Abstract
Introduction
Widespread utilization of telemedicine in our practice to date has been limited to the evaluation of certain post-surgical patients. The COVID-19 pandemic acutely stressed our established system and required us to enhance our utilization of telemedicine. We hypothesized that expansion of telemedicine to new and follow up patient visits for pediatric urology could be done effectively in a way that satisfied patient and parental expectations.
Materials and methods
Using a pre-COVID-19 established telemedicine program based in our electronic medical record (EMR), patients and providers transitioned to primarily virtual visits when clinically appropriate. Guidelines were formulated to direct patient scheduling, provider and staff education was provided, including a process map designed for multiple providers to complete video visits (VV), and the EMR was redesigned to incorporate telehealth terminology. The number of VV per provider was recorded using the electronic medical record, and patient reported outcomes (PRO) were measured using a standardized questionnaire.
Results
A total of 631 VV met inclusion criteria during the period of May 2018–April 2020. This included 334 follow up, 172 new, and 125 postoperative visits. The median age of patients at time of visit was 7 years (IQR 2–12 years), median visit time was 20 min (IQR 15–30 min), and the median travel distance saved by performing a VV was 12.2 miles (IQR 6.3–26.8 miles). Diagnoses were varied and included the entire breadth of a standard pediatric urology practice. The PRO questionnaire was completed for 325 of those patient visits. Families reported a high overall satisfaction with the video visits (median score of 10 out of 10) and felt that the visit met their child's medical needs. 90% stated that they would strongly recommend a telehealth visit to other families. Patients and parents reported benefits of VV including decreased travel costs and less time taken off from work and school.
Conclusion
The EMR enabled nimble redirection of clinical care in the setting of a global pandemic. The enhanced use of telemedicine has proved to be an alternative method to provide care for pediatric urology patients. Families indicate a high degree of satisfaction with this technology in addition to significant time and cost savings. Telemedicine should remain a key aspect of medical care and expanded from post-operative visits to new patient and follow up visits, even as we return to our normal practices as the pandemic restrictions soften.
Summary figure.
Program map depicting the sequence of a video visit (VV). The process begins with our scheduling team which provides the necessary information to the family and ensures that they can be scheduled properly. The family is encouraged to conduct the visit in a quiet place with at least one parent and the child present. Relevant records, imaging, and laboratory studies should be uploaded prior to the visit. In addition, pictures and/or videos uploaded by the family prior to the visit can facilitate the examination portion of the visit. VV = video visit; AVS = after visit summary.
Keywords: Telehealth, Telemedicine, Video visits (VV), Patient-reported outcomes (PRO), Provider experience, Pediatric urology
Introduction
Telehealth is a rapidly growing aspect of healthcare and involves the exchange between a patient and provider via an electronic medium [1]. From 2016 to 2019, the national usage of telehealth increased more than any other venue of healthcare, doubling from 14% to 28% of providers [2]. Specifically, telemedicine – a subset of telehealth that refers to clinical care – provides positive patient outcomes and favorable economic advantages [3,4]. These include improvements in patient quality of life, enabling access to care in underserved locations, reductions in travel time and costs, shorter waiting times, and decreases in hospital admissions [[5], [6], [7]]. Telemedicine has been used nearly universally across all medical specialties to varying degrees.
During the current global COVID-19 pandemic, telemedicine has played a critical role in providing timely patient care while providing the social and physical distancing recommended to prevent the spread of communicable diseases [8]. Video visits (VV), in particular, have given a live audio-visual alternative to traditional in-person visits. This interactive modality has enabled real time communication between providers, patients and families. Moreover, patients have reported that time with providers and level of care they received were commensurate to that of in-person visits [4].
Prior to the increased demand from the COVID-19 pandemic, the use of telemedicine and its adoption into pediatrics specialty care, including pediatric urology, was low. Only a fraction of pediatric hospitals have utilized telemedicine in their practices [9]. Review of our own practice showed limited utilization of telemedicine despite its availability and known potential benefits for families for 18 months prior to the pandemic restrictions.
In an effort to meet the demands of COVID-19 contact restrictions and to maintain continuity of care for our patients, we endeavored to increase utilization of telemedicine in our practice. As rapid expansion of VV in pediatric urology has been recently reported [10], we sought to evaluate patient satisfaction for completed visits, as this is a critical factor in assessing the longevity of telemedicine expansion. We hypothesized that implementation of a process map would facilitate the increase in utilization of VV so that telemedicine would be perceived as favorable by patients and families. We report on the development of our telemedicine program, our experiences with this transition, and most importantly, patient reported outcomes after implementation of the change.
Materials and Methods
Using an IRB-approved registry of pediatric urology clinic patients, all pediatric urology patients who completed a VV from May 2018 to April 2020 within the urology division at The Children's Hospital of Philadelphia (CHOP) were identified and included. The expansion of VV began in March 2020, coinciding with the rise of the COVID-19 pandemic. Exclusion criteria included patients seen in person and visits in which telehealth was not provided due to technical issues. Visits were stratified by type, including post-operative visits, new patient consultations and follow up visits. Patient demographic information (age, gender, and home address), visit diagnoses, scheduled visit location (main hospital or satellite office location), and provider for the visit were retrieved from the electronic medical record (EMR). Distance traveled was calculated using Google Maps data as the distance traveled from their home to the office location that had been originally scheduled. Patients who had a VV were contacted by email after the visit to provide feedback through an anonymous questionnaire.
Ambulatory order sets and telemedicine visit progress note templates in the EMR were created to appropriately match the standards and requirements of the state. Documentation included a history of present illness, review of systems, system-focused physical exam with visual inspection, and attestation statement that care was provided and appropriate for telemedicine.
Telemedicine Workflow Outline
Scheduling coordinators were educated on scheduling needs, patient educational materials, and how to register families for the EMR application. A help line number is emailed to families in advance to assist with common technical concerns. Prior to clinic, the schedule is reviewed by the physician and non-physician provider, along with images, reports, and lab work. Providers, if not working at the same location, communicate amongst themselves via email or telephone to facilitate the visit. Patients are encouraged to arrive 5–10 min prior to the scheduled visit time. If orders are required, they are sent via the EMR application or email. If surgery is recommended, consent is obtained “verbally” with 2 providers to complete the verification process. The after visit summary, supplementary documents, and patient education materials can be provided to families through the EMR application.
Provider education on video visits occurred daily during the first few weeks of our adaptation to the pandemic. There was an assigned provider who was readily available to answer all trouble shooting questions as they arose. An updated tip sheet for video visits was sent out via email to all providers on a weekly basis.
Patient reported outcome (PRO) questionnaire
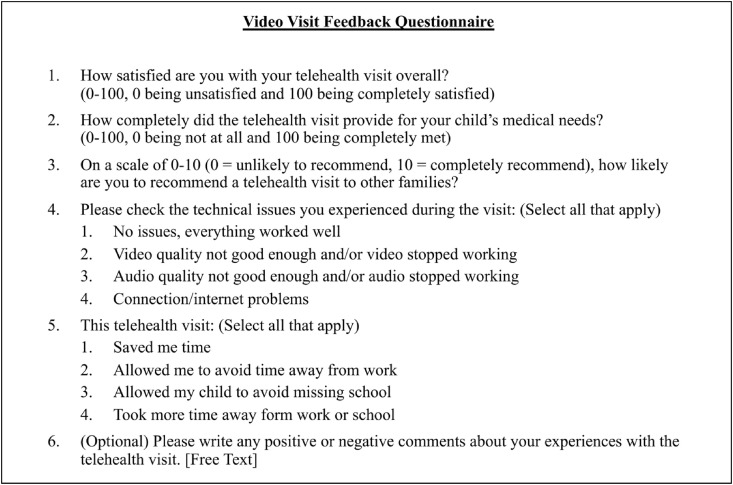
A PRO questionnaire was designed that consisted of six questions focused on the quality and effectiveness of the video visits (Fig. 1 ). The six questions were created using the National Quality Forum telehealth measures framework, which encompasses a visit's impact on access to care, patient/family experience and a visit's effectiveness [11], and the Telehealth Usability Questionnaire (TUQ), which measures the quality and reliability of a telehealth questionnaire [12]. Patients and families who had a video visit from November 2019 to April 2020 were contacted 3–5 days after the video visit via a secure web survey application (RedCap) to complete the questionnaire. They were given two reminders via email to complete the questionnaire the following week.
Figure 1.
Video visit feedback questionnaire.
The open-ended comments reported in the PRO questionnaire were autocoded for sentiment using NVivo software (released March 2020) [13]. The Nvivo software analyzes individual words for positive and negative sentiment. Because the software does not take context into account, the results were reviewed by 2 authors (CJL and ZSG), and the comments were further classified into the following categories based on the sentiment(s) expressed: positive, negative, both positive and negative, and neutral (no sentiment expressed).
Results
A total of 631 video visits were conducted during the study interval. 453 patients were male (72%) and 178 were female (28%). The median age of patients at time of visit was 7 years (IQR 2–12 years), median visit time was 20 min (IQR 15–30 min), and the median travel distance saved by performing a VV was 12.2 miles (IQR 6.3–26.8 miles). Prior to the onset of the COVID-19 pandemic, 100% of VV were post-operative visits. Since the onset of the pandemic, the majority of visits were follow up evaluations (334 patients, 53%), though new patient visits (172 patients, 27%) and post-operative visits (125 patients, 20%) were frequent as well. The number of monthly VV increased substantially from 1 to 10 patients prior to the pandemic to 308 patients in March 2020 and 283 in April 2020 (Supplementary Fig. 1). Visit diagnoses are further summarized in Table 1 , the most common of which were nocturnal enuresis and foreskin concerns.
Table 1.
Top 10 diagnoses for telehealth visits and corresponding satisfaction scores.
| Number | Diagnosis | ICD-10 | Frequency (% of total visits) | Median overall satisfaction score (0–100) |
|---|---|---|---|---|
| 1 | Nocturnal enuresis | N39.44 | 75 (11.9%) | 98 |
| 2 | Redundant prepuce and phimosis | N47.8 | 56 (8.9%) | 92 |
| 3 | Urinary tract infection, uncomplicated | N39.0 | 35 (5.5%) | 91 |
| 4 | Other hydrocele | N43.2 | 25 (4.0%) | 91 |
| 5 | Urge incontinence | N39.41 | 22 (3.5%) | 89.5 |
| 6 | Kidney stone | N20.0 | 21 (3.3%) | 99 |
| 7 | Hypospadias | Q54.0 | 21 (3.3%) | 100 |
| 8 | Congenital hydronephrosis | Q62.0 | 20 (3.2%) | 96 |
| 9 | Penoscrotal hypospadias | Q54.2 | 18 (2.9%) | 96 |
| 10 | Vesicoureteral reflux without reflux nephropathy | N13.71 | 17 (2.7%) | 67 |
A total of 325/631 (51.5%) families completed the PRO questionnaire from November 2019 to April 2020. Results are summarized in Table 2 . Families reported a high overall satisfaction with the video visits (median score of 10/10) and perceived that the video visits adequately provided for their child's medical needs. 90% of families stated that they would strongly recommend a telehealth visit to other families. The vast majority of families experienced no technical difficulties, with only 15.6% of families reporting either audio or video issues and 7.6% reporting internet connection issues. For the top 10 diagnoses, satisfaction scores were generally around 90 or higher, with the exception of vesicoureteral reflux (Table 1). Based on corresponding parent comments, the lower scores in this category were attributed to technical difficulties. The median score for various diagnoses related to undescended testicles (ICD codes Q53.10, Q53.112, Q53.20, Q53.212, Q53.9) was only 71.
Table 2.
Patient satisfaction survey results.
| Question | Median (IQR) |
|---|---|
| How satisfied are you with your telehealth visit overall? (0–100, 0 being unsatisfied and 100 being completely satisfied) | 96 (79–100) |
| How completely did the telehealth visit provide for your child's medical needs? (0–100, 0 being not at all and 100 being completely met) | 97.5 (81–100) |
| On a scale of 0–10 (0 = unlikely to recommend, 10 = completely recommend), how likely are you to recommend a telehealth visit to other families? | 10 (8–10) |
| Please check the technical issues you experienced during the telehealth visit: | |
| No issues, everything worked well | 81.6% |
| Video quality not good enough and/or video stopped working | 8.8% |
| Audio quality not good enough and/or audio stopped working | 6.8% |
| Connection/Internet problems | 7.5% |
| This telehealth visit: | |
| Saved me travel time | 95.2% |
| Allowed me to avoid time away from work | 37.4% |
| Allowed my child to avoid missing school | 18.4% |
| Took more time away from work/school | 0% |
Sample comments by classification are provided in Table 3 . Of the comments completed by 158 respondents in the PRO questionnaire, 72.8% were deemed positive. Of these comments, families mentioned saved travel time and avoidance of missed work and school as benefits, as well as the desire to continue VVs after the pandemic. 7.2% of comments were negative; common themes identified were technical difficulties and the perception that an in-person evaluation would be preferable or more thorough. 10.0% of comments were deemed to have both positive and negative sentiments. Several of these comments acknowledged the convenience of VVs while expressing a need or preference for an in-person visit. 10.0% of comments were neutral.
Table 3.
Sample comments from the video visit feedback questionnaire.
| Positive (72.8%) | “It saved us driving a long distance, having to pay for a sitter for our other children, the cost of meals while traveling, and was a very quick appointment with no waiting room time!” “Telehealth visits are a great tool for us as we live approx 2 h from the physical location and this provided us with great flexibility in today's world.” “This is great - right now I'm working from home due to Covid but when life goes back to normal this could save me from missing multiple days from work and him missing school.” “I realize this telehealth visit was due to COVID-19, but I would highly recommend this as an option for certain visits once we are out of the pandemic.” |
| Negative (10.0%) | “I did not feel like the doctor could provide a thorough evaluation.” “I still prefer face to face for a medical doctor visit.” “While the visit was fine, it was very unnerving to have my child expose himself on the camera.” “We tried it on both my husband's and my computer and it didn't work on either- one is a PC and mine is a brand new Mac, and our internet was at full strength so I'm not sure exactly why we couldn't get connected!” |
| Both positive and negative (10.0%) | “We unfortunately still need to see the doctor in person for a possible ongoing issue, but overall we were able to get our questions answered and it saved us from having to go in just to have an incision checked.” “In general I liked the convenience, but again I do worry a little that the examination wasn't as effective as it would have been in person.” “It would be nice to have my doctor examine my child in person, but this is a nice alternative to avoid the extensive travel that some patients do and/or the exposure to Covid.” “Teleheath may be more difficult if she was ill, however, it is perfect for routine visits and follow up.” |
| Neutral (7.2%) | “Purpose of telehealth visit was due to the pandemic going on.” “Many thanks for the survey!” |
Discussion
Despite the availability of telehealth for 2 years in our large pediatric urology practice, its utilization has been limited. The COVID-19 pandemic contact restrictions led to calls within the urologic community to broaden the applications of VV, expanding the use of telemedicine beyond limited postoperative evaluations to include routine follow up visits in addition to new patient visits [14,15]. Our VV volume before included 46 visits over a 21-month period to a current volume of 585 visits over the course of 2 months.
Existing telemedicine studies in pediatric urology have demonstrated good patient satisfaction for video visits, specifically post-operative visits6-8 and new patient referrals9. To our knowledge, our study is the first in the pediatric urology telemedicine literature to demonstrate positive patient-reported outcomes in a cohort including return patient visits outside of the immediate post-operative setting, while also including the largest number of new patient visits to date. We have demonstrated high patient satisfaction in a cohort with a wide variety of diagnoses, including dysfunctional voiding, neurogenic bladder, circumcision evaluation, and urinary tract dilation. Families who reported high satisfaction with the video visits overall recounted experiences such as the convenience of completing a visit in their homes and the ability to connect with multiple providers at the same time. Families’ willingness to recommend telehealth visits to other families indicates that they found the visits to be effective in communicating their needs and determining a plan of care. Considering travel time saved for patients among other benefits, telemedicine at this larger scale may have a role in routine care delivery even beyond the COVID-19 pandemic.
We experienced some challenges inherent to telemedicine. There were various technical and connectivity issues reported by families and providers alike, including poor quality of the audio and/or visual of the visit and difficulty logging into the mobile app. Some of the technical and connectivity issues were resolved before the start of the visit's scheduled time, but there were some persistent issues that led to video visits being converted to telephone visits. In addition, as the most frequently encountered barrier to telemedicine adoption at the staff level has previously been identified as technically-challenged staff [16], our process involves routine education of all providers and staff involved in the care of the patient. This includes not only the attending physicians and advanced practice providers, but also surgery schedulers, outpatient schedulers, and the billing team. Continued education will be a critical approach to continue in the future to ensure sustainability of VV.
While a large portion of visits are amenable to a VV, the limitations of remote evaluations were a challenge for some diagnoses. For instance, the evaluation of an undescended testicle was inconsistent, and our preference going forward would be for an in-person evaluation. This preference is reflected by the relatively low median satisfaction score of 71 for patients with undescended testicles. Another challenge that is present, but more easily addressed, is the need for radiographic imaging. In this setting, some families obtained studies and either mailed hard copies to our office or had them transferred electronically prior to the scheduled video visit, facilitating review. Coordinating this process can be time-consuming for all parties involved.
At the institutional level, a primary barrier to more widespread telehealth implementation has been a lack of reimbursement from insurance companies. Traditionally, Medicare could only cover telehealth on a limited basis, such as when the patient is in a designated rural area and leaves their home to go to a medical facility – essentially where an in-person encounter would have taken place – for service. Other payers typically did not cover telehealth either. However, during the early onset of the pandemic in March 2020, the 1135 Stafford Act waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act was implemented, allowing Medicare to pay for both new and established patient visits conducted via telehealth from a range of providers, including doctors, nurse practitioners, and licensed clinical social workers, with time-based tiers of reimbursement and without location or geographic restrictions [17]. Thus, when reimbursement restrictions were nearly universally eliminated during the pandemic, institutions were allowed to explore the feasibility of the telehealth option for their patient population. Based on the patient satisfaction data, the telehealth visits allowed during this exploration period were clearly on par with if not an improvement to prior visits for a large number of our patients. This access to a different form of health care delivery warrants continued consideration going forward, considering the benefits of a remote evaluation for families given the restraints of school, work, and travel costs.
This study is not without limitations. We performed this analysis within a single health system and thus the results may not be applicable to all pediatric urologic practices. EMRs vary by institution; therefore, our platform may not be transferrable to other institutions, although the basic principles of telemedicine should be applicable, as should some of the workflow concepts (for example, providing role-specific educational materials to patients, providers, and all staff involved, providing patients with a help line number beforehand, sending weekly tip sheets to providers, etc. – described in the “Telemedicine Workflow Outline” section under “Materials and Methods”). Families included in the study required an electronic device (desktop or preferably mobile device) and either a mobile app on their phone or access to the institution's website, which may not be accessible for all patients. Our demonstration of high patient satisfaction is limited to completed VVs and does not provide a comparison with in-person visits, which may be incorporated into future studies. Regardless, telemedicine provides an adjunct to patient care, and expanding its use more broadly to follow up and new patient visits may ultimately improve health care delivery.
Conclusions
Telemedicine can be effectively utilized for multiple visit types in pediatric urology, including new, return, and postoperative visits, with overall positive feedback from families. Consideration should be given to the continued utilization of telemedicine for a wide range of visits in the future beyond the COVID-19 pandemic.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This work was approved by the Institutional Review Board of the Children's Hospital of Philadelphia.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpurol.2021.05.012.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Mechanic O.J., Kimball A.B. StatPearls. Treasure Island; FL: 2020. Telehealth systems. [PubMed] [Google Scholar]
- 2.American Medical Association . 2020. Digital Health Research: physicians' motivations and requirements for adopting digital health - adoption and attitudinal shifts from 2017-2019.https://www.ama-assn.org/system/files/2020-02/ama-digital-health-study.pdf Retrieved from. [Google Scholar]
- 3.Whited J.D. Economic analysis of telemedicine and the teledermatology paradigm. Telemed J e Health. 2010;16:223–228. doi: 10.1089/tmj.2009.0100. [DOI] [PubMed] [Google Scholar]
- 4.Powell R.E., Stone D., Hollander J.E. Patient and health system experience with implementation of an enterprise-wide telehealth scheduled video visit program: mixed-methods study. JMIR Med Inform. 2018;6:e10. doi: 10.2196/medinform.8479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finkelstein J.B., Cahill D., Young K., Humphrey K., Campbell J., Schumann C. Telemedicine for pediatric urological postoperative care is safe, convenient and economical. J Urol. 2020 Jul;204(1):144–148. doi: 10.1097/JU.0000000000000750. Epub 2020 Jan 17. PMID: 31951495. [DOI] [PubMed] [Google Scholar]
- 6.Larson J.L., Rosen A.B., Wilson F.A. The effect of telehealth interventions on quality of life of cancer survivors: a systematic review and meta-analysis. Health Inf J. 2018 Jun;24(6):397–405. doi: 10.1089/tmj.2017.0112. Epub 2017 Nov 7. PMID: 29112484. [DOI] [PubMed] [Google Scholar]
- 7.Committee On Pediatric W., Marcin J.P., Rimsza M.E., Moskowitz W.B. The use of telemedicine to address access and physician workforce shortages. Pediatrics. 2015;136:202–209. doi: 10.1542/peds.2015-1253. [DOI] [PubMed] [Google Scholar]
- 8.Smith A.C., Thomas E., Snoswell C.L., Haydon H., Mehrotra A., Clemensen J. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020 Jun;26(5):309–313. doi: 10.1177/1357633X20916567. Epub 2020 Mar 20. PMID: 32196391; PMCID: PMC7140977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ray K.N., Mehrotra A., Yabes J.G., Kahn J.M. Telemedicine and outpatient subspecialty visits among pediatric medicaid beneficiaries. Acad Pediatr. 2020 Jul;20(5):642–651. doi: 10.1016/j.acap.2020.03.014. Epub 2020 Apr 8. PMID: 32278078; PMCID: PMC7194998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Winkelman A.J., Beller H.L., Morgan K.E., Corbett S.T., Leroy S.V., Noona S.W. Benefits and barriers to pediatric tele-urology during the COVID-19 pandemic. J Pediatr Urol. 2020 Dec;16(6):840.e1–840.e6. doi: 10.1016/j.jpurol.2020.09.028. Epub 2020 Oct 8. PMID: 33077389; PMCID: PMC7543732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Quality Forum . 2017. Creating a framework to support measure development for telehealth; pp. 1–80.http://www.qualityforum.org/Publications/2017/08/Creating_a_Framework_to_Support_Measure_Development_for_Telehealth.aspx [Google Scholar]
- 12.Parmanto B., Lewis A.N., Jr., Graham K.M., Bertolet M.H. Development of the telehealth usability questionnaire (TUQ) Int J Telerehabilitation. 2016;8:3–10. doi: 10.5195/ijt.2016.6196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.QSR International Pty Ltd 2020. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home NVivo (released in March 2020)
- 14.Connor M.J., Winkler M., Miah S. COVID-19 pandemic - is virtual urology clinic the answer to keeping the cancer pathway moving? BJU Int. 2020;125:E3–E4. doi: 10.1111/bju.15061. [DOI] [PubMed] [Google Scholar]
- 15.Gadzinski A.J., Gore J.L., Ellimoottil C., Odisho A.Y., Watts K.L. Implementing telemedicine in Response to the COVID-19 pandemic. J Urol. 2020;204:14–16. doi: 10.1097/JU.0000000000001033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scott Kruse C., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24:4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Medicare telemedicine health care provider fact sheet. Centers for Medicare & medicaid services newsroom. March 17, 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.