Abstract
Gorlin–Goltz syndrome (GGS) is a rare autosomal dominant disorder with multisystemic involvement. It is characterized by the triad of multiple baso-cellular epitheliomas, odontogenic keratocysts (OKC) in the jaws and skeletal anomalies. Later, it was found that calcification of falx is also highly specific. We present radiological findings in case series of two cases, one with multiple OKC, calcified falx, skin lesions, and fibrous dysplasia of sphenoid and second with multiple OKC, calcified falx, vertebral anomaly and medulloblastoma.
Keywords: Gorlin-Goltz syndrome, noncontrast computerized tomography, odontogenic keratocysts
BACKGROUND
Gorlin-Goltz syndrome (GGS) is a rare genetic disorder that was defined by Gorlin and Goltz in 1960 with a classical triad of odontogenic keratocysts (OKC), Multiple basal cell nevi and skeletal anomalies.[1,2,3] It has high penetrance with a variety of dermatologic or radiologic findings along with various types of neoplasms.[4,5]
GGS is a rare disorder with the autosomal dominant inheritance that occurs due to mutation of tumor suppressor gene PTCH-1 located in the long arm of the chromosome 9q22.3-q31.[6] The prevalence of GGS is about 1/60,000[7] with equal affliction for males and females.[8] It is usually diagnosed in the second or third decades. Patients suffer significant morbidity from complications.
Kimonis et al. proposed that Gorlin's syndrome can be diagnosed when 2 major or 1 major and 2 minor criteria are present.[9]
Major criteria
Two or more basal cell carcinomas or one in persons younger than 20 years
Histologically proven OKC of the jaw
Three or more palmar or plantar pits
Bilamellar calcification of the falx cerebri
Bifid, fused, or markedly splayed ribs
First-degree relative with Gorlin syndrome.
Minor criteria
Macrocephaly
Congenital malformations (cleft lip or palate, frontal bossing, coarse face, hypertelorism)
Other skeletal abnormalities (Sprengel deformity, marked pectus deformity, or syndactyly of the digits)
Radiologic abnormalities (bridging of the sella turcica, vertebral anomalies like hemivertebrae, fusion or elongation of the vertebral bodies, modeling defects of the hands and feet, or flame-shaped lucencies of the hands or feet)
Ovarian/cardiac fibroma.
We present radiological findings in two cases of GGS.
CASES
Case 1
A 13-year-old boy with multiple macular lesions on the face along with jaw swelling, prognathism, frontal bossing and exophthalmos presents to the out-patient department of dental college. The patient had multiple ulcerated lesions on the chest and back. There was a family history of similar complaints in the father but was not evaluated. Noncontrast computerized tomography (NCCT) of head and brain is advised which reveals evidence of two radiolucent lesions along with unerupted tooth in the mandible [Figure 1] and single para-midline radiolucent lesion in the maxilla [Figure 2] consistent with OKCs. There was evidence of calcified falx [Figure 3] and tentorium cerebelli. There was evidence of ground glassing and expansion of greater wings of sphenoid supporting Fibrous Dysplasia [Figure 4]. Genetic analysis revealed mutation in the PTCH-1 gene consistent with GGS. Histological analysis of ulcerated lesions revealed basal cell carcinoma [Figure 5].
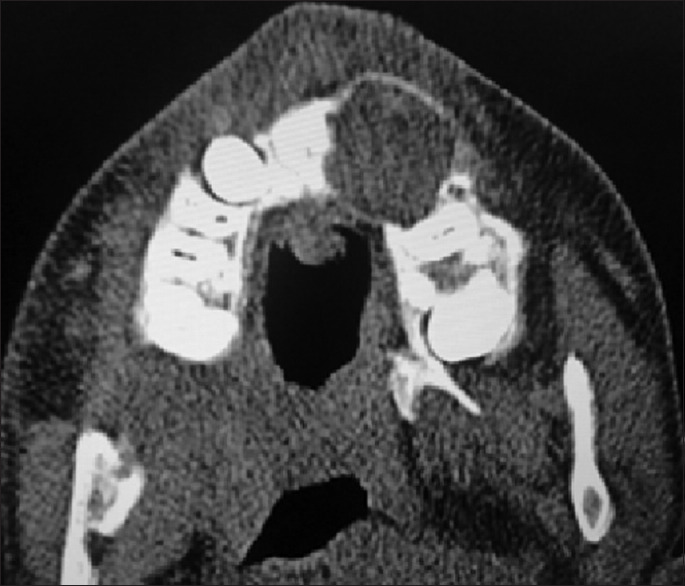
Figure 1.

Axial computerized tomography image revealing evidence of two radiolucent lesions with associated unerupted tooth involving mandible anteriorly
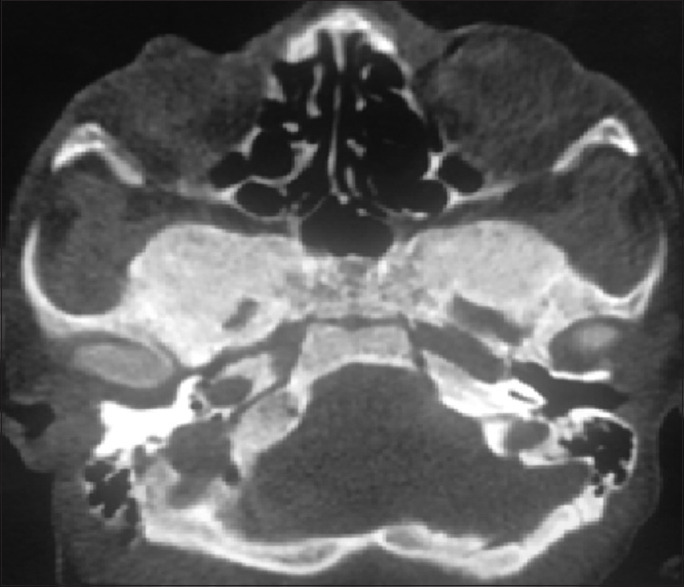
Figure 2.
Axial computerized tomography image revealing evidence of radiolucent lesion in the maxilla
Figure 3.

Coronal computerized tomography image revealing calcified falx
Figure 4.
Axial computerized tomography image revealing evidence of ground glassing and expansion of greater wings of sphenoid
Figure 5.
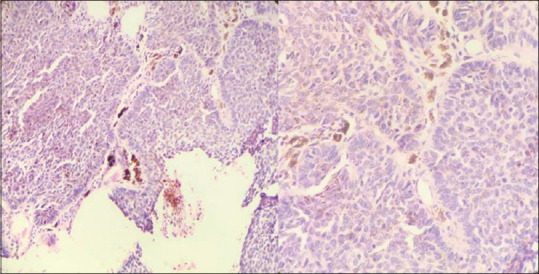
Hematoxylin and eosin stained histopathological images (×20 and ×40) Showing nests of basaloid cells with peripheral palisading with retraction artifact suggestive of Basal cell carcinoma with areas of intracytoplasmic and extracellular melanin pigment
Case 2
A 19-year-old boy with a history of long-standing jaw swelling presents to pediatric clinic with vomiting, strabismus and headache. Physical examination reveals evidence of pectus excavatum and macrocephaly. There was no visible skin lesion. He was stabilized with antiemetics and analgesics. Previous records in form of orthopantomogram reveal evidence of two radiolucent lesions with the associated unerupted tooth in the mandible [Figure 6]. Emergency NCCT of the head is advised. CT reveals evidence of hyperdense mass in the left cerebellar hemisphere and calcified falx. She is advised to undergo magnetic resonance imaging (MRI) for the characterization of the cerebellar lesion. MRI reveals evidence of T1 hypointense, T2/fluid-attenuated inversion recovery heterogeneous mass [Figure 7] with diffusion restriction and post contrast enhancement [Figure 8] centered upon middle cerebellar peduncle and left cerebellar hemisphere with mild compression effect on the fourth ventricle and mild lateral ventriculomegaly consistent with medulloblastoma. NCCT of the chest which was done in view of pectus carinatum revealed evidence of butterfly thoracic vertebra [Figure 9]. Enucleation of radiolucent mandible lesion was done and histopathology revealed odontogenic keratocyst [Figure 10]. In view of the association of lytic mandible lesions, medulloblastoma, calcified falx, vertebral anomaly in form of butterfly vertebra along with pectus excavatum, and enlarged head size provisional diagnosis of GGS was made. The diagnosis was finally confirmed by genetic analysis.
Figure 6.

Orthopantomogram revealing evidence of two radiolucent lesions near angle of mandible with associated unerupted tooth
Figure 7.

Axial space magnetic resonance imaging image revealing evidence of heterogeneous hyperintense lesion centered on left cerebellar hemisphere with mild compression effect on fourth ventricle
Figure 8.
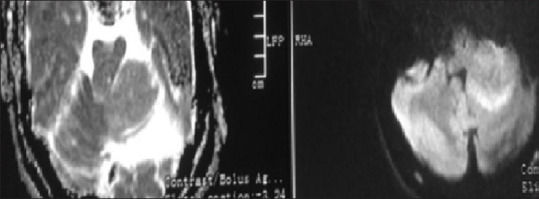
Apparent diffusion and diffusion-weighted magnetic resonance images revealing evidence of diffusion restriction in lesion
Figure 9.
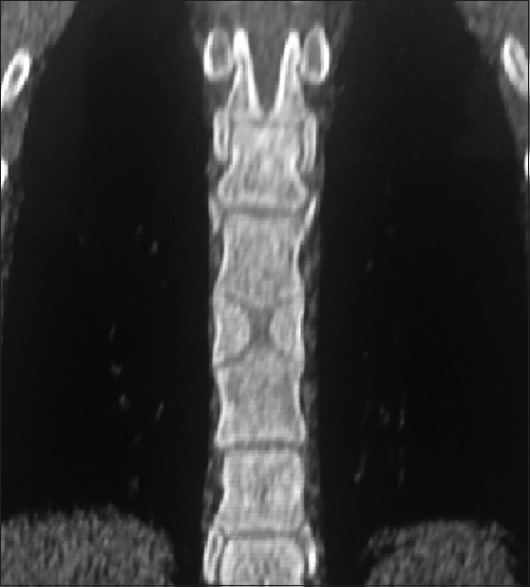
Coronal computerized tomography image revealing evidence of butterfly vertebra
Figure 10.
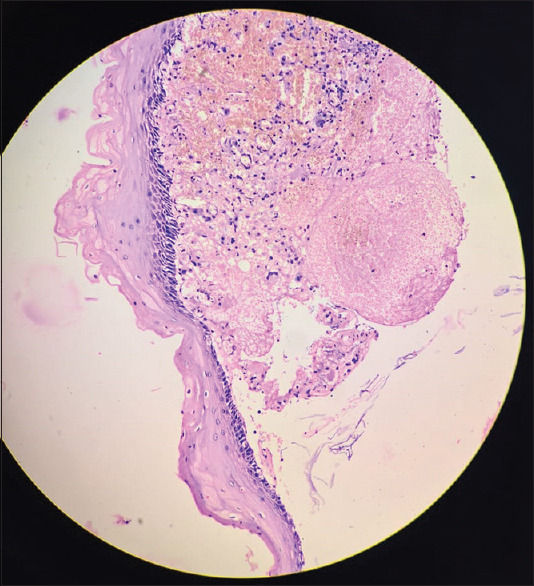
Histomicroscopic photograph showing parakeratotic corrugated luminal surface with palisaded hyperchromatic basal cell layer consistent with odontogenic keratocyst
DISCUSSION
GGS was first reported by Jarish in 1894.[10] The syndrome has been designated by a variety of different terms including Gorlin syndrome, nevoid basal cell carcinoma syndrome, basal cell nevus syndrome, syndrome of jaw cysts and jaw cyst-basal cell nevus-bifid rib syndrome.[11,12,13,14,15] There have been case reports of Gorlin Goltz with fibrous dysplasia earlier also.[16] After typical clinical and radiological features of GGS final diagnosis was confirmed by genetic mutation analysis.
In case no. 2, presence of mandibular radiolucent lesions with the associated unerupted tooth, calcified falx, medulloblastoma and vertebral anomaly in form of butterfly vertebra, diagnosis of GGS was made. Later, enucleation of the radiolucent lesion revealed OKC. 5%–10% of the patients may develop brain medulloblastoma, a potential cause of early death, thus requiring intervention by a neurologist.
Learning points
Proper knowledge of different Radiological findings in GGS can help in earlier diagnosis of this syndrome
Sometimes, syndrome can present without classical features.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initial s will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gorlin RJ, Goltz RW. Multiple nevoid basal-cell epithelioma, jaw cysts and bifid rib. A syndrome. N Engl J Med. 1960;262:908–12. doi: 10.1056/NEJM196005052621803. [DOI] [PubMed] [Google Scholar]
- 2.Manfredi M, Vescovi P, Bonanini M, Porter S. Nevoid basal cell carcinoma syndrome: A review of the literature. Int J Oral Maxillofac Surg. 2004;33:117–24. doi: 10.1054/ijom.2003.0435. [DOI] [PubMed] [Google Scholar]
- 3.Casaroto AR, Loures DC, Moreschi E, Veltrini VC, Trento CL, Gottardo VD, et al. Early diagnosis of Gorlin-Goltz syndrome: Case report. Head Face Med. 2011;7:2. doi: 10.1186/1746-160X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snoeckx A, Vanhoenacker FM, Verhaert K, Chappelle K, Parizel PM. Gorlin-Goltz syndrome in a child: Case report and clinical review. JBR-BTR. 2008;91:235–9. [PubMed] [Google Scholar]
- 5.Daneswari M, Reddy MS. Genetic mutations in Gorlin-Goltz syndrome. Indian J Hum Genet. 2013;19:369–72. doi: 10.4103/0971-6866.120810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsuzawa N, Nagao T, Shimozato K, Niikawa N, Yoshiura KI. Patched homologue 1 mutations in four Japanese families with basal cell nevus syndrome. J Clin Pathol. 2006;59:1084–6. doi: 10.1136/jcp.2005.029439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee BD, Kim JH, Choi DH, Koh KS, Lee SR. Recurrent odontogenic keratocysts in basal cell nevus syndrome: Report of a case. Korean J Oral Maxillofac Radiol. 2004;34:203–7. [Google Scholar]
- 8.Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, DiGiovanna JJ, et al. Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet. 1997;69:299–308. [PubMed] [Google Scholar]
- 9.Kimonis VE, Mehta SG, Digiovanna JJ, Bale SJ, Pastakia B. Radiological features in 82 patients with nevoid basal cell carcinoma (NBCC or Gorlin) syndrome. Genet Med. 2004;6:495–502. doi: 10.1097/01.gim.0000145045.17711.1c. [DOI] [PubMed] [Google Scholar]
- 10.Jarish W. Zur lehre von den autgeschwulsten. Arch Jur Dermatol Syphilogic. 1894;28:163–222. [Google Scholar]
- 11.Markt JC. Implant prosthodontic rehabilitation of a patient with nevoid basal cell carcinoma syndrome: A clinical report. J Prosthet Dent. 2003;89:436–42. doi: 10.1016/s0022-3913(03)00072-6. [DOI] [PubMed] [Google Scholar]
- 12.Honavar SG, Shields JA, Shields CL, Eagle RC, Jr, Demirci H, Mahmood EZ. Basal cell carcinoma of the eyelid associated with Gorlin-Goltz syndrome. Ophthalmology. 2001;108:1115–23. doi: 10.1016/s0161-6420(01)00560-7. [DOI] [PubMed] [Google Scholar]
- 13.Doede T, Seidel J, Riede FT, Vogt L, Mohr FW, Schier F. Occult, life-threatening, cardial tumor in syndactylism in Gorlin Goltz syndrome. J Pediatr Surg. 2004;39:e17–9. doi: 10.1016/j.jpedsurg.2004.06.042. [DOI] [PubMed] [Google Scholar]
- 14.Deepa MS, Paul R, Balan A. Gorlin Goltz syndrome: A review. J Indian Acad Oral Med Radiol. 2003;15:203–9. [Google Scholar]
- 15.Gorlin RJ, Cohen MM, Levin LS. Syndromes of the Head and Neck. 3rd ed. New York: Oxford University Press; 1990. pp. 372–8. [Google Scholar]
- 16.Pandeshwar P, Jayanthi K, Mahesh D. Hindawi Publishing Corporation Case Reports in Dentistry. 2012:4. doi: 10.1155/2012/247239. doi: 10.1155/2012/247239. Article ID 247239. [DOI] [PMC free article] [PubMed] [Google Scholar]


