Abstract
Background & aims
The study aimed to evaluate emotional eating tendency of Turkish individuals during COVID-19 pandemic.
Methods
The study comprised an online questionnaire and it was conducted from August to September 2020. The survey was distributed through social networks.
Results
A total of 1626 adults have been included in the study, aged between 18 and 65 years (69.6% females and 30.4% males). The average BMI of all participants was 24.4 ± 4.7 kg/m2, 6% were underweight, and 11.6% were obese. A total of 32.7% of the participants had an increase in appetite and 34.4% had a weight gain. It was found that most of the participants (75.7%) were emotional eaters at different levels. Emotional eating was more common in obese people (43.5%) than normal weight (33.5%) and underweight (18.4%) people. It was examined the increasing food intake according to the BMI, the obese increased the consumption of fresh vegetables, fruits, pastries, and, eggs; underweight increased the consumption of fresh vegetables and fruits, milk and, eggs. As in other countries, a weight gain was observed in the individuals. However, the participants resorted to emotional eating to cope with negative emotions such as depression, anxiety, and stress caused by the pandemic.
Conclusions
In this study, it has been provided preliminary data that can be used in future studies to determine the emotional eating behaviors during the COVID-19 pandemic.
Keywords: Nutrition, Body mass index, COVID-19, Emotional eating, Eating habits
Abbreviations: BMI, Body mass index; EES, Emotional Eating Scale; WHO, World Health Organization
1. Introduction
COVID-19 has been declared as a global health emergency on the 30th January 2020 by the WHO Emergency Committee [1]. The first case of COVID-19 in Turkey was reported on 11th March 2020, and then the number of cases increased rapidly. On the 3rd July 2021, a total of 5.440.368 cases and 49.874 deaths were reported in Turkey [2]. As a result of the increasing number of cases, during weekends and public holidays, bans were imposed for leaving the house; the ban was imposed for a maximum of four consecutive days.
Due to the measures of COVID-19, a drastic change has occurred in the lifestyles and habits of the individuals. Self-isolation and lockdown on some days strongly impacted both economic and psychological aspects, in particular affecting eating habits [3].
Limited access to daily grocery shopping has led to reduce the consumption of fresh fruit and vegetables and increased the highly processed food with long shelf life. The change of work and daily routine has caused more time to spend at home and boredom, this leads to an increase in energy intake [4]. In addition, the loss of a dearest person, the fear of the disease, and death due to COVID-19 could increase the stress level. Stress leads subjects to increase energy intake, particularly ‘comfort foods’ rich in sugar, referred as “food craving” [5,6]. Simple carbohydrates contain of these foods are high. The consumption of these foods increases the production of serotonin and have a positive effect on mood [7]. However, glycemic index levels are higher than other foods, therefore they are associated with the increased risk of cardiovascular diseases, obesity, and chronic inflammation. In particular, studies have shown that a chronic state of inflammation worsens COVID-19 complications [8,9]. Furthermore, emotional and psychological responses to the COVID-19 could lead to dysfunctional eating behaviors [10,11]. Previous studies reported that negative emotions increase the risk of emotional eating behavior [12,13]. Emotional eating is defined as overeating after stress and negative emotions [14]. People tend to eat as a mechanism to cope with mood changes [15]. During this period, the consumption of foods with a short shelf life such as fresh vegetables, fruits, meat, chicken, and fish are decreased; instead, the consumption of highly processed food with long life rich in high in fat, sugar and salt are increased [16,17].
Lifestyle and eating habit changes may lead to a considerable problem for public health. Maintaining a healthy diet is crucial, especially during the COVID-19 pandemic, to support and improve the immune system. Previously, emotional eating behavior has not been searched in a large Turkish individuals during the COVID-19 pandemic. Therefore, the aim of the study was to evaluate the emotional eating behavior during the COVID-19 pandemic in Turkey.
2. Material and methods
2.1. Study design and individuals
This cross-sectional study was planned to evaluate eating habits and lifestyle changes in Turkey during the COVID-19 pandemic. The study was carried out online and the data was obtained with a web-survey. The survey, accessible through any device with an internet connection, was conducted from August to September 2020 among the Turkish individuals aged between 18 and 65 years. Individuals under the age of 18 and pregnant women were excluded. The survey was distributed through email and social networks (Twitter, Instagram, Whatsapp, and Facebook). Participants completed the questionnaire by connecting directly to the Google platform. To determinate the sample size of the research a table called “predicts the rate in a society with a certain accuracy” was used [18]. The ratio (48.6%) reported by Di Renzo et al. was used as an indication (weight gain rate) of the prevalence of the population [19]. The sample size was determined as minimum 1067 people, taking into account the 95% confidence interval and 3% relative precision.
Before the research, the required permission was obtained from the “T.C. Ministry of Health COVID-19 Scientific Research Assessment Commission”. After that, the ethical approval was obtained from Necmettin Erbakan University Health Sciences Scientific Research Ethics Board (decision number 2020/1, 26 August 2020). The study was conducted in accordance with the principle of the Declaration of Helsinki. Online informed consent form was obtained from all participants.
2.2. Sociodemographic, anthropometric characteristics and eating habits
The questionnaire included sociodemographic characteristics, body weight, and height. Moreover, the questionnaire included hours of sleep, physical activity, appetite, changes in body weight, and work life before and after the COVID-19 pandemic.
The changes in eating habits were analyzed; foods related to stress in previous studies (fresh fruit, fresh vegetables, pastry, pasta-rice, bread, dessert, eggs, red meat, poultry, fish, milk, biscuits, chocolate, ice cream, chips) were selected and it was asked if there had been an increase or a reduction in their consumption.
2.3. Emotional Eating Scale
This scale was used to determine emotional eating during the COVID-19 pandemic in Turkey individuals. Emotional Eating Scale (EES) was developed by Garaulet et al. They applied this original scale to obese individuals to evaluate emotional eating behaviors [20]. The emotional eating scale consists of 10 sections and three subscales (disinhibition, type of food, and guilt). The questions are given on a likert type scale with four options (“0” Never, “1” Sometimes, “2” Usually, and “3” Always). There is no reverse item in the scale. In the scale, the lowest total score is “0” and the highest total score is “30”. High scores on the scale showed a high level of emotional eating behavior. According to Garaulet et al. scale, a score between 0 and 5 is equal to “non-emotional eater”, a score between 6 and 10 is equal to “low emotional eater”, a score between 11 and 20 is equivalent to “emotional eater” and a score between 21 and 30 is equal to “very emotional eater”. The validity and reliability of the scale in Turkish was conducted by Arslantaş et al. [21]. Similar to the original scale, the Turkish version also shows three subscales: disinhibition, type of food, and guilt. For the use of the Emotional Eating Scale was obtained the permission from Dr. Arslantaş.
2.4. Statistical analyses
Quantitative data were presented as average, standard deviation, minimum, and maximum values; the number and percentage tables of qualitative data were presented. Mann–Whitney U and Kruskal–Wallis tests were used to compare continuous variables between two or more groups. Binary and multinomial logistic regression analyses were conducted to analyze the association between categorical variables (dependent) and continuous or categorical ones (independent) [22]. These tests were used to compare the WHO groups to the body mass index (BMI) groups and to compare BMI groups and eating habits. Statistical analysis was performed using SPSS (Statistical Package for Social Sciences) for Windows ver. 21.0 (IBM, Chicago, IL, USA). The p value < 0.05 was considered to be statistically significant.
3. Results
3.1. Demographic and anthropometric characteristics
A total of 1626 adults, 69.6% women and 30.4% men, were included in the study. Participants’ demographic and anthropometric characteristics are reported in Table 1 . The majority of the participants group aged between 18 and 30 years (48.3%). The average BMI of all participants was 24.4 ± 4.7 kg/m2 and 53.3% were normal weight, 6% were underweight, 29.2% were overweight and 11.6% were obese. In terms of disease, 7.6% of participants had a chronic disease diagnosed by the physician and 8.2% of participants had COVID-19 diagnosis.
Table 1.
Participants’ demographic and anthropometric characteristics.
| n | % | |
|---|---|---|
| Gender | ||
| Female | 1131 | 69.6 |
| Male | 495 | 30.4 |
| Age (years) | Mean ± SD 30 ± 11 |
Min-Max 18–64 |
| Age groups (years) | ||
| 18-25 | 786 | 48.3 |
| 26-35 | 444 | 27.3 |
| 36-45 | 177 | 10.9 |
| >45 | 219 | 13.5 |
| Marital status | ||
| Married | 714 | 43.9 |
| Single | 912 | 56.1 |
| Educational status | ||
| Illiterate | 6 | 0.4 |
| Literate | 28 | 1.7 |
| Primary school graduate | 110 | 6.8 |
| Secondary school graduate | 52 | 3.2 |
| High school graduate | 524 | 32.2 |
| University graduate | 747 | 45.9 |
| Postgraduate | 159 | 9.8 |
| Weight (kg) | Mean ± SD 68.0 ± 15.0 |
Min-Max 37–140 |
| BMI (kg/m2) | Mean ± SD 24.4 ± 4.7 |
Min-Max 15–50 |
| Class of BMI | ||
| Underweight | 98 | 6.0 |
| Normal weight | 866 | 53.3 |
| Overweight | 473 | 29.1 |
| Obesity | 189 | 11.6 |
| Live location | ||
| City | 1126 | 69.2 |
| County | 402 | 24.7 |
| Village | 98 | 6.0 |
| Disease diagnosed by the physician | ||
| Yes | 123 | 7.6 |
| No | 1503 | 92.4 |
| COVID-19 diagnosis status | ||
| Yes | 132 | 8.2 |
| No | 1472 | 91.8 |
BMI: Body mass index.
According to educational status and location, most of the participants lived in a city (69.2%) and almost half (45.9%) had a university degree (Table 1).
3.2. Emotional eating behaviors
According to Emotional Eating scale, 36.9% of the participants were low emotional eaters, 34.8% were emotional eaters, 24.3% were non-emotional eaters and only 4% of participants were very emotional eaters. The obese ones were 43.5% emotional eaters and 30.6% low emotional eaters. 33.5% of the normal body weight and 18.4% of underweight people were emotional eaters. The Kruskal–Wallis test showed a statistically significant association between Emotional Eating score and BMI values (p < 0.001) (Table 2 ).
Table 2.
Association between Emotional Eating score and BMI.
| Emotional Eating Behaviora | Class of BMI |
Total |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Underweight |
Normal weight |
Overweight |
Obesity |
|||||||
| n | % | n | % | n | % | n | % | n | % | |
| Non-emotional eater | 38 | 38.8 | 223 | 25.8 | 107 | 22.7 | 26 | 14.0 | 394 | 24.3 |
| Low emotional eater | 42 | 42.9 | 325 | 37.6 | 173 | 36.7 | 57 | 30.6 | 597 | 36.9 |
| Emotional eater | 18 | 18.4 | 290 | 33.5 | 175 | 37.2 | 81 | 43.5 | 564 | 34.8 |
| Very emotional eater | 0 | 0.0 | 27 | 3.1 | 16 | 3.4 | 22 | 11.8 | 65 | 4.0 |
KW; p < 0,001 BMI: Body mass index.
The EES total score of the participants was 9.58 ± 5.46. Notably, the association between EES score and BMI values showed that obese subjects had the highest score.
Furthermore, females had a higher EES score than males and the difference was statistically significant (p < 0.001) (Table 3 ).
Table 3.
Association between EES score and BMI, and between EES score and Gender.
| BMI Class |
Total |
||||
|---|---|---|---|---|---|
| Underweight |
Normal weight |
Overweight |
Obesity |
||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Total score | 6.98 ± 3.75 | 9.27 ± 5.28 | 9.77 ± 5.48 | 11.89 ± 6.16 | 9.58 ± 5.46 |
| Gendera | Female 10.23 ± 5.48 |
Male 8.10 ± 5.12 |
|||
MWU, p < 0,001. BMI: Body mass index, EES: Emotional eating score.
3.3. Eating habits
With regard to eating habits, a total of 49.9% participants did not change eating habits during the COVID-19 pandemic. During COVID-19 emergency, 28.0% of adults reported a more balanced and healthy diet, on the other hand, 22.1% of adults reported a more unbalanced and unhealthy diet. There was a statistically significant difference in the change of eating habits according to BMI values (KW; p < 0.005). Underweight and normal weight participants followed a healthier diet (30.6% and 30.9%; respectively); overweight and obese ones followed an unhealthier diet (Table 2). Moreover, 78.7% of subjects reported an increased food intake and 49.6% of subjects reported a decreased food intake during the COVID-19 pandemic. There was no statistically significant difference between the change in eating habits and food intake according to BMI values (p = 0.097; p = 0.053, respectively) (Table 4 ).
Table 4.
Change in eating habits and food intake according to BMI.
| Total |
Underweight |
Normal weight |
Overweight |
Obesity |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| Eating habits changesa | ||||||||||
| No | 810 | 49.9 | 45 | 45.9 | 410 | 47.5 | 266 | 56.2 | 89 | 47.1 |
| More unbalanced and unhealthy diet | 359 | 22.1 | 23 | 23.5 | 187 | 21.6 | 100 | 21.1 | 49 | 25.9 |
| More balanced and healthy diet | 455 | 28.0 | 30 | 30.6 | 267 | 30.9 | 107 | 22.6 | 51 | 27.0 |
| Increased food intakeb | ||||||||||
| Yes | 1280 | 78.7 | 75 | 76.5 | 702 | 81.1 | 357 | 75.5 | 146 | 77.2 |
| No | 346 | 21.3 | 23 | 23.5 | 164 | 18.9 | 116 | 24.5 | 43 | 22.8 |
| Reduced food intakec | ||||||||||
| Yes | 806 | 49.6 | 49 | 50.0 | 445 | 51.4 | 210 | 44.4 | 102 | 54.0 |
| No | 820 | 50.4 | 49 | 50.0 | 421 | 48.6 | 263 | 55.6 | 87 | 46.0 |
KW; p = 0,005.
KW; p = 0,097.
KW; p = 0,053. BMI: Body mass index.
During this pandemic, 58.6% of the individuals started to work at home or distance learning at home. Before the COVID-19 pandemic, the majority of individuals (62.2%) slept 7–9 h, whereas with the COVID-19 33.1% of participants increased sleep hours and 9.7% decreased sleep hours. Furthermore, 39.5% of the participants had regular physical activity before COVID-19, whereas 26.1% of participants maintained their physical activity. During the COVID-19 pandemic, a total of 55.1% of the participants had no change in appetite, 32.7% of the participants had an increase in appetite, and 12.2% had less appetite. Concerning the body weight, 34.4% of the individuals had a weight gain in this period and 20% had a lose weight. The mean of body weight gain and lose was 4.4 ± 2.9 and 4.4 ± 3.7 kg, respectively (Table 5 ). There was a weak inverse correlation between emotional eating score with weight gain (p < 0.01, r = 0.165).
Table 5.
Assessment of lifestyle and body weight changes during the COVID-19 pandemic.
| n | % | |
|---|---|---|
| Changed work/school habitsa | ||
| I work at home distance learning at home | 816 | 58.6 |
| Some days of the week I work at home and some days I go to the work. | 166 | 12.0 |
| I go to the work as usual | 381 | 27.4 |
| I got fired/I quit the job | 28 | 2.0 |
| Sleep habits pre-COVID-19 | ||
| <7 h/night | 553 | 34.0 |
| 7–9 h/night | 1010 | 62.2 |
| >9 h/night | 62 | 3.8 |
| Changed sleep habits during COVID-19 | ||
| No difference | 929 | 57.2 |
| Increased sleep hours | 538 | 33.1 |
| Decreased sleep hours | 158 | 9.7 |
| Sport habits pre-COVID-19 | ||
| Yes | 643 | 39.5 |
| No | 983 | 60.5 |
| Sport habits during COVID-19 | ||
| Yes | 424 | 26.1 |
| No | 1202 | 73.9 |
| Changed appetite during COVID-19 | ||
| No difference | 896 | 55.1 |
| More appetite | 532 | 32.7 |
| Less appetite | 198 | 12.2 |
| Body weight changes | ||
| No difference | 739 | 45.6 |
| Body weight gain | 560 | 34.4 |
| Body weight loss | 325 | 20.0 |
| Body weight gain (kg) | Mean ± SD 4.4 ± 2.9 |
Min-Max 0–25 |
| Body weight loss (kg) | Mean ± SD 4.4 ± 3.7 |
Min-Max 0–23 |
Housewives are not included.
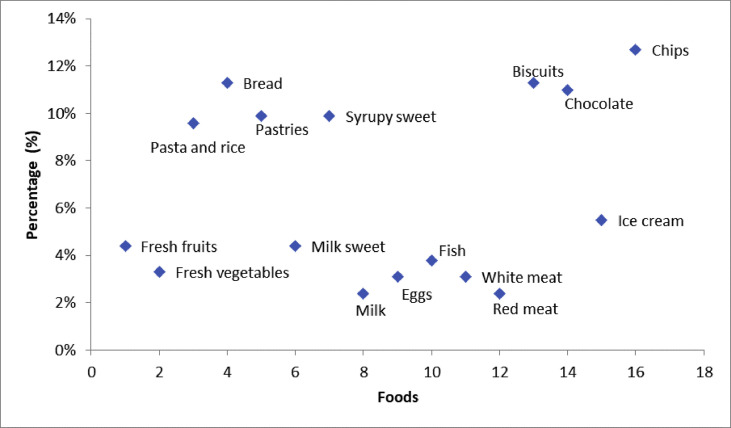
Considering the food consumption, the highest increase was reported in the consumption of fresh fruits and vegetables (44.2% and 31.4%; respectively); the highest decrease was observed in the consumption of chips, biscuits, and bread (12.7%, 11.3% and 11.3%; respectively) (Fig. 1, Fig. 2 ).
Fig. 1.
Increased consumption of food and food groups during the COVID-19 emergency.
Fig. 2.
Decreased consumption of food and food groups during the COVID-19 emergency.
Moreover, increased food intake according to BMI values showed that the obese participants increased the consumption of fresh vegetables and fruits, pastries, and eggs. On the other hand, underweight ones increased their consumption of fresh vegetables and fruits, milk, and eggs (Fig. 3 ).
Fig. 3.
Increased consumption of food and food groups (%) according to BMI.
4. Discussion
The study was conducted to evaluate emotional eating behavior with a large participation of Turkish individuals during the COVID-19 pandemic. The results of the study do not reflect the Turkish population, as online data were collected due to COVID-19. The results of the study should be supported by studies representing Turkish population.
Emotional eating disorders has spread during this period, because it regulates and reduces negative emotions such as depression, anxiety, and stress caused by the pandemic [23]. The majority of the individuals (75.7%) were emotional eating of different levels, only 24.3% were non-emotional eaters. The restrictions of individual freedom, loss of jobs, loss of a dearest person, alteration of habitual behaviors, fear of the disease due to COVID-19 increase the stress level and this influences emotional eating behavior [24]. Furthermore, prolonged containment measures make difficult to maintain a healthy lifestyle, because changes in physical activity, sleep habits, psychology, and eating habits [25,26]. Lifestyle changes, such as sleep habits or physical activity, can trigger emotional eating disorders [27,28]. Several studies have confirmed that stress or anxiety can affect emotional eating disorders [29,30]. Tan and Chow [30] determined that high levels of stress alters the control of eating behaviors and this is directly related to emotional eating. In addition, Hearon et al. [31] reported that anxiety and emotional eating are related, and people eat to cope with anxiety. In another study, high body mass index and low weight control are related to more frequent emotional eating behaviors [32]. Supporting the results of this study, Adrianne et al. [33] determined that the obese have more emotional eating behaviors. Lazarevich et al. [34] found a correlation without gender difference between BMI in1453 university students and emotional eating. Similarly, this study reported that obese individuals have higher emotional eating scores (11.89 ± 6.16) (Table 3).
According to this study, the emotional eating score of women was higher than men (10.23 ± 5.48 and 8.10 ± 5.12, respectively). However, in a study conducted on college students, stress affected eating behavior in both male and female individuals, but men eat less in the event of stress than women [29]. Other studies supported that women show more emotional eating behaviors than men [35,36].
In this study, 78.7% of the individuals reported an increase in food intake. Studies show that staying home for an extended period increased food intake because of an easier and free access to food. These results support this study.
However, the change in the metabolic cycle pattern, alterations of time-limited diet, increases the risk of dysmetabolism and obesity [37]. Although during quarantine obese and overweight tend to increase food intake [38], this study reported a higher increase of food intake in participants with normal BMI (81.1%). On the contrary, a total of 77.2% of obese increase their food intake. In addition, the obese individuals had the highest decrease in food intake (54.0%).
This can be associated with obese individuals' hesitation or lack of awareness of the actual food intake. Moreover, studies reported that 70% of obese indicate levels of food intake that do not make a physiological sense [39].
The COVID-19 pandemic has led to behavioral, psychosocial, and environmental changes in almost all societies and has brought a rapid weight gain. Khan and Smith [40] call this situation “covibesity”. According to results of the study, 34.4% of participants gained weight (4.4 ± 2.9 kg) during the pandemic. Similarly, during this period in Poland a total %30 of the population (n = 1097) gained weight (3.0 ± 1.6 kg), and in Chile 38.1% of women and 25.6% of men (n = 750) gained weight [10,11]. In Italy, 48.6% of participants (n = 3533) gained weight [19]. During the COVID-19 pandemic, weight gain is due to decrease in the frequency and duration of physical activity [11,41]. However, Italian population had no significant change in physical activity habits during the lockdown, but 34.4% of the population reported an increased appetite [19]. In this study, 32.7% of participants reported an increase in their appetite. Before the COVID-19 emergency, 39.5% of subjects regularly did physical activity, but during this period it decreased to 26.1%. In particular, these two factors may have caused a weight gain.
Obese and overweight reported an unhealthier and unbalanced diet during this period, similar to subjects that expressed a healthier and balanced diet (25.9% and 27.0% obese, 21.1% and 22.6% overweight, respectively). Underweight and normal weight had a bigger difference between who had an unhealthier and a healthier diet (23.5% and 30.6% underweight, 21.6% and 30.9% normal weight, respectively). Psychological conditions of obese and overweight may have had a greater influence on tending to eat. These results are supported by numerous studies [10,[42], [43], [44]].
Participants reported an increase in consumption of fresh fruit and vegetables, protein sources such as eggs, milk, and red meat; while they reported a decrease in consumption of junk food such as biscuits, chips, chocolates, and carbohydrates such as pastries, syrupy desserts and bread. During the COVID-19 pandemic, other studies, as opposed to this study, found that people consumed more unhealthy food and less fresh fruit vegetables. Sidor et al. [10] observed that the more adults increase their BMI, they eat the less fruit, vegetables, and the more meat, dairy products, and fast food. However, the study in Poland was conducted for a period of 6 weeks of lockdown. Nevertheless, the longest quarantine in Turkey has lasted four days (with the weekend included). This allowed more accessible fresh fruits and vegetables to all, and reduced the consumption of fast food.
In addition, during the quarantine period, markets were not closed and individuals were allowed to shop at places within walking distance. Moreover, people find more time to cook at home because of working at home, and this reduces the consumption of ready-to-eat food.
The first case in Turkey was later compared to other countries and this increased awareness on healthy nutrition. Even before COVID-19, in Turkey reported a higher consumption of fresh vegetables and fruits compared to other countries [45]. This is associated with the abundance and easily accessible of fresh vegetables and fruit in Turkey. In particular, vegetables and fruits are rich in anti-oxidant and anti-inflammatory compounds such as vitamin C, B vitamins, and polyphenols. Many studies reported these compounds improve health [[46], [47], [48]].
Therefore, the consumption of high-quality nutrients is important against viral infections. This study showed that underweights have the highest consumption of fresh vegetables and fruit, eggs and milk (Fig. 3). In Italy, a study found that during lockdown, the population preferred Mediterranean diet and healthy nutrients, especially people with a low BMI [49]. These results, as this study, observed that people are looking for healthier foods.
The study showed that, surprisingly, participants reduced the consumption of carbohydrate-rich foods. Stress and quarantine, in contrast to this study, show an increase in the consumption of carbohydrate-rich foods [10,44,50].
However, in a similar study, reported that adults reduced carbohydrate-rich foods during quarantine [51].
5. Conclusion
The COVID-19 pandemic, lifestyle changes and psychological conditions affected eating habits. During this emergency it was assessed the changes of weight and eating habits, due to factors such as working at home, digital education at home, change in physical activity habits, and alteration of sleep hours of Turkish individuals. Furthermore, in the study there were differences in food intake and emotional eating between obese and normal weight individuals. Participants reported an increased food intake and the majority are emotional eater at different levels; the obese ones have a higher emotional eating score. Sudden lifestyle changes and the increase in stress levels may affect emotional eating behavior. The study surprisingly reported that participants reduced the consumption of carbohydrate-rich foods, and especially underweight preferred nutrients of high quality.
In conclusion, the study showed the emotional eating behaviors, changes in weight, appetite, and eating habits of Turkish individuals during the COVID-19. However, as the pandemic is still ongoing, the data is an example for further research.
The study has some limitations. The data was collected through an online questionnaire. The conventional face to face interviews could not be applied because of pandemic precautions (travel restriction etc.) therefore online survey was chosen. Body weight and height information were obtained according to the statements of the participants.
Statement of authorship
All authors planned and discussed the results of this study. All authors have approved the final article.
Funding
The author received no specific funding for this work.
Declaration of competing interest
The authors have declared that no competing interests exist.
References
- 1.Velavan T.P., Meyer C.G. The COVID-19 epidemic. Trop Med Int Health. 2020;25:278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Republic of Turkey Ministry of Health . 2021. Turkey COVID-19 patient table. [Google Scholar]
- 3.Turkish Academy of Sciences . 2020. COVID-19 global outbreak evaluation report. [Google Scholar]
- 4.Batlle-Bayer L., Aldaco R., Bala A., Puig R., Laso J., Margallo M., et al. Environmental and nutritional impacts of dietary changes in Spain during the COVID-19 lockdown. Sci Total Environ. 2020;748:141410. doi: 10.1016/j.scitotenv.2020.141410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodríguez-Martín B.C., Meule A. Food craving: new contributions on its assessment, moderators, and consequences. Front Psychol. 2015;6 doi: 10.3389/fpsyg.2015.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yılmaz C., Gökmen V. Neuroactive compounds in foods: occurrence, mechanism and potential health effects. Food Res Int. 2020;128:108744. doi: 10.1016/j.foodres.2019.108744. [DOI] [PubMed] [Google Scholar]
- 7.Ma Y., Ratnasabapathy R., Gardiner J. Carbohydrate craving: not everything is sweet. Curr Opin Clin Nutr Metab Care. 2017;20:261–265. doi: 10.1097/MCO.0000000000000374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muscogiuri G., Pugliese G., Barrea L., Savastano S., Colao A. Obesity: the “achilles heel” for COVID-19? Metabolism. 2020;108:154251. doi: 10.1016/j.metabol.2020.154251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sidor A., Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. 2020;12:1657. doi: 10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reyes-Olavarría D., Latorre-Román P.Á., Guzmán-Guzmán I.P., Jerez-Mayorga D., Caamaño-Navarrete F., Delgado-Floody P. Positive and negative changes in food habits, physical activity patterns, and weight status during COVID-19 confinement: associated factors in the Chilean population. Int J Environ Res Publ Health. 2020;17:1–14. doi: 10.3390/ijerph17155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evers C., Dingemans A., Junghans A.F., Boevé A. Feeling bad or feeling good, does emotion affect your consumption of food? A meta-analysis of the experimental evidence. Neurosci Biobehav Rev. 2018;92:195–208. doi: 10.1016/j.neubiorev.2018.05.028. [DOI] [PubMed] [Google Scholar]
- 13.van Strien T. Causes of Emotional eating and matched treatment of obesity. Curr Diabetes Rep. 2018;18(6) doi: 10.1007/s11892-018-1000-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Risica P.M., Nelson T., Kumanyika S.K., Camacho Orona K., Bove G., Odoms-Young A.M., et al. Emotional eating predicts weight regain among black women in the SisterTalk Intervention. Obesity. 2021;29:79–85. doi: 10.1002/oby.23045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shriver L.H., Dollar J.M., Calkins S.D., Keane S.P., Shanahan L., Wideman L. Emotional eating in adolescence: effects of emotion regulation, weight status and negative body image. Nutrients. 2021;13:1–12. doi: 10.3390/nu13010079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav Immun. 2020;87:23–24. doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Publ Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lemeshow S., Hosmer D.W., Klar J., Lwanga S.K., World Health Organization . Wiley; Chichester: 1990. Adequacy of sample size in health studies; p. 95p. [Google Scholar]
- 19.Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attinà A., Cinelli G., et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;(1):229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garaulet M., Canteras M., Morales E., López-Guimera G., Sánchez-Carracedo D., Corbalán-Tutau M.D. Validation of a questionnaire on emotional eating for use in cases of obesity: the Emotional Eater Questionnaire (EEQ) Nutr Hosp. 2012;27:645–651. doi: 10.1590/S0212-16112012000200043. [DOI] [PubMed] [Google Scholar]
- 21.Arslantaş H., Dereboy F., Yüksel R., İnalkaç S. Duygusal yeme ölçeği’nin türkçe çevirisinin geçerlik ve güvenirlik çalışması. Türk Psikiyatri Derg. 2019;30:122–130. doi: 10.5080/u23520. [DOI] [PubMed] [Google Scholar]
- 22.Spor Alpar R. Detay Yayıncılık; Ankara: 2016. Sağlık ve eğitim bilimlerinden örneklerle uygulamalı istatistik ve geçerlik-güvenirlik. [Google Scholar]
- 23.Al-Musharaf S. Prevalence and predictors of emotional eating among healthy young Saudi women during the COVID-19 pandemic. Nutrients. 2020;12:2923. doi: 10.3390/nu12102923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abbas A.M., Kamel M.M. Dietary habits in adults during quarantine in the context of COVID-19 pandemic. Obes Med. 2020;19:100254. doi: 10.1016/j.obmed.2020.100254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Antunes R., Frontini R., Amaro N., Salvador R., Matos R., Morouço P., et al. Exploring lifestyle habits, physical activity, anxiety and basic psychological needs in a sample of Portuguese adults during COVID-19. Int J Environ Res Publ Health. 2020;17:1–13. doi: 10.3390/ijerph17124360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dohle S., Hartmann C., Keller C. Physical activity as a moderator of the association between emotional eating and BMI: evidence from the Swiss Food Panel. Psychol Health. 2014;29:1062–1080. doi: 10.1080/08870446.2014.909042. [DOI] [PubMed] [Google Scholar]
- 28.Palmer C.A., Alfano C.A. Sleep and emotion regulation: an organizing, integrative review. Sleep Med Rev. 2017;31:6–16. doi: 10.1016/j.smrv.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Bennett J., Greene G., Schwartz-Barcott D. Perceptions of emotional eating behavior. A qualitative study of college students. Appetite. 2013;60:187–192. doi: 10.1016/j.appet.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 30.Tan C.C., Chow C.M. Stress and emotional eating: the mediating role of eating dysregulation. Pers Indiv Differ. 2014;66:1–4. [Google Scholar]
- 31.Hearon B.A., Utschig A.C., Smits J.A.J., Moshier S.J., Otto M.W. The role of anxiety sensitivity and eating expectancy in maladaptive eating behavior. Cognit Ther Res. 2013;37:923–933. [Google Scholar]
- 32.Sevincer G., Konuk N. Emotional eating. J Mood Disord. 2013;3:171. [Google Scholar]
- 33.Adriaanse M.A., de Ridder D.T.D., Evers C. Emotional eating: eating when emotional or emotional about eating? Psychol Health. 2011;26:23–39. doi: 10.1080/08870440903207627. [DOI] [PubMed] [Google Scholar]
- 34.Lazarevich I., Irigoyen Camacho M.E., Velázquez-Alva M. del C., Zepeda Zepeda M. Relationship among obesity, depression, and emotional eating in young adults. Appetite. 2016;107:639–644. doi: 10.1016/j.appet.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Snoek H.M., Van Strien T., Janssens J.M.A.M., Engels R.C.M.E. Emotional, external, restrained eating and overweight in Dutch adolescents. Scand J Psychol. 2007;48:23–32. doi: 10.1111/j.1467-9450.2006.00568.x. [DOI] [PubMed] [Google Scholar]
- 36.Quakenbush M., Anstrom C. Emotional eating (EE) trends of students among various stress levels, levels of restrained eating, genders, majors, and extracurricular ınvolvement. J Acad Nutr Diet. 2020;120:A23. [Google Scholar]
- 37.Zarrinpar A., Chaix A., Panda S. Daily eating patterns and their impact on health and disease. Trends Endocrinol Metabol. 2016;27:69–83. doi: 10.1016/j.tem.2015.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Larsen S.C., Heitmann B.L. More frequent intake of regular meals and less frequent snacking are weakly associated with lower long-term gains in body mass index and fat mass in middle-aged men and women. J Nutr. 2019;149:824–830. doi: 10.1093/jn/nxy326. [DOI] [PubMed] [Google Scholar]
- 39.Blundell J.E., Gillett A. Control of food intake in the obese. Obes Res. 2001;9:263–270. doi: 10.1038/oby.2001.129. [DOI] [PubMed] [Google Scholar]
- 40.Khan M.A., Moverley Smith J.E. “Covibesity,” a new pandemic. Obes Med. 2020;19:100282. doi: 10.1016/j.obmed.2020.100282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sánchez-Sánchez E., Ramírez-Vargas G., Avellaneda-López Y., Orellana-Pecino J.I., García-Marín E., Díaz-Jimenez J. Eating habits and physical activity of the Spanish population during the COVID-19 pandemic period. Nutrients. 2020;12:2826. doi: 10.3390/nu12092826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bhutani S., Cooper J.A. COVID-19–related home confinement in adults: weight gain risks and opportunities. Obesity. 2020;28:1576–1577. doi: 10.1002/oby.22904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robinson E., Gillespie S., Jones A. Weight-related lifestyle behaviours and the COVID-19 crisis: an online survey study of UK adults during social lockdown. Obes Sci Pract. 2020;6:735–740. doi: 10.1002/osp4.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2021;156:104853. doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.FAO . 2010. Nutrition country profiles: Turkey summary. [Google Scholar]
- 46.Bacchetti T., Turco I., Urbano A., Morresi C., Ferretti G. Relationship of fruit and vegetable intake to dietary antioxidant capacity and markers of oxidative stress: a sex-related study. Nutrition. 2019;61:164–172. doi: 10.1016/j.nut.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 47.Duthie S.J., Duthie G.G., Russell W.R., Kyle J.A.M., Macdiarmid J.I., Rungapamestry V., et al. Effect of increasing fruit and vegetable intake by dietary intervention on nutritional biomarkers and attitudes to dietary change: a randomised trial. Eur J Nutr. 2018;57:1855–1872. doi: 10.1007/s00394-017-1469-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Poniedziałek B., Rzymski P., Pięt M., Gąsecka M., Stroińska A., Niedzielski P., et al. Relation between polyphenols, malondialdehyde, antioxidant capacity, lactate dehydrogenase and toxic elements in human colostrum milk. Chemosphere. 2018;191:548–554. doi: 10.1016/j.chemosphere.2017.10.098. [DOI] [PubMed] [Google Scholar]
- 49.Miranda A.M., Steluti J., Fisberg R.M., Marchioni D.M. Dietary intake and food contributors of polyphenols in adults and elderly adults of Sao Paulo: a population-based study. Br J Nutr. 2016;115:1061–1070. doi: 10.1017/S0007114515005061. [DOI] [PubMed] [Google Scholar]
- 50.Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M., Faith M., Zoller T., et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity. 2020;28:1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Matsungo T.M., Chopera P. The effect of the COVID-19 induced lockdown on nutrition, health and lifestyle patterns among adults in Zimbabwe. BMJ Nutr Prev Health. 2020;3:205–212. doi: 10.1136/bmjnph-2020-000124. [DOI] [PMC free article] [PubMed] [Google Scholar]