Abstract
Background/Objectives:
The purpose of this study was to determine the joint associations of weight status and physical activity with mobility disability in older men and women.
Subjects/Methods:
We analyzed prospective data from 135 220 participants in the NIH-AARP Diet and Health Study between 1995-1996 and 2004-2005.
Methods:
Height and weight, as well as light- and moderate-to-vigorous-intensity physical activity typical of the past 10 years (h/week) were self-reported at baseline, and body mass index (BMI: kg/m2) was categorized into normal weight (BMI 18-<25 kg/m2); overweight (BMI 25-<30 kg/m2); and obese (BMI ≥30 kg/m2). Mobility was assessed by self-report at follow-up and mobility disability was defined as reporting “unable to walk” or an “easy usual walking pace (<2 mph)”. Multivariable logistic regression determined the independent and joint associations of weight status and total physical activity with the odds of mobility disability.
Results:
Twenty-one percent of men and 37% of women reported a mobility disability at follow-up. We observed a curvilinear dose-response association between increasing categories of weight status and mobility disability within each tertile of physical activity, with the highest odds experienced by men and women with overweight (OR=2.45; 95%CI: 2.25, 2.67 for men and OR=2.99; 95%CI: 2.78, 3.22 for women) and obesity (OR=3.93; 95%CI: 3.58, 4.32 for men and OR=5.08; 95%CI: 4.65, 5.54 for women) in combination with low physical activity. Moreover, among those reporting 7 or fewer hours/week of total physical activity, being of normal body weight did not eliminate the excess odds of mobility disability.
Conclusions:
These findings highlight the combined importance of obesity prevention and physical activity promotion to mobility in older age. Given aging demographics and the global economic burden associated with aging- and disuse-related disability, there is tremendous public health benefit to understanding how various modifiable determinants of mobility disability can interact in older age.
Keywords: Aging, Body Weight, Exercise, Physical Function
Introduction
Physical disability is present in approximately 36% of non-institutionalized older adults living in the United States, with mobility disability being the most common form (27%).1 Mobility impairments increase the risk of isolation, hospitalization, institutionalization, and associated health care costs.2, 3 The overall prevalence of mobility disability tends to be higher in older women compared with older men, and is inversely associated with income and level of educational attainment.1–3
There is now ample evidence that older people with obesity [defined as a body mass index (BMI) ≥30 kg/m2] are particularly susceptible to mobility disability.4 A number of epidemiologic studies indicate, however, that the relation between body mass index and disability in older people is curvilinear, with increased risk experienced by those at the lowest (BMI<18 kg/m2) and the highest ends of the BMI distribution, and the greatest risk observed in those with class II obesity or higher (BMI ≥35 kg/m2).5 Several studies also now report that the lowest risk for physical disability is observed among those considered to be overweight (i.e., BMI 25-<30 kg/m2). 5, 6
Physical activity can lower the risk of aging-related mobility disability – even among older people with obesity.7–10 The level of physical activity necessary to achieve this risk reduction in older people with obesity has not been determined, however, and may depend on one’s physical activity and obesity history.11 Prospective data from the Health ABC Study suggest that among older people with obesity, high levels of physical activity (i.e., the highest quartile of the distribution) mitigated the risk of mobility limitations, whereas, moderate and low levels did not.8 Another study among the InCHIANTI cohort reported that walking speed showed a exponentially steeper decline over 6 years among those with the combination of low muscle strength and obesity, compared with those having only low strength or obesity and those having neither,12 suggesting that the combined effects of excess weight and low fitness on mobility loss may be especially deleterious in older age.
We know of only one other study that examined prospectively the unique and joint contributions of weight status and physical activity on the risk of mobility disability8. Moreover, to our knowledge, no studies have considered light-, as well as moderate-to-vigorous intensity physical activity in the analyses while also adjusting for television (TV) viewing time and other lifestyle-related factors such as smoking and caloric intake. Accordingly, we analyzed prospective data from 135 220 participants in the National Institutes of Health (NIH) –American Association of Retired Persons (AARP) Diet and Health Study between 1995-1996 and 2004-2005. We hypothesized that a higher BMI and weight status at baseline would significantly increase the odds of self-reported mobility loss at follow-up, independent of baseline levels of light-, moderate-, and vigorous-intensity physical activity. We further proposed that this increased risk would be accelerated among those with overweight and obesity combined with the lowest levels of physical activity.
Materials/Subjects and Methods
The NIH-AARP Diet and Health Study was established in 1995-1996 and comprised 566 398 AARP members (50-71 years) in six states and two metropolitan areas who responded to a baseline questionnaire about their medical history, diet, physical activity and sedentary behaviors. This baseline cohort represents about 17.6% of the 3.5 million AARP members who were sent the initial questionnaire.13 A follow-up questionnaire was completed in 2004-2006 by 318,714 participants. Those respondents who provided complete data on both questionnaires and who were free of chronic disease (e.g., diabetes, heart disease, emphysema, cancer, or stroke) at baseline were eligible to be included in the analysis. To ensure the healthiest cohort possible, we also only included people who reported their health status as fair or better (N=135 220; Figure 1). All participants signed informed written consent forms approved by the institutional review boards of the National Cancer Institute and the George Washington University.
Figure 1 –
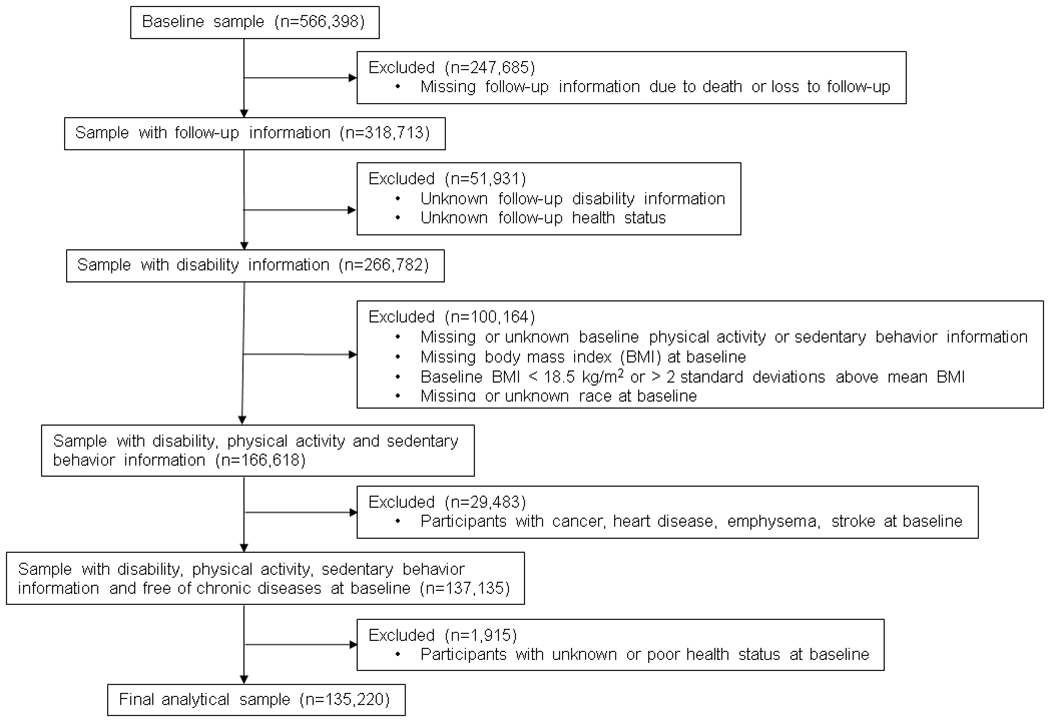
Participant selection from the NIH-AARP Diet and Health Study cohort. Those respondents who provided complete data on both questionnaires and who were free of chronic disease (e.g., diabetes, heart disease, emphysema, cancer, or stroke) at baseline were eligible to be included in the analysis. To ensure the healthiest cohort possible, we also only included people who reported their health status as fair or better at baseline (N=135 220).
Assessment of primary study variables
Height and weight were assessed by self–report on the risk factor questionnaire at baseline and the body mass index calculated as weight (kg)/height (m)2. Weight status was then defined as normal weight (BMI 18-<25 kg/m2); overweight (BMI 25-<30 kg/m2); and obese (BMI ≥30 kg/m2). Participants were also asked about the typical amount of time per week spent in light-intensity (e.g., housework, walking, shopping) and in moderate-to-vigorous intensity (e.g., brisk walking, yard work, jogging) physical activity over the past 10 years. Response categories to the physical activity questions were <1 h/week; 1-3 h/week; 4-7 h/week; and >7 h/week. Television viewing time typical of a 24-h period during the past 12 months was also assessed using response categories of 0-2 h/day; 3-4 h/day; and ≥5 h/day. Physical activity and TV viewing time questions from the risk factor questionnaire were not validated directly, but they have demonstrated expected associations with colon, rectal, and endometrial cancer risk and mortality in this cohort.14–16 Self-reported mobility status at the 2004-2005 follow-up was assessed by a question about normal walking pace (unable to walk; easy (< 2mph); normal (2-2.9 mph); brisk (3-3.9mph); very brisk (≥4mph)). Mobility disability was defined as a response of “unable to walk” or “easy (<2mph)”.
Statistical analysis
Univariate analyses (means±SD, frequencies (%)) first were generated on all study variables in order to determine their distributions within the study population. We assessed collinearity and associations among the study variables using correlation and chi-square tests. Given our fixed cohort with little variation in follow-up time, we used logistic regression to evaluate the simple associations of each study variable and covariable on the odds of mobility disability. Multivariable logistic regression models were then used to determine associations between weight status (or BMI) and mobility disability when adjusting for light- and moderate-to vigorous intensity physical activity, as well as for the self-reported covariables age at entry, race, level of educational attainment, baseline smoking status, caloric intake, daily TV viewing, and self-reported health at follow-up. These covariables were chosen based on their associations with mobility disability in the simple analysis, as well as on their relationship to weight status or to mobility in the literature.
In order to determine the joint effects of weight status and physical activity on mobility disability, categorical scores for light activity (0=<1 h/week; 1=1-3 h/week; 2=4-7 h/week; 3=>7 h/week) were added to scores of moderate-to-vigorous intensity physical activity (0=<1 h/week; 1=1-3 h/week; 2=4-7 h/week; 3=>7 h/week) to create a total physical activity variable with scores ranging from 0 to 6. Total physical activity score was then divided into tertiles based on its distribution (0=>7 h/week; 1=4-7 h/week; and 2=≤3 h/week). We tested the joint effects of weight status (0=normal weight; 1= overweight; and 2= obese) within each tertile of total physical activity on mobility disability by creating 9 indicator variables. This allowed us to compare directly groups with varying amounts of body weight and physical activity against those who were of normal weight and also had the most physical activity (referent group). All multivariable models were adjusted for age, sex, race, level of educational attainment, smoking, TV viewing time, as well as for reported health status at follow-up. Odds ratios (OR) and 95% confidence intervals (CI) are reported from the final logistic regression models to describe the excess odds of mobility disability within each level of weight status and physical activity relative to the referent group. All analyses are presented separately for men and women.
Results
The average follow-up time in this cohort was 8.6±0.42 years, with a mean age of entry of 61.2±5.3 years. Approximately 58% of the NIH-AARP cohort were men; 94% were white, and nearly 45% had a college degree. Twenty-one percent of men and 37% of women reported a mobility disability at follow-up. Table 1 displays subject characteristics at baseline according to sex and mobility status at follow-up. Baseline BMI was significantly higher in those reporting mobility disability compared with those who did not (p<0.001). Among men, however, unadjusted reported mobility disability was greatest in those who were overweight compared with those who were of normal weight or obese (p<0.001), while among women, reported disability was lowest among those who were obese (p<0.001) (Figure 2). Also, those who reported lower educational attainment, poorer self-reported health at baseline and follow-up, and smoking at baseline were significantly more likely to report mobility disability at follow-up (p<0.001). Baseline levels of light- and moderate-to-vigorous intensity physical activity were significantly associated with reported mobility disability at follow-up (p<0.001), with the association appearing stronger for moderate-to-vigorous compared with light-intensity activity.
Table 1.-.
Baseline characteristics of the NIH-AARP cohort (N=135 220) by sex and mobility status.
| Variable | Men (n=78 040) | p-value | Women (n=57 180) | p-value | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Mobility Disability (n=16 139) | No Mobility Disability (n=61 901) | Mobility Disability (n=21 067) | No Mobility Disability (n=36 113) | |||
| Age (years) | 62.9±5.1 | 60.0±5.3 | <0.001 | 62.4±5.1 | 60.4±5.3 | <0.001 |
| BMI (kg/m2) | 27.8±3.6 | 26.4±3.2 | <0.001 | 27.1±4.2 | 25.0±3.7 | <0.001 |
| Race (%) | <0.001 | <0.001 | ||||
| White | 95.5 | 93.2 | 91.8 | 94.3 | ||
| Black | 3.2 | 1.6 | 5.1 | 3.1 | ||
| Hispanic | 2.1 | 1.4 | 1.8 | 1.4 | ||
| Other | 1.5 | 1.4 | 1.3 | 1.2 | ||
| Education (%) | <0.001 | <0.001 | ||||
| ≤ High school | 30.1 | 14.6 | 36.1 | 24.6 | ||
| Post-high school | 32.7 | 29.0 | 36.6 | 36.0 | ||
| College or above | 37.2 | 56.4 | 26.5 | 39.5 | ||
| Baseline health status (%) | <0.001 | <0.001 | ||||
| Fair | 9.8 | 2.7 | 10.2 | 2.8 | ||
| Good | 46.5 | 26.1 | 41.5 | 25.4 | ||
| Very Good | 36.2 | 44.1 | 36.1 | 43.5 | ||
| Excellent | 12.5 | 27.0 | 12.2 | 28.4 | ||
| Current smoker (%) | 13.8 | 6.7 | <0.001 | 15.3 | 9.4 | <0.001 |
| Light PA in past 10 y (%) | <0.001 | <0.001 | ||||
| < 1 h/week | 22.1 | 17.3 | 11.9 | 7.6 | ||
| 1-3 h/week | 26.1 | 25.3 | 22.5 | 19.4 | ||
| 4-7 h/week | 24.8 | 27.7 | 27.7 | 28.4 | ||
| > 7 h/week | 27.0 | 29.7 | 38.0 | 44.7 | ||
| MVPA in past 10 y (%) | <0.001 | <0.001 | ||||
| < 1 h/week | 34.2 | 18.7 | 30.6 | 17.0 | ||
| 1-3 h/week | 25.7 | 25.3 | 26.6 | 25.2 | ||
| 4-7 h/week | 21.3 | 28.6 | 22.8 | 29.2 | ||
| > 7 h/week | 18.8 | 27.4 | 20.1 | 28.7 | ||
Data are self-reported from the baseline (1994-1995) questionnaire with the exception of follow-up health status and mobility, which were reported in 2004-2005. Mobility disability was defined as a self-reported walking speed of “unable to walk” or “easy (<2 mph)” at the follow-up. NIH-AARP= National Institutes of Health - American Association of Retired Persons.
Figure 2 –
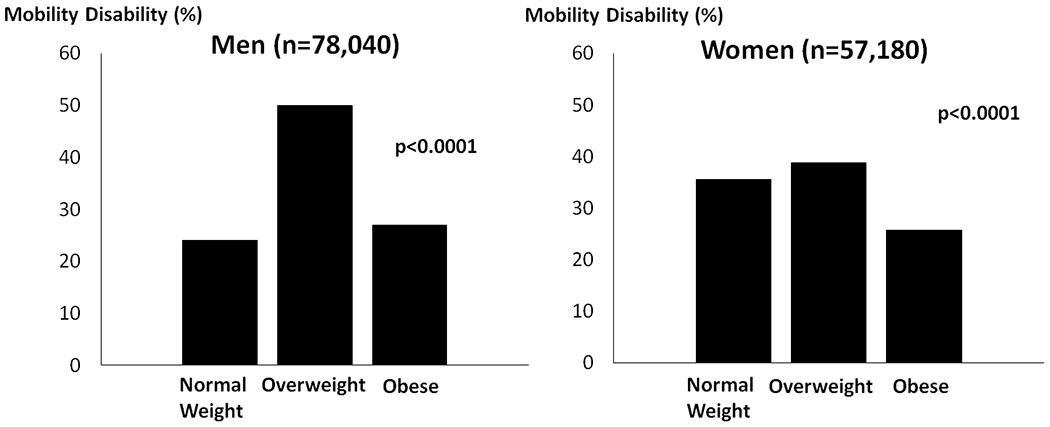
Reported mobility disability at follow-up by sex and weight status in the NIH-AARP Diet and Health Study cohort (N=135 220). Mobility disability was defined as a self-reported walking speed of “unable to walk” or “easy (<2 mph)” at the follow-up. Normal weight = BMI 18-<25 kg/m2; Overweight= BMI 25-<30 kg/m2; Obese= BMI ≥30 kg/m2.
Multivariable parameter estimates for the independent associations of weight status and physical activity with mobility disability are shown in Table 2. After adjustment for light- and moderate-to-vigorous intensity physical activity, TV viewing time, and the other covariables of interest, the odds of mobility disability increased significantly by weight status in a curvilinear manner, and this was especially so among women. Both light- and moderate-to-vigorous physical activity also were significantly associated with mobility disability in the multivariable model, with the odds progressively lower with increasing frequency and intensity of physical activity. Daily TV viewing time of 5 hours or more increased the odds of disability by 44% in men and by about 50% in women (p<0.001). When BMI was substituted for weight status in the modeling, the results indicated that the odds of mobility disability increased by about 9% (OR=1.09; 95%CI: 1.08, 1.10) in men and by 11% (OR=1.11; 95%CI: 1.10, 1.12) per unit increase (kg/m2 or about 6 kg) in BMI. On average, BMI changed very little over the follow-up period (0.09±1.85 kg/m2 and 0.39±2.17 kg/m2 for men and women, respectively). When we repeated the logistic regression analysis with BMI change included in the modeling, the parameter estimates for weight status, and light- and moderate-to-vigorous physical activity were virtually unchanged. Similarly, when the analysis was stratified by age-group (≤60/>60 years), the between-group differences in the sex-specific estimates were negligible, suggesting no effect modification by age.
Table 2. –
Independent associations of baseline weight status and physical activity with mobility disability at follow-up in the NIH-AARP Diet and Health Study cohort.
| Men | Women | |||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Weight status | 1.00 | 1.00 | ||
| Normal weight (BMI 18-<25 kg/m2) | 1.30 | 1.24, 1.36 | 1.58 | 1.52, 1.65 |
| Overweight (BMI 25-<30 kg/m2) | 2.08 | 1.96, 2.20 | 2.63 | 2.49, 2.78 |
| Obese (BMI ≥30 kg/m2) | ||||
| Light physical activity | ||||
| <3 hours/week | 1.00 | 1.00 | ||
| 1-3 hours/week | 0.89 | 0.84, 0.94 | 0.87 | 0.81, 0.94 |
| 4-7 hours/week | 0.83 | 0.78, 0.88 | 0.79 | 0.73, 0.85 |
| >7 hours/week | 0.90 | 0.84, 0.95 | 0.79 | 0.73, 0.85 |
| Moderate/Vigorous physical activity | ||||
| <3 hours/week | 1.00 | 1.00 | ||
| 1-3 hours/week | 0.68 | 0.65, 0.72 | 0.69 | 0.52, 0.58 |
| 4-7 hours/week | 0.53 | 0.50, 0.56 | 0.55 | 0.52, 0.58 |
| >7 hours/week | 0.47 | 0.44, 0.50 | 0.50 | 0.47, 0.53 |
| TV viewing | ||||
| 0-2 hours/day | 1.00 | 1.00 | ||
| 3-4 hours/day | 1.15 | 1.10, 1.2 | 1.22 | 1.17, 1.28 |
| ≥5 hours/day | 1.44 | 1.36, 1.52 | 1.49 | 1.41, 1.57 |
Estimates are based on multivariable logistic regression modeling, with adjustment for age, race, education, baseline smoking, baseline caloric intake, and follow-up health status. For men: normal weight (n=25 157); overweight (n=39,791); and obese (n=13,092). For women: normal weight (n=27 884); overweight (n=19 849); and obese (n=9 447). Odds ratios (OR) and 95% confidence intervals (95%CI) are reported to describe the excess risk of disability for each level of weight status and each level of light- and moderate-to-vigorous intensity physical activity relative to the referent group (normal weight for weight status; <3 h/week for physical activity; and <2 h/day for TV viewing).
The odds ratios for the joint associations of weight status and total physical activity with mobility disability are shown in Figure 3. We observed a dose-response association between increasing categories of weight and mobility disability within each tertile of physical activity, with the highest odds experienced by men and women with obesity. Even in the most active group (those reporting >7 h/week), both men with overweight (OR=1.39; 95% CI: 1.27, 1.53) and with obesity (OR=2.37; 95% CI: 2.11, 2.67) men had a significantly higher odds of mobility disability relative to those of normal weight who were the most active (referent group). In the middle tertile of physical activity (4-7 h/week), men who were normal weight (OR=1.22; 95% CI: 1.11, 1.35), overweight (OR=1.61; 95% CI: 1.48, 1.76) and obese (OR=2.62; 95% CI: 2.37, 2.91) had a slightly greater excess odds of mobility disability compared with their counterparts in the most active group. Among those in the lowest tertile of physical activity (≤3 h/week), however, even men of normal weight nearly doubled their odds of mobility disability (OR=1.95; 95% CI=1.77, 2.15), while men with overweight increased their odds of mobility disability by nearly 2 ½-fold (OR=2.45; 95% CI: 2.25, 2.67), and men with obesity increased their odds nearly 4-fold (OR=3.93; 95% CI: 3.58, 4.33), compared with the referent group. Among women, the results were more striking (Figure 3). Indeed women in the lowest physical activity tertile who were also obese experienced 5 times the odds of disability, compared with women who were normal weight in the most active tertile (OR=5.08; 95% CI: 4.65, 5.54). The statistical interaction between weight status and total physical activity was significant in women (Wald χ2=17.42; df=4; p<0.01) but not in men (Wald χ2=5.00; df=4; p<0.29), indicating a multiplicative burden on mobility disability in older women. These findings were independent of age, race, level of educational attainment, smoking, caloric intake, TV viewing time, and reported health status at follow-up, and were not altered by the addition of BMI change to the multivariable modeling.
Figure 3 –
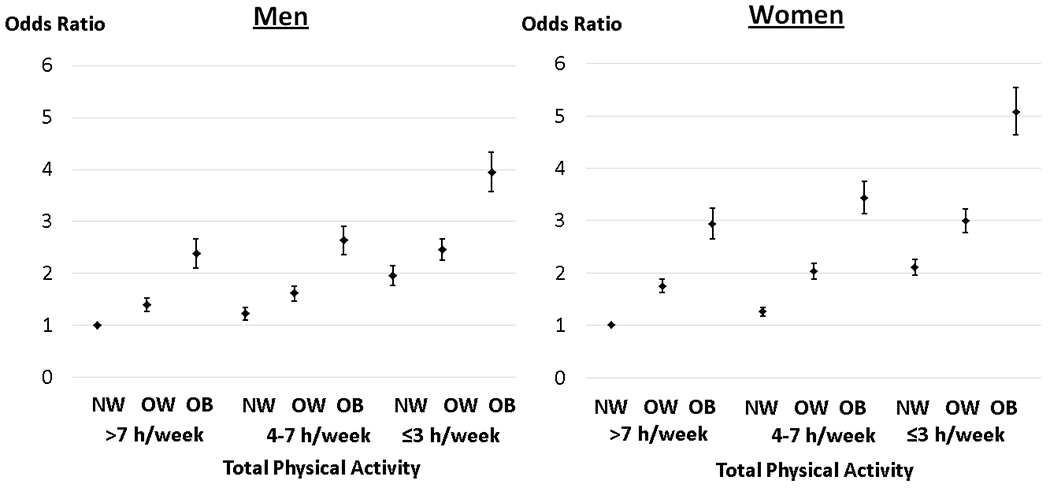
The joint association between weight status and total physical activity (h/week) on mobility disability in the NIH-AARP Diet and Health Study cohort (N=135 220). This joint analysis allowed us to compare directly groups with varying amounts of body mass index and physical activity against those who were of normal weight status (BMI 18-<25 kg/m2) and also had the most physical activity (referent group). Odds ratios (OR) and 95% confidence intervals (CI) are reported from the final logistic regression models to describe the excess odds of mobility disability within each level of weight status and physical activity relative to the referent group. All models were adjusted for age, sex, race, level of educational attainment, smoking, TV viewing, as well as for reported health status at follow-up. NW=normal weight (BMI 18-<25 kg/m2); OW=overweight (BMI 25-<30 kg/m2); OB=obese (BMI ≥30 kg/m2).
Discussion
Our findings indicate that overweight and obesity are potent risk factors for mobility disability in older age that are independent of several important socio-demographic and lifestyle related (i.e., total physical activity, TV viewing, smoking, caloric intake) factors. Moreover, the combination of overweight and obesity with low levels of total physical activity is especially deleterious for mobility loss. In both men and women, the odds of mobility disability increased in a curvilinear dose-response manner within all three tertiles of physical activity – with an accelerated increase among men and women with obesity who were the least active. In addition, being of normal body weight did not completely eliminate the excess risk of disability when total physical activity levels were ≤7 hours/week, suggesting the potential importance of an active lifestyle to health and function across the body weight spectrum.
Our findings are consistent with those of others in that we observed a greater burden of mobility disability among women and those of lower educational attainment.1–3 We also observed that the associations between overweight and obesity with mobility disability were stronger in older women, compared with men, which is also corroborated by data from several other studies.17–19 Similar to our findings, Brach, et al.,7 reported data indicating that older women who were never active in combination with being overweight or obese experienced the greatest disability in gait speed over 14-years; however, this effect was attenuated in women with overweight and obesity who were physically active. Studies that have examined muscle strength (rather than physical activity) and weight status in relation to mobility disability report that both low muscle strength and obesity are powerful predictors of a decline in gait speed and an increase in risk of mobility disability, 6, 12 while the combination of these two risk factors was exponentially deleterious.12 Sex-differences in the aging-related loss of muscle mass and lower-body muscle strength may partially explain our observation that the combination of greater body weight with low physical activity carries a multiplicative burden for women in older age. Unfortunately, data on muscle mass and strength were not collected from the NIH-AARP cohort and therefore, we were not able to determine whether or not this was so.
Some excess weight may be beneficial in older age; however, contrary to other studies 2,4,6, 20–26, our data and those of others7 indicate that being overweight or obese was not protective against mobility disability. Since mobility is characterized by the ability to generate a moderate walking speed and to lift the center of gravity,27 our finding of a lower BMI risk threshold may be that a mobility task such as gait speed is compromised more by excess weight, compared with many of the general tasks associated with overall functional ability. Indeed, Rejeski and colleagues argue that failure at mobility-related tasks will precede a loss of function with activities of daily living (ADLs) in older people.28
People who have been physically active throughout adulthood experience a lower risk of mobility disability in older age, compared with their less active counterparts.11, 29 Despite the known benefits of regular physical activity to physical function and mobility, however, the amount of physical activity that is necessary to mitigate the excess risk of mobility disability with overweight and obesity is not clear. Recent data from the Lifestyle Interventions and Independence for Elders (LIFE) Study randomized trial indicate that the 2-year change in objectively-measured physical activity had a significant dose-response relation to mobility and physical function at follow-up (independent of BMI) in older people at risk for mobility loss.30 In fact, small increases in activity over 24 months (48 min/week) had clinically relevant effects. When the LIFE Study data were stratified by weight status,10 the effect of the physical activity (relative to the health education) intervention on mobility disability was stronger in those having a BMI ≥30 kg/m2 [hazard ratio (HR)=0.77; 95% CI: 0.60, 0.99] compared with those who did not (HR=0.88; 95% CI:0.68, 1.13), and the strongest effects were observed among persons with class II obesity or more [BMI ≥35 kg/m2 (HR=0.69; 95% CI: 0.48, 0.98)]. The authors propose that the larger intervention effects in those with the greatest level of obesity are attributable to greater between-group differences in self-reported physical activity at 6-months (30 min/week in the health education group vs. 135 min/week in the physical activity group).
In other studies, Bruce and colleagues9 reported that vigorous physical activity performed for more than 60 min/week minimized the risk of disability (assessed using the Stanford HAQ Disability Index31) in healthy, overweight older people over a 13-year follow-up period. Similarly, prospective data from the Health ABC Study indicate that the 6.5-year risk of mobility limitations was attenuated in obese older people who reported performing high levels of physical activity (>106.5 kcal/kg/week) in the prior 7 days; however, this was not the case in those reporting moderate or low levels of activity.8 We report that total reported physical activity (light- and moderate-to-vigorous intensity) performed for 7 or fewer hours/week over the previous 10 years was not sufficient to eliminate the excess odds of mobility disability, even among older people of normal body weight.
We note the limitations to our analysis. Our findings are based on only 24% of the original NIH-AARP cohort and 94% of this sample was white, of higher educational attainment, and relatively healthy, thereby limiting the generalizability of the findings to those older survivors who completed the follow-up survey. We performed a sensitivity analysis in which we compared estimates for the primary study variables (physical activity and BMI) between the analytic sample and the entire baseline cohort (Supplemental Table 1). The findings indicated that there were no meaningful differences in these variables between those who were included in the final analysis and those who were not. All information on body weight, physical activity, and mobility disability was self-reported. People tend to under-report their weight32 and over-report their physical activity;33 however, in this prospective study where our exposure measures preceded our outcome assessment we expect the misclassification of body weight and physical activity to be non-differential by mobility disability status, thus attenuating our findings toward the null. Finally, scores for the frequency of light- and moderate-to-vigorous physical activity were added together to create a summary index ranging from 0-6. Similar to other composite scores (e.g., MET-h/week) it therefore was not possible to discern the distinct contributions of light-, moderate-, or vigorous intensity to a given summary score.
Mobility disability status was not assessed by the baseline risk factor questionnaire, and even though we restricted the analysis to those without chronic disease and who reported their health as fair or better, we may have missed some prevalent cases of mobility disability at baseline. We therefore performed a second sensitivity analysis in which we excluded those participants who reported a baseline health status of fair, as well as of poor, and the results were essentially unchanged from the original analysis (Supplemental Table 2). Also, the question assessing mobility was based on perceived usual walking pace and may have lacked accuracy. Moreover, we were not able to account for factors that may influence walking speed, such as a previous injury, medications causing dizziness, or fear of falling. The Walking Impairment Questionnaire (WIQ)34 was developed as a measure of self-perceived walking performance and contains questions about walking speed similar to ours that have correlated significantly with timed walking speed.
We note that our analysis is very similar to one that we published previously, which described the joint associations of sedentary behavior and physical activity with mobility disability in this same cohort.35 We acknowledge that in general, sedentary behavior and body weight are strongly correlated. These current findings, however, are distinct from our previous ones in that they describe the excess risk of mobility disability for specific categories of weight status in combination with decreasing levels of physical activity, rather than simply adjusting for body mass index in the analysis. Moreover, the current findings are presented separately for men and women and highlight the multiplicative burden of obesity and low physical activity in women, but not in men.
In sum, our findings and those of others indicate that even among healthy older people, obesity prevention, as well as physical activity promotion are necessary to maintain health and function in older age –particularly among women. Given aging demographics and the global economic burden associated with aging- and disuse-related disability, there is tremendous public health benefit to understanding how various modifiable determinants of mobility disability can interact in older age.
Supplementary Material
Acknowledgements
All persons who contributed significantly to this manuscript have been listed as authors. We are grateful to the participants in the NIH-AARP Diet and Health Study for their outstanding cooperation. This work was supported, in part, by the Intramural Research Program of the US National Institutes of Health, National Cancer Institute.
Footnotes
Competing Interests
The authors have no financial or personal conflicts of interest to report.
References
- 1.Morbidity and Mortality Weekly Report (MMWR). Prevalence of Disability and Disability Type among Adults — United States, 2013. July31, 2015. / 64(29);777–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Health Statistics. Health, United States, 2014: with special feature on adults aged 55–64. Hyattsville, MD: National Center for Health Statistics, CDC; 2015. Available at http://www.cdc.gov/nchs/data/hus/hus14.pdf. [PubMed] [Google Scholar]
- 3.Brault MW. Americans with disabilities: 2010. Washington, DC: Census Bureau; 2012. Current Population Report P70–131. Available at http://www.census.gov/prod/2012pubs/p70-131.pdf. [Google Scholar]
- 4.Vincent HK, Vincent KR, and Lamb KM. Obesity and mobility disability in the older adult. Obesity Reviews 2010; 11: 568–579. [DOI] [PubMed] [Google Scholar]
- 5.Rajeski WJ, Marsh AP, Chmelo E, and Rejeski JJ. Obesity, intentional weight loss and physical disability in older adults. Obesity Reviews 201011:671–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marsh AP, Rejeski WJ, Espeland MA, et al. , Muscle strength and BMI as predictors of major mobility disability in the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P). J Gerontol. Med Sci 2011; 66A: 1376–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brach JS, VanSwearingen JM, FitzGerald SJ, Sorti KL, Kriska AM. The relationship among physical activity, obesity, and physical function in community-dwelling older women. Prev Med 2004; 39:74–80. [DOI] [PubMed] [Google Scholar]
- 8.Koster A, Patel KV, Visser M, van Eijk JTM, Kanaya AM, de Rekeneire N, Newman AB, Tylavsky FA, Kritchevsky SB, and Harris TB. Joint effects of adiposity and physical activity on incident mobility limitations in older adults. J Am Geriatr Soc 2008; 56: 636–643. [DOI] [PubMed] [Google Scholar]
- 9.Bruce B, Fries JF, and Hubert H. Regular vigorous physical activity and disability development in healthy overweight and normal weight seniors: a 13-year study. Am J Public Health 2008; 168:284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kritchevsky SB, Lovato L, Handing EP, Blair S, Botoseneanu A, Guralnik JM, et al. Exercise’s effects on mobility disability in older adults with and without obesity: The LIFE Study Randomized Clinical Trial. Obesity 2017; 25:1199–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stenholm S, Koster A, Valkeinen H, Patel KV, Bandinelli S, Guralnik JM, and Ferrucci L. Association of physical activity history with physical function and mortality in old age. J Gerontol: Med Sci 2016; 71:496–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stenholm S, Ally D, Bandinelli S, Griswold ME, Koskinen S, Rantanen T, Guralnik JM, and Ferrucci L. The effect of obesity combined with low muscle strength on decline in mobility in older persons: results from the InCHIANTI Study. International Journal of Obesity 2009; 33:635–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schatzkin A, Subar AF, Thompson FE, et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions: The National Institutes of Health-American Association of Retired Persons diet and health study. Am J Epidemiol. 2001; 154:1119–1125. doi: 10.1093/aje/154.12.1119. [DOI] [PubMed] [Google Scholar]
- 14.Gierach GL, Chang SC, Brinton LA, et al. Physical activity, sedentary behavior, and endometrial cancer risk in the NIH-AARP Diet and Health Study. Int J Cancer. 2009; 124:2139–2147. doi: 10.1002/ijc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howard RA, Freedman DM, Park Y, et al. Physical activity, sedentary behavior, and the risk of colon and rectal cancer in the NIH-AARP Diet and Health Study. Cancer Causes Control. 2008; 19:939–953. doi: 10.1007/s10552-008-9159-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arem H, Pfeiffer RM, Engels EA, Alfano CM, Hollenbeck A, Park Y, and Matthews CE. Pre- and Post-diagnosis Physical Activity, Television Viewing, and Mortality among Patients with Colorectal Cancer in the National Institutes of Health–AARP Diet and Health Study. J Clin Oncol. 2014; 33:180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wray LA, Blaum CS. Explaining the role of sex on disability: a population-based study. Gerontologist 2001; 41:499–510. [DOI] [PubMed] [Google Scholar]
- 18.Reynolds SL, Saito Y, Crimmons EM. The impact of obesity on active life expectancy in older American men and women. Gerontologist 2005; 45:438–444. [DOI] [PubMed] [Google Scholar]
- 19.Friedmann JM, Elasy T, Jensen GL. The relationship between body mass index and self-reported functional limitation among older adults: a gender difference. J Am Geriatr Soc 2001; 44:206–216. [DOI] [PubMed] [Google Scholar]
- 20.Ferraro KF, Booth TL. Age, body mass index, and functional illness. J Gerontol B Psychol Sci Soc Sci 1999; 54:S339–S348. [DOI] [PubMed] [Google Scholar]
- 21.Al Snih S, Ottenbacher KJ,Markides KS, Kuo YF, Eschbach K, Goodwin JS. The effect of obesity on disability vs mortality in older Americans. Arch Intern Med 2007; 167:774–780. [DOI] [PubMed] [Google Scholar]
- 22.Mendes de Leon CF, Hansberry MR, Bienias JL, Morris MC, Evans DA. Relative weight and mobility: a longitudinal study in a biracial population of older adults. Ann Epidemiol 2006; 16:770–776. [DOI] [PubMed] [Google Scholar]
- 23.Galanos AN, Pieper CF, Cornoni-Huntley JC, Bales CW,Fillenbaum GG. Nutrition and function: is there a relationship between body mass index and the functional capabilities of community-dwelling elderly? J Am Geriatr Soc 1994; 42:368–373. [DOI] [PubMed] [Google Scholar]
- 24.Chen H, Guo X. Obesity and functional disability in elderly Americans. J Am Geriatr Soc 2008; 56:689–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jensen GL, Friedmann JM. Obesity is associated with functional decline in community-dwelling rural older persons. J Am Geriatr Soc 2002; 50:918–923. [DOI] [PubMed] [Google Scholar]
- 26.Jensen GL, Silver HJ, Roy MA, Callahan E. Still C, Dupont W. Obesity is a risk factor for reporting homebound status among community-dwelling older persons. Obesity (Silver Spring) 2006; 14:509–517. [DOI] [PubMed] [Google Scholar]
- 27.Zoico E, DiFrancesco V, Mazzali G, Zivelonghi A, Volpato S, Bortolani A, et al. High baseline values of fat mass, independently of appendicular skeletal mass, predict 2-year onset of disability in elderly subjects at the high end of the functional spectrum. Aging Clin Exp Res 2007; 19:154–159. [DOI] [PubMed] [Google Scholar]
- 28.Rejeski WJ, Ip EH, Marsh AP, Zhang Q, Miller ME. Obesity influences translational states of disability in older adults with knee pain. Arch Phys Med Rehabil 2008; 89:2102–2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stenholm S, Sainio P, Rantanen T, Koskinen S, Jula A, Heliovaara M, Aromaa A. High body mass index and physical impaiments as predictors of walking limitation 22 years later in adult Finns. Int J Obes 2007; 62:859–865. [DOI] [PubMed] [Google Scholar]
- 30.Fielding RA, Guralnik JM, King AC, Pahor M, McDermott MM, Tudor-Locke C, et al. Dose of physical activity, physical functioning, and disability risk in mobility-limited older adults: Results from the LIFE study randomized trial. PLOS ONE 12:e0182155. 10.1371/journal.pone.0182155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: a review of its history, issues, progress, and documentation. J Rheumatol 2003; 30:167–178. [PubMed] [Google Scholar]
- 32.Kyulo NL1, Knutsen SF, Tonstad S, Fraser GE, Singh PN. Validation of recall of body weight over a 26-year period in cohort members of the Adventist Health Study 2. Ann Epidemiol. 2012October;22(10):744–6. doi: 10.1016/j.annepidem.2012.06.106. Epub 2012 Aug 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71:S1–14. doi: 10.1080/02701367.2000.11082780. [DOI] [PubMed] [Google Scholar]
- 34.McGrae McDermott M, Liu K, Guralnik JM, Martin GJ, Criqui MH, and Greenland P. Measurement of walking endurance and walking velocity with questionnaire: validation of the walking impairment questionnaire in men and women with peripheral arterial disease. J Vasc Surg. 1998;28:1072–81. 10.1016/S0741-5214(98)70034-5. [DOI] [PubMed] [Google Scholar]
- 35.DiPietro L, Jin Y, Talegawkar S, and Matthews CE. The joint associations of sedentary time and physical activity on mobility disability in older people. The NIH-AARP Diet and Health Study. J Gerontol A Biol Sci Med Sci, 2017, Vol. 00, No. 00, 1–7. doi: 10.1093/gerona/glx122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


