Abstract
Objective
To identify the risk factors for psychological distress in electroencephalography (EEG) technicians during the coronavirus disease 2019 (COVID-19) pandemic.
Method
In this national-level cross-sectional survey initiated by Japan Young Epilepsy Section (YES-Japan), which is a national chapter of The Young Epilepsy Section of the International League Against Epilepsy (ILAE-YES), a questionnaire was administered to 173 technicians engaged in EEG at four clinics specializing in epilepsy care and 20 hospitals accredited as (quasi-) epilepsy centers or epilepsy training facilities in Japan from March 1 to April 30, 2021. We collected data on participants’ profiles, information about work, and psychological distress outcome measurements, such as the K-6 and Tokyo Metropolitan Distress Scale for Pandemic (TMDP). Linear regression analysis was used to identify the risk factors for psychological distress. Factors that were significantly associated with psychological distress in the univariate analysis were subjected to multivariate analysis.
Results
Among the 142 respondents (response rate: 82%), 128 were included in the final analysis. As many as 35.2% of EEG technicians have been under psychological distress. In multivariate linear regression analysis for K-6, female sex, examination for patients (suspected) with COVID-19, and change in salary or bonus were independent associated factors for psychological distress. Contrastingly, in multivariate linear regression analysis for TMDP, female sex, presence of cohabitants who had to be separated from the respondent due to this pandemic, and change in salary or bonus were independent associated factors for psychological distress.
Conclusion
We successfully identified the risk factors associated with psychological distress in EEG technicians during the COVID-19 pandemic. Our results may help in understanding the psychological stress in EEG technicians during the COVID-19 pandemic and improving the work environment, which is necessary to maintain the mental health of EEG technicians.
Abbreviations: COVID-19, coronavirus disease 2019; EEG, electroencephalography; PPE, personal protective equipment; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2
Keywords: COVID-19, Epilepsy, Technician, Clinical neurophysiology, Stress, EEG
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had a great influence on society worldwide [1]. Medical staff are vulnerable to psychological stress because they are at high risk of exposure to severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), and they see COVID-19 critically ill patients [2], [3], [4].
Clinical neurophysiology staff, like other medical staff, can be exposed to psychological stress due to the impact of COVID-19. The International Federation of Clinical Neurophysiology has described the importance of mental health considerations for clinical neurophysiology staff during a pandemic [5]. Electroencephalography (EEG) is one of the most common clinical neurophysiological examinations, which is helpful in multiple clinical settings, especially for the diagnosis of epilepsy [6]. Electroencephalography technologists could be vulnerable to stress during the COVID-19 pandemic because they are physically closer to the patient when performing EEG tests. In addition, EEG technicians have been warned about hyperventilation activation in EEG during the COVID-19 pandemic due to the risk of exposure to the virus for EEG technicians [7]. Therefore, EEG technicians who perform hyperventilation activation tests may experience high levels of psychological stress.
However, the actual burden on the mental health of EEG technicians has not yet been investigated. We hypothesized that during the COVID-19 pandemic, (1) EEG technicians in Japan have a psychological distress, and if so (2) there are some risk factors associated with it. Therefore, we conducted national-level cross-sectional survey across Japan.
2. Materials and methods
2.1. Survey design and data collection
This study adhered to the principles of the Declaration of Helsinki. The study was registered at each participating hospital/clinic in line with the applicable regulations. The study was approved by the ethical committee (#A201200010) of Yokohama City University, which is the initiating facility. We conducted a cross-sectional survey to achieve our objectives.
After the initial screening of applications from epilepsy centers and clinics throughout Japan by the official email list of the Japanese Epilepsy Society, 20 hospitals and 4 clinics were nominated. Our survey was conducted using Google Forms and sent to 173 clinical neurophysiology technicians who engaged in EEG by email. Details of the participating facilities are provided in Supplementary Fig. S1. The study was conducted from March 1 to April 30, 2021. The questionnaire included an informative letter summarizing the purpose of the research and an informed consent form, which was written briefly and clearly in Japanese to avoid misinterpretation. The questionnaire took 3–5 min to complete. This questionnaire was piloted by 12 volunteers from Japanese medical staff, and its validity was confirmed.
The inclusion criteria were as follows: (1) technicians who engaged in EEG tests at least once within two weeks before answering and (2) technicians who completed all the questions of the survey.
2.2. Questions included in the survey
The questionnaire consisted of three parts. The first part included questions on participants’ profiles, the second part included questions about their work, and the third part examined psychological distress as an outcome measure.
2.3. Participant profile
In the first part of this survey, we asked about participants’ profiles: (a) sex, (b) age category (years, 24, 25–34, 35–44, 45–54, 55–64, ≥65), (c) type of facility (hospital or clinic), (d) whether the facility is located within an endemic area of COVID-19, (e) risk factors in the respondent for COVID-19 infection or stress related to the COVID-19 pandemic, (f) risk factors in the respondent’s cohabitants for COVID-19 infection or stress related to the COVID-19 pandemic [8], (g) presence of cohabitants who had to be separated from the respondent due to this pandemic [9], (h) history of COVID-19 infection in the respondents [10], [11], and (i) vaccination against COVID-19. To incorporate the variable of (d) whether an endemic area of COVID-19 into the analysis, we categorized the location of the facility into two groups (endemic area or non-endemic area) according to the total number of COVID-19-positive cases per population in each prefecture as of February 28, 2021, which is one day prior to starting the survey (Supplementary Fig. S2). Regarding the risk factors for COVID-19 infection or stress related to the COVID-19 pandemic in (e), we defined the risk factors as pregnant [6], [8], breastfeeding [8], living alone [9], over 65 years old [8], medically dependent state [8], smoking [8], obesity (BMI ≥ 30) [8], medical history of diabetes mellitus [8], hypertension [8], chronic heart disease [8], chronic pulmonary disease [8], chronic kidney disease [8], neoplasm [8], or immunocompromised state [8]. Regarding the risk factors in (f), we added the factor cohabitants under 17 years old [12], [13], [14] into the same cohabitant’s risk factors as in (e).
2.4. Work-associated factors
We examined the work-associated factors of the participants; these factors included the following variables: (j) duration per study [7], [15], (k) examination frequency in the last two weeks [15], (l) presence of unscheduled examination [15], [16], (m) type of examination performed (EEG with hyperventilation [7], EEG without hyperventilation [7], EEG monitoring [5], [7], [15]), (n) whether the test was performed on outpatients, inpatients, or both [5], [15], (o) examination for patients with COVID-19 or suspected with COVID-19 within two weeks [15], [17], (p) presence of infection prevention protocols, screening interviews/examinations, guidelines, or agreements regarding examination during the pandemic at the respondent’s facility [5], [7], [15], (q) presence of a counseling/consultation office to talk about mental stress related to the pandemic in the facility [5], (r) availability of personal protective equipment (PPE) [5], [7], [15], [18], (s) change in salary/bonus (decrease, no change, or increase) during the pandemic, including benefits due to work related to COVID-19 [19].
2.5. Outcome measurements of psychological distress
We surveyed the following two outcome measures of psychological distress: the K-6 and Tokyo Metropolitan Distress Scale for Pandemic (TMDP) in the Japanese version [20], [21]. K-6 is an international score used worldwide [20]. K-6 includes a total of six questions regarding personal experiences and feelings within 30 days. The scores range from 0 to 24, with higher scores indicating higher stress [20]. K-6 is not specific to the COVID-19 pandemic; however, many studies have investigated psychological distress during the COVID-19 pandemic using K-6 [22], [23], [24], [25]. On the other hand, TMDP is a scale developed in Japan to assess mental and social stress in medical personnel during the COVID-19 pandemic [21]. The TMDP includes a total of nine questions regarding personal experiences and feelings within two weeks. The score ranged from 0 to 36, with higher scores indicating higher stress. The TMDP is validated as being correlated with PHQ-9 and GAD-7, which are international scores for assessing psychological distress [21]. Both K-6 and TMDP have validated Japanese versions [21], [26].
2.6. Statistical analysis
Statistical analysis was performed using IBM SPSS statistical software version 27 (IBM Corp., Armonk, NY). Multivariate linear regression analysis was used to determine which factors were independently associated with each outcome measurement of psychological distress. Variables that were associated (p < 0.10) with each psychological distress scale using univariate linear regression analysis were incorporated into the multivariate linear regression analysis. A two-sided p-value of 0.05 was considered to be significant in the multivariate linear regression analysis.
2.7. Sensitivity analysis
We conducted a sensitivity analysis to assess the robustness of the results. In the sensitivity analysis, binary logistic regression analysis was used for each psychological distress outcome. The cutoff value of the binary classification in both outcome measurement scales was 5 for K-6 and 14 for TMDP, based on previous reports [21], [26]. Multivariate binary logistic regression analysis was used to determine which variables were independent associated factor with each outcome measurement of psychological distress. Variables that were associated (p < 0.10) with each psychological distress scale using univariate binary logistic regression analysis were incorporated into the multivariate binary logistic regression analysis. A two-sided p-value of 0.05 was considered to be significant in the multivariate binary logistic regression analysis.
3. Results
3.1. Total number of respondents and descriptive analysis
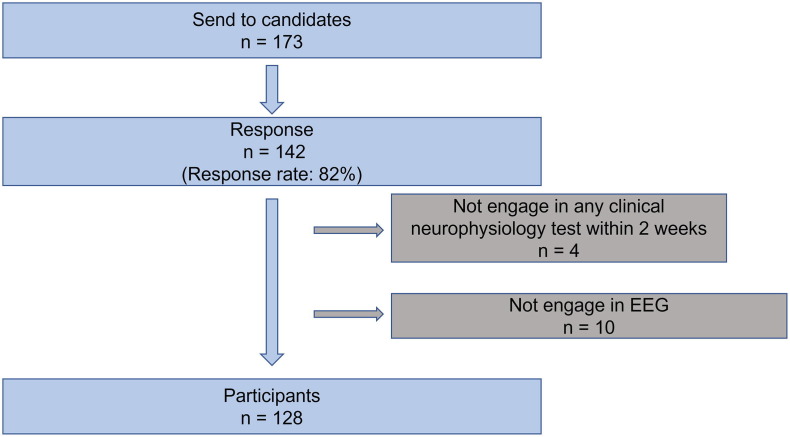
Responses were collected from 142 technicians, giving a response rate of 82% (142/173). Among the 142 respondents, 14 were excluded because they had not engaged in EEG within two weeks before answering. Of the remaining respondents, we included respondents who completed the survey. Finally, 128 responses were used for the analysis (Fig. 1 ).
Fig. 1.
A flowchart showing the participant selection process. After the initial screening of applications from epilepsy centers/clinics throughout Japan according to the official email list of the Japanese Epilepsy Society, 19 hospitals and 4 clinics were nominated. We sent our questionnaire to 173 candidates, of which 142 responded. Among the 142 respondents, 4 were excluded because they had not engaged in any clinical neurophysiology test within 2 weeks. Another 10 respondents were excluded for not engaging in any EEG study. Finally, 128 responses were analyzed of this study. EEG: electroencephalography.
We show the participants’ profiles and the proportion of each answer to every question in Table 1 . The proportion of female patients was 71.1% (91/128). The age group with the highest number of respondents was 25–34 years (52/128: 40.6%). The majority of the participants were working at a hospital (117/128, 91.4%). The number of participants who worked in the endemic area was 99 (77.3%). Importantly, 35.2% of EEG technicians have been under psychological distress based on K-6 and TMDP scores. Then the linear regression analysis was conducted with the association of these scores.
Table 1.
Summary of participants’ profiles.
| Participants (n = 128) | |
|---|---|
| Profile of participants | |
| Sex, No. (%) | Male: 37 (28.9), Female: 91 (71.1) |
| Category of age (years), No. (%) | ≤24, 12 (9.4), |
| 25–34, 52 (40.6), | |
| 35–44, 27 (21.1), | |
| 45–54, 20 (15.6), | |
| 55–64, 13 (10.2), | |
| ≥65, 4 (3.1) | |
| Type of facility, No. (%) | Hospital: 117 (91.4), |
| Clinic: 11 (8.6) | |
| Location of facility, No. (%) | Endemic area: 99 (77.3), |
| Non-endemic area: 29 (22.7) | |
| Risk factors for COVID-19 in the participants, No. (%) | At least one risk factor: 63 (49.2), |
| none: 65 (50.8) | |
| Risk factors for COVID-19 in the participants’ cohabitants, No. (%) | At least one risk factor: 61 (47.7), |
| none: 67 (52.3) | |
| Presence of cohabitants who had to be separated from respondents due to this pandemic, No. (%) | 3 (2.3) |
| History of COVID-19 infection in the respondent, No. (%) | 1 (0.8) |
| Vaccination against COVID-19, No. (%) | Not planned: 30 (23.4), |
| Planned: 71 (55.5), | |
| 1st dose: 24 (18.8), | |
| 2nd dose: 3 (2.3) | |
| Factors related to work | |
| Duration per study, median [IQR] | 60 [40–60] min |
| Examination frequency in the last two weeks, median [IQR] | 20 [10–40 |
| Experience of unexpected tests in two weeks, No. (%) | 87 (68.0) |
| Experience of EEG with hyperventilation in two weeks, No. (%) | 47 (36.7) |
| Experience of EEG monitoring in two weeks, No. (%) | 60 (46.9) |
| Test for outpatient, inpatients, or both, No. (%) | Outpatient: 14 (10.9), |
| inpatient: 11 (8.6), | |
| both 103 (80.5) | |
| Examination for patients with COVID-19 or suspected of having COVID-19, No. (%) | 12 (9.4) |
| Infection prevention protocols, screening interviews/examinations, guidelines, or agreements regarding examination, No. (%) | 121 (94.5) |
| Counseling/consultation office to talk about mental stress related to the pandemic, No. (%) | 89 (69.5) |
| Availability of N95 mask, No. (%) | 35 (27.3) |
| Change in salary/bonus during the pandemic, No. (%) | Down: 17 (13.3), |
| No change: 54 (42.2), | |
| Up: 57 (44.5) | |
| Outcome measurements | |
| K-6 5, No. (%) | 45 (35.2) |
| TMDP 14, No. (%) | 45 (35.2) |
SD: standard deviation; IQR: interquartile range; TMDP: Tokyo Metropolitan Distress Scale for Pandemic; EEG: electroencephalography.
3.2. Univariate and multivariate linear regression analyses for K-6
Table 2 shows the results of the univariate and multivariate linear regression analyses for K-6. The associated factors (p < 0.10) in univariate linear regression analysis with K-6 were female sex (p = 0.014), test for outpatients (p = 0.093), examination for patients (suspected) with COVID-19 (p = 0.036), and change in salary or bonus (p = 0.076). Based on the results of the univariate analysis, multivariate linear regression analysis incorporated the aforementioned variables. Multivariate linear regression analysis identified independent risk factors for high K-6 scores as female (estimate = 1.55; p = 0.031), examination of patients (suspected) with COVID-19 (estimate = 2.45; p = 0.030), and change in salary or bonus (estimate = −1.03; p = 0.030).
Table 2.
Results of univariate and multivariate linear regression analyses based on the outcome of K-6.
| Univariate |
Multivariate |
|||||
|---|---|---|---|---|---|---|
| P-value | Unstandardized Coefficients | 95% C.I. | P-value | Unstandardized Coefficients | 95% C.I. | |
| Sex (male: 0, female: 1) | 0.014 | 1.80 | 0.37 to 3.24 | 0.031 | 1.55 | 0.14 to 2.95 |
| Age: category | 0.148 | −0.38 | −0.90 to 0.14 | |||
| Type of facility (Hospital: 0, Clinic: 1) | 0.669 | −0.51 | −2.89 to 1.86 | |||
| Endemic area | 0.679 | −0.33 | −1.92 to 1.26 | |||
| At least one risk factor in the participant | 0.862 | −0.12 | −1.45 to 1.21 | |||
| At least one risk factor in the cohabitant | 0.554 | 0.40 | −0.93 to 1.73 | |||
| Living apart due to the pandemic | 0.177 | 3.00 | −1.37 to 7.36 | |||
| COVID-19 infectious | 0.845 | −0.75 | −8.30 to 6.81 | |||
| Vaccine (None: 0, At least 1st dose: 1) | 0.209 | −1.03 | −2.66 to 0.59 | |||
| Duration per test (min) | 0.426 | −0.01 | −0.01 to 0.01 | |||
| Test frequency (/2 weeks) | 0.354 | 0.01 | −0.01 to 0.03 | |||
| Unexpected test | 0.943 | 0.05 | −1.37 to 1.48 | |||
| EEG with hyperventilation | 0.919 | 0.07 | −1.31 to 1.45 | |||
| EEG monitoring | 0.443 | 0.52 | −0.81 to 1.85 | |||
| Test for outpatients | 0.093 | 2.01 | −0.34 to 4.35 | 0.189 | 1.52 | −0.76 to 3.80 |
| Examination for patients (suspected) with COVID-19 | 0.036 | 2.40 | 0.16 to 4.64 | 0.030 | 2.45 | 0.24 to 4.66 |
| Protocol or screening | 0.823 | 0.33 | −2.59 to 3.26 | |||
| Counseling/Consultation office | 0.224 | −0.89 | −2.32 to 0.55 | |||
| Availability of N95 mask | 0.639 | 0.36 | −1.14 to 1.85 | |||
| Change in salary or bonus during the COVID-19 pandemic (Down: 0, No change: 1, Up: 2) | 0.076 | −0.86 | −1.80 to 0.09 | 0.030 | −1.03 | −1.95 to −0.10 |
C.I.: confidence interval; EEG: electroencephalography.
P < 0.10 in Univariate analysis and P < 0.05 in multivariate analysis indicated significance (in bold).
3.3. Univariate and multivariate linear regression analyses for TMDP
Table 3 shows the results of the univariate and multivariate linear regression analyses for TMDP. The associated factors (p < 0.10) in the univariate linear regression analysis with TMDP were female sex (p = 0.002), presence of cohabitants who had to be separated from the respondent due to this pandemic (p = 0.088), and changes in salary or bonuses (p < 0.001). Based on the results of the univariate analysis, multivariate linear regression analysis incorporated the aforementioned variables. Multivariate linear regression analysis identified independent risk factors for high TMDP scores as female (estimate = 2.48; p < 0.001), presence of cohabitants who had to be separated from the respondent due to this pandemic (estimate = 4.28; p = 0.041), and change in salary or bonus (estimate = −1.69; p < 0.001).
Table 3.
Results of univariate and multivariate linear regression analyses based on the outcome of TMDP.
| Univariate |
Multivariate |
|||||
|---|---|---|---|---|---|---|
| P-value | Unstandardized Coefficients | 95% C.I. | P-value | Unstandardized Coefficients | 95% C.I. | |
| Sex (male: 0, female: 1) | 0.002 | 2.33 | 0.88 to 3.77 | <0.001 | 2.48 | 1.12 to 3.85 |
| Age: category | 0.126 | 0.42 | −0.12 to 0.95 | |||
| Type of facility (Hospital: 0, Clinic: 1) | 0.252 | 1.40 | −1.01 to 3.82 | |||
| Endemic area | 0.279 | −0.89 | −2.51 to 0.73 | |||
| At least one risk factor in the participant | 0.670 | 0.29 | −1.07 to 1.65 | |||
| At least one risk factor in the cohabitant | 0.108 | 1.10 | −0.25 to 2.45 | |||
| Living apart due to the pandemic | 0.088 | 3.86 | −0.59 to 8.31 | 0.041 | 4.28 | 0.18 to 8.34 |
| COVID-19 infectious | 0.979 | 0.10 | −7.63 to 7.83 | |||
| Vaccine | ||||||
| (None: 0, At least 1st dose: 1) | 0.792 | 0.22 | −1.45 to 1.89 | |||
| Duration per test (min) | 0.688 | −0.001 | −0.01 to 0.01 | |||
| Test frequency (/2 weeks) | 0.192 | −0.01 | −0.04 to 0.01 | |||
| Unexpected test | 0.703 | 0.28 | −1.18 to 1.74 | |||
| EEG with hyperventilation | 0.646 | 0.33 | −1.08 to 1.74 | |||
| EEG monitoring | 0.276 | −0.75 | −2.11 to 0.61 | |||
| Test for outpatients | 0.577 | 0.69 | −1.74 to 3.11 | |||
| Examination for patients (suspected) with COVID-19 | 0.359 | −1.08 | −3.41 to 1.24 | |||
| Protocol or screening | 0.977 | 0.04 | −2.95 to 3.04 | |||
| Counseling/Consultation office | 0.114 | −1.18 | −2.64 to 0.29 | |||
| Availability of N95 mask | 0.177 | −1.04 | −2.56 to 0.48 | |||
| Change in salary or bonus during the COVID-19 pandemic (Down: 0, No change: 1, Up: 2) | < 0.001 | −1.77 | −2.70 to −0.84 | <0.001 | −1.69 | −2.58 to −0.80 |
C.I.: confidence interval; EEG: electroencephalography.
P < 0.10 in Univariate analysis and P < 0.05 in multivariate analysis indicated significance (in bold).
3.4. Sensitivity analysis for K-6 using univariate and multivariate binary logistic regression analyses
Supplementary Table S1 shows the results of univariate and multivariate binary logistic regression analyses for K-6. The associated factors (p < 0.10) in the univariate binary logistic regression analysis with K-6 were female (p = 0.017), at least 1st dose of vaccination against COVID-19 (p = 0.048), and test for outpatients (p = 0.092). Based on the results of the univariate analysis, multivariate binary logistic regression analysis incorporated the aforementioned variables. Multivariate binary logistic regression analysis identified an independent risk factor for K-6 ≥ 5 as an examination for patients suspected of having COVID-19 (odds ratio = 5.91; p = 0.014).
3.5. Sensitivity analysis for TMDP using univariate and multivariate binary logistic regression analyses
Supplementary Table S2 shows the results of the univariate and multivariate binary logistic regression analyses for TMDP. The associated factors (p < 0.10) in the univariate binary logistic regression analysis with TMDP were the presence of cohabitants who had to be separated from the respondent due to this pandemic (p = 0.093), engaging in EEG monitoring (p = 0.061), and changes in salary or bonuses (p = 0.004). Based on the results of the univariate analysis, multivariate binary logistic regression analysis incorporated the aforementioned variables. Multivariate binary logistic regression analysis identified an independent risk factor for TMDP ≥ 14 as a change in salary or bonus (odds ratio = 0.46; p = 0.008).
4. Discussion
4.1. Summary and interpretation of our findings
Performing a national-level cross-sectional survey with a high response rate (82%), we identified risk factors for mental distress in EEG technicians during the COVID-19 pandemic in Japan. Although there have been papers discussing the need for guidelines and staff considerations for clinical neurophysiology testing during the COVID-19 pandemic [5], [7], [15], [16], few research papers have addressed this issue. In this regard, we conducted a study of mental stress specifically among clinical neurophysiology staff on a nationwide scale in Japan, and succeeded in identifying risk factors.
As many as 35.2 % of EEG technicians have been under psychological distress. Furthermore, female sex, examination for patients (suspected) with COVID-19, and change in salary or bonus were risk factors for higher K-6 score in our study. Regarding the examination of patients suspected of having COVID-19, its robustness was confirmed by sensitivity analysis. On the other hand, the analysis for higher TMDP identified factors associated with the presence of cohabitants who had to be separated from respondents due to this pandemic, and changes in salaries or bonuses, as well as females. In addition, the robustness of the change in salary or bonus was confirmed by sensitivity analysis.
The results of this study can help in understanding the psychological stress in EEG technicians during the COVID-19 pandemic. In our study, a decrease in bonus or salary was significantly related to psychological stress. This is an intervenable factor, and it is possible that increasing bonuses and salaries can reduce mental stress. However, the actual effects should be examined by conducting further interventional studies.
4.2. Psychological stress due to the COVID-19 pandemic on medical staff
Various studies have already been conducted on the mental stress of medical staff in COVID-19 situations [27], [28], [29]. Other studies reported that, similar to our findings, female medical staff are more likely to suffer from psychological stress than their male counterparts [9], [30], [31]. Another study reported the psychological stress of providing medical care to patients with COVID-19 or suspected COVID-19, which also supports the findings of this study [17], [31]. This can be interpreted in two ways: 1) the increased risk of COVID-19 infection and 2) stigma due to COVID-19 exposure [32].
In addition, we found that changes in salary/bonus during the pandemic and the presence of cohabitants who had to be separated from respondents due to this pandemic are also independent risk factors for psychological stress. These factors are not specified by the clinical neurophysiology staff. Economic difficulty has been reported as a risk factor for psychological distress in a previous study [9].
Under the COVID-19 pandemic, the guideline recommends that EEG testing with hyperventilation activation should be avoided as much as possible [7]. This is because hyperventilation could expose the EEG technician to SARS-CoV-2 from an infected patient. Based on this recommendation, we hypothesized that EEG with hyperventilation is a risk factor for psychological distress in technicians. However, engaging in EEG tests with hyperventilation was not significantly associated with psychological distress among technicians. The reasons for this were considered to be as follows: (1) hyperventilation activation in EEG testing is performed only for limited patients during a short period of time, (2) only two people, including themselves, are in the room at a time, and (3) EEG technicians can reduce the risk of infection by using PPE. However, it should be noted that the risk of COVID-19 transmission by EEG with hyperventilation was not assessed in this study. Until the risk is investigated, clinicians still need to consider not ordering unnecessary hyperventilation activation tests, as warnings have been issued [7].
4.3. Methodological considerations
Although various measures of mental stress during the COVID-19 pandemic have been reported [33], we measured K-6 and TMDP in this study. K-6 is simple and has been reported to be useful in various studies worldwide. It has been used in studies assessing mental stress during the COVID-19 pandemic [22], [23], [24], [25]. Another strength of K-6 is that the Japanese version has been validated in a previous study [26]. In contrast, TMDP is a new measure developed in 2020 [21], and it is not widely used around the world at this time. However, one of the strengths of the TMDP, as opposed to the K-6, is that it is a scale specifically designed to measure stress in medical personnel during the COVID-19 pandemic. Another strength of the TMDP is that this scale was developed in Japan. Considering these two strengths, the TMDP was considered to be the most specific and appropriate scale for measuring psychological stress among medical professionals in Japan during the COVID-19 pandemic.
Our study has some limitations. First, this cross-sectional questionnaire survey retrospectively captured subjects’ experiences and perceptions at only one point in time. Thus, recall bias was unavoidable. Second, there was no control or baseline psychological status. Ideally, similar outcome measurements should be taken before the COVID-19 pandemic and its quantitative comparison before and during the COVID-19 pandemic should be made using the same outcome measurement. However, because the COVID-19 pandemic was unpredictable, quantitative measurements could not be made before the COVID-19 pandemic. For this reason, our study design had to be a cross-sectional survey, which could not determine the causality between associated factors and outcomes. The third limitation is that we did not collect the variables such as pre-existing psychological comorbidities or psychotropic medications, which would affect the outcomes of this study. The last limitation is the generalizability. In this study, we focused on clinical neurophysiology staff engaged in EEG in Japan. The impact of COVID-19 and its effects on mental health varies across countries. Future research should consider the applicability of these results to other countries. Although our primary aim was to investigate the potential risk factors in EEG technicians who play an essential role in epilepsy clinics, another applicability should be considered for clinical neurophysiology staff not limited to EEG in further studies.
5. Conclusions
We successfully identified the risk factors associated with psychological distress in EEG technicians during the COVID-19 pandemic by performing a national-level cross-sectional survey in Japan with a high response rate. The results of this study may help understanding the psychological stress in EEG technicians during the COVID-19 pandemic. Our results would also help in improving the work environment, which is necessary to maintain the mental health of EEG technicians.
Declarations of competing interests
None.
Acknowledgments
Acknowledgments
The authors are grateful to Dr. Eishi Asano at the Children’s Hospital of Michigan, Detroit Medical Center, Wayne State University, for his advice on the statistical analysis. The authors are also grateful to all the participants of this survey-based study.
Funding
This work was supported by JSPS KAKENHI (Grant Number 19K18435).
Conflict of interest statement
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.yebeh.2021.108361.
Contributor Information
IMPACT-J EPILEPSY (In-depth Multicenter analysis during Pandemic of Covid19 Throughout Japan for Epilepsy practice) study group:
Kousuke Kanemoto, Akio Ikeda, Kiyohito Terada, Hiroko Goji, Shinji Ohara, Koichi Hagiwara, Takashi Kamada, Koji Iida, Nobutsune Ishikawa, Hideaki Shiraishi, Osato Iwata, Hidenori Sugano, Yasushi Iimura, Takuichiro Higashi, Hiroshi Hosoyama, Ryosuke Hanaya, Akihiro Shimotake, Takayuki Kikuchi, Takeshi Yoshida, Hiroshi Shigeto, Jun Yokoyama, Takahiko Mukaino, Masaaki Kato, Masanori Sekimoto, Masahiro Mizobuchi, Yoko Aburakawa, Masaki Iwasaki, Eiji Nakagawa, Tomohiro Iwata, Kentaro Tokumoto, Takuji Nishida, Yukitoshi Takahashi, Kenjiro Kikuchi, Ryuki Matsuura, Shin-ichiro Hamano, Hideo Yamanouchi, Satsuki Watanabe, Ayataka Fujimoto, Hideo Enoki, Kyoichi Tomoto, Masako Watanabe, Youji Takubo, Toshihiko Fukuchi, Hidetoshi Nakamoto, Yuichi Kubota, Naoto Kunii, Yuichiro Shirota, Eiichi Ishikawa, Nobukazu Nakasato, Taketoshi Maehara, Motoki Inaji, Shunsuke Takagi, Takashi Enokizono, Yosuke Masuda, and Takahiro Hayashi
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368 doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 4.Gold J.A. Covid-19: Adverse mental health outcomes for healthcare workers. BMJ. 2020;369 doi: 10.1136/bmj.m1815. [DOI] [PubMed] [Google Scholar]
- 5.San-Juan D., Jiménez C.R., Camilli C.X., de la Cruz Reyes L.A., Galindo E.G.A., Burbano G.E.R., et al. Guidance for clinical neurophysiology examination throughout the COVID-19 pandemic. Latin American chapter of the IFCN task force - COVID-19. Clin Neurophysiol. 2020;131(7):1589–1598. doi: 10.1016/j.clinph.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noachtar S., Rémi J. The role of EEG in epilepsy: a critical review. Epilepsy Behav. 2009;15(1):22–33. doi: 10.1016/j.yebeh.2009.02.035. [DOI] [PubMed] [Google Scholar]
- 7.Canadian Society of Clinical Neurophysiologists (CSCN), Canadian Association of Electroneurophysiology Technologists (CAET), Association of Electromyography Technologists of Canada (AETC), Board of Registration of Electromyography Technologists of Canada (BRETC), Canadian Board of Registration of Electroencephalograph Technologists (CBRET), et al. Practice guidelines for Canadian Neurophysiology Laboratories during the COVID-19 pandemic. Can J Neurol Sci. 2021;48(1):25–30. doi: 10.1017/cjn.2020.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Center for Disease Control and Prevention. Underlying medical conditions associated with high risk for severe COVID-19: Information for healthcare providers, https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html;2021. [PubMed]
- 9.Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. 2020;291:113190. doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Magnavita N., Tripepi G., Di Prinzio R.R. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. Int J Environ Res Public Health. 2020;17(14):5218. doi: 10.3390/ijerph17145218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang X., Zhang Y., Li S., Chen X. Risk factors for anxiety of otolaryngology healthcare workers in Hubei Province fighting coronavirus disease 2019 (COVID-19) Soc Psychiatry Psychiatr Epidemiol. 2021;56(1):39–45. doi: 10.1007/s00127-020-01928-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cluver L., Lachman J.M., Sherr L., Wessels I., Krug E., Rakotomalala S., et al. Parenting in a time of COVID-19. Lancet. 2020;395(10231):e64. doi: 10.1016/S0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang S., Xiang M., Cheung T., Xiang Y.T. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent–child discussion. J Affect Disord. 2021;279:353–360. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halvorsen E., Stamu-O’Brien C., Carniciu S., Jafferany M. Psychological effects of COVID-19 on parenting and maternal-fetal mental health. Dermatol Ther. 2020;33(4):e13579. doi: 10.1111/dth.13579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grippo A., Assenza G., Scarpino M., Broglia L., Cilea R., Galimberti C.A., et al. Electroencephalography during SARS-CoV-2 outbreak: practical recommendations from the task force of the Italian Society of Neurophysiology (SINC), the Italian League Against Epilepsy (LICE), and the Italian Association of Neurophysiology Technologists (AITN) Neurol Sci. 2020;41(9):2345–2351. doi: 10.1007/s10072-020-04585-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krysl D., Beniczky S., Franceschetti S., Arzimanoglou A. The COVID-19 outbreak and approaches to performing EEG in Europe. Epileptic Disord. 2020;22(5):548–554. doi: 10.1684/epd.2020.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alshekaili M., Hassan W., Al Said N., Al Sulaimani F., Jayapal S.K., Al-Mawali A., et al. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ Open. 2020;10(10):e042030. doi: 10.1136/bmjopen-2020-042030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arnetz J.E., Goetz C.M., Sudan S., Arble E., Janisse J., Arnetz B.B. Personal protective equipment and mental health symptoms among nurses during the COVID-19 pandemic. J Occup Environ Med. 2020;62(11):892–897. doi: 10.1097/JOM.0000000000001999. [DOI] [PubMed] [Google Scholar]
- 19.Fonseca E., Quintana M., Lallana S., Luis Restrepo J., Abraira L., Santamarina E., et al. Epilepsy in time of COVID-19: a survey-based study. Acta Neurol Scand. 2020;142(6):545–554. doi: 10.1111/ane.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L., et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 21.Shiwaku H., Doi S., Miyajima M., Matsumoto Y., Fujino J., Hirai N., et al. Novel brief screening scale, Tokyo Metropolitan Distress Scale for Pandemic (TMDP), for assessing mental and social stress of medical personnel in COVID-19 pandemic. Psychiatry Clin Neurosci. 2021;75(1):24–25. doi: 10.1111/pcn.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hao X., Zhou D., Li Z., Zeng G., Hao N., Li E., et al. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia. 2020;61(6):1166–1173. doi: 10.1111/epi.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma M., Fang J., Li C., Bao J., Zhang Y., Chen N., et al. The status and high-risk factors of severe psychological distress in migraine patients during nCOV-2019 outbreak in Southwest China: a cross-sectional study. J Headache Pain. 2020;21(1) doi: 10.1186/s10194-020-01168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graf-Vlachy L., Sun S., Zhang S.X. Predictors of managers’ mental health during the COVID-19 pandemic. Eur J Psychotraumatol. 2020;11(1):1834195. doi: 10.1080/20008198.2020.1834195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neshige S., Aoki S., Shishido T., Morino H., Iida K., Maruyama H. Socio-economic impact on epilepsy outside of the nation-wide COVID-19 pandemic area. Epilepsy Behav. 2021;117:107886. doi: 10.1016/j.yebeh.2021.107886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sakurai K., Nishi A., Kondo K., Yanagida K., Kawakami N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin Neurosci. 2011;65(5):434–441. doi: 10.1111/j.1440-1819.2011.02236.x. [DOI] [PubMed] [Google Scholar]
- 27.Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S.Ø., et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 2020;293:113441. doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giorgi G., Lecca L.I., Alessio F., Finstad G.L., Bondanini G., Lulli L.G., et al. COVID-19-Related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. 2020;17(21):7857. doi: 10.3390/ijerph17217857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lamb D, Gnanapragasam S, Greenberg N, Bhundia R, Carr E, Hotopf M, et al. Psychosocial impact of the COVID-19 pandemic on 4378 UK healthcare workers and ancillary staff: Initial baseline data from a cohort study collected during the first wave of the pandemic. Occup Environ Med 2021:oemed-2020-107276. doi: 10.1136/oemed-2020-107276. [DOI] [PMC free article] [PubMed]
- 31.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus Disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schubert M., Ludwig J., Freiberg A., Hahne T.M., Romero Starke K., Girbig M., et al. Stigmatization from work-related COVID-19 exposure: a systematic review with meta-analysis. Int J Environ Res Public Health. 2021;18(12):6183. doi: 10.3390/ijerph18126183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cortez P.A., Joseph S.J., Das N., Bhandari S.S., Shoib S. Tools to measure the psychological impact of the COVID-19 pandemic: What do we have in the platter? Asian J Psychiatr. 2020;53:102371. doi: 10.1016/j.ajp.2020.102371. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.