) | |
| Financial Control | > .99 | ||
| Investor/For-Profit | 3 (7%) | 0 (0%) | |
| Non-Profitb | 40 (91%) | 10 (100%) | |
| Unknown | 1 (2%) | 0 (0%) | |
| Driving Time to Nearest Resourcedc Hospital (min)d | .73 | ||
| 0-30 | 1 (2%) | 0 (0%) | |
| >30-60 | 9 (21%) | 1(10%) | |
| >60 | 33 (77%) | 9 (90%) | |
| Derived Characteristics from 2011 Individual Encounters, median (IQR) | |||
| Overall Pediatric Encounters | 2,194 (1,350-4,412) | 2,696 (1,618-4,694) | .70 |
| Non-injured pediatric encounters | 1,442 (803-2,924) | 1,814 (963-3,045) | .70 |
| Medicaid Percent | 52 (40-63) | 61 (56-66) | .10 |
| Non-white Percent | 37 (25-62) | 24 (14-26) | .01 |
| Illness Severity (4 or 5) Percent | 6.3 (5.6-8.1) | 6.52 (5.7-7.5) | .84 |
P value calculations did not include missing/unknown categories. Categorical variables were compared using Pearson chi-square tests (or Fisher exact tests) and continuous variables were compared using Wilcoxon rank-sum tests.
Includes Church-related, City, District and University of California hospitals
A hospital that has a pediatric emergency department, pediatric inpatient and pediatric intensive care unit.
One hospital in the low pediatric readiness score category did not have a driving time since it was located on an island.
Table 2.
Patient Characteristics by Outcome
| Variable | Non-Transfersa n = 133,432 |
Transfers n = 1956 | P b |
|---|---|---|---|
| Patient Characteristics, n (%) | |||
| Patient age | <.01 | ||
| 0-27d | 1,812 (92.6%) | 144 (7.4%) | |
| 28d-12m | 18,295 (98.0%) | 369 (2.0%) | |
| 13m-24m | 17,486 (98.9%) | 193 (1.1%) | |
| 2y-5y | 37,090 (99.0%) | 383 (1.0%) | |
| 6y-11y | 28,026 (98.7%) | 375 (1.3%) | |
| 12y-17y | 30,723 (98.4%) | 492 (1.6%) | |
| Gender | <.01 | ||
| Female | 66,276 (98.8%) | 838 (1.2%) | |
| Male | 67,149 (98.4%) | 1118 (1.6%) | |
| Other or Unknown | 7 (100%) | 0 (0%) | |
| Race/Ethnicity | <.01 | ||
| Non-Hispanic White | 59,418 (98.4%) | 980 (1.6%) | |
| Hispanic or Latino | 59,851 (98.7%) | 782 (1.3%) | |
| Non-Hispanic Black or African American | 7,867 (98.6%) | 108 (1.4%) | |
| Other, mixed or unknown | 6,296 (98.6%) | 86 (1.4%) | |
| Primary spoken language | <.01 | ||
| English | 115,263 (98.5%) | 1734 (1.5%) | |
| Spanish | 17,873 (98.8%) | 216 (1.2%) | |
| Other language or unknown | 296 (98.0%) | 6 (2.0%) | |
| Percent Bachelors or Higher Degreec,d, median (IQR) | 16 (10-20) | 17 (11-22) | <.01 |
| Median Household Incomec,d, median (IQR) | 48,000 (41,000-58,000) | 50,000 (42,000-60,000) | <.01 |
| Encounter Characteristics, n (%) | |||
| Complex Chronic Condition | <.01 | ||
| No | 132,809 (98.6%) | 1837 (1.4%) | |
| Yes | 623 (84.0%) | 119 (16.0%) | |
| Severity of Illness | <.01 | ||
| 1 (least severe) | 4,904 (99.9%) | 4 (0.1%) | |
| 2 | 64,010 (99.8%) | 108 (0.2%) | |
| 3 | 51,548 (98.4%) | 811 (1.6%) | |
| 4 | 7,080 (90.2%) | 771 (9.8%) | |
| 5 (most severe) | 233 (60.1%) | 150 (39.1%) | |
| Missing | 5,657 (98.1%) | 112 (1.9%) | |
| Primary Payer | <.01 | ||
| Medicaid | 71,809 (98.7%) | 957 (1.3%) | |
| Private | 48,486 (98.3%) | 825 (1.7%) | |
| Uninsured/Self-pay | 9,715 (99%) | 129 (1.3%) | |
| Other | 3,410 (98.7%) | 45 (1.3%) | |
| Missing | 12 (100%) | 0 (0%) | |
Non-transfers = Discharged home or admitted at index hospital
P value calculations did not include missing/unknown categories. Categorical variables were compared using Pearson chi-square tests (or Fisher exact tests) and continuous variables were compared using Wilcoxon rank-sum tests.
Estimated from ZIP Code tabulation area census data.
Missing in non-transfers 3,777 (2.8%), missing in transfers 46 (2.4%)
Missing in non-transfers 3,856 (2.9%), missing in transfers 48 (2.5%)
Pediatric Readiness and Transfer
The intraclass correlation for the transfer outcome was 11.3% (95% CI: 7.5%-16.6%). None of the covariates presented in the final model had a statistically significant interaction term with the exposure of interest. Presented in Table 3, patients that presented to hospitals with a high pediatric readiness score (>70) had decreased odds of transfer (odds ratio (OR): 0.64, 95% confidence interval (CI): 0.55-0.74). Adjusting for covariates and a random intercept for the index hospital resulted in an adjusted odds ratio (aOR) of 0.55 (95% CI: 0.33-0.93).
Table 3.
Unadjusted and Adjusted Models of Pediatric Readiness and Odds of Transfer
| n=129,601 | |
|---|---|
| Unadjusted | OR (95% CI) |
| High Pediatric Readiness Score (>70) | 0.64 (0.55-0.74) †† |
| Adjusted | |
| High Pediatric Readiness Score (>70) | 0.55 (0.33-0.93) † |
| Age | |
| 0-27d | 5.41 (4.26-6.87) †† |
| 28d-12m | 4.05 (3.45-4.76) †† |
| 13m-24m | 2.16 (1.79-2.61) †† |
| 2y-5y | 1.67 (1.44-1.94) †† |
| 6y-11y | 1.36 (1.18-1.58) †† |
| 12y-17y | Ref |
| Gender1 | |
| Male | Ref |
| Female | 0.71 (0.64-0.79) †† |
| Race/Ethnicity | |
| White | Ref |
| Hispanic/Latino | 1.02 (0.90-1.15) |
| Black or African American | 1.06 (0.85-1.33) |
| Other or mixed | 0.88 (0.70-1.13) |
| Insurance | |
| Private | Ref |
| Medicaid | 0.81 (0.72-0.91) †† |
| Uninsured/self-pay | 0.92 (0.74-1.13) |
| Other | 0.80 (0.57-1.11) |
| Severity of Illness | |
| 1 (least severe) | Ref |
| 2 | 0.04 (0.02-0.11) †† |
| 3 | 0.09 (0.07-0.13) †† |
| 4 | 8.74 (7.82-9.78) †† |
| 5 (most severe) | 30.6 (24.1-38.9) †† |
| Complex Chronic Condition | 2.74 (2.16-3.47) †† |
| Index Hospital… | |
| …Pediatric Inpatient Capabilities | 1.04 (0.70-1.55) |
| … Pediatric Volumea,b | 0.90 (0.65-1.23) |
| … Proportion Medicaida,b | 1.06 (0.81-1.40) |
P < .05,
P < .01
Missing or unknown data were excluded.
Standardized by subtracting mean and dividing result by standard deviation
When the non-transfer, comparison group was limited to discharges home the aOR was 0.57 (95% CI: 0.34-0.95, n=127,617). When compared to admissions, the aOR was 0.43 (95% CI: 0.19-0.96, n=3,828). When limiting the sample to encounters at critical access hospitals, the adjusted association was more pronounced at 0.38 (95% CI: 0.17-0.86).
Pediatric Readiness Components and Transfer
As seen in Table 4, out of the 6 sections of pediatric readiness, only 1 section was associated with decreases in odds of transfer in unadjusted analyses: Policies, Procedures and Protocols. When adjusting for the covariates in the core model, this section remained significant. EDs in the highest readiness quartile had lower odds of transfer than EDs in the lowest readiness quartile (aOR: 0.54, 95% CI: 0.31-0.91). When adjusting for multiple components simultaneously, the precision of the estimates decreased, and all the confidence intervals included 1. When looking at the individual items in the “Policies, Procedures, and Protocols” section, only 1 item was statistically significant: “Pediatric assessment and reassessment” (aOR: 0.65, 95% CI: 0.43-0.99). The other 7 items were non-significant but were consistent with lowered odds of transfer except for “Transfer guidelines,” which was closer to 1 (aOR: 1.01, 95% CI: 0.64-1.61).
Table 4.
Unadjusted and Adjusteda Associations Between the Components of Pediatric Readiness and Odds of Transfer
| Unadjusted | Single component in modela | Multiple components in modela | ||
|---|---|---|---|---|
| Section | Transferred | |||
| d | P b | OR (95% CI) | OR (95% CI) | |
| Pediatric Readiness Score | .008 | |||
|
| ||||
| ≤ 70 | 1.53% | Ref | - | |
| > 70 | 0.98% | 0.56 (0.34-0.93) | - | |
| Pediatric Emergency Care Coordinators | .10 | |||
|
| ||||
| Neither | 1.32% | Ref | Ref | |
| Nurse or Physician | 1.92% | 1.13 (0.74-1.73) | 1.12 (0.4-1.67) | |
| Competency Evaluations | .36 | |||
|
| ||||
| Neither | 1.66% | Ref | Ref | |
| Nurse or Physician | 1.35% | 0.83 (0.54-1.26) | 0.80 (0.50-1.29) | |
| Quality Improvement (QI) | .58 | |||
|
| ||||
| QI/Performance plan absent | 1.41% | Ref | Ref | |
| QI/Performance plan present | 1.57% | 1.09 (0.65-1.82) | 1.07 (0.61-1.88) | |
| Safety c | .06 | |||
|
| ||||
| Q1 | 2.11% | Ref | Ref | |
| Q2 | 1.56% | 0.85 (0.40-1.80) | 1.23 (0.58-2.62) | |
| Q3-Q4 | 1.31% | 0.67 (0.40-1.11) | 0.74 (0.44-1.24) | |
| Policies/Procedures/Protocols d | .002 | |||
|
| ||||
| Q1 | 1.96% | Ref | Ref | |
| Q2 | 1.54% | 0.72 (0.40-1.32) | 0.82 (0.42-1.59) | |
| Q3 | 1.92% | 0.88 (0.50-1.56) | 1.01 (0.55-1.86) | |
| Q4 | 0.98% | 0.54 (0.31-0.91) † | 0.55 (0.29-1.03) | |
| Equipment and Supplies for Children e | .30 | |||
|
| ||||
| Q1 | 1.52% | Ref. | Ref | |
| Q2 | 1.45% | 0.99 (0.53-1.85) | 0.76 (0.41-1.41) | |
| Q3 | 1.81% | 1.30 (0.75-2.22) | 1.43 (0.84-2.44) | |
| Q4 | 1.21% | 0.95 (0.56-1.65) | 1.09 (0.63-1.87) | |
P < .05
Models include the covariates from the core model in Table 3 and random intercepts. Coefficients for these other covariates not shown.
Chi-square tests adjusted for clustering at the hospital level.
Aggregate weighted section score divided into quartiles: Quartile 1 (0 to <9.45 pts), Quartile 2 (9.45 to <12.6 pts), Quartiles 3-4 (12.6 to < 14 pts)
Aggregate weighted section score divided into quartiles: Quartile 1 (0 to <4.24 pts), Quartile 2 (4.24 to < 8.48 pts), Quartile 3 (8.48 to < 10.6 pts), Quartile 4 (10.6 to 17 pts)
Aggregate weighted section score divided into quartiles: Quartile 1 (0 to <26.2 pts), Quartile 2 (26.2 to <28.8 pts), Quartile 3 (28.8 to < 31.2 pts), Quartile 4 (31.2 to 33 pts)
Discussion
In this study of pediatric encounters starting at 54 small rural California hospitals, high ED pediatric readiness scores (>70) were associated with decreased odds of transfer. Having a higher score indicated that the ED had more of the components recommended by the 2009 “Guidelines of Care of Children in the Emergency Department.” This effect was more pronounced after limiting the comparison group to admissions at the index hospital and after limiting the sample to encounters at CAHs. This study found that having a higher score for “Policies, Procedures, and Protocols” was associated with lower odds of transfer.
The section with the strongest decrease in transfer was the section “Policies, Procedures, and Protocols.” Most of the individual policies in that section conceptually would be consistent with lower odds of transfer. For example, having a triage policy may enable the ED to more accurately assess the severity of a child’s symptoms and the level of appropriate care. The policy that had the most impact on transfer rate was one on pediatric assessment and reassessment. This suggests that ongoing assessment practices can allow for stabilization and avert the need for transfer. The one policy that was not consistent was the presence of transfer guidelines. The association between transfer guidelines and transfer was very close to 1. This could indicate that hospitals may be relying on informal agreements with other hospitals or that transfer guidelines may be focusing on transfer logistics rather than appropriateness of transfer. Alternatively, the transfer guidelines could be outdated, or the ED staff may not be aware of existing transfer guidelines. In contrast, a previous study hypothesized that using protocols during the transfer process could possibly decrease transfers.16 However, that study focused on trauma patients and made these indirect inferences based on the presence or absence of a mature trauma network which would likely have protocols established. More work is needed to identify how to make transfer guidelines more relevant and effective.
Other sections that did not seem to be associated with transfer were the presence of pediatric emergency care coordinators or pediatric specific equipment and supplies. The lack of an association with pediatric care coordinators was surprising. Previously, a quasi-experimental study found a decrease in pediatric transfers after implementing a bundled intervention that included a pediatric care coordinator.34 These findings suggest that a pediatric care coordinator might be a critical component of a bundled intervention, but the coordinator should be combined with other intervention elements to impact transfer rates. Higher scores on the pediatric-specific equipment and supplies were not associated with decreased transfers. This may indicate that the need for sub-specialty expertise and equipment may be a stronger driver than the presence of items such as a pediatric-sized blood pressure cuff and endotracheal tube.
This study lends preliminary evidence that pediatric readiness may be associated with the transfer process in small rural hospitals. Previous studies examining risk factors for transfer found non-actionable risk factors. Low pediatric volume makes emergency care challenging in small, community hospitals.2,35 In other studies, a driver of pediatric transfers was the need for sub-specialty consults.36,37 In contrast, this study found that meeting the 2009 “Guidelines of Care of Children in the Emergency Department” regarding “Policies, Procedures and Protocols,” could be associated with decreased transfers. This study complements the findings that there are modifiable risk factors that critical access hospitals could improve for pediatric readiness.2 This exploratory analysis suggests a need for further study of the true impact of the components of the assessment on various outcomes, including transfer.
Limitations
The biggest limitation of this study was that it was cross-sectional and we were unable to conduct causal inference. To mitigate possible confounding, this study included individual- and hospital-level covariates and a random intercept for clustering at the hospital level. However, there may still be residual confounding of unmeasured variables such as family preference for transfer and the use of telemedicine to access sub-specialty care.37 Furthermore, we were unable to capture all factors that may have affected the transfer decision. For example, patients with less time-sensitive conditions may have been able to bypass small rural hospitals, but patients with more time-sensitive conditions might have been taken to the closest small rural hospital. Although these data allow for linking through an encoded social security number, this field was missing for most of the patient encounters. There was also a possibility that individuals may have been double counted in ED to ED transfers. This study also had limited generalizability as it focused on a specific patient population seen at small rural hospitals in California. Larger hospitals tend to have additional financial and personnel resources that may alter pediatric readiness and tendency to transfer. Although the findings may not be generalizable outside of the state of California, the methods used in this study could be translated to other states and other pediatric populations, such as injured and poisoned children. Only 10 hospitals were considered to have high pediatric readiness, and this small number could bias the study. Pediatric readiness was a dichotomized continuous variable, which carries many statistical drawbacks and may have obfuscated linear relationships between pediatric readiness and transfer.38 However, preliminary analysis indicated there seemed to be a threshold effect rather than a linear association between pediatric readiness and transfer. Lastly, pediatric readiness was assessed by self-reported assessment in hospitals and there is likely variability based on the respondent. Decreasing this source of potential bias would likely narrow confidence intervals and improve the confidence of the estimates.
Conclusion
EDs at small rural hospitals with high pediatric readiness scores are less likely to transfer children to a higher level of care than those with lower scores. This study reinforces the importance of providing high quality pediatric emergency care to reduce transfers and keep children within their communities.
Supplementary Material
Acknowledgements:
The authors would like to thank the National Pediatric Readiness Project and California Office of Statewide Health Planning and Development for the provision of data.
Funding: This study was supported by the Health Resources and Services Administration’s Emergency Medical Services for Children Program SPROC TACTICAL grant (H3AMC24073). Monica K. Lieng was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through grant number UL1 TR001860 and linked award TL1 TR001861. Jennifer L. Rosenthal was supported by NCATS, NIH, through grant number UL1 TR001860 and linked award KL2 TR001859. These funding sources had no involvement in the following: study design; collection, analysis and interpretation of the data; writing of the report; and decision to submit the article for publication. The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Gausche-Hill M, Schmitz C, Lewis RJ. Pediatric Preparedness of US Emergency Departments: A 2003 Survey. Pediatrics. 2007;120(6):1229–1237. doi: 10.1542/peds.2006-3780 [DOI] [PubMed] [Google Scholar]
- 2.Pilkey D, Edwards C, Richards R, Olson LM, Ely M, Edgerton EA. Pediatric Readiness in Critical Access Hospital Emergency Departments. J Rural Health. 2019;35(4):480–489. doi: 10.1111/jrh.12317 [DOI] [PubMed] [Google Scholar]
- 3.Nacht J, Macht M, Ginde AA. Interhospital Transfers from U.S. Emergency Departments: Implications for Resource Utilization, Patient Safety, and Regionalization. Acad Emerg Med. 2013;20(9):888–893. doi: 10.1111/acem.12209 [DOI] [PubMed] [Google Scholar]
- 4.Mohr NM, Harland KK, Shane DM, Miller SL, Torner JC. Potentially Avoidable Pediatric Interfacility Transfer Is a Costly Burden for Rural Families: A Cohort Study. Acad Emerg Med. 2016;23(8):885–894. doi: 10.1111/acem.12972 [DOI] [PubMed] [Google Scholar]
- 5.França UL, McManus ML. Trends in Regionalization of Hospital Care for Common Pediatric Conditions. Pediatrics. 2018;141(1):e20171940. doi: 10.1542/peds.2017-1940 [DOI] [PubMed] [Google Scholar]
- 6.Bertrand J, Fehlmann C, Grosgurin O, Sarasin F, Kherad O. Inappropriateness of Repeated Laboratory and Radiological Tests for Transferred Emergency Department Patients. J Clin Med. 2019;8(9). doi: 10.3390/jcm8091342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaichotjinda K, Chantra M, Pandee U. Assessment of interhospital transport care for pediatric patients. Clin Exp Pediatr. 2020;63(5):184–188. doi: 10.3345/kjp.2019.00024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Britto J, Nadel S, Maconochie I, Levin M, Habibi P. Morbidity and severity of illness during interhospital transfer: impact of a specialised paediatric retrieval team. BMJ. 1995;311(7009):836–839. doi: 10.1136/bmj.311.7009.836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barry PW, Ralston C. Adverse events occurring during interhospital transfer of the critically ill. Arch Dis Child. 1994;71(1):8–11. doi: 10.1136/adc.71.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gausche-Hill M, Ely M, Schmuhl P, et al. A national assessment of pediatric readiness of emergency departments. JAMA Pediatr. 2015;169(6):527–534. doi: 10.1001/jamapediatrics.2015.138 [DOI] [PubMed] [Google Scholar]
- 11.Ames SG, Davis BS, Marin JR, et al. Emergency Department Pediatric Readiness and Mortality in Critically Ill Children. Pediatrics. 2019;144(3):e20190568. doi: 10.1542/peds.2019-0568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barata I, Auerbach M, Badaki-Makun O, et al. A Research Agenda to Advance Pediatric Emergency Care Through Enhanced Collaboration Across Emergency Departments. Acad Emerg Med. 2018;25(12):1415–1426. doi: 10.1111/acem.13642 [DOI] [PubMed] [Google Scholar]
- 13.Remick K, Kaji AH, Olson L, et al. Pediatric Readiness and Facility Verification. Ann Emerg Med. 2016;67(3):320–328.e1. doi: 10.1016/j.annemergmed.2015.07.500 [DOI] [PubMed] [Google Scholar]
- 14.About Our Data - Patient Discharge Data (PDD) and Emergency Data (ED). California’s Office of Statewide Health Planning and Development (OSHPD). Accessed May 10, 2019. https://oshpd.ca.gov/data-and-reports/request-data/tools-resources/
- 15.Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP) Accessed February 28, 2019. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp [Google Scholar]
- 16.Acosta CD, Delgado MK, Gisondi MA, et al. Characteristics of Pediatric Trauma Transfers to a Level I Trauma Center: Implications for Developing a Regionalized Pediatric Trauma System in California. Acad Emerg Med Off J Soc Acad Emerg Med. 2010;17(12):1364–1373. doi: 10.1111/j.1553-2712.2010.00926.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang Y, Natale JE, Kissee JL, Dayal P, Rosenthal JL, Marcin JP. The Association Between Insurance and Transfer of Noninjured Children From Emergency Departments. Ann Emerg Med. 2016;69(1):108–116.e5. doi: 10.1016/j.annemergmed.2016.06.007 [DOI] [PubMed] [Google Scholar]
- 18.California Health And Safety Code. Vol 124840.; 1996. Accessed May 30, 2019. https://leginfo.legislature.ca.gov/faces/codes_displaySection.xhtml?lawCode=HSC§ionNum=124840 [Google Scholar]
- 19.Hospital Quarterly Financial and Utilization Report - 2011 Sum of Four Quarters. California’s Office of Statewide Health Planning and Development (OSHPD). Accessed May 7, 2018. https://www.oshpd.ca.gov/HID/Hospital-Quarterly.html
- 20.Katz MH. Multivariable Analysis: A Practical Guide for Clinicians and Public Health Researchers. 3rd edition. Cambridge University Press; 2011. [Google Scholar]
- 21.Office ACS. 2012 - 2016 ACS 5-Year Data Profiles. S1903 Median Income in the Past 12 Months (in 2016 Inflation Adjusted Dollars). Accessed February 21, 2020. https://www.census.gov/acs/www/data/data-tables-and-tools/data-profiles/2016/
- 22.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14(1):199. doi: 10.1186/1471-2431-14-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alessandrini EA, Alpern ER, Chamberlain JM, Shea JA, Holubkov R, Gorelick MH. Developing a Diagnosis-based Severity Classification System for Use in Emergency Medical Services for Children. Acad Emerg Med. 2012;19(1):70–78. doi: 10.1111/j.1553-2712.2011.01250.x [DOI] [PubMed] [Google Scholar]
- 24.California’s Office of Statewide Health Planning and Development (OSHPD). 2011 Calendar Year Hospital Utilization. California Health and Human Services Agency (CHHS). Accessed May 14, 2019. https://data.chhs.ca.gov/dataset/pre-2012-hospital-annual-utilization-report-pivot-tables/resource/7b07cf58-db62-4aa3-81c2-731b0b5bad8b
- 25.Ray KN, Marin JR, Li J, Davis BS, Kahn JM. Referring Hospital Characteristics Associated With Potentially Avoidable Emergency Department Transfers. Acad Emerg Med. Published online July 18, 2018:acem.13519. doi: 10.1111/acem.13519 [DOI] [PubMed] [Google Scholar]
- 26.Sturm JJ, Hirsh DA, Lee EK, Massey R, Weselman B, Simon HK. Practice characteristics that influence nonurgent pediatric emergency department utilization. Acad Pediatr. 2010;10(1):70–74. doi: 10.1016/j.acap.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 27.van Rein EAJ, Sadiqi S, Lansink KWW, et al. The role of emergency medical service providers in the decision-making process of prehospital trauma triage. Eur J Trauma Emerg Surg Off Publ Eur Trauma Soc. 2020;46(1):131–146. doi: 10.1007/s00068-018-1006-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zarruk RAM& & DRT& D. Gmapsdistance: Distance and Travel Time Between Two Points from Google Maps.; 2018. Accessed June 23, 2020. https://CRAN.R-project.org/package=gmapsdistance
- 29.Sommerhalter KM, Insaf TZ, Akkaya-Hocagil T, et al. Proximity to Pediatric Cardiac Surgical Care among Adolescents with Congenital Heart Defects in 11 New York Counties. Birth Defects Res 2017;109(18):1494–1503. doi: 10.1002/bdr2.1129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Textor J, van der Zander B, Gilthorpe MS, Liśkiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package ‘dagitty.’ Int J Epidemiol. 2016;45(6):1887–1894. doi: 10.1093/ije/dyw341 [DOI] [PubMed] [Google Scholar]
- 31.Williams TC, Bach CC, Matthiesen NB, Henriksen TB, Gagliardi L. Directed acyclic graphs: a tool for causal studies in paediatrics. Pediatr Res. 2018;84(4):487–493. doi: 10.1038/s41390-018-0071-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang Y, Kissee JL, Dayal P, Wang NE, Sigal IS, Marcin JP. Association Between Insurance and Transfer of Injured Children From Emergency Departments. Pediatrics. 2017;140(4). doi: 10.1542/peds.2016-3640 [DOI] [PubMed] [Google Scholar]
- 33.Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLOS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oakley E, Crellin D, Barty N, Braitberg G, Young S. Improving emergency care for children: A model of collaboration between emergency departments. Emerg Med. 2004;16(5-6):417–424. doi: 10.1111/j.1742-6723.2004.00667.x [DOI] [PubMed] [Google Scholar]
- 35.Goldman MP, Wong AH, Bhatnagar A, Emerson BL, Brown LL, Auerbach MA. Providers’ Perceptions of Caring for Pediatric Patients in Community Hospital Emergency Departments: A Mixed-methods Analysis. Acad Emerg Med. 2018;25(12):1385–1395. doi: 10.1111/acem.13509 [DOI] [PubMed] [Google Scholar]
- 36.Li J, Pryor S, Choi B, et al. Profile of Interfacility Emergency Department Transfers: Transferring Medical Providers and Reasons for Transfer. Pediatr Emerg Care. 2019;35(1):38–44. doi: 10.1097/PEC.0000000000000848 [DOI] [PubMed] [Google Scholar]
- 37.Mollen CJ, Henien M, Jacobs LM, Myers S. Parent Perceptions on Transfers to Pediatric Emergency Departments and the Role of Telemedicine: Pediatr Emerg Care. 2019;35(3):180–184. doi: 10.1097/PEC.0000000000000957 [DOI] [PubMed] [Google Scholar]
- 38.Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332(7549):1080. doi: 10.1136/bmj.332.7549.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


