Introduction
This image shows a novel, real-time method of locating the stellate ganglion using near-infrared (NIR) intraoperative imaging with indocyanine green (ICG) during bilateral cardiac sympathetic denervation (CSD). The research reported here adhered to Helsinki Declaration guidelines.
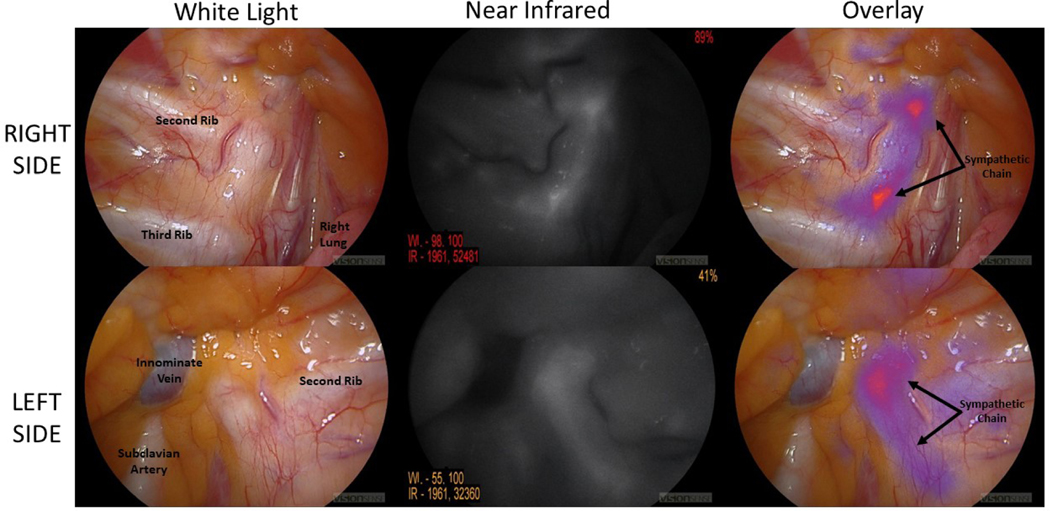
The patient is a 40-year-old female with recurrent ventricular tachyarrhythmias due to a familial cardiomyopathy caused by a variant in NKX2.5, a transcription factor which functions in heart development. She had failed multiple prior attempts at catheter ablation. She was referred for CSD and was systemically infused with 5 mg/kg ICG 24 hours preoperatively. Intraoperatively, a thoracoscope (VisionSense, New York, NY) capable of white light and NIR imaging was used. The sympathetic chain was not well visualized under white light guidance. NIR imaging clearly located the stellate ganglion, which was divided bilaterally (Figure 1). The patient had no complications from the procedure and has not had any further episodes of VT over a follow-up period of two years.
Figure 1.
Near-infrared intraoperative imaging localizes the stellate ganglion bilaterally. The top row of images depicts the patient’s right side with the sympathetic chain not clearly identifiable by white-light thoracoscopy in the far left column. NIR and fused images in the center and right columns, respectively, show clear visualization of the stellate ganglion under IMI guidance. The bottom row depicts similar images on the patient’s left side.
CSD has shown efficacy in treating refractory tachyarrhythmias in several recent case series.1–3 Despite these encouraging findings, CSD is not effective in a significant proportion of patients. This failure may be explained in part by pathologic neural remodeling in these patients, which can make sympathetic chain identification challenging.2 There are no prior reports of real-time, intraoperative methods of cardiac sympathetic nerve imaging as an adjunct to CSD.
Previous work by our group has shown the efficacy of NIR intraoperative imaging with ICG as a tumor mapping agent during oncologic surgery.4 ICG has been used previously to image nerves but this is the first use of ICG-based imaging as an adjunct for CSD.5 This case underscores the feasibility of this technique, which may improve success rates for CSD.
Footnotes
Disclosures: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Assis FR et al. Cardiac sympathectomy for refractory ventricular tachycardia in arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm. 2019;16(7):1003–1010. [DOI] [PubMed] [Google Scholar]
- 2.Krishnan A et al. Sympathectomy for stabilization of heart failure due to drug-refractory ventricular tachycardia. The Annals of thoracic surgery. 2018;105(2):e51–e53. [DOI] [PubMed] [Google Scholar]
- 3.Vaseghi M et al. Cardiac sympathetic denervation for refractory ventricular arrhythmias. J Am Coll Cardiol. 2017;69(25):3070–3080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kennedy GT et al. Intraoperative near-infrared imaging of mesothelioma. Translational lung cancer research. 2017;6(3):279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walsh EM et al. Fluorescence imaging of nerves during surgery. Ann Surg. 2019;270(1):6976. [DOI] [PubMed] [Google Scholar]