Abstract
Objective:
Design, implement, and evaluate a rounding checklist with deeply embedded, dynamic electronic health record (EHR) integration.
Design:
Before-after quality improvement study.
Setting:
Quaternary PICU in an academic, free-standing children’s hospital.
Patients:
All patients in the PICU during daily morning rounds.
Interventions:
Implementation of an updated dynamic checklist (eSIMPLER) providing clinical decision support (CDS) prompts with display of relevant data automatically pulled from the EHR.
Measurements and Main Results:
The prior daily rounding checklist, eSIMPLE, was implemented for 49,709 patient-days (7,779 patients) between October 30, 2011 and October 7, 2018. eSIMPLER was implemented for 5,306 patient-days (971 patients) over 6 months. Checklist completion rates were similar (eSIMPLE: 95% (95% confidence interval (CI), 88% – 98%) vs. eSIMPLER: 98% (95% CI, 92% – 100%) of patient-days, p = 0.40). eSIMPLER required less time per patient (28 ± 1 vs. 47 ± 24 s, p < 0.001). Users reported improved satisfaction with eSIMPLER (p = 0.009). Several checklist-driven process measures—discordance between EHR orders for stress ulcer prophylaxis (SUP) and user-recorded indication for SUP, rate of VTE prophylaxis prescribing, and recognition of reduced renal function—improved during the eSIMPLER phase.
Conclusions:
eSIMPLER, a dynamic, EHR-informed checklist, required less time to complete and improved certain care processes compared to a prior, static checklist with limited EHR data. By focusing on the “Five Rights” of CDS, we created a well-accepted CDS tool that was integrated efficiently into daily rounds. Generalizability of eSIMPLER’s effectiveness and its impact on patient outcomes needs to be examined.
Keywords: Checklist, Decision Support Systems, Clinical, Intensive Care Units, Pediatric
INTRODUCTION
Since gaining traction in the context of perioperative care (1), use of checklists in routine patient care has expanded to pediatric surgery (2), anesthesia (3), and critical care (4). In many intensive care units (ICUs), checklists have been implemented as an integral part of daily patient rounds (5–7). In a complex intensive care environment, just-in-time prompts and structured review of key aspects of patients’ care allow evidence-based practices to reach the patient. Although checklists have been associated with reductions in morbidity and mortality in randomized trials (1, 8), barriers to their widespread implementation include the time necessary to complete them, ambiguity in checklist prompts, and duplication with other processes (6, 9). These limitations may be due in part to the content of most checklists being static (10, 11). Even when incorporated into electronic health records (EHRs), most checklists include the same set of questions for each patient, and these checklists only ask clinicians questions, rather than providing suggested answers and best practices (12). For instance, though estimated glomerular filtration rate (eGFR) may be available in the EHR, a typical checklist only reminds clinicians to consider whether medications should be adjusted for renal insufficiency.
More recently, attention has shifted to dynamic checklists, which not only display data appropriate to a patient’s clinical context (e.g., questions related to endotracheal tube position are relevant only for intubated patients), but also provide EHR data relevant to the checklist items (10, 13). In addition, dynamic checklists enhance situational awareness by allowing comparison of the patient’s intended care plan with actual care ordered and documented. For instance, a dynamic checklist may highlight discrepancies between intended stress ulcer prophylaxis (SUP) and a patient’s actual medication orders. Such checklists provide a means for closed loop communication and cross-checking in patients’ often fragmented care. We describe development and implementation of a dynamic, EHR-integrated checklist for daily rounds in a pediatric intensive care unit (PICU). We compared the new dynamic checklist to the former, static checklist used since 2011.
METHODS
Setting and Population
We undertook a quality improvement (QI) initiative in a quaternary medical-surgical PICU. All patients present during morning rounds were included. As a QI study, this study was deemed exempt from review by the institutional review board at Boston Children’s Hospital.
In 2006, we developed the first iteration of a daily rounding checklist, called SIMPLE as a mnemonic for its components (Supplementary Figure 1). During daily bedside multidisciplinary rounds, a physician or nurse practitioner led a discussion of checklist items and recorded a response to or acknowledgement of each prompt on a templated paper form (Supplementary Figure 1). In 2011, we digitized SIMPLE into a web-based, static checklist (eSIMPLE), followed by gradual incorporation of limited EHR data.
eSIMPLER Design, Development, and Implementation
In 2017, we began an overhaul of eSIMPLE, which we named “eSIMPLE in Real-Time” (eSIMPLER). This iteration aimed to enhance situational awareness and clinical decision support (CDS) with display of relevant data automatically pulled from the EHR. We upgraded the application to ensure accurate and relevant data were presented clearly and in a user-friendly format (Supplementary Figure 2). The guiding principle of eSIMPLER was that actual practice (sedation scores, orders, laboratory values, etc.) ought to be readily visible to the user in the context of relevant components of the checklist. Furthermore, these data were used to populate responses to prompts and drive the hierarchical logic of eSIMPLER wherever possible to minimize users’ cognitive load and effort. For instance, eSIMPLER was able to determine whether a patient was mechanically ventilated at the moment the checklist was loaded based on the respiratory support documented in the EHR. Perhaps more importantly, if a patient was mechanically ventilated days prior to accessing the checklist (but had been extubated in the interim), eSIMPLER was aware of the prior charted mechanical ventilation and distinguished this patient from a patient who was never mechanically ventilated, thus providing context to the patient’s care that was otherwise not immediately available.
This dynamic checklist also provided the opportunity to incorporate clinical decision support (CDS) to guide users toward best practices. In eSIMPLE, users were asked whether SUP was indicated for a patient (Supplementary Figure 3A). In eSIMPLER, best-practice potential indications for SUP were highlighted alongside EHR data showing if the patient was then receiving SUP (Supplementary Figure 3B). eSIMPLER’s updates emphasized workflows to address key QI areas identified by unit leadership, including sedation, dosing adjustment of medications in renal dysfunction, early discontinuation of central venous and urinary catheters, SUP, and venous thromboembolism (VTE) prophylaxis. Supplementary Table 1 summarizes the changes made in updating from eSIMPLE to eSIMPLER. Details of eSIMPLER’s programming are provided in the Supplementary Appendix.
Checklist Evaluation
We allowed a wash-in period of three months after eSIMPLER deployment before collecting post-implementation statistics. We evaluated the update from eSIMPLE to eSIMPLER from two perspectives. The first was feasibility, acceptability, and usability of the checklists. Trained administrative staff performed direct observation of rounding teams. Observers recorded variables related to checklist usage in a standard case report form. Feasibility was assessed based on completion rates and time taken to discuss and complete documentation of checklists on rounds. Time to completion was regarded as an important measure of feasibility, particularly as new features were added to eSIMPLER, because time to completion has been described as a primary barrier to checklist acceptability (9). Time to completion of the checklist was determined from direct observation of rounding teams and was defined as the time from initiating discussion of the first element in the checklist until completion of any checklist-generated discussion (defined below) and recording of responses. Acceptability and usability were evaluated by direct observations of checklist users, and by surveys sent by e-mail to all pediatric critical care medicine fellows who used both versions of the checklist. Discussion on rounds prompted by the checklist were recorded in accordance with prior studies (11, 14) using direct observation. If a checklist item prompted discussion of patient care related to that item, the observer recorded that the checklist generated discussion of that item; if the care element was discussed prior to prompting from the checklist, then the observer did not record that a discussion occurred due to the checklist.
Second, we evaluated the checklists from the perspective of several patient care process measures: 1) improvement in optimal SUP utilization; 2) increased prescription of mechanical or pharmacologic VTE prophylaxis; 3) recognition of renal dysfunction; 4) central venous catheter (CVC) utilization; and 5) frequency of weight, height/length, and head circumference measurements. Details of process measure evaluation and statistical testing are provided in the Supplementary Appendix. Analyses were performed using base R version 4.0.2 (15), except for incidence rate ratio for anthropomorphic measurements, which was performed using the epiR package (16). A p-value less than 0.05 was considered statistically significant.
RESULTS
Feasibility, Acceptability, and Usability
eSIMPLE was completed for 49,709 patient-days (7,779 unique patients) between October 30, 2011 and October 7, 2018. eSIMPLER was completed for 5,306 patient-days (971 unique patients) between January 1, 2019 and July 31, 2019. Patient characteristics are shown in Table 1. Rounds were directly observed for 91 patient-days when eSIMPLE was in use and 65 patient-days with eSIMPLER. Directly observed completion rates were similar for both eSIMPLE and eSIMPLER (86 (95%, 95% confidence interval (CI), 88% – 98%) of patient-days vs. 64 (98%, 95% CI, 92% – 100%) of patient-days, p = 0.40). We also assessed long-term compliance with eSIMPLER completion using electronic logs of eSIMPLER completion in January 2020. Of 872 eligible patient-days, 859 (99%, 95% CI, 97% – 99%) checklists were completed.
Table 1. Patient characteristics during eSIMPLE and eSIMPLER evaluation.
Values shown are N (%) for categorical variables and mean (standard deviation) for continuous variables.
| Variable | eSIMPLE (N = 14,040) | eSIMPLER (N = 1,189) | p-value |
|---|---|---|---|
| Sex = Female | 6,116 (44) | 538 (45) | 0.26 |
| Age (years) | 8.5 (7.3) | 8.5 (7.4) | 0.74 |
| Length of stay (days) | 5.6 (12.3) | 5.6 (11.7) | 0.54 |
| Diagnosis category | < 0.001 | ||
| BMT/SCT | 341 (2.4) | 35 (2.9) | |
| Medical | 2,170 (15.5) | 187 (15.7) | |
| Neurology | 5,426 (38.6) | 520 (43.7) | |
| Oncology | 1,350 (9.6) | 123 (10.3) | |
| Surgical | 4,749 (33.8) | 324 (27.2) | |
| Unknown | 4 (0.03) | -- | |
| PIM2 score | −5.2 (1.6)a | −5.4 (1.7)b | < 0.001 |
| PIM3 score | −5.3 (1.7)c | −5.3 (1.8)d | 0.71 |
PIM = Pediatric index of mortality
PIM2 score was available for 9,781 admissions
PIM2 score was available for 1,169 admissions
PIM3 score was available for 7,075 admissions
PIM3 score was available for 1,169 admissions
Based on direct observation, as compared to eSIMPLE, eSIMPLER took less time per patient to complete (28 ± 1 s vs. 47 ± 24 s, p < 0.001). Eight of 13 fellows (62% response rate) responded to our survey comparing utility of and satisfaction with eSIMPLER as compared to eSIMPLE (Figure 1). Fellows found eSIMPLER easier to use (p = 0.01), more clear and concise (p = 0.04), more accurate (p = 0.02), more useful (p = 0.02), and an improvement from eSIMPLE (p = 0.009). Overall, most fellows were somewhat satisfied or very satisfied with eSIMPLER (p = 0.02). Clinicians using eSIMPLE/eSIMPLER interjected less often during rounds with the newer checklist (at least one interjection on 17 (26%, 95% CI, 16% – 39%) patient-days vs. 49 (54%, 95% CI, 43% – 64%) patient-days, p < 0.001).
Figure 1. Survey results comparing satisfaction with eSIMPLE and eSIMPLER.
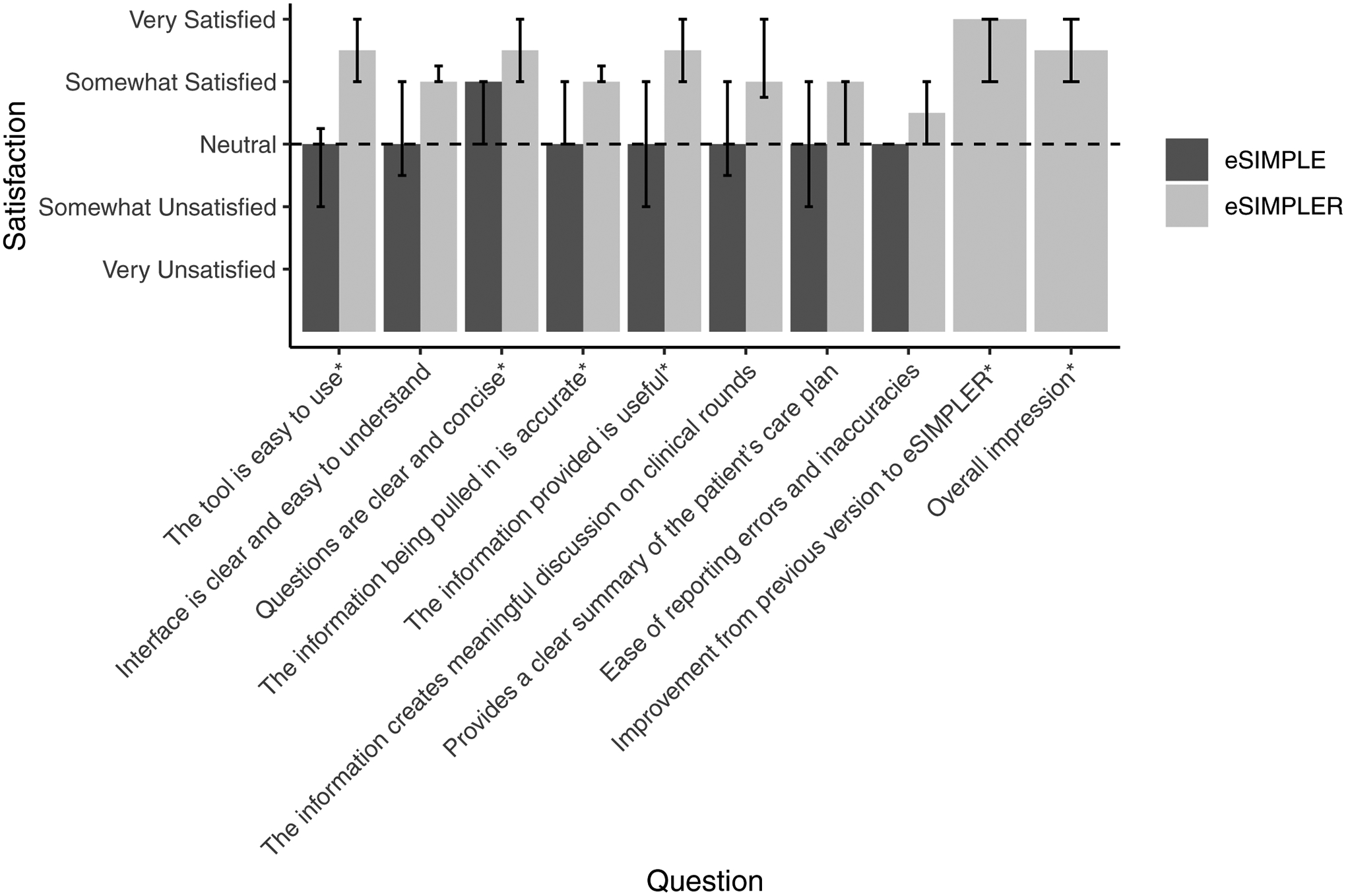
Bars indicate median satisfaction with each aspect of the checklist. Error bars indicate interquartile range. An asterisk (*) next to the question indicates that differences between eSIMPLE and eSIMPLER were statistically significant (p < 0.05), or that the satisfaction with eSIMPLER was significantly greater than “neutral.”
Process Measures
During eSIMPLER use, adherence to SUP best practices improved significantly. During the eSIMPLER phase, users identified a need for SUP less often (85% vs. 88% of patient-days, odds ratio (OR) = 0.74 (95% CI, 0.68 – 0.80), p < 0.001) and, when SUP was indicated, an appropriate corresponding order for SUP was found in the EHR more often (93% vs. 88% of patient-days, OR = 1.8 (95% CI, 1.6 – 2.1), p < 0.001). Overall, the incidence of discordance between EHR orders for SUP and indications for SUP was significantly decreased with eSIMPLER compared with eSIMPLE (9% vs. 14%, OR = 0.56 (95% CI, 0.50 – 0.63), p < 0.001).
Clinician recognition of need for VTE prophylaxis increased significantly when eSIMPLER was in use (47% of patient-days) compared to when eSIMPLE was in use (31%, OR = 1.9 (95% CI, 1.8 – 2.1), p < 0.001). Correspondingly, prescription for VTE prophylaxis increased from 35% to 46% of patient-days (OR = 1.6 (95% CI, 1.5 – 1.7), p < 0.001).
When eGFR was calculable (85% of patient-days for eSIMPLE and 86% for eSIMPLER), eGFR was < 90 mL/min/m2 for 18% of patient-days while eSIMPLE was in use and for 17% while eSIMPLER was in use. When eGFR was < 90 mL/min/m2, need to adjust medications for renal dysfunction was recognized more frequently with eSIMPLER (51% of patient-days) than with eSIMPLE (42%, OR = 1.5 (95% CI, 1.3 – 1.7), p < 0.001).
CVC utilization did not change between the eSIMPLE and eSIMPLER epochs (36% vs. 36%, OR = 1.0 (95% CI 0.86 – 1.2), p = 0.903). Weight and height/length were measured more frequently when eSIMPLER was in use (24.1 and 8.2 measurements per 100 patient-days, respectively) than when eSIMPLE was in use (21.1 and 6.6 measurements per 100 patient-days, respectively; IRR = 1.2 (95% CI 1.1 – 1.2), p < 0.001), but head circumference measurement frequency decreased with eSIMPLER (5.3 per 100 patient-days) vs. eSIMPLE (9.0 per 100 patient-days, IRR = 0.59 (95% CI 0.39 – 0.86), p < 0.001).
DISCUSSION
eSIMPLER, a dynamic, EHR-informed checklist for daily rounds, required less time to complete, provided opportunities to optimize care processes, and improved adherence to ongoing QI initiatives as compared to a static checklist with more limited incorporation of EHR data. In particular, we increased adherence in our PICU to best practices around SUP usage, VTE prophylaxis prescribing, adjustment of medications for renal dysfunction, and frequency of updating weight and height measurements. The revised checklist was well received by users. Overall, these changes were achieved through increased clarity of checklist content, better integration of EHR data, and emphasis on CDS best practices.
Checklists have been widely adopted in critical care (4, 5), but barriers to their effectiveness are prevalent. Nan and colleagues state that the static nature of most checklists, even when presented in an electronic format, limits their utility (10). An iteration of their “context-aware” checklist, Tracebook, was evaluated by De Bie and colleagues (13). Unlike our study, which examined real-world clinical use of eSIMPLER, their evaluation was performed using simulated patient cases. In four of six scenarios examined, the dynamic checklist took significantly longer to complete than the local standard of care (13). Similarly, rounding time increased by 2 minutes per patient when Hulyalkar and colleagues evaluated CERTAINp (17). eSIMPLER, in contrast, typically required less time to complete than eSIMPLE in our PICU. This difference is particularly important since time to completion of checklists has been identified as a barrier to their widespread acceptance (9). The shorter time to completion may be because eSIMPLER contained half as many “checkable items” compared to the study by de Bie and colleagues (13). Automatic responses to some questions based on EHR data allowed fewer clicks in eSIMPLER as compared to eSIMPLE. Improved clarity of information display may also have contributed to eSIMPLER’s effectiveness. Finally, a rounding checklist was already embedded in our daily rounds for 12 years prior to the introduction of eSIMPLER, and unit culture around checklist use may affect usability.
We designed eSIMPLER with the “Five Rights” of CDS in mind. The Five Rights postulate that CDS is most effective when the right information is delivered to the right person, through the right intervention format and the right channel, and at the right time in workflow (18). The use of eSIMPLER during multidisciplinary rounds allowed clinicians leading discussion of checklist items to direct care instructions to appropriate team members (residents to place new orders; nurses to send laboratory tests; etc.). Contextual information was displayed within eSIMPLER as part of the CDS. Finally, CDS within eSIMPLER was non-interruptive, and thus could be incorporated into the team’s rounding workflow when most appropriate.
Similar to other studies of pediatric rounding checklists (17), eSIMPLER use improved adherence to standard of care guidelines, specifically around appropriate use of SUP, VTE prophylaxis, and adjustment of medications for renal dysfunction. A strength of our study is that we examined not only adherence to discussion of crucial patient care elements, as was done in prior studies (8, 11, 14), but also (in the case of SUP and VTE prophylaxis) whether that discussion led to a change in actual patient care. Specifically, we decreased overall SUP use, which is particularly notable since no other QI initiatives actively targeted SUP use during the time of eSIMPLER implementation and evaluation. In contrast, McKelvie and colleagues found that discussion of SUP spurred by a rounding checklist rarely led to a change in patient management (14). We speculate that eSIMPLER’s clear display of CDS for indications, current EHR orders (or lack thereof), and a prompt to indicate whether the team believed SUP was indicated each day led to a “pause” and team discussion whether to initiate, continue or discontinue SUP and ultimately reduced discrepancies between SUP indications, team intent, and SUP prescribing. Although we did not specifically evaluate whether SUP use was clinically indicated, prior studies have shown high rates of SUP use in the PICU, but low incidence of clinically significant gastrointestinal bleeding (19, 20). We also showed that VTE prophylaxis prescribing increased in proportion to increased need for VTE prophylaxis recorded in eSIMPLER. While we believe that some of this improvement is attributable to eSIMPLER’s clearer prompts regarding VTE prophylaxis and display of what type of, if any, VTE prophylaxis was ordered for the patient, secular trends and other QI efforts may have also contributed to this change. In contrast, no change was observed in CVC utilization, likely because changes to this section were minimal and cosmetic in nature.
Our study has several limitations. First, we did not assess if changes in process measures affected patient outcomes. Not all changes between eSIMPLE and eSIMPLER were designed to have measurable process or outcome metrics. Many of the changes improved situational awareness (e.g., display of sedation scores) but no discrete change in care practice was expected in response. Second, generalizability of our findings to other settings and institutions may depend on institutional culture and workflow. Because we do not use a common data model, in order to implement eSIMPLER in another unit, extensive customization and mapping to local EHRs would be necessary. Future work to update eSIMPLER to use normalized ontologies and interoperable standards such as Fast Healthcare Interoperability Resources (FHIR) is planned but may be limited by the number of ICU-specific elements that have been mapped to FHIR. Third, because eSIMPLE did not implement logging of loading times or errors, we were not able to assess any changes to these potential balancing measures with implementation of eSIMPLER. Finally, we had a relatively small number of direct observations of checklist use and of fellow surveys.
CONCLUSION
An electronic, EHR-informed, dynamic checklist was used consistently, did not prolong checklist completion time, and improved adherence to best practices around several process measures. Future studies must examine the impact of checklists that provide just-in-time clinical decision support on improving patient outcomes, and future software development should emphasize cross-platform interoperability using open standards and common data models.
Supplementary Material
REPORT IN CONTEXT.
Checklists are commonly used in ICUs.
Time burden, lack of clarity, and static nature make their widespread adoption challenging.
We implemented and evaluated a novel, dynamic, electronic health record-informed rounding checklist
AT THE BEDSIDE.
Dynamic, electronic health record-informed checklists can be successfully incorporated into daily patient rounds and improve process measures. Focusing on the “Five Rights” of clinical decision support in designing such systems improves their effectiveness.
Generalizability of such a checklist will require increased uptake of open standards and common data models to support cross-platform interoperability.
Future studies should examine the effect of such smart checklists on patient outcomes.
Conflicts of Interest and Source of Funding:
Dr. Geva was supported by grants T32 HD040128 and K12 HD047349 from the NICHD/NIH and grant L40 HL133929 from the NHLBI/NIH. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. For the remaining authors none were declared.
Copyright Form Disclosure: Dr. Geva’s institution received funding from the National Institute of Child Health and Human Development/the National Institutes of Health (NIH) and the National Heart, Lung, and Blood Institute, and he received support for article research from the NIH. Dr. Harty disclosed work for hire. Dr. Kleinman disclosed Volunteer service for American Heart Association and International Liaison Committee on Resuscitation. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009;360(5):491–499. [DOI] [PubMed] [Google Scholar]
- 2.Oak SN, Dave NM, Garasia MB, et al. Surgical checklist application and its impact on patient safety in pediatric surgery. J Postgrad Med 2015;61(2):92–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krombach JW, Marks JD, Dubowitz G, et al. Development and implementation of checklists for routine anesthesia care: A proposal for improving patient safety. Anesth Analg 2015;121(4):1097–1103. [DOI] [PubMed] [Google Scholar]
- 4.Dubose J, Teixeira PG, Inaba K, et al. Measurable outcomes of quality improvement using a daily quality rounds checklist: one-year analysis in a trauma intensive care unit with sustained ventilator-associated pneumonia reduction. J Trauma 2010;69(4):855–860. [DOI] [PubMed] [Google Scholar]
- 5.Lane D, Ferri M, Lemaire J, et al. A systematic review of evidence-informed practices for patient care rounds in the ICU. Crit Care Med 2013;41(8):2015–2029. [DOI] [PubMed] [Google Scholar]
- 6.Ullman A, Long D, Horn D, et al. The KIDS SAFE checklist for pediatric intensive care units. Am J Crit Care 2013;22(1):61–69. [DOI] [PubMed] [Google Scholar]
- 7.Barcellos RA, Chatkin JM. Impact of a multidisciplinary checklist on the duration of invasive mechanical ventilation and length of ICU stay. J Bras Pneumol 2020;46(3):e20180261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Vries EN, Prins HA, Crolla RM, et al. Effect of a comprehensive surgical safety system on patient outcomes. N Engl J Med 2010;363(20):1928–1937. [DOI] [PubMed] [Google Scholar]
- 9.Fourcade A, Blache JL, Grenier C, et al. Barriers to staff adoption of a surgical safety checklist. BMJ Qual Saf 2012;21(3):191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nan S, Gorp PV, Korsten HHM, et al. Tracebook: A dynamic checklist support system. In: 2014 IEEE 27th International Symposium on Computer-Based Medical Systems; 27–29 May 2014. p. 48–51. [Google Scholar]
- 11.Centofanti JE, Duan EH, Hoad NC, et al. Use of a daily goals checklist for morning ICU rounds: a mixed-methods study. Crit Care Med 2014;42(8):1797–1803. [DOI] [PubMed] [Google Scholar]
- 12.Tarrago R, Nowak JE, Leonard CS, et al. Reductions in invasive device use and care costs after institution of a daily safety checklist in a pediatric critical care unit. Jt Comm J Qual Patient Saf 2014;40(6):270–278. [DOI] [PubMed] [Google Scholar]
- 13.De Bie AJR, Nan S, Vermeulen LRE, et al. Intelligent dynamic clinical checklists improved checklist compliance in the intensive care unit. Br J Anaesth 2017;119(2):231–238. [DOI] [PubMed] [Google Scholar]
- 14.McKelvie BL, McNally JD, Menon K, et al. A PICU patient safety checklist: rate of utilization and impact on patient care. Int J Qual Health Care 2016;28(3):371–375. [DOI] [PubMed] [Google Scholar]
- 15.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. https://www.-R-project.org. [Google Scholar]
- 16.Stevenson M, Sergeant E. epiR: Tools for the Analysis of Epidemiological Data. 2020. https://CRAN.R-project.org/package=epiR.
- 17.Hulyalkar M, Gleich SJ, Kashyap R, et al. Design and alpha-testing of an electronic rounding tool (CERTAINp) to improve process of care in pediatric intensive care unit. J Clin Monit Comput 2017;31(6):1313–1320. [DOI] [PubMed] [Google Scholar]
- 18.Blecker S, Pandya R, Stork S, et al. Interruptive versus noninterruptive clinical decision support: Usability study. JMIR Hum Factors 2019;6(2):e12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duffett M, Chan A, Closs J, et al. Stress ulcer prophylaxis in critically ill children: A multicenter observational study. Pediatr Crit Care Med 2020;21(2):e107–e113. [DOI] [PubMed] [Google Scholar]
- 20.Costarino AT, Dai D, Feng R, et al. Gastric acid suppressant prophylaxis in pediatric intensive care: Current practice as reflected in a large administrative database. Pediatr Crit Care Med 2015;16(7):605–612. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


