Abstract
Treatment of cartilage defects such as osteoarthritis (OA) and osteochondral defect (OCD) remains a huge clinical challenge in orthopedics. OA is one of the most common chronic health conditions and is mainly characterized by the degeneration of articular cartilage, shown in the limited capacity for intrinsic repair. OCD refers to the focal defects affecting cartilage and the underlying bone. The current OA and OCD management modalities focus on symptom control and on improving joint functionality and the patient’s quality of life. Cell-based therapy has been evaluated for managing OA and OCD, and its chondroprotective efficacy is recognized mainly through paracrine action. Hence, there is growing interest in exploiting extracellular vesicles to induce cartilage regeneration. In this review, we explore the in vivo evidence of exosomes on cartilage regeneration. A total of 29 in vivo studies from the PubMed and Scopus databases were identified and analyzed. The studies reported promising results in terms of in vivo exosome delivery and uptake; improved cartilage morphological, histological, and biochemical outcomes; enhanced subchondral bone regeneration; and improved pain behavior following exosome treatment. In addition, exosome therapy is safe, as the included studies documented no significant complications. Modifying exosomal cargos further increased the cartilage and subchondral bone regeneration capacity of exosomes. We conclude that exosome administration is a potent cell-free therapy for alleviating OA and OCD. However, additional studies are needed to confirm the therapeutic potential of exosomes and to identify the standard protocol for exosome-based therapy in OA and OCD management.
Keywords: extracellular vesicle, exosome, chondrocyte, cartilage, osteoarthritis
Introduction
Osteoarthritis (OA) is a common disease linked to mobility-related disability. In 2020, an estimated 654 million people worldwide had knee OA.1 Rising obesity and population aging are the main contributors to the increasing prevalence and incidence of OA.2 OA is a chronic inflammatory disease that causes the deterioration of articular cartilage, which leads to joint pain and stiffness.3 OA is not confined to the articular cartilage, but also affects the synovium, subchondral bone, and joint ligaments.4 Osteochondral defect (OCD) develops when cartilage lesions caused by OA affect the subchondral bone.5 However, OCD can also be caused by traumatic injury.6
Currently, no treatment can halt the progression of OA. However, treatments are available for relieving the symptoms. Treatments for OA can be classified into non-pharmacologic, pharmacologic, surgical, and alternative therapies such as regenerative therapy. Non-pharmacologic treatments are recommended for OA caused by modifiable risk factors (eg obesity). Weight loss is associated with improvement in cartilage structure by reducing the joint load.7 Exercise has also been proven to relieve pain and improve muscle strength in OA patients.8,9 Nevertheless, these treatments are more effective for lower limb OA. Pain is the hallmark symptom of OA. Therefore, pharmacologic treatment is mainly used for managing pain. The classical pain-relieving treatments for OA include acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs).10 However, the usage of these drugs increases the risk of gastrointestinal and cardiovascular toxicity.11 The surgical approach is preferred when conservative treatments are not effective. Although most patients have improved quality of life after surgery, potential complications such as pain, infection, and poorer knee function must be taken into consideration when opting for surgical intervention.12 In addition, knee replacement implants have limited lifespans and may fail eventually.13 OCD treatment can be categorized into non-surgical and surgical. Non-surgical treatment includes rest, joint immobilization, and pain-relieving medication. OCD can also be corrected surgically by removing the lesion, microfracture drilling, retrograde drilling, antegrade drilling, cancellous bone graft implantation, osteochondral transplantation, and autologous chondrocyte implantation.14
Regenerative therapy is a rapidly growing approach used for treating OA and OCD due to conventional therapies being unsatisfactory, only managing to provide symptom control and short-term functional improvement. The conventional therapies fail to address the underlying problem of cartilage and osteochondral bone loss.15 Several preclinical studies have proven that intra-articular injection of mesenchymal stem/stromal cells (MSCs) enhances cartilage and meniscal tissue regeneration, and slows OA progression by attenuating synovial membrane inflammation.16,17 Similarly, a few preclinical studies have reported OCD regeneration by MSCs.18,19 Clinically, intra-articular injection of adipose-derived MSCs (AD-MSCs) is safe and produces significant functional improvement in OA and OCD patients.20–22 Recently published systematic reviews have shown that MSC therapy is safe and can improve pain and joint function significantly, but the improvement in cartilage regeneration, based on structural assessment by magnetic resonance imaging (MRI), is not statistically significant.23,24 Although no major adverse effects have been reported, we should remain aware of the possible risks associated with cell therapies. These include differentiation into undesirable cell types or tissues and the pro-tumorigenic effect of MSCs.25–30 The transplantation of autologous AD-MSCs caused renal fibrosis and inflammatory cell infiltration in the interstitium of a patient with chronic kidney disease, and the reason might be the differentiation of the multipotent stem cells recruited by the MSCs into myofibroblasts or the differentiation of the transplanted MSCs into myofibroblasts.31,32
A paradigm shift has recently occurred, as MSCs and their conditioned medium were found to have similar therapeutic effects.33–35 Many papers have summarized that the primary mechanism of action of MSC therapy is paracrine signaling via extracellular vesicles (EVs).36–38 The use of EVs can mitigate the risk of transdifferentiation of transplanted MSCs into the wrong cells in response to the local milieu while retaining the beneficial therapeutic effects exerted by MSC paracrine secretion. Furthermore, the use of EVs can also minimize the risk of rejection of donor stem cells and tumor formation (especially for embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs)).
EVs can be categorized into three groups based on their biogeneses, ie microvesicles, exosomes, and apoptotic bodies.39 Lai et al40 found that the exosome is the active component in MSC-conditioned medium. Exosomes are nanosized intraluminal vesicles in multi-vesicular bodies (MVBs) secreted by various cell types upon MVB fusion with the plasma membrane.41 They play a major role in cell–cell communication by transferring their contents, including proteins, lipids, and nucleic acids.42 MSC-derived exosomes have drawn much attention recently for their broad therapeutic effect on various diseases such as myocardial infarction, liver fibrosis, cutaneous wound healing, and OA.43–47 A recent study reported that exosomes aid bidirectional signaling between MSCs and chondrocytes for chondrogenesis, ECM deposition, and cell proliferation, suggesting that they are important in communication between native heterogeneous cell populations of cartilage tissue, and thus are the crucial paracrine factors in cartilage repair.48
Apart from identifying the biogenesis pathway, a concrete means of distinguishing the EV subtypes is absent due to the lack of techniques for purifying and specific markers for the EV subtypes.49 Moreover, the size of EVs is heterogeneous and overlap among the subtypes.50,51 In fact, the generic term “extracellular vesicles” or “EVs” should be used.49 In the present systematic review, the term “exosomes” essentially refers to 50–200 nm EVs, without demonstration of their origin and/or purity, with regard to the nomenclature used by the authors.
Recently, several systematic reviews reported the potential of using MSC-derived EVs to promote cartilage regeneration in preclinical in vivo studies.52–54 However, EVs derived from other cell sources have also been used for promoting cartilage regeneration. Thus, the present review was aimed at summarizing the broad literature and evidence on the effects of exosome therapy derived from all cell sources on cartilage repair. Only results from preclinical in vivo studies were considered.
Literature Search, Article Selection and Data Extraction
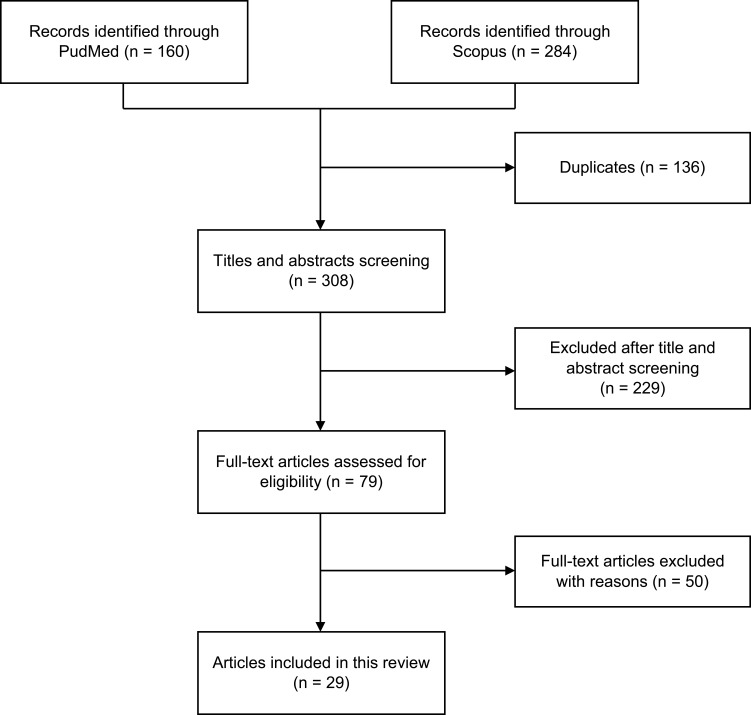
The literature search was conducted from December 30, 2020, to January 6, 2021, on the PubMed and Scopus databases using the following keywords: (exosome OR extracellular vesicle) AND (cartilage OR osteoarthritis OR osteochondral). We included all preclinical and clinical studies reporting the safety and efficacy of EVs on cartilage regeneration. Studies reporting only in vitro findings were excluded. We also excluded secondary literature, studies only available in abstract form, conference/proceeding papers, letters to the editor, theses, and articles written in languages other than English. Figure 1 shows the article identification and selection process. In brief, a total of 160 articles from PubMed and 284 articles from Scopus were identified. After deduplication and title and abstract screening, 79 articles were obtained for full-text screening. Finally, a total of 29 articles published between 2016 and 2021 were included in this review. All included articles reported in vivo findings without any clinical data. Two reviewers (C.Y.N. and J.Y.C.) conducted the literature search, article selection, and data extraction independently. The methodological quality of the studies was assessed using the Systematic Review Center for Laboratory Animal Experimentation (SYRCLE) risk of bias tool.55 Meta-analysis was not performed due to the lack of quantitative data for pooling because of the heterogeneity in the scoring systems and exosome isolation methods used. Thus, the results extracted were analyzed qualitatively.
Figure 1.
Flow diagram of article selection process.
Results and Discussion
Quality of Studies
The included studies were graded using the SYRCLE risk of bias assessment tool.55 Table 1 summarizes the risk of bias analysis. There is no high risk of bias among the 29 included studies. All the included studies have low risk of selective outcome for reporting bias and other sources of bias were not detected. However, only nine studies (31.0%) were assigned low risk of bias and 20 studies (69.0%) had unclear risk of bias for baseline characteristics (ie animal species, age, gender, and weight) in selection bias. Furthermore, all studies showed unclear risk in most of the domains, including sequence generation and allocation concealment for selection bias, random housing and blinding for performance bias, random outcome assessment and blinding for detection bias, and incomplete outcome data for attrition bias. The lack of detailed documentation in the included articles resulted in a high unclear risk of bias and ambiguous methodological quality.
Table 1.
Summary of Risk of Bias Analysis Using SYRCLE Tool
| References | Selection Bias | Performance Bias | Detection Bias | Attrition Bias | Reporting Bias | ||||
|---|---|---|---|---|---|---|---|---|---|
| Sequence Generation | Baseline Characteristics | Allocation Concealment | Random Housing | Blinding | Random Outcome Assessment | Blinding | Incomplete Outcome Data | Selective Outcome Reporting | |
| Zhang et al68 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Cosenza et al74 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Liu et al58 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Tao et al60 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Wang et al61 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Zhu et al72 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Mao et al59 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Wang et al79 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Zhang et al69 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Chen et al73 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Liu et al82 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Wu et al64 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Zhang et al70 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Zheng et al81 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Chen et al56 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| He et al75 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Jin et al76 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Jin et al57 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Liang et al77 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Liu et al78 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Qiu et al83 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Wong et al63 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Yan and Wu66 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Zavatti et al67 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Zhang et al84 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Zhou et al71 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Wang et al80 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Wang et al62 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
| Yan et al65 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk |
Source of Exosomes
Exosomes were extracted from a variety of cell sources. Seventeen studies used human exosomes,56–72 nine studies used murine exosomes,73–81 one study used rabbit exosomes,82 and two studies did not mention the cell origin83,84 (Table 2).
Table 2.
Cell Sources, Exosome Isolation, and Characterization
| References | Cell Sources | Cell Types | Exosome Isolation | Exosome Characterization |
|---|---|---|---|---|
| Zhang et al68 | Human | HuES9 ESC-MSCs | Size fractionation and TFF Exosomes were stored at −20 °C until use |
NTA: Homogenously sized with modal size of 100 nm Western blot: Positive for CD81, ALIX, and TSG101 RNA detection: Majority less than 300 nucleotides |
| Cosenza et al74 | Murine | BM-MSCs from C57BL/6 mice | Ultracentrifugation | DLS: 96 nm NTA: 112 ± 6.6 nm Flow cytometry: Positive for CD9 and CD81 |
| Liu et al58 | Human | iPSC (iPSC-01)-MSCs | Ultracentrifugation and ultrafiltration | TEM: Spherical morphology; 30 to 60 nm TRPS: 50 to 150 nm Western blot: Positive for CD9, CD63, and CD81 |
| Tao et al60 | Human | Normal SM-MSCs and miR-140-5p-overexpressing SM-MSCs from knee joint synovial membrane tissue of 30 to 35 years old donors | Ultrafiltration and ultracentrifugation on 30% sucrose/D2O cushion Used freshly |
TEM: Hollow spherical microvesicles DLS: 30 to 150 nm Western blot: Positive for CD63, CD9, CD81, and ALIX RT-qPCR: Increased miR-140-5p expression level in miR-140-5p overexpressed SM-MSC-Exos |
| Wang et al61 | Human | Male H1 ESC-MSCs | Ultracentrifugation Exosomes were stored in PBS at −80 °C |
TEM: Round lipid bilayer vesicles; 38 to 169 nm Western blot: Positive for CD63 and CD9 |
| Zhu et al72 | Human | iPSC (C1P33)-MSCs | Ultrafiltration The exosomes aliquot was stored −80 °C or used freshly |
TEM: Cup or round-shaped TPRS: 50 to 150 nm Western blot: Positive for CD9, CD63, and TSG101 |
| Human | SM-MSCs from 3 donors (2 males and 1 female, age range 22 to 28 years) | Ultrafiltration The exosomes aliquot was stored −80 °C or used freshly |
TEM: Cup or round-shape TPRS: 50 to 150 nm. Western blot: Positive for CD9, CD63, and TSG101 |
|
| Mao et al59 | Human | Normal BM-MSCs and miR-92a-3p-overexpressing BM-MSCs from 6 donors (3 males and 3 females, ranged of 32 to 38 years old) | Ultracentrifugation | TEM: Cup-shaped or round morphology; 50 to 150 nm NTA: 50 to 150 nm. Western blot: Positive for CD9, CD63, CD81, and HSP70 |
| Wang et al79 | Murine | Normal MSCs, TGF-β1 stimulated MSCs and miR-135b inhibited MSC from SD rats | Exosome extraction kit | TEM: Hollow-spherical morphology Western blot: Positive for CD63, CD9, and CD81; higher CD81 and ALIX levels in TGF-β1-MSC-Exos RT-qPCR: Increased miR-135b expression level in TGF-β1-MSC-Exos |
| Zhang et al69 | Human | Immortalized E1-MYC 16.3 ESC-MSCs | Size fractionation and TFF Exosomes were stored at −20 °C until use |
Size determination: Homogenously sized particles; 100 nm model size Western blot: Positive for CD81, ALIX, and TSG101 Flotation density: 1.10 to 1.19 g/mL |
| Chen et al73 | Murine | BM-MSCs from articular cartilage from femoral condyles and tibial plateau of C57BL/6 mice | Ultrafiltration and ultracentrifugation on 30% sucrose/D2O cushion | TEM: Hollow spherical vesicles DLS: 40 to 110 nm in diameter Western blot: Positive for TSG101, CD9, and CD63 |
| Liu et al82 | Rabbit | PRP isolated from whole blood of New Zealand white rabbits | Membrane-based affinity binding step using exoEasy Maxi Kit Exosomes were stored at −80 °C until used |
TEM: Round-shaped morphology NTA: 145.6 ± 50.4 nm Western blot: Positive for CD9, CD63, CD81, and HSP101 |
| Wu et al64 | Human | IPFP-MSCs from patients with primary knee OA | Precipitation (ExoQuick reagent kit) or ultrafiltration Exosomes were stored at −80 °C for further use |
No significant differences between exosomes isolated from precipitation and ultrafiltration TEM: Sphere-shaped bilayer membrane structure about 100 nm in diameter NTA: 121.9 nm Western blot: Positive for CD81, CD9, and CD63 Flow cytometry with CiO-labeling: 30 nm to 150 nm |
| Zhang et al70 | Human | Immortalized E1-MYC 16.3 ESC-MSCs | Size fractionation and TFF Exosomes were stored at −20 °C until use |
Size determination: 100 to 200 nm Western blot: Positive for CD81, ALIX, and TSG101 Flotation density: 1.10 to 1.19 g/mL |
| Zheng et al81 | Murine | Primary chondrocytes from knee articular cartilage of 5 to 6 days old C57BL/6 mice cultured in standard or inflammatory environment (degenerative chondrocytes) | Ultrafiltration and ultracentrifugation with 30% sucrose/D2O | TEM: Hollow and spherical-like morphology DLS: 40 to 110 nm Western blot: Positive for TSG101, CD9, and CD63 Mass spectrometry: 2409 and 2077 proteins were identified in primary chondrocytes and degenerative chondrocytes, respectively |
| Chen et al56 | Human | Normal BM-MSCs and miR-136-5p-overexpressed BM-MSCs from femur bone marrow of traumatized patients | Ultrafiltration and ultracentrifugation with 30% sucrose/D2O | TEM: Hollow spherical microvesicles DLS: 50 to 150 nm Western blot: Positive for CD63, CD9, CD81, and ALIX; but very low TSG101 RT-qPCR: Upregulated miR-136-5p expression level in miR-136-5p overexpressed BM-MSC-Exos |
| He et al75 | Murine | BM-MSCs from SD rats | Ultracentrifugation | TEM: Oval in shape DLS: 153 nm Western blot: Positive for flotillin-1, TSG101, and CD63; negative for calnexin |
| Jin et al76 | Murine | Normal BM-MSCs and miR-9-5p overexpressed BM-MSCs | Ultracentrifugation Exosomes were stored at −80 °C |
TEM: Round or tea-shaped with outer membrane; 40 to 100 nm Western blot: Positive for CD9, TSG101, and CD63; negative for calnexin |
| Jin et al57 | Human | Normal BM-MSCs and miRNA-26a-5p overexpressed-BM-MSCs from ilium of healthy volunteers | Precipitation (ExoQuick-TC reagent kit) | TEM: Round or oval-shaped; 30 to 100 nm DLS: 50 to 100 nm Western blot: Positive for CD63, Hsp70, and CD90 RT-qPCR: Upregulated miR-26a-5p expression level in miR-26a-5p overexpressed BM-MSC-Exos |
| Liang et al77 | Murine | CAP-Lamp2b dendritic cells | Ultracentrifugation Exosomes were stored at −80 °C miR-140 mimic is introduced into exosomes by electroporation |
TEM: Cup-shaped morphology; 40 to 200 nm NTA: 40 to 200 nm Western blot: Positive for CD63 and CD9 Confocal microscope: Fluorescence signals of CAP-GFP-Exos |
| Liu et al78 | Murine | Normal BM-MSCs from SD rats and BM-MSCs treated with kartogenin | TFF and HPLC Exosomes were stored at −80 °C |
TEM: Cup or round-shaped morphology NTA: 50 to 200 nm Western blot: Positive for CD63 and CD81 |
| Qiu et al83 | Not reported | Normal BM-MSCs and curcumin pre-treated BM-MSCs | Ultrafiltration | TEM: Round-shaped morphology; 50 to 150 nm Western blot: Positive for CD9, CD63, and CD81 |
| Wong et al63 | Human | E1-MYC 16.3 ESC-MSCs | Size fractionation and TFF Exosomes were stored at −20 °C until use |
Size determination: 100 to 200 nm Western blot: Positive for CD81, ALIX, and TSG101 |
| Yan and Wu66 | Human | UC-MSCs cultured in 2D and 3D (hollow-fiber bioreactor) | Ultracentrifugation Exosomes were stored at −80 °C until used |
TEM: Cup-shaped morphology NTA: 120 nm Western blot: Positive for CD63, CD81, and TSG101; negative for calnexin |
| Zavatti et al67 | Human | AFSCs from pregnant women (mean age of 35.7) between the 16th and 17th weeks of gestation | Precipitation (total exosome isolation solution) | Western blot: Positive for CD9, CD63, CD81, and Rab5 |
| Zhang et al84 | Not reported | BM-MSCs | Ultrafiltration and ultracentrifugation with sucrose cushion Exosomes were stored at −80 °C or used freshly |
TEM: Cup-like shape NTA: 140 nm Western blot: Positive for CD63, CD81, and CD9; negative for cerulean |
| Zhou et al71 | Human | Polydactyly BM-MSCs | Precipitation (total exosome isolation kit) | TEM: 30 to 150 nm Western blot: Positive for CD63 and CD9 |
| Human | BM-MSCs | Precipitation (total exosome isolation kit) | TEM: 30 to 150 nm Western blot: Positive for CD63 and CD9 |
|
| Wang et al80 | Murine | OA serum from OA mice and sham serum from sham mice | Norgen’s proprietary resin-based purification (Serum Exosome Purification Mini Kit) ATF4-OA-Exos were constructed by introducing ATF4 mRNA into OA-Exos through electroporation. |
TEM: Spherical-shaped morphology NTA: 0 to 150 nm Western blot: Positive for ALIX and CD63 RT-qPCR: Highest expression level of ATF4 in ATF4-OA-Exos, followed by OA-Exos and sham-Exos |
| Wang et al62 | Human | Normal SM-MSCs and miR-155-5p-overexpressing SM-MSCs | Not reported | TEM: Cup-shaped morphology NTA: 100 to 120 nm Western blot: Positive for CD63 and CD81; negative for TFIIB RT-qPCR: 60-fold higher miR-155-5p expression in miR-155-5p overexpressed SM -MSC-Exos compared to SM-MSC-Exos |
| Yan et al65 | Human | UC-MSCs cultured in static environment and rotary cell culture system | Ultracentrifugation Exosomes were stored at −80 °C |
TEM: Cup-shaped morphology NTA: 120 nm Western blot: Positive for CD63, CD81, and TSG101; low calnexin RT-qPCR: Increased lncRNA H19 expression level in exosomes collected from cells cultured in rotary cell culture system |
Abbreviations: AFSC, amniotic fluid stem cell; BM-MSC, bone marrow-derived mesenchymal stem/stromal cell; CAP-Lamp2b, chondrocyte-affinity peptide-lysosome-associated membrane glycoprotein 2b; D2O, deuterium oxide; DLS, dynamic light scattering; ESC-MSC, embryonic stem cell-derived mesenchymal stem/stromal cell; Exo, exosome; IPFP-MSC, infrapatellar fat pad-derived mesenchymal stem/stromal cell; iPSC-MSC, induced pluripotent stem cell-derived mesenchymal stem/stromal cell; lncRNA, long non-coding RNA; miR, microRNA; MSC, mesenchymal stem/stromal cell; NTA, nanoparticle tracking analysis; PBS, phosphate-buffered saline; PRP, platelet-rich plasma; RT-qPCR, reverse transcription quantitative polymerase chain reaction; SD rat, Sprague Dawley rat; SM-MSC, synovial membrane-derived mesenchymal stem/stromal cell; TEM, transmission electron microscopy; TFF, tangential flow filtration; TGF-β1, transforming growth factor beta 1; TPRS, tunable resistive pulse sensing; UC-MSC, umbilical cord-derived mesenchymal stem/stromal cell.
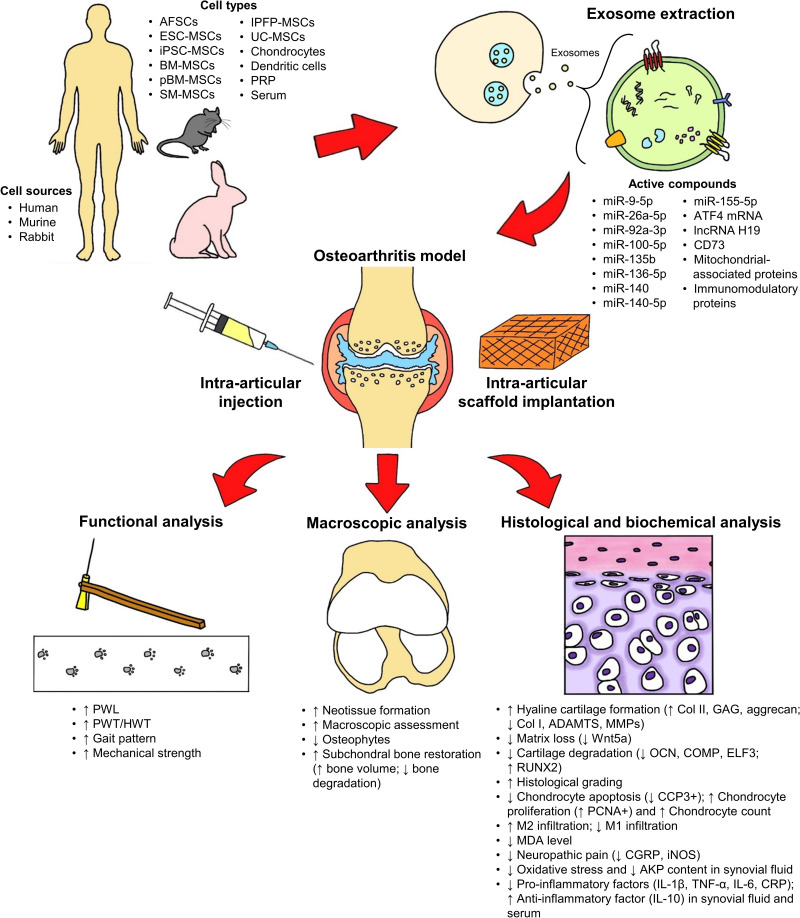
Regarding cell type, 25 studies reported the use of exosomes from stem cells, namely ESC-derived MSCs (ESC-MSCs),61,63,68–70 iPSC-derived MSCs (iPSC-MSCs),58,72 amniotic fluid stem cells (AFSCs)67 and other adult stem cells, including bone marrow-derived MSCs (BM-MSCs),56,57,59,71,73–76,78,83,84 synovial membrane-derived MSCs (SM-MSCs),60,62,72 infrapatellar fat pad-derived MSCs (IPFP-MSCs),64 umbilical cord-derived MSCs (UC-MSCs),65,66 polydactyly BM-derived MSCs (pBM-MSCs),71 and commercial MSCs of unknown tissue origin.79 Exosomes from primary chondrocytes,81 platelet-rich plasma (PRP),82 dendritic cells,77 and serum80 were also studied.
Exosomes have similar biological functions as parental cells.39,85 Most of the studies included in this review used MSCs as the source of exosomes due to the predominant therapeutic benefits of MSCs in tissue repair and regeneration. MSCs have self-renewal, differentiation, anti-apoptotic, anti-fibrotic, pro-mitotic, anti-oxidative, and immunomodulatory properties.86–88 Besides, MSCs can be harvested from many tissue sources using minimally invasive techniques.89 MSCs can also be expanded easily for many passages without significant changes in characteristics and functionality, and produce more exosomes.90,91 Currently, the most ideal cell source of exosomes for promoting cartilage regeneration remains ambiguous. In the present review, only two studies compared the efficacy of exosomes secreted by different cell sources.71,72 Zhu et al72 used exosomes secreted by iPSC-MSCs and SM-MSCs, and found that iPSC-MSC-secreted exosomes were more effective in supporting cartilage regeneration. Neotissue of the iPSC-MSC-derived exosome-treated group presented typical hyaline features and intense type II collagen staining in the superficial and deep zones of cartilage tissue, which were comparable to the healthy cartilage in the control group. On the other hand, the SM-MSC-derived exosome-treated group exhibited moderate cartilage repair and very weak type II collagen staining in the superficial cartilage zone, but the results were nevertheless better compared to the untreated cartilage in the OA group. Zhou et al71 reported that pBM-MSC-secreted exosomes were more potent in facilitating cartilage repair compared to those secreted by BM-MSCs, as demonstrated by the lower Osteoarthritis Research Society International (OARSI) scores. Exosomes secreted by MSCs of different tissue sources show distinctive therapeutic results, as the exosomal cargo varies according to the tissue origin.92–94 The therapeutic potential of exosomes secreted by MSCs isolated from different tissues has been summarized in the reviews of Álvarez-Viejo,95 Nikfarjam et al,96 Yin et al,97 and Tang et al.98
Modification of Exosomal Cargo for Enhancing Efficacy
Exosomes mediate cell–cell communication by transporting bioactive lipids, proteins, and RNAs, including mRNAs, and non-coding RNAs such as microRNAs (miRNAs) and long non-coding RNAs (lncRNAs).99 We identified 15 studies that only used exosomes derived from naïve cells.58,61,63,67–75,81,82,84 All naïve exosomes promoted the repair and regeneration of damaged cartilage. Zhang et al69,70 reported that exosomal CD73 from naïve ESC-MSCs contributed to cartilage repair by inducing AKT and ERK phosphorylation in chondrocytes. Chen et al73 suggested that BM-MSC-derived exosomes restored the mitochondrial dysfunction of degenerated chondrocytes by supplementing mitochondrial-related proteins. Another study noted that normal chondrocyte-derived exosomes carried proteins that involved in mitochondrial function and immune system process, which are important in alleviating OA progression.81 On the contrary, 14 articles modified and loaded exosomes with specific therapeutic agents, and reported enhanced therapeutic efficacy of cartilage regeneration compared to naïve exosomes.56,57,59,60,62,64–66,76–80,83 Exosomal cargo can be modified via preconditioning of the exosome-secreting cells; incubating the exosome-secreting cells with the therapeutic cargo (eg drugs, proteins, RNAs, nanomaterials); transfection of the exosome-secreting cells; and physical treatments such as electroporation, sonication, extrusion, surfactant treatment, dialysis, and freeze-thawing.100
The genomic molecules within exosomes aid the regulation of gene expression.101 Valadi et al102 were the first to discover the presence of mRNAs and miRNAs in exosomes, and indicated that exosomes could modify the protein production and gene expression of target cells by transferring exosomal mRNAs or miRNAs. Wang et al80 investigated the therapeutic effect of the activating transcription factor 4 (ATF4) gene in cartilage regeneration by introducing ATF4 mRNA into exosomes via electroporation. The effects of exosomes derived from OA serum (OA-Exos) and ATF4 mRNA-overexpressing exosomes (ATF4-OA-Exos) were compared, and showed that the ATF4-OA-Exos were more potent compared to the OA-Exos in preventing and alleviating cartilage degeneration via the stimulation of autophagy.
miRNAs play a critical role in the post-transcriptional regulation of a wide range of physiological processes, including cartilage homeostasis, and the pathological processes in disorders such as OA.103,104 In the past few years, there has been growing emphasis on determining the biological function of miRNAs in regenerative medicine.105,106 Given the eminent role of miRNAs in cartilage regeneration, six studies included here used transfection to upregulate specific miRNAs, ie miR-9-5p, miR-26a-5p, miR-92a-3p, miR-136-5p, miR-140-5p, and miR-155-5p, in exosomes.56,57,59,60,62,76 All miRNA-overexpressing exosomes showed superior therapeutic potential compared to the naïve exosomes by regulating the target genes and their downstream signaling pathways in the recipient cells. Mao et al59 revealed that exosomal miR-92a-3p downregulated the Wnt signaling pathway via WNT5A, eventually causing lower ECM degradation. Comparing the results of exosome-treated groups with and without antagomir-miR-100-5p, Wu et al64 reported that IPFP-MSC-derived exosomes ameliorated cartilage damage and the gait patterns of OA mice by delivering miR-100-5p into the recipient chondrocytes, leading to activation of the miR-100-5p-mediated mTOR autophagy pathway. In another study, miR-140 was loaded into exosomes through electroporation, and the miR-140-overexpressing exosomes were more effective compared to the naïve exosomes in suppressing the progression of cartilage degeneration and in enhancing cartilage regeneration.77 Additionally, miR-135b was increased in exosomes secreted by transforming growth factor (TGF)-β1-stimulated MSCs.79 The exosomal miR-135b downregulated Sp1 protein expression, leading to better cartilage regeneration in rats with OA.79
LncRNAs are involved in the transcriptional and post-transcriptional regulation of many biological processes related to cartilage development, degeneration, and regeneration, and can be transferred by exosomes to recipient cells.107,108 Yan et al studied the role of exosomal lncRNA H19 in cartilage regeneration.65 The exosomal lncRNA H19 played an important role in cartilage regeneration by promoting chondrocyte proliferation and matrix production whilst suppressing apoptosis. In vivo, injecting exosomes rich in lncRNA H19 led to greater improvement in cartilage repair, with uniform tissue, obscured boundaries, and lower T2 values on MRI analysis compared to that of cartilage tissue treated with exosomes secreted by UC-MSCs transfected with small interfering RNA (siRNA) against H19.65 In that study, the 10-fold increase in exosomal lncRNA H19 was achieved by exposing the cells to mechanical stimulus via culture in a rotary cell culture system (RCCS).
These results clearly show that exosomal cargo can be modulated by modifying the culture condition. The changes in exosomal cargo, such as higher miR-135b expression in TGF-β1-stimulated MSC-derived exosomes and higher lncRNA H19 expression in exosomes secreted by UC-MSCs exposed to mechanical stimulus, enhanced cartilage regeneration in vivo.65,79 Additionally, preconditioning BM-MSCs with kartogenin and curcumin improved the therapeutic potential of the secreted exosomes for treating OA.78,83 However, the studies did not examine the differences in the exosomal cargos of preconditioned and naïve cells.
Apart from modulating the exosomal cargo, cell preconditioning can also stimulate exosome secretion. Yan and Wu66 collected exosomes secreted by UC-MSCs cultured in 2D and 3D (using a hollow-fiber bioreactor) conditions. The 3D culture had increased exosome yield (7.5-fold higher), and the exosomes secreted by 3D-culture UC-MSCs showed more potent therapeutic effects in promoting cartilage repair compared to the exosomes secreted by the 2D-culture UC-MSCs, as indicated by the greater surface regularity and better thickness of OA cartilage in vivo. Similarly, Yan et al65 also found that UC-MSCs cultured in 3D conditions using a RCCS secreted exosomes with increased yield and therapeutic potential in treating OA. Consistent with this, Yang et al109 and Cao et al110 attained higher exosome yields from cells cultured in 3D conditions, and the exosomes showed improved therapeutic potential, albeit for different indications.
The above results demonstrate the importance of exosomal cargo modification for achieving better performance. Additionally, exosomal cargo profiling is crucial for elucidating the mechanism of action.
In vivo Delivery and Exosome Uptake
Cartilage is an avascular and alymphatic tissue.111 Thus, unlike in other tissue injuries, exosomes are not suitable for infusing intravenously for treating cartilage defects. In fact, all of the included studies administered exosomes directly to the affected joint, as intra-articular administration increases bioavailability and reduces off-target effects, thereby improving the delivery of exosomes to the cartilage and decreasing the dose of exosomes needed.112 The exosomes were either injected or encapsulated in a scaffold. Some studies used a single injection and others used multiple injections to treat cartilage injuries. Currently, it remains unclear if multiple injections are more effective compared to single injection for promoting cartilage regeneration, as none of the studies compared the therapeutic effect of single and multiple injections. Cosenza et al74 and Wang et al80 showed that the effect of exosomes from a single intra-articular injection may be month-long. This is most probably due to the direct exosome administration to the target site (cartilage is avascular and alymphatic; thus, the clearance of the injected exosomes is slower) and the exosomes might induce cellular reprogramming and remodel resident or injured cells by activating regenerative mechanisms by transferring bioactive molecules.113–115
The findings of the 29 studies are summarized in Table 3 and illustrated in Figure 2. To date, direct injection appears to be a more popular cell delivery method, as only a few studies58,73,78 used a scaffold to deliver exosomes to the injured cartilage tissues. A scaffold is beneficial for sustaining the delivery of exosomes for a longer period and also aids exosome homing to the injury site. Additionally, combining exosomes and biomaterial can create a synergistic effect to promote cartilage regeneration. Liu et al58 found that the implantation of in situ hydrogel glue with iPSC-MSC-derived exosomes was more potent for promoting cartilage regeneration compared to in situ hydrogel glue implantation and iPSC-MSC-derived exosome injection, supported by the formation of a smoother surface with fully filled regenerated tissue that integrated with the surrounding cartilage. The histological findings were supported by the results of optical coherence tomography (OCT), which displayed a uniform and well-organized articular cartilage structure in the in situ formed iPSC-MSC-exosome–hydrogel tissue patch implantation group.
Table 3.
Summary of Efficacy and Safety Findings
| References | Animal Models | Method of Delivery | Treatment Groups | Euthanasia | Efficacy Outcome | Safety Outcome | ||
|---|---|---|---|---|---|---|---|---|
| Macroscopic and Functional Analysis | Imaging | Histological and Biochemical Analysis | ||||||
| Zhang et al68 | SD rats Surgically induced OCD |
Multiple intra-articular injections after surgery and thenceforth weekly | 1. Exo group: 100 µg/100 µL of ESC-MSC-Exos 2. Contralateral control: 100 µL PBS 3. Un-operated control |
Week 6 or 12 post-surgery | ● Exo group demonstrated almost complete neotissue filling with good surface regularity and complete integration of neotissue with surrounding cartilage by 12 weeks | Not reported | ● Exo group exhibited almost complete regeneration and bonding of cartilage and underlying subchondral bone after 12 weeks ● Distinctly higher modified O’Driscoll histological scores in the Exo group ● Exo group showed hyaline cartilage formation with high amount of GAG, Col II, and low amount of Col I |
No detrimental responses were observed in all animals |
| Cosenza et al74 | C57BL/6 mice Collagenase-induced OA |
Single intra-articular injection at day 7 after OA induction | 1. Cell group: 2.5×105 BM-MSCs/5 µL 2. MP group: 500 ng/5 µL of BM-MSC-microvesicles 3. Exo group: 250 ng/5 µL of BM-MSC-Exos 4. OA group 5. Healthy control |
Day 42 post-collagenase induction | Not reported | ● CLSM showed structural improvement in articular cartilage which comparable with healthy control group in all treatment groups ● µCT showed higher bone volume, lower bone degradation, lower osteophyte formation and lower calcification of menisci and ligaments in all treatment groups compared to the OA group |
● Exo group showed the greatest improvement with the lowest OA scores | Not reported |
| Liu et al58 | New Zealand rabbits Surgically created OCD |
Scaffold implantation or single intra-articular injection immediately after surgery | 1. EHG group: 20 µL in situ formed EHG tissue patch containing 1 × 1011/mL iPSC-MSC-Exos 2. HG group: 20 µL in situ formed HG tissue patch 3. Pre-EHG group: 20 µL in vitro preformed EHG containing 1 × 1011/mL iPSC-MSCs-Exos 4. Inj-Exo group: 20 µL of 1 × 1011/mL iPSC-MSCs-Exos suspension 5. OA group: Saline rinsing |
Week 12 post-surgery | ● EHG group showed the best repair with smooth surface with white regenerated tissue fully filled the defects and integrated with surrounding cartilage | ● OCT displayed uniform and well-organized articular cartilage structure in EHG group | ● EHG group has the highest ICRS score and the neotissue was almost entirely hyaline cartilage (strong safranin O and Col II staining, weak Col I staining) | Not reported |
| Tao et al60 | SD rats Surgically induced OA |
Multiple intra-articular injections on the first day of week 5 to 8 after surgery | 1. Exo group: 100 µL of 1011 SM-MSC-Exos particles/mL 2. Exo-miR-140-5p group: 100 µL of 1011 miR-140-5p overexpressed SM-MSC-Exos particles/mL 3. OA group: Saline 4. Healthy control: Saline |
Week 12 post-surgery | Not reported | Not reported | ● Exo-miR-140-5p group showed the lowest OARSI assessment scores ● Significant increased chondrocyte count, higher Col II and aggrecan expression, and lower Col I in the Exo-miR-140-5p group compared to the Exo and OA groups |
No adverse events occurred |
| Wang et al61 | C57BL/6 J mice DMM induced OA |
Intra-articular injections at week 4 after surgery (once for Cell and Cell-OA group; multiple injections every 3 days for 4 weeks for Exo and Exo-OA group) | 1. Cell group: 5 μL of 1×106 ESC-MSC suspension 2. OA group: 5 µL of PBS 3. Sham control 1. Exo group: 5 µL ESC-MSC-Exos 2. OA group: 5 µL of PBS 3. Sham control |
Week 8 post-surgery | Not reported | Not reported | ● Exo group exhibited similar regenerative effect as Cell group. ● Exo group revealed milder OA pathology compared to the OA group which was concomitant with lower OARSI scores and stronger Col II staining and weaker ADAMTS5 and aggrecan neoepitope staining |
Not reported |
| Zhu et al72 | C57B/L10 mice Collagenase-induced OA |
Multiple intra-articular injections on day 7, 14 and 21 after collagenase administration | 1. iPSC-MSC-Exo group: 8 µL of 1×1010 particles/mL iPSC-MSC-Exos 2. SM-MSC-Exo group: 8 µL of 1×1010 particles/mL SM-MSC-Exos 3. OA group: 8 µL of PBS 4. Normal control: 8 µL of PBS |
Day 28 post-collagenase induction | ● No significant differences in ICRS macroscopic analysis scores among the normal, iPSC-MSC-Exo and SM-MSC-Exo groups, but significant higher than the OA group | Not reported | ● Neotissue of iPSC-MSC-Exo group presented smooth cartilage, regular cellular organization and normal proteoglycan content that similar to control group; SM-MSC-Exo exhibited moderate surface irregularity, superficial fibrillation in neotissue and lower proteoglycan in cartilage, but the results were better compared to the OA group ● No significant differences in OARSI scores between the iPSC-MSC-Exo and normal group, but notable lower than the SM-MSC-Exo and OA groups ● More intense Col II staining in the iPSC-MSC-Exo group compared to the SM-MSC-Exo group |
Not reported |
| Mao et al59 | C57B/L10 mice Collagenase-induced OA |
Multiple intra-articular injections on day 7, 14 and 21 after collagenase administration | 1. Exo group: 15 µL of 500 µg/mL BM-MSC-Exos 2. Exo-miR-92a-3p group: 15 µL of 500 µg/mL miR-92a-3p overexpressed BM-MSC-Exos 3. OA group: 15 µL of PBS 4. Healthy control: 15 µL of PBS |
Day 28 after collagenase induction | Not reported | Not reported | ● Exo-miR-92a-3p group demonstrated significant reduced severity of cartilage matrix loss with higher Col II and aggrecan, and lower Wnt5a and MMP13 expressions in both gene and protein levels compared to the Exo and OA groups | Not reported |
| Wang et al79 | SD rats Surgically induced OA |
Intra-articular injection | 1. Exo group: 100 µL of 1×1011 particles/mL MSC-Exos 2. TGF-β1-Exo group: 100 µL of 1×1011 particles/mL TGF-β1-MSC-Exos 3. TGF-β1-NC-Exo group: 100 µL of 1×1011 particles/mL TGF-β1-MSC-NC-Exos 4. TGF-β1-miR135b inhibitor-Exo group: 100 µL of 1×1011 particles/mL TGF-β1-MSC-miR135b inhibitor-Exos |
Week 12 post-surgery | Not reported | Not reported | ● Significant lower OARSI scores in the TGF-β1-Exo group than the Exo group, with high OARSI scores in the TGF-β1-miR135b inhibitor-Exo group ● TGF-β1-Exo group showed elevated number of chondrocytes, while dropped in chondrocyte number was recorded in the Exo and TGF-β1-miR135b inhibitor-Exo groups |
Not reported |
| Zhang et al69 | SD rats Surgically induced OCD |
Multiple intra-articular injections immediately after surgery on weekly basis | 1. Exo group: 100 µg/100 µL ESC-MSC-Exos 2. Contralateral control: 100 µL PBS |
Week 2, 6 or 12 | Not reported | Not reported | ● Exo group demonstrated predominately hyaline cartilage regeneration (mostly Col II and very low Col I expression) and complete integration of neotissue with adjacent native cartilage with a smooth surface regularity and complete regeneration of subchondral bone at week 12 ● Wakitani scores of Exo group decreased from week 2 to 12 and the results were significantly lower than the contralateral control ● Enhanced proliferation, attenuated apoptosis, increased M2 macrophages and reduced M1 macrophages in both cartilage and synovium tissues, and decreased in M1-associated cytokines, ie, IL-1β and TNF-α, in synovial fluid of the Exo group |
Not reported |
| Chen et al73 | New Zealand white rabbits Surgically induced OCD |
3D printed scaffold implantation | 1. ECM/GelMA group: ECM/GelMA scaffold 2. GelMA group: GelMA scaffold 3. ECM/GelMA/Exo group: 3D printed ECM/GelMA/BM-MSC-Exo scaffold 4. OA group: untreated |
Week 6 or 12 post-surgery | ● ECM/GelMA/Exo group exhibited smooth and intact tissues and gave the highest ICRS macroscopic analysis scores | ● MRI scanning demonstrated smooth neo-cartilage and great defect filling in both ECM/GelMA and ECM/GelMA/Exo groups ● µCT displayed increased ratio of bone volume to tissue volume, trabecular thickness and ossified tissues in the subchondral bone of both ECM/GelMA and ECM/GelMA/Exo groups |
● ECM/GelMA and ECM/GelMA/Exo groups showed hyaline-like cartilage regeneration in the defect sites ● ECM/GelMA/Exo group has higher ICRS visual histological scores at week 12 ● Increased Col II and decreased of MMP13 expression in the synovial membrane of ECM/GelMA and ECM/GelMA/Exo groups ● ECM/GelMA/Exo group expressed the lowest MDA levels |
No apparent pathological effects in myocardium, liver, and kidney 1 to 2 weeks after transplantation |
| Liu et al82 | New Zealand white rabbits Surgically induced OA |
Multiple intra-articular injections once a week | 1. Exo group: 100 µg/mL PRP-Exos 2. PRP-As group: 100 µg/mL activated PRP 3. OA group: normal saline 4. Control: normal saline |
Week 6 after surgery | Not reported | Not reported | ● Exo group exhibited more regular arrangement of chondrocytes, clearer tidal line, reduced hyperplasia on articular cartilage surface and lower OARSI scores than the PRP-As and OA groups ● Exo group showed increased expression of Col II and RUNX2 |
No adverse events occurred |
| Wu et al64 | C57BL/6 mice DMM induced OA |
Multiple intra-articular injections twice a week, starting at week 4 after surgery | 1. Exo group: 10 µL of 1010 particles/mL IPFP-MSC-Exos 2. OA group: 10 µL PBS 3. Sham control: 10 µL PBS |
Week 8 post-surgery | ● Improved gait pattern (CatWalk gait analysis) after 6 weeks of exosome treatment | ● Obvious green fluorescent dots (DiO-labeled IPFP-MSC-Exos) can be found at the defect sites | ● Exo group showed integration of cartilage with smooth surface and lower OARSI scores confirming cartilage lesion was healed ● Exo group showed higher expression of Col II as well as lower expression of ADAMTS5 and MMP13 |
Not reported |
| 3 weeks of 10 µL antagomir pre-injection (once a week), starting at week 1 after surgery, followed by injection of Exos and antagomir twice a week for 4 weeks | 1. PBS + antagomir-NC group: 10 µL PBS + antagomir-NC; 2. Exo + antagomir-NC group: 10 µL 1010 particles/mL IPFP-MSC-Exos + antagomir-NC 3. Exo + antagomir-100-5p group: 10 µL 1010 particles/mL IPFP-MSC-Exos + antagomir-100-5p |
Week 8 post-surgery | Not reported | Not reported | ● Exo + antagomir-100-5p group reversed the results of the Exo group | Not reported | ||
| Zhang et al70 | SD rats MIA-induced TMJ-OA |
Multiple intra-articular injections once a week, starting 2 weeks after OA induction | 1. Exo group: 100 µg/50 µL of ESC-MSC-Exos 2. OA group: 50 µL of PBS 3. Sham control: needle pricks |
Week 2, 4 or 8 post-treatment | ● HWT improved gradually in the Exo group and reached the baseline level of the sham group at week 5 | ● µCT showed Exo group restored subchondral bone volume and architecture at week 8 | ● Exo group revealed significant reduced gene expressions of pro-inflammation (IL-1β), apoptosis (BAX), fibrosis (α-SMA) and pain (Substance P, CGRP, NGF, P75NTR and TrkA) and upregulated TIMP 2 and downregulated ADAMTS5 in condylar cartilage tissues ● Significant lower Mankin scores at week 4 and 8 in the Exo group ● Exo group showed smoother cartilage surface, improved cellularity, reduced fibrous cartilage thickening, minimal depletion of s-GAG in condylar cartilage lesion at week 4 and marked restoration of TMJ condylar structure at week 8 ● Exo group has lesser MMP13+ cells in condyle region at week 4; lesser IL-1β+ and iNOS+ cells, higher proliferative PCNA+ cells and lesser CCP3+ apoptotic cells at week 4 and 8 |
No adverse immune reactions observed |
| Zheng et al81 | C57BL/6 mice Surgically induced OA |
Multiple intra-articular injections once per week, starting 10 days after surgery | 1. Exo group: 200 µg of primary chondrocyte-Exos 2. OA group: 20 µL saline 3. Sham control: Untreated |
Week 4, 6 or 8 post-surgery | Not reported | ● µCT demonstrated lower subchondral bone mineral density and smaller osteophyte formation at the joint margins in the Exo group | ● Both femoral and tibia cartilage of the Exo group showed nearly complete preservation ● No obvious synovitis appearance in all groups ● Exo group expressed marked repression in MMP13 staining and elevated Col II staining in joint samples ● Significant lower OARSI scores in the Exo group ● Exo group exhibited higher level of M2 macrophages infiltration in the synovium and cartilage tissues |
Not reported |
| Chen et al56 | C57BL/6 mice Mechanical load induced OA |
Single intra-articular injection immediately after mechanical induction | 1. Exo group: 100 µL of 1011 particles/mL BM-MSC-Exos 2. Exo-miR-136-5p group: 100 µL of 1011 particles/mL miR-136-5p overexpressed BM-MSC-Exos 3. OA group: Untreated 4. Normal control: Untreated |
One hour after injury | Not reported | Not reported | ● Exo-miR-136-5p group showed lesser loss of cartilage matrix followed by the Exo and OA groups ● Exo-miR-136-5p group revealed higher level of Col II and aggrecan gene and protein expressions, decreased in ELF3 and MMP13 gene and protein expressions |
Not reported |
| He et al75 | SD rats MIA-induced OA |
Multiple intra-articular injections once a week, starting one week after OA induction | 1. Exo group: 40 µg/100 µL BM-MSC-Exos 2. OA group: 100 µL of normal saline 3. Sham control: 100 µL of normal saline |
Week 6 post-treatment | ● Joint injuries were alleviated in the Exo group ● Thermal PWL and mechanical PWT improved at weeks 2,4 and 6 in the Exo group |
● In vivo imaging showed accumulation of PKH26 labeled BM-MSC-Exos in the joint cavity | ● Articular cartilage of the Exo group regenerated, with small number of defects and fractures on cartilage surface ● Exo group has significantly reduced OARSI scores ● Exo group demonstrated notably increased in Col 2 protein expression level in chondrocytes and ECM, and decreased of MMP13 and Col 1 protein levels in cartilage tissue ● Exo group showed reduced expression of CGRP and iNOS in DRG ● Lower inflammatory cytokines (IL-1β, IL-6 and TNF-α) and higher anti-inflammatory cytokine (IL-10) in serum of Exo group |
Not reported |
| Jin et al76 | SD rats Surgically induced OA |
Intra-articular injection, starting two weeks after OA induction | 1. Exo group: BM-MSC-Exos 2. OA group: Normal saline |
Week 7 post-treatment | Not reported | Not reported | ● Lower observation and Mankin scores in the cartilage of the Exo group ● Notably decreased in inflammatory factors, AKP content and oxidative stress injury indicators, but increased in SOD in synovial fluid of the Exo group. ● Cartilage tissue of Exo group showed significant reduced MMP13, OCN and COMP gene and protein expressions |
Not reported |
| 1. Exo group: BM-MSC-Exos 2. Exo-miR-9-5p group: miR-9-5p overexpressed BM-MSC-Exos 3.Exo-miR-9-5p inhibitor group: miR-9-5p inhibited BM-MSC-Exos 4.Exo-miR-mimic-NC group: miR-9-5p mimic NC BM-MSC-Exos 5. Exo-miR-inhibitor-NC group: miR-9-5p inhibitor NC BM-MSC-Exos 6. Liposomes miR-9-5p group: miR-9-5p-embedded liposomes 7. Sham control |
Not reported | Not reported | ● Exo-miR-9-5p group exhibited the lowest observation and Mankin scores among the treated groups ● Lower OA infiltration in the Exos, Exo-miR-mimic-NC and Exo-miR-inhibitor-NC group, and improved cartilage regeneration in the exo-miR-9-5p group ● Exo-miR-9-5p group has the lowest expression level of inflammatory factors, AKP content, and oxidative stress injury indicators, as well as highest level of SOD in synovial fluid among all the treated groups ● Exo-miR-9-5p group showed the lowest gene and protein expressions of MMP13, OCN and COMP in cartilage tissue compared to all the treated groups |
Not reported | ||||
| Jin et al57 | Wistar rats Surgically induced OA |
One-week intra-articular injection of treatments after surgery | 1. Exo-miR-26a-5p group: 250 ng/5 µL of miR-26a-5p overexpressed BM-MSC-Exos 2. Exo-miR-NC group: 250 ng/5 µL of miR-NC BM-MSC-Exos 3. OA group: Untreated 4. Sham control: Untreated 5. Healthy control: Untreated |
Week 8 post-surgery | Not reported | Not reported | ● Exo-miR-26a-5p group has less pathological changes with the concomitant of reduced synovial tissue proliferation and suppressed inflammation ● Exo-miR-26a-5p group has lower MMP3 and MMP13 expression and higher apoptotic index in synovial cells ● Notably increased of miR-26a-5p expression and declined of PTGS2 expression in synovial tissue of the Exo-miR-26a-5p group ● Exo-miR-26a-5p group showed reduced serum IL-1β levels |
Not reported |
| Liang et al77 | SD rats DMM induced OA |
Multiple intra-articular injections post-injury, once per week | 1. Exo group: 100 µg of Exos particles in 100 µL PBS 2. Exo-miR140 group: 100 µg of Exo-miR140 particles in 100 µL PBS 3. CAP-Exo-miR140 group: 100 µg of CAP-Exo-miR140 particles in 100 µL PBS 4. OA group: Untreated 5. Sham control: Untreated |
Week 8 post-surgery | Not reported | ● Fluorescence microscopy showed that CAP-Exo-miR-140 mainly stayed in the articular cavity, while Exo-miR-140 distributed to other body parts and enriched in kidney | ● CAP-Exo-miR140 group displayed smooth and flat cartilage surface, small joint space, proper cell alignment, normal subchondral bone and dense proteoglycan which was almost identical to the sham control and comparable OARSI scores with sham control ● CAP-Exo-miR140 group suppressed the MMP13 and Adamts5 protein levels in cartilage tissue ● Upregulation of miR-140 and downregulation of MMP13 gene expression in cartilage tissue in the CAP-Exo-miR140 group |
Non-toxic to major organs (heart, liver, kidney, lung, and spleen) |
| Liu et al78 | SD rats Surgically induced OCD |
Intra-articular implantation | 1. Exo group: Col-Tgel hydrogel with BM-MSC-Exos 2. KGN-Exo group: Col-Tgel hydrogel with KGN-BM-MSC-Exos 3. Gel group: Col-Tgel hydrogel 4. OA group: untreated 5. Normal control: untreated |
Week 4, 6 and 8 post-surgery | ● Better cartilage regeneration in the KGN-Exo group as indicated by smoother articular surface and better integration of newly formed cartilage with adjacent host cartilage ● KGN-Exo group exhibited higher ICRS macroscopic scores which were comparable with the normal group at 8 weeks |
Not reported | ● KGN-Exo group revealed better cartilage reconstruction with hyaline cartilage predominantly, corresponding to notable high ICRS visual histological scores ● KGN-Exo group showed increased s-GAG in cartilage tissue started at week 2 ● More lubricin and Col II positive cells and less Col I positive cells in KGN-Exo group compared to other groups except for the normal control group |
Not reported |
| Qiu et al83 | Mice Surgically induced OA |
Not mentioned | 1. Exo-Cur group: Curcumin pre-treated BM-MSC-Exos 2. Exo group: BM-MSC-Exos 3. OA group 4.Sham control |
Not reported | Not reported | Not reported | ● Exo-Cur group showed higher gene expression of miR-124 and miR-143 as well as lower protein expression of ROCK1, NF-kB and TLR9 that were similar to the sham control group ● Exo-Cur group has less apoptotic chondrocytes compared to the OA and Exo groups |
Not reported |
| Wong et al63 | New Zealand white rabbits Surgically induced OCD |
Multiple intra-articular injections at day 0, day 7 and day 14 post-surgery | 1. Exo + HA group: 1 mL of 3% (w/v) hyaluronic acid with 200 µg ESC-MSC-Exos 2. HA group: 1 mL of 3% (w/v) hyaluronic acid |
Week 6 or 12 post-treatment | ● Significant improvement in ICRS scores of Exo + HA group at week 6 and 12, associated with marked improvements of neotissue integration at the border zone ● Exo + HA group displayed improved mean Young’s moduli and stiffness of the repaired cartilage that approximated the normal tissue |
Not reported | ● Exo + HA group showed improvements in cartilage regeneration over time as confirmed by complete defect coverage by neotissue characterized by the presence of hyaline cartilage, normal cellularity and chondrocytic-like cells, high GAG and Col II deposition, and lower Col I deposition at week 12 ● Exo + HA group exhibited higher modified O’Driscoll scores than the HA group at week 6 and 12 |
No adverse events |
| Yan and Wu66 | New Zealand rabbits Surgically induced cartilage defect |
Multiple intra-articular injections on a weekly interval | 1. 2D-Exo group: 500 µL of 1×1010 particles/mL 2D cultured UC-MSC-Exos 2. 3D-Exo group: 500 µL of 1×1010 particles/mL 3D cultured UC-MSC-Exos 3. OA group: 500 µL PBS |
Week 4 post-treatment | ● Significant improvement in ICRS macroscopic scores in the 3D-Exo group compared to the 2D-Exo and OA groups ● 3D-Exo group demonstrated more neotissue formation with smoother surface and better integration with the native hyaline cartilage at the surrounding |
Not reported | ● 3D-Exo group displayed partly hyaline cartilage and the defects showed greater surface regularity and better thickness of cartilage than the 2D-Exo group ● 3D-Exo group exhibited lower Wakitani score than the 2D-Exo and OA groups |
Not reported |
| Zavatti et al67 | CD rats MIA-induced OA |
Intra-articular injection 3 weeks after OA induction (once for Cell and OA groups; twice for Exo group with 10 days interval) | 1. Cell group: 50 µL of 5×105 AFSCs 2. Exo group: 50 µL of 100 µg AFSC-Exos 3. OA group: 50 µL of glucose/PBS 4.Contralateral control |
Week 3 post-treatment | ● Cell and Exo groups have higher pain tolerance, and the results were comparable to the normal control group | Not reported | ● Exo group showed better cartilage regeneration as indicated by complete neotissue formation with good surface regularity compared to the cell-treated defects which exhibited few fissures on the cartilage surface ● Uniformed GAG distribution was demonstrated in the Exo group ● Both Exo and Cell groups exhibited improved OARSI scores ● Cell group displayed more intense Col II staining, whereas Exo group showed more regular distribution of Col II |
No adverse inflammatory responses were observed |
| Zhang et al84 | SD rats Surgically induced OA |
Intra-articular injection every 3 days for 4 weeks, starting at week 4 post-operation | 1. Exo group: 10 µL 1010 particles/mL BM-MSC-Exos 2. OA group: 10 µL PBS 3. Sham control |
Week 4 post-treatment | Not reported | ● µCT showed less cartilage degradation, near-normal chondrocyte morphology and distribution, and less osteophyte formation around the joint treated with Exo ● Dil-labeled Exo were observed in the knee joint and taken up by the synovial cells |
● Lower OARSI scores in the Exo group compared to the OA group ● Exo group demonstrated upregulated chondrogenic gene expressions and downregulated hypertrophic gene expressions ● Exo group has decreased synovial hyperplasia and cell filtration ● Exo group has less M1-positive cells and more M2-positive cells ● Exo group exhibited reduced pro-inflammatory cytokines (IL-1β, TNF-A) and increased anti-inflammatory cytokine (IL-10) in synovial fluid ● Exo group showed significant reduction in synovitis scores |
Not reported |
| Zhou et al71 | C57BL/6J mice Collagenase VII induced OA |
Multiple intra-articular injections at day 7, 14 and 21 after collagenase induction | 1. Exo group: BM-MSC-Exos 2. pExo group: polydactyly BM-MSC-Exos 3. OA group: Saline 4.Normal control |
Day 28 post-collagenase VII injection | Not reported | Not reported | ● pExo group alleviated cartilage damage evidenced by the significant lower OARSI scores than the OA and Exo groups | Not reported |
| Wang et al80 | C57BL/6J mice Surgically induced OA |
Single intra-articular injection at week 4 post-operation | 1. Sham-Exo group: 200 µg sham-Exos 2. OA-Exo group: 200 µg OA-Exos 3. ATF4-OA-Exo group: 200 µg ATF4-OA-Exos 4. OA group 5.Sham control |
Week 8 post-surgery | Not reported | ● µCT showed reduced osteophyte formation in Sham-Exo and ATF4-OA-Exo groups, while OA-Exo group displayed enlarged osteophytes | ● Sham-Exo and ATF4-OA-Exo groups alleviated pathological injury of articular tissues observed in the OA group, whereby the ATF4-OA-Exo group exerted greater therapeutic effect and lesser proteoglycan loss ● ATF4-OA-Exo group exhibited lower Mankin scores than the Sham-Exo group, while OA-Exo group aggravated the cartilage damage and exhibited the highest Mankin scores among all groups ● ATF4-OA-Exo group gave stronger effect in upregulating Col II levels and downregulating MMP13 levels ● ATF4-OA-Exo group was more potent in decreasing inflammatory cytokine levels in the cartilage ● ATF4-OA-Exo group partially restored the impeded autophagy of the OA cartilage |
Not reported |
| Wang et al62 | BALB/C mice 4°C water stimulated OA |
Multiple intra-articular injection once a day, starting from day 20 after OA induction | 1. Exo group: 30 µL of 1011 particles/mL SM-MSC-Exos 2. Exo-155-5p group: 30 µL of 1011 particles/mL miR-155-5p overexpressed SM -MSC-Exos 3. OA group: normal saline 4.Normal control |
Two weeks post-treatment | Not reported | Not reported | ● Exo-155-5p group revealed lower OARSI scores and higher chondrocyte number in femoral condyle ● Exo and Exo-155-5p groups reversed the increased caspase-3 and decreased Col II expressions in OA femoral condyle sections, but Exo-155-5p was more effective |
Not reported |
| Yan et al65 | SD rats Surgically induced cartilage defects |
Multiple intra-articular injections on a weekly interval | 1. S-Exo group: 100 µL of 1 mg/mL rotary cell culture system cultured UC-MSC-Exos 2. si-Exo group: 100 µL of 1 mg/mL rotary cell culture system cultured siRNA H19 transfected UC-MSC-Exos 3. OA group: 100 µL PBS |
Week 4 or 8 | ● S-Exo group revealed reduced pain with higher LWT at week 3 ● Defects covered with neotissue at week 4 and were filled with uniform tissue and obscured boundaries at week 8 in the S-Exo group ● S-Exo group showed the highest ICRS scores |
● Defects of S-Exo group displayed similar intensity to the adjacent cartilage through MRI at week 8 ● S-Exo group exhibited the lowest T2 values at week 4 and 8 |
● S-Exo group has the best surface regularity, highest glycosaminoglycan, most orderly tissues and best subchondral bone repair among the groups ● S-Exo group has significant lower Wakitani scores compared to the other groups ● S-Exo group displayed the highest matrix synthesis which consists mainly of Col II |
Not reported |
Abbreviations: µCT, micro computed tomography; ADAMTS, ADAM metallopeptidase with thrombospondin motifs; AFSC, amniotic fluid stem cell; AKP, alkaline phosphatase; BAX, Bcl-2 associated X-protein; BM-MSC, bone marrow-derived mesenchymal stem/stromal cell; CAP, chondrocyte-affinity peptide; CCP3, cleaved caspase-3; CGRP, calcitonin gene-related peptide; CLSM, confocal laser scanning microscopy; col I, type I collagen; col II, type II collagen; COMP, cartilage oligomeric matrix protein; DMM, destabilization of medial meniscus; DRG, dorsal root ganglion; ECM, extracellular matrix; EHG, exosome encapsulating hydrogel; ELF3, E74-like factor 3; ESC-MSC, embryonic stem cell-derived mesenchymal stem/stromal stem/stromal cell; Exo, exosome; GAG, glycosaminoglycan; GelMA, gelatin methacrylate; HWT, head withdrawal threshold; ICRS, International Cartilage Repair Society; IL, interleukin; iNOS, inducible nitric oxide synthase; IPFP-MSC, infrapatellar fat pad-derived mesenchymal stem/stromal cell; iPSC-MSC, induced pluripotent stem cell-derived mesenchymal stem/stromal cell; KGN, kartogenin; LWT, leg withdrawal threshold; MDA, malondialdehyde; MIA, monosodium iodoacetate; MMP, matrix metalloproteinase; MRI, magnetic resonance imaging; MSC, mesenchymal stem/stromal cell; NC, negative control; NGF, nerve growth factor; OA, osteoarthritis; OARSI, Osteoarthritis Research Society International; OCD, osteochondral defect; OCN, osteocalcin; OCT, optical coherence tomography; P75NTR, p75 neurotrophin receptor; PBS, phosphate-buffered saline; PCNA, proliferating cell nuclear antigen; PRP, platelet-rich plasma; PWL, paw withdrawal latency; PWT, paw withdrawal threshold; RUNX2, runt-related transcription factor 2; SD rat, Sprague Dawley rat; SMA, smooth muscle actin; SM-MSC, synovial membrane-derived mesenchymal stem/stromal cell; SOD, superoxide dismutase; TGF-β1, transforming growth factor beta 1; TIMP, tissue inhibitor of metalloproteinase; TMJ, temporomandibular joint; TNF-α, tumor necrosis factor-alpha; TrkA, tropomyosin receptor kinase A; UC-MSC, umbilical cord-derived mesenchymal stem/stromal cell.
Figure 2.
Overview of the studies. The exosomes tested in the included studies were derived from human, murine, or rabbit amniotic fluid stem cells (AFSCs), embryonic stem cell-derived mesenchymal stem/stromal cells (ESC-MSCs), induced pluripotent stem cell-derived MSCs (iPSC-MSCs), bone marrow-derived MSCs (BM-MSCs), polydactyly BM-MSCs, synovial membrane-derived MSCs (SM-MSCs), infrapatellar fat pad-derived MSCs (IPFP-MSCs), umbilical cord-derived MSCs (UC-MSCs), chondrocytes, dendritic cells, platelet-rich plasma (PRP), and serum. The exosomes were administrated to the osteoarthritic joint through intra-articular injection or scaffold implantation. The exosomal bioactive compounds played an important role in cartilage and subchondral bone repair and regeneration. Overall, exosome therapy restored joint function, reduced joint pain, and improved the joint macroscopic, histological, and biochemical features.
In vitro studies have shown that exosomes promote chondrocyte proliferation and migration, impede chondrocyte apoptosis and the expression of pro-inflammatory markers, and restore the balance between chondrocyte catabolism and anabolism in a dose-dependent manner.69,74,78,82,116 However, no article included in the present review reported on the in vivo response to exosome dosage.
We also noted that the studies used several exosome quantitation methods, ie nanoparticle analyzer, protein quantitation assay, and enzyme-linked immunosorbent assay (ELISA). The number of exosome particles (particles/mL) was detected using nanoparticle analyzers such as nanoparticle tracking analysis (NTA) and tunable resistive pulse sensing (TRPS). Some of the studies used an ExoELISA kit to quantify exosomes based on the presence of exosome markers such as CD63. The exosome concentration was also determined by exosome protein mass concentration (µL/mL) using the bicinchoninic acid (BCA) or Bradford assay. Although all included studies reported that exosomes promoted cartilage repair and prevented lesion progression compared to the control group, none conducted in vivo study for identifying the optimal dosage and number of injections. Based on the different quantification methods used in the 29 included studies, the quantity of exosomes used ranged from 8 × 107–1 × 1010 particles and 7.5–200 µg in mouse models; 1 × 108–1 × 1010 and 1.25–100 µg in rat models; and 2 × 109–5 × 109 and 100–200 µg in rabbit models, and the injection number and time varied in each study.
Intercellular communication via exosomes mainly takes place through three mechanisms: (1) direct interaction of exosome ligands and receptors on target cells that activate the intracellular signaling cascades; (2) direct fusion; or (3) endocytosis. Direct fusion and endocytosis resulted in the release of exosomal contents into the cytosol.117 Wu et al,64 He et al,75 Liang et al,77 and Zhang et al84 monitored exosome uptake in joint tissues. Fluorescent labeled exosomes were mainly observed in the articular cavity, suggesting that exosomes acted locally after intra-articular injection. Zhang et al84 noted BM-MSC-derived exosomes could be taken up by synovial cells in vivo. Liang et al77 reported that dendritic cell-derived exosomes were distributed to other body parts and enriched in the kidney. Exosome retention in the articular cavity was improved by fusing a chondrocyte-affinity peptide on the exosome surface. The peptide confined the exosomes to the articular cavity and facilitated exosome penetration into the middle zone of the cartilage tissue to achieve targeted delivery of exosomes to chondrocytes for better therapeutic efficacy.77 Another study reported on the improved tissue-targeting ability of modified exosomes.118
Cartilage Gross Morphological and Morphometric Analysis
Macroscopic assessment of cartilage degradation in small animals, especially mice, is technically difficult due to their small size.119 Hence, most of the included studies used rat and rabbit OA models to conduct cartilage gross morphological analysis. Eight studies graded the gross appearance of treated joints according to the International Cartilage Repair Society (ICRS) macroscopic assessment scale.58,63,65,66,68,72,73,78 Higher ICRS macroscopic assessment scores indicated morphological improvement in exosome-treated defects. Generally, the cartilage defects of the negative control group exhibited incomplete neotissue coverage, surface irregularity, and distinct border areas even at 12 weeks. On the other hand, exosome-treated cartilage defects showed much better and improved gross appearance. For example, Zhang et al68 stated that exosome-treated cartilage defects displayed almost complete neotissue filling, with good surface regularity and full integration with the surrounding cartilage at 12 weeks. Another study used confocal laser scanning microscopy (CLSM) analysis to evaluate cartilage defects, and reported improvement in articular cartilage volume and thickness, as well as lower cartilage degradation in collagenase-induced defects treated with BM-MSCs, BM-MSC-derived exosomes, and BM-MSC-derived microvesicles as compared to the untreated control defects.74
Apart from gross morphological assessment, Wong et al63 also performed biomechanical assessment of regenerated cartilage tissue. The mean Young’s moduli and stiffness of the repaired cartilage at the center and periphery of the defects improved significantly over time in the hyaluronic acid (HA) + ESC-MSC-derived exosome group in comparison to the HA group, suggesting that exosomes not only promote cartilage tissue morphology repair, but also contribute to functional improvement, ie better mechanical strength.
Cartilage Histological Analysis
Histological assessment is vital for determining tissue regeneration, repair, and pathological changes at the microscopic level. Various histological stains are used for identifying different cellular and tissue components.120 Hematoxylin–eosin (H&E) staining is widely used for revealing cell and tissue structure, and has become a common practice in histological study. Safranin O/fast green, toluidine blue, and Alcian blue are used for examining cartilaginous and chondrogenic differentiated tissues by visualizing the proteoglycans.121 In all 29 included studies, exosome treatment contributed to notable improvements in cartilage regeneration at the histological level. The studies used multiple histological grading systems for joint repair to grade the defects, ie the OARSI,60–62,64,67,71,72,74,75,77,79,81,82,84 ICRS visual histological assessment scale,58,73,78 O’Driscoll histological cartilage repair score,63,68 Wakitani histological scoring system,65,66,69 and Mankin scoring system.70,76,80 Other than that, Jin et al57 scored the pathological changes of condylar joint and synovial tissues using a 0–3 subjective grading system with the parameters of synovitis inflammation, synovial thickening, and subchondral bone erosion. All studies recorded improved histological scores after exosome treatment. For example, Zhang et al68 reported that ESC-derived exosome-treated defects demonstrated good cartilage and subchondral bone restorations by week 6 post-surgery. Near complete regeneration and bonding of cartilage with the underlying subchondral bone, which was very similar to that of the age-matched native control, were recorded at week 12. The O’Driscoll histological cartilage repair scores were significantly higher at week 6 and 12 in the exosome-treated group compared to the phosphate-buffered saline (PBS)-treated group. Similarly, Liu et al82 reported that, at week 6, articular cartilage defects treated with PRP-derived exosomes had regularly arranged chondrocytes, clearer tidal line, reduced hyperplasia, and better OARSI scores compared to defects treated with activated PRP.
Immunohistochemistry is used for detecting specific antigens in tissue sections by incubating the tissue sections with the appropriate antibody. Anabolic and catabolic markers of cartilage metabolism in regenerated tissue are identified to analyze the cartilage regeneration properties. Type II collagen and aggrecan, a major cartilage ECM component and a core proteoglycan of articular cartilage, respectively, are always determined for evaluating cartilage regeneration.122,123 Cartilage degradation is mostly indicated by key enzymes in cartilage matrix degradation: matrix metalloproteinases (MMPs) and ADAM metallopeptidase with thrombospondin motifs (ADAMTS).124 Generally, exosome-treated cartilage defects had upregulated type II collagen and aggrecan expression and downregulated MMP13 and ADAMTS5 expression. Wong et al63 treated surgically induced OCD with ESC-MSC-derived exosomes and found that the regenerated tissue was mainly hyaline cartilage with high glycosaminoglycan (GAG) and type II collagen, as well as low type I collagen deposition. The accumulation of type I collagen is a marker of fibrocartilage formation.
Zhang et al69 reported increased proliferating cell nuclear antigen (PCNA)+ cells in reparative cartilage and synovium, and decreased cleaved caspase-3 (CCP3)+ apoptotic cells on reparative cartilage, suggesting that exosomes derived from ESC-MSCs mediate cartilage repair by promoting cell proliferation and suppressing apoptosis. The research team reported similar results in a subsequent study using ESC-MSC-derived exosomes for treating temporomandibular joint OA.70 Chondrocyte apoptosis may abrogate cartilage homeostasis, eventually leading to cartilage degeneration.125 Qiu et al83 and Jin et al57 used the TUNEL (terminal deoxynucleotidyl transferase dUTP nick-end labeling) assay to examine apoptosis. Qiu et al83 stated that curcumin-treated BM-MSC-derived exosomes were more effective in inhibiting chondrocyte apoptosis compared to naïve BM-MSC-derived exosomes. Jin et al57 found that miR-26a-5p overexpression in BM-MSC-derived exosomes enhanced synovium fibroblast apoptosis to alleviate cartilage damage.
Furthermore, Zhang et al69 indicated that MSC-derived exosomes mediate cartilage repair by modulating the pro-inflammatory environment in defects, as demonstrated by the increase in M2 macrophages (CD163+ cells) and reduction in M1 macrophages (CD86+ cells) in both cartilage and the overlying synovium in the ESC-MSC-derived exosome group, with a concomitant reduction in M1-associated cytokines, ie interleukin-1 beta (IL-1β) and tumor necrosis factor-alpha (TNF-α), in synovial fluid. Aside from this, exosomes induced regenerative M2 macrophage infiltration and attenuated inflammatory M1 macrophage infiltration in defect sites, evident in the higher abundance of CD163+ or arginase-1+ cells and scarcity of CD86+, inducible nitric oxide synthase (iNOS)+ or IL-1β+ cells.67,70,81,84 The results are consistent with studies reporting that exosomes have anti-inflammatory and immunomodulatory functions for attenuating disease progression.126–129
Subchondral Bone Regeneration Analysis
OA may lead to pathophysiological changes in subchondral bone and cartilage, also known as the bone–cartilage unit, that perform complementary work in the load-bearing of joints.130,131 Microstructural alterations of subchondral bone and the osteochondral junction, including osteophytes, subchondral sclerosis, subchondral cysts, or bone marrow lesions, are observed in the different stages of OA.132 Increasing evidence has shown that subchondral bone disturbance is associated with OA initiation and progression.133–136 There is molecular crosstalk between cartilage and subchondral bone, and cartilage is partly dependent on the neighboring subchondral bone for its nutrient supply.137,138 Subchondral bone migration is involved in OCD repair.139
Among the 29 included studies, six evaluated subchondral bone regeneration.70,73,74,80,81,84 Bone parameters including bone volume (bone volume/tissue volume); bone degradation (bone surface/bone volume); osteophyte formation; meniscal or ligament calcification; and trabecular thickness, separation, and number were quantified. The six studies used micro-computed tomography (µCT) to examine the joint microarchitecture and reported that exosome-treated groups showed a lower extent of osteophyte formation, whereas the groups treated with normal saline exhibited a rough joint surface with osteophytes on the bone edge.70,73,74,80,81,84 Interestingly, osteophytes formed in the OA serum-derived exosome-treated group were impeded by the introduction of ATF4 mRNA into the OA serum-derived exosomes.80 Apart from that, Cosenza et al74 reported higher epiphyseal and subchondral bone volume, lower bone degradation, and decreased calcification of menisci and ligaments in the groups treated with BM-MSCs, BM-MSC-derived exosomes, and BM-MSC-derived microvesicles. Zhang et al reported notable differences in bone volume, trabecular thickness, trabecular separation, and trabecular number at week 8 post-treatment,70 proving that ESC-MSC-derived exosomes restored subchondral bone volume and architecture in monosodium iodoacetate (MIA)-induced OA. Moreover, subchondral bone regeneration has been reported in cartilage defects treated with exosomes loaded in a scaffold. Chen et al73 reported that more ossified tissues were regenerated in OCD that received implantation of a 3D-printed cartilage ECM/gelatine methacrylate (GelMA)/BM-MSC-derived exosome scaffold.
Pain Behavior Analysis
Joint pain is the major symptom of OA. Recent studies indicate that sensory innervation in osteoarthritic subchondral bone or neuronal hypersensitivity as a result of aberrant subchondral bone remodeling during OA progression may contribute to arthritic pain.140,141 Hence, behavioral and functional assessments are important in OA evaluation. Pain cannot be measured directly in animals, but can be estimated through pain-like behaviors.142 Withdrawal response, a pain-like behavior towards a nociceptive stimulus, is the most commonly used method for examining pain in animals.143 Yan et al,65 Zhang et al,70 and He et al75 measured the withdrawal threshold of OA animals using the von Frey microfilament procedure, while Zavatti et al used a pressure application measurement device to do so.67 He et al75 also tested the paw withdrawal latency of rats treated with BM-MSC-derived exosomes using a plantar test and measured the thermal threshold. The results showed that exosome-treated OA animals have high pain tolerance levels and that the results were comparable to that of healthy control animals. Furthermore, increasing evidence supports the notion that neuropathic pain also contributes to OA pain.144–146 He et al75 reported neuropathic pain in OA rats, and demonstrated that exosome injection relieved inflammatory and neuropathic pain, as shown by the decreased protein levels of calcitonin gene-related peptide (CGRP) and iNOS in the dorsal root ganglion tissue.
In addition, OA animals may have altered gait patterns to reduce the pain from movement or loading force.147 Wu et al64 performed gait analysis using the CatWalk method to measure motion-related pain in OA mice, and found that IPFP-MSC-derived exosomes ameliorated gait disturbance, indicated by the marked increase in duty cycle at week 10.
Safety Profile
Exosomes have low immunogenicity and potent immunoregulatory properties.148,149 So far, in vivo studies using single or repeated doses of exosomes have not reported severe immune reactions.150,151 Among the included studies, nine reported the safety outcome.60,63,67,68,70,73,77,82 No adverse events or inflammatory responses occurred in those studies, regardless of the cell source, ie MSC- or non-MSC-derived exosomes, and method of administration, ie intra-articular administration in solution form or encapsulated within a scaffold. Liang et al77 demonstrated via H&E staining that dendritic cell-derived exosome injections did not cause toxicity to major organs such as the heart, kidney, lung, and spleen. Similarly, no apparent pathological effects were shown in the myocardium, liver, and kidney 1–2 weeks after 3D printed ECM/GelMA/exosome scaffold implantation.73
The majority of the included studies used human exosomes to promote cartilage repair in animal models. No study reported adverse events related to the use of xenogeneic and allogeneic exosomes. Thus, allogeneic exosomes may be considered safe for use in humans. Nonetheless, clinical trials are needed to validate the safety of allogeneic exosomes.
Cells or Exosomes?
Previously, stem cell therapy was believed to exert its tissue repair mechanism through the replacement of injured cells. However, many studies have shown that most of the MSCs injected are trapped and cleared in the blood circulation and that only a small fraction of the transplanted cells reach the target tissues.152 Despite the low cell homing to the injured tissues, the therapeutic effect of MSCs remains significant, indicating that MSCs support tissue repair and regeneration via the secretion of paracrine factors.153
Several studies showed that exosomes have comparable therapeutic effects to cell-based therapy in managing OA. Wang et al61 reported that ESC-MSC-derived exosomes were as effective as ESC-MSCs for treating DMM (destabilization of medial meniscus)-induced OA animal models. However, the experiments were carried out sequentially, and the study compared single cell suspension injection versus multiple exosome injections. Thus, it might not be a fair comparison. According to Cosenza et al74 and Zavatti et al,67 cell therapy using BM-MSCs and AFSCs, respectively, promoted cartilage regeneration. However, more spectacular results were recorded when exosomes derived from these cells were used. Zavatti et al67 stated that both AFSCs and AFSC-derived exosomes improved the pain threshold of OA rats, whereby the results were comparable to that of the healthy group. However, histological and immunohistochemical analyses showed that the exosome-treated group displayed better cartilage regeneration compared to the AFSC-treated group. Additionally, the lower OARSI grading scores and higher volume of cartilage tissue with lower fibrous connective tissue composition in the neotissue in exosome-treated defects indicated that AFSC-derived exosomes were superior for repairing and regenerating cartilage tissue as compared to AFSC therapy. The AFSC-derived exosomes were also more potent for reducing osteoarthritic joint inflammation compared to AFSCs, as indicated by the presence of more M2 macrophages. Nonetheless, the OA animals received two intra-articular injections of exosomes whilst the AFSCs were only administered once, as the authors postulated that the transplanted cells may exert their therapeutic effects for a longer period, ie up to 3 weeks. Cosenza et al74 reported that single injection of BM-MSCs, BM-MSC-derived exosomes, and BM-MSC-derived microvesicles exhibited similar chondroprotective effects. Yet, exosome treatment led to greater improvement in modified Pritzker OARSI scores and reduction in osteophyte formation compared to BM-MSC and microvesicle treatments. These results suggest that exosomes might be a more effective and safer alternative to cell-based therapy for OA. Nevertheless, more studies, especially clinical trials, are needed to validate the safety and efficacy of exosome therapy.
Nowadays, many researchers advocate the transition from cell-based therapy to cell-free therapy, driven by several factors. Generally, the heterogeneity of living cells often leads to inconsistent curative effects. Long-term in vitro expansion might lead to cell dedifferentiation and senescence, thus compromising the therapeutic potential.154 Furthermore, stem cells carry the risk of mutation and tumor formation.155 Tumor formation is a hurdle to overcome for the clinical use of ESCs and iPSCs.156 Exosome therapy is a cell-free therapeutic option available for overcoming the drawbacks of cell-based therapy. Exosomes are easier to handle and store, and are less costly and less time-consuming to produce compared to cells.101,157 Furthermore, exosome dosage and potency are easier to optimize.37 Apart from that, exosomes can be developed as nanosized carriers to deliver the desired therapeutic cargo to the target cells.158,159 However, the most prominent shortcoming of exosomes is that they cannot replicate or reproduce in vivo. Coupled with their short half-life, multiple dosages might be required to achieve the desired treatment results.160,161
Conclusion and Perspective
The promising in vivo findings indicate that exosomes promote cartilage repair and regeneration, and modulate the pro-inflammatory environment, subchondral bone regeneration, and pain behavior in both OA and OCD models. More importantly, none of the included studies reported adverse events, indicating the low immunogenicity and excellent immunomodulatory property of exosomes. The modification of exosomal cargo further enhanced the therapeutic efficacy of exosomes.
On the other hand, despite many preclinical studies reporting that exosomes enhance cartilage regeneration, research on the therapeutic efficacy of exosomes for OA is still in its infancy. The exact mechanism and detailed signaling cascade mediated by exosomes in cartilage repair and regeneration are not fully understood. Hence, there should be more studies examining the mechanism of action. Moreover, exosomes demonstrate dose-dependent therapeutic efficacy in terms of promoting chondrocyte migration and proliferation, reducing chondrocyte apoptosis and pro-inflammatory markers, and restoring cartilage anabolic–catabolic marker equilibrium in vitro. However, the optimum source and dose of exosomes for OA management have not been determined in animal models. Furthermore, multiple intra-articular injections of exosomes cause pain and discomfort to the recipients and increase the risk of other complications such as inflammation, arthritis, and neuropathy.162 Encapsulating exosomes within a scaffold might reduce the number of injections needed, as it allows the controlled release of exosomes. A scaffold also provides an ECM that mimics the native cartilage tissue to facilitate regeneration. However, more studies are needed to identify a scaffold with all the desired biological and physicochemical properties that could hasten the regeneration of damaged cartilage without causing adverse events. Finally, the term “exosome” used in the studies is controversial, as the identity of exosomes cannot be confirmed through size, density, or protein markers due to the lack of specific isolation methods and characterization techniques. “Exosome” is used mostly due to perceived popularity.163 To be more precise, EVs should be defined based on their physical characteristics, biochemical composition, culture condition, and cell of origin.49
The low yield of EV production with existing harvesting methods is a challenge for clinical application. Large-scale EV production can be achieved by manipulating the culture condition, such as with a microcarrier-based 3D culture system and human platelet lysate supplementation.164,165 Batch-to-batch biological variation of EV therapy also cannot be ignored. To address this issue, Chen et al166 transformed human ESC-MSCs into immortalized cells, which enabled the consistent supply of therapeutic EVs or delivery vesicles. Besides, Lian et al167 proposed a protocol for producing human ESC-MSCs that are reproducible and able to generate consistent batches of cells and conditioned medium on a large scale. iPSCs, iPSC-derived MSCs, and iPSC-derived MSC-like mesenchymal progenitor cells could also be alternative inexhaustible EV production sources due to their unlimited proliferative potential.168,169 In addition, there is no standard protocol for ensuring exosome or EV quality.
In summary, studies examining the therapeutic efficacy of exosomes on cartilage regeneration remain limited to small-animal models. Therefore, studies using large-animal models that are more clinically relevant should be carried out in the future to validate the safety and efficacy of EV therapy. The standardization of EV therapy is needed to achieve consistent and optimum therapeutic outcomes. More efforts are required to identify the most ideal cell source, culture condition, exosome dosage, and frequency of administration, as well as the method of administration, to achieve the best therapeutic results without causing adverse events.
Funding Statement
This work was supported by research grant from the Ministry of Higher Education Malaysia (FRGS/1/2020/SKK0/UKM/02/5).
Abbreviations
2D, two-dimensional; 3D, three-dimensional; ADAMTS, ADAM metallopeptidase with thrombospondin motifs; AFSC, amniotic fluid stem cell; ATF4, activating transcription factor 4; BM-MSC, bone marrow-derived mesenchymal stem/stromal cell; ECM, extracellular matrix; ELISA, enzyme-linked immunosorbent assay; ESC-MSC, embryonic stem cell-derived mesenchymal stem/stromal cell; EV, extracellular vesicle; GelMA, gelatin methacrylate; H&E, hematoxylin-eosin; ICRS, International Cartilage Repair Society; IL-1β, interleukin-1 beta; iNOS, inducible nitric oxide synthase; IPFP-MSC, infrapatellar fat pad-derived mesenchymal stem/stromal cell; iPSC-MSC, induced pluripotent stem cell-derived mesenchymal stem/stromal cell; lncRNA, long non-coding RNA; miR/miRNA, microRNA; MMP, matrix metalloproteinase; MRI, magnetic resonance imaging; MSC, mesenchymal stem/stromal cell; MVB, multi-vesicular bodies; OA, osteoarthritis; OARSI, Osteoarthritis Research Society International; OCD, osteochondral defect; PRP, platelet-rich plasma; RCCS, rotary cell culture system; SM-MSC, synovial membrane-derived mesenchymal stem/stromal cell; SYRCLE, Systematic Review Center for Laboratory Animal Experimentation; TGF-β1, transforming growth factor beta 1; UC-MSC, umbilical cord-derived mesenchymal stem/stromal cell.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Author Contributions
C.Y.N. and J.Y.C. conducted the literature search, article selection, and data extraction. All authors contributed to data analysis, drafting, or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29–30. doi: 10.1016/j.eclinm.2020.100587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mobasheri A, Batt M. An update on the pathophysiology of osteoarthritis. Ann Phys Rehabil Med. 2016;59(5–6):333–339. doi: 10.1016/j.rehab.2016.07.004 [DOI] [PubMed] [Google Scholar]
- 3.Abramoff B, Caldera FE. Osteoarthritis: pathology, diagnosis, and treatment options. Med Clin North Am. 2020;104(2):293–311. doi: 10.1016/j.mcna.2019.10.007 [DOI] [PubMed] [Google Scholar]
- 4.Buckwalter JA, Mankin HJ. Articular cartilage: degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect. 1998;47:487–504. [PubMed] [Google Scholar]
- 5.Re’Em T, Witte F, Willbold E, Ruvinov E, Cohen S. Simultaneous regeneration of articular cartilage and subchondral bone induced by spatially presented TGF-beta and BMP-4 in a bilayer affinity binding system. Acta Biomater. 2012;8(9):3283–3293. doi: 10.1016/j.actbio.2012.05.014 [DOI] [PubMed] [Google Scholar]
- 6.van Dijk CN, Reilingh ML, Zengerink M, van Bergen CJA. Osteochondral defects in the ankle: why painful? Knee Surg Sports Traumatol Arthrosc. 2010;18(5):570–580. doi: 10.1007/s00167-010-1064-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anandacoomarasamy A, Leibman S, Smith G, et al. Weight loss in obese people has structure-modifying effects on medial but not on lateral knee articular cartilage. Ann Rheum Dis. 2012;71(1):26–32. doi: 10.1136/ard.2010.144725 [DOI] [PubMed] [Google Scholar]
- 8.Lund H, Weile U, Christensen R, et al. A randomized controlled trial of aquatic and land-based exercise in patients with knee osteoarthritis. J Rehabil Med. 2008;40(2):137–144. doi: 10.2340/16501977-0134 [DOI] [PubMed] [Google Scholar]
- 9.Uthman OA, Van Der Windt DA, Jordan JL, et al. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. BMJ (Online). 2013;347(7928). doi: 10.1136/bmj.f5555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Towheed T, Maxwell L, Judd M, Catton M, Hochberg MC, Wells GA. Acetaminophen for osteoarthritis. Cochrane Database Syst Rev. 2006;2010(1). doi: 10.1002/14651858.cd004257.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Richette P, Latourte A, Frazier A. Safety and efficacy of paracetamol and NSAIDs in osteoarthritis: which drug to recommend? Expert Opin Drug Saf. 2015;14(8):1259–1268. doi: 10.1517/14740338.2015.1056776 [DOI] [PubMed] [Google Scholar]
- 12.SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am. 2006;88(3):480–485. doi: 10.2106/JBJS.E.00629 [DOI] [PubMed] [Google Scholar]
- 13.Atkinson HDE. The negatives of knee replacement surgery: complications and the dissatisfied patient. Orthop Trauma. 2017;31(1):25–33. doi: 10.1016/j.mporth.2016.09.011 [DOI] [Google Scholar]
- 14.Badekas T, Takvorian M, Souras N. Treatment principles for osteochondral lesions in foot and ankle. Int Orthop. 2013;37(9):1697–1706. doi: 10.1007/s00264-013-2076-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Block TJ, Garza JR. Regenerative cells for the management of osteoarthritis and joint disorders: a concise literature review. Aesthet Surg J. 2017;37(suppl_3):S9–S15. doi: 10.1093/asj/sjx015 [DOI] [PubMed] [Google Scholar]
- 16.Murphy JM, Fink DJ, Hunziker EB, Barry FP. Stem cell therapy in a caprine model of osteoarthritis. Arthritis Rheum. 2003;48(12):3464–3474. doi: 10.1002/art.11365 [DOI] [PubMed] [Google Scholar]
- 17.Desando G, Cavallo C, Sartoni F, et al. Intra-articular delivery of adipose derived stromal cells attenuates osteoarthritis progression in an experimental rabbit model. Arthritis Res Ther. 2013;15(1):R22. doi: 10.1186/ar4156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murata D, Kunitomi Y, Harada K, Tokunaga S, Takao S, Nakayama K. Osteochondral regeneration using scaffold-free constructs of adipose tissue-derived mesenchymal stem cells made by a bio three-dimensional printer with a needle-array in rabbits. Regen Ther. 2020;15:77–89. doi: 10.1016/j.reth.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamasaki A, Kunitomi Y, Murata D, et al. Osteochondral regeneration using constructs of mesenchymal stem cells made by bio three-dimensional printing in mini-pigs. J Orthop Res. 2019;37(6):1398–1408. doi: 10.1002/jor.24206 [DOI] [PubMed] [Google Scholar]
- 20.Lee WS, Kim HJ, Kim KI, Kim GB, Jin W. Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: a phase IIb, randomized, placebo-controlled clinical trial. Stem Cells Transl Med. 2019;8(6):504–511. doi: 10.1002/sctm.18-0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Freitag J, Bates D, Wickham J, et al. Adipose-derived mesenchymal stem cell therapy in the treatment of knee osteoarthritis: a randomized controlled trial. Regen Med. 2019;14(3):213–230. doi: 10.2217/rme-2018-0161 [DOI] [PubMed] [Google Scholar]
- 22.Freitag J, Wickham J, Shah K, Tenen A. Effect of autologous adipose-derived mesenchymal stem cell therapy in the treatment of an osteochondral lesion of the ankle. BMJ Case Rep. 2020;13(7):e234595. doi: 10.1136/bcr-2020-234595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei ZJ, Wang QQ, Cui ZG, Inadera H, Jiang X, Wu CA. Which is the most effective one in knee osteoarthritis treatment from mesenchymal stem cells obtained from different sources? - A systematic review with conventional and network meta-analyses of randomized controlled trials. Ann Transl Med. 2021;9(6):452. doi: 10.21037/atm-20-5116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song Y, Zhang J, Xu H, et al. Mesenchymal stem cells in knee osteoarthritis treatment: a systematic review and meta-analysis. J Orthop Transl. 2020;24:121–130. doi: 10.1016/j.jot.2020.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lukomska B, Stanaszek L, Zuba-Surma E, Legosz P, Sarzynska S, Drela K. Challenges and controversies in human mesenchymal stem cell therapy. Stem Cells Int. 2019;2019:e9628536. doi: 10.1155/2019/9628536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonzo Di LV, Ferrero I, Cravanzola C, et al. Human mesenchymal stem cells as a two-edged sword in hepatic regenerative medicine: engraftment and hepatocyte differentiation versus profibrogenic potential. Gut. 2008;57(2):223–231. doi: 10.1136/gut.2006.111617 [DOI] [PubMed] [Google Scholar]
- 27.Jeong JO, Han JW, Kim JM, et al. Malignant tumor formation after transplantation of short-term cultured bone marrow mesenchymal stem cells in experimental myocardial infarction and diabetic neuropathy. Circ Res. 2011;108(11):1340–1347. doi: 10.1161/CIRCRESAHA.110.239848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Boeck A, Pauwels P, Hensen K, et al. Bone marrow-derived mesenchymal stem cells promote colorectal cancer progression through paracrine neuregulin 1/HER3 signalling. Gut. 2013;62(4):550–560. doi: 10.1136/gutjnl-2011-301393 [DOI] [PubMed] [Google Scholar]
- 29.Spaeth E, Dembinski J, Sasser A, et al. Mesenchymal stem cell transition to tumor-associated fibroblasts contributes to fibrovascular network expansion and tumor progression. PLoS One. 2009;4(4):e4992. doi: 10.1371/journal.pone.0004992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karnoub AE, Dash AB, Vo AP, et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449(7162):557–563. doi: 10.1038/nature06188 [DOI] [PubMed] [Google Scholar]
- 31.Kim JS, Lee JH, Kwon O, et al. Rapid deterioration of preexisting renal insufficiency after autologous mesenchymal stem cell therapy. Kidney Res Clin Pract. 2017;36(2):200–204. doi: 10.23876/j.krcp.2017.36.2.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Broekema M, Harmsen MC, van Luyn MJA, et al. Bone marrow-derived myofibroblasts contribute to the renal interstitial myofibroblast population and produce procollagen I after ischemia/reperfusion in rats. J Am Soc Nephrol. 2007;18(1):165–175. doi: 10.1681/ASN.2005070730 [DOI] [PubMed] [Google Scholar]
- 33.Aslam M, Baveja R, Liang OD, et al. Bone marrow stromal cells attenuate lung injury in a murine model of neonatal chronic lung disease. Am J Respir Crit Care Med. 2009;180(11):1122–1130. doi: 10.1164/rccm.200902-0242OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Timmers L, Lim SK, Arslan F, et al. Reduction of myocardial infarct size by human mesenchymal stem cell conditioned medium. Stem Cell Res. 2007;1(2):129–137. doi: 10.1016/j.scr.2008.02.002 [DOI] [PubMed] [Google Scholar]
- 35.Goolaerts A, Pellan-Randrianarison N, Larghero J, et al. Conditioned media from mesenchymal stromal cells restore sodium transport and preserve epithelial permeability in an in vitro model of acute alveolar injury. Am J Physiol Lung Cell Mol Physiol. 2014;306(11):L975–L985. doi: 10.1152/ajplung.00242.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liang X, Ding Y, Zhang Y, Tse HF, Lian Q. Paracrine mechanisms of mesenchymal stem cell-based therapy: current status and perspectives. Cell Transplant. 2014;23(9):1045–1059. doi: 10.3727/096368913X667709 [DOI] [PubMed] [Google Scholar]
- 37.Bjørge IM, Kim SY, Mano JF, Kalionis B, Chrzanowski W. Extracellular vesicles, exosomes and shedding vesicles in regenerative medicine - a new paradigm for tissue repair. Biomater Sci. 2017;6(1):60–78. doi: 10.1039/c7bm00479f [DOI] [PubMed] [Google Scholar]
- 38.Zhao AG, Shah K, Cromer B, Sumer H. Mesenchymal stem cell-derived extracellular vesicles and their therapeutic potential. Stem Cells Int. 2020;2020:e8825771. doi: 10.1155/2020/8825771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maas SLN, Breakefield XO, Weaver AM. Extracellular vesicles: unique intercellular delivery vehicles. Trends Cell Biol. 2017;27(3):172–188. doi: 10.1016/j.tcb.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lai RC, Arslan F, Lee MM, et al. Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. Stem Cell Res. 2010;4(3):214–222. doi: 10.1016/j.scr.2009.12.003 [DOI] [PubMed] [Google Scholar]
- 41.Colombo M, Raposo G, Théry C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Dev Biol. 2014;30(1):255–289. doi: 10.1146/annurev-cellbio-101512-122326 [DOI] [PubMed] [Google Scholar]
- 42.Lo Cicero A, Stahl PD, Raposo G. Extracellular vesicles shuffling intercellular messages: for good or for bad. Curr Opin Cell Biol. 2015;35:69–77. doi: 10.1016/j.ceb.2015.04.013 [DOI] [PubMed] [Google Scholar]
- 43.Teng X, Chen L, Chen W, Yang J, Yang Z, Shen Z. Mesenchymal stem cell-derived exosomes improve the microenvironment of infarcted myocardium contributing to angiogenesis and anti-inflammation. Cell Physiol Biochem. 2015;37(6):2415–2424. doi: 10.1159/000438594 [DOI] [PubMed] [Google Scholar]
- 44.Li T, Yan Y, Wang B, et al. Exosomes derived from human umbilical cord mesenchymal stem cells alleviate liver fibrosis. Stem Cells Dev. 2013;22(6):845–854. doi: 10.1089/scd.2012.0395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang J, Guan J, Niu X, et al. Exosomes released from human induced pluripotent stem cells-derived MSCs facilitate cutaneous wound healing by promoting collagen synthesis and angiogenesis. J Transl Med. 2015;13(1):49. doi: 10.1186/s12967-015-0417-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ni Z, Zhou S, Li S, et al. Exosomes: roles and therapeutic potential in osteoarthritis. Bone Res. 2020;8:25. doi: 10.1038/s41413-020-0100-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Toh WS, Lai RC, Hui JHP, Lim SK. MSC exosome as a cell-free MSC therapy for cartilage regeneration: implications for osteoarthritis treatment. Semin Cell Dev Biol. 2017;67:56–64. doi: 10.1016/j.semcdb.2016.11.008 [DOI] [PubMed] [Google Scholar]
- 48.Kim YG, Park U, Park BJ, Kim K. Exosome-mediated bidirectional signaling between mesenchymal stem cells and chondrocytes for enhanced chondrogenesis. Biotechnol Bioprocess Eng. 2019;24(5):734–744. doi: 10.1007/s12257-019-0332-y [DOI] [Google Scholar]
- 49.Théry C, Witwer KW, Aikawa E, et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the international society for extracellular vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7(1):1535750. doi: 10.1080/20013078.2018.1535750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yáñez-Mó M, Siljander PRM, Andreu Z, et al. Biological properties of extracellular vesicles and their physiological functions. J Extracell Vesicles. 2015;4(1):27066. doi: 10.3402/jev.v4.27066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Willms E, Cabañas C, Mäger I, Wood MJA, Vader P. Extracellular vesicle heterogeneity: subpopulations, isolation techniques, and diverse functions in cancer progression. Front Immunol. 2018;9:738. doi: 10.3389/fimmu.2018.00738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang B, Tian X, Qu Z, Liu J, Yang L, Zhang W. Efficacy of extracellular vesicles from mesenchymal stem cells on osteoarthritis in animal models: a systematic review and meta-analysis. Nanomedicine (Lond). 2021;16(15):1297–1310. doi: 10.2217/nnm-2021-0047 [DOI] [PubMed] [Google Scholar]
- 53.Tan SSH, Tjio CKE, Wong JRY, et al. Mesenchymal stem cell exosomes for cartilage regeneration: a systematic review of preclinical in vivo studies. Tissue Eng Part B Rev. 2021;27(1):1–13. doi: 10.1089/ten.TEB.2019.0326 [DOI] [PubMed] [Google Scholar]
- 54.To K, Romain K, Mak C, Kamaraj A, Henson F, Khan W. The treatment of cartilage damage using human mesenchymal stem cell-derived extracellular vesicles: a systematic review of in vivo studies. Front Bioeng Biotechnol. 2020;8:580. doi: 10.3389/fbioe.2020.00580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hooijmans CR, Rovers MM, de Vries RBM, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014;14(1):43. doi: 10.1186/1471-2288-14-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen X, Shi Y, Xue P, Ma X, Li J, Zhang J. Mesenchymal stem cell-derived exosomal microRNA-136-5p inhibits chondrocyte degeneration in traumatic osteoarthritis by targeting ELF3. Arthritis Res Ther. 2020;22(1):256. doi: 10.1186/s13075-020-02325-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jin Z, Ren J, Qi S. Human bone mesenchymal stem cells-derived exosomes overexpressing microRNA-26a-5p alleviate osteoarthritis via down-regulation of PTGS2. Int Immunopharmacol. 2020;78:105946. doi: 10.1016/j.intimp.2019.105946 [DOI] [PubMed] [Google Scholar]
- 58.Liu X, Yang Y, Li Y, et al. Integration of stem cell-derived exosomes with in situ hydrogel glue as a promising tissue patch for articular cartilage regeneration. Nanoscale. 2017;9(13):4430–4438. doi: 10.1039/c7nr00352h [DOI] [PubMed] [Google Scholar]
- 59.Mao G, Zhang Z, Hu S, et al. Exosomes derived from miR-92a-3p-overexpressing human mesenchymal stem cells enhance chondrogenesis and suppress cartilage degradation via targeting WNT5A. Stem Cell Res Ther. 2018;9(1):247. doi: 10.1186/s13287-018-1004-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tao SC, Yuan T, Zhang YL, Yin WJ, Guo SC, Zhang CQ. Exosomes derived from miR-140-5p-overexpressing human synovial mesenchymal stem cells enhance cartilage tissue regeneration and prevent osteoarthritis of the knee in a rat model. Theranostics. 2017;7(1):180–195. doi: 10.7150/thno.17133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang Y, Yu D, Liu Z, et al. Exosomes from embryonic mesenchymal stem cells alleviate osteoarthritis through balancing synthesis and degradation of cartilage extracellular matrix. Stem Cell Res Ther. 2017;8(1):189. doi: 10.1186/s13287-017-0632-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang Z, Yan K, Ge G, et al. Exosomes derived from miR-155-5p–overexpressing synovial mesenchymal stem cells prevent osteoarthritis via enhancing proliferation and migration, attenuating apoptosis, and modulating extracellular matrix secretion in chondrocytes. Cell Biol Toxicol. 2021;37(1):85–96. doi: 10.1007/s10565-020-09559-9 [DOI] [PubMed] [Google Scholar]
- 63.Wong KL, Zhang S, Wang M, et al. Intra-articular injections of mesenchymal stem cell exosomes and hyaluronic acid improve structural and mechanical properties of repaired cartilage in a rabbit model. Arthroscopy. 2020;36(8):2215–2228.e2. doi: 10.1016/j.arthro.2020.03.031 [DOI] [PubMed] [Google Scholar]
- 64.Wu J, Kuang L, Chen C, et al. MiR-100-5p-abundant exosomes derived from infrapatellar fat pad MSCs protect articular cartilage and ameliorate gait abnormalities via inhibition of mTOR in osteoarthritis. Biomaterials. 2019;206:87–100. doi: 10.1016/j.biomaterials.2019.03.022 [DOI] [PubMed] [Google Scholar]
- 65.Yan L, Liu G, Wu X. Exosomes derived from umbilical cord mesenchymal stem cells in mechanical environment show improved osteochondral activity via upregulation of LncRNA H19. J Orthop Transl. 2021;26:111–120. doi: 10.1016/j.jot.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yan L, Wu X. Exosomes produced from 3D cultures of umbilical cord mesenchymal stem cells in a hollow-fiber bioreactor show improved osteochondral regeneration activity. Cell Biol Toxicol. 2020;36(2):165–178. doi: 10.1007/s10565-019-09504-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zavatti M, Beretti F, Casciaro F, Bertucci E, Maraldi T. Comparison of the therapeutic effect of amniotic fluid stem cells and their exosomes on monoiodoacetate-induced animal model of osteoarthritis. BioFactors. 2020;46(1):106–117. doi: 10.1002/biof.1576 [DOI] [PubMed] [Google Scholar]
- 68.Zhang S, Chu WC, Lai RC, Lim SK, Hui JHP, Toh WS. Exosomes derived from human embryonic mesenchymal stem cells promote osteochondral regeneration. Osteoarthritis Cartilage. 2016;24(12):2135–2140. doi: 10.1016/j.joca.2016.06.022 [DOI] [PubMed] [Google Scholar]
- 69.Zhang S, Chuah SJ, Lai RC, Hui JHP, Lim SK, Toh WS. MSC exosomes mediate cartilage repair by enhancing proliferation, attenuating apoptosis and modulating immune reactivity. Biomaterials. 2018;156:16–27. doi: 10.1016/j.biomaterials.2017.11.028 [DOI] [PubMed] [Google Scholar]
- 70.Zhang S, Teo KYW, Chuah SJ, Lai RC, Lim SK, Toh WS. MSC exosomes alleviate temporomandibular joint osteoarthritis by attenuating inflammation and restoring matrix homeostasis. Biomaterials. 2019;200:35–47. doi: 10.1016/j.biomaterials.2019.02.006 [DOI] [PubMed] [Google Scholar]
- 71.Zhou X, Liang H, Hu X, et al. BMSC-derived exosomes from congenital polydactyly tissue alleviate osteoarthritis by promoting chondrocyte proliferation. Cell Death Discov. 2020;6(1):142. doi: 10.1038/s41420-020-00374-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhu Y, Wang Y, Zhao B, et al. Comparison of exosomes secreted by induced pluripotent stem cell-derived mesenchymal stem cells and synovial membrane-derived mesenchymal stem cells for the treatment of osteoarthritis. Stem Cell Res Ther. 2017;8(1):64. doi: 10.1186/s13287-017-0510-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen P, Zheng L, Wang Y, et al. Desktop-stereolithography 3D printing of a radially oriented extracellular matrix/mesenchymal stem cell exosome bioink for osteochondral defect regeneration. Theranostics. 2019;9(9):2439–2459. doi: 10.7150/thno.31017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cosenza S, Ruiz M, Toupet K, Jorgensen C, Noël D. Mesenchymal stem cells derived exosomes and microparticles protect cartilage and bone from degradation in osteoarthritis. Sci Rep. 2017;7(1):16214. doi: 10.1038/s41598-017-15376-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.He L, He T, Xing J, et al. Bone marrow mesenchymal stem cell-derived exosomes protect cartilage damage and relieve knee osteoarthritis pain in a rat model of osteoarthritis. Stem Cell Res Ther. 2020;11(1):276. doi: 10.1186/s13287-020-01781-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jin Z, Ren J, Qi S. Exosomal miR-9-5p secreted by bone marrow-derived mesenchymal stem cells alleviates osteoarthritis by inhibiting syndecan-1. Cell Tissue Res. 2020;381(1):99–114. doi: 10.1007/s00441-020-03193-x [DOI] [PubMed] [Google Scholar]
- 77.Liang Y, Xu X, Li X, et al. Chondrocyte-targeted microRNA delivery by engineered exosomes toward a cell-free osteoarthritis therapy. ACS Appl Mater Interfaces. 2020;12(33):36938–36947. doi: 10.1021/acsami.0c10458 [DOI] [PubMed] [Google Scholar]
- 78.Liu C, Li Y, Yang Z, Zhou Z, Lou Z, Zhang Q. Kartogenin enhances the therapeutic effect of bone marrow mesenchymal stem cells derived exosomes in cartilage repair. Nanomedicine (Lond). 2020;15(3):273–288. doi: 10.2217/nnm-2019-0208 [DOI] [PubMed] [Google Scholar]
- 79.Wang R, Xu B, Xu H. TGF-β1 promoted chondrocyte proliferation by regulating Sp1 through MSC-exosomes derived miR-135b. Cell Cycle. 2018;17(24):2756–2765. doi: 10.1080/15384101.2018.1556063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang Y, He SH, Liang X, Zhang XX, Li S-S, Li TF. ATF4-modified serum exosomes derived from osteoarthritic mice inhibit osteoarthritis by inducing autophagy. IUBMB Life. 2021;73(1):146–158. doi: 10.1002/iub.2414 [DOI] [PubMed] [Google Scholar]
- 81.Zheng L, Wang Y, Qiu P, et al. Primary chondrocyte exosomes mediate osteoarthritis progression by regulating mitochondrion and immune reactivity. Nanomedicine (Lond). 2019;14(24):3193–3212. doi: 10.2217/nnm-2018-0498 [DOI] [PubMed] [Google Scholar]
- 82.Liu X, Wang L, Ma C, Wang G, Zhang Y, Sun S. Exosomes derived from platelet-rich plasma present a novel potential in alleviating knee osteoarthritis by promoting proliferation and inhibiting apoptosis of chondrocyte via Wnt/β-catenin signaling pathway. J Orthop Surg Res. 2019;14(1):470. doi: 10.1186/s13018-019-1529-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Qiu B, Xu X, Yi P, Hao Y. Curcumin reinforces MSC-derived exosomes in attenuating osteoarthritis via modulating the miR-124/NF-kB and miR-143/ROCK1/TLR9 signalling pathways. J Cell Mol Med. 2020;24(18):10855–10865. doi: 10.1111/jcmm.15714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang J, Rong Y, Luo C, Cui W. Bone marrow mesenchymal stem cell-derived exosomes prevent osteoarthritis by regulating synovial macrophage polarization. Aging (Albany NY). 2020;12(24):25138–25152. doi: 10.18632/aging.104110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cai J, Wu J, Wang J, et al. Extracellular vesicles derived from different sources of mesenchymal stem cells: therapeutic effects and translational potential. Cell Biosci. 2020;10(1):69. doi: 10.1186/s13578-020-00427-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liau LL, Al-Masawa ME, Koh B, et al. The potential of mesenchymal stromal cell as therapy in neonatal diseases. Front Pediatr. 2020;8:591693. doi: 10.3389/fped.2020.591693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Looi QH, Eng SP, Liau LL, et al. Mesenchymal stem cell therapy for sports injuries-from research to clinical practice. Sains Malays. 2020;49(4):825–838. doi: 10.17576/jsm-2020-4904-12 [DOI] [Google Scholar]
- 88.Gao F, Chiu SM, Motan DAL, et al. Mesenchymal stem cells and immunomodulation: current status and future prospects. Cell Death Dis. 2016;7(1):e2062. doi: 10.1038/cddis.2015.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pittenger MF, Discher DE, Péault BM, Phinney DG, Hare JM, Caplan AI. Mesenchymal stem cell perspective: cell biology to clinical progress. NPJ Regen Med. 2019;4(1):22. doi: 10.1038/s41536-019-0083-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lian J, Lv S, Liu C, et al. Effects of serial passage on the characteristics and cardiac and neural differentiation of human umbilical cord Wharton’s jelly-derived mesenchymal stem cells. Stem Cells Int. 2016;2016:9291013. doi: 10.1155/2016/9291013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liau LL, Looi QH, Chia WC, Subramaniam T, Ng MH, Law JX. Treatment of spinal cord injury with mesenchymal stem cells. Cell Biosci. 2020;10:112. doi: 10.1186/s13578-020-00475-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lopez-Verrilli MA, Caviedes A, Cabrera A, Sandoval S, Wyneken U, Khoury M. Mesenchymal stem cell-derived exosomes from different sources selectively promote neuritic outgrowth. Neuroscience. 2016;320:129–139. doi: 10.1016/j.neuroscience.2016.01.061 [DOI] [PubMed] [Google Scholar]
- 93.Del Fattore A, Luciano R, Saracino R, et al. Differential effects of extracellular vesicles secreted by mesenchymal stem cells from different sources on glioblastoma cells. Expert Opin Biol Ther. 2015;15(4):495–504. doi: 10.1517/14712598.2015.997706 [DOI] [PubMed] [Google Scholar]
- 94.Katsuda T, Tsuchiya R, Kosaka N, et al. Human adipose tissue-derived mesenchymal stem cells secrete functional neprilysin-bound exosomes. Sci Rep. 2013;3(1):1197. doi: 10.1038/srep01197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Álvarez-viejo M. Mesenchymal stem cells from different sources and their derived exosomes: a pre-clinical perspective. World J Stem Cells. 2020;12(2):100. doi: 10.4252/wjsc.v12.i2.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nikfarjam S, Rezaie J, Zolbanin NM, Jafari R. Mesenchymal stem cell derived-exosomes: a modern approach in translational medicine. J Transl Med. 2020;18(1):449. doi: 10.1186/s12967-020-02622-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yin K, Wang S, Zhao RC. Exosomes from mesenchymal stem/stromal cells: a new therapeutic paradigm. Biomark Res. 2019;7(1):8. doi: 10.1186/s40364-019-0159-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tang Y, Zhou Y, Li H-J. Advances in mesenchymal stem cell exosomes: a review. Stem Cell Res Ther. 2021;12(1):71. doi: 10.1186/s13287-021-02138-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kourembanas S. Exosomes: vehicles of intercellular signaling, biomarkers, and vectors of cell therapy. Annu Rev Physiol. 2015;77(1):13–27. doi: 10.1146/annurev-physiol-021014-071641 [DOI] [PubMed] [Google Scholar]
- 100.Fu S, Wang Y, Xia X, Zheng JC. Exosome engineering: current progress in cargo loading and targeted delivery. NanoImpact. 2020;20:100261. doi: 10.1016/j.impact.2020.100261 [DOI] [Google Scholar]
- 101.Gholami L, Nooshabadi VT, Shahabi S, et al. Extracellular vesicles in bone and periodontal regeneration: current and potential therapeutic applications. Cell Biosci. 2021;11(1):16. doi: 10.1186/s13578-020-00527-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9(6):654–659. doi: 10.1038/ncb1596 [DOI] [PubMed] [Google Scholar]
- 103.Wu C, Tian B, Qu X, et al. MicroRNAs play a role in chondrogenesis and osteoarthritis (review). Int J Mol Med. 2014;34(1):13–23. doi: 10.3892/ijmm.2014.1743 [DOI] [PubMed] [Google Scholar]
- 104.Mihanfar A, Shakouri SK, Khadem-Ansari MH, et al. Exosomal miRNAs in osteoarthritis. Mol Biol Rep. 2020;47(6):4737–4748. doi: 10.1007/s11033-020-05443-1 [DOI] [PubMed] [Google Scholar]
- 105.Peng B, Chen Y, Leong KW. MicroRNA delivery for regenerative medicine. Adv Drug Deliv Rev. 2015;88:108–122. doi: 10.1016/j.addr.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Schwarzenbach H, Gahan PB. MicroRNA shuttle from cell-to-cell by exosomes and its impact in cancer. Noncoding RNA. 2019;5(1). doi: 10.3390/ncrna5010028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Conigliaro A, Costa V, Lo Dico A, et al. CD90+ liver cancer cells modulate endothelial cell phenotype through the release of exosomes containing H19 lncRNA. Mol Cancer. 2015;14(1):155. doi: 10.1186/s12943-015-0426-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhang C, Wang P, Jiang P, et al. Upregulation of lncRNA HOTAIR contributes to IL-1β-induced MMP overexpression and chondrocytes apoptosis in temporomandibular joint osteoarthritis. Gene. 2016;586(2):248–253. doi: 10.1016/j.gene.2016.04.016 [DOI] [PubMed] [Google Scholar]
- 109.Yang L, Zhai Y, Hao Y, Zhu Z, Cheng G. The regulatory functionality of exosomes derived from hUMSCs in 3D culture for Alzheimer’s disease therapy. Small. 2019;16:3. doi: 10.1002/smll.201906273 [DOI] [PubMed] [Google Scholar]
- 110.Cao J, Wang B, Tang T, et al. Three-dimensional culture of MSCs produces exosomes with improved yield and enhanced therapeutic efficacy for cisplatin-induced acute kidney injury. Stem Cell Res Ther. 2020;11(1):206. doi: 10.1186/s13287-020-01719-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Liau LL, Hassan MN, Tang YL, Ng MH, Law JX. Feasibility of human platelet lysate as an alternative to foetal bovine serum for in vitro expansion of chondrocytes. Int J Mol Sci. 2021;22(3):1269. doi: 10.3390/ijms22031269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Evans CH, Kraus VB, Setton LA. Progress in intra-articular therapy. Nat Rev Rheumatol. 2014;10(1):11–22. doi: 10.1038/nrrheum.2013.159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pinheiro A, Silva AM, Teixeira JH, et al. Extracellular vesicles: intelligent delivery strategies for therapeutic applications. J Control Release. 2018;289:56–69. doi: 10.1016/j.jconrel.2018.09.019 [DOI] [PubMed] [Google Scholar]
- 114.Patil M, Henderson J, Luong H, Annamalai D, Sreejit G, Krishnamurthy P. The art of intercellular wireless communications: exosomes in heart disease and therapy. Front Cell Dev Biol. 2019;7:315. doi: 10.3389/fcell.2019.00315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Quesenberry PJ, Aliotta J, Deregibus MC, Camussi G. Role of extracellular RNA-carrying vesicles in cell differentiation and reprogramming. Stem Cell Res Ther. 2015;6(1):153. doi: 10.1186/s13287-015-0150-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Qi H, Liu DP, Xiao DW, Tian DC, Su YW, Jin SF. Exosomes derived from mesenchymal stem cells inhibit mitochondrial dysfunction-induced apoptosis of chondrocytes via p38, ERK, and Akt pathways. In Vitro Cell Dev Biol Anim. 2019;55(3):203–210. doi: 10.1007/s11626-019-00330-x [DOI] [PubMed] [Google Scholar]
- 117.De Jong OG, Van Balkom BWM, Schiffelers RM, Bouten CVC, Verhaar MC. Extracellular vesicles: potential roles in regenerative medicine. Front Immunol. 2014;5:608. doi: 10.3389/fimmu.2014.00608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wang Y, Yao J, Cai L, et al. Bone-targeted extracellular vesicles from mesenchymal stem cells for osteoporosis therapy. Int J Nanomedicine. 2020;15:7967–7977. doi: 10.2147/IJN.S263756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Glasson SS, Chambers MG, Berg WBVD, Little CB. The OARSI histopathology initiative – recommendations for histological assessments of osteoarthritis in the mouse. Osteoarthritis Cartilage. 2010;18:S17–S23. doi: 10.1016/j.joca.2010.05.025 [DOI] [PubMed] [Google Scholar]
- 120.Paramitha D, Fakhrul Ulum M, Purnama A, Wicaksono D, Noviana D, Hermawan H. Monitoring degradation products and metal ions in vivo. In: Narayan R, editor. Monitoring and Evaluation of Biomaterials and Their Performance in vivo. Sawston: Woodhead Publishing; 2016:19–43. doi: 10.1016/B978-0-08-100603-0.00002-X [DOI] [Google Scholar]
- 121.Bergholt NL, Lysdahl H, Lind M, Foldager CB. A standardized method of applying toluidine blue metachromatic staining for assessment of chondrogenesis. Cartilage. 2019;10(3):370–374. doi: 10.1177/1947603518764262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Henrotin Y, Sanchez C, Bay-Jensen AC, Mobasheri A. Osteoarthritis biomarkers derived from cartilage extracellular matrix: current status and future perspectives. Ann Phys Rehabil Med. 2016;59(3):145–148. doi: 10.1016/j.rehab.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 123.Roughley PJ, Mort JS. The role of aggrecan in normal and osteoarthritic cartilage. J Exp Orthop. 2014;1(1):8. doi: 10.1186/s40634-014-0008-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hoshi H, Akagi R, Yamaguchi S, et al. Effect of inhibiting MMP13 and ADAMTS5 by intra-articular injection of small interfering RNA in a surgically induced osteoarthritis model of mice. Cell Tissue Res. 2017;368(2):379–387. doi: 10.1007/s00441-016-2563-y [DOI] [PubMed] [Google Scholar]
- 125.Hwang HS, Kim HA. Chondrocyte apoptosis in the pathogenesis of osteoarthritis. Int J Mol Sci. 2015;16(11):26035. doi: 10.3390/ijms161125943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Liu H, Liang Z, Wang F, et al. Exosomes from mesenchymal stromal cells reduce murine colonic inflammation via a macrophage-dependent mechanism. JCI Insight. 2019;4(24):131273. doi: 10.1172/jci.insight.131273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Li X, Liu L, Yang J, et al. Exosome derived from human umbilical cord mesenchymal stem cell mediates miR-181c attenuating burn-induced excessive inflammation. EBioMedicine. 2016;8:72–82. doi: 10.1016/j.ebiom.2016.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang B, Yin Y, Lai RC, Tan SS, Choo ABH, Lim SK. Mesenchymal stem cells secrete immunologically active exosomes. Stem Cells Dev. 2014;23(11):1233–1244. doi: 10.1089/scd.2013.0479 [DOI] [PubMed] [Google Scholar]
- 129.Lee C, Mitsialis SA, Aslam M, et al. Exosomes mediate the cytoprotective action of mesenchymal stromal cells on hypoxia-induced pulmonary hypertension. Circulation. 2012;126(22):2601–2611. doi: 10.1161/CIRCULATIONAHA.112.114173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Li G, Yin J, Gao J, et al. Subchondral bone in osteoarthritis: insight into risk factors and microstructural changes. Arthritis Res Ther. 2013;15(6):223. doi: 10.1186/ar4405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hu W, Chen Y, Dou C, Dong S. Microenvironment in subchondral bone: predominant regulator for the treatment of osteoarthritis. Ann Rheum Dis. 2020;80(4):413–422. doi: 10.1136/annrheumdis-2020-218089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Donell S. Subchondral bone remodelling in osteoarthritis. EFORT Open Rev. 2019;4(6):221–229. doi: 10.1302/2058-5241.4.180102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bellido M, Lugo L, Roman-Blas JA, et al. Improving subchondral bone integrity reduces progression of cartilage damage in experimental osteoarthritis preceded by osteoporosis. Osteoarthritis Cartilage. 2011;19(10):1228–1236. doi: 10.1016/j.joca.2011.07.003 [DOI] [PubMed] [Google Scholar]
- 134.Hayami T, Pickarski M, Zhuo Y, Wesolowski GA, Rodan GA, Duong LT. Characterization of articular cartilage and subchondral bone changes in the rat anterior cruciate ligament transection and meniscectomized models of osteoarthritis. Bone. 2006;38(2):234–243. doi: 10.1016/j.bone.2005.08.007 [DOI] [PubMed] [Google Scholar]
- 135.Hayami T, Pickarski M, Wesolowski GA, et al. The role of subchondral bone remodeling in osteoarthritis: reduction of cartilage degeneration and prevention of osteophyte formation by alendronate in the rat anterior cruciate ligament transection model. Arthritis Rheum. 2004;50(4):1193–1206. doi: 10.1002/art.20124 [DOI] [PubMed] [Google Scholar]
- 136.Burr DB, Schaffler MB. The involvement of subchondral mineralized tissues in osteoarthrosis: quantitative microscopic evidence. Microsc Res Tech. 1997;37(4):343–357. doi: [DOI] [PubMed] [Google Scholar]
- 137.Lories RJ, Luyten FP. The bone-cartilage unit in osteoarthritis. Nat Rev Rheumatol. 2011;7(1):43–49. doi: 10.1038/nrrheum.2010.197 [DOI] [PubMed] [Google Scholar]
- 138.Yuan XL, Meng HY, Wang YC, et al. Bone-cartilage interface crosstalk in osteoarthritis: potential pathways and future therapeutic strategies. Osteoarthritis Cartilage. 2014;22(8):1077–1089. doi: 10.1016/j.joca.2014.05.023 [DOI] [PubMed] [Google Scholar]
- 139.Zhang W, Lian Q, Li D, et al. Cartilage repair and subchondral bone migration using 3d printing osteochondral composites: a one-year-period study in rabbit trochlea. Biomed Res Int. 2014;2014:e746138. doi: 10.1155/2014/746138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Zhu S, Zhu J, Zhen G, et al. Subchondral bone osteoclasts induce sensory innervation and osteoarthritis pain. J Clin Invest. 2019;129(3):1076–1093. doi: 10.1172/JCI121561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhu J, Zhen G, An S, et al. Aberrant subchondral osteoblastic metabolism modifies NaV1.8 for osteoarthritis. Elife. 2020;9. doi: 10.7554/eLife.57656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Sousa M, Ferraresi C, Carolina A, Yoshimura E, Hamblin M. Building, testing and validating a set of home-made von Frey filaments: a precise, accurate and cost effective alternative for nociception assessment. J Neurosci Methods. 2014;232:1–5. doi: 10.1016/j.jneumeth.2014.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Deuis JR, Dvorakova LS, Vetter I. Methods used to evaluate pain behaviors in rodents. Front Mol Neurosci. 2017;10:284. doi: 10.3389/fnmol.2017.00284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Hawker GA, Stewart L, French MR, et al. Understanding the pain experience in hip and knee osteoarthritis–an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 2008;16(4):415–422. doi: 10.1016/j.joca.2007.12.017 [DOI] [PubMed] [Google Scholar]
- 145.Duarte RV, Raphael JH, Dimitroulas T, et al. Osteoarthritis pain has a significant neuropathic component: an exploratory in vivo patient model. Rheumatol Int. 2014;34(3):315–320. doi: 10.1007/s00296-013-2893-y [DOI] [PubMed] [Google Scholar]
- 146.Valdes AM, Suokas AK, Doherty SA, Jenkins W, Doherty M. History of knee surgery is associated with higher prevalence of neuropathic pain-like symptoms in patients with severe osteoarthritis of the knee. Semin Arthritis Rheum. 2014;43(5):588–592. doi: 10.1016/j.semarthrit.2013.10.001 [DOI] [PubMed] [Google Scholar]
- 147.Lakes EH, Allen KD. Gait analysis methods for rodent models of arthritic disorders: reviews and recommendations. Osteoarthritis Cartilage. 2016;24(11):1837–1849. doi: 10.1016/j.joca.2016.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478):eaau6977. doi: 10.1126/science.aau6977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gomzikova MO, James V, Rizvanov AA. Therapeutic application of mesenchymal stem cells derived extracellular vesicles for immunomodulation. Front Immunol. 2019;10:2663. doi: 10.3389/fimmu.2019.02663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Elahi FM, Farwell DG, Nolta JA, Anderson JD. Preclinical translation of exosomes derived from mesenchymal stem/stromal cells. Stem Cells. 2020;38(1):15–21. doi: 10.1002/stem.3061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Robbins PD, Morelli AE. Regulation of immune responses by extracellular vesicles. Nat Rev Immunol. 2014;14(3):195–208. doi: 10.1038/nri3622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Toma C, Wagner WR, Bowry S, Schwartz A, Villanueva F. Fate of culture-expanded mesenchymal stem cells in the microvasculature: in vivo observations of cell kinetics. Circ Res. 2009;104(3):398–402. doi: 10.1161/CIRCRESAHA.108.187724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Caplan AI, Dennis JE. Mesenchymal stem cells as trophic mediators. J Cell Biochem. 2006;98(5):1076–1084. doi: 10.1002/jcb.20886 [DOI] [PubMed] [Google Scholar]
- 154.Beltrami AP, Cesselli D, Beltrami CA. Stem cell senescence and regenerative paradigms. Clin Pharmacol Ther. 2012;91(1):21–29. doi: 10.1038/clpt.2011.262 [DOI] [PubMed] [Google Scholar]
- 155.Sverdlov ED, Mineev K. Mutation rate in stem cells: an underestimated barrier on the way to therapy. Trends Mol Med. 2013;19(5):273–280. doi: 10.1016/j.molmed.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 156.Lee AS, Tang C, Rao MS, Weissman IL, Wu JC. Tumorigenicity as a clinical hurdle for pluripotent stem cell therapies. Nat Med. 2013;19(8):998–1004. doi: 10.1038/nm.3267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Vizoso FJ, Eiro N, Cid S, Schneider J, Perez-Fernandez R. mesenchymal stem cell secretome: toward cell-free therapeutic strategies in regenerative medicine. Int J Mol Sci. 2017;18(9):1852. doi: 10.3390/ijms18091852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Naseri Z, Oskuee RK, Jaafari MR, Forouzandeh Moghadam M. Exosome-mediated delivery of functionally active miRNA-142-3p inhibitor reduces tumorigenicity of breast cancer in vitro and in vivo. Int J Nanomedicine. 2018;13:7727–7747. doi: 10.2147/IJN.S182384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Huyan T, Li H, Peng H, et al. Extracellular vesicles - advanced nanocarriers in cancer therapy: progress and achievements. Int J Nanomedicine. 2020;15:6485–6502. doi: 10.2147/IJN.S238099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Imai T, Takahashi Y, Nishikawa M, et al. Macrophage-dependent clearance of systemically administered B16BL6-derived exosomes from the blood circulation in mice. J Extracell Vesicles. 2015;4(1):26238. doi: 10.3402/jev.v4.26238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lai CP, Mardini O, Ericsson M, et al. Dynamic biodistribution of extracellular vesicles in vivo using a multimodal imaging reporter. ACS Nano. 2014;8(1):483–494. doi: 10.1021/nn404945r [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Cheng J, Abdi S. Complications of joint, tendon, and muscle injections. Tech Reg Anesth Pain Manag. 2007;11(3):141–147. doi: 10.1053/j.trap.2007.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Witwer KW, Théry C. Extracellular vesicles or exosomes? On primacy, precision, and popularity influencing a choice of nomenclature. J Extracell Vesicles. 2019;8(1):1648167. doi: 10.1080/20013078.2019.1648167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Haraszti RA, Miller R, Stoppato M, et al. Exosomes produced from 3D cultures of MSCs by tangential flow filtration show higher yield and improved activity. Mol Ther. 2018;26(12):2838–2847. doi: 10.1016/j.ymthe.2018.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Pachler K, Lener T, Streif D, et al. A good manufacturing practice-grade standard protocol for exclusively human mesenchymal stromal cell-derived extracellular vesicles. Cytotherapy. 2017;19(4):458–472. doi: 10.1016/j.jcyt.2017.01.001 [DOI] [PubMed] [Google Scholar]
- 166.Chen T, Arslan F, Yin Y, et al. Enabling a robust scalable manufacturing process for therapeutic exosomes through oncogenic immortalization of human ESC-derived MSCs. J Transl Med. 2011;9(1):47. doi: 10.1186/1479-5876-9-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lian Q, Lye E, Suan Yeo K, et al. Derivation of clinically compliant MSCs from CD105+, CD24- differentiated human ESCs. Stem Cells. 2007;25(2):425–436. doi: 10.1634/stemcells.2006-0420 [DOI] [PubMed] [Google Scholar]
- 168.Herrmann M, Diederichs S, Melnik S, et al. Extracellular vesicles in musculoskeletal pathologies and regeneration. Front Bioeng Biotechnol. 2021;8:624096. doi: 10.3389/fbioe.2020.624096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sabapathy V, Kumar S. hiPSC‐derived iMSCs: NextGen MSCs as an advanced therapeutically active cell resource for regenerative medicine. J Cell Mol Med. 2016;20(8):1571–1588. doi: 10.1111/jcmm.12839 [DOI] [PMC free article] [PubMed] [Google Scholar]