Abstract
Objective
Optimism is modifiable and may be associated with healthy ageing. We aim to investigate whether dispositional optimism is associated with all-cause mortality in adults aged 70 years and older.
Methods
Between 2010 and 2014, older adults free of serious cardiovascular disease and dementia were recruited through primary care physicians, and enrolled in the Aspirin Reducing Events in the Elderly (ASPREE) clinical trial. Australian ASPREE participants were invited to participate in the ASPREE Longitudinal Study of Older Persons (ALSOP) that was running in parallel to ASPREE. Optimism was assessed at baseline using the Life Orientation Test – Revised (LOT-R). The association between optimism, divided into quartiles, and all-cause mortality was assessed using Cox Proportional Hazard models.
Results
11,701 participants (mean age: 75.1 years, SD 4.24; 46.6% men) returned the ALSOP Social questionnaire and completed the LOT-R. During the median 4.7 years follow-up, 469 deaths occurred. The fully adjusted model was not significant (HR 0.78, 95% CI 0.58-1.06). There was evidence that age was an effect modifier of the association between optimism and longevity. Higher optimism was associated with lower mortality risk in the oldest individuals only (77+ years) (HR 0.61, 95% CI 0.39-0.96).
Conclusions
We observed no independent relationship between optimism and all-cause mortality in the total sample, although optimism appeared to be associated with lower risk among oldest old (adults aged 77 years and over).
Keywords: Dispositional optimism, mortality, effect modification, older adults, cohort study
Introduction
In 2019, 703 million people globally were aged 65 years or older; and the proportion of those aged 65 years or older is predicted to increase from one in 11 people in 2019 to one in six people by 2050 (1). Ageing is associated with increased risk of chronic disease, such as cardiovascular disease, cancer, osteoarthritis and dementia (2). With population ageing across the world, the burden of chronic disease continues to grow (3). Psychological wellbeing may play an important role in mitigating the risk of chronic diseases in older age (4), and decreasing the risk of all-cause mortality (5). Positive psychological constructs, such as optimism, are increasingly recognised as being associated with better health outcomes in older adults (6).
There are two main theoretical perspectives that explain the nature of optimism, though there is no one accepted definition of optimism, or standard instrument used to measure optimism (7). One theory suggests that optimism is a personality trait characterised by positive expectations for the future (dispositional optimism), whilst it is also proposed that optimism describes a characteristic way of explaining the causes of both positive and negative events (attributional optimism) (8, 9, 10, 11).
Optimism has both a trait and state component, with the ‘trait’ describing a relatively stable individual difference in level of optimism and ‘state’ optimism being a level of optimism that is amenable to change according to context or situation (12). The heritability of optimism, at approximately 25%, is reported as being lower than the heritability of some other personality traits, including the ‘Big 5’ (neuroticism, extraversion, openness for experience, conscientiousness and agreeableness) (13, 14). The results of a meta-analysis of randomised controlled intervention studies of optimism training indicate that psychological interventions can increase optimism, indicating that state optimism is modifiable (15).
Previous research has reported that optimism is associated with positive outcomes in cardiovascular disease (16), cancer (17), and immune function (18), as well as predicting lower pain classifications (19). Optimism has been associated with healthy ageing (survival with functional ability that enables wellbeing with age) in men and women (20, 21); and with a greater likelihood of individuals surviving to 85 years of age (22). However, evidence is scarce on whether optimism assessed relatively late in the trajectory of lifespan is beneficial. Only two studies to date have included older individuals (65 years and older), with varying disease status and disability, and observed that higher optimism was associated with a lower risk of all-cause mortality. Whether levels of optimism in older individuals who reached later life in good health are beneficial, is unknown. Therefore, the aim of this study was to explore the association between optimism and all-cause mortality among men and women aged 70 years and over living independently and free of cardiovascular disease, dementia or major disability.
Methods
Study Population
This study used data from the Aspirin Reducing Events in the Elderly (ASPREE) study and the ASPREE Longitudinal Study of Older Persons (ALSOP) sub-study. (23, 24). Between 2010 and 2014, healthy older adults living in the United States of America (USA) or Australia, and who were living independently and free of cardiovascular disease, dementia or major disability, were enrolled in the ASPREE. The ASPREE was a primary prevention trial to assess the effects of a daily dose of aspirin (24), and the major findings of the ASPREE study have been previously published (23, 25, 26).
The present study focuses on the Australian participants who were recruited through general practice with willing general practitioners (primary care physicians) acting as ASPREE co-investigators and assessing their patients for suitability to take part in the study (27, 28). The 16,703 Australian ASPREE clinical trial participants were also eligible to participate in the ASPREE Longitudinal Study of Older Persons (ALSOP) sub-study. ALSOP constituted a series of questionnaires at baseline and then biannually. The second baseline questionnaire was returned by 12,896 participants. Out of these, 11,866 completed the Life Orientation Test, Revised (LOT-R), while complete data for the rest of the variables of interest for this study were available for 11,701 participants (Figure 1). The ALSOP participants were considered to be broadly representative of the population of older Australians who had reached the age of 70 in relatively good health (24). ALSOP assessed overall health and lifestyle, as well as behavioural, social, economic and environmental factors related to healthy ageing (24).
Figure 1.
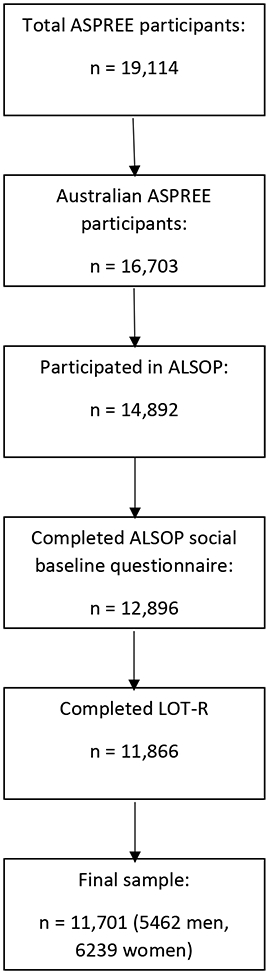
Flow diagram of selection of participants
Measures and Scales
Assessment of optimism
The analysis of optimism was assessed through the LOT-R. The LOT-R consists of ten items - three positively worded items, three negatively worded items, and four items that are not actually used to calculate the optimism score (known as filler questions) . Controversy surrounds whether the LOT-R measures one factor, i.e. is a unidimensional scale, or whether the LOT-R measures two distinct factors (i.e. optimism and pessimism) (29). The scale developers intended for all items to be pooled to provide a composite score of total optimism, so this approach was adopted in the current analyses (30). As per the recent study by Kim et al. (21), we chose to reduce burden to participants by omitting the filler questions and utilised the six-item version of the LOT-R, which has been found to have convergent and discriminant validity, and good test-retest reliability (29). For the purpose of this study, LOT-R scores (from 6 – 30) were divided into quartiles based on data distribution (21). Quartile 1 (Q1) included those with LOT-R scores ≤ 20; Q2 those with scores 21 – 24; Q3 scores 25 - 28, and Q4 scores from 29 – 30, with higher scores representing greater optimism.
Assessment of mortality
Mortality was an adjudicated endpoint for the primary analysis in the principal ASPREE study (23). ALSOP has no defined endpoint; mortality data for the purpose of our analysis was sourced from ASPREE. The trial involved contact with study participants – by telephone (quarterly) and face-to-face (annually) – and clinical records were routinely examined. Therefore, death was generally identified through the course of the study. When participants were not able to be contacted, health records were reviewed; alternatively, the next of kin or other close contact notified the trial centre of the death. Each death was confirmed by two independent sources (family, primary care physician, or public death notice). At the end of the trial, the names of all participants who had withdrawn or were lost to follow-up were linked to the National Death Index.
Potential confounders
Confounders were selected a priori based on the available evidence of the variables commonly associated with both the exposure (optimism) and outcome (all-cause mortality), and all putative confounders were assessed prior or at the same time as the exposure.
Age was classified into four approximately equal categories (70 – 71.99 years, 72-73.99 years, 74 – 76.99 years, 77 years and older), to determine the potential modifying effect of age and because when a continuous measure was used in the regression models, the proportional hazards assumption was not met. Binary variables were created for sex (women, men), living situation (living alone, living with others), education level (≤ 12 years, > 12 years), smoking status (never having smoked, being a current or former smoker), daily alcohol use alcohol use (low risk/never drank alcohol was defined as ‘none or no more than four standard drinks in any one day, and no more than ten standard drinks in a week, compared to over this limit: not adherent) (31), and physical activity (rarely/never or light activity in a typical week as ‘not/less physically active’, moderate or vigorous activity in a typical week as ‘physically active’).
Statistical analysis
Summary statistics were calculated, and the association between the sociodemographic variables and health-related behaviours with mortality was examined using χ2 tests (Table 1). The relationship between optimism (exposure, LOT-R scores ranging between 6 and 30 were considered as baseline level of optimism) and all-cause mortality (outcome) was assessed using the Cox Proportional Hazards models, and hazard ratios and 95% confidence intervals are reported (Table 2). We note the possibility that several of our potential confounding variables may be ‘overlapping’ given that they tap into similar constructs and they are assessed at a similar time (32). Therefore, we tested whether the variables were intercorrelated, by computing Spearman rank correlation coefficients (Table S1, Supplemental Digital Content). Considering low correlation coefficients, all a priori selected putative confounders were retained in the model.
Table 1:
Baseline characteristics of 11,701 ALSOP study participants
| Total: n = 11,701 | Alive: n = 11,232 | Dead: n = 469 | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| LOT-R Optimism score: | |||
| Q1 (≤20) | 3197 (27.32) | 3053 (27.18) | 144 (30.70) |
| Q2 (21 – 24) | 3239 (27.68) | 3107 (27.66) | 132 (28.14) |
| Q3 (25 – 28) | 3050 (26.07) | 2921 (26.01) | 129 (27.51) |
| Q4 (29 – 30) | 2215 (18.93) | 2151 (19.15) | 64 (13.65) |
| Age (years): | |||
| 70 – 71.99 | 3475 (29.70) | 3416 (30.41) | 59 (12.58) |
| 72 – 73.99 | 2504 (21.40) | 2427 (21.61) | 77 (16.42) |
| 74 – 76.99 | 2545 (21.75) | 2461 (21.91) | 84 (17.91) |
| ≥ 77 | 3177 (27.15) | 2928 (26.07) | 249 (53.09) |
| Sex: | |||
| Males | 5462 (46.68) | 5175 (46.07) | 287 (61.19) |
| Females | 6239 (53.32) | 6057 (53.93) | 182 (38.81) |
| Living situation: | |||
| Lives alone | 3573 (30.54) | 3397 (30.24) | 176 (37.53) |
| Lives with others | 8128 (69.46) | 7835 (69.76) | 293 (62.47) |
| Education Level: | |||
| ≤ 12 years | 6781 (57.95) | 6494 (57.82) | 287 (61.19) |
| > 12 years | 4920 (42.05) | 4738 (42.18) | 182 (38.81) |
| Smoking status: | |||
| Never smoked | 6494 (55.50) | 6275 (55.87) | 219 (46.70) |
| Current smoker | 327 (2.79) | 300 (2.67) | 27 (5.76) |
| Former smoker | 4880 (41.71) | 4657 (41.46) | 223 (47.55) |
| Alcohol use 1 : | |||
| Low risk/never drank alcohol | 8750 (74.78) | 8411 (74.88) | 339 (72.28) |
| Not adherent (to NHMRC guidelines) | 2951 (25.22) | 2821 (25.12) | 130 (27.72) |
| Physical activity: | |||
| Not/less physically active | 3927 (33.56) | 3719 (33.11) | 208 (44.35) |
| Physically active | 7774 (66.44) | 7513 (66.89) | 261 (55.65) |
NHMRC guidelines for safe alcohol consumption in (Australian) adults: consuming ≤ 4 standard drinks on any one day, and no more than 10 standard drinks in a week. Low risk is equivalent to adhering to NHMRC guidelines (31).
Table 2:
The association between optimism and all-cause mortality in 11,701 ALSOP participants: the results of the Cox proportional hazards regression
| Q2 v Q1 HR (95% CI) P |
Q3 v Q1 HR (95% CI) P |
Q4 v Q1 HR (95% CI) p |
|
|---|---|---|---|
| Model one (crude): | |||
| 0.90 (0.71 – 1.14) 0.38 |
0.94 (0.74 – 1.19) 0.59 |
0.63 (0.47 – 0.85) 0.002 |
|
| Model two (+ age, sex): | |||
| 0.90 (0.71 – 1.14) 0.38 |
0.98 (0.77 – 1.24) 0.85 |
0.72 (0.54 – 0.97) 0.031 |
|
| Model three (+ living situation, education level): | |||
| 0.92 (0.73 – 1.16) 0.48 |
1.00 (0.79 – 1.27) 0.98 |
0.74 (0.55 – 1.00) 0.050 |
|
| Model four (+ smoking status, alcohol use, and physical activity): | |||
| 0.96 (0.76 – 1.22) 0.73 |
1.05 (0.83 – 1.34) 0.67 |
0.78 (0.58 – 1.06) 0.11 |
|
Cox Proportional Hazards regression used.
LOT-R scores: Q1: ≤ 20; Q2: 21 – 24; Q3: 25 – 28; Q4: 29 - 30
Calibration (goodness of fit):
Model one: χ2 = 3.84, p = 0.15
Model two: χ2 = 17.63, p = 0.040
Model three: χ2 = 10.31, p = 0.33
Model four: χ2 = 22.04, p = 0.009
Model one was unadjusted, model two adjusted for age and sex, model three additionally adjusted for living situation and education level, and model four additionally adjusted for smoking status, alcohol intake and physical activity. For each model in the Cox regression, the proportional hazard assumption was tested, and found not to be statistically significant. We tested the goodness of fit of each Cox PH model using the Gronnesby and Borgan test (33)
To examine whether the relationship between optimism and mortality differed among age and sex categories, tests for interaction were performed by entering cross-product terms for each of the covariates and optimism into the Cox regression model. All regression models and summary statistics were performed in STATA version 15.0.
Ethical approval
The project was reviewed and approved by the Monash University Human Research Ethics committee, reference number: 21906. All participants provided informed written consent prior to taking part in the ASPREE and ALSOP studies.
Results
Baseline participant characteristics
A total of 11,866 individuals completed six items of the LOT-R and complete data on the rest of the variables were available for 11,701 of these participants. Compared to participants with complete data, those who had some of the data points missing were more likely to be older, a woman, live with others, have 12 years of formal education or less, to have never smoked, and less likely to be physically active (Table S2, Supplemental Digital Content). At baseline, the average age of ALSOP participants was 75.1 years (SD 4.24), and there was a slightly higher proportion of women (53.3%). During the follow-up period (median 4.7 years), 469 deaths occurred. Compared to the rest of participants, those who died during the follow up were more likely to be in the highest age category, a man, live alone, be either a current or former smoker, drink more than recommended safe levels of alcohol and be less physically active (Table 1).
The majority of participants scored greater than 25 on the LOT-R (Q3 or Q4) and 13.0% of all participants scored the maximum of 30.
Optimism and risk of all-cause mortality
The most optimistic participants (top quartile) had a lower risk of mortality (HR (95%CI) = 0.63 (0.47 – 0.85), p = 0.002) compared to the least optimistic individuals (bottom quartile) (Table 2; Figure 2). After further adjustment for age, sex, sociodemographic variables (living situation and education level), and health-related behaviours, the association between optimism and all-cause mortality was no longer statistically significant.
Figure. 2. Kaplan-Meier survival curve for optimism of participants (n= 11,701) in quartiles.

LOT-R scores: Q1: ≤ 20; Q2: 21 – 24; Q3: 25 – 28; Q4: 29 - 30
We explored whether age or sex modify the association between optimism and all-cause mortality. Interaction analyses were conducted, and found to be significant for age (p < 0.001) but not sex (p = 0.61). Subsequently, analyses were therefore stratified by age (Table 3). Among the oldest participants (aged 77 years or older), in the fully adjusted model, the most optimistic participants (top quartile) had a lower risk of mortality compared to the least optimistic individuals (bottom quartile) (HR (95%CI) = 0.61 (0.39 – 0.96)).
Table 3:
The relationship between optimism and all-cause mortality across age categories in 11,701 ALSOP Participants: the results of the Cox proportional hazards regression
| Deaths/n | Q2 v Q1 HR (95% CI) p |
Q3 v Q1 HR (95% CI) p |
Q4 v Q1 HR (95% CI) p |
|
|---|---|---|---|---|
| Model one (crude): | ||||
| 70 – 71.99 years | 59/3475 | 0.52 (0.24 – 1.10) 0.087 |
0.58 (0.28 – 1.21) 0.15 |
1.14 (0.60 – 2.16) 0.68 |
| 72 – 73.99 years | 77/2504 | 1.20 (0.66 – 2.21) 0.55 |
1.31 (0.72 – 2.77) 0.38 |
0.73 (0.34 – 1.57) 0.42 |
| 74 – 76.99 years | 84/2545 | 0.83 (0.47 – 1.47) 0.52 |
1.13 (0.66 – 1.95) 0.65 |
0.58 (0.28 – 1.21) 0.14 |
| ≥ 77 years | 249/3177 | 0.93 (0.68 – 1.27) 0.63 |
0.89 (0.64 – 1.23) 0.48 |
0.54 (0.34 – 0.84) 0.006 |
| Model two (+ sex): | ||||
| 70 – 71.99 years | 59/3475 | 0.53 (0.25 – 1.14) 0.10 |
0.60 (0.29 – 1.25) 0.17 |
1.26 (0.67 – 2.39) 0.47 |
| 72 – 73.99 years | 77/2504 | 1.20 (0.65 – 2.20) 0.56 |
1.30 (0.71 – 2.36) 0.39 |
0.79 (0.37 – 1.69) 0.54 |
| 74 – 76.99 years | 84/2545 | 0.83 (0.47 – 1.47) 0.55 |
1.16 (0.67 – 1.99) 0.60 |
0.61 (0.29 – 1.28) 0.19 |
| ≥ 77 years | 249/3177 | 0.94 (0.69 – 1.28) 0.69 |
0.92 (0.67 – 1.28) 0.64 |
0.57 (0.37 – 0.89) 0.014 |
| Model three (+ living situation, education level): | ||||
| 70 – 71.99 years | 59/3475 | 0.56 (0.26 – 1.20) 0.14 |
0.66 (0.31 – 1.39) 0.28 |
1.42 (0.74 – 2.73) 0.29 |
| 72 – 73.99 years | 77/2504 | 1.25 (0.68 – 2.31) 0.47 |
1.38 (0.76 – 2.53) 0.29 |
0.85 (0.39 – 1.84) 0.68 |
| 74 – 76.99 years | 84/2545 | 0.81 (0.46 – 1.45) 0.48 |
1.11 (0.64 – 1.93) 0.71 |
0.58 (0.27 – 1.21) 0.15 |
| ≥ 77 years | 249/3177 | 0.96 (0.70 – 1.32) 0.82 |
0.95 (0.68 – 1.32) 0.75 |
0.59 (0.37 – 0.92) 0.019 |
| Model four (+ smoking status, alcohol use, physical activity): | ||||
| 70 – 71.99 years | 59/3475 | 0.57 (0.26 – 1.21) 0.14 |
0.71 (0.33 – 1.50) 0.37 |
1.50 (0.78 – 2.89) 0.22 |
| 72 – 73.99 years | 77/2504 | 1.27 (0.69 – 2.33) 0.45 |
1.40 (0.76 – 2.56) 0.28 |
0.86 (0.40 – 1.88) 0.71 |
| 74 – 76.99 years | 84/2545 | 0.84 (0.47 – 1.49) 0.55 |
1.21 (0.69 – 2.10) 0.51 |
0.63 (0.30 – 1.33) 0.23 |
| ≥ 77 years | 249/3177 | 1.01 (0.74 – 1.38) 0.96 |
0.99 (0.71 – 1.38) 0.96 |
0.61 (0.39 – 0.96) 0.032 |
Statistical test: Cox Proportional Hazards regression, stratified by age category
LOT-R scores: Q1: ≤ 20; Q2: 21 – 24; Q3: 25 – 28; Q4: 29 - 30
Discussion
This study comprised of 11,701 Australian older adults recruited through general medical practices, and it is the largest study of both men and women to determine whether optimism is a significant predictor of all-cause mortality in adults 70 years and older. The results of the study indicate that, over the 4.7 years median follow-up, individuals in the highest category of optimism had a lower risk of all-cause mortality compared to those in the lowest category of optimism, after adjustment for age and sex. There was no association between optimism and mortality when living situation, education, and health-related behaviours were additionally adjusted for. However, for participants aged 77 years or older the most optimistic participants had a lower risk of mortality compared to least optimistic participants in the fully adjusted model.
Two prior studies similarly reported that there was no significant relationship between optimism and all-cause mortality in older adults after adjustment for covariates. Anthony et al. (35) included 876 participants of comparable mean age to our study (74.1 years and 75.1 years respectively), and after a mean follow-up period of 8.1 years, they observed that with adjustment for age, optimism did not significantly predict all-cause mortality. Kubzansky et al. (16) also reported that with adjustment for multiple covariates, there was no significant association between optimistic explanatory style and all-cause mortality in a sample of 1306 males of mean age 60.8 years. Our study and those of Anthony et al (35) and Kubzansky et al. (16) were similar in that participants had access to publicly funded health-care and were free of major chronic disease at baseline.
The results of our study are in contrast to findings of Danish study on nonagenerians (34), who observed a negative association between optimism and all-cause mortality in women but not in men. Similarly, a study on Dutch men and women aged 65 to 85 years (36), also observed a negative association between optimism and all-cause mortality. However, the latter two studies recruited older men and women irrespective or disease or disability status, while we add to the current evidence by reporting the association between optimism and all-cause mortality exclusively in older adults that reached older age in good health. We also add to the findings of previous studies by additionally exploring the groups of older adults that could potentially benefit the most from interventions to increase optimism. We identified that among oldest old in our cohort (77 years and over), the most optimistic individuals, compared to less optimistic ones, had a lower risk of all-cause mortality.
Recent research into the developmental trajectory of optimism across the lifespan, has had mixed results. With a combined sample size of 74,866, a recent analysis of three panel studies reported that for samples from the USA and The Netherlands, optimism increased during younger adulthood, then plateaued during the midlife before declining in older age (37). The German sample, however, displayed inconsistent trends in terms of patterns across age-groups and changes in optimism across the lifespan, with individuals increasing in optimism as they aged (37), and the authors proposed that this result possibly reflected cohort effects or factors specific to the sample.
Sociodemographics and health-related behaviours explained the association between optimism and mortality, though not for the oldest participants. According to the results of the English Longitudinal Study of Ageing and US Health and Retirement Study, higher socioeconomic status (SES) is associated with longer life free from disability (38). Among older adults, lower SES is associated in engaging in less healthy behaviours (39); and individuals of lower SES are less optimistic compared to their more affluent counterparts (40). Optimism is associated with more positive health behaviours, which in turn promote reduced mortality risk (41). Optimists’ tendency to use problem-focused coping, and self-belief that their goals are attainable, also means that they are more likely to change health-behaviour (42, 43). Optimists are more likely to engage in regular physical activity (44), eat a nutrient rich diet (45) and abstain from smoking (46). Optimism is also positively related to quality of sleep (30).
Emerging research (47) suggests that positive psychological interventions which increase wellbeing may lead to improved engagement in health-related behaviours in cardiac patients (such as doing moderate to vigorous physical activity). However, it remains unclear whether increasing optimism specifically (with a psychological intervention) may result in increased health-promoting behaviours in non-patient populations, such as by encouraging less smoking, moderate consumption of alcohol, improved diet and increases in physical activity. To determine whether there is a causal effect of optimism on mortality, a randomized trial could be done to assess whether a psychological intervention that is effective in promoting higher levels of optimism also confers a lower risk of all-cause mortality.
Inherent in the study were some limitations. Volunteering for a long-term trial (such as the ASPREE/ALSOP study) is likely to attract people with particular characteristics, including optimism (as evidenced by the skew in optimism scores for our cohort). Another limitation was that data were not available on diet quality, which is a factor that has been associated with optimism (45), and mortality (48). Although the sample was considered to be representative of Australian adults who had reached the age of 70 in relatively good health, the ALSOP cohort had very few non-white participants, and all were community dwelling older adults free of disabling chronic disease at baseline. The fact that the participants were in reasonably good health at baseline may also have contributed to the relatively lower percentage of deaths (4%), though this may also have been due to the relatively short length of follow-up time (median 4.7 years). This low rate of mortality may have affected our statistical results by reducing the magnitude of the effect size. We also note that the lack of clinically significant variation in the LOT-R scores (primary exposure) may have contributed to our null finding.
Our sample consists exclusively of adults aged 70 years and over who were free of major disease or disability, which allowed us to explore the question of whether optimism is associated with reduced risk of mortality for older adults in relatively good health. However, we acknowledge the potential selection bias, in that individuals with the lowest levels of optimism may have died before 70 years, and thus were not represented in the current study. This healthy survivor effect may have contributed to the null finding in the overall cohort of older adults aged 70 years and over. Furthermore, reverse causality may also be a factor to consider – that people with better health are more optimistic; this appears plausible given the ceiling effect of the LOT-R scores in our cohort. It has also been argued that the beneficial effects of optimism have a cumulative effect across the lifespan (49); however, our model is limited to only capturing approximately 4 years of each participant’s life.
Promoting optimism may improve health-related behaviours such as engaging in physical activity and not smoking (44, 46). Therefore, it is possible that health behaviours may mediate, rather than confound, the relationship between optimism and all-cause mortality. By treating health-related behaviours as confounders, we may have overadjusted our analyses and removed some of the effect of optimism on all-cause mortality that goes via health-related behaviour pathways. However, this approach enabled us to explore whether the relationship between optimism and all-cause mortality was independent of differences in health-related behaviours.
Despite the limitations, this is among the largest studies of both men and women to determine whether optimism is a significant predictor of all-cause mortality in adults 70 years and older living independently and free of cardiovascular disease, dementia or major disability. Our study also adds evidence for a modifying effect of age on the association between optimism and mortality in older adults.The sample is considered to adequately represent those older individuals in Australia who have reached the age of 70 years in relatively good health (24). We used the LOT-R to measure optimism, which is well researched and validated.
Conclusions
Among 11,701 adults aged 70 years and older, we observed no independent relationship between optimism and all-cause mortality in the total sample, although age at study entry appeared to moderate the effect of optimism on mortality with the oldest adults (77 years and over) living longer when more optimistic. Future research is warranted to clarify correlates of optimism, and explore the trajectory of optimism throughout the latter years or life – as it appears from our findings that in oldest old, optimism may contribute to lowered risk of mortality.
Supplementary Material
Conflicts of interest and sources of funding:
Supported by grants (U01AG029824 and U19AG062682) from the National Institute on Aging and the National Cancer Institute at the National Institutes of Health, by grants (334047 and 1127060) from the National Health and Medical Research Council of Australia, and by Monash University and the Victorian Cancer Agency. No conflicts of interest declared; RFP is supported by an Australian Heart Foundation post-doctoral fellowship (101927), JR is supported by NHMRC Dementia Research Leader Fellowship (APP1135727)
Abbreviations
- ASPREE
Aspirin Reducing Events in the Elderly
- ALSOP
ASPREE Longitudinal Study of Older Persons
- USA
United States of America
- LOT-R
Life Orientation Test (Revised)
- SES
Socioeconomic status
References
- 1.United Nations, Department of Economic and Social Affairs, Population Division (2019). World Population Ageing 2019: Highlights (ST/ESA/SER.A/430).
- 2.Jaul E, Barron J. Age-related diseases and clinical and public health implications for the 85 years old and over population. Front Pub Health, 2017; 5:335. doi: 10.3389/fpubh.2017.00335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014; 384 (9937): 45–52. 10.1016/S0140-6736(14)60648-6 [DOI] [PubMed] [Google Scholar]
- 4.Steptoe A, Deaton A, Stone AA. Psychological wellbeing, health and ageing. Lancet 2015; 385 (9968): 640–648. doi: 10.1016/50140-6736(13)61489-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tamosiunas A, Sapranaviciute-Zabazlajeva L, Luksiene D, Virviciute D, Peasey A. Psychological well-being and mortality: longitudinal findings from Lithuanian middle-aged and older adults study. Soc Psychiatry Psychiatr Epidemiol 2019; 54 (7): 803 – 811. doi: 10.1007/s00127-019-01657-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ranzijn R. The potential of older adults to enhance community quality of life: Links between positive psychology and productive aging. Ageing Int 2002; 27(2): 30–55. 10.1007/s12126-002-1001-5 [DOI] [Google Scholar]
- 7.Chang R. Optimism and pessimism as personality variables linked to adjustment. In: Boyle GJ, Matthews G, Saklofske DH, editors. The SAGE Handbook of Personality Theory and Assessment: Volume 1 - Personality Theories and Models. California: SAGE Publications; 2008. p 470–485. 10.4135/9781849200462.n22 [DOI] [Google Scholar]
- 8.Maruta T, Colligan RC, Malinchoc M, Offord KP. (2000). Optimists vs Pessimists: Survival Rate Among Medical Patients Over a 30-Year Period. Mayo Clin Proc 2000; 75(2): 140–143. 10.4065/75.2.140 [DOI] [PubMed] [Google Scholar]
- 9.Scheier ME, Carver CS. Dispositional Optimism and Physical Well-Being: The Influence of Generalized Outcome Expectancies on Health. J Pers 1987; 55(2): 169–210. 10.1111/j.1467-6494.1987.tb00434.x [DOI] [PubMed] [Google Scholar]
- 10.Scheier M, Carver F. Effects of optimism on psychological and physical well-being: Theoretical overview and empirical update. Cognit Ther Res 1992; 16(2): 201–228. 10.1007/BF01173489 [DOI] [Google Scholar]
- 11.Scheier MF, Carver CS. Optimism, Coping, and Health: Assessment and Implications of Generalized Outcome Expectancies. Health Psychol 1985; 4(3): 219–247. 10.1037/0278-6133.4.3.219 [DOI] [PubMed] [Google Scholar]
- 12.Kluemper DH, Little LM, DeGroot T, Wright T A, Quick JC. State or trait: effects of state optimism on job-related outcomes. J Organ Behav 2009; 30(2): 209–231. 10.1002/job.591 [DOI] [Google Scholar]
- 13.Plomin R, Scheier MF, Bergeman C, Pedersen N, Nesselroade J, Mcclearn G. Optimism, pessimism and mental health: A twin/adoption analysis. Pers Individ Dif 1992; 13(8): 921–930 10.1016/0191-8869(92)90009-E [DOI] [Google Scholar]
- 14.Power RA, Pluess M. (2015). Heritability estimates of the Big Five personality traits based on common genetic variants. Transl Psychiatry 2015; 5(7): e604. 10.1038/tp.2015.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malouff JM, Schutte NS. (2017). Can psychological interventions increase optimism? A meta-analysis. J Posit Psychol 2017; 12(6): 594 – 604. 10.1080/17439760.2016.1221122 [DOI] [Google Scholar]
- 16.Kubzansky LD, Sparrow D, Vokonas P, Kawachi I. Is the Glass Half Empty or Half Full? A Prospective Study of Optimism and Coronary Heart Disease in the Normative Aging Study. Psychosom Med 2001; 63(6): 910–916. 10.1097/00006842-200111000-00009 [DOI] [PubMed] [Google Scholar]
- 17.de Rooij BH, Thong MSY, van Roij J, Bonhof CS, Husson O, Ezendam NPM. Optimistic, realistic, and pessimistic illness perceptions; quality of life; and survival among 2457 cancer survivors: the population-based PROFILES registry. Cancer 2018; 124 (17): 3609–3617. 10.1002/cncr.31634 [DOI] [PubMed] [Google Scholar]
- 18.Roy B, Diez-Roux AV, Seeman T, Ranjit N, Shea S, Cushman M (2010) Association of optimism and pessimism with inflammation and hemostasis in the Multi-Ethnic Study of Atherosclerosis (MESA). Psychosom Med 72(2):134–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bargiel-Matusiewicz K, Krzyszkowska A Dispositional optimism and coping with pain. Eur J Med Res 2009; 14: 271–274. doi: 10.1186/2047-783X-14-S4-271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James P, Kim ES, Kubzansky LD, Zevon ES, Trudel-Fitzgerald C, Grodstein F. Optimism and Healthy Aging in Women. Am J Prev Med 2019; 56(1): 116–124. 10.1016/j.amepre.2018.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim ES, James P, Zevon ES, Trudel-Fitzgerald C, Kubzansky LD, Grodstein F. Optimism and Healthy Aging in Women and Men. Am J Epidemiol 2019; 188(6): 1084–1091. 10.1093/aje/kwz056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee LO, James P, Zevon ES, Kim ES, Trudel-Fitzgerald C, Spriro A, Grodstein F, Kubzansky LD. Optimism is associated with exceptional longevity in two epidemiologic cohorts of men and women. Proc Natl Acad Sci USA 2019; 116 (37): 18357 – 18362. 10.1073/pnas.1900712116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mcneil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, Kirpach B, Shah RC, Ives DG, Storey E, Ryan J, Tonkin AM, Newman AB, Williamson JD, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Orchard SG, Trevaks RE, Beilin LJ, Donnan GA, Gibbs P, Johnston CI, Radziszewska B, Grimm R, Murray AM. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med 2018; 379 (16): 1519–1528. 10.1056/NEJMoa1803955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McNeil JJ, Woods RL, Ward SA, Britt CJ, Lockery JE, Beilin LJ, Owen AJ. Cohort Profile: The ASPREE Longitudinal Study of Older Persons (ALSOP). Int J Epidemiol 2019; 48(4): 1048–1049h. 10.1093/ije/dyy279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mcneil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, Storey E, Shah RC, Lockery JE, Tonkin AM, Newman AB, Williamson JD, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Orchard SG, Trevaks RE, Beilin LJ. Effect of Aspirin on Disability-free Survival in the Healthy Elderly. N Engl J Med 2018; 379(16): 1499 – 1508. 10.1056/NEJMoa1800722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, Reid CM, Lockery JE, Kirpach B, Storey E, Shah RC, Williamson JD, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Orchard SG, Trevaks RE, Beilin LJ, Johnston CI, Ryan J, Radziszewska B, Jelinek M, Malik M, Eaton CB, Brauer D, Cloud G, Wood EM, Mahady SE, Satterfield S, Grimm R, Murray AM. Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly. N Engl J Med 2018; 379(16): 1509–1518. 10.1056/NEJMoa1805819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grimm RH, McNeil JJ, Applegate W, Beilin L, Espinoza S, Johnston CI, Kirpach B, Margolis K, Murray A, Nelson MR, Reid CM, Shah R, Storey E, Tonkin AM, Wilson P, Wolfe R, Woods RL, Abhayaratna W, Ames D, Cobiac L, Donnan G, Gibbs P, Head R, Krum H, Ives D, Tonkin AM, Jelnik M, Malik M, Williamson J, Eaton C, Weissfeld J, Macrae F, Rodriguez LM, Newman A, Demons J, Workman B, Wood E, Satterfield S, Lockery JE, Shah RC, Radziszewska B, Thomas A, Gill G, Jackson C, Kidd M, Russell G. Study design of ASPirin in Reducing Events in the Elderly (ASPREE): A randomized, controlled trial. Contemp Clin Trials 2013; 36(2): 555–564. Grimm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McNeil JJ, Woods RL, Nelson MR, Murray AM, Reid CM, Kirpach B, Storey E, Shah RC, Wolfe RS, Tonkin AM, Newman AB, Williamson JD, Lockery JE, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Trevaks RE, Orchard SG, Beilin LJ, Donnan GA, Gibbs P, Johnston CI, Grimm RH. Baseline Characteristics of Participants in the ASPREE (ASPirin in Reducing Events in the Elderly) Study. J Gerontol A Biol Sci Med Sci 2017; 72(11): 1586 – 1593. doi: 10.1093/Gerona/glw342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scheier MF, Carver CS, Bridges MW. Distinguishing Optimism From Neuroticism (and Trait Anxiety, Self-Mastery, and Self-Esteem): A Reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994; 67(6): 1063–1078. 10.1037/0022-3514.67.6.1063 [DOI] [PubMed] [Google Scholar]
- 30.Hernandez R, Bassett SM, Boughton SW, Schuette SA, Shiu EW, Moskowitz JT. Psychological Well-Being and Physical Health: Associations, Mechanisms, and Future Directions. Emot Rev 2018; 10(1): 18–29. 10.1177/1754073917697824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Health and Medical Research Council (NHMRC) (2020). Australian guidelines to reduce health risks from drinking alcohol. Retrieved from https://nhmrc.gov.au/health-advice/alcohol
- 32.Kraemer HC. Current concepts of risk in psychiatric disorders. Curr Opin Psychiatry 2003; 16(4): 421–430. 10.1097/01.yco.0000079210.36371.52 [DOI] [Google Scholar]
- 33.Demler OV, Paynter NP, Cook NR. Tests of calibration and goodness-of-fit in the survival setting. Stat Med 2015; 34(10): 1659–1680. 10.1002/sim.6428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Engberg H, Jeune B, Anderson-Ranberg K, Martinussen T, Vaupel J, Christensen W. Optimism and survival: does an optimistic outlook predict better survival at advanced ages? A twelve-year follow-up of Danish nonagenarians. Aging Clin Exp Res 2013; 25: 517–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anthony EG, Kritz-Silverstein D, Barrett-Connor E. Optimism and Mortality in Older Men and Women: The Rancho Bernardo Study. J Aging Res 2016; 2016: 5185104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giltay EJ, Geleijinse JM, Zitman FG. Dispositional optimism and all-cause and cardiovascular mortality in a prospective cohort of elderly Dutch men and women. ACC Curr J Rev 2005; 14: 17. [DOI] [PubMed] [Google Scholar]
- 37.Chopik WJ, Oh J, Kim ES, Schwaba T, Krämer MD, Richter D, Smith J. Changes in optimism and pessimism in response to life events: Evidence from three large panel studies. J Res Pers 2020; 88. 10.1016/j.jrp.2020.103985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zaninotto P, Batty GD, Stenholm S, Kawachi I, Hyde M, Goldberg M, Westerlund H, Vahtera J, Head J. Socioeconomic inequalities in disability-free life expectancy in older people from England and the United States: A cross-national population-based study. J Gerontol A Biol Sci Med Sci 2020; 75 (5): 906 – 913. doi: 10.1093/Gerona/glz266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shankar A, McMunn A, Steptoe A. Health-related behaviors in older adults: Relationships with socioeconomic status. Am J Prev Med 2010; 38 (1): 39 – 46. 10.1016/j.amepre.2009.08.026 [DOI] [PubMed] [Google Scholar]
- 40.Robb KA, Simon AE, Wardle J. Socioeconomic disparities in optimism and pessimism. Int J Behav Med 2009; 16: 331. 10.1007/s12529-008-9018-0 [DOI] [PubMed] [Google Scholar]
- 41.Salovey P, Rothman AJ, Detweiler JB, Steward WT. Emotional States and Physical Health. Am Psychol 2000; 55(1): 110–121. 10.1037/0003-066X.55.1.11 [DOI] [PubMed] [Google Scholar]
- 42.Rasmussen HN, Wrosch C, Scheier MF, Carver CS. Self-Regulation Processes and Health: The Importance of Optimism and Goal Adjustment. J Pers 2006; 74(6): 1721–1748. 10.1111/j.1467-6494.2006.00426.x [DOI] [PubMed] [Google Scholar]
- 43.Nes LS, Segerstrom SC. Dispositional optimism and coping: A meta-analytic review. Pers Soc Psychol Rev 2006; 10(3): 235–251. 10.1207/s15327957pspr1003_3 [DOI] [PubMed] [Google Scholar]
- 44.Progovac AM, Donohue JM, Matthews KA, Chang CCH, Habermann EB, Kuller LH, Saquib J, Lamonte MJ, Salmoirago-Blotcher E, Zaslavsky O, Tindle HA. Optimism predicts sustained vigorous physical activity in postmenopausal women. Prev Med Rep 2017; 8: 286–293. 10.1016/j.pmedr.2017.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hingle MD, Wertheim BC, Tindle HA, Tinker L, Seguin RA, Rosal MC, Thomson CA. Optimism and diet quality in the Women's Health Initiative. J Acad Nutr Diet 2014; 114(7): 1036–1045. 10.1016/j.jand.2013.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: Associations with healthy ageing. Br J Health Psychol 2006; 11(1): 71–84. 10.1348/135910705X42850 [DOI] [PubMed] [Google Scholar]
- 47.Celano CM, Albanese AM, Millstein RA, Mastromauro CA, Chung WJ, Campbell KA, Legler SR, Park ER, Healy BC, Collins LM, Lanuzzi JL, Huffman JC. Optimizing a Positive Psychology Intervention to Promote Health Behaviors after an Acute Coronary Syndrome: The Positive Emotions after Acute Coronary Events III (PEACE-III) Randomized Factorial Trial. Psychosom Med 2018; 80(6): 526–534. 10.1097/PSY.0000000000000584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, Willett WC, Rimm EB, Hu FB. Association of Changes in Diet Quality with Total and Cause-Specific Mortality. N Engl J Med 2017; 377(2): 143–153. 10.1056/NEJMoa1613502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chopik WJ, Kim ES, Smith J. Changes in Optimism Are Associated With Changes in Health Over Time Among Older Adults. Soc Psychol Personal Sci 2015; 6(7): 814–822. 10.1177/1948550615590199 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


