Abstract
Objective:
To identify subgroups of urban youth based on their self- and teacher-reported mental health symptoms, and to explore characteristics of these subgroups.
Methods:
Cross-sectional data from 426 eighth grade students (Mage = 13.22 years; 70.1% Black/African American; 58.7% female) across 20 Baltimore City public schools were analyzed using latent profile analysis and latent regressions. Variables for latent profile analysis included self-reported symptoms (i.e., anxiety, depression, trauma, interpersonal issues, social problems, and behavioral dysfunction) and teacher-reported symptoms (i.e., externalizing, internalizing, and problems in social and emotional competence). Regressions used profile membership to predict trauma exposure, coping mechanisms, and substance use.
Results:
A 3-profile solution was found from the latent profile analysis. The profile with high student- and teacher-reported symptoms had more trauma exposures, greater use of maladaptive coping mechanisms, and higher substance use.
Conclusions:
The current study may help in the identification of urban youth who are at risk of developing multiple co-occurring psychological disorders to target for prevention efforts.
Keywords: comorbidity, urban youth, coping, trauma exposure, substance use
While comorbidity of mental health disorders in adolescence is common and has been linked with negative outcomes in adulthood, more research is needed to adequately target prevention efforts toward youth who are at greatest risk for developing multiple mental health disorders. Low-income urban adolescents are at particular risk of developing multiple mental health disorders as they are more likely to experience various stressors from their environment, such as neighborhood violence, instability in family and housing, and interpersonal violence (Farahmand et al., 2012; Woolf et al., 2015). Thus, more research is needed on comorbid mental health disorders with vulnerable urban youth populations.
Comorbidity of Psychological Symptoms in Adolescents
Comorbidity of mental health disorders is a fairly common phenomenon, with prior research reporting that up to 60% of youth with a mental health disorder having a co-occurring second disorder (Essau & de la Torre-Luque, 2019; Teplin et al., 2003). Many of the studies exploring the co-occurrence of multiple mental health disorders in youth have placed particular focus on the overlap between depression and anxiety (Ferdinand et al., 2005; Peiper et al., 2015; van Lang et al., 2006; Wadsworth et al., 2001). However, a few studies with youth samples have included a broader scope of psychological symptoms when exploring comorbidity, such as internalizing, externalizing, aggressive behavior, and substance use (Gomez & Vance, 2014; Hogue & Dauber, 2013; Liu et al., 2017). In prior research on comorbidity in youth, very few studies included trauma or PTSD symptoms (Hogue & Dauber, 2013), which are often experienced by urban youth in communities with high rates of violence (Horowitz et al., 2005). To address this gap, the current study includes trauma symptoms, as well as symptoms of depression and anxiety. Urban youth samples in studies of comorbidity have primarily been enrolled from clinical or juvenile justice settings. The current study examines comorbid psychological symptoms in a sample of urban youth recruited from public schools, providing clearer insight into symptoms experienced by a general urban youth population. Finally, few studies on comorbidity in youth have included data on mental health provided by multiple raters (Fergusson et al., 1994; Hogue & Dauber, 2013; Neuman et al., 2001). The current study uses both self-reported and teacher-reported data on youth symptoms to create subgroups of youth with distinct symptom profiles.
Studies utilizing person-centered analyses, such as latent class analysis or latent profile analysis, have grown in popularity in mental and behavioral health research. The goal of this methodology is to describe the underlying heterogeneity in a population and identify subgroups of people who are similar to each other based on their answers indicated on measures (Nylund et al., 2007). A study of over 10,000 adolescents who were administered the Composite International Diagnostic Instrument (CIDI) identified three classes of comorbid symptoms: 1) comorbid emotional disorders, 2) comorbid behavioral disorders, and 3) normative level of symptoms (Essau & de la Torre-Luque, 2019). However, in a study of approximately 15,000 middle and high schools students who were administered the K6 scale, four classes of comorbid symptoms were identified, including 1) comorbid moderate severity symptoms, 2) comorbid high severity symptoms, 3) moderate anxiety symptoms, and 4) high severity depressive symptoms (Peiper et al., 2015). In a study that focused on comorbidity of depressive and anxiety symptoms in 2,029 adolescents, five classes were identified using LCA, which included 1) high anxiety and mild depression, 2) high anxiety and severe depression, 3) moderate anxiety and depression, 4) moderate anxiety and eating and sleeping problems, and 5) low symptoms (van Lang et al., 2006). Finally, a small study of community-referred adolescents who were administered the Mini International Neuropsychiatric Interview used LCA to identify five classes that were differentiated by internalizing and externalizing symptoms, including 1) basic externalizers, 2) comorbid externalizers, 3) adolescent distress, 4) severely distressed, and 5) parental concern (Hogue & Dauber, 2013). In summary, studies using person-centered methodology in modeling comorbid symptoms among youth typically find between three to five subgroups, depending on a variety of factors, including symptoms measured, sample size, and population differences (Essau & de la Torre-Luque, 2019; Ferdinand et al., 2005; Hogue & Dauber, 2013; Peiper et al., 2015; van Lang et al., 2006; Wadsworth et al., 2001).
Correlates of Comorbid Psychological Symptoms in Adolescents
Exploring correlates and characteristics associated with comorbidity of mental health issues in youth can inform intervention approaches. Trauma exposure, coping styles, and substance use are factors that have been associated with comorbidity of mental health issues in youth, although few studies have examined these associations with psychological comorbidity in urban youth. Each of these factors merits further investigation among urban youth.
Exposure to adverse childhood events (ACEs) and other traumas has been linked with many psychological issues, such as anxiety, depression, and PTSD (Briere et al., 2010). One study examined the association of stressful life events, racial discrimination, and exposure to violence with comorbidity of externalizing and internalizing symptoms in youth (Liu et al., 2017). Comorbidity was associated with more stressful life events and violence exposure (Liu et al., 2017). In a study of youth in need of mental health services, latent classes of psychological symptoms were compared by psychosocial variables, such as having a member of the household who uses substances or participating in illegal activities (Hogue & Dauber, 2013). In this study, students who were classified as experiencing comorbid externalizing symptoms were more likely to have a member of the household who ever used substances than youth in the other classes (Hogue & Dauber, 2013). The current study builds on this field of research by asking about lifetime exposure to adverse childhood experiences, rather than being limited to current or past-year exposure. Moreover, the current study looks at the associations between experiencing multiple traumas and psychological comorbidity.
Impaired capacity to cope effectively with stress, an aspect of self-regulation, has been identified as key to the development of psychological disorders in adolescents (Gunnar & Vasquez, 2006; Kessler et al., 1985; Taylor & Stanton, 2007; Wigman et al., 2014). Using positive or adaptive coping strategies, such as problem solving, is associated with fewer internalizing and externalizing problems, while the opposite has been found for maladaptive coping strategies, such as disengagement (Compas et al., 2001). While little research has focused on coping and comorbid psychological disorders in urban youth, one study of youth with comorbid mental health and substance use disorders found that coping ability was associated with fewer substance use days over six months (Anderson et al., 2006). In a study with urban youth, negative religious coping and avoidant coping were found to be associated with psychological distress, while positive religious coping and active coping were associated with healthy psychological adjustment (Terreri & Glenwick, 2013). The current study addresses the need for further research into coping strategies and co-occurring psychological symptoms in youth.
In addition to adverse childhood experiences and coping, some studies have explored the associations between comorbid disorders and substance use in youth. In the Hogue & Dauber (2013) study described above, youth who were identified as experiencing comorbid externalizing symptoms were more likely to have a parent who reported suspicion that the adolescent used substances compared to the other subgroups. Peiper et al. (2015) explored subgroups of youth based on their reported anxiety and depressive symptoms, which resulted in four subgroups that differed by symptom severity and type. Past-month cigarette use was a significant predictor for membership in any of the four classes, while students who reported binge drinking in the past two weeks were more likely to be in the group that reported high levels of comorbid symptoms (Peiper et al., 2015). The current study addresses a key gap in the literature, which is blunt use by adolescents. Prior studies show that blunt use is more prevalent in youth who live in low-SES settings (Trapl & Gonzalez, 2017); however, few studies of comorbidity ask about this specific route of marijuana and tobacco use. The current study asks about lifetime use of alcohol, tobacco, marijuana, and blunts.
Current Study
The current study addresses several key gaps in the literature on comorbidity and its correlates, including the recruitment of a sample of urban youth from the general population, inclusion of multiple data sources and psychological symptoms, and the measurement of lifetime exposure to key adverse childhood events and illicit substances. The first goal of the current study was to explore whether distinct groups of youth could be identified based on their self-reported and teacher-reported mental health symptoms. Secondly, the current study aimed to examine the characteristics of these subgroups of urban youth, including their trauma exposure, coping strategies, and substance use. To that end, we used latent profile analysis (LPA) to assign a sample of urban middle school students into mutually exclusive profiles based on the pattern of responses from their self-reported and teacher-reported symptoms of depression, anxiety, trauma, internalizing, externalizing, and social functioning. We then used latent regressions to understand how profile membership was associated with trauma exposure, use of maladaptive and adaptive coping strategies, and use of various substances, including tobacco, alcohol, and marijuana. The decision to use a categorical latent modeling approach, as opposed to a dimensional approach, was based on the utility of identifying subgroups for interventionists and practitioners. Based on prior research, we hypothesized that we would identify approximately three to four groups, including one with low symptoms and one with high comorbidity symptoms. We also expected to have one group with high internalizing symptoms (i.e., depression, anxiety, and general internalizing symptoms) and one group with high externalizing symptoms (i.e., social issues and general externalizing symptoms), as was seen in prior work with community-referred adolescents (Hogue & Dauber, 2013). Findings from the current study could inform prevention efforts by providing further characterization of youth based on the symptoms they experience, as well as trauma exposures and coping mechanisms, improving screening for selective prevention programming.
Methods
Participants
This study used baseline data from 426 8th grade students across 20 Baltimore City public schools. Eighth graders were recruited in three different cohorts across three years to participate in a randomized controlled trial assessing a school-based mindfulness program (RAP Club) compared to an active control program focused on general health education. Data for the current study were collected prior to students being randomized into the intervention or control program. Parental consent and student assent were collected for each participating student. The randomized controlled trial received approval from the Baltimore City Public Schools Institutional Review Board; moreover, both the randomized controlled trial and the current study received approval from the Johns Hopkins University Institutional Review Board.
Measures
Prior to being randomized into either RAP Club or the active control program, students completed self-report surveys on their current psychological functioning and behavior. Additionally, two 8th grade teachers from each school rated participating students’ symptoms and behavior.
Self-Report Measures
Social and demographic factors in student surveys included sex (male, female) and race (Black/African American, White, American Indian/Alaskan Native, Asian/South Asian, Native Hawaiian/Other Pacific Islander, Multicultural). Students also reported on their age and ethnicity.
Four self-report items were selected from the Patient-Reported Outcomes Measurement Information System (PROMIS) Pediatric Anxiety Item Bank v2.0 (Pilkonis et al., 2013) to measure anxiety symptoms over the past seven days. The items asked about students’ feelings of being worried, nervous, worried while at home, and feelings that something awful might happen. Items were scored on a Likert scale ranging from 1 (Never) to 5 (Almost Always). Raw sum scores were converted to standardized t-scores. The measure has undergone rigorous testing for use with adolescent samples (Irwin et al., 2010), and it demonstrated adequate reliability in the current sample (see Table 1). The Children’s Depression Inventory – Short Form (CDI-S; Kovacs, 1992) was used to measure depressive symptoms in youth. The CDI-S is a 10-item self-report measure of depressive symptoms over the past two weeks. Items were rated on a 3-point Likert scale, with responses differing depending on the item (e.g., 0 = I am sad once in a while, 1 = I am sad many times, 2 = I am sad all of the time). Items were summed to create a total score that ranged from 0 – 20. The measure demonstrated adequate reliability within the current sample and has shown adequate reliability and validity in prior samples of racial minority adolescents (Sibinga et al., 2016). The Child PTSD Symptom Scale (CPSS; Foa et al., 2001) was used to measure trauma symptoms in participating students. The measure consists of 17 self-report symptom items, which are summed to create an overall symptom severity score. Items assessed a range of trauma symptoms, including re-experiencing the traumatic event, avoidance, and hyperarousal (e.g., How often in the past 2 weeks have you tried not to think about, talk about, or have feelings about the event?). The original version of the measure includes an initial item asking youth to report the most difficult event that they had ever experienced. However, for this study, the item was removed to preserve student privacy. Items were scored on a Likert scale ranging from 0 (not at all or only at one time) to 3 (5 or more times a week or almost always). For the current sample, the measure demonstrated adequate reliability, and has shown adequate reliability in other samples of urban youth (Sibinga et al., 2016). The Youth Outcome Questionnaire – Self Report (YOQSR; Wells et al., 2003) was used to measure students’ behavior. The measure is comprised of five subscales, including intrapersonal distress, somatic symptoms, interpersonal relations, social problems, and behavioral dysfunction. Due to their consistency with the teacher measures, the interpersonal relations, social problems, and behavioral dysfunction subscales were used for the current study. Items were rated on a Likert scale ranging from 0 (never or almost never) to 4 (almost always or always). Two interpersonal relations items, one social problems item, and two behavioral dysfunction items were recoded to −2 (never or almost never) to 2 (almost always or always) as per scoring instructions. The interpersonal relations subscale has a score range of −6 to 34, with higher scores indicating greater difficulty in interactions with family, peers, or other adults including verbal aggression or defiance (e.g., I argue or speak rudely to others). The social problems subscale has a score range of −2 to 26, with higher scores indicating more behaviors that violate social norms, including truancy, physical aggression, or vandalism (e.g., I steal or lie.). Finally, the behavioral dysfunction subscale has a score range of −4 to 40, with higher score indicating more difficulties with attention and concentration, issues in managing impulsive behaviors and organization (e.g., I have a hard time sitting still [or I have too much energy]). The interpersonal problems and behavioral dysfunction subscales demonstrated adequate reliability, but the social problems subscale demonstrated reliability slightly below the common reliability cut-off of .70 in the current sample. However, given that the reliability was close to the conventional cut-off, we decided to include the social problems subscale in the current study. The YOQSR has shown adequate reliability and validity in prior samples of adolescents (Ridge et al., 2009).
Table 1.
Student Demographics
| Characteristics | (n = 426) | ||
|
| |||
| Age in years, mean (range) | 13.22 (11–15) | ||
| Female sex, n (%) | 250 (58.69) | ||
| Race, n (%) | |||
| American Indian/Alaskan Native | 13 (3.24) | ||
| Asian or South Asian | 7 (1.75) | ||
| Black/African American | 281 (70.07) | ||
| Native Hawaiian/Pacific Islander | 7 (1.75) | ||
| White | 42 (10.47) | ||
| Multicultural | 51 (12.72) | ||
| Hispanic/Latinx, n(%) | 57 (13.48) | ||
| Psychological Symptoms | Reporter | Cronbach’s α | M(SD) |
| Anxiety symptoms (PROMIS) | Student | .83 | 57.03 (10.13) |
| Depression symptoms (CDI) | Student | .86 | 3.39 (3.83) |
| Trauma symptoms (CPSS) | Student | .92 | 16.64 (12.38) |
| Interpersonal Relations (YOQSR) | Student | .73 | 4.47 (6.38) |
| Social Problems (YOQSR) | Student | .66 | 2.28 (3.50) |
| Behavioral Dysfunction (YOQSR) | Student | .79 | 10.00 (6.95) |
| Externalizing (SDQ) | Teacher | .88 | 5.59 (4.36) |
| Internalizing (SDQ) | Teacher | .76 | 4.46 (3.32) |
| Problems in Social and Emotional Competence (SCS) | Teacher | .96 | 1.98 (0.96) |
| Correlates | n (%) | ||
| Parent/guardian divorce or separation | Student | N/A | 223 (53.35) |
| Parent/guardian death | Student | N/A | 49 (11.64) |
| Parent/guardian served jail time | Student | N/A | 143 (34.54) |
| Witnessing violence between parents/guardians | Student | N/A | 72 (17.31) |
| Witnessed or victim of neighborhood violence | Student | N/A | 112 (26.86) |
| Lived with someone with mental illness | Student | N/A | 73 (17.46) |
| Lived with someone with substance use disorder | Student | N/A | 64 (15.27) |
| Treated/Judged unfairly because of race/ethnicity | Student | N/A | 56 (13.37) |
| Cigarette use (YRBS) | Student | N/A | 19 (4.49) |
| Alcohol use (YRBS) | Student | N/A | 59 (14.01) |
| Marijuana use (YRBS) | Student | N/A | 29 (6.84) |
| Blunt use (YRBS) | Student | N/A | 33 (7.80) |
| M(SD) | |||
| Total ACES Score | Student | N/A | 1.86 (1.65) |
| Maladaptive coping (Brief COPE) | Student | .75 | 23.66 (5.92) |
| Adaptive coping (Brief COPE) | Student | .85 | 36.74 (9.50) |
| Rumination (CRSQ) | Student | .90 | 1.23 (0.75) |
Participants were also asked to respond to 8 items drawn from a measure of Adverse Childhood Experiences (ACES; Data Resource Center for Child & Adolescent Health, 2016). Students indicated if they had ever experienced any of the following events: the divorce/separation of their parents, a parent/guardian death, parent/guardian in jail, witnessed violence between parents/guardians, witnessed or was a victim of neighborhood violence, lived with someone with mental illness, lived with someone who used drugs or alcohol, or were judged unfairly for their race/ethnicity. An overall count of the number of ACEs experienced was calculated for each participant (range 0–8).
Students completed two measures of coping strategies: the Children’s Response Style Questionnaire (CRSQ; Abela & Vanderbilt, 2000) and the Brief COPE (Carver, 1997). The full CRSQ includes three subscales of coping styles, however students were only asked to complete the 14 items pertaining to rumination. Items were rated on a Likert scale ranging from 0 (almost never) to 3 (almost always), and items were averaged to create an overall rumination score. Higher scores on this measure indicate greater rumination in the face of distress. The measure demonstrated adequate reliability in the sample and has shown adequate reliability in other samples of urban youth (Sibinga et al., 2016). The Brief COPE is a 28-item measure of 14 coping strategies and the frequency of their use by participants. Each coping strategy was measured using two items, and items were rated on a Likert scale ranging from 1 (I usually don’t do this at all) to 4 (I usually do this a lot). Two overall scores were calculated from the Brief COPE: adaptive coping (16 items of strategies including positive reframing, seeking emotional support, seeking instrumental support, active coping, humor, planning, acceptance, and religious/spiritual coping) and maladaptive coping (12 items of strategies including self-blame, denial, self-distraction, behavioral disengagement, venting, and substance use). Both subscales demonstrated adequate reliability in the current sample, as well as prior samples of urban youth (Sibinga et al., 2016).
Students also filled out four questions about lifetime substance use (Centers for Disease Control and Prevention, 2013). Questions asked if students had ever smoked cigarettes, consumed alcohol, used marijuana, or used a blunt. Each item was rated as (0) never used (zero days), (1) one or two days, or (2) more than three days.
Teacher Measures
Teachers completed the Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997) and the Social Competence Scale (SCS; Kam & Greenberg, 1998). The SDQ is a 25-item measure of students’ behavior and potential difficulties along five subscales: emotional symptoms, conduct problems, hyperactivity, peer problems, and prosocial behavior. Items were rated on a Likert scale ranging from 0 (not true) to 2 (certainly true). Two scores were calculated from the SDQ. Externalizing symptoms (including losing one’s temper and being easily distracted) was calculated by combining the 10 items in the conduct problems and hyperactivity subscales. Internalizing symptoms (including worrying and feeling unhappy or depressed) was calculated by combining the 10 items of the emotion problems and peer problems subscales. Both subscales demonstrated adequate reliability in the study sample. The measure has also shown adequate reliability and validity in prior samples of youth (Stone et al., 2010). The SCS is a 31-item measure of students’ behavioral symptoms, along four subscales: aggressive behaviors, oppositional behavior/dysregulation, attention and concentration, and social and emotional competence. Items were rated on a Likert scale ranging from 0 (almost never) to 5 (almost always). For the current study, the 7-item social and emotional competence subscale was used (e.g., “Student listens carefully to others”). Items were reverse scored and averaged to create a score where higher values indicated greater problems with competence. The subscale demonstrated adequate reliability in the study sample.
Statistical Analyses
A three-step latent modeling approach was used to identify latent profiles and test their associations with correlates (Masyn, 2017). In the first step, student self-reported psychological symptoms (anxiety, depressive, and trauma symptoms) and behavior (interpersonal relations, social problems, and behavioral dysfunction), and teacher-rated behavior (internalizing and externalizing symptoms, and problems in social and emotional competence) were z-scored and analyzed using latent profile analysis, to determine the optimal number of symptom profiles in the participating students. As LPA does not require partial conditional independence for model identification, models were estimated across four within-class variance-covariance structures. These structures differ on whether they allow or prohibit variances to vary across latent profiles (i.e., class-varying vs. class-invariant), and on allowing or prohibiting covariance between indicators within profiles (i.e., unrestricted vs. diagonal); thus the four structures being compared are 1) class-invariant diagonal, 2) class-varying diagonal, 3) class-invariant unrestricted, and 4) class-varying unrestricted (Masyn, 2013). The number of latent profiles within each structure was selected using standard fit indices, including Bayesian Information Criteria (BIC), Consistent Akaike Information Criteria (CAIC), Approximate Weight of Evidence Criterion (AWE), Lo-Mendell-Rubin adjusted likelihood ratio test (LMR-LRT), bootstrapped likelihood ratio test (BLRT), Bayes Factor comparisons (BF), approximate correct model probability (cmP), and entropy (Masyn, 2013; Nylund et al., 2007). cmP is then used to compare the selected model from each within-class variance-covariance structure to select a final model. CAIC and AWE are assessed in a similar fashion to BIC, where smaller values are preferred (Masyn, 2013). Much like the commonly used LMR-LRT, BLRT assesses whether adding an additional class or profile significantly improves the fit of the model to the data (Nylund-Gibson & Choi, 2018). Within mixture modeling, these tests are preferred, as prior research has shown them to be robust across various conditions and models (Nylund-Gibson & Choi, 2018). When assessing BF, a model with moderate evidence, or one with a BF > 3 is considered a better fit compared to the model with one additional class. For cmP, which can compare more than two models, the best model is one with the highest cmP value. Entropy, another common model fit indicator in mixture modeling, is an omnibus test of classification of individuals into classes or profiles, where lower scores indicate greater overlap between groups (Nylund-Gibson & Choi, 2018).
In step 2, individual students were assigned to their most likely profile, accounting for measurement error with BCH weights (Nylund et al., 2007). In step 3, the mostly likely membership variable was analyzed as a predictor of the outcome variables (i.e., student self-reported ACEs, coping strategies, and lifetime substance use) using the BCH weights (Nylund et al., 2007). Clustering of students within school was accounted for in Step 3 latent regressions with the inclusion of the “CLUSTER” command for each outcome. The inclusion of this command within a complex mixture model performs a post-hoc adjustment to the standard errors to account for students nested within school (Muthen & Muthen, 2017). Latent regressions also included sex, race, and study cohort year as covariates. Stata 14 was used to generate descriptive statistics, and MPlus Version 8 was used for latent profile analyses and latent regressions.
Results
The study sample consisted of 426 eighth grade students (Mage = 13.22 years, SD = 0.50 years; 58.7% female). Descriptive statistics for the sample are displayed in Table 1. The sample was primarily Black/African American (70.1%) or multicultural (12.7%). For psychological symptoms, 40% of the sample reported elevated trauma symptoms at the cut-off score of 17 or higher on the CPSS (Nixon et al., 2013), and approximately 63% reported elevated symptoms of anxiety above the t-score cut-off of 55 on the PROMIS anxiety measure. However, only approximately 9% of the sample reported elevated depressive symptoms at the cut-off score of 15 or higher, or a score of 7 or higher with endorsement of both feelings of sadness and crying on the CDI-S (Kovacs, 1992).
Latent Profile Analysis
Table 2 reports the fit indices (BIC, CAIC, AWE, LMR-LRT, BF, cmP) for the latent profile analysis (LPA) and includes results only from models that were well-identified. The LPA revealed that the class-varying, diagonal 3-profile solution fit the data the best. For each within-class variance-covariance structure, a single model was selected by comparing fit statistics as well as sample size of profiles within each solution. Prior simulation studies have shown that low estimated class proportions can be problematic, as it may indicate that the solution is unstable and not reproducible in smaller samples (Nylund-Gibson & Choi, 2018). When comparing cmP across the four selected solutions, the class-varying diagonal 3-profile solution was deemed to be the best-fitting model. Profile 1 was composed of 161 adolescents (37.8%), profile 2 was composed of 96 adolescents (22.5%), and profile 3 included 169 adolescents (39.7%).
Table 2.
Model Fit Indices for Exploratory Latent Profile Analysis Using Four Different Within-Class Variance-Covariance Structure Specifications (n = 426)
| # of classes (K) |
LL | npar | BIC | CAIC | AWE | Adj. LMR-LRT p-value (H0: K classes; H1: K↓1 classes) |
BFK,K↓1 | cmPK | cmP. | |
|---|---|---|---|---|---|---|---|---|---|---|
| Class-invariant, diagonal | 1 | −4987.32 | 18 | 10083.62 | 10039.97 | 10048.97 | < 0.01 | < 0.10 | < 0.01 | -- |
| 2 | −4654.96 | 28 | 9479.44 | 9411.54 | 9425.54 | 0.02 | <0.10 | < 0.01 | -- | |
| 3 | −4530.86 | 38 | 9291.79 | 9199.64 | 9218.64 | < 0.01 | < 0.10 | < 0.01 | -- | |
| 4 | −4436.40 | 48 | 9163.42 | 9047.01 | 9071.01 | 0.01 | <0.10 | < 0.01 | < 0.01 | |
| 5 | −4365.61 | 58 | 9082.38 | 8941.73 | 8970.73 | -- | -- | > 0.99 | -- | |
| Class-varying, diagonal | 1 | −4987.32 | 18 | 10083.62 | 10039.97 | 10048.97 | < 0.01 | < 0.10 | < 0.01 | -- |
| 2 | −4465.27 | 37 | 9154.55 | 9064.83 | 9083.33 | 0.01 | < 0.10 | < 0.01 | -- | |
| 3 | −4276.02 | 56 | 8891.09 | 8755.29 | 8783.29 | 0.33 | < 0.10 | < 0.01 | > 0.99 | |
| 4 | −4190.22 | 75 | 8834.53 | 8652.65 | 8690.15 | -- | -- | > 0.99 | -- | |
| Class-invariant, unrestricted | 1 | −4420.63 | 54 | 9168.20 | 9037.25 | 9064.25 | 0.12 | < 0.10 | < 0.01 | -- |
| 2 | −4351.38 | 64 | 9090.24 | 8935.04 | 8967.04 | 0.31 | > 10 | < 0.01 | < 0.01 | |
| 3 | −4305.86 | 74 | 9059.74 | 8880.30 | 8917.30 | 0.48 | > 10 | < 0.01 | -- | |
| 4 | −4270.56 | 84 | 9049.68 | 8845.99 | 8887.99 | 0.23 | > 10 | < 0.01 | -- | |
| 5 | −4232.12 | 94 | 9033.36 | 8805.40 | 8852.40 | -- | -- | > 0.99 | -- | |
| Class-varying, unrestricted | 1 | −4420.63 | 54 | 9168.20 | 9037.25 | 9064.25 | < 0.01 | < 0.10 | < 0.01 | -- |
| 2 | −4181.35 | 109 | 9022.64 | 8758.31 | 8812.81 | 0.67 | <0.10 | <0.01 | -- | |
| 3 | −3985.80 | 164 | 8964.53 | 8566.82 | 8648.82 | -- | <0.10 | > 0.99 | < 0.01 |
Note: LL = log likelihood; npar = number of parameters estimated; BIC = Bayesian Information Criterion; CAIC = Consistent Akaike’s Information Criterion; AWE = Approximate Weight of Evidence; Adj. LMR-LRT = Lo-Mendell-Rubin adjusted likelihood ratio test; BF = Bayes Factor; cmP = approximate correct model probability.
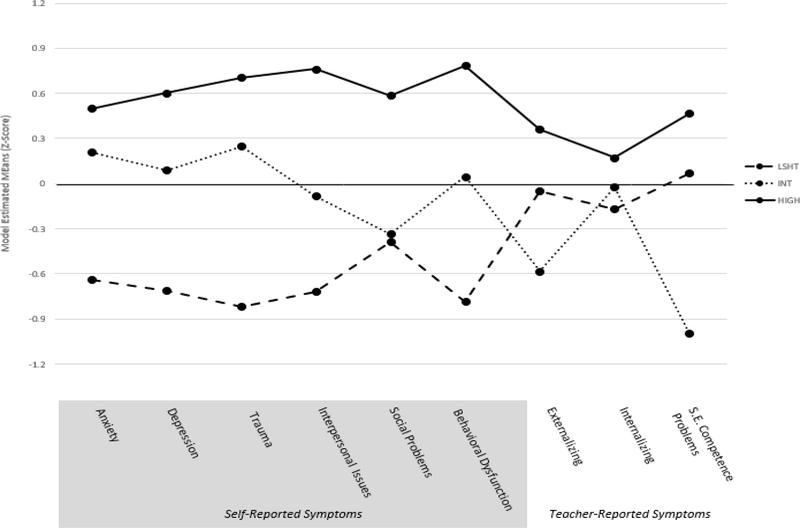
Table 3 lists the model-estimated, class-specific means and standard deviations for all variables included in the LPA. Profile 1 showed that students self-reported generally low symptoms, while teachers reported higher symptoms and problems in social and emotional competence; thus, profile 1 was deemed the low student-reported, high teacher-reported symptoms group (LSHT). Profile 2 had higher student self-reported symptoms, particularly symptoms of internalizing disorders, including anxiety, depression, and trauma. Teacher-reported symptoms were overall low for this profile with the exception of internalizing; thus, profile 2 was deemed the internalizing group (INT). Finally, model estimated means indicated that adolescents in profile 3 had both high student- and teacher-reported symptoms; thus, they were deemed the high symptoms group (HIGH).
Table 3.
Model-Estimated, Class-Specific Means and Standard Deviations with Corresponding 95% Confidence Intervals Based on Class-Varying, Diagonal Three-Class Latent Profile Analysis
| Indicators | Mean | SD | |
|---|---|---|---|
| Class 1: LSHT (37.8%) | Anxiety | −0.64 (−0.80, −0.48) | 0.83 (0.76, 0.89) |
| Depression | −0.71 (−0.80, −0.62) | 0.23 (0.06, 0.32) | |
| Trauma | −0.82 (−0.94, −0.70) | 0.47 (0.37, 0.56) | |
| Interpersonal Issues | −0.72 (−0.85, −0.60) | 0.63 (0.54, 0.71) | |
| Social Problems | −0.39 (−0.47, −0.31) | 0.44 (0.39, 0.50) | |
| Behavioral Dysregulation | −0.78 (−1.01, −0.56) | 0.56 (0.34, 0.72) | |
| Externalizing | −0.05 (−0.26, 0.15) | 1.03 (0.88, 1.15) | |
| Internalizing | −0.17 (−0.36, 0.02) | 0.95 (0.75, 1.12) | |
| Problems in S.E. Competence | 0.07 (−0.13, 0.27) | 0.92 (0.80, 1.02) | |
| Class 2: INT (22.5%) | Anxiety | 0.21 (−0.06, 0.48) | 0.93 (0.77, 1.07) |
| Depression | 0.09 (−0.20, 0.38) | 0.84 (0.64, 1.00) | |
| Trauma | 0.24 (−0.05, 0.54) | 0.85 (0.72, 0.97) | |
| Interpersonal Issues | −0.09 (−0.32, 0.15) | 0.71 (0.58, 0.82) | |
| Social Problems | −0.34 (−0.49, −0.18) | 0.60 (0.53, 0.67) | |
| Behavioral Dysregulation | 0.05 (−0.20, 0.29) | 0.72 (0.62, 0.81) | |
| Externalizing | −0.58 (−0.77, −0.40) | 0.66 (0.50, 0.79) | |
| Internalizing | −0.02 (−0.29, 0.24) | 1.00 (0.86, 1.13) | |
| Problems in S.E. Competence | −1.00 (−1.02, −0.98) | 0.05 (0.03, 0.07) | |
| Class 3: HIGH (39.7%) | Anxiety | 0.50 (0.32, 0.68) | 0.84 (0.71, 0.95) |
| Depression | 0.60 (0.38, 0.82) | 1.09 (0.93, 1.23) | |
| Trauma | 0.71 (0.47, 0.94) | 0.85 (0.71, 0.98) | |
| Interpersonal Issues | 0.76 (0.52, 1.00) | 0.89 (0.75, 1.01) | |
| Social Problems | 0.59 (0.33, 0.85) | 1.27 (1.09, 1.42) | |
| Behavioral Dysregulation | 0.79 (0.61, 0.96) | 0.86 (0.76, 0.95) | |
| Externalizing | 0.36 (0.20, 0.52) | 0.97 (0.87, 1.05) | |
| Internalizing | 0.17 (0.003, 0.34) | 1.01 (0.87, 1.13) | |
| Problems in S.E. Competence | 0.46 (0.30, 0.63) | 0.96 (0.88, 1.04) | |
Note: LSHT = Low student-rated, high teacher-rated symptoms; INT = internalizing symptoms; HIGH = high student- and teacher-reported symptoms; S.E. = social and emotional.
Latent Regressions
Regarding trauma exposure, adolescents in the HIGH symptom profile had significantly greater numbers of adverse childhood experiences than adolescents in the INT profile (see Table 4). Moreover, students in the LSHT profile had significantly greater numbers of adverse childhood experiences than students in the INT profile. In examining specific trauma exposures, students in the HIGH profile, compared to the INT profile, were significantly more likely to experience all the measured traumas, except for parent/guardian death and experiencing racial discrimination. Compared to the LSHT profile, students in the HIGH profile were significantly more likely to have had a parent or guardian who served jail time. Compared to the INT profile, students in the LSHT profile were more likely to have witnessed violence between parents/guardians, experience neighborhood violence, and have lived with someone with a substance use disorder.
Table 4.
Latent regression models of comorbidity profile membership with trauma exposure, coping, and substance use
| Variables | Global Wald Test | LSHT vs. INT | LSHT vs. HIGH | INT vs. HIGH |
|---|---|---|---|---|
| W (p) | β (p) | β (p) | β (p) | |
|
| ||||
| Parent/guardian divorce or separation (ACES) |
10.40
(.01) |
0.09 (.22) |
−0.08 (.29) |
−0.17
(.001) |
|
| ||||
| Parent/guardian death (ACES) | 0.53 (.77) |
0.03 (.59) |
0.003 (.96) |
−0.03 (.50) |
|
| ||||
| Parent/guardian served jail time (ACES) |
8.20
(.02) |
0.004 (.95) |
−0.17
(.02) |
−0.18
(.01) |
|
| ||||
| Witnessing violence between parents/guardians (ACES) |
19.80
(< .001) |
0.19
(.002) |
0.02 (.74) |
−0.17
(< .001) |
|
| ||||
| Witnessed or victim of neighborhood violence (ACES) |
20.76
( <.001) |
0.19
(.001) |
−0.05 (.52) |
−0.24
(< .001) |
|
| ||||
| Lived with someone with mental illness (ACES) |
18.15
(< .001) |
0.10 (.07) |
−0.07 (.34) |
−0.17
(< .001) |
|
| ||||
| Lived with someone with substance use disorder (ACES) |
14.03
(< .001) |
0.16
(.01) |
0.01 (.90) |
−0.15
(< .001) |
|
| ||||
| Treated/Judged unfairly because of race/ethnicity (ACES) | 2.47 (.29) |
0.01 (.82) |
−0.06 (.18) |
−0.07 (.14) |
|
| ||||
| Total ACES Score |
25.41
(< .001) |
0.81
(.001) |
−0.41 (.15) |
−1.22
(< .001) |
|
| ||||
| Maladaptive coping (Brief COPE) |
113.36
(< .001) |
3.91
(< .001) |
−3.84
(< .001) |
−7.75
(< .001) |
|
| ||||
| Adaptive coping (Brief COPE) | 5.38 (.07) |
1.12 (.46) |
−1.72 (.24) |
−2.84 (.02) |
|
| ||||
| Rumination (CRSQ) |
80.70 (< .001) |
0.64 (< .001) |
−0.14 (.13) |
−0.79
(< .001) |
|
| ||||
| Cigarette use (YRBS) | 2.65 (.27) |
0.01 (.84) |
−0.05 (.18) |
−0.05 (.12) |
|
| ||||
| Alcohol use (YRBS) |
24.27 (< .001) |
0.18 (< .001) |
0.01 (.92) |
−0.17 (.002) |
|
| ||||
| Marijuana use (YRBS) |
10.29
(.01) |
0.02 (.67) |
−0.10 (.11) |
−0.13 (.002) |
|
| ||||
| Blunt use (YRBS) |
15.38
(< .001) |
0.03 (.53) |
−0.14 (.02) |
−0.17 (< .001) |
Note: LSHT = low self-reported, high teacher-reported symptoms; INT = internalizing symptoms; HIGH = overall high symptoms
The use of maladaptive coping strategies differed significantly by profile, with those in the HIGH profile characterized by the greatest level of maladaptive coping, followed in descending order by the LSHT profile, and the INT profile. No significant differences were seen in adaptive coping. Students in the INT profile had significantly lower rumination than students in the LSHT or HIGH profiles.
In models predicting substance use, students the HIGH profile had significantly higher use of all alcohol, marijuana, and blunts than students in the INT profile. Compared to the LSHT profile, students in the HIGH group had significantly greater use of blunts. Finally, students in the LSHT group had significantly higher use of alcohol than students in the INT group.
Discussion
The aim of the current study was to identify subgroups of urban youth based on their psychological symptoms as reported by both themselves and their teachers, and to explore group differences by important characteristics. The results of the LPA produced three profiles of comorbid symptoms based on student and teacher reports. Overall, the profile with high student- and teacher-reported symptoms (HIGH) had more trauma exposure, greater use of maladaptive coping mechanisms, and higher substance use. Moreover, the profile with low student-reported, but high teacher-reported symptoms (LSHT) had similar characteristics to the students in the HIGH group. The current study added to the literature on comorbidity in urban youth by including a range of symptoms (e.g., trauma symptoms), information from multiple reporters, and a community sample.
We hypothesized that profiles may differ by groupings of symptoms, such as externalizing and internalizing symptoms, and that we may find groups with overall high or overall low symptoms. Consistent with our hypothesis, we found a group with internalizing symptoms and an overall high symptom group. We also found differences in prevalence of comorbid psychological symptoms as reported by youth themselves versus by teachers. Specifically, we identified a profile with low student-reported and high teacher-reported symptoms (LSHT), which had similar characteristics to the HIGH symptom profile. This supports prior research underscoring the importance of using a multiple informant approach in assessing adolescent mental health, as youth may display symptoms in certain contexts, but not others, and ratings may differ across informants (De Los Reyes et al., 2015).
When students rated themselves as experiencing one type of symptom (e.g., anxiety symptoms), they also tended to rate highly on other self-reported symptoms (e.g., trauma symptoms). This is true with the exception of the measures of their self-reported behaviors (i.e., interpersonal issues and social problems). For example, students in the INT group reported elevated depressive, anxiety, and trauma symptoms, but lower interpersonal issues and social problems. Moreover, students in the INT group tended to report more severe symptoms of anxiety, depression, and trauma than the internalizing symptoms reported by their teachers. In the sample, the average internalizing reported by teachers was 4.46, which is relatively low for the subscale. Therefore, while teachers reported higher internalizing compared to other symptoms within this profile, their reporting of internalizing symptoms was lower than those reported by the students themselves. This is supported by prior research showing that teachers tend to underreport internalizing symptoms compared to students’ self-reports (De Los Reyes et al., 2015).
Findings from this study are consistent with a growing body of research linking adverse childhood events and psychological disorders in youth (McLaughlin, 2017; Schilling et al., 2007). The group with high levels of self- and teacher-reported symptoms (HIGH) experienced more adverse childhood experiences than other urban youth, followed by youth with low self-reported symptoms and high teacher-reported symptoms (LSHT). Of note, youth in the HIGH symptom profile were more likely to have had a parent or guardian incarcerated than youth in the other profile groups. Moreover, youth in the LHST and HIGH groups were more likely to have experienced adverse events related to violence (i.e., witnessing or experiencing neighborhood violence, or witnessing violence between parents/guardians) than youth in the INT subgroups. The association between adverse childhood events and comorbidity seen in this study of urban youth underscores the need for systems that promote positive emotional development for youth who have experienced multiple traumas to prevent the development of psychological disorders (Bethell, Carle, et al., 2017; Bethell, Solloway, et al., 2017).
With respect to coping styles, maladaptive coping and rumination each differed across youth subgroups. There was a significant increase in these negative coping factors from the INT to LSHT to HIGH groups (with the exception that rumination did not increase between the LSHT and HIGH groups). By contrast, adaptive coping--the only protective factor or positive characteristic tested--did not differ significantly by subgroup. These findings are consistent with prior studies examining coping and adolescent mental health (Groth et al., 2019; Thompson et al., 2010). In a meta-analysis examining coping as a mediator in the relationship between locus of control and mental health, maladaptive coping was found to be a significant mediator between locus of control and mental health, while adaptive coping was not a significant mediator, nor was it significantly associated with mental health (Groth et al., 2019). This suggests that maladaptive coping strategies may play a more significant role in the development or exacerbation of psychological symptoms among urban youth, and that having adaptive coping strategies may not be protective against mental health disorders when maladaptive coping strategies are also being utilized. However, it is also possible that our measure of adaptive coping strategies when facing stress did not capture the most relevant strategies used by urban youth, and that salient factors associated with resilience and promotion of mental health were not represented in our measure.
In examining substance use, students in the HIGH symptom group reported greater use of alcohol, marijuana, and blunts. However, there were no significant differences in cigarette use across any of the groups. Results showed that the largest differences in substance use across subgroups were in alcohol and blunt use. While alcohol use in the general U.S. adolescent population has significantly decreased over the past 20–30 years (Peiper et al., 2016), recent research shows that youth who live in low-income urban neighborhoods use alcohol at higher rates than youth in wealthier urban settings (Davis & Grier, 2015). Moreover, youth in low-SES settings are more likely to use blunts and less likely to use bongs, joints, or pipes as their route of marijuana consumption compared to their high-SES counterparts (Trapl & Gonzalez, 2017). While higher prevalence of alcohol and blunt use may have improved our ability to see differences between comorbidity subgroups, the low prevalence of cigarette use may have limited our ability to see subgroup differences.
Limitations
The current study has several limitations. The relatively small size of the sample for the LPA and latent regressions, while exceeding the theoretical minimum, may have limited our ability to detect some possible differences between groups in characteristics low in prevalence, such as cigarette use. The small sample size also limited our ability to explore potential alternative models, such as testing for measurement invariance. Additionally, the small sample size may limit generalizability to other urban youth. Data used for the current study were cross-sectional so it was not possible to establish temporality with respect to development of symptom profiles versus correlates tested. For example, it is not clear whether maladaptive coping strategies led to the onset of symptoms or vice versa or whether causal pathways were bidirectional.
Future Directions
This study’s identification and evaluation of distinct psychological subgroups may help inform assessments and interventions for urban youth. Future research seeking to understand the development of comorbid psychological symptoms in urban youth would benefit from prospective designs to track risk and protective factors and their effects on mental health. By establishing temporality with longitudinal study designs, risk and protective factors emerging earlier in the developmental pathway of comorbid symptoms could be clearly identified to target for prevention efforts. Moreover, future research with the goal of modeling the latent nature of comorbid symptoms experienced by adolescents would benefit from exploring more complex models and measurement invariance. The current study may assist the progression of prevention research in identifying urban youth who are most at-risk of developing comorbid mental health disorders.
This research can also inform culturally and developmentally appropriate programs to promote positive development in urban youth. As the current study was conducted with primarily Black and Latinx urban youth in the U.S., the greater impact of systems and social determinants on mental health disparities must be considered when discussing future directions of prevention and intervention work. The adolescents in our sample are exposed to high levels of trauma from their environment caused by poverty and systemic racism. While our study found that adaptive coping was not predictive of comorbid psychological symptoms, perhaps future work could focus on prevention efforts built to address the use of maladaptive coping strategies that are trauma-informed and address mental health disparities.
Figure 1.
Z-score conditional response means by comorbidity profile membership
Note: LSHT = low self-reported, high teacher-reported symptoms; INT = internalizing symptoms; HIGH = overall high symptoms; S.E. = social and emotional
Acknowledgements
The parent study from which the data for the current study was collected was supported by grants from IES (Grant #: R305A160082, PI: Tamar Mendelson, PhD) and NICHD (Grant #: 1R01HD090022; PI: Tamar Mendelson, PhD). L.W. received support through a training grant from NIDA (Grant #: 5T32DA007292-25, PI: Renee Johnson, PhD). The funders did not play a role in the design or conduct of the current study; analysis and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The authors do not have any potential conflicts.
References
- Abela JRZ, & Vanderbilt E (2000). The Children’s Response Style Questionnaire. McGill University. [Google Scholar]
- Anderson KG, Ramo DE, & Brown SA (2006). Life stress, coping and comorbid youth: An examination of the stress-vulnerability model for substance relapse. Journal of Psychoactive Drugs, 38(3), 255–262. 10.1080/02791072.2006.10399851 [DOI] [PubMed] [Google Scholar]
- Bethell CD, Carle A, Hudziak J, Gombojav N, Powers K, Wade R, & Braveman P (2017). Methods to assess adverse childhood experiences of children and families: Toward approaches to promote child well-being in policy and practice. Academic Pediatrics, 17(7), S51–S69. 10.1016/j.acap.2017.04.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethell CD, Solloway MR, Guinosso S, Hassink S, Srivastav A, Ford D, & Simpson LA (2017). Prioritizing possibilities for child and family health: An agenda to address adverse childhood experiences and foster the social and emotional roots of well-being in pediatrics. Academic Pediatrics, 17(7), S36–S50. 10.1016/j.acap.2017.06.002 [DOI] [PubMed] [Google Scholar]
- Briere J, Hodges M, & Godbout N (2010). Traumatic stress, affect dysregulation, and dysfunctional avoidance: A structural equation model. Journal of Traumatic Stress, 23(6), 767–774. 10.1002/jts.20578 [DOI] [PubMed] [Google Scholar]
- Carver CS (1997). You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2013). Youth Risk Behavior Survey Questionnaire. Youth Risk Behavior Survey Questionnaire. www.cdc.gov/yrbs
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, & Wadsworth ME (2001). Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin, 127(1), 87–127. 10.1037/0033-2909.127.1.87 [DOI] [PubMed] [Google Scholar]
- Data Resource Center for Child & Adolescent Health. (2016). Guide to topics & questions. Guide to Topic & Questionts. http://www.childhealthdata.org/learn/nhis-child/topics_questions/3.3.9-2011-2012-nhis-family-guide-to-topics-and-questions
- Davis B, & Grier S (2015). A tale of two urbanicities: Adolescent alcohol and cigarette consumption in high and low-poverty urban neighborhoods. Journal of Business Research, 68(10), 2109–2116. 10.1016/j.jbusres.2015.03.009 [DOI] [Google Scholar]
- De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DAG, Burgers DE, & Rabinowitz J (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141(4), 858–900. 10.1037/a0038498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau CA, & de la Torre-Luque A (2019). Comorbidity profile of mental disorders among adolescents: A latent class analysis. Psychiatry Research, 278, 228–234. 10.1016/j.psychres.2019.06.007 [DOI] [PubMed] [Google Scholar]
- Farahmand FK, Duffy SN, Tailor MA, DuBois DL, Lyon AL, Grant KE, Zarlinski JC, Masini O, Zander KJ, & Nathanson AM (2012). Community-based mental health and behavioral programs for low-income urban youth: A meta-analytic review. Clinical Psychology: Science and Practice, 19(2), 195–215. 10.1111/j.1468-2850.2012.01283.x [DOI] [Google Scholar]
- Ferdinand RF, de Nijs PFA, van Lier P, & Verhulst FC (2005). Latent class analysis of anxiety and depressive symptoms in referred adolescents. Journal of Affective Disorders, 88(3), 299–306. 10.1016/j.jad.2005.08.004 [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, & Lynskey MT (1994). The comorbidities of adolescent problem behaviors: A latent class model. Journal of Abnormal Child Psychology; New York, 22(3), 339–354. 10.1007/BF02168078 [DOI] [PubMed] [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, & Treadwell KRH (2001). The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child & Adolescent Psychology, 30(3), 376–384. 10.1207/S15374424JCCP3003_9 [DOI] [PubMed] [Google Scholar]
- Gomez R, & Vance A (2014). Confirmatory factor analysis, latent profile analysis, and factor mixture modeling of the syndromes of the Child Behavior Checklist and Teacher Report Form. Psychological Assessment, 26(4), 1307–1316. 10.1037/a0037431 [DOI] [PubMed] [Google Scholar]
- Goodman R (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38(5), 581–586. 10.1111/j.1469-7610.1997.tb01545.x [DOI] [PubMed] [Google Scholar]
- Groth N, Schnyder N, Kaess M, Markovic A, Rietschel L, Moser S, Michel C, Schultze-Lutter F, & Schmidt SJ (2019). Coping as a mediator between locus of control, competence beliefs, and mental health: A systematic review and structural equation modelling meta-analysis. Behaviour Research and Therapy, 121, 103442. 10.1016/j.brat.2019.103442 [DOI] [PubMed] [Google Scholar]
- Gunnar MR, & Vasquez D (2006). Stress, neurobiology and developmental psychopathology. In Cicchetti D & Cohen DJ (Eds.), Developmental psychopathology: Developmental neuroscience (pp. 533–577). Wiley & Sons, Inc. [Google Scholar]
- Hogue A, & Dauber S (2013). Diagnostic profiles among urban adolescents with unmet treatment needs: Comorbidity and perceived need for treatment. Journal of Emotional and Behavioral Disorders, 21(1), 18–32. 10.1177/1063426611407500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz K, McKay M, & Marshall R (2005). Community violence and urban families: Experiences, effects, and directions for intervention. American Journal of Orthopsychiatry, 75(3), 356–368. 10.1037/0002-9432.75.3.356 [DOI] [PubMed] [Google Scholar]
- Irwin DE, Stucky B, Langer MM, Thissen D, DeWitt EM, Lai J-S, Varni JW, Yeatts K, & DeWalt DA (2010). An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Quality of Life Research, 19(4), 595–607. 10.1007/s11136-010-9619-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kam C, & Greenberg MT (1998). Technical measurement report on the Teacher Social Competence Rating Scale [Unpublished]. Prevention Research Center for the Promotion of Human Development, The Pennsylvania State University. [Google Scholar]
- Kessler RC, Price RH, & Wortman CB (1985). Social factors in psychopathology: Stress, social support, and coping processes. Annual Review of Psychology, 36, 531–572. 10.1146/annurev.ps.36.020185.002531 [DOI] [PubMed] [Google Scholar]
- Kovacs M (1992). Children’s Depression Inventory (CDI) Manual. Multi-Health Systems. [Google Scholar]
- Liu J, Mustanski B, Dick D, Bolland J, & Kertes DA (2017). Risk and protective factors for comorbid internalizing and externalizing problems among economically disadvantaged African American youth. Development and Psychopathology, 29(3), 1043–1056. 10.1017/S0954579416001012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masyn KE (2013). Latent class analysis and finite mixture modeling. In Nathan PE (Ed.), The Oxford Handbook of Quantitative Methods (Vol. 2, pp. 551–611). Oxford University Press. [Google Scholar]
- Masyn KE (2017). Measurement Invariance and Differential Item Functioning in Latent Class Analysis With Stepwise Multiple Indicator Multiple Cause Modeling. Structural Equation Modeling: A Multidisciplinary Journal, 24(2), 180–197. 10.1080/10705511.2016.1254049 [DOI] [Google Scholar]
- McLaughlin KA (2017, April). The long shadow of adverse childhood experiences: Adverse environments early in life have lasting consequences for children’s health and development. Social Science Agenda. https://www.apa.org/science/about/psa/2017/04/adverse-childhood
- Muthen LK, & Muthen BO (2017). MPlus User’s Guide (8th ed.). Los Angeles, CA: Muthen & Muthen. [Google Scholar]
- Neuman RJ, Heath A, Reich W, Bucholz KK, Madden PAF, Sun L, Todd RD, & Hudziak JJ (2001). Latent class analysis of ADHD and comorbid symptoms in a population sample of adolescent female twins. Journal of Child Psychology and Psychiatry, 42(7), 933–942. 10.1111/1469-7610.00789 [DOI] [PubMed] [Google Scholar]
- Nixon RDV, Meiser-Stedman R, Dalgleish T, Yule W, Clark DM, Perrin S, & Smith P (2013). The Child PTSD Symptom Scale: An update and replication of its psychometric properties. Psychological Assessment, 25(3), 1025–1031. 10.1037/a0033324 [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo Simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Nylund-Gibson K, & Choi AY (2018). Ten frequently asked questions about latent class analysis. Translational Issues in Psychological Science, 4(4), 440–461. 10.1037/tps0000176 [DOI] [Google Scholar]
- Peiper NC, Ridenour TA, Hochwalt B, & Coyne-Beasley T (2016). Overview on prevalence and recent trends in adolescent substance use and abuse. Child and Adolescent Psychiatric Clinics of North America, 25(3), 349–365. 10.1016/j.chc.2016.03.005 [DOI] [PubMed] [Google Scholar]
- Peiper N, Clayton R, Wilson R, Illback R, O’Brien E, Kerber R, Baumgartner R, & Hornung C (2015). Empirically derived subtypes of serious emotional disturbance in a large adolescent sample. Social Psychiatry and Psychiatric Epidemiology, 50(6), 983–994. 10.1007/s00127-015-1017-2 [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Salsman JM, Butt Z, Moore TL, Lawrence SM, Zill N, Cyranowski JM, Kelly MAR, Knox SS, & Cella D (2013). Assessment of self-reported negative affect in the NIH Toolbox. Psychiatry Research, 206(1), 88–97. 10.1016/j.psychres.2012.09.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridge NW, Warren JS, Burlingame GM, Wells MG, & Tumblin KM (2009). Reliability and validity of the youth outcome questionnaire self-report. Journal of Clinical Psychology, 65(10), 1115–1126. 10.1002/jclp.20620 [DOI] [PubMed] [Google Scholar]
- Schilling EA, Aseltine RH, & Gore S (2007). Adverse childhood experiences and mental health in young adults: A longitudinal survey. BMC Public Health, 7(1), 30. 10.1186/1471-2458-7-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibinga EMS, Webb L, Ghazarian SR, & Ellen JM (2016). School-Based Mindfulness Instruction: An RCT. Pediatrics, 137(1), e20152532. 10.1542/peds.2015-2532 [DOI] [PubMed] [Google Scholar]
- Stone LL, Otten R, Engels RCME, Vermulst AA, & Janssens JMAM (2010). Psychometric Properties of the Parent and Teacher Versions of the Strengths and Difficulties Questionnaire for 4- to 12-Year-Olds: A Review. Clinical Child and Family Psychology Review, 13(3), 254–274. 10.1007/s10567-010-0071-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE, & Stanton AL (2007). Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology, 3(1), 377–401. 10.1146/annurev.clinpsy.3.022806.091520 [DOI] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, & Dulcan MK (2003). Comorbid psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry, 60(11), 1097–1108. 10.1001/archpsyc.60.11.1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terreri CJ, & Glenwick DS (2013). The relationship of religious and general coping to psychological adjustment and distress in urban adolescents. Journal of Religion and Health, 52(4), 1188–1202. 10.1007/s10943-011-9555-8 [DOI] [PubMed] [Google Scholar]
- Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, & Gotlib IH (2010). Maladaptive coping, adaptive coping, and depressive symptoms: Variations across age and depressive state. Behaviour Research and Therapy, 48(6), 459–466. 10.1016/j.brat.2010.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trapl E, & Gonzalez SJK (2017). Adolescent marijuana use and co-occurrence with tobacco use: Implications for tobacco regulation. Journal of Applied Research on Children: Informing Policy for Children at Risk, 8(2), 17. [Google Scholar]
- van Lang NDJ, Ferdinand RF, Ormel J, & Verhulst FC (2006). Latent class analysis of anxiety and depressive symptoms of the Youth Self-Report in a general population sample of young adolescents. Behaviour Research and Therapy, 44(6), 849–860. 10.1016/j.brat.2005.06.004 [DOI] [PubMed] [Google Scholar]
- Wadsworth ME, Hudziak JJ, Heath AC, & Achenbach TM (2001). Latent class analysis of Child Behavior Checklist Anxiety/Depression in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 40(1), 106–114. 10.1097/00004583-200101000-00023 [DOI] [PubMed] [Google Scholar]
- Wells M, Burlingame G, & Rose P (2003). Youth Outcome Questionnaire Self Report. American Professional Credentialing Services. [Google Scholar]
- Wigman JT, Devlin N, Kelleher I, Murtagh A, Harley M, Kehoe A, Fitzpatrick C, & Cannon M (2014). Psychotic symptoms, functioning and coping in adolescents with mental illness. BMC Psychiatry, 14(1), 97–105. 10.1186/1471-244X-14-97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH, Aron L, Dubay L, Simon SM, Zimmerman E, & Luk KX (2015). How are income and wealth linked to health and longevity? 22. [Google Scholar]