Abstract
Background
In the United States, distribution plans for the COVID-19 vaccination were established at the state level. However, some states, such as Connecticut, followed an age-based strategy without considering occupations or co-morbid conditions due to its simplicity in implementation. This strategy raised concerns about exacerbating health inequities because it did not prioritize vulnerable communities, specifically, minorities and low-income groups. The study aims to examine the vaccination inequities among different population groups for people aged 65+.
Methods
A cross-sectional analysis of quantile-based independent sample t-test was employed to examine the relationship between eight social vulnerability indices (SVIs, i.e., below poverty, unemployed, without high school diploma, disability, minority, speaks English less than well, no vehicle, and mobile homes) and vaccination rates at the town level in Connecticut during the second phase of the vaccine distribution plan when individuals aged 65 and over were eligible. Negative binomial regressions were employed to further justify the relationships between SVIs and vaccination rates.
Results
The report shows that the differences in vaccination rates were statistically significant between the most vulnerable and the least vulnerable towns with respect to six SVIs (i.e., below poverty, without high school diploma, disability, minority, speaks English less than well, and no vehicle). The vaccination gap was greater for people aged 75+ than people aged 65–74. Among the selected SVIs, below poverty was negatively correlated with the vaccination rate for 75+, and without high school diploma was negatively correlated with both rates.
Conclusions
This report reveals the significant health inequities in COVID-19 vaccination among the elderly population at the early vaccination phase. It can shed insights into health policy initiatives to improve vaccination coverage in the elderly communities, such as promoting onsite scheduling and increasing at-home vaccination services.
Keywords: COVID-19, Elderly, Vaccination, Health inequity, Social vulnerability
Introduction
In the United States, distribution plans for the Coronavirus Disease 2019 (COVID-19) vaccination have been established at the state level. Like many states, Connecticut’s first phase included vaccinating health care workers and nursing home residents, followed by people aged 75 and older starting on January 18, 2021. However, unlike most states, Connecticut continued a primarily age-based strategy: people 65 and over were eligible on February 11, 2021, followed by other age groups in reverse chronological order [1].
The rationale provided by state leaders for this approach was its simplicity: it did not require proof of a particular occupation (e.g., front-line worker) or co-morbid condition. However, this strategy raised concerns about exacerbating health inequities because it did not prioritize communities that have been disproportionately affected by COVID-19, specifically, minorities and low-income groups [2,3]. These population groups were found to lack access to quality health care because of the under-coverage of health insurance, language barriers, and distrust of medical professionals [4].
This short report aims to examine the relationship between social vulnerability and vaccination rates at the town level during the second phase of the vaccine distribution plan when individuals aged 65 and over were eligible. Existing studies identified that low socioeconomic status US counties had lower vaccination rates, and such vaccination disparities enlarged as the vaccine eligibility expanded [5,6]. However, few studies have focused on the elderly population at a small geographic scale, such as the town level. Findings from this report can help reveal the vaccination gap in current vaccination practices for the elderly population, eventually providing evidence to increase the vaccination coverage and develop equitable health policy.
Methods
We performed a cross-sectional analysis to employ the association of COVID-19 vaccination rates with selected social vulnerability variables in Connecticut towns (n = 168). We collected town-level vaccination rates for those having received at least one dose from the Connecticut Department of Public Health (CTDPH) as of March 8, 2021 [1]. The vaccination data included two population groups: those aged 65–74 and those aged 75+. To characterize the towns, we selected eight social vulnerability variables from the 2018 United States Centers for Disease Control (CDC)’s Social Vulnerability Index (SVI). These variables were: below poverty, unemployed, without high school diploma, disability, minority, speaks English less than well, no vehicle, and mobile homes [7].
Specifically, to explore the relationship between social vulnerability and vaccination rates among the elderly population, we examined the vaccination inequities between the towns in the lower SVI quartile (Q1) and those in the upper SVI quartile (Q4). We applied an independent sample t-test to identify if a significant difference existed in the vaccination rates of those aged 65–74 and those aged 75+ between the towns in Q1 and Q4 with respect to each SVI. As a robustness check, we also included all SVIs in the same model using negative binomial regression analysis (see details in Appendix in Supplementary material). The statistical analysis was completed in IBM SPSS 18. The data visualization was completed in ESRI ArcGIS Pro 2.6.
Results
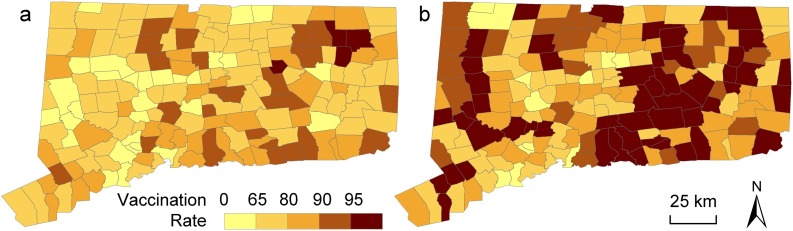
As of March 8, the vaccination rates in Connecticut were 72.89% and 80.17% for age groups 65–74 and 75+, respectively. Both rates were comparatively higher in the eastern part of the state (Fig. 1 ). The differences in vaccination rates were statistically significant between Q1 and Q4 with respect to six SVIs (i.e., below poverty, without high school diploma, disability, minority, speaks English less than well, and no vehicle; Table 1 ). Specifically, the difference in vaccination rate for 65–74 was the largest with respect to lack of education (i.e., difference = 12.91%), and the difference in vaccination rate for 75+ was the largest with respect to no vehicle (i.e., difference = 25.19%). Our secondary analysis employing negative binomial regressions (see details in Appendix in Supplementary material) shows that among the selected SVIs, poverty was negatively correlated with the vaccination rate for 75+ (coefficient: −0.00725, p < 0.05), and lack of education was negatively correlated with both rates (coefficient for 65–74: −0.0251, p < 0.001; coefficient for 75+: −0.0249, p < 0.001).
Fig. 1.
Spatial distribution of vaccination rates for population (a) aged 65–74, and (b) aged 75+ in Connecticut towns.
Table 1.
Vaccination rates for the least (Q1) and most (Q4) vulnerable towns.
| SVIa | Quartileb | SVI rangea | Rate for 65–74 (std.)c | Rate for 75+ (std.)c |
|---|---|---|---|---|
| Below poverty | Q1 | 0.80–3.45 | 79.58 (9.99) | 98.01 (14.92) |
| Q4 | 37.57–28.51 | 69.12 (12.37) | 73.87 (13.70) | |
| Difference estimated | 10.46*** | 24.14*** | ||
| Difference 95% CIe | 5.59–15.35 | 17.92–30.35 | ||
| Unemployed | Q1 | 0.22–2.01 | 75.60 (9.39) | 88.75 (15.64) |
| Q4 | 3.57–7.15 | 70.99 (12.43) | 83.72 (19.24) | |
| Difference estimated | 4.61 | 5.03 | ||
| Difference 95% CIe | −0.14 to 9.36 | −2.54 to 12.58 | ||
| Without high school diploma | Q1 | 0.91–2.95 | 79.77 (8.19) | 98.62 (13.53) |
| Q4 | 6.09–15.72 | 66.86 (10.14) | 74.47 (14.91) | |
| Difference estimated | 12.91*** | 24.15*** | ||
| Difference 95% CIe | 8.91–16.92 | 17.97–30.33 | ||
| Disability | Q1 | 5.01–8.76 | 78.54 (9.47) | 96.80 (15.31) |
| Q4 | 12.57–17.15 | 70.69 (11.59) | 80.52 (17.03) | |
| Difference estimated | 7.85*** | 16.28*** | ||
| Difference 95% CIe | 3.25–12.45 | 9.25–23.31 | ||
| Minority | Q1 | 3.28–7.39 | 78.81 (11.05) | 95.80 (17.39) |
| Q4 | 20.16–85.23 | 70.18 (11.49) | 74.80 (10.88) | |
| Difference estimated | 8.63*** | 21.00*** | ||
| Difference 95% CIe | 3.74–13.53 | 14.70–27.30 | ||
| Speaks English less than well | Q1 | 0–0.29 | 78.07 (10.33) | 94.38 (15.05) |
| Q4 | 1.92–12.21 | 70.28 (13.24) | 74.46 (13.23) | |
| Difference estimated | 7.79** | 19.92*** | ||
| Difference 95% CIe | 2.63–12.95 | 13.76–26.07 | ||
| No vehicle | Q1 | 0–0.82 | 79.30 (8.94) | 98.84 (13.78) |
| Q4 | 2.4 –11.75 | 70.50 (11.84) | 73.65 (12.02) | |
| Difference estimated | 8.80*** | 25.19*** | ||
| Difference 95% CIe | 4.24–13.36 | 19.58–30.80 | ||
| Mobile homes | Q1 | 0–0 | 76.36 (11.53) | 89.94 (16.57) |
| Q4 | 0.55–4.82 | 76.14 (10.32) | 87.49 (12.69) | |
| Difference estimated | 0.22 | 2.45 | ||
| Difference 95% CIe | −4.54 to 4.96 | −3.96 to 8.87 |
p < 0.01.
p < 0.001.
Town-level SVI was rescaled from the census tract-level SVI based on the total census tract population in a town. The variable in percentage (%) was normalized with respect to town population. A higher SVI score means that the town has higher levels of social vulnerability.
To correspond to the census tract-level SVI data, we merged the towns of Canaan and Norfolk in the county of Litchfield, thus leading to a total of 168 towns. Each quartile had 42 towns.
The vaccination rates are mean values in percentage (%); std. is the standard deviation.
A positive number in the difference estimate means the Q1 rate was higher than Q4 rate.
CI is the confidence interval.
Discussion
Past research shows that people residing in socioeconomically disadvantaged areas were more vulnerable to COVID-19 diagnosis and death [3,8]. This report further strengthens that such health inequities existed in the COVID-19 vaccination within the two elderly age groups by comparing the most and least vulnerable towns in Connecticut. It also reveals that the vaccination gap was greater among people aged 75+ than people aged 65–74. The differences in vaccination rates were further correlated with two social vulnerability variables: below poverty and without high school diploma.
Although the US and many other countries have generally adopted an age-based criterion for vaccine prioritization, it has been found that age was negatively correlated with the willingness to receive COVID-19 vaccines [9]. The finding suggests that although the elderly population was prioritized in health care, they were more reluctant to take vaccines and thus more vulnerable to the infection. Such vaccination reluctance within the elderly population needs to be further explored, such as which age group had a wider vaccination gap and which socioeconomic variable most contributed to the vaccination disparities. By revealing the relationships between vaccination rates and SVI-based social vulnerability variables among people aged 65+ in Connecticut, the study sheds further insights into health policy initiatives to improve vaccination coverage among the elderly in the state and beyond.
Specifically, the study justifies that the socioeconomically disadvantaged elderly groups, especially those aged 75+, had a lower vaccination rate. Also, poverty and under-education contributed most to the lack of vaccination. The relative lack of vaccination among the socially vulnerable elderly group, especially those in poverty and undereducated, could result from the scarcity of transportation resources to access vaccination clinics and a lack of computer literacy in scheduling appointments [10]. Thus, promoting onsite scheduling and increasing at-home vaccination services in the elderly communities in the US and other countries will be a necessity to reducing health inequities.
In this report, we focused on Connecticut towns, and thus the conclusion cannot be extended to another region or at a different geographical scale. The cross-sectional study does not account for individual-level inferences or consider the temporality in vaccination phases. Since the state government administers the COVID-19 vaccination with largely different timelines and eligibility criteria, it is advisable to fully examine the geographical heterogeneity in vaccination policy among states and even across countries in order to justify health inequities.
Funding
No funding sources.
Conflict of interest
None declared.
Ethical approval and consent to publish
The study does not require ethical approval.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jiph.2021.07.013.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.CTDPH . 2021. COVID-19 vaccine distribution in Connecticut.https://data.ct.gov/stories/s/CoVP-COVID-Vaccine-Distribution-Data/bhcd-4mnv/ [Accessed 6 April 2021] [Google Scholar]
- 2.NASEM . National Academies of Sciences, Engineering, Medicine; 2020. Framework for equitable allocation of COVID-19 vaccine. [PubMed] [Google Scholar]
- 3.Karaye I.M., Horney J.A. The impact of social vulnerability on COVID-19 in the US: an analysis of spatially varying relationships. Am J Prev Med. 2020;59(3):317–325. doi: 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szczepura A. Access to health care for ethnic minority populations. Postgrad Med J. 2005;81(953):141–147. doi: 10.1136/pgmj.2004.026237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hughes M.M., Wang A., Grossman M.K., Pun E., Whiteman A., Deng L. County-level COVID-19 vaccination coverage and social vulnerability—United States, December 14, 2020–March 1, 2021. Morb Mortal Wkly Rep. 2021;70(12):431. doi: 10.15585/mmwr.mm7012e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barry V., Dasgupta S., Weller D.L., Kriss J.L., Cadwell B.L., Rose C. Patterns in COVID-19 Vaccination Coverage, by Social Vulnerability and Urbanicity–United States, December 14, 2020?May 1, 2021. Morb Mortal Wkly Rep. 2021;70(22):818. doi: 10.15585/mmwr.mm7022e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CDC . 2021. CDC Social Vulnerability Index.https://www.atsdr.cdc.gov/placeandhealth/svi/index.html [Accessed 6 April 2021] [Google Scholar]
- 8.Khazanchi R., Beiter E.R., Gondi S., Beckman A.L., Bilinski A., Ganguli I. County-level association of social vulnerability with COVID-19 cases and deaths in the USA. J Gen Intern Med. 2020;35(9):2784–2787. doi: 10.1007/s11606-020-05882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kreps S., Prasad S., Brownstein J.S., Hswen Y., Garibaldi B.T., Zhang B. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Network Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.25594. e2025594-e2025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramsetty A., Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.