Abstract
The search for effective COVID-19 management strategies continues to evolve. Current understanding of SARS-CoV-2 mechanisms suggests a central role for exaggerated activation of the innate immune system as an important contributor to COVID-19 adverse outcomes. The actions of colchicine, one of the oldest anti-inflammatory therapeutics, target multiple mechanisms associated with COVID-19 excessive inflammation. While many COVID-19 trials have sought to manipulate SARS-CoV-2 or dampen the inflammatory response once patients are hospitalised, few examine therapeutics to prevent the need for hospitalisation. Colchicine is easily administered, generally well tolerated and inexpensive, and holds particular promise to reduce the risk of hospitalisation and mortality due to COVID-19 in the outpatient setting. Successful outpatient treatment of COVID-19 could greatly reduce morbidity, mortality and the demand for rare or expensive care resources (front-line healthcare workers, hospital beds, ventilators, biological therapies), to the benefit of both resource-replete and resource-poor regions.
INTRODUCTION
As of 27 October 2020, almost 1 year after the first reported cases, the SARS-CoV-2 had resulted in over 43 million people infected and over 1.1 million deaths from COVID-19 worldwide.1 Clinical experience and data underline the role of excessive inflammation in the pathophysiology of the disease and suggest a potential role for colchicine, a drug with pleiotropic effects.
BIOLOGY OF COVID-19: THE ROLE OF INFLAMMATION
COVID-19 progression can be divided into three distinct phases (figure 1) including: (1) early infection phase, wherein the virus infiltrates host cells in the lung parenchyma; (2) pulmonary phase, in which viral propagation causes lung tissue injury as the host immune response is activated and (3) the inflammatory cascade, which is triggered by pathogen-associated molecular patterns (ie, viral RNA) and damage-associated molecular patterns (DAMPs, ie, cellular debris released during pyroptosis) exposed during active viral replication and release. This third phase of the inflammatory cascade may occur even as viral titers are falling and is comprised of components targeted by colchicine (activation of the inflammasome that drives the cytokine storm, activation of neutrophils and the neutrophil/thrombosis interface)2 (figure 2).
Figure 1.
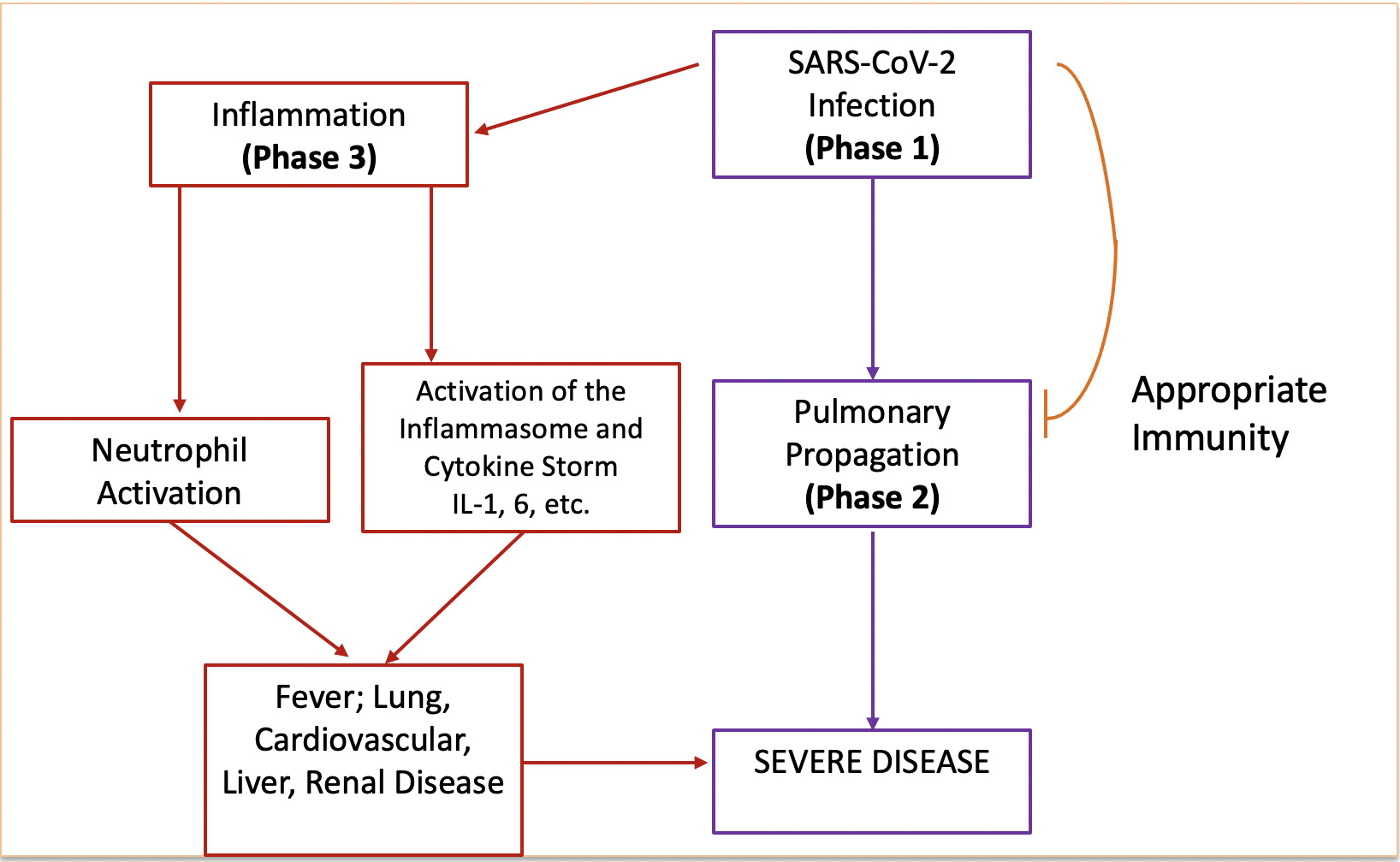
Model of COVID-19 severity. IL, interleukin.
Figure 2.
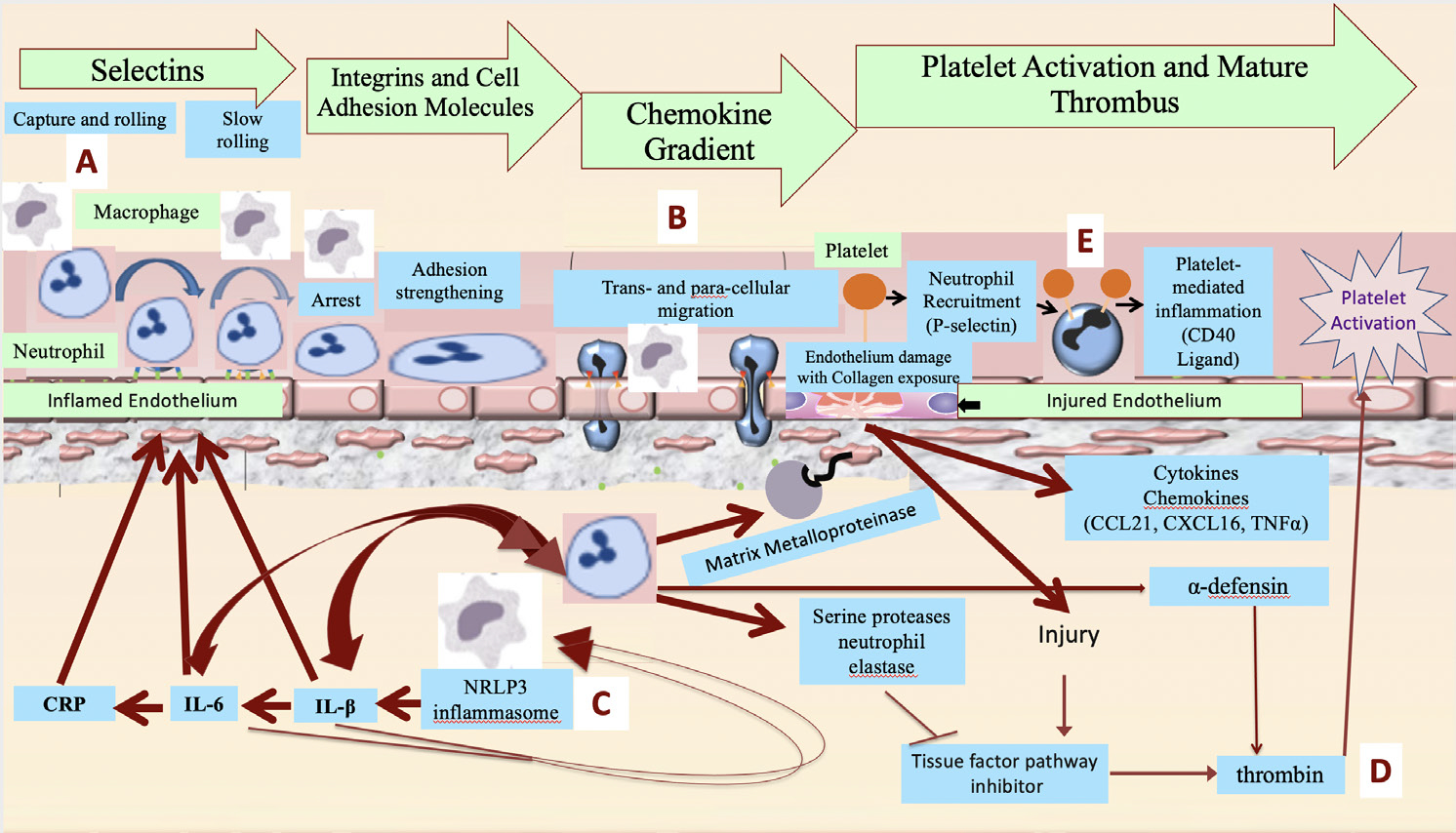
Proposed pathophysiology of acute vascular inflammation in SARS-CoV-2 viral illness and potential therapeutic targets of colchicine. (A) Macrophage-driven inflammation leads to inflammasome activity, cytokine production and endothelial and neutrophil activation, with surface expression of selectins, integrins and intercellular adhesion molecules promoting neutrophil adhesion to the vasculature. Colchicine inhibits E-selectin and L-selectin expression on neutrophil and endothelial surfaces. (B) Neutrophils migrate through the endothelium following chemoattractant gradients. Colchicine impairs the rheologic properties of the neutrophil cytoskeleton, limiting theirability to transmigrate. (C) Inflammasome-generated cytokines, including IL-1β and IL-6, drive additional macrophage activation and cytokine production, in an accelerating pattern known as a cytokine storm. Colchicine inhibits the NLRP3 inflammasome, with the potential to prevent the development of cytokine storm. (D) Neutrophil activation releases neutrophil elastase, which inhibits tissue factor pathway inhibitor. Diminished tissue factor pathway inhibitor activity, along with endothelial injury, promote thrombin generation and platelet activation. In addition, neutrophils release α-defensin, associated with larger and more extensive thrombi. Colchicine inhibits neutrophil elastase and α-defensin release. (E) Neutrophils interact with platelets to form aggregates that are a feature of thrombosis. Colchicine decreases neutrophil-platelet aggregation. CRP, C reactive protein; IL, interleukin; NLRP3, nod-like receptor protein 3; TNF, tumour necrosis factor.
Activation of the inflammasome
Signals driven by SARS-CoV-2 act on macrophages and other myeloid cells to drive assembly of a proinflammatory protein complex, the nod-like receptor protein 3 (NLRP3) inflammasome,3 composed of NLRP3, apoptosis-associated speck-like protein adaptor and cysteine-dependent aspartate-directed protease-1 (caspase-1).4 Activated caspase-1 activity then converts the precursors pro-interleukin (IL)-1β and pro-IL-18 to their active forms. Additionally, caspase-1 activates Gasdermin-D, forming pores in the cell membrane permitting large-scale secretion of IL-1β that, among other actions, induces macrophages to release large quantities of additional pro-inflammatory cytokines.5,6 IL-1β, tumour necrosis factor (TNF) and ligation of toll-like receptors activate NF-κB3 and further upregulate the inflammasome. IL-1β and other cytokines additionally recruit large numbers of leukocytes from the marrow, which in turn undergo activation and cytokine production in an accelerating spiral. In the related SARS-CoV-1, a small envelope (E) protein augments this reaction by self-assembling into an ion channel within the host cell membrane, causing calcium dysregulation that promotes further assembly and activation of the NLRP3 inflammasome.7 More study is needed to determine if the E protein of SARS-CoV-2 has a similar effect on the inflammasome.
The production of IL-1β drives the synthesis of IL-6, a cytokine that induces C reactive protein (CRP) and has been especially implicated as a major proinflammatory agent in the COVID-19 cytokine storm.8–11
Activation of neutrophils
Cytokines including IL-1β and IL-6 prime neutrophils for activation by chemoattractants and upregulate intercellular adhesion molecules on endothelial cells. The resulting neutrophil adhesion to the vasculature promotes neutrophil diapedesis and infiltration into the affected tissues—in COVID-19 infection, initially into lung parenchyma, but later into other organs. Once neutrophils migrate to sites of inflamed tissue, they degranulate and release proinflammatory cytokines and chemokines, proteases, antiviral proteins and toxic oxygen radicals. In the myocardium, neutrophils -play a prominent role in the development of myocarditis and cardiogenic shock.12–14
Neutrophil/thrombosis interface
Neutrophils trigger a cascade of events in arteries that promote plaque destabilisation/rupture and thrombosis.15–18 Neutrophils release the serine protease neutrophil elastase, which inhibits tissue factor pathway inhibitor and leads to generation of thrombin, the most potent activator of platelets. Neutrophil extracellular traps provide a platform to activate coagulation via active neutrophil elastase adherent to extracellular neutrophil DNA.19,20 Activated neutrophils and other leukocytes also aggregate with platelets directly to further exacerbate inflammothrombosis.21–23,24 In the setting of extreme inflammatory states, activated neutrophils adhere directly to each other (leukoaggregation), producing effective but usually transient vascular occlusions.25 Finally, neutrophils contribute to thrombosis via cytokine-induced release of α-defensin from neutrophil granules.26,27 Murine studies suggest that α-defensin, at concentrations similar to those observed in inflammatory conditions, results in accelerated, larger and denser thrombus formation.28,29 Human data suggest that patients with COVID-19 infection have elevated levels of serum α-defensin proportional to COVID-19 disease severity.30
Clinical implications
The connections between inflammation, thrombosis and poor COVID-19 outcomes are well established. On admission, patients from our own institution who were admitted to regular floors but subsequently transferred to the intensive care unit (ICU) had higher CRP concentrations (159±86 mg/L) than patients admitted to the regular floors overall (114±81 mg/L). On transfer to the ICU, CRP concentrations (184 mg/L±104) were higher still (unpublished, figure 3). Manifestations of profound inflammation in severe COVID-19 include acute respiratory distress syndrome and distributive shock.14,15,17 Myocardial injury due to acute coronary syndrome (type 1) and/or supply-demand mismatch in the setting of profound inflammatory response and haemodynamic changes (type 2) is also significantly greater in those with severe COVID-19.31 Vascular inflammation is associated with a large burden of both venous (deep venous thrombosis, pulmonary embolism) and arterial (myocardial infarction, stroke) thrombus.
Figure 3.
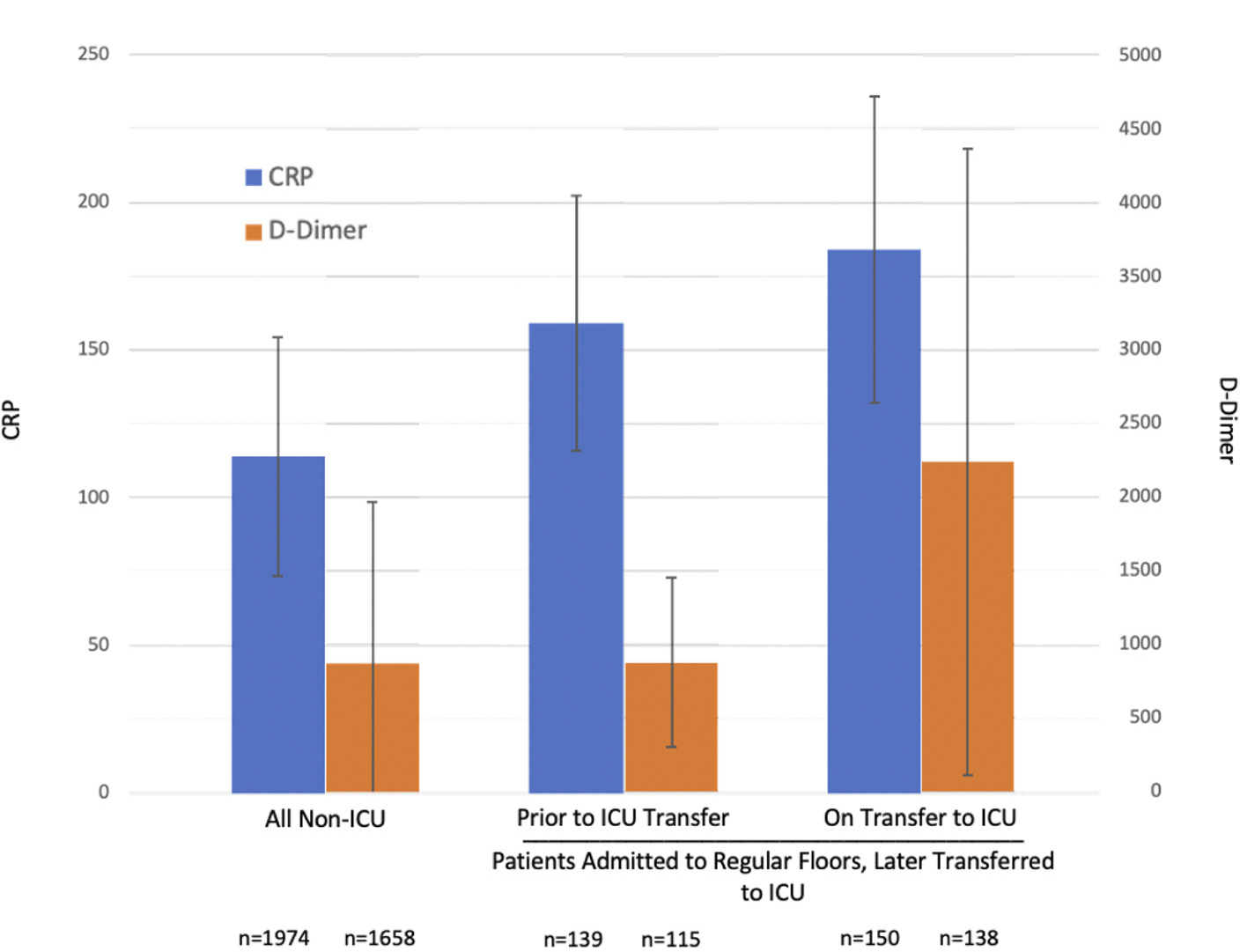
Markers of inflammation and thrombosis in patients admitted to the hospital for COVID-19. Admission inflammatory markers were obtained for all patients admitted to the regular (non-ICU) floors of NYU Langone Hospital for the first weeks (March–April 2020) of the COVID-19 pandemic surge in New York City. Among patients admitted to the regular floors, those who were subsequently transferred to the intensive care unit (ICU) had higher C reactive protein (CRP) levels than the group overall; among those transferred to the ICU, both CRP and D-dimer levels in the ICU were increased compared with prior to transfer, indicating that a worsening inflammatory state is a feature of more severe disease. Not shown in the figure: individuals admitted to the regular floors who were subsequently transferred to directly to the ICU also had higher ferritin levels than the non-ICU group overall (1452 vs 1178 mg/dL), and their mean ferritin level was found to be increased further on transfer to the ICU (1876 mg/dL).
Severe COVID-19 has also been characterised by extrapulmonary and extravascular manifestations. Acute kidney injury may be a result of direct inflammatory injury, given evidence of acute tubular necrosis with lymphocyte and macrophage infiltration of the tubulointerstitium on histopathology.32 The mechanism(s) of COVID-related hepatic injury remains unclear but preliminary studies suggest that the ACE2 receptor is preferentially expressed in cholangiocytes, suggesting that liver involvement may require direct SARS-CoV-2 infection and injury of cholangiocytes.33,34 Cytokine storm itself can drive multisystem organ injury overall.
Together, these observations suggest that an anti-inflammatory agent with limited immunosuppressive potential could prove useful in preventing severe inflammatory injury and promoting improved patient outcomes.
COLCHICINE
Historical perspective
Although colchicine first received approval from the US Food and Drug Administration in 2009, its modern use dates back two centuries. Indeed, papyri dating from 1500 BC describe the use of colchicine’s source plant—Colchicum autumnale—for pain and inflammation, making colchicine one of the world’s oldest anti-inflammatory therapeutics.35 Currently, colchicine is approved for treating and preventing acute gout and familial Mediterranean fever, and is used off label in Behçet’s disease, pericarditis and other inflammatory conditions.36
Colchicine and microtubules: inhibition of neutrophil activity
Microtubules are dynamic proteins that form via polymerisation of α-/β-tubulin dimers. Colchicine irreversibly intercalates into free α/β dimers that incorporate into and block microtubule extension.37 During inflammation, microtubules facilitate the movement of adhesion molecules onto cell surfaces. Colchicine concentrations are much higher in neutrophils than other leukocytes due to diminished activity of the P-glycoprotein membrane efflux pump that serves as an energy-dependent colchicine efflux transporter.38 Thus, neutrophils appear to be more sensitive than other cells to lower serum concentrations of colchicine. Cronstein et al demonstrated that colchicine causes a quantitative decrease in leucocyte (L)-selectin expression and diminishes qualitative expression of endothelial (E)-selectin, two proteins involved in rolling and adhesion of neutrophils on endothelium.39 Disruption of microtubules also inhibits neutrophil rheologic capacity, inhibiting their transmigration out of blood vessels.40
Additional studies show that colchicine directly inhibits intracellular neutrophil signalling and lysosomal enzyme release during phagocytosis. Colchicine-mediated inhibition of chemoattractant release (eg, leukotriene B4) suppresses neutrophil adhesion to inflamed endothelium.41 Colchicine also inhibits calcium influx, which raises intracellular cyclic adenosine monophosphate (cAMP) levels and dampens neutrophil responses.42 In lipopolysachharide-stimulated neutrophils, we observed that colchicine can dampen stimulated neutrophil metabolism as measured by extracellular acidification (unpublished, figure 4).
Figure 4.
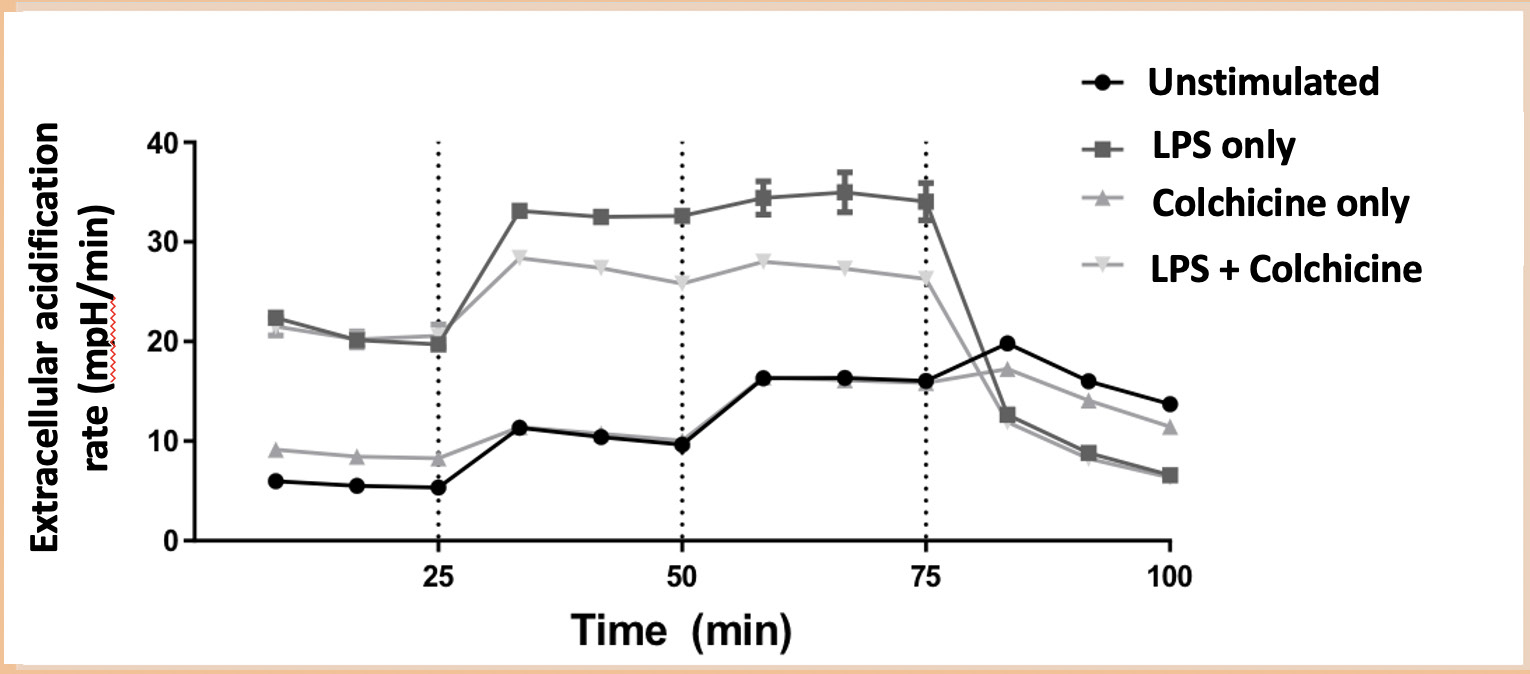
Neutrophil metabolism in the presence of colchicine. Neutrophils were purified from healthy volunteer whole blood using the MACSxpress whole blood neutrophil isolation kit (Miltenyi Biotec, Bergisch Gladbach, Germany) and separated into four aliquots. Neutrophils were coincubated with and without lipopolysaccharide (LPS) and with and without colchicine. In vitro quantification of neutrophil metabolism, measured as extracellular acidification rate (ECAR) (mpH/min), was evaluated using a glycolysis stress test using a Seahorse XFe24 analyzer (Agilent Technologies, Santa Clara, California, USA). Using a modified assay, cells were first incubated with activators (LPS 10 ng/mL with or without colchicine 15 nM) for 10 min.
Colchicine and the inflammasome: inhibition of IL-1β and prevention of the cytokine storm
More recently, colchicine has been shown to decrease cytokine production by inhibiting activation of the NLRP3 inflammasome (figure 5). The mechanism(s) of colchicine’s action on the inflammasome remain an area of ongoing investigation.43,44 Colchicine’s interruption of inflammasome activation reduces IL-1β production, which in turn prevents the induction of IL-6 and TNF and the recruitment of additional neutrophils and macrophages.45,46 Whereas the effect of specific anti-IL-6 inhibition for COVID-19 treatment is somewhat controversial (online supplemental text 1), the ability of colchicine to affect multiple cytokines may offer unique advantages.
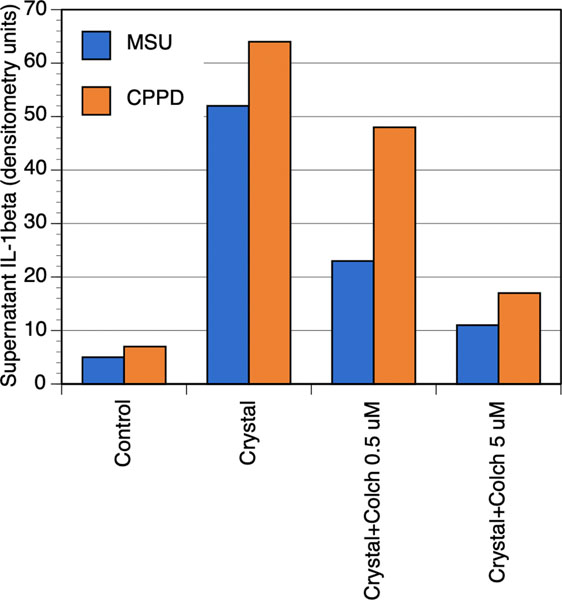
Figure 5.
Colchicine inhibits inflammasome action and reduces supernatant levels of IL-1β. THP1 cells (macrophage cell line) were stimulated with monosodium urate (MSU) or calcium pyrophosphate dihydrate (CPPD) crystals in the presence or absence of colchicine. Supernatants were analysed for IL-1β by Western blot. For the purposes of this figure, the original published blot was quantified using Image J. Adapted from Martinon et al.43
Colchicine and the Inflammation/thrombosis interface
Murine models show that colchicine inhibits neutrophil release of α-defensin, thereby potentially preventing large thrombus burdens.29,47 At supratherapeutic concentrations, colchicine, through its microtubule effects, converts normal discoid platelets to rounded, irregular structures and inhibits platelet activation by decreasing calcium entry.48 These mechanisms diminish in vitro platelet-to-platelet aggregation. In contrast, we demonstrated that standard clinical doses of colchicine do not decrease platelet-to-platelet aggregation but do diminish neutrophil-to-platelet aggregation,49 suggesting that colchicine at physiological doses may provide an inhibitory role at the inflammation/thrombosis interface without comprising homeostatic platelet-to-platelet function. Indeed, in vivo colchicine has not been shown to inhibit non-inflammatory-related thrombosis.
Adverse effects of colchicine
Colchicine metabolism occurs primarily inside hepatocytes via the cytochrome P450 3A4 (CYP3A4). Medications that strongly inhibit CYP3A4 metabolism (eg, ritonavir, ketoconazole, clarithromycin, cyclosporine, diltiazem, verapamil) pose a risk of drug-drug interactions. A small number of publications report cases of death after coadministration of clarithromycin and colchicine in patients with severe chronic renal disease.50,51 Similar cases have been rarely reported in patients receiving atorvastatin, a statin that is also processed by CYP-3A4, but not with statins that are not metabolised through CYP3A4. In a recent placebo-controlled randomised trial of 4745 patient with a recent myocardial infarction, patients receiving daily colchicine experienced no adverse effects related to the coadministration of statins, including atorvastatin.52 In another recent placebo-controlled randomised trial of 5522 patients with stable coronary artery disease, daily colchicine resulted in numerically higher rates of myalgia (HR 1.15, 95% CI 1.01 to 1.31) and one case of rhabdomyolysis (the patient made a full recovery).53 However, a non-significant trend towards increased non-cardiovascular death was observed that requires further investigation. Overall, reports of severe colchicine toxicity tend to occur in the setting of errors in colchicine prescribing.
Approximately 10%–20% of colchicine is excreted renally.36 However, dose reductions may only be necessary in patients with severe renal impairment.54 As a lipophilic molecule, colchicine is usually protein-bound in plasma, with P-glycoprotein in the intestinal lining serving as the primary protein for gut excretion of colchicine. Cyclosporine and ranolazine compete for the ligand site on P-glycoprotein and can therefore lead to delayed elimination. At higher concentrations for longer durations, particularly in the setting of kidney disease, colchicine has been reported to occasionally induce a reversible neuromyopathy. Acute overdose may cause multiorgan system failure and death. Furthermore, increased adverse events may be noted in the simultaneous presence of moderate renal insufficiency with use of multiple CYP3A4 inhibitors.
A meta-analysis of 35 randomised trials of colchicine versus placebo found that the most common and significant adverse effect was diarrhoea.55,56 The only other adverse effect that occurred at a greater frequency than placebo was a set of pooled gastrointestinal symptoms including nausea, vomiting, diarrhoea, abdominal pain, loss of appetite, and bloating. A striking finding in this meta-analysis was the absence of increased infection rates in the colchicine compared with the placebo arm. However, in contrast to most available data, one retrospective and one prospective study did report increased pneumonia risk with colchicine (online supplemental table 1).
COLCHICINE AND COVID-19: THE CLINICAL CASE
Several of the biological therapies that have been studied and/or used in the setting of severe SARS-CoV-2 infection target some of the same pathways as colchicine, including IL-1β (ie, anakinra) and IL-6 (ie, tocilizumab and sarilumab).57 Colchicine differs from these agents in having pleotropic mechanisms of action, being less potent on any single target, and being an oral agent. In contrast to the biological agents used in the midst of cytokine storm, colchicine is not immunosuppressive, is not known to increase risk of infection, and is inexpensive. A review of the mechanisms of SARS-CoV-2 and colchicine in parallel reveals a potential intervention point that may prevent the progression from inflammatory activation (phase 2) to a hyperinflammatory state (phase 3). Taken together with the clinical data described herein, the potential benefits of colchicine are suggested to be maximised when used early in the disease process (ideally prior to phase 2, but certainly prior to phase 3), such as in non-hospitalised patients within a few days of diagnosis regardless of symptoms and/or within a few days of hospitalisation if not already critically ill. However, the optimal timing continues to require further investigation.
Colchicine in non-rheumatological inflammatory conditions
Multiple randomised studies have evaluated the use of colchicine in non-rheumatologic inflammatory conditions. Two randomised trials in acute pericarditis demonstrated lower recurrence rate with colchicine versus conventional or placebo therapy.58 Colchicine reduced symptom persistence 72 hours after treatment initiation, and colchicine was beneficial even in the setting of recurrent pericarditis.59 Used after cardiac surgery, colchicine appears to prevent the inflammatory postpericardiotomy syndrome.60
Colchicine may reduce risk of acute myocardial infarction (AMI). We demonstrated an association between daily colchicine use and decreased prevalence of AMI in patients with gout, a non-traditional cardiovascular risk factor.61,62 These findings were subsequently reproduced in an independent gout population.63 Two open-label prospective studies of daily colchicine use versus no colchicine use in patients with stable coronary artery disease already on aspirin and high-intensity statin therapy demonstrated a decrease in CRP levels with low-dose colchicine, and a significant reduction in cardiovascular events with daily colchicine vs no colchicine.64,65 The reduction in the primary clinical outcome was driven primarily by a reduction in AMI.65 The multicentre, double-blind COLchicine Cardiovascular Outcomes Trial (COLCOT) randomised 4745 patients within 30 days of AMI to colchicine or placebo and demonstrated a reduction in the primary composite endpoint of cardiovascular death, resuscitated cardiac arrest, AMI, stroke or urgent revascularisation with colchicine.52 The multicentre, double-blind Low Dose Colchicine 2 (LoDoCo 2) trial randomised 5522 patients with stable coronary artery disease and also demonstrated a reduction in the primary composite endpoint of cardiovascular death, AMI, stroke or urgent revascularisation.53 Finally, in cases where the thrombus burden remains refractory to standard antiplatelet and anticoagulant therapies, colchicine has been shown to be associated with thrombus resolution.66
Our 400-patient randomised Colchicine in Percutaneous Coronary Intervention (Colchicine-PCI) trial demonstrated that when given as a standard loading dose prior to tissue injury (coronary stent placement), colchicine significantly dampened the upregulation of IL-6 and CRP.67 These effects were observed 22–24 hours after the acute event, providing a rationale to administer colchicine earlier in the disease process to prevent clinical manifestations of cytokine-induced injury. Consistent with a possible preventive role, colchicine is effective to prevent cytokine-based disease flares in gout and familial Mediterranean fever.45 Finally, colchicine has also been shown to dampen the inflammatory response and reduce CRP levels among subjects with metabolic syndrome.68 These data support the general anti-inflammatory effect of colchicine, independent of a specific disease state.
Colchicine trials in COVID-19
The recent open-label, multicentre Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial in the UK demonstrated a reduction in 28-day mortality with dexamethasone (n=2104) vs usual care (n=4321) in patients hospitalised with severe COVID-19.69 These data support the principle that an anti-inflammatory strategy in COVID-19 may be helpful. However, glucocorticoids such as dexamethasone have intrinsic immunosuppressive drawbacks that colchicine does not share.
Several early studies have evaluated the benefit of colchicine in COVID-19 patients. A retrospective single-centre study of 87 ICU patients with COVID-19 demonstrated a lower risk of death in patients on colchicine (adjusted HR 0.41, 95% CI 0.17 to 0.98).70 The Greek Effects of Colchicine in COVID-19 (GRECO-19) trial was the first prospective open-label randomised trial evaluating colchicine versus usual care in early hospitalised patients. This study of 105 patients found a significant reduction in the primary clinical outcome of a two-point deterioration on WHO disease severity scale.71 The authors additionally noted suppression of D-dimer levels in the colchicine vs control group.71 An Italian study compared 122 hospitalised patients who received colchicine plus standard-of-care (lopinavir/ritonavir, dexamethasone or hydroxychloroquine) with 140 hospitalised patients receiving standard-of-care alone. Colchicine had a significant mortality benefit (84% vs 64% survival) vs controls.72 A third prospective study randomised 38 hospitalised COVID-19 patients to colchicine or placebo in a double-blinded manner.73 Patients receiving colchicine had less need for supplemental oxygen at day 7 (6% vs 39%) and were more likely to be discharged at day 10 (94% vs 83%). Colchicine subjects also had greater reduction of CRP, and no increase in serious adverse events.73 Additional inpatient studies are ongoing (online supplemental table 2). Although the permitted use of other treatments could have biased the impact of colchicine in these studies, in the GRECO-19 trial no glucocorticoids were administered and other medications did not differ between the two groups; in the Italian study, there was no difference in outcomes among patients given colchicine who did or did not also receive dexamethasone.
Given its ease of use, tolerability and low cost, an argument for studying colchicine in the outpatient setting, to reduce hospitalisation and adverse outcomes, may be even more compelling. Unfortunately, data on the use of colchicine in the setting of outpatient COVID-19 cases are sparse. In a very small case series from Italy, nine outpatients with COVID-19 were administered colchicine, of whom only one subject was ultimately hospitalised. The hospitalised patient received 4 days of oxygen therapy and was discharged.74 Moreover, all patients experienced defervescence within 72 hours of colchicine initiation, suggesting an antipyretic effect. While these reports are insufficient to recommend colchicine for COVID-19 in clinical practice, they provide support for further study of colchicine in COVID-19, including in the outpatient setting. The ongoing ColCorona Trial (www.colcorona.net) is a large placebo-controlled trial of colchicine use within 2 days of COVID-19 diagnosis, regardless of symptoms, in patients with comorbidities that place patients at a higher risk of developing complications related to COVID-19 that may provide additional information.
CONCLUSIONS
Given the large body of data demonstrating colchicine’s inhibitory effects on neutrophil activity, cytokine generation and the inflammation/thrombosis interface, together with an overall lack of evidence for systemic immunosuppression, there is a rationale to study colchicine as a potential treatment for COVID-19. Given that colchicine is generally well tolerated, simple to take and inexpensive, demonstration of colchicine as a useful agent in COVID-19 would potentially spare patients morbidity and mortality, help to conserve valuable clinical resources (hospital floor and ICU beds, ventilators, etc), and dramatically reduce the cost of COVID-19 care. Colchicine might be of particular use in resource-poor rural and developing world settings, both of which have been increasingly affected by COVID-19. However, unless and until evidence is obtained from adequately designed and randomised placebo-controlled trials, this hypothesis must remain speculative.
The optimal dose of colchicine for daily use, even in well-established conditions such as gout, is unknown. Many but not all patients tolerate up to 1.2 mg daily in divided doses; whether lower doses such as 0.5 mg or less daily can be equally effective is unknown. The largest colchicine study for COVID-19 (ColCorona) is testing a dose of 0.5 mg daily based on prior cardiology trials. The duration of colchicine therapy for SARS-COV2 infection would also need to be determined. Most studies to date test a treatment duration of 2–4 weeks, concordant with the acute course of the infection; whether a shorter or longer treatment would be optimal is unknown. Finally, the timing of colchicine initiation is uncertain, with some studies beginning treatment in the outpatient setting, and others in the early inpatient setting. Given the recent track record of failure of treatment of severe COVID-19 treatment with anti-IL-6 biologics such as tocilizumab (a much more potent but also more specific immunosuppressive agent), it is likely that the severe inpatient setting is not the optimal condition under which to assess colchicine efficacy.
Supplementary Material
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests For the purposes of full disclosure, we note that BS receives support from the NIH/NHLBI (1R01HL146206, 3R01HL146206-02S1) and VA ORD (iK2CX001074) for her work on colchicine in cardiovascular disease and COVID-19. J-CT reports grants and personal fees from Amarin, grants and personal fees from AstraZeneca, grants, personal fees and other from DalCor, grants from Esperion, grants from Ionis, grants and personal fees from Pfizer, grants and personal fees from Sanofi, grants and personal fees from Servier, personal fees from HLS Therapeutics, outside the submitted work; In addition, J-CT has a patent on pharmacogenomics-guided CETP inhibition issued, and a patent on the use of colchicine after myocardial infarction pending. MHP holds investigator-initiated grants from Horizon Therapeutics (to study urate deposition in the spines of gout patients) and Hikma Pharmaceuticals (to study the possible benefit of colchicine in knee osteoarthritis) and has served as a consultant for Horizon and Sobi. MHP also receives salary support from a CTSA award (1UL1TR001445) to New York University from the National Centre for the Advancement of Translational Science, National Institutes of Health. TLWM is supported by an NYU-HHC Clinical and Translational Science Institute KL2 grant and a Doris Duke Fund to Retain Clinical Scientists award. TLWM has served on an advisory board for Novartis and as a consultant to Regeneron, unrelated to this work
Footnotes
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
This article is made freely available for use in accordance with BMJ’s website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
Additional material is published online only. To view, please visit the journal online (http://dx.doi.org/10.1136/annrheumdis-2020–219174).
REFERENCES
- 1.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akhmerov A, Marbán E. COVID-19 and the heart. Circ Res 2020;126:1443–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395:1033–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He Y, Hara H, Núñez G. Mechanism and regulation of NLRP3 inflammasome activation. Trends Biochem Sci 2016;41:1012–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schroder K, Tschopp J. The inflammasomes. Cell 2010;140:821–32. [DOI] [PubMed] [Google Scholar]
- 6.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol 2020;20:355–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nieto-Torres JL, Verdiá-Báguena C, Jimenez-Guardeño JM, et al. Severe acute respiratory syndrome coronavirus E protein transports calcium ions and activates the NLRP3 inflammasome. Virology 2015;485:330–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020;180:934–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banu N, Panikar SS, Leal LR, et al. Protective role of ACE2 and its downregulation in SARS-CoV-2 infection leading to macrophage activation syndrome: therapeutic implications. Life Sci 2020;256:117905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang C, Wu Z, Li J-W, et al. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int J Antimicrob Agents 2020;55:105954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis 2020;71:762–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belkaid Y, Rouse BT. Natural regulatory T cells in infectious disease. Nat Immunol 2005;6:353–60. [DOI] [PubMed] [Google Scholar]
- 13.Alhogbani T Acute myocarditis associated with novel middle East respiratory syndrome coronavirus. Ann Saudi Med 2016;36:78–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ruan Q, Yang K, Wang W, et al. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;46:846–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bangalore S, Sharma A, Slotwiner A, et al. ST-segment elevation in patients with Covid-19 - a case series. N Engl J Med 2020;382:2478–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harari R, Bangalore S, Chang E, et al. COVID-19 complicated by acute myocardial infarction with extensive thrombus burden and cardiogenic shock. Catheter Cardiovasc Interv 2020. doi: 10.1002/ccd.28992. [Epub ahead of print: 19 May 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruf W, Ruggeri ZM. Neutrophils release brakes of coagulation. Nat Med 2010;16:851–2. [DOI] [PubMed] [Google Scholar]
- 21.Clark SR, Ma AC, Tavener SA, et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nat Med 2007;13:463–9. [DOI] [PubMed] [Google Scholar]
- 22.McEver RP. P-Selectin/PSGL-1 and Other Interactions Between Platelets, Leukocytes, and Endothelium. In: Michelson A, ed. Platelets. 2 edn. San Diego: Elsevier/Academic Press, 2007: 231–49. [Google Scholar]
- 23.Arber N, Berliner S, Pras E, et al. Heterotypic leukocyte aggregation in the peripheral blood of patients with leukemia, inflammation and stress. Nouv Rev Fr Hematol 1991;33:251–5. [PubMed] [Google Scholar]
- 24.Furman MI, Barnard MR, Krueger LA, et al. Circulating monocyte-platelet aggregates are an early marker of acute myocardial infarction. J Am Coll Cardiol 2001;38:1002–6. [DOI] [PubMed] [Google Scholar]
- 25.Abramson SB, Dobro J, Eberle MA, et al. Acute reversible hypoxemia in systemic lupus erythematosus. Ann Intern Med 1991;114:941–7. [DOI] [PubMed] [Google Scholar]
- 26.Ganz T, Selsted ME, Szklarek D, et al. Defensins. natural peptide antibiotics of human neutrophils. J Clin Invest 1985;76:1427–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joseph G, Tarnow L, Astrup AS, et al. Plasma alpha-defensin is associated with cardiovascular morbidity and mortality in type 1 diabetic patients. J Clin Endocrinol Metab 2008;93:1470–5. [DOI] [PubMed] [Google Scholar]
- 28.Vordenbäumen S, Sander O, Bleck E, et al. Cardiovascular disease and serum defensin levels in systemic lupus erythematosus. Clin Exp Rheumatol 2012;30:364–70. [PubMed] [Google Scholar]
- 29.Abu-Fanne R, Stepanova V, Litvinov RI, et al. Neutrophil α-defensins promote thrombosis in vivo by altering fibrin formation, structure, and stability. Blood 2019;133:481–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leichman AK. Hadassah researchers pinpoint source of corona blood clots. ISRAEL21c [Internet], 2020. Available: https://www.israel21c.org/hadassah-researchers-find-source-of-corona-blood-clots/ [Accessed 25 Aug 2020]. [Google Scholar]
- 31.Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis 2020;63:390–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diao B, Wang C, Wang R, et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. medRxiv 2020. doi: 10.1101/2020.03.04.20031120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang C, Shi L, Wang F-S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol 2020;5:428–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chai X, Hu L, Zhang Y, et al. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. Biorxiv 2020. doi: 10.1101/2020.02.03.931766 [DOI] [Google Scholar]
- 35.Nerlekar N, Beale A, Harper RW. Colchicine--a short history of an ancient drug. Med J Aust 2014;201:687–8. [DOI] [PubMed] [Google Scholar]
- 36.Leung YY, Yao Hui LL, Kraus VB. Colchicine--Update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum 2015;45:341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Andreu JM, Timasheff SN. Tubulin bound to colchicine forms polymers different from microtubules. Proc Natl Acad Sci U S A 1982;79:6753–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ben-Chetrit E, Levy M. Does the lack of the P-glycoprotein efflux pump in neutrophils explain the efficacy of colchicine in familial Mediterranean fever and other inflammatory diseases? Med Hypotheses 1998;51:377–80. [DOI] [PubMed] [Google Scholar]
- 39.Cronstein BN, Molad Y, Reibman J, et al. Colchicine alters the quantitative and qualitative display of selectins on endothelial cells and neutrophils. J Clin Invest 1995;96:994–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paschke S, Weidner AF, Paust T, et al. Technical advance: inhibition of neutrophil chemotaxis by colchicine is modulated through viscoelastic properties of subcellular compartments. J Leukoc Biol 2013;94:1091–6. [DOI] [PubMed] [Google Scholar]
- 41.Reibman J, Haines KA, Rich AM, et al. Colchicine inhibits ionophore-induced formation of leukotriene B4 by human neutrophils: the role of microtubules. J Immunol 1986;136:1027–32. [PubMed] [Google Scholar]
- 42.Rudolph SA, Greengard P, Malawista SE. Effects of colchicine on cyclic AMP levels in human leukocytes. Proc Natl Acad Sci U S A 1977;74:3404–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martinon F, Pétrilli V, Mayor A, et al. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature 2006;440:237–41. [DOI] [PubMed] [Google Scholar]
- 44.Martínez GJ, Celermajer DS, Patel S. The NLRP3 inflammasome and the emerging role of colchicine to inhibit atherosclerosis-associated inflammation. Atherosclerosis 2018;269:262–71. [DOI] [PubMed] [Google Scholar]
- 45.Slobodnick A, Shah B, Krasnokutsky S, et al. Update on colchicine, 2017. Rheumatology 2018;57:i4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fordham JN, Kirwan J, Cason J, et al. Prolonged reduction in polymorphonuclear adhesion following oral colchicine. Ann Rheum Dis 1981;40:605–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Higazi M, Abdeen S, Abu-Fanne R, et al. Opposing effects of HNP1 (α-defensin-1) on plasma cholesterol and atherogenesis. PLoS One 2020;15:e0231582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Menche D, Israel A, Karpatkin S. Platelets and microtubules. Effect of colchicine and D2O on platelet aggregation and release induced by calcium ionophore A23187. J Clin Invest 1980;66:284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shah B, Allen N, Harchandani B, et al. Effect of colchicine on Platelet-Platelet and platelet-leukocyte interactions: a pilot study in healthy subjects. Inflammation 2016;39:182–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cheng VCC, Ho PL, Yuen KY. Two probable cases of serious drug interaction between clarithromycin and colchicine. South Med J 2005;98:811–3. [DOI] [PubMed] [Google Scholar]
- 51.Dogukan A, Oymak FS, Taskapan H, et al. Acute fatal colchicine intoxication in a patient on continuous ambulatory peritoneal dialysis (CapD). Possible role of clarithromycin administration. Clin Nephrol 2001;55:181–2. [PubMed] [Google Scholar]
- 52.Tardif J-C, Kouz S, Waters DD, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med 2019;381:2497–505. [DOI] [PubMed] [Google Scholar]
- 53.Nidorf SM, Fiolet ATL, Mosterd A, et al. Colchicine in patients with chronic coronary disease. N Engl J Med 2020;383:1838–47. [DOI] [PubMed] [Google Scholar]
- 54.Wason S, Mount D, Faulkner R. Single-dose, open-label study of the differences in pharmacokinetics of colchicine in subjects with renal impairment, including end-stage renal disease. Clin Drug Investig 2014;34:845–55. [DOI] [PubMed] [Google Scholar]
- 55.Stewart S, Yang KCK, Atkins K, et al. Adverse events during oral colchicine use: a systematic review and meta-analysis of randomised controlled trials. Arthritis Res Ther 2020;22:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Levy M, Spino M, Read SE. Colchicine: a state-of-the-art review. Pharmacotherapy 1991;11:196–211. [PubMed] [Google Scholar]
- 57.Prieto-Peña D, Dasgupta B. Biologic agents and small-molecule inhibitors in systemic autoimmune conditions: an update. Pol Arch Intern Med 2020. doi: 10.20452/pamw.15438. [Epub ahead of print: 18 Jun 2020]. [DOI] [PubMed] [Google Scholar]
- 58.Imazio M, Brucato A, Cemin R, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med 2013;369:1522–8. [DOI] [PubMed] [Google Scholar]
- 59.Imazio M, Belli R, Brucato A, et al. Efficacy and safety of colchicine for treatment of multiple recurrences of pericarditis (CORP-2): a multicentre, double-blind, placebo-controlled, randomised trial. Lancet 2014;383:2232–7. [DOI] [PubMed] [Google Scholar]
- 60.Imazio M, Brucato A, Ferrazzi P, et al. Colchicine for prevention of postpericardiotomy syndrome and postoperative atrial fibrillation: the COPPS-2 randomized clinical trial. JAMA 2014;312:1016–23. [DOI] [PubMed] [Google Scholar]
- 61.Crittenden DB, Lehmann RA, Schneck L, et al. Colchicine use is associated with decreased prevalence of myocardial infarction in patients with gout. J Rheumatol 2012;39:1458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shah B, Jeurling S, Crittenden DB, et al. Colchicine use and the development of stable coronary artery disease in gout patients: results of a ten-year retrospective cohort study [Preprint] 2020. [Google Scholar]
- 63.Solomon DH, Liu C-C, Kuo I-H, et al. Effects of colchicine on risk of cardiovascular events and mortality among patients with gout: a cohort study using electronic medical records linked with Medicare claims. Ann Rheum Dis 2016;75:1674–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nidorf M, Thompson PL. Effect of colchicine (0.5 Mg twice daily) on high-sensitivity C-reactive protein independent of aspirin and atorvastatin in patients with stable coronary artery disease. Am J Cardiol 2007;99:805–7. [DOI] [PubMed] [Google Scholar]
- 65.Nidorf SM, Eikelboom JW, Budgeon CA, et al. Low-Dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol 2013;61:404–10. [DOI] [PubMed] [Google Scholar]
- 66.Nonaka D, Takase H, Machii M, et al. Colchicine therapy for deep vein thrombosis in a patient with vascular-type Behçet disease: a case report. Medicine 2020;99:e19814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shah B, Pillinger M, Zhong H, et al. Effects of acute colchicine administration prior to percutaneous coronary intervention: COLCHICINE-PCI randomized trial. Circ Cardiovasc Interv 2020;13:e008717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Demidowich AP, Levine JA, Onyekaba GI, et al. Effects of colchicine in adults with metabolic syndrome: a pilot randomized controlled trial. Diabetes Obes Metab 2019;21:1642–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19 - preliminary report. N Engl J Med 2020. doi: 10.1056/NEJMoa2021436. [Epub ahead of print: 17 Jul 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rodriguez-Nava G, Trelles-Garcia DP, Yanez-Bello MA, et al. Atorvastatin associated with decreased hazard for death in COVID-19 patients admitted to an ICU: a retrospective cohort study. Crit Care 2020;24:429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Deftereos SG, Giannopoulos G, Vrachatis DA, et al. Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: the GRECCO-19 randomized clinical trial. JAMA Netw Open 2020;3:e2013136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Scarsi M, Piantoni S, Colombo E, et al. Association between treatment with colchicine and improved survival in a single-centre cohort of adult hospitalised patients with COVID-19 pneumonia and acute respiratory distress syndrome. Ann Rheum Dis 2020;79:1286–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lopes MIF, Bonjorno LP, Giannini MC, et al. Beneficial effects of colchicine for moderate to severe COVID-19: an interim analysis of a randomized, double-blinded, placebo controlled clinical trial. medRxiv 2020. doi: 10.1101/2020.08.06.20169573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Della-Torre E, Della-Torre F, Kusanovic M, et al. Treating COVID-19 with colchicine in community healthcare setting. Clin Immunol 2020;217:108490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.