Abstract
The coronavirus disease 2019 (COVID-19) pandemic has had a profound and often devastating impact on global healthcare systems. Healthcare systems have had to repurpose programs and staff as part of COVID-19 relief efforts. The infrastructure and skilled personnel of antimicrobial stewardship programs (ASPs) have been utilized in new ways as part of COVID-19 pandemic response efforts. A critical focus of ASPs both before and during the pandemic has been on limiting the development of antimicrobial resistance. Fortunately, existing data indicate that rates of bacterial co-infection are relatively low and ASPs should continue aggressive efforts to limit unnecessary antimicrobial use. ASPs have taken a lead role in COVID-19 focused guideline creation and curation, as well as in helping to steward access to potential novel therapeutic agents. Disparities in ASP program resources and personnel exist, and ASP activities focused on the COVID-19 response should be tailored to individual settings. There is an urgent need for research to help inform ASP best practices within pandemic response efforts that take into account local resources. Investment in infrastructure and personnel is urgently needed both in the context of current relief efforts and to prepare for future pandemics.
KEYWORDS: COVID-19, Antimicrobial Stewardship, Antimicrobial Resistance, SARS-CoV-2, Viral infections
Key issues
-
•
Rates of bacterial co-infection with coronavirus disease 2019 (COVID-19) are relatively low, but antibiotic use is high; judicious antibiotic use is critical to reduce the emergence of antibiotic resistance and to decrease toxicity from unnecessary antibiotics.
-
•
Existing antimicrobial stewardship program (ASP) infrastructure for guideline development, prospective audit, and feedback, along with antimicrobial restriction can be utilized directly in COVID-19 pandemic relief efforts.
-
•
ASPs can play important roles in stewarding access to novel or investigational therapeutic agents for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
-
•
Data on specific antimicrobial stewardship activities focused on COVID-19 relief are limited.
-
•
There is an urgent need for research to help inform antimicrobial stewardship best practices within pandemic response efforts that take into account local resources.
-
•
Investment in infrastructure and personnel is urgently needed both in the context of current relief efforts and to prepare for future pandemics.
1. Known facts
1.1. Scope of the pandemic
As of May 20, 2021 there have been 164 922 114 cases and 3 418 084 deaths from coronavirus disease 2019 (COVID-19) worldwide according to the COVID-19 Dashboard maintained by the Center for Systems Science and Engineering at Johns Hopkins University. Additionally, healthcare workers have comprised a significant number of cases ranging from 3.9% to 13.1% and 0.5–1.9% of deaths in various studies (Bandyopadhyay et al., 2020; Guerrero-Torres et al., 2020; Lapolla et al., 2021). The current pandemic has placed an unprecedented strain on global healthcare systems, which in addition to the loss of life has caused significant economic disruption, leading to shortages of personal protective equipment (PPE) and medications (Badreldin and Atallah, 2021). The pandemic has also caused disruptions in routine access to care, including routine procedures and mental healthcare. According to the United States Centers for Disease Control and Prevention (CDC), an estimated 41% of adults in the United States delayed or avoided medical care relating to concerns about COVID-19 (Czeisler et al., 2020).
1.2. Antimicrobial overuse
1.2.1. Antimicrobial use patterns during the COVID-19 pandemic [Au?2]
The potential financial and human impacts of increasing antimicrobial resistance are well established (O'Neill, 2016; World Health Organization, 2015). Prior to the COVID-19 pandemic, rates of antimicrobial resistance were increasing globally (Oldenkamp et al., 2021). A major concern with the COVID-19 pandemic is that antimicrobial use in patients with COVID-19 will drive antimicrobial resistance. Furthermore, there is concern that strained and overwhelmed healthcare systems will not be able maintain compliance with infection prevention and antimicrobial stewardship best practices, further driving the potential cross-transmission of antimicrobial-resistant organisms.
There are some data to suggest antimicrobial prescribing in the outpatient setting has decreased during the pandemic, according to data summarized from the IQVIA National Prescription Audit databases (Buehrle et al., 2020). Initial decreases in prescribing patterns were attributed to a decrease in overall outpatient visits. However, sustained reductions in azithromycin, amoxicillin, and levofloxacin were seen from April 2020 to July 2020, despite a rebound in ciprofloxacin, trimethoprim–sulfamethoxazole, clindamycin, doxycycline, nitrofurantoin, and cephalexin to pre-pandemic levels (Buehrle et al., 2020).
According to a recent meta-analysis including more than 30 000 patients, the prevalence of bacterial infection in COVID-19 is approximately 8.6% (Langford et al., 2021). However, on average 64% of patients received antibiotics (Langford et al., 2021). Out of the 154 studies examined, 115 were conducted in China. It was noted that as the pandemic continued, the rate of prescribing decreased from a high of 82.8% of patients in January 2020 to 62.6% in April 2020. The largest absolute prescribing rates were seen in Southeast and East Asia (excluding China) at 87.5% and the lowest rates in Europe at 63.1% (Langford et al., 2021).
In addition to the potential effect on antimicrobial resistance, significant increases in antimicrobial consumption in a pandemic setting can strain global supply and lead to medication shortages. Antimicrobial stewardship program (ASP) interventions are essential to prevent unnecessary antimicrobial prescribing.
1.3. Summary of the available literature on the role of the antimicrobial stewardship program during COVID-19
1.3.1. Antimicrobial stewardship interventions targeting COVID-19
Existing ASP tools can be repurposed to serve a supporting role during a pandemic. Two of the most powerful tools in the ASP arsenal are prospective audit and feedback (PAF) and formulary restriction and pre-authorization. These tools have shown success in impacting the care of patients with COVID-19 (Kubin et al., 2021; Mazdeyasna et al., 2020; Tande et al., 2020).
PAF can be applied to determine which patients may benefit most from diagnostic testing when resources are limited, or to review the appropriate use of COVID-19 focused medications and concomitant antimicrobial use (Mazdeyasna et al., 2020). ASPs can also utilize PAF to assist with medication toxicity monitoring. An academic medical system in New York City reported generating ASP alerts for hydroxychloroquine without QTc monitoring and remdesivir without liver function studies. They also reported utilizing PAF to review the frequency of antimicrobial administration in order to limit entering isolation rooms for medication administration (Kubin et al., 2021).
ASP interventions have been expanded successfully to guide the use of novel and investigational therapeutics such as hydroxychloroquine, remdesivir, and lopinavir/ritonavir to help ameliorate potential medication shortages. An observational study from the Mayo Clinic examined the effect of expanding ASP PAF activities to include hydroxychloroquine use review after seeing an 85% increase in utilization early in the pandemic. After PAF services were deployed, they reported a reduction in hydroxychloroquine use to pre-pandemic levels (Tande et al., 2020). Other programs have implemented antimicrobial restriction on potential COVID-19 therapeutics (Mazdeyasna et al., 2020). Although antimicrobial restriction typically has occurred in the inpatient setting, some ASPs have been involved in outpatient antimicrobial restriction for therapeutics such as hydroxychloroquine and monoclonal antibodies.
Additional core ASP activities can include local guideline development. Many ASPs already have local use guidelines, and their knowledge with guideline development, dissemination, and monitoring for guideline compliance can be utilized in COVID-19 focused pandemic relief efforts. Anecdotally, this is one area where many ASPs have provided tremendous value during the pandemic. ASPs have taken leadership roles in the creation and curation of COVID-19 focused treatment guidelines that incorporate novel therapeutic agents, comments on existing literature, and also delineate clinical trial options, when available. One of the authors of this paper notes that his ASP spent over 300 hours in the first year of the pandemic on guidelines creation and curation, with over 85 updates being released.
Guidelines and protocols can be disseminated rapidly to providers via numerous mechanisms. Some programs have utilized local intranet or internet sites, some have used Word documents, and others have utilized more sophisticated methods including dissemination via mobile phone applications. Mass e-mail alerts or newsletters can also be utilized and may be more attractive in resource-limited settings. The Commonwealth Partnerships for Antimicrobial Stewardship Programme is a non-profit organization funded by the United Kingdom Department of Health. The program offers a free web-based or mobile application that includes the World Health Organization (WHO) AWaRE (Access, Watch, Reserve) categorization of antibacterials, national prescribing guidance for Ghana, Tanzania, Uganda, and Zambia, along with regional and international guidance on COVID-19 (https://viewer.microguide.global/CPA/CWPAMS).
ASPs can also work in coordination with microbiology to provide regular updates on institutional/local COVID-19 infection [Au?3] rates and to trend resistance in key organisms as well.
ASPs can also be involved in helping to obtain access to novel therapeutics via other mechanisms, such as assisting with completing paperwork for expanded access investigational drug applications and helping providers and patients navigate enrolling in clinical trials (Stevens Michael et al., 2020). Additionally, in the United States, medications such as remdesivir and monoclonal antibodies available under emergency use authorization were provided by the federal government via local state health departments. Access to novel therapeutic agents under this mechanism can include local monitoring and reporting requirements. ASPs have taken leadership roles in helping providers and health systems navigate state-specific access and reporting requirements.
Health system stresses related to the COVID-19 pandemic can also impact existing, non-COVID-19 focused ASP activities. A case study from a six-hospital New York City academic medical system comprising 2600 beds located within an early epicenter for COVID-19, reported a significant increase in alerts for post prescription review during the height of the pandemic. Additionally, these authors noted that time dedicated to traditional PAF activities was diverted to monitoring the use of investigational agents and coordination with COVID-19 focused clinical trials. It was also noted that antimicrobial restriction was rescinded for levofloxacin in order to encourage less frequent dosing schedules, which allowed decreased healthcare worker exposure to isolation rooms (Kubin et al., 2021).
A separate report from a 1500-bed academic medical center noted a significant strain on the infectious diseases (ID) consult service relating to patients with known or suspected COVID-19. They describe a modification to their ASP workflow to identify patients with suspected or confirmed COVID-19 infection [Au?3]. These lists were reviewed daily by the ASP team to evaluate for therapeutic interventions, clinical trial enrollment, drug toxicity, antibiotic use, and the need for formal ID consultation (Davis et al., 2020). During a pandemic, ASP resources and personnel may need to be expanded to prevent delays in approval and ensure pre-pandemic activities are not negatively impacted.
One of the authors of the current paper quantified the time impact of COVID-19 focused activities over a 13-month time span for his ASP: this included approximately 1200 hours of work focused solely on COVID-19. The data in the literature are sparse, but significant concern exists that a shift in focus to COVID-19 relief activities may have eroded traditional ASP efforts during the pandemic. It is also conceivable that some programs may have taken steps to bolster their ASPs during the pandemic. This may have included enhanced collaboration (or even integration) with infection prevention programs, the expansion of existing personnel, and the development of new data access and reporting infrastructure. Program enhancements that occurred during or as a result of the pandemic may enhance non-COVID-19 focused activities post-pandemic.
1.3.2. Regional practices
A survey conducted in May 2020 in Ireland among 98 antimicrobial stewardship and ID personnel found that 76% of respondents reported a significant decrease in traditional ASP program effectiveness as a result of the pandemic (Martin et al., 2021). Respondents had noted increased broad-spectrum antimicrobial use, decreased adherence to local guidelines, resistance to de-escalation recommendations, decreased multidrug-resistant organism (MDRO) monitoring, and drug shortages (Martin et al., 2021). Conversely, a study from Singapore demonstrated that ASP acceptance rates were maintained during the pandemic, and patients with ASP interventions had decreased broad-spectrum antimicrobial usage and length of stay (Liew et al., 2020). There is significant disparity in regional rates of COVID-19 infection [Au?3], resource availability, and infrastructure. ASPs will need to develop policies and procedures that are suited for local institutions.
1.4. Resource-limited settings
1.4.1. Limited availability of infectious diseases expertise
A 2012 global survey of 660 hospitals across 67 countries conducted by the European Society of Clinical Microbiology and Infectious Diseases, revealed that only 12% of hospitals in Africa reported the existence of an antimicrobial stewardship committee (Howard et al., 2014). An additional survey conducted in 2019 revealed that only five of 37 (13.5%) Nigerian hospitals had a formal antimicrobial stewardship team (Abubakar and Tangiisuran, 2020). The COVID-19 pandemic has highlighted the critical need for health systems to have formal, well-resourced ASPs. Health systems without ASPs should prioritize their creation. General guidance on establishing an ASP in low-to-middle-income countries (LMIC) is available separately (Pierce et al., 2020).
1.4.2. Optimal practice in areas with treatment availability limitations as well as less robust antimicrobial stewardship infrastructure
In regions where ASP access is not available or limited, the development of national guidelines for the management of COVID-19 can be adopted and utilized by local healthcare facilities. Local stewardship champions should be identified at individual institutions, who can be drawn from physician, pharmacy, or nursing positions. Established infection prevention and control teams can also take on responsibilities of stewardship.
1.5. Medication shortages
The disruption of global trade relating to the COVID-19 pandemic, combined with increased medication utilization, has led to widespread drug shortages (Badreldin and Atallah, 2021). Even high-income countries have not been immune to medication shortages during the COVID-19 pandemic. According to data compiled by the American Society of Health-System Pharmacists from the University of Utah Drug Information Service, drug shortages were already increasing prior to the pandemic, and there were 271 drug shortages reported in the United States in quarter 1 of 2021. Additionally, 29 of 40 drugs listed as critical for the management of COVID-19 were included among the shortages (The American Society of Health-System Pharmacists, 2021). According to the Center for Infectious Disease Research and Policy, factory shutdowns in China from the start of the pandemic produced a shortage of raw materials for generic medication production in India (Seifert et al., 2020). They note that nearly 80% of the global antibiotic supply is dependent on China. Additionally, Italy was the largest producer of antibiotics for the European Unions and was hit early in the pandemic. The Center for Infectious Disease Research and Policy argues for greater transparency in the pharmaceutical supply chain to predict drug shortages more accurately in the future.
The importance of the ASP strategy of formulary restriction with pre-authorization has been highlighted during the pandemic: impacting both access to potential novel therapeutics and non-COVID-19 focused medications that may be in short supply. PAF and formulary restriction with pre-authorization are proven strategies to decrease antimicrobial consumption and can be applied to novel therapeutic agents for COVID-19, as mentioned previously. Additionally, some ASPs have been involved in stewarding non-antibiotic medications such as tocilizumab. ASPs have also been involved in helping to develop new mechanisms for the monitoring of key drug stocks, which often include non-antimicrobial medications, including dexamethasone and tocilizumab, among others.
Comprehensive management of medication shortages is beyond the scope of this review. However, the WHO COVID-19 essential supplies forecasting tool (COVID-ESFT) can be utilized to help predict shortages of medications, oxygen, and PPE (available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Tools-Essential_forecasting-Overview-2020.1).
2. Suggested practice
2.1. Restriction of medications
Local policies and guidelines should be developed for the distribution of novel and investigational therapeutic agents for COVID-19. Where resources allow, restriction and pre-authorization measures should be instituted and led by an ASP or pharmacy. National and international guidance is available that can be adapted for local institutions (National Institutes of Health, 2020; World Health Organization, 2021). Processes should be put in place that allow for the frequent and rapid review of new literature and professional and government guidelines in order to allow the optimization of restriction and pre-authorization measures in as close to real-time as possible.
2.2. Development of treatment guidelines
Guidelines are available through the WHO, the Infectious Diseases Society of America (IDSA), United Kingdom National Institute for Health and Care Excellence (NICE), and the United States National Institutes of Health (NIH) that can be adapted for individual regions. These can be accessed from their respective websites free of charge.
2.3. Use of empiric antibiotics in patients with COVID-19
The WHO recommends against the use of empiric antibiotics in patients with mild COVID-19 (World Health Organization, 2021). In patients with moderate disease, antibiotics should not be considered unless there is clinical concern for bacterial pneumonia, with a recommendation to utilize WHO Access category antibiotics where appropriate. For patients with COVID-19 and shock, the WHO recommends empiric antibiotics as a part of standard empiric bacterial sepsis coverage (World Health Organization, 2021).
The NICE guidelines state that antibiotics should not be prescribed if COVID-19 is the likely cause of respiratory illness, unless there is a suspicion for bacterial infection (National Institute for Health and Care Excellence, 2021). According to the United States NIH, there are insufficient data to recommend empiric broad-spectrum antibiotics in patients with COVID-19, even those with severe or critical illness, without a clear indication. They suggest that if antimicrobials are initiated, they should be addressed daily for de-escalation (National Institutes of Health, 2020).
Diagnostic tools are needed to identify patients with potential bacterial superinfection. Some patients with COVID-19 and superimposed bacterial infection have increased procalcitonin levels (May et al., 2021). A retrospective study in the United Kingdom examining the impact of expanding National Health Service guidelines on limiting antibiotic use in patients with a procalcitonin level of less than 0.25 ng/ml, found a more than two-fold reduction in defined daily doses of antibiotic use without any increase in mortality among 368 patients (Williams et al., 2021). A separate retrospective descriptive study discovered that procalcitonin levels were elevated in patients with COVID-19 who were not believed to have bacterial pneumonia in 21% of cases. This population of patients with elevated procalcitonin and no evidence of bacterial pneumonia was found to have 1.8 additional days of antibiotics compared to patients with a negative procalcitonin (P < 0.01) (Fabre et al., 2021). An alternative marker, the ferritin-to-procalcitonin ratio, has a reported sensitivity of 85% and specificity of 56% for differentiating COVID-19 from bacterial pneumonia at a cutoff level of ≥877 [Au?4]. However, patients with bacterial co-infection were excluded (Gharamti et al., 2021). Other authors examined the baseline white blood cell count and the change in C-reactive protein with 48 hours of antibiotics and were able to exclude bacterial co-infection in 46% of cases among a cohort of 619 patients with COVID-19. They reported a sensitivity of greater than 90% and a specificity of 43% for differentiating COVID-19 from bacterial pneumonia with this strategy (Mason et al., 2021). Overall, the data regarding the use of laboratory markers to risk-stratify patients with COVID-19 who may have bacterial pneumonia are limited.
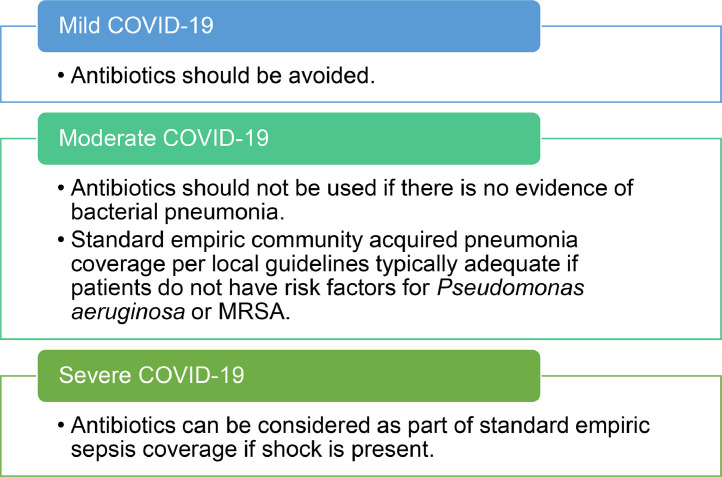
ASP programs can assist with appropriate utilization of antibiotics in patients with COVID-19 using previously mentioned strategies of guideline development, PAF, and antimicrobial restriction. Where resources allow, a process to review all antimicrobial prescribing in patients with COVID-19 can be considered. A recommended practice for antimicrobial prescribing in patients with COVID-19 can be seen in Figure 1 .
Figure 1.
Recommended practice for antimicrobial prescribing in patients with SARS-CoV-2 infection. Disease severity as classified by the World Health Organization.
2.4. Coordination with infection prevention and control
2.4.1. Isolation precautions
Close collaboration between antimicrobial stewardship and infection prevention and control teams is essential. Decreased antimicrobial use can directly impact PPE usage and nursing exposures to COVID-19 by limiting patient encounters (Jones et al., 2021). Many organizations (including the WHO and IDSA) have produced guidelines for infection prevention during the COVID-19 pandemic for both conventional and respiratory PPE shortage settings.
2.4.2. Diagnostic stewardship
The CDC has provided guidance on criteria for diagnostic testing for patients with suspected COVID-19. A recent Cochrane review demonstrated that questionnaire or temperature-based screening methods have poor sensitivity for detecting patients with COVID-19 (Viswanathan et al., 2020). Some inpatient institutions have implemented universal PCR testing for all admitted patients (Sastry et al., 2020). Particularly in resource-limited settings, ASPs can be involved in the diagnostic stewardship for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) through developing guidelines for testing and helping to identify patients who qualify for testing, in coordination with infection prevention programs and microbiology laboratories. The WHO has provided interim guidance on identifying patients for testing, along with specimen collection and handling (World Health Organization, 2020a). Data remain limited on ASP involvement in these activities.
2.5. Implementation of telehealth to limit the infection transmission risk
2.5.1. Clinic visits
As of December 2020, the WHO has recommended limiting face-to-face encounters where possible in order to conserve PPE, through the use of telemedicine where available (World Health Organization, 2020b).
The CDC has provided guidance for implementing telehealth during the COVID-19 pandemic (Centers for Disease Control and Prevention, 2020). Additional benefits of telehealth include limiting healthcare worker exposure to infectious individuals and allowing continued preventative or routine care. Cultural perceptions of telehealth and the availability of relevant technology are notable limitations.
A review article summarizing the available literature and providing practical guidance for the implementation of telehealth during COVID-19 is available (Bokolo Anthony Jnr, 2020).
2.5.2. ‘FaceTime’ interaction with inpatients
During the pandemic, regulatory bodies in the United States have relaxed regulations on the utilization of commonly available mobile applications such as FaceTime, Zoom, Cisco Webex, and Skype for telehealth (Bokolo Anthony Jnr, 2020). Anecdotal experience suggests that these strategies can be employed in the inpatient setting, but evidence on their use is lacking.
When implementing telehealth, it will be important to consult local laws and regulations regarding its use, along with addressing patient privacy concerns.
3. Controversial issues
3.1. Regional availability of novel agents
Global disparities in the distribution of novel therapeutic agents exist, and LMICs are most likely to be negatively impacted. It is critical that studies be done that ultimately will be relevant to all practice settings, such as the WHO Solidarity trial (WHO Solidarity Trial Consortium, 2021). It is also critical that trial results be analyzed in the most robust and practical way possible, to make sure that limited resources are being assigned to the potential therapeutics that are most likely to help patients.
3.2. Role of ASPs with regard to novel non-antimicrobial therapeutics and vaccinations
Although outside the traditional scope of ASPs, and there are limited data to support the practice, ASPs have been involved in pre-authorization and formulary restriction activities focused on non-antimicrobial agents such as tocilizumab during the current pandemic. Additionally, a role for ASPs in the distribution of convalescent plasma has been proposed (Stevens Michael et al., 2020). Similar principles have also been put forth to ration and appropriately allocate SARS-CoV-2 vaccinations (Nori et al., 2020) and monoclonal antibodies (Patel et al., 2020). Data on practical application of ASP initiatives in these domains are lacking currently.
3.3. Appropriate use of antifungal agents in patients with COVID-19
There is emerging evidence of co-infections with invasive pulmonary aspergillosis associated with COVID-19, although the exact incidence is unknown, with rates reported in the literature ranging from 3.8% to 34% and with significant heterogeneity in diagnostic definitions (Marr et al., 2021). The impact of COVID-19 on antifungal prescribing remains unknown. One study demonstrated no significant increase in antifungal prescribing after the onset of the pandemic (Nestler et al., 2021) and another demonstrated that patients with COVID-19 were more likely to be prescribed antifungal therapy (Seaton et al., 2020).
An expert consensus from the European Confederation of Medical Mycology and the International Society for Human and Animal Mycology provides suggested criteria for the testing, diagnosis, and treatment of invasive aspergillosis associated with COVID-19 (Koehler et al., 2021). It should be noted that there is also emerging evidence of increased rates of mucormycosis in patients with COVID-19, potentially related to corticosteroid use. This condition has significant associated mortality and could also drive antifungal prescriptions (Singh et al., 2021).
ASPs are essential in helping to determine the appropriate use of antifungal therapy through interpretation of the available literature and the development of local guidelines, along with the potential restriction of antifungal agents where resources allow.
4. Knowledge gaps and need for further research
The impact of COVID-19 on antimicrobial resistance is unknown and will serve as a key target for future studies. Continued research on appropriate biomarkers to exclude bacterial co-infection in patients with COVID-19 is also needed. Additionally, the optimal role of ASPs in the restriction of non-antimicrobial medications such as tocilizumab and dexamethasone is unknown. Similarly, the ideal role of ASPs in the pre-authorization and distribution of monoclonal antibodies, as well as vaccines, is unclear. Further data will be needed to characterize how ASP resources can best be utilized in a pandemic setting. Such data could be utilized to rationalize the formation or expansion of ASPs as a part of pandemic preparedness. The ultimate impact of the COVID-19 pandemic on ASPs globally remains unknown.
5. Summary
The long-term impact of COVID-19 on antimicrobial stewardship, antimicrobial resistance, and healthcare in general remains largely unknown. Available evidence suggests that rates of bacterial co-infection with COVID-19 are low, but empiric antibiotic use is high, and ASPs will be critical in limiting unnecessary antimicrobial use. ASPs have taken on new roles during the pandemic, such as the creation and maintenance of COVID-19 focused treatment guidelines and the restriction of potential novel therapeutic agents, including some non-antimicrobial agents. ASPs have also had to develop new mechanisms for real-time data review and dissemination. Disparities exist in access to both ASP personnel and program infrastructure that likely are only going to worsen, given the stress on healthcare systems due to the COVID-19 pandemic. Additional research is needed to determine the most optimal ASP program resources and activities by setting, as well as the ultimate impact of the pandemic on critical outcomes such as antimicrobial resistance. Major opportunities exist to bolster programs to both help with ongoing pandemic response efforts and to prepare for future pandemics.
Funding sources
None.
Ethical approval
Not required.
Conflict of interest
None.
References
- Abubakar U, Tangiisuran B. Nationwide survey of pharmacists’ involvement in antimicrobial stewardship programs in Nigerian tertiary hospitals. J Glob Antimicrob Resist. 2020;21:148–153. doi: 10.1016/j.jgar.2019.10.007. [DOI] [PubMed] [Google Scholar]
- Badreldin HA, Atallah B. Global drug shortages due to COVID-19: Impact on patient care and mitigation strategies. Res Soc Adm Pharm. 2021;17:1946–1949. doi: 10.1016/j.sapharm.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandyopadhyay S, Baticulon RE, Kadhum M, Alser M, Ojuka DK, Badereddin Y, et al. Infection and mortality of healthcare workers worldwide from COVID-19: A systematic review. BMJ Glob Heal. 2020;5 doi: 10.1136/bmjgh-2020-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokolo Anthony Jnr. Use of Telemedicine and Virtual Care for Remote Treatment in Response to COVID-19 Pandemic. J Med Syst. 2020;44:132. doi: 10.1007/s10916-020-01596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buehrle DJ, Nguyen MH, Wagener MM, Clancy CJ. Impact of the coronavirus disease 2019 pandemic on outpatient antibiotic prescriptions in the United States. Open Forum Infect Dis. 2020;7:1–4. doi: 10.1093/ofid/ofaa575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Using Telehealth to Expand Access to Essential Health Services during the COVID-19 Pandemic 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html.
- Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MW, McManus D, Koff A, Jaszczur GR, Malinis M. Dela Cruz C, et al. Repurposing antimicrobial stewardship tools in the electronic medical record for the management of COVID-19 patients. Infect Control Hosp Epidemiol. 2020;41:1335–1337. doi: 10.1017/ice.2020.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabre V, Karaba S, Amoah J, Robinson M, Jones G, Dzintars K, et al. The Role of Procalcitonin in Antibiotic Decision-Making in Covid-19 Infection. Infect Control Hosp Epidemiol. 2021:1–24. doi: 10.1017/ice.2021.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gharamti AA, Mei F, Jankousky KC, Huang J, Hyson P, Chastain DB, et al. Diagnostic Utility of a Ferritin-to-Procalcitonin Ratio to Differentiate Patients With COVID-19 From Those With Bacterial Pneumonia: A Multicenter Study. Open Forum Infect Dis. 2021;8:0–1. doi: 10.1093/ofid/ofab124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero-Torres L, Caro-Vega Y, Crabtree-Ramírez B, Sierra-Madero JG. Clinical Characteristics and Mortality of Health-Care Workers With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Mexico City. Clin Infect Dis. 2020;2:199–205. doi: 10.1093/cid/ciaa1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard P, Pulcini C, Levy Hara G, West RM, Gould IM, Harbarth S, et al. An international cross-sectional survey of antimicrobial stewardship programmes in hospitals. J Antimicrob Chemother. 2014;70:1245–1255. doi: 10.1093/jac/dku497. [DOI] [PubMed] [Google Scholar]
- Jones KA, Watson M, Jacob JT, Wiley Z. Antimicrobial stewardship interventions to minimize healthcare worker exposure to SARS-CoV-2. Infect Control Hosp Epidemiol. 2021;42:645–646. doi: 10.1017/ice.2020.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehler P, Bassetti M, Chakrabarti A, Chen SCA, Colombo AL, Hoenigl M, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2021;3099 doi: 10.1016/S1473-3099(20)30847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubin CJ, Loo AS, Cheng J, Nelson B, Mehta M, Mazur S, et al. Antimicrobial stewardship perspectives from a New York City hospital during the COVID-19 pandemic: Challenges and opportunities. Am J Health Syst Pharm. 2021;78:743–750. doi: 10.1093/ajhp/zxaa419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford BJ, So M, Raybardhan S, Leung V, Soucy JPR, Westwood D, et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021;27:520–531. doi: 10.1016/j.cmi.2020.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapolla P, Mingoli A, Lee R. Deaths from COVID-19 in healthcare workers in Italy-What can we learn? Infect Control Hosp Epidemiol. 2021;42:364–365. doi: 10.1017/ice.2020.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liew Y, Lee WHL, Tan L, Kwa ALH, Thien SY, Cherng BPZ, et al. Antimicrobial stewardship programme: a vital resource for hospitals during the global outbreak of coronavirus disease 2019 (COVID-19) Int J Antimicrob Agents. 2020;56 doi: 10.1016/j.ijantimicag.2020.106145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marr KA, Platt A, Tornheim JA, Zhang SX, Datta K, Cardozo C, et al. Aspergillosis Complicating Severe Coronavirus Disease. Emerg Infect Dis. 2021;27:18–25. doi: 10.3201/eid2701.202896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin E, Philbin M, Hughes G, Bergin C, Fe Talento A. Antimicrobial stewardship challenges and innovative initiatives in the acute hospital setting during the COVID-19 pandemic. J Antimicrob Chemother. 2021;76:272–275. doi: 10.1093/JAC/DKAA400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason CY, Kanitkar T, Richardson CJ, Lanzman M, Stone Z, Mahungu T, et al. Exclusion of bacterial co-infection in COVID-19 using baseline inflammatory markers and their response to antibiotics. J Antimicrob Chemother. 2021;76:1323–1331. doi: 10.1093/jac/dkaa563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May M, Chang M, Dietz D, Shoucri S, Laracy J, Sobieszczyk ME, et al. Limited Utility of Procalcitonin in Identifying Community-Associated Bacterial Infections in Patients Presenting with Coronavirus Disease 2019. Antimicrob Agents Chemother. 2021;65:1–5. doi: 10.1128/aac.02167-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazdeyasna H, Nori P, Patel P, Doll M, Godbout E, Lee K, et al. Antimicrobial Stewardship at the Core of COVID-19 Response Efforts: Implications for Sustaining and Building Programs. Curr Infect Dis Rep. 2020;22 doi: 10.1007/s11908-020-00734-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. COVID-19 rapid guideline: managing COVID-19, 2021. https://www.nice.org.uk/guidance/ng191 (accessed July 26, 2021). [PubMed]
- National Institutes of Health. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines 2020:130. https://covid19treatmentguidelines.nih.gov/ (accessed April 2, 2021). [PubMed]
- Nestler M, Godbout E, Lee K, Kim J, Noda AJ, Taylor P, et al. Fungal superinfection in patients with COVID-19: Role of antifungal stewardship? Am J Infect Control. 2021;49:279–280. doi: 10.1016/j.ajic.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nori P, Patel PK, Stevens MP. Rational allocation of COVID-19 vaccines to healthcare personnel and patients: A role for antimicrobial stewardship programs? Infect Control Hosp Epidemiol. 2020 doi: 10.1017/ice.2020.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill J. Tackling drug-resistant infections globally: Final report and recommendations. Rev Antimicrob Resist. 2016:84. [Google Scholar]
- Oldenkamp R, Schultsz C, Mancini E, Cappuccio A. Filling the gaps in the global prevalence map of clinical antimicrobial resistance. Proc Natl Acad Sci U S A. 2021;118 doi: 10.1073/PNAS.2013515118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel PK, Nori P, Stevens MP. Antimicrobial stewardship and bamlanivimab: Opportunities for outpatient preauthorization? Infect Control Hosp Epidemiol. 2020:1–3. doi: 10.1017/ice.2020.1343. [DOI] [PubMed] [Google Scholar]
- Pierce J, Apisarnthanarak A, Schellack N, Cornistein W, Al A, Adnan S, et al. International Journal of Infectious Diseases Global Antimicrobial Stewardship with a Focus on Low- and Middle-Income Countries. Int J Infect Dis. 2020;96:621–629. doi: 10.1016/j.ijid.2020.05.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sastry SR, Pryor R, Raybould JE, Reznicek J, Cooper K, Patrick A, et al. Universal screening for the SARS-CoV-2 virus on hospital admission in an area with low COVID-19 prevalence. Infect Control Hosp Epidemiol. 2020;41:1231–1233. doi: 10.1017/ice.2020.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaton RA, Gibbons CL, Cooper L, Malcolm W, McKinney R, Dundas S, et al. Survey of antibiotic and antifungal prescribing in patients with suspected and confirmed COVID-19 in Scottish hospitals. J Infect. 2020;81:952–960. doi: 10.1016/j.jinf.2020.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifert J, Mueller M, Williamson I, Osterholm MT. The CIDRAP Viewpoint 2020.
- Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab Syndr Clin Res Rev. 2021;15 doi: 10.1016/j.dsx.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens Michael P, Patel PK, Nori P. Involving antimicrobial stewardship programs in COVID-19 response efforts: All hands on deck. Infect Control Hosp Epidemiol. 2020;41:744–745. doi: 10.1017/ice.2020.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens Michael P., Patel PK, Nori P. Antimicrobial Stewardship Programs and Convalescent Plasma for COVID-19: A New Paradigm for Pre-Authorization? Infect Control Hosp Epidemiol. 2020:1–2. doi: 10.1017/ice.2020.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tande AJ, Stevens RW, Wermers RA, Estes LL. Leveraging Existing Strategies of Medication Stewardship to Preserve and Appropriately Use Critical Supplies. Mayo Clin Proc. 2020;95:S29–S32. doi: 10.1016/j.mayocp.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The American Society of Health-System pharmacist. Drug Shortages Statistics 2021. https://www.ashp.org/Drug-Shortages/Shortage-Resources/Drug-Shortages-Statistics?loginreturnUrl=SSOCheckOnl.
- Viswanathan M, Kahwati L, Jahn B, Giger K, Dobrescu AI, Hill C, et al. Universal screening for SARS-CoV-2 infection: a rapid review. Cochrane Database Syst Rev. 2020;2020 doi: 10.1002/14651858.CD013718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Solidarity Trial Consortium Repurposed Antiviral Drugs for Covid-19 — Interim WHO Solidarity Trial Results. N Engl J Med. 2021;384:497–511. doi: 10.1056/nejmoa2023184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams EJ, Mair L, de Silva TI, Green DJ, House P, Cawthron K, et al. Evaluation of procalcitonin as a contribution to antimicrobial stewardship in SARS-CoV-2 infection: a retrospective cohort study. J Hosp Infect. 2021;110:103–107. doi: 10.1016/j.jhin.2021.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. COVID-19 Clinical management Living guidance 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1 (accessed April 2, 2021).
- World Health Organization. Diagnostic testing for SARS-CoV-2 2020a. https://www.who.int/publications/i/item/diagnostic-testing-for-sars-cov-2 (accessed April 2, 2021).
- World Health Organization. Rational use of personal protective equipment for COVID-19 and considerations during severe shortages 2020b:1–32.
- World Health Organization. Global action plan on antimicrobial resistance 2015. https://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/ (accessed April 2, 2021). [DOI] [PubMed]